Abstract
Objectives. We compared the extent of socioeconomic differences in use of health care services based on wealth (i.e., accumulated assets) as the socioeconomic ranking variable with the extent of differences based on income to explore the sensitivity of the estimates of equity to the choice of the socioeconomic indicator.
Methods. We used data from the Health and Retirement Study in the United States and the Survey of Health, Ageing, and Retirement in Europe to estimate levels of income- and wealth-related disparity in use of physician and dental services among adults 50 or older in 12 countries.
Results. We found socioeconomic differences in use of physician services after standardizing for need in about half of the countries studied. No consistent pattern in levels of disparity measured by wealth versus those measured by income was found. However, the rich were significantly more likely to use dental services in all countries. Wealth-related differences in dental service use were consistently higher than were income-related differences.
Conclusions. We found some support for wealth as a more sensitive indicator of socioeconomic status among older adults than was income. Wealth may thus allow more accurate measurements of socioeconomic differences in use of health care services for this population.
Governments try to protect the population from the financial consequences of ill health by providing health care services on the basis of need and not ability to pay. In Europe, such policies have been implemented at both the national and supranational levels1; in the United States, publicly funded programs such as Medicare, Medicaid, and the State Children's Health Insurance Program strive for similar ends. Distributing health care resources according to need may improve population health and may even reduce the health inequalities that are widespread in high-income countries.2
Analyses based on the concept of the concentration curve, which compares the cumulative distribution of use of health care services with the cumulative distribution of income in a population, consistently reveal, after control for need, that use of health care services is greater among higher-income groups (i.e., a distribution that is more concentrated among the rich) in member countries of the Organisation for Economic Co-Operation and Development (OECD).3,4 Although evidence for income-related differences in use of general practitioner or inpatient services is weaker, evidence exists for significant differences, by income, in the probability and number of specialist physician and dentist visits in almost all OECD countries.3,4 Studies that focused on older populations also revealed evidence of differences in use of health care services by income5–9 and education.10 In the United States, income-related differences in use of health care services appear to be greatest among those 65 years and older.11
Research on health inequalities in later life is complicated by “survival selection” caused by structural inequalities in society.12 Some population subgroups (e.g., manual workers) have higher-than-average mortality and morbidity rates; in such groups, late-life survivors, by being healthier than those who have died, are not representative of the group. Therefore, researchers expect health inequalities across socioeconomic groups to narrow with age.
Another complicating factor is the difficulty of measuring socioeconomic status (SES) in later life.12 Among people who are retired, income and occupation status lose their significance, and wealth (i.e., accumulated economic assets) becomes more important.13–17 One indicator of wealth, home ownership without debt, is important to consider in this connection because it effectively substitutes income that would otherwise be spent on rent or mortgage payments for income that is spent on health care.18 The level of highest educational attainment is also an important indicator of SES.15 There is likely a dynamic relationship between education and wealth, such that those who are better educated will also be able to accumulate more wealth by having higher levels of income, savings, and investment. One would therefore expect SES to be incorrectly measured if wealth is not considered.18 Indeed, a study measuring the effects of housing assets on health status among those 55 years and older in Spain found that assets (but not income) were significantly and positively associated with better self-reported health and that inequalities in health were almost completely explained by differences in housing wealth.19
Because population rankings based on income differ from those based on wealth, analyses of socioeconomic health inequalities and socioeconomic differences in use of health care services will yield different results depending on which indicator is chosen as the ranking indicator for SES. Among the retired population, levels of income are likely to vary much less than levels of wealth, as is shown in the descriptive analysis of the Health and Retirement Study (HRS).20 In addition, when comparing retired and employed groups, income is less comparable than broader measures of wealth. But there has been no attempt yet to systematically investigate differences in use of health care services using wealth as the ranking variable instead of income.
In our study, we addressed the following question: Are socioeconomic differences in use of health care services greater when they are measured by wealth than by income? We hypothesized that wealth would be a more sensitive indicator of socioeconomic status than would income in a population in which many people are retired. Therefore, differences in use by wealth were expected to be greater than were differences by income.
METHODS
Data and Variables
We used data from the first wave (2004) of the Survey of Health, Ageing and Retirement in Europe (SHARE), which studied populations in 11 European nations: Austria, Belgium, France, Denmark, Greece, Germany, Italy, the Netherlands, Spain, Sweden, and Switzerland. Our US data came from the 2004 wave of the HRS.21 SHARE is modeled after the HRS, although it is administered annually and the HRS is administered biennially. These surveys examine the health and living conditions of people 50 years and older. The 2004 wave of SHARE had a relatively low overall response rate of 62% (ranging from 38% in Switzerland to 74% in France), in part because 2004 was the first year the survey was administered. Still, this response rate is comparable to response rates for other European surveys.21 The overall response rate for the HRS in 2004 was 86%. To compensate for nonresponse, we used sampling weights as provided for both surveys.
