Abstract
Objectives. We compared the association between advancing maternal age and risk of preterm delivery across 4 groups (Black smokers, Black nonsmokers, White smokers, White nonsmokers) and within the context of neighborhood deprivation levels.
Methods. We obtained data from linked census and birth records for singletons (n = 182 938) delivered by women aged 20 to 39 years in Philadelphia, Pennsylvania; Baltimore, Maryland; 16 Michigan cities; 3 Maryland counties; and 2 North Carolina counties. Results from area-specific multilevel logistic regression models were combined to obtain pooled estimates of relations between maternal age and risk of preterm delivery. We repeated the models after categorizing women by neighborhood deprivation level (low, medium, and high).
Results. Among multiparous women, there was a significant age-related increase in preterm delivery in 3 of the 4 groups. The adjusted odds ratio per 5-year age increase was 1.31 in Black smokers, 1.11 in Black nonsmokers, and 1.16 in White smokers. In each group, the odds ratio increased as neighborhood deprivation increased.
Conclusions. These results support the “weathering” hypothesis, suggesting that Black women, women with high-risk behaviors, and women living in high-deprivation neighborhoods may develop “accelerated aging” that increases preterm delivery risk.
The elevated risks of infant mortality1 and long-term disability2 associated with preterm birth are well-documented. Studies have repeatedly shown higher preterm delivery rates among Black women in the United States3 and women in lower socioeconomic strata.4–7 The association between preterm delivery risk and maternal age has also been frequently studied by means of data from vital records8–12 or epidemiologic studies.13–17 Overall, these studies suggest a curvilinear relation, with slightly higher preterm delivery risk in adolescents, lower risk in early adulthood, and increasing risk with advancing maternal age. The shape of this curve might be influenced by multiple factors, including age-related differences in maternal behaviors and physiologic and disease states. There is also self-selection in timing of pregnancies, and later-age pregnancies may include a higher proportion of women with a history of infertility or fetal loss.
Building on the observations that adverse pregnancy outcomes increase with advancing maternal age, and noting the marked Black–White disparities in these adverse outcomes, Geronimus proposed a “weathering” or “accelerated aging” hypothesis.18 This hypothesis states that: (1) a decline in health status contributes to poorer reproductive outcomes as women age and (2) social inequalities lead to an earlier and disproportionately greater decline in the health status of Blacks, which results in a widening health differential between Blacks and Whites with advancing age. In support of the weathering hypothesis, Geronimus and others have shown an increase in Black–White disparities with advancing maternal age for outcomes such as neonatal mortality18,19 and low and very low birth weight (LBW),18,20–23 but results for preterm delivery have been inconsistent.9,12,24 There have also been reports of increasing disparities in adverse pregnancy outcomes with advancing age when women are categorized by measures of disadvantage or socioeconomic status.20,23,25
Based on the framework described by Williams,26 there are multiple potential causes in the pathway to accelerated aging among Black and disadvantaged women, such as delays in accessing health care, employment-related adverse health effects, more obstacles to and fewer opportunities for a healthy lifestyle (e.g., exercise and diet), exposure to air pollutants, high-risk coping behaviors (e.g., smoking, alcohol use, and drug use), and excess stress caused by discrimination, violence, financial troubles, housing insecurity, and lack of instrumental social support. Many of these causes are endemic, and perhaps “infectious,” in neighborhoods with high levels of deprivation.27 Among previous studies that have examined effects of neighborhood poverty level on the associations among race, maternal age, and risk of LBW deliveries, results have been mixed,20,22,23 and no study has assessed preterm delivery as the primary outcome.
In our study we linked birth records to census data from a multisite project to compare the association between advancing maternal age and risk of preterm delivery across groups of women categorized by race and reported smoking status during pregnancy. Although smoking is thought to have direct effects on preterm delivery risk, we also considered smoking to be a potential indicator of high-risk coping behaviors and unhealthy lifestyle. We also examined effects of neighborhood deprivation on the age–preterm delivery relation within the different maternal groups as defined by race and smoking status. We hypothesized that the slope of increasing preterm delivery risk with advancing maternal age would be steeper for Black women, smokers, and women living in neighborhoods with high levels of deprivation.
METHODS
The Multilevel Modeling of Disparities Explaining Preterm Delivery project involved investigators from 4 universities and public health professionals from state and local health departments.28,29 This multisite collaboration linked census and vital record data to examine policy-relevant contextual factors that might contribute to racial and social-class disparities in adverse birth outcomes. A total of 8 geographic areas were included: 3 urban centers (Philadelphia, PA; Baltimore, MD; and 16 combined cities in Michigan), 3 economically and racially diverse suburban Maryland counties (Baltimore County, Montgomery County, and Prince George's County), and 2 counties in North Carolina (Durham County and Wake County). Michigan's 16 cities, selected based on common urban-related problems, were combined because analyses revealed similar contextual characteristics across cities, comparable results when cities were analyzed separately or together, and improved statistical power as a result of pooling smaller cities into a single area. By contrast, the multiple areas in other states, 4 in Maryland and 2 in North Carolina, were analyzed separately because they exhibited sociodemographic and birth outcome heterogeneity across areas. Data were restricted to only non-Hispanic Whites and non-Hispanic Blacks (hereafter Whites and Blacks, respectively).
