Abstract
Latex agglutination has been used to detect capsular polysaccharides from a variety of bacteria in body fluids. A latex agglutination assay was constructed for detection of the poly-γ-d-glutamic acid (γdPGA) capsular polypeptide of Bacillus anthracis in serum from animal models of pulmonary anthrax. The assay was able to detect γdPGA in serum from infected animals at concentrations of 100–200 ng/ml.
Latex agglutination immunoassay for capsular antigen has been used as an aid for diagnosis of infection by encapsulated bacteria such as Group B Streptococcus, Haemophilus influenza type b, Streptococcus pneumonia and Neisseria meningitidis and the encapsulated yeast Cryptococcus neoformans (1, 4). In each instance, the target antigen has been a capsular polysaccharide. Bacillus anthracis is the etiological agent of anthrax. Interestingly, the B. anthracis capsule is a polypeptide composed of poly-γ-d-glutamic acid (γdPGA) (2, 3). In a murine model of pulmonary anthrax serum γdPGA levels were determined to exceed 500 µg/ml during the latter stage of infection (6). Diagnosis of anthrax is problematic because identification by culture of blood or other clinical samples can take several days for a definitive identification. During that time, the clinical disease may progress to the point where successful treatment with antibiotics is very difficult (5). In a previous study, we reported that immunoassay by ELISA for γdPGA in serum can be an effective surrogate for bacterial culture in early diagnosis of pulmonary anthrax (6). However, identification of antigenemia by ELISA can take several hours and requires careful quality control for the reagents. The goal of the present study was to evaluate the extent to which a latex agglutination assay can serve as a substitute for a quantitative ELISA for detection of γdPGA in a manner similar to latex agglutination assays for capsular polysaccharides.
A quantitative ELISA for detection of γdPGA was constructed using the γdPGA mAb F26G3 in the solid capture phase and HRPO-labeled mAb F26G3 as the indicator as described (6). A carbodiimide kit was used to covalently link 0.982 µm diameter carboxylated latex microparticles (Polysciences, Inc.) to mAb F26G3 according to the manufacturer’s directions.