We measured use of health care services as the likelihood of a doctor visit or dentist visit, as well as the number of doctor visits. In SHARE, doctor visits were measured by answers to this question: “In the past 12 months, about how many times in total have you seen or talked to a medical doctor about your health? Please exclude dentist visits and hospital stays, but include emergency room or outpatient clinic visits.” Dentist visits were measured by answers to this question: “During the last 12 months, have you seen a dentist or dental hygienist?” In HRS, doctor visits were elicited by this question: “In the last 2 years/since the previous wave, aside from any hospital stays and outpatient surgery, how many times have you seen or talked to a medical doctor about your health, including emergency room or clinic visits?” We divided the total number of visits by 2 to estimate the number of yearly doctor visits; however, for our sensitivity analyses, we calculated the number of doctor visits as 75% of the 2-year number. Dentist visits were elicited by this question: “In the last 2 years/since the previous wave, have you seen a dentist for dental care, including dentures?”
The explanatory variables used in the models predicting health care utilization included health, demographic, and socioeconomic factors (Appendix Table A1, available as a supplement to the online version of this article at http://www.ajph.org). Need for health care services was measured by age category (in years; 50–59, 60–69, 70–79, ≥ 80), gender, and health status. Self-assessed health was reported as excellent (reference category), very good, fair, poor, or very poor. We included self-reported activity limitations, categorized as no limitations, moderate limitations (defined in the United States as limitations in 1–2 activities of daily living; defined in SHARE as “limited, but not severely” because of health problems), or severe limitations (defined in the United States as limitations in 3 or more activities of daily living; defined in SHARE as “severely limited” because of health problems). Also included was whether the respondent reported any chronic condition or was permanently sick or disabled (the latter was based on a question about current employment). Need for dental care was measured by age, using the same 4 categories listed for health care services. For the European countries we also included whether the respondent wore dentures and could bite hard foods without difficulty, 2 variables that have been used to indicate need for dental care.22
Variables not related to the need for health care services included whether the respondent was retired, unemployed, or a homemaker; whether the respondent smoked or used to smoke; and whether the respondent lived alone. We quantified education with a slightly modified version of the International Standard Classification of Education (ISCED), grouping its 7 levels into 6: preprimary and primary education; lower secondary education; (upper) secondary education; postsecondary nontertiary education; first stage of tertiary education; second stage of tertiary education. For some countries, not all levels of education were relevant. In the United States, the educational categories were: no degrees or unknown (reference category; considered equivalent to ISCED level 2), high school diploma (equivalent to ISCED level 3), college degree (2 or 4 years; equivalent to ISCED level 4), master's degree (equivalent to ISCED level 5), and professional degree (equivalent to ISCED level 6). We also included quintiles of income and quintiles of assets.
Our analysis included coverage by voluntary private health insurance, defined as benefits that supplemented a statutory benefits package, such as direct access to specialists; dental care; coverage of user charges for drugs, hospitalization, or other costs; a larger choice of drugs; and long-term care. In Germany and the Netherlands, where substitutive insurance (private insurance that substitutes for public insurance) was available for high-income earners in 2004, 2 voluntary private health insurance variables were included: one to capture voluntary private health insurance, and another to capture supplementary private health insurance. For the United States, we included dummy variables indicating whether the respondent was covered by Medicare, Medicaid, or private medical insurance. The reference category in the United States was the uninsured. The possible endogeneity of private medical insurance or voluntary private health insurance was largely offset by the inclusion of a comprehensive set of health-status variables.23
We measured income as the sum of income from employment, self-employment, pension, regular private transfers (e.g., alimony), long-term care, and capital assets income (interest from bank accounts, bonds, stocks or shares, or mutual funds) at the household level. We used the modified OECD equivalence scale to calculate individual income for equivalent adults.24 We measured wealth as the sum of household income plus total assets (also referred to as net worth). We defined total assets as the sum value of the primary residence net of mortgage, value of other real estate, owned share of own business, owned cars, and the value of financial assets (bank accounts, government and corporate bonds, stocks, mutual funds, individual retirement accounts, and contractual savings for housing and life insurance policies owned by the household) minus financial liabilities.