Individual-Level Data
Analyses used birth record data from singletons delivered by women aged 20 to 39 years. Birth years ranged from 1995 through 2001 and varied by site on the basis of data availability and years of interest as negotiated with each government health department (appendix A, available as a supplement to the online version of this article at http://www.ajph.org). A small percentage of birth records (< 5%) were excluded from each geographic area, as a result of missing data on age, race, education, parity, or maternal smoking during pregnancy. The exceptions were Montgomery and Prince George's Counties, which had higher percentages of missing data on maternal smoking (19% and 8% of the White mothers and 10% and 28% of the Black mothers, respectively). Gestational age at delivery was based on physician estimates recorded on birth certificates. Preterm delivery was defined as delivery at less than 37 completed weeks. Preterm infants with birth weights greater than 3887 grams (99th percentile at 37 weeks) were excluded because of the high probability of incorrect recording of weight or gestational age. Women were categorized as nonsmokers or smokers during pregnancy based on birth record information. The final sample consisted of singleton births for 87 630 Whites and 95 308 Blacks.
Neighborhood-Level Data
Maternal addresses in birth file records were geocoded to census tracts (n = 1773) and linked to year 2000 census data. A neighborhood-level deprivation index with census variables that represented 5 policy-relevant sociodemographic domains (income and poverty, education, employment, housing, and occupation) was developed by means of a method described elsewhere.28
Analyses
The first goal was to estimate the association between maternal age and risk of preterm delivery in 4 groups: White nonsmokers, White smokers, Black nonsmokers, and Black smokers. Modeling was performed separately for primiparous and multiparous women. For each of the study's 8 geographic areas, we used a multilevel logistic regression model with random intercepts to assess the relation between maternal age (independent variable) and preterm delivery risk (dependent variable) in the 4 maternal groups. The multilevel modeling software used (HLM30 or Stata31) varied by site. Results from the 8 sites were pooled with a random-effects meta-analysis to obtain a single summary slope coefficient and intercept for each of the 4 maternal groups. The pooled coefficient for each group was evaluated for magnitude and tested to determine if it was significantly greater than zero. In addition, the pooled coefficients for each maternal group were compared (2-sided t test).
A second goal was to examine the maternal-group-specific relation between maternal age and preterm delivery risk in the context of neighborhood deprivation levels. Women were assigned to 1 of 3 categories on the basis of their census tract deprivation level: low (< −1.0 SD), medium (–1.0 to +1.0 SD), and high (> +1.0 SD). We used the deprivation index score distribution from all 8 sites combined to construct the categories. The modeling strategy just described was repeated; i.e., results from the 8 geographic areas were pooled to obtain a single summary slope coefficient and intercept. These analyses resulted in 12 pooled slope coefficients because each of the 4 maternal groups had 3 separate coefficients for the age–preterm delivery relation corresponding to women living in neighborhoods with a low, medium, or high deprivation score.
All modeling was repeated with maternal education level added as a covariate. Previous analyses of these multisite data showed that there was sufficient homogeneity across geographic areas in the association between neighborhood deprivation level and preterm delivery risk to support pooling.29 However, in analyses that separated women by parity and grouped them by race, smoking status, and neighborhood deprivation level, there occasionally were unstable area-specific slope coefficients for the age–preterm delivery association (i.e., coefficients that had large standard errors). In these instances, areas were excluded from the summary pooled estimate for a particular race-smoking-deprivation group.
RESULTS
There was a wide range of eligible births across the 8 geographic areas: 3444 (Prince George's County) to 27 008 (16 Michigan cities) Whites, and 3559 (Durham County) to 41 122 (16 Michigan cities) Blacks (appendix A, available online). The percentage of singleton births delivered preterm ranged from 5.9 (Montgomery County) to 8.9 (Baltimore City) among Whites and from 10.1 (Montgomery County) to 16.1 (Baltimore City) among Blacks. The percentages of women who reported smoking during pregnancy ranged from 3.6 (Montgomery County) to 20.4 (16 Michigan cities) among Whites and from 3.2 (Montgomery County) to 17.6 (16 Michigan cities) among Blacks.
