Abstract
Background
Millions of people seek emergency department care for injuries each year, the majority for minor injuries. Little is known about the effect of psychiatric co-morbid disorders that emerge after minor injury on functional recovery. This study examined the effect of post-injury depression on return to pre-injury levels of function.
Method
This was a longitudinal cohort study with follow-up at 3, 6, and 12 months post-injury: 275 adults were randomly selected from those presenting to the emergency department with minor injury; 248 were retained over the post-injury year. Function was measured with the Functional Status Questionnaire. Psychiatric disorders were diagnosed using the Structured Clinical Interview for DSM IV-TR disorders (SCID).
Results
18.1% (95%CI 13.3 – 22.9) were diagnosed with depression during the post-injury year. Adjusting for clinical and demographic covariates, the depressed group was less likely to return to pre-injury levels of activities of daily living (OR 8.37, 95%CI 3.78 – 18.53) and instrumental activities of daily living (OR 3.25, 95%CI 1.44 – 7.31); less likely to return to pre-injury work status (OR 2.37, 95%CI 1.04 – 5.38); and were more likely to spend days in bed because of health (OR 2.41, 95%CI 1.15 – 5.07).
Conclusions
Depression was the most frequent psychiatric diagnosis in the year after minor injury requiring emergency care. Individuals with depression did not return to pre-injury levels of function during the post-injury year.
Injuries threaten health worldwide; eight of the 15 leading causes of death for people between the ages of 15 and 29 years are injury-related (WHO, 2007). For every injury-related death, hundreds of people seek medical care. In the United States, approximately 30 million Americans seek care for injury in emergency departments (ED) annually (CDC, 2005). The majority of injuries are minor and are not life threatening. However, the emotional and functional impact of minor injury may be considerable. While many individuals are thought to fully recover from minor injuries, an appreciable number may not recover completely (Mooney et al. 2005).
Patients with minor injuries are generally treated and discharged from the ED with instructions for follow-up with their primary or specialty care provider. Emergency care focuses exclusively on treatment of the physical injury and little follow-up assessment is made regarding emotional or functional outcome. The focused evaluation in the ED is not unexpected given the burden currently on the emergency care system (Committee on the Future of Emergency Care, 2007). This narrow focus, however, may contribute to sub-optimal recovery.
Most studies of functional recovery after injury have focused on specific at-risk groups such as older adults (Kempen et al. 2003; De Jonge et al 2006), serious injury patients (Rapoport et al. 2006), or assault victims (Elklit, 2002). Studies indicate that psychological responses to injury are common and may contribute to impaired function. These studies focus primarily on serious injury, thus a substantial gap in knowledge about the millions of patients who sustain minor injuries exists and excess disability from these injuries and related psychological responses could have considerable public health ramifications. The purpose of this study was to describe the influence of post-injury depression on functional recovery in the year after minor injury. We hypothesized that individuals who have post-injury depression would be less likely to return pre-injury levels of function in the year after minor injury when compared to than individuals without post-injury depression.
Methods
This prospective cohort study followed participants for 12 months after minor injury. The study was approved by the Institutional Review Board of the University of Pennsylvania.
Setting
Participants were recruited from a University hospital ED that treats approximately 57,000 patients yearly. All patients seen arriving at the ED were triaged immediately upon arrival and assigned a preliminary diagnosis.
Participants
Participants were enrolled over 4.5 years (October 2002 – March, 2007); follow-up was completed by March, 2008. Adults age 18 years and older who presented for care or a minor injury to the ED were candidates for inclusion. Minor injury was defined as an anatomical injury with an injury severity score (ISS) of 2–8 and normal physiology, defined by a triage-Revised Trauma Score of 12. The ISS is derived from injury severity across 6 body systems; scores range from 1 (least severe) to 75 (most severe) (Baker et al. 1974; Baker & O’Neil, 1976). The triage-Revised Trauma Score is based on systolic blood pressure, respiratory rate, and Glasgow Coma Scale (Champion et al 1989). Only patients with a normal triage-Revised Trauma Score of 12 qualified for the study and this score indicated normal mental status. The combination of a triage-Revised Trauma Score of 12 and an ISS 2–8 provided a cohort of patients with truly minor injury based on an internationally accepted standard classification (Kilgo et al. 2006). Blood alcohol levels were not routinely drawn in practice and were not drawn for the purpose of this study however no patients considered for this study were intoxicated at the level that affected cognition. Patients were excluded if they reported a physical injury requiring ED care in the prior 2 years, a current injury directly resulting from a concurrent medical illness or domestic violence, current major depressive or psychotic disorder.