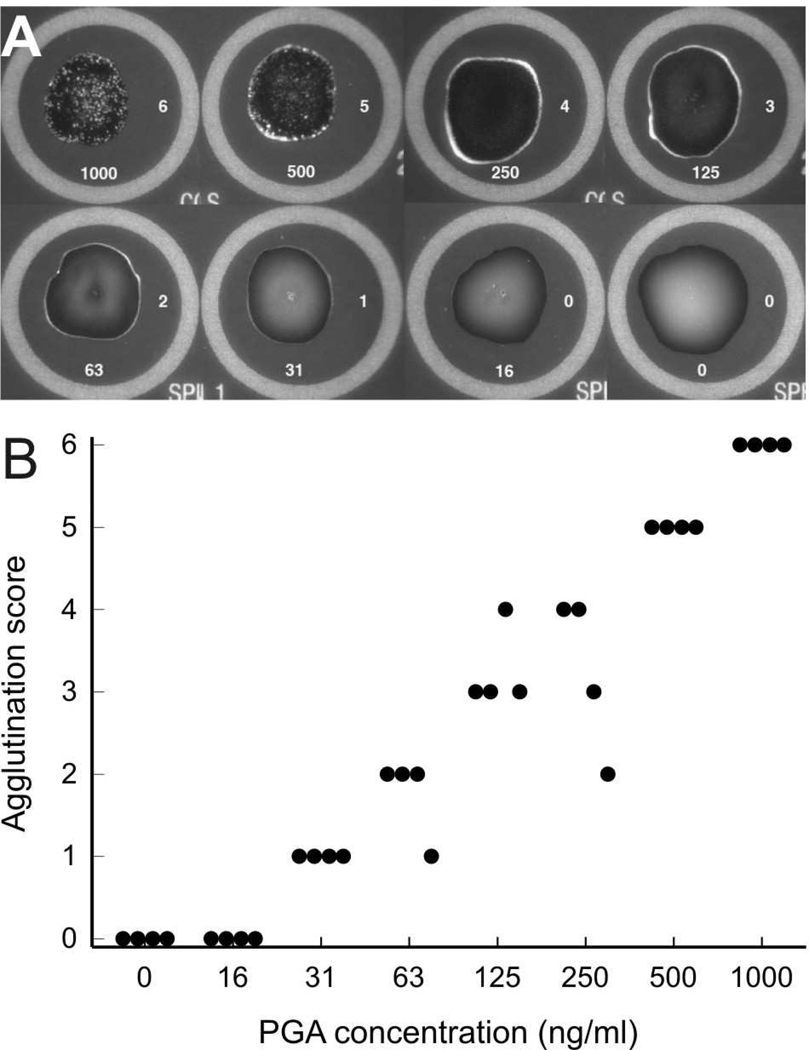
An initial experiment evaluated the extent to which mAb-coated latex beads were agglutinated by purified γdPGA. γdPGA was purified from culture supernatant fluid of B. anthracis (Pasteur) as described (6). The agglutination assay was done by pipetting 20 µl of sample containing γdPGA diluted in phosphate buffered saline (PBS) or negative controls (PBS alone or uninfected samples) onto a Directigen Meningitis Combo Test Card (Becton Dickinson). mAb F26G3-conjugated latex beads (10 µl) were added to the sample, mixed and spread into a larger circle with a diameter of approximately 12 mm. The test card was then rocked in a circular motion for 2 min. As shown in Fig. 1A, the strongest reaction occurred at 1000 ng/ml; this was assigned an agglutination score of 6 (the concentration of PGA is listed below each reaction and the agglutination score is listed to the right of each reaction in Fig 1A). Agglutination begins to accumulate at the outer edge of the sample at 500 ng/ml (score of 5). Between γdPGA concentrations of 250 and 31 ng/ml, the agglutination reaction that forms at the edge of the sample progressively diminishes (score 4−1). No agglutination was evident at 16 ng/ml. This concentration series was tested at least three times with identical results. The ability of four other individuals to independently reproduce the agglutination reactions of the concentration series is shown in Fig. 1B. The observed scores closely tracked the expected agglutination scores shown in Fig. 1A.
Fig. 1.
Panel A – Agglutination of latex beads coated with γdPGA MAb F26G3 by purified γdPGA. The concentration of γdPGA (ng/ml) is indicated at the bottom of each reaction mixture. The agglutination score assigned to each reaction is indicated at the right of each reaction mixture. Panel B – Agglutination reactions were scored in a blind fashion by four individuals. Scoring was based on the images shown in Panel A. Results of scoring for γdPGA at various concentrations by individual readers is shown for each γdPGA concentration.
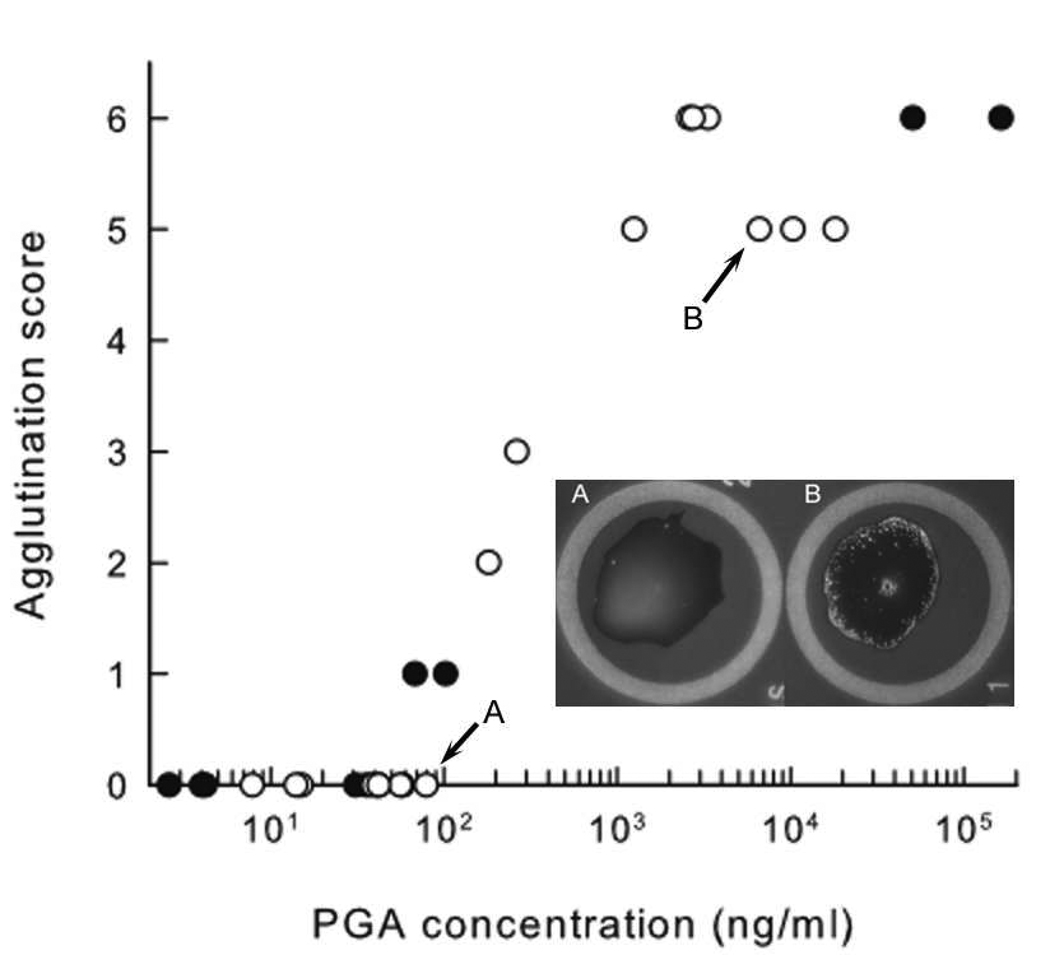