Age and Preterm Risk by Race and Smoking Status
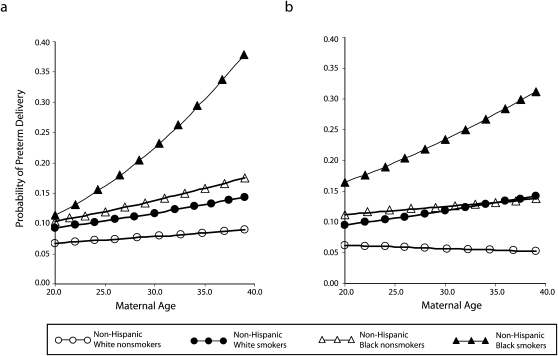
Odds ratios (ORs) for preterm delivery were calculated per 5-year increase in maternal age. Results displayed in figures were expressed as probabilities of preterm delivery.32 In analyses that grouped women by race and smoking status, preterm delivery risk increased with advancing maternal age in all groups except for multiparous, White nonsmokers (Table 1, Figure 1). Among primiparous women, the age-related increase in preterm delivery risk among Black smokers (5-year unadjusted OR = 1.51) was significantly greater than that among White nonsmokers, White smokers, and Black nonsmokers (5-year unadjusted OR range 1.08–1.17). Among multiparous women, the steepest slope was again for Black smokers (5-year unadjusted OR = 1.25), and the standardized parameter estimates were significantly different for each pairwise comparison of race and smoking groups, with 1 exception: White smokers and Black nonsmokers were not significantly different from each other. In each model, adjustment for maternal education level resulted in slightly larger odds ratios and did not alter comparisons across groups (Table 1).
TABLE 1.
5-Year Associations Between Maternal Age and Risk of Preterm Delivery, by Race, Smoking Status, and Neighborhood Deprivation (n = 182 938): 8 US Geographic Areas, 1995–2001
| Primiparous Women |
Multiparous Women |
|||
| Unadjusted OR (95% CI) | AORa (95% CI) | Unadjusted OR (95% CI) | AORa (95% CI) | |
| Non-Hispanic White nonsmokers | ||||
| Nonsmokers | 1.08* (1.03, 1.14) | 1.11* (1.05, 1.17) | 0.95 (0.90, 1.02) | 1.00 (0.94, 1.06) |
| Deprivation scale | ||||
| Low | 1.03 (0.93, 1.14) | 1.04 (0.94, 1.15) | 0.99 (0.91, 1.06) | 1.02 (0.95, 1.10) |
| Medium | 1.16* (1.08, 1.23) | 1.18* (1.11, 1.26) | 0.98 (0.89, 1.07) | 1.02 (0.93, 1.12) |
| High | 1.14 (0.93, 1.41) | 1.18 (0.96, 1.45) | 1.09 (0.94, 1.27) | 1.12 (0.97, 1.30) |
| Non-Hispanic White smokers | ||||
| Smokers | 1.14* (1.02, 1.28) | 1.17* (1.04, 1.32) | 1.13* (1.05, 1.21) | 1.16* (1.08, 1.25) |
| Deprivation scale | ||||
| Low | 1.07 (0.78, 1.45) | 1.08 (0.79, 1.48) | 1.10 (0.86, 1.41) | 1.14 (0.90, 1.46) |
| Medium | 1.16* (1.01, 1.34) | 1.19* (1.03, 1.38) | 1.09 (0.96, 1.25) | 1.13 (0.99, 1.28) |
| High | 1.45* (1.04, 2.02) | 1.51* (1.08, 2.14) | 1.25* (1.08, 1.43) | 1.26* (1.10, 1.45) |
| Non-Hispanic Black nonsmokers | ||||
| Nonsmokers | 1.17* (1.12, 1.23) | 1.20* (1.14, 1.26) | 1.06* (1.03, 1.11) | 1.11* (1.07, 1.15) |
| Deprivation scale | ||||
| Low | 1.17 (0.98, 1.40) | 1.19 (1.00, 1.43) | 1.04 (0.95, 1.14) | 1.08 (0.98, 1.19) |
| Medium | 1.17* (1.11, 1.23) | 1.19* (1.13, 1.25) | 1.05* (1.02, 1.09) | 1.09* (1.05, 1.13) |
| High | 1.28* (1.18, 1.40) | 1.31* (1.20, 1.43) | 1.11* (1.02, 1.19) | 1.15* (1.08, 1.23) |
| Non-Hispanic Black smokers | ||||
| Smokers | 1.51* (1.34, 1.69) | 1.56* (1.38, 1.75) | 1.25* (1.14, 1.36) | 1.31* (1.20, 1.43) |
| Deprivation scale | ||||
| Low | 1.50* (1.06, 2.12) | 1.54* (1.09, 2.18) | 1.20 (0.90, 1.61) | 1.26 (0.94, 1.68) |
| Medium | 1.54* (1.30, 1.83) | 1.59* (1.34, 1.89) | 1.24* (1.09, 1.41) | 1.33* (1.16, 1.54) |
| High | 1.54* (1.29, 1.82) | 1.59* (1.34, 1.88) | 1.34* (1.26, 1.40) | 1.36* (1.30, 1.43) |
Note. AOR = adjusted odds ratio; CI = confidence interval.
Adjusted for maternal education.
P < .05.
FIGURE 1.