Data Analysis
We modeled the probability of at least 1 doctor or dentist visit by means of separate logistic regression models for the full set of explanatory variables. For physicians, we also modeled the number of visits made by individuals who had at least 1 visit, i.e., the number of visits conditional on use of physician services. We used a negative binomial regression model for the number of physician visits because of its count nature and skewed distribution.25
We then calculated “horizontal inequity” of use of physician services, a measure based on the concept of the concentration curve.26,27 We defined horizontal inequity as the degree to which use of health care services was related to SES once differences in need by SES were controlled. Horizontal inequity was calculated separately both by income and by wealth for each country. We compared the distribution of use of physician services with the distributions of income and of wealth separately (ranked in ascending order) to obtain the concentration index (i.e., disparity) of unadjusted use of physician services (unadjusted concentration index). Then, based on the estimates of the needs variables from the regression models (holding the non-needs variables at their means), we obtained the concentration index of needs-adjusted use of physician services (adjusted concentration index).
Horizontal inequity (which can range from −1 to 1) was calculated as the difference between the levels of disparity demonstrated in actual use of physician services and needs-adjusted use of physician services. An inequity index of 0 implies that, after control for differences in need across income or wealth groups, all individuals have an equal probability of using health services. A positive horizontal inequity index indicates that after adjusting for need, use of health care services is more concentrated among higher-income or greater-wealth groups. A negative horizontal inequity index implies the opposite.
RESULTS
Levels of health care services utilization in the 12 countries studied are reported in Table 1. The majority of the population in each country reported having made a physician visit in the previous year (ranging from 78% in Sweden to 94% in France). The number of doctor visits conditional on 1 visit ranged from 3.8 visits in the past year in Sweden to more than 10 visits in Italy and Spain. The proportion of the population reporting a recent dentist visit ranged more widely, from 26% in Spain to 77% in Denmark and Sweden. The United States fell at approximately the middle of the 12 countries, both in mean use of physician services in the past 2 years and in the probability of a dentist visit. (Remember that for the United States, the probability of a visit covered a 2-year period, as opposed to a 1-year period for the European countries).
TABLE 1.
Sample Sizes and Mean Number of Doctor and Dentist Visits, by Country: Health and Retirement Study, United States, 2004, and Survey of Health, Ageing, and Retirement in Europe, 2004
| Sample Size, No. | Doctor Visits, Conditional Number, Mean (SD) | Doctor Visit, Probability, Mean (SD) | Dentist Visit, Probability, Mean (SD) | |
| Austria | 1828 | 7.44 (9.8) | 0.86 (0.35) | 0.51 (0.50) |
| Belgium | 3626 | 8.99 (10.6) | 0.93 (0.25) | 0.48 (0.50) |
| Denmark | 1585 | 5.31 (8.46) | 0.81 (0.39) | 0.77 (0.42) |
| France | 2937 | 7.52 (7.44) | 0.94 (0.24) | 0.44 (0.50) |
| Germany | 2909 | 8.63 (11.1) | 0.93 (0.37) | 0.73 (0.47) |
| Greece | 2636 | 7.06 (8.13) | 0.79 (0.41) | 0.37 (0.48) |
| Italy | 2473 | 10.65 (13.9) | 0.84 (0.26) | 0.32 (0.45) |
| Netherlands | 2836 | 5.63 (7.96) | 0.82 (0.39) | 0.61 (0.61) |
| Spain | 2300 | 10.42 (13.43) | 0.89 (0.32) | 0.26 (0.49) |
| Sweden | 2972 | 3.83 (4.56) | 0.78 (0.42) | 0.77 (0.42) |
| Switzerland | 932 | 5.7 (8.56) | 0.84 (0.37) | 0.69 (0.46) |
| United States | 18 148 | 5.43 (10.03) | 0.93 (0.25) | 0.66 (0.47) |
Note. In the United States, the measures of utilization were for the past 2 years (and divided by 2 for the mean number of visits); for the other countries, they were the past year.
Table 2 reports the results of the model predicting the probability of a physician visit. (Appendix Table A3, which reports the results of the model for the number of conditional physician visits, is available as a supplement to the online version of this article at http://www.ajph.org.) In general, factors related to health care need were significantly associated with physician visits (see Appendix Table A4, available as a supplement to the online version of this article at http://www.ajph.org.). There was no clear trend toward significance among the non-needs variables. Higher educational attainment significantly increased the odds of visiting a physician in Greece, Spain, Sweden, and the United States. Health insurance facilitated use of physician services in Belgium, France, the Netherlands, and the United States. (In the United States, whereas those enrolled in Medicaid had increased odds of a physician visit, those enrolled in private health insurance had even higher odds of a physician visit.)
TABLE 2.