We next evaluated the γdPGA agglutination assay with serum from murine and non-human primate models of pulmonary anthrax. BALB/c mice were infected by the pulmonary route with spores of B. anthracis as described (6). Also, sera from cynomolgus monkeys that were infected via the pulmonary route with B. anthracis spores were also used. The sera were collected at various times after challenge and evaluated by the quantitative ELISA and by the latex agglutination immunoassay. We have previously shown that the concentration of γdPGA in serum (determined by ELISA) with spleen CFU (6). Interestingly, pulmonary anthrax is asynchronous in both animal models due to the fact that dissemination of B. anthracis from the lung is complex (8). As a consequence, plotting antigen concentration as a function of time after challenge does not accurately reflect the extent of disseminated disease in individual animals. Instead, the results are plotted as the latex agglutination score vs. the serum γdPGA concentration as determined by quantitative ELISA for serum samples taken at various times after infection. The results (Fig. 2) showed that γdPGA concentrations as determined by latex agglutination closely tracked results from the quantitative ELISA, with detection of serum γdPGA occurring at 100–200 ng γdPGA per ml serum. Detection of γdPGA at concentrations below 100 ng per ml in serum was variable; there is a slight loss of sensitivity when compared to γdPGA diluted in PBS.
Fig. 2.
Detection of γdPGA by quantitative antigen capture ELISA (X-axis) and by latex agglutination (Y-axis) in serum from murine (●) and non-human primate (○) models of pulmonary anthrax. Mice and cynomolgus monkeys were challenged by the pulmonary route with lethal doses of B. anthracis spores. Blood was collected at various times after challenge and assayed for γdPGA. Each data point represents a single serum sample that was analyzed by both the ELISA (PGA concentration) and by latex agglutination (Agglutination score). Results from the latex agglutination immunoassay of undiluted sera are reported as the agglutination score as described in Fig. 1A. Two agglutination reactions are shown that correspond to the samples labeled A and B.