Estimated probability of preterm delivery by maternal age, race, and smoking status for (a) primiparous women and (b) multiparous women: 8 US geographic areas, 1995–2001.
Note. The sample size was n = 182 938.
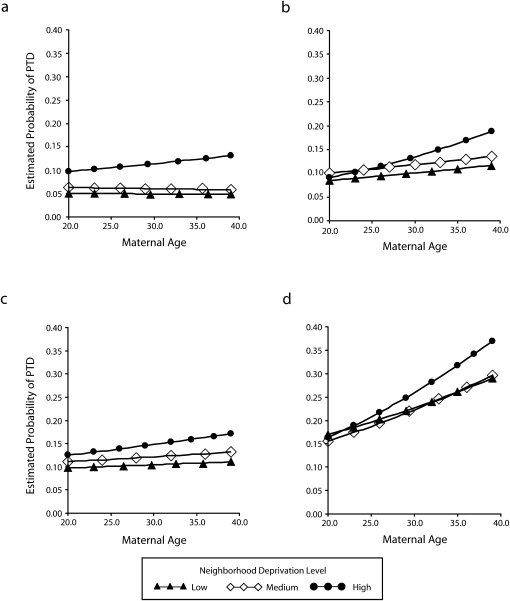
Age and Delivery Risk by Race, Smoking Status, and Neighborhood Deprivation
Each of the 4 maternal groups defined by race and smoking status was further separated into 3 categories according to neighborhood deprivation level (low deprivation, medium deprivation, and high deprivation), and analyses were parity-specific (Table 1 and Figure 2; see also appendix B, available as a supplement to the online version of this article at http://www.ajph.org). White nonsmokers living in low-deprivation areas showed little evidence of increasing preterm delivery risk with advancing age; for those living in medium- or high-deprivation areas, the 5-year unadjusted ORs were modest (0.98–1.16) and most often not statistically significant. White smokers living in low- or medium-deprivation areas had 5-year unadjusted ORs similar to those of White nonsmokers; those living in high-deprivation areas had considerably larger 5-year unadjusted ORs (1.45 for primiparous women and 1.25 for multiparous women).
FIGURE 2.
Estimated probability of preterm delivery by maternal age, stratified by level of neighborhood deprivation (low, medium, and high), for (a) multiparous White nonsmokers, (b) multiparous White smokers, (c) multiparous Black nonsmokers, and (d) multiparous Black smokers: 8 US geographic areas, 1995–2001.
Note. The sample size was n = 182 938.
Black nonsmokers living in low- or medium-deprivation areas had 5-year unadjusted ORs (1.04–1.17) similar to those of White nonsmokers living in high-deprivation areas. Black nonsmokers living in high-deprivation areas had 5-year unadjusted ORs that were as high as 1.28 and were statistically significant. Among Black smokers, all 5-year unadjusted ORs were greater than 1.20, and most were statistically significant. In the high-deprivation group of Black smokers, 5-year unadjusted ORs were 1.54 (primiparous) and 1.34 (multiparous). For primiparous Black smokers, the low-deprivation group intercept appeared to be above those of the medium- and high-deprivation groups (appendix B, available online). This result was most likely caused by unstable estimates resulting from small sample sizes in this particular low-deprivation group. Overall, for primiparous and multiparous women, the 5-year unadjusted ORs for risk of preterm delivery increased with increasing deprivation level from low to high. Adjustment for maternal education resulted in slightly larger 5-year adjusted ORs and did not attenuate the neighborhood effects.
DISCUSSION
In our multisite study, the lowest-risk group—multiparous White women who delivered singleton births, did not smoke during pregnancy, and lived in neighborhoods with the lowest levels of deprivation—showed no signs of age-related increases in risk of preterm delivery from ages 20 through 39 years. Women with behavioral (smoking) or demographic (Black) characteristics associated with preterm delivery risk in previous studies experienced age-related increases in risk of preterm delivery. These findings support the weathering hypothesis, suggesting that Black women and women with high-risk behaviors may develop accelerated aging that adversely affects pregnancy outcomes. In addition, age-related increases in preterm delivery in Blacks and smokers appeared lowest among women living in neighborhoods with low levels of deprivation and most pronounced among women living in neighborhoods with high levels of deprivation, even after adjusting for maternal education.
A few studies have used individual-level effect modifiers, such as race and maternal education, to explore effect modification of the relation between maternal age and preterm delivery risk. For example, an analysis of more than 15 million US singleton births covering every fifth year from 1975 to 1995 found that preterm delivery risk increased after ages 25 to 29 years among Black and White multiparous women, but the slopes of the 2 racial/ethnic groups were similar (no interaction).9 By contrast, a study of slightly less than 11 million US singleton births delivered in 2000 through 2002 noted that among multiparous women, the slope for increasing preterm delivery after ages 25 to 29 years was greater for Blacks than for Whites, especially for deliveries at less than 32 weeks.12 A study of vital data from Italy, stratified according to education level (high vs low) as opposed to race, showed that preterm delivery risk advanced with maternal age most strongly in the low-education group.25 Others have reported on overall preterm delivery risk in relation to neighborhood-level conditions,5,6,29,33–37 including an interaction with smoking status,38 but these studies did not address neighborhood effects on the association between preterm delivery risk and advancing maternal age.