Variables - Data Sources/Measurements
Standard demographic and injury data were obtained from the ED record. Pre-injury and post-injury function were measured with the Functional Status Questionnaire (FSQ; Cleary & Jette, 2003) a generic measure used across diseases (Murphy et al. 1998). The FSQ provides a comprehensive assessment of physical (activities of daily living), role (instrumental activities of daily living), psychosocial (well-being), and social functioning across 6 subscales, and measures of work performance, social function, and social interaction. It includes items on bed disability days, days lost from usual activities, and an overall assessment of health status. Scores were transformed to a scale of 0 to 100 with higher scores indicating higher levels of function. Reliability, construct and criterion validity are well established (Jette et al. 1986; Jette & Cleary, 1987).
The Structured Clinical Interview for the Diagnostic Statistical Manual-IV (DSM-IV-TR) Axis I Disorders, Patient Version (SCID) is a semi-structured psychiatric interview that yields judgments with respect to all five axes of the DSM IV (APA, 1994; First et al. 1994). It served as the primary instrument for psychiatric diagnostic case ascertainment (Zimmerman et al. 1986). The SCID captured alcohol and/or drug use, abuse, and dependence.
The Longitudinal Interval Follow-up Evaluation (LIFE) (Keller et al. 1987) was used to detect emergence of a new psychiatric disorder during the post-injury year. The LIFE provides an interval, retrospective diagnostic assessment based upon a semi-structured interview. LIFE screens for depression, mania/hypomania, psychotic disorders, anxiety disorders, posttraumatic stress disorder, alcohol and substance use disorders. When participants screened positive on LIFE, the full module of the SCID was used for diagnostic verification.
Social support was measured by the brief version of Social Support Questionnaire (Sarason, Sarason, Shearin, Pierce, 1987). The brief version is a 6-item psychometrically sound instrument that has performed well in ethnically diverse samples (Richmond & Kauder, 2000). Social network scores range from 0 to 54 and support scores from 0 to 6.
Procedure
Consecutively admitted patients with a triage diagnosis of injury had the ISS and the triage-Revised Trauma Score calculated in the ED, under the supervision of the attending ED physician. All patients with an injury triage diagnosis, and ISS of 2–8 and a triage-Revised Trauma score of 12 underwent a brief screening interview in the ED to establish inclusion and exclusion criteria. Patients were asked if they had a history of psychiatric disorders, if they were being treated for a current psychiatric disorder, and to report any injuries they had experienced in the previous 2 years. Those who reported a current depression, psychotic disorder, or an injury requiring care in an ED in the previous 2 years were excluded from the sample at this point. Those meeting entry criteria were given a general description of the study by our enrollment team (Hollander et al. 2004) and were asked for verbal permission to release their contact information to the research team. At this time we obtained injury information from the ED record and all potential participants completed the FSQ to document pre-injury level of function to reduce recall bias, This technique of acquiring pre-injury information has been widely used in injury studies to obtain the patient’s pre-injury level of function (Holbrook et al. 1999; MacKenzie et al. 1987; Richmond, 1997). This group served as the population from whom the sample was randomly drawn.
Intake data were confidentially faxed to the research team. Because the intensity of follow-up precluded the use of a consecutive sample, we enrolled 6.41 patients a month based on a computerized randomization protocol (using STATA’s built in random number generator). This protocol generated a list of 114 random numbers (STATA software) that correspond with hours 1 through 114 within each 4.75 day block. The smallest random number within a block identified the enrollment hour used for each 4.75 day period. The randomization was automatically weighted to reflect the flow of patients into the ED (85% arrive between 8am and 12 midnight). When randomly selected, the study coordinator called the randomly selected patient, explained the study and answered all questions. If verbal consent was provided, an appointment for the in-person intake interview was made. If consent was not provided, the patient with the next treatment room admission time closest to the randomly selected date and time was enrolled.