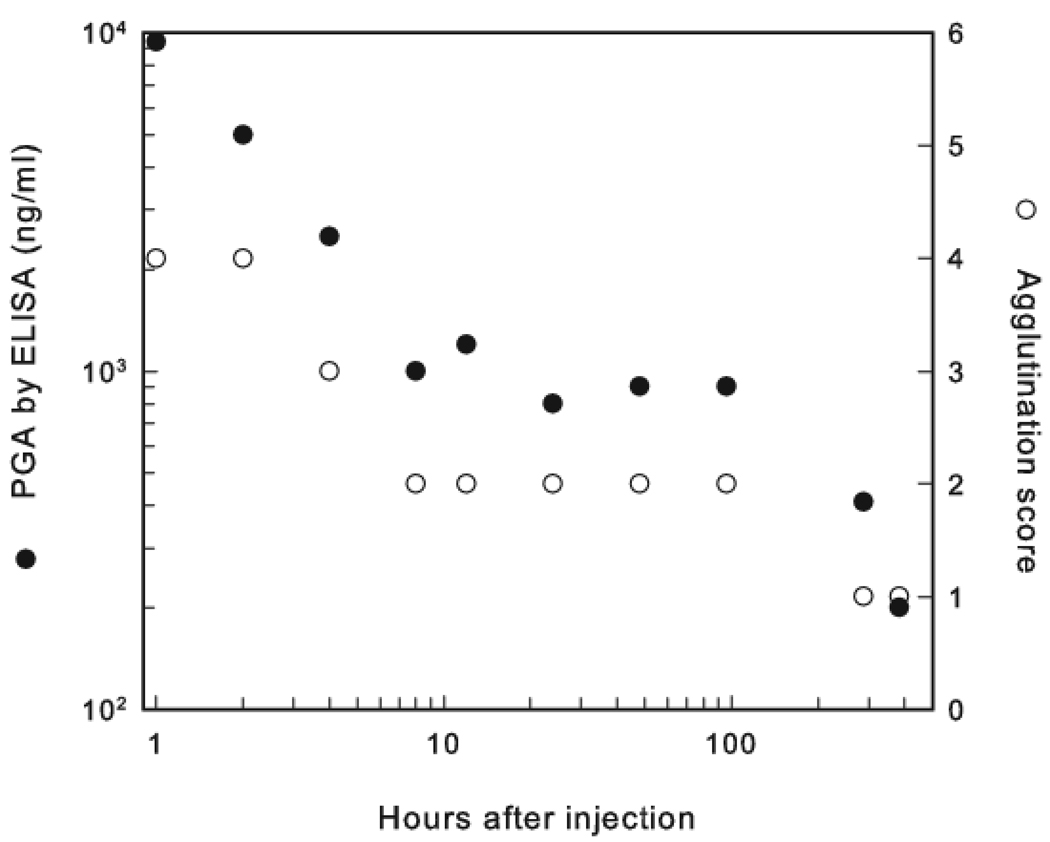
Our previous studies in mice and an addition study in rabbits determined that injected γdPGA is degraded in vivo and shed into the urine (9, 10). As a consequence, this study evaluated the ability of the latex agglutination assay to detect degraded γdPGA in urine. BALB/c mice were injected via the intravenous route with 500 µg γdPGA, and urine was collected at various times after treatment. Concentrations of γdPGA in the urine were determined by the quantitative ELISA, and agglutination of the latex beads was assessed as described in Fig. 1. As shown in Figure 3, urine samples collected after 1 and 2 h showed γdPGA concentrations of 9,400 and 5,000 ng/ml, respectively. However, the agglutination score was only 4. A similar loss of sensitivity was observed with the remaining urine samples. Compared to testing the urine samples by ELISA, the sensitivity of the latex agglutination assay decreased in each sample by a minimum of 15-fold. By ELISA six of the urine samples had γdPGA concentrations of between 800–1200 ng/ml; in serum or PBS these concentrations would produce an agglutination rank of five or six but in urine they produced a rank of two. In a previous report we determined that the ELISA has shown a decrease in sensitivity in detecting short γdPGA 25-mers like those found in urine (10). Therefore, the loss in sensitivity of the latex agglutination assay is probably underestimated. There was no loss in sensitivity of the latex agglutination assay when naïve BALB/c urine was spiked with purified native γdPGA, ruling out the possibility of an inhibitor in the urine (data not shown).
Fig. 3.