Some studies have considered neighborhood context, race, and effect of maternal aging on risk of delivering an LBW infant. LBW can result from preterm delivery, poor fetal growth, or both, and it therefore encompasses a complex array of adverse pregnancy outcomes. A Michigan study reported a widening Black–White disparity for delivery of an LBW infant as maternal age advanced, but there was effect modification by neighborhood-level mean income in Black women.20 Those living in high-socioeconomic-status neighborhoods showed no age-related increase in risk of LBW across the age span of 15 to 34 years. A similar study in Chicago found that after adjusting for multiple covariates, the association between maternal age and delivery of an LBW infant was modified by smoking status and neighborhood-level poverty but not by race.23 A New York City study found a Black–White disparity in risk of delivering an LBW infant with advancing maternal age but no interaction with neighborhood-level poverty.22 Methodologically, these studies differed in important ways, including the range of maternal age studied, the approach used to define “neighborhoods” by census-tract groups, sample size, modeling strategies, and individual-level covariates modeled as main effects and interactions; yet all 3 studies found increasing Black–White disparities in LBW with advancing maternal age in unadjusted models.
These studies tell us what is happening but not how it is happening. Studies of proximate biologic measures, such as pregnancy complications and underlying health conditions, help to shed light on mechanisms that might mediate age-related increases in adverse pregnancy outcomes and interactions with race and social class. In pregnant women, advancing maternal age has been linked to higher prevalences of hypertension,10 chronic disease,10 abruption,10,39 gestational diabetes,39,40 placenta previa,10,39,40 and premature rupture of membranes.39 Data from the National Health and Nutrition Examination Survey IV (1999–2002) showed that nonpregnant women aged 15 to 44 years experienced age-related increases in the prevalence of hypertension41 and in a composite adverse-health measure called “allostatic load,” defined by levels of blood pressure, body mass index, glycated hemoglobin, creatinine clearance, albumin, triglycerides, C-reactive protein, total cholesterol, and homocysteine.42 The age-related increases in these adverse-health indices were more dramatic among Black women than among White women and among poorer women than among richer women. Similarly, a US study of nonpregnant women reported that the risk of death related to coronary heart disease at age 35 to 44 years was significantly higher for Black women than for White women, with the magnitude of disparity varying by geographic area.43
Limitations
Inferences about smoking effects on preterm delivery risk should be made with caution. Smoking is related to other lifestyle factors that may act as unmeasured confounders.44,45 Given the limitations of birth-record data, we considered smoking in pregnancy to be the best available indicator of high-risk coping behaviors. Other studies of smoking, maternal age, and preterm delivery have primarily evaluated age as an effect modifier. In these studies, the increased risk of preterm delivery associated with smoking or exposure to secondhand smoke was most evident among older women.17,46,47 Relevant to the weathering hypothesis, a recent US study of smoking prevalence among pregnant women in the 1990s found that among younger mothers, Blacks were less likely than Whites to smoke during pregnancy, but the pattern was reversed among older mothers.48
As in other observational studies, critical elements in our study, such as neighborhood residence and maternal age at pregnancy, were not randomly assigned. Therefore, we cannot rule out the possibility that results were biased by self-selection, a hypothesis that stands as an alternative to the weathering hypothesis. Slope differences across neighborhood deprivation levels persisted after adjusting for maternal education, but we lacked other individual-level data that could have been used to further disentangle individual and neighborhood effects.
Our findings were based on cross-sectional data that led to inferences about maternal aging effects, but young, multiparous women aged 20 to 24 years are likely to be different in many ways when compared with older, multiparous women. Primiparous women aged 35 to 39 years may be a mixed group, with some delaying pregnancy because of career demands and others finally pregnant after a history of infertility or pregnancy loss. Although it might be useful to repeat these analyses with longitudinal datasets and linked birth records that track women over time, most women have 2 or 3 births that are closely spaced; thus, an individual woman's history of live births would represent only a small portion of the maternal age span of 20 to 39 years. We chose to exclude women younger than 20 years from our analyses, primarily because adolescents who become pregnant and complete the pregnancy are a unique group in a society where this is not the norm. They differ in many ways other than age, and these differences can produce unmeasured confounding. Such confounding is especially problematic among multiparous adolescents.
Inaccuracies in smoking status49,50 and gestational age estimates,51 particularly from birth records,52,53 may have introduced some measurement bias, but it seems unlikely that these measurement errors could completely explain our results. Women who deliver preterm may be more likely to have their smoking recorded (which would alter the intercept), but there is no reason to suspect that the biases in recording would increase with advancing maternal age and thereby bias the slope.