Adjusted Odds Ratios (ORs) for Socioeconomic Indicators in Models Predicting Likelihood of Doctor and Dentist Visits, by Country: Health and Retirement Study, United States, 2004, and Survey of Health, Ageing, and Retirement in Europe, 2003
| Austria | Belgium | Denmark | France | Germany | Greece | Italy | Netherlands | Spain | Sweden | Switzerland | United States | |
| Likelihood of physician visit | ||||||||||||
| Income and assets | ||||||||||||
| Income quintile 2 | 2.32*** | 0.76 | 0.98 | 1.13 | 1.27 | 0.83 | 1.08 | 1.13 | 1.11 | 1.11 | 1.75* | 1.19 |
| Income quintile 3 | 1.96*** | 1.27 | 1.51 | 0.80 | 1.42 | 0.96 | 1.22 | 1.06 | 1.00 | 1.25 | 2.09** | 1.47*** |
| Income quintile 4 | 1.66** | 1.38 | 1.11 | 1.08 | 2.04*** | 0.82 | 1.56** | 1.07 | 1.12 | 1.10 | 1.76* | 1.61*** |
| Income quintile 5 | 1.70** | 0.92 | 1.02 | 0.97 | 1.79** | 0.86 | 1.47* | 0.94 | 1.16 | 1.24 | 1.72* | 2.09*** |
| Assets quintile 2 | 0.89 | 0.97 | 1.05 | 0.79 | 1.44 | 1.04 | 1.06 | 1.16 | 1.39 | 1.23 | 1.04 | 1.11 |
| Assets quintile 3 | 0.76 | 0.76 | 0.83 | 0.96 | 1.22 | 1.20 | 0.79 | 1.04 | 1.12 | 1.24 | 0.64 | 1.17 |
| Assets quintile 4 | 1.05 | 0.95 | 1.12 | 0.77 | 1.37 | 1.43** | 1.09 | 1.13 | 1.38 | 1.43** | 1.15 | 1.26* |
| Assets quintile 5 | 0.86 | 0.61** | 0.84 | 1.14 | 1.10 | 1.24 | 1.10 | 1.10 | 1.09 | 1.74** | 0.97 | 1.85*** |
| Education and insurance | ||||||||||||
| ISCED 3 | 0.76 | 0.97 | 0.55*** | 0.92 | 1.11 | 1.49* | 1.05 | 1.03 | 1.30 | 0.74** | 1.13 | 1.32*** |
| ISCED 4 | 0.88 | 0.93 | 0.73* | 1.08 | 1.21 | 1.45** | 1.45 | 0.99 | 1.59** | 1.14 | 0.72 | 1.92*** |
| ISCED 5 | 0.58 | 0.89 | 2.06 | 2.86** | 0.52 | 1.81* | 1.32 | 2.67*** | ||||
| ISCED 6 | 1.75*** | 1.24 | 1.13 | 2.59*** | ||||||||
| VHI/Medicare | 1.36 | 2.06*** | 1.42** | 2.07*** | 0.97 | 0.73 | 0.95 | 1.30** | 1.09 | 0.78 | 1.36 | 1.27* |
| VHIb/Medicaid | 0.76 | 1.13 | 1.84*** | |||||||||
| PMI | 2.66*** | |||||||||||
| Likelihood of dentist visit | ||||||||||||
| Income and assets | ||||||||||||
| Income quintile 2 | 1.12 | 1.11 | 1.92*** | 1.11 | 0.97 | 1.07 | 1.49** | 0.93 | 0.56*** | 1.35** | 0.98 | 1.08 |
| Income quintile 3 | 1.08 | 1.11 | 1.33 | 1.10 | 1.01 | 1.12 | 1.30 | 1.01 | 0.79 | 1.97*** | 1.80** | 1.36*** |
| Income quintile 4 | 1.04 | 1.28** | 1.26 | 1.49*** | 1.09 | 1.02 | 1.36* | 1.05 | 1.02 | 1.61*** | 1.94** | 1.75*** |
| Income quintile 5 | 1.18 | 1.38*** | 1.05 | 1.45*** | 0.96 | 1.30* | 1.64*** | 0.91 | 0.99 | 1.98*** | 1.56* | 2.15*** |
| Asset quintile 2 | 1.16 | 1.42*** | 1.79*** | 1.12 | 1.87*** | 1.00 | 1.14 | 1.35* | 0.88 | 1.40** | 1.48 | 1.10 |
| Asset quintile 3 | 1.10 | 1.58*** | 2.18*** | 1.28 | 1.56*** | 1.34** | 1.21 | 1.53*** | 1.15 | 1.48** | 1.50 | 1.79*** |
| Asset quintile 4 | 1.14 | 1.88*** | 2.70*** | 1.60*** | 2.33*** | 1.27 | 1.15 | 1.55*** | 1.30 | 1.90*** | 1.63* | 2.68*** |
| Asset quintile 5 | 1.62*** | 1.92*** | 2.68*** | 1.38** | 2.78*** | 1.17 | 1.29 | 1.80*** | 1.12 | 1.55** | 2.33** | 3.44*** |
| Education and insurance | ||||||||||||
| ISCED 3 | 0.48*** | 0.59*** | 0.42*** | 0.84* | 0.53*** | 1.44** | 1.38** | 0.88 | 0.98 | 1.37** | 0.66** | 1.81*** |
| ISCED 4 | 0.63*** | 0.68*** | 0.56*** | 0.90 | 1.03 | 1.43*** | 1.75*** | 1.01 | 1.10 | 1.88*** | 0.99 | 3.11*** |
| ISCED 5 | 0.82 | 0.97 | 1.15 | 2.42** | 1.83*** | 2.43*** | 4.45*** | |||||