Detection of γdPGA in urine of mice that were injected by the intravenous route with 500 µg γdPGA. Urine was collected at various times after treatment and analyzed by the quantitative ELISA (Y-axis, left - •) and by latex agglutination (Y-axis axis, right - ◦). Latex agglutination scores were determined with undiluted samples as described in Fig. 1A.
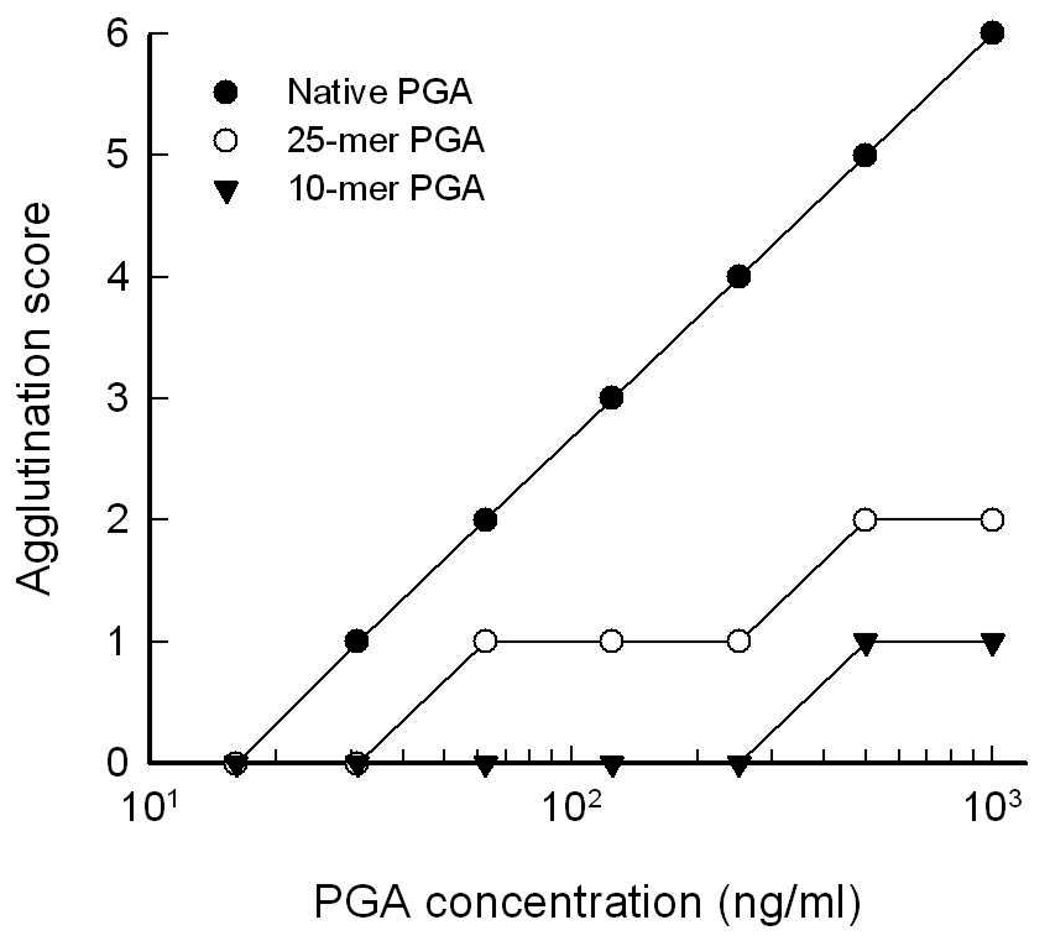
In an effort to assess the impact of molecular size of γdPGA on the sensitivity of the latex agglutination assay, latex agglutination scores were evaluated for various concentrations of native purified γdPGA as well as synthetic 25-mer (3.5 kD) and 10-mer (1.3 kD) γdPGA. Synthetic γdPGA was prepared as described (7). The results (Fig. 4) showed a substantial loss of sensitivity of the latex agglutination assay for detection of the 25-mer compared with native γdPGA. The latex agglutination assay had little ability to detect the 10-mer. These results suggest that the presence of partially degraded γdPGA in urine accounts for the decreased sensitivity of the latex agglutination assay in γdPGA-treated mice.