Within each maternal group characterized by parity, race/ethnicity, smoking status, and neighborhood deprivation level, we assessed the effect of maternal age on preterm delivery risk by determining the magnitude of the slope and testing whether the slope was significantly greater than zero. Interpretations of these results were influenced by occasional instances when 2 groups had comparable slope estimates, but the slope was not statistically significant in the group with the smaller sample size, e.g., multiparous Black smokers living in low-deprivation areas. Thus, we could not rule out a type II error.
Other studies examining racial/ethnic differences in preterm delivery risk related to maternal age have used all US births from particular years. This was not an option in our study because of our added focus on examining neighborhood effects. We selected multiple geographic areas in which we had an opportunity to link geocoded birth records with census data. The generalizability of our results is enhanced by our inclusion of urban, suburban, and rural populations from several areas of the country, but we did not draw a statistically representative sample from the population of all US births. We did carefully develop and incorporate a comprehensive measure of neighborhood deprivation that was highly reproducible across the geographic areas we selected.28
Conclusions
Additional in-depth studies could help clarify links between maternal “weathering,” neighborhood conditions, and risk of preterm delivery. It would be helpful to uncover biologic intermediaries that both increase the risk of preterm delivery and are central to weathering (e.g., blood pressure, vascular reactivity, insulin resistance, lipid levels, immune function, and oxidative stress). There is also a need for longitudinal studies comparing age-related trajectories of these biologic intermediaries across groups of women (e.g., women grouped by race, socioeconomic status, high-risk behaviors, and neighborhood conditions).
Inferences from our results can be viewed from 2 vantage points: the glass half-full or half-empty. Changes in preterm delivery risk from age 20 to 39 years seem minimal to negligible among low-risk women delivering singleton infants. It also appears that better neighborhoods might attenuate weathering effects in higher-risk women, i.e., Blacks and smokers. Conversely, the combination of being in a high-risk group and living in a poorer neighborhood might accelerate the pace of weathering. If correct, these inferences would be relevant to other aspects of women's health beyond pregnancy outcomes and would emphasize the need to intervene at an early age at both the individual and contextual levels. It is sobering to think that many US women may be experiencing premature acceleration in aging and resultant declining health. Knowing that this effect is related to neighborhoods raises the importance of place in public health priorities.
Acknowledgments
This work was supported by contracts that the Maternal and Child Health Bureau of the Health Resources and Services Administration awarded to the four states in the study (02-0287P, 03-MCHB-047B, HHSH240200415028P, HHSH240200515112P).
The authors acknowledge the essential roles played by their public health partners in the state and city health departments at the four study sites: Isabelle Horon at the Vital Statistics Administration of the Maryland Department of Health and Mental Hygiene, Violanda Grigorescu at the Bureau of Epidemiology of the Michigan Department of Community Health, Brian Castrucci at the Division of Maternal, Child, and Family Health of the Philadelphia Department of Public Health, and Paul Buescher at the North Carolina State Center for Health Statistics of the North Carolina Department of Health and Human Services. The authors also acknowledge the assistance received from Mary Kay Kenney and Michael Kogan of the Maternal and Child Health Bureau.
Human Participant Protection
This study was approved by multiple institutional review boards that protect human subjects. These boards were affiliated with participating governmental or academic institutions.
References
- 1.Callaghan WM, MacDorman MF, Rasmussen SA, Qin C, Lackritz EM. The contribution of preterm birth to infant mortality rates in the United States. Pediatrics 2006;118(4):1566–1573 [DOI] [PubMed] [Google Scholar]
- 2.Lindstrom K, Winbladh B, Haglund B, Hjern A. Preterm infants as young adults: a Swedish national cohort study. Pediatrics 2007;120(1):70–77 [DOI] [PubMed] [Google Scholar]
- 3.Vahratian A, Buekens P, Alexander GR. State-specific trends in preterm delivery: are rates really declining among non-Hispanic African Americans across the United States? Matern Child Health J 2006;10(1):27–32 [DOI] [PubMed] [Google Scholar]