| ISCED 6 | 2.22*** | 1.91 | 1.45** | 4.41*** | ||||||||
| VHI/Medicare | 1.54*** | 1.34*** | 2.18*** | 1.22* | 0.89 | 1.17 | 1.24 | 1.39*** | 2.14*** | 1.90*** | 1.28 | 0.94 |
| VHIb/Medicaid | 0.93 | 1.92*** | 1.10 | |||||||||
| PMI | 1.68*** | |||||||||||
Note. ISCED = International Standard Classification of Education; VHI = voluntary private health insurance; VHIb = supplementary heath insurance; PMI = private medical insurance. ISCED numbers refer to highest education level achieved.
*P ≤ .10; **P ≤ .05; ***P ≤ .01.
Only Austria and the United States demonstrated a positive relationship between income and the probability of a physician visit. (Appendix Table A3, available as a supplement to the online version of this article at http://www.ajph.org, shows that Austria and the United States also demonstrated a positive relationship between income and the conditional number of physician visits.) In Greece and Sweden, being in the third or fourth asset quintile (with the fifth quintile being the highest) was associated with increased odds of a physician visit. However, in interpreting these results, it is important to note that because there is large heterogeneity in sample sizes, a relevant odds ratio might not be statistically significant in countries with a small sample size.
Socioeconomic factors related to the likelihood of a dentist visit are shown in Table 2. The odds of a dentist visit increased with the level of education in most countries, especially in Greece, Italy, Sweden, and the United States. In almost all countries, the odds of visiting a dentist were higher for richer individuals, both in terms of income and wealth. Wealth had a stronger, more significant effect on dentist visits than income in Belgium, Denmark, Germany, the Netherlands, and the United States.
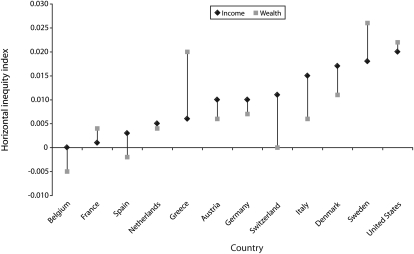
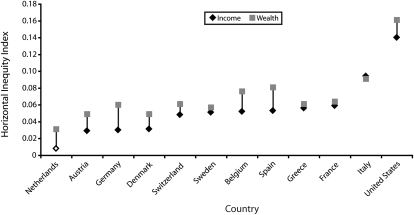
The analysis of horizontal inequity revealed significant differences by income and wealth in the likelihood of a physician visit in about half of the countries studied. There was an even greater difference in the likelihood of a dentist visit in all countries. Regarding the probability of a physician visit, there was no clear pattern demonstrating whether differences related to income were more or less prevalent than differences related to wealth. In some countries, wealth-related difference was greater (Greece, Sweden, and the United States), whereas for others it was lower (Belgium, Spain, Austria, Germany, Switzerland, Italy, and Denmark; Figure 1). Levels of disparity were higher for dentist services than for physicians across the board (Figure 2). (Note that the scales of Figures 1 and 2 differ.) Use of dental care was more inequitable than was use of physician visits when wealth, instead of income, was the ranking variable in all but 1 of the countries.
FIGURE 1.
Inequity in the probability of a doctor visit related to income and wealth in 12 countries: Health and Retirement Study, United States, 2004, and Survey of Health, Ageing, and Retirement in Europe, 2004.
Note. Horizontal inequity in the probability of a visit to the doctor was significantly different from zero for socioeconomic status measured by wealth in Greece, income in Italy and Denmark, and both income and wealth in Germany, Sweden, and the United States (P < .05).
FIGURE 2.