Fig. 4.
Agglutination of latex beads coated with γdPGA MAb F26G3 by various concentrations of native γdPGA and synthetic γdPGA of 10 or 25 amino acids. Concentrations of γdPGA were determined from the dry weight of each antigen. Latex agglutination was scored as described in Fig. 1A.
Our results indicate that purified γdPGA and γdPGA in serum from murine and non-human primate models of pulmonary anthrax is readily detected by a latex agglutination immunoassay constructed with a mAb that is specific for γdPGA. In contrast, latex agglutination is less effective in detection of smaller molecular weight fragments of γdPGA that might be found in urine.
Acknowledgement
This study was supported by Public Health Service grants R01-AI059348 and U01-AI061200 from the National Institute of Allergy and Infectious Diseases. Synthesis of γdPGA was supported by NIH Grant P20 RR-016464 from the INBRE Program of the National Center for Research Resources.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Literature cited
- 1.Bloomfield N, Gordon MA, Elmendorf DF., Jr Detection of Cryptococcus Neoformans Antigen in Body Fluids by Latex Particle Agglutination. Proc Soc Exp Biol Med. 1963;114:64–67. doi: 10.3181/00379727-114-28586. [DOI] [PubMed] [Google Scholar]
- 2.Bruckner V, Kovacs J, Denes G. Structure of poly-D-glutamic acid isolated from capsulated strains of B. anthracis. Nature. 1953;172:508. doi: 10.1038/172508a0. [DOI] [PubMed] [Google Scholar]
- 3.Bruckner V, Kovacs J, Nagy H. The Structure of Native Poly-D-glutamic Acid. Part III. J. Chem. Soc. 1953:148–150. [Google Scholar]
- 4.Gill VJ, Fedorko DP, Witebsky FG. The clinician and the microbiology laboratory. vol. 1. Elsevier Inc.; 2005. [Google Scholar]
- 5.Inglesby TV, O'Toole T, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Friedlander AM, Gerberding J, Hauer J, Hughes J, McDade J, Osterholm MT, Parker G, Perl TM, Russell PK, Tonat K. Anthrax as a biological weapon, 2002: updated recommendations for management. Jama. 2002;287:2236–2252. doi: 10.1001/jama.287.17.2236. [DOI] [PubMed] [Google Scholar]
- 6.Kozel TR, Murphy WJ, Brandt S, Blazar BR, Lovchik JA, Thorkildson P, Percival A, Lyons CR. mAbs to Bacillus anthracis capsular antigen for immunoprotection in anthrax and detection of antigenemia. Proc Natl Acad Sci U S A. 2004;101:5042–5047. doi: 10.1073/pnas.0401351101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kozel TR, Thorkildson P, Brandt S, Welch WH, Lovchik JA, AuCoin DP, Vilai J, Lyons CR. Protective and immunochemical activities of monoclonal antibodies reactive with the Bacillus anthracis polypeptide capsule. Infect Immun. 2007;75:152–163. doi: 10.1128/IAI.01133-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lyons CR, Lovchik J, Hutt J, Lipscomb MF, Wang E, Heninger S, Berliba L, Garrison K. Murine model of pulmonary anthrax: kinetics of dissemination, histopathology, and mouse strain susceptibility. Infect Immun. 2004;72:4801–4809. doi: 10.1128/IAI.72.8.4801-4809.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roelants GE, Whitten LF, Hobson A, Goodman JW. Immunochemical studies on the poly-gamma-D-glutamyl capsule of Bacillus anthracis. VI. The in vivo fate and distribution to immunized rabbits of the polypeptide in immunogenic and nonimmunogenic forms. J Immunol. 1969;103:937–943. [PubMed] [Google Scholar]
- 10.Sutherland MD, Thorkildson P, Parks SD, Kozel TR. In vivo fate and distribution of poly-gamma-D-glutamic acid, the capsular antigen from Bacillus anthracis. Infect Immun. 2008;76:899–906. doi: 10.1128/IAI.01176-07. [DOI] [PMC free article] [PubMed] [Google Scholar]