- 4.Farley TA, Mason K, Rice J, Habel JD, Scribner R, Cohen DA. The relationship between the neighbourhood environment and adverse birth outcomes. Paediatr Perinat Epidemiol 2006;20(3):188–200 [DOI] [PubMed] [Google Scholar]
- 5.Luo ZC, Kierans WJ, Wilkins R, Liston RM, Mohamed J, Kramer MS. Disparities in birth outcomes by neighborhood income: temporal trends in rural and urban areas, British Columbia. Epidemiology 2004;15(6):679–686 [DOI] [PubMed] [Google Scholar]
- 6.Luo ZC, Wilkins R, Kramer MS. Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. Can Med Assoc J 2006;174(10):1415–1421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith GC, Shah I, White IR, Pell JP, Crossley JA, Dobbie R. Maternal and biochemical predictors of spontaneous preterm birth among nulliparous women: a systematic analysis in relation to the degree of prematurity. Int J Epidemiol 2006;35(5):1169–1177 [DOI] [PubMed] [Google Scholar]
- 8.Aldous MB, Edmonson MB. Maternal age at first childbirth and risk of low birth weight and preterm delivery in Washington State. JAMA 1993;270(21):2574–2577 [PubMed] [Google Scholar]
- 9.Ananth CV, Misra DP, Demissie K, Smulian JC. Rates of preterm delivery among Black women and White women in the United States over two decades: an age-period-cohort analysis. Am J Epidemiol 2001;154(7):657–665 [DOI] [PubMed] [Google Scholar]
- 10.Joseph KS, Allen AC, Dodds L, Turner LA, Scott H, Liston R. The perinatal effects of delayed childbearing. Obstet Gynecol 2005;105(6):1410–1418 [DOI] [PubMed] [Google Scholar]
- 11.Machado CJ. Impact of maternal age on birth outcomes: a population-based study of primiparous Brazilian women in the city of Sao Paulo. J Biosoc Sci 2006;38(4):523–535 [DOI] [PubMed] [Google Scholar]
- 12.Schempf AH, Branum AM, Lukacs SL, Schoendorf KC. Maternal age and parity-associated risks of preterm birth: differences by race/ethnicity. Paediatr Perinat Epidemiol 2007;21(1):34–43 [DOI] [PubMed] [Google Scholar]
- 13.Barkan SE, Bracken MB. Delayed childbearing: no evidence for increased risk of low birth weight and preterm delivery. Am J Epidemiol 1987;125(1):101–109 [DOI] [PubMed] [Google Scholar]
- 14.Cnattingius S, Forman MR, Berendes HW, Isotalo L. Delayed childbearing and risk of adverse perinatal outcome: a population-based study. JAMA 1992;268(7):886–890 [PubMed] [Google Scholar]
- 15.Ekwo EE, Moawad A. Maternal age and preterm births in a black population. Paediatr Perinat Epidemiol 2000;14(2):145–151 [DOI] [PubMed] [Google Scholar]
- 16.Prysak M, Lorenz RP, Kisly A. Pregnancy outcome in nulliparous women 35 years and older. Obstet Gynecol 1995;85(1):65–70 [DOI] [PubMed] [Google Scholar]
- 17.Wen SW, Goldenberg RL, Cutter GR, et al. Smoking, maternal age, fetal growth, and gestational age at delivery. Am J Obstet Gynecol 1990;162(1):53–58 [DOI] [PubMed] [Google Scholar]
- 18.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis 1992;2(3):207–221 [PubMed] [Google Scholar]
- 19.Buescher PA, Mittal M. Racial disparities in birth outcomes increase with maternal age: recent data from North Carolina. N C Med J 2006;67(1):16–20 [PubMed] [Google Scholar]
- 20.Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med 1996;42(4):589–597 [DOI] [PubMed] [Google Scholar]
- 21.Khoshnood B, Wall S, Lee KS. Risk of low birth weight associated with advanced maternal age among four ethnic groups in the United States. Matern Child Health J 2005;9(1):3–9 [DOI] [PubMed] [Google Scholar]
- 22.Rauh VA, Andrews HF, Garfinkel RS. The contribution of maternal age to racial disparities in birthweight: a multilevel perspective. Am J Public Health 2001;91(11):1815–1824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rich-Edwards JW, Buka SL, Brennan RT, Earls F. Diverging associations of maternal age with low birthweight for Black and White mothers. Int J Epidemiol 2003;32(1):83–90 [DOI] [PubMed] [Google Scholar]
- 24.Osypuk TL, Acevedo-Garcia D. Are racial disparities in preterm birth larger in hypersegregated areas? Am J Epidemiol 2008;167(11):1295–1304 [DOI] [PubMed] [Google Scholar]
- 25.Astolfi P, Zonta LA. Delayed maternity and risk at delivery. Paediatr Perinat Epidemiol 2002;16(1):67–72 [DOI] [PubMed] [Google Scholar]
- 26.Williams DR. Race and health: basic questions, emerging directions. Ann Epidemiol 1997;7(5):322–333 [DOI] [PubMed] [Google Scholar]
- 27.Crane J. The epidemic theory of ghettos and neighborhood effects on dropping out and teenage childbearing. Am J Sociol 1991;96(5):1226–1259 [Google Scholar]