Inequity in the probability of a dentist visit by income and wealth in 12 countries: Health and Retirement Study, United States, 2004, and Survey of Health, Ageing, and Retirement in Europe, 2004.
Note. All horizontal inequity indices were significantly different from zero at P < .05, except for socioeconomic status measured by income in the Netherlands.
Sensitivity analyses testing the effects of redefining use of physician services in the past year in the United States as 0.75 (vs one half) of the 2-year utilization level caused no substantive changes in the results. We also tested whether excluding assets from the models of utilization changed the effects of income on use of physician services. The effects of that change were negligible, even in the countries with correlations between income and assets greater than 30%.
We also ran the analyses with only the population 65 years and older to test whether the effect of using wealth as opposed to income as the ranking variable would be stronger in a more homogeneous and noneconomically active group. In the United States, results for this population revealed slightly lower levels of disparity for doctor visits and slightly higher levels of disparity for dentist visits than were found in the full specification. For dental care, the gap between socioeconomic differences by wealth and differences by income was slightly greater in this population (the index of inequity by income was 0.16 and by wealth was 0.19), though no gap in disparity was found in the analysis of doctor visits. The gap between income-related disparity and wealth-related disparity in the probability of a doctor visit increased for this population only in Sweden (0.02 for differences by income and 0.035 for differences by wealth), whereas for dentist visits this population exhibited a greater difference in Belgium (0.07 for differences by income, 0.11 for differences by wealth), France (0.09 for differences by income, 0.10 for differences by wealth), and Spain (0.05 for differences by income, 0.10 for differences by wealth). The results of this sensitivity analysis were not robust in countries with small sample sizes (e.g., Switzerland).
We also tested the correlation between the rank of income and the rank of wealth, which ranged from 30% to 65% and was only slightly higher than the correlation between absolute levels of income and wealth in most countries (see Appendix Table A2, available as a supplement to the online version of this article at http://www.ajph.org.). Despite a change in population rankings (only 2 countries had a correlation higher than 50%), there was only a small change in the findings.
DISCUSSION
We expected that wealth, as opposed to income, would better capture variations in financial security and socioeconomic position among adults 50 years and older, a large proportion of whom are retired. To test this hypothesis, we assessed the roles of income and wealth in predicting use of physician and dentist services, then we examined whether differences in use of health care services were greater when ranking populations by wealth than by income. The analyses of use of physician services did not support our hypothesis, but the analyses of use of dentist services did.
A significant (though small in magnitude) disparity in the likelihood of a physician visit was found in about half the countries studied. The levels of disparity found in the United States, Sweden, Greece, and Italy were about 2 to 3 times higher than those found in the other countries. For the number of physician visits among those who had at least 1 visit, disparities were only found in the United States and Switzerland—the 2 countries with the heaviest reliance on private sources of financing in terms of private health insurance and patient cost-sharing.
Consistent with previous studies of the general population,3 separate analyses of use of general practitioner services and of specialist services revealed disparity in specialist care, particularly for the probability of a visit, but little evidence of disparity for general practitioner care (results not reported here). (These analyses were not run for the United States because the HRS did not distinguish between the 2 groups.) Measuring socioeconomic disparity by wealth as opposed to measuring it by income did not reveal a consistent pattern in disparities in use of physician services, suggesting that the choice of the ranking variable does not affect results of analyses for differences in use of physician services. Although the level of disparity was twice as high for wealth as for income in Greece and one third higher in Sweden, the level of disparity by income was twice as high as disparity by wealth in Denmark and Switzerland.
In most countries, greater wealth predicted dentist use more strongly than did higher income. Moreover, significant socioeconomic differences in the probability of visiting a dentist were found for all countries; in most, the level of disparity related to wealth was higher than that related to income. For the probability of a dentist visit, levels of disparity by wealth were twice as high as difference by income in Germany, 3 times as high in the Netherlands, and about 1.5 times as high in Austria, Belgium, Denmark, and Spain. In the United States, the level of disparity in dentist visits was much higher than in the other countries, and difference by wealth was 15% greater than difference by income.
Therefore, the choice of socioeconomic ranking variable (wealth vs income) appears to have affected the findings, despite being moderately to strongly correlated. The finding of higher disparity in dental care than in physician care is consistent with previous studies.3,28,29 We expected that wealth would have a stronger effect than income on the decision to use services that require more patient cost-sharing, because assets such as home ownership without debt create disposable income that can be used to pay such fees. The finding that wealth-related difference is greater than income-related difference in dental care—the most privatized sector of health care in each of the 12 countries we studied––provides some support for this hypothesis.