- 28.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health 2006;83(6):1041–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Campo P, Burke JG, Culhane J, et al. Neighborhood deprivation and preterm birth among non-Hispanic Black and White women in eight geographic areas in the United States. Am J Epidemiol 2008;167(2):155–163 [DOI] [PubMed] [Google Scholar]
- 30.HLM [computer program]. Version 6.01. Lincolnwood, IL: Scientific Software International; 2006 [Google Scholar]
- 31.Stata [computer program]. Version 8. College Station, TX: StataCorp LP; 2006 [Google Scholar]
- 32.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed.Thousand Oaks, CA: Sage Publications; 2002 [Google Scholar]
- 33.Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Soc Sci Med 2006;63(12):3030–3045 [DOI] [PubMed] [Google Scholar]
- 34.Huynh M, Parker JD, Harper S, Pamuk E, Schoendorf KC. Contextual effect of income inequality on birth outcomes. Int J Epidemiol 2005;34(4):888–895 [DOI] [PubMed] [Google Scholar]
- 35.Kaufman JS, Dole N, Savitz DA, Herring AH. Modeling community-level effects on preterm birth. Ann Epidemiol 2003;13(5):377–384 [DOI] [PubMed] [Google Scholar]
- 36.Pickett KE, Collins JW, Jr, Masi CM, Wilkinson RG. The effects of racial density and income incongruity on pregnancy outcomes. Soc Sci Med 2005;60(10):2229–2238 [DOI] [PubMed] [Google Scholar]
- 37.Reagan PB, Salsberry PJ. Race and ethnic differences in determinants of preterm birth in the USA: broadening the social context. Soc Sci Med 2005;60(10):2217–2228 [DOI] [PubMed] [Google Scholar]
- 38.Ahern J, Pickett KE, Selvin S, Abrams B. Preterm birth among African American and White women: a multilevel analysis of socioeconomic characteristics and cigarette smoking. J Epidemiol Community Health 2003;57(8):606–611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cleary-Goldman J, Malone FD, Vidaver J, et al. Impact of maternal age on obstetric outcome. Obstet Gynecol 2005;105(5 pt 1):983–990 [DOI] [PubMed] [Google Scholar]
- 40.Jolly M, Sebire N, Harris J, Robinson S, Regan L. The risks associated with pregnancy in women aged 35 years or older. Hum Reprod 2000;15(11):2433–2437 [DOI] [PubMed] [Google Scholar]
- 41.Geronimus AT, Bound J, Keene D, Hicken M. Black–White differences in age trajectories of hypertension prevalence among adult women and men, 1999–2002. Ethn Dis 2007;17(1):40–48 [PubMed] [Google Scholar]
- 42.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. Am J Public Health 2006;96(5):826–833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williams JE, Massing M, Rosamond WD, Sorlie PD, Tyroler HA. Racial disparities in CHD mortality from 1968–1992 in the state economic areas surrounding the ARIC study communities. Ann Epidemiol 1999;9(8):472–480 [DOI] [PubMed] [Google Scholar]
- 44.Cuco G, Fernandez-Ballart J, Sala J, et al. Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. Eur J Clin Nutr 2006;60(3):364–371 [DOI] [PubMed] [Google Scholar]
- 45.MacKenzie TD, Steiner JF, Davidson AJ, Marine WM, Judson FN. Tobacco use and other risk behaviors among adolescents in an STD clinic. Prev Med 1998;27(6):792–797 [DOI] [PubMed] [Google Scholar]
- 46.Ahluwalia IB, Grummer-Strawn L, Scanlon KS. Exposure to environmental tobacco smoke and birth outcome: increased effects on pregnant women aged 30 years or older. Am J Epidemiol 1997;146(1):42–47 [DOI] [PubMed] [Google Scholar]
- 47.Windham GC, Hopkins B, Fenster L, Swan SH. Prenatal active or passive tobacco smoke exposure and the risk of preterm delivery or low birth weight. Epidemiology 2000;11(4):427–433 [DOI] [PubMed] [Google Scholar]
- 48.Ananth CV, Kirby RS, Kinzler WL. Divergent trends in maternal cigarette smoking during pregnancy: United States 1990–99. Paediatr Perinat Epidemiol 2005;19(1):19–26 [DOI] [PubMed] [Google Scholar]
- 49.England LJ, Grauman A, Qian C, et al. Misclassification of maternal smoking status and its effects on an epidemiologic study of pregnancy outcomes. Nicotine Tob Res. 2007;9(10):1005–1013 [DOI] [PubMed] [Google Scholar]
- 50.Jedrychowski W, Whyatt RM, Cooper TB, Flak E, Perera FP. Exposure misclassification error in studies on prenatal effects of tobacco smoking in pregnancy and the birth weight of children. J Expo Anal Environ Epidemiol 1998;8(3):347–357 [PubMed] [Google Scholar]
- 51.Hakim RB, Tielsch JM, See LC. Agreement between maternal interview– and medical record–based gestational age. Am J Epidemiol 1992;136(5):566–573 [DOI] [PubMed] [Google Scholar]
- 52.Northam S, Knapp TR. The reliability and validity of birth certificates. J Obstet Gynecol Neonatal Nurs 2006;35(1):3–12 [DOI] [PubMed] [Google Scholar]
- 53.Pearl M, Wier ML, Kharrazi M. Assessing the quality of last menstrual period date on California birth records. Paediatr Perinat Epidemiol 2007;21(suppl 2):50–61 [DOI] [PubMed] [Google Scholar]