Limitations
Our findings should be interpreted in light of the study's limitations. The SHARE survey's response rates were low in some countries, and sample sizes were relatively small. Also, SHARE's limitation to 1 year of data did not permit us to estimate the extent of selection bias. In addition, although the sample included a large proportion of older age groups, only part of the institutionalized population was included. Individuals represented by the survey were likely healthier than were those in institutions—and wealthier, in some countries, because of the ability to afford private care. Both possibilities would lead to an underestimation of difference by reducing the sample's variability in both health status and wealth.
Income and occupation status lose their significance among retired people, whereas wealth becomes more important.13–17 Therefore, we expected that socioeconomic differences in use of health care services would be underestimated if the measurements were based on income instead of wealth. An assumption underlying these analyses is that social context leading to illness (i.e., causation) explains socioeconomic differences in health and use of health care service, as opposed to health status influencing SES (i.e., selection). This assumption is consistent with the relevant literature on health inequalities.
Income and education are indeed considered determinants of ill health and hence of use of health care services. However, wealth is accumulated throughout the life course. Sick individuals are more likely to lose their jobs and remain unemployed and thus are less likely to accumulate wealth than are healthy people,30 which makes health a determinant of wealth. When wealth is considered as a source of disparity (in addition to income and education), causation may be even more difficult to differentiate from selection, and the possibility of selection increases, with sick people less likely to accumulate wealth. However, it is well known that the relation between health and SES may be bidirectional, and the 2 processes are not mutually exclusive. Longitudinal analysis could disentangle causation and selection effects.
Conclusions
The choice of the socioeconomic ranking variable—income versus wealth—affected measurements of socioeconomic differences for dentist visits but not for physician visits. Therefore, we found some support for using wealth instead of income to measure SES for older adult populations that include both economically active and noneconomically active individuals. Using wealth to measure SES instead of income appears to be more important when analyzing utilization differences for dental care than for physician services. Further research that extends this analysis to the long-term care sector—which, like dental care, draws heavily on service users' own payments—will help test the hypothesis that socioeconomic differences in health care are greater when measured by wealth as opposed to income.
Acknowledgments
The authors would like to acknowledge a grant received from the European Commission, DG Employment and Social Affairs, as part of the Observatory on the Social Situation and Demography. We used data from the Survey of Health, Ageing and Retirement in Europe (SHARE), wave 1. SHARE data collection in 2004 to 2007 was primarily funded by the European Commission through its 5th and 6th framework programmes (project numbers QLK6-CT-2001- 00360; RII-CT- 2006-062193; CIT5-CT-2005-028857). Additional funding to SHARE by the US National Institute on Aging (grant numbers U01 AG09740-13S2; P01 AG005842; P01 AG08291; P30 AG12815; Y1-AG-4553-01; OGHA 04-064; R21 AG025169) as well as by various national sources is gratefully acknowledged (see http://www.share-project.org for a full list of funding institutions).
The authors are grateful for comments received from Cristina Hernández-Quevedo, Joan Costa-Font, and 2 anonymous reviewers.
References
- 1.European Commission Communication From the Commission: Consultation Regarding Community Action on Health Services. Brussels, Belgium: European Commission; 2006 [Google Scholar]
- 2.Fuhrer R, Shipley MJ, Chastang JF, et al. Socioeconomic position, health, and possible explanations: a tale of two cohorts. Am J Public Health 2002;92:1290–1294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Doorslaer E, Masseria C, the OECD Health Equity Research Group Members Income-Related Inequality in the Use of Medical Care in 21 OECD Countries. Paris, France: Organisation for Economic Co-Operation and Development; 2004 [Google Scholar]
- 4.van Doorslaer E, Koolman X, Jones A. Explaining income-related inequalities in doctor utilisation in Europe. Health Econ 2004;13:629–647 [DOI] [PubMed] [Google Scholar]
- 5.Merlo J, Gerdtham U, Lynch J, Beckman A, Norlund A, Lithman T. Social inequalities in health—do they diminish with age? Int J Equity Health 2003;2:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hakkinen U, Luoma K. Determinants of expenditure variation in health care and care of the elderly among Finnish municipalities. Health Econ 1995;4:199–211 [DOI] [PubMed] [Google Scholar]
- 7.Schellhorn M, Stuck AE, Minder CE, Beck JC. Health services utilization of elderly Swiss: evidence from panel data. Health Econ 2000;9:533–545 [DOI] [PubMed] [Google Scholar]
- 8.Evandrou M. Growing Old in London: Socio-Economic Inequalities. London, England: Stimulating Social Policy in an Ageing Society (SAGE); 2003. SAGE discussion paper no. 15 [Google Scholar]
- 9.Allin S, Masseria C, Mossialos E. Inequality in health care use among older people in the United Kingdom: an analysis of panel data. London, England: LSE Health; 2006. LSE Health working paper no. 1 [Google Scholar]
- 10.Santos-Eggimenn B, Junod J, Cornaz S. Health services utilisation in older Europeans. Borsch-Supan A, Brugiavini A, Jurges H, Machenbach J, Siegrist J, Weber G, eds.Health, Ageing and Retirement in Europe: First Results From the Survey of Healthy Ageing and Retirement in Europe. Mannheim, Germany: Mannheim Research Institute for the Economics of Ageing; 2005:133–140 [Google Scholar]
- 11.Chen AY, Escarce JJ. Quantifying income-related inequality in healthcare delivery in the United States. Med Care 2004;42:38–47 [DOI] [PubMed] [Google Scholar]
- 12.Arber S, Ginn J. Gender and inequalities in health in later life. Soc Sci Med 1993;36:33–46 [DOI] [PubMed] [Google Scholar]
- 13.van Ourti T. Socio-economic inequality in ill-health amongst the elderly: should one use current or permanent income? J Health Econ 2003;22:219–241 [DOI] [PubMed] [Google Scholar]
- 14.Feinstein J. The relationship between SES and health: a review of the literature. Milbank Q 1993;71:279–322 [PubMed] [Google Scholar]
- 15.Buckley NJ, Denton FT, Robb AL, Spencer BG. Healthy aging at older ages: are income and education important? Can J Aging 2004;23(suppl 1):S155–S169 [DOI] [PubMed] [Google Scholar]
- 16.Torrey BB, Taeuber CM. The importance of asset income among the elderly. Rev Income Wealth 1986;32:443–449 [Google Scholar]
- 17.Alessie R, Lusardi A, Aldershof T. Income and wealth over the life cycle: evidence from panel data. Rev Income Wealth 1997;43:1–32 [Google Scholar]
- 18.Crystal S, Shea D. The economic well-being of the elderly. Rev Income Wealth 1990;36:227–247 [Google Scholar]
- 19.Costa-Font J. Housing assets and the socio-economic determinants of health and disability in old age. Health Place 2008;14:478–491 [DOI] [PubMed] [Google Scholar]
- 20.Growing Older in America: The Health & Retirement Study. Bethesda, MD: National Institute on Aging; 2007 [Google Scholar]
- 21.Borsch-Supan A, Jurges H, eds.The Survey of Health, Ageing, and Retirement in Europe—Methodology. Mannheim, Germany: Mannheim Research Institute for the Economics of Ageing; 2005 [Google Scholar]
- 22.McGrath C, Bedi R, Dhawan N. Factors influencing older people's self-reported use of dental services in the UK. Gerodontology 1999;16:97–102 [DOI] [PubMed] [Google Scholar]
- 23.Buchmueller T, Grumbach K, Kronick R, Kahn JG. The effect of health insurance on medical care utilization and implications for insurance expansion: a review of the literature. Med Care Res Rev 2005;62:3–30 [DOI] [PubMed] [Google Scholar]
- 24.Social Policy Division, Directorate for Employment, Labour and Social Affairs What Are Equivalence Scales? Paris, France: Organisation for Economic Co-Operation and Development; 2005. Available at: http://www.oecd.org/dataoecd/61/52/35411111.pdf. Accessed February 2, 2007 [Google Scholar]
- 25.Jones A, Rice N, Bago d'Uva T, Balia S. Applied Health Economics Abingdon, England: Routledge; 2007 [Google Scholar]
- 26.Wagstaff A, van Doorslaer E. Equity in health care finance and delivery. Culyer AJ, Newhouse JP, eds.Handbook of Health Economics Amsterdam, the Netherlands: North-Holland; 2000:1803–1862 [Google Scholar]
- 27.O'Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation. Washington, DC: World Bank; 2008 [Google Scholar]
- 28.Zavras D, Economou C, Kvriopoulos J. Factors influencing dental utilisation in Greece. Community Dent Health 2004;21:181–188 [PubMed] [Google Scholar]
- 29.Wamala S, Merlo J, Boström G. Inequity in access to dental care services explains current socioeconomic disparities in oral health: the Swedish National Surveys of Public Health 2004–2005. J Epidemiol Community Health 2006;69:1027–1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mackenbach JP, Bakker MJ, Kunst AE, Diderichsen F. Socioeconomic inequalities in health in Europe: an overview. Mackenbach JP, Bakker MJ, eds.Reducing Inequalities in Health London, England: Routledge; 2002:3–24 [Google Scholar]