Psychiatric diagnostic interviews were performed by one social worker with over 30 years of experience in this area. For this study, he had 40 hours of additional training at the Depression Research Unit at the University of Pennsylvania. Training included reviewing SCID I and II interview training tapes with scoring; administering and videotaping practice SCIDs to students and clinic patients; supervising his taped interviews; and training on the LIFE. Training was considered complete when all diagnoses (or absence of diagnoses) concurred with the study psychiatrist. During the study, on 10 occasions diagnostic queries or patient-related concerns were resolved by consensus between the diagnostic rater and the study psychiatrist. Less urgent questions were discussed during monthly team meetings that were attended by the interviewer, principal investigator, and study psychiatrist. At this time, the interviewer and study psychiatrist reviewed the diagnoses to assure accuracy.
The SCID intake interview was conducted within 1–2 weeks of the ED visit. Written informed consent was obtained. Participants completed detailed demographic and injury data, underwent the Structured Clinical Interview Diagnosis (SCID) and completed the post-injury FSQ and other covariate instruments (e.g., social support, drug and alcohol use). All interviews were face-to-face. The intake interview was specifically scheduled within 2 weeks of the injury in order to eliminate participants who met criteria for a current major depressive episode (meaning that they had a major depression at the time of injury). If so, they were discontinued from the study and not included in the analysis. At interview completion, participants were told to call the study team prior to the next visit if they experienced any physical or emotional problems that concerned them. Face-to-face follow-up interviews were conducted at 3, 6, and 12 months after injury to diagnostically determine if a depression emerged in the interim time periods. The LIFE was used at follow-up interviews and if participants screened positive for a new disorder, the full SCID module was used to determine if diagnostic criteria were met. At each interview, FSQ measures focused on the month prior to the visit. Incentives to continue participation in the study were provided at the completion of each interview with payment of $30, $30, $30 & $60 (intake, 3, 6, & 12 months, respectively).
Statistical methods
Sample size calculations were conducted using Nquery sample size calculation software based on the premise that 15% of participants would have depression (Elashoff, 1999). For a comparison of means between participants who did and did not have depression, based on a one-sided two sample t-test with 250 participants there was 80% power, with α = 0.05 to detect an effect size of 0.44 SD.
Frequencies with 95% confidence intervals (95%CI) described the proportion of participants diagnosed with a depression in the year after injury. Participants were categorized as depressed if they met diagnostic criteria for a major depressive disorder, depression not otherwise specific (NOS), or dysthymia. Means and standard deviations (SD) for all function measures for the depressed and non-depressed groups were calculated and compared using t-tests.
To test the hypothesis that individuals with depression in the post-injury year would be less likely to return to their pre-injury levels of function, the individual was placed in the depressed group if the symptoms leading to the diagnosis emerged prior to the structured interview at 3, 6, or 12 months. Regardless of whether the depression resolved, the individual remained coded as depressed for the remainder of the analyses. Thus, the diagnosis of depression was determined to precede the outcome of return to pre-injury function. Function, as measured by the FSQ consisted of several subscales and each scale was dichotomized to yes/no on return to pre-injury baseline of function. This allowed each participant to serve as his/her own control.
Clinically and theoretically relevant covariates, present prior to or as a result of the injury were included in the multivariate models. All covariates (see Table 1) were entered into the multivariate logistic regressions. No significant interactions were found. To be the most conservative, we also used the pre-injury FSQ scores as a covariate minimize potentially spurious effects of varying levels pre-injury function.
Table 1.
Pre-Injury & Injury Co-Variates in the Multivariate Models (n=275 unless otherwise noted)
| Variable | Mean (SD) | |
|---|---|---|
| Age | 40.4 (16.8) | |
|
| ||
| Years of Education | 13.7 (2.65) | |
|
| ||
| Pre-Injury Function – FSQ Activities of Daily Living Scale | 96.8 (10.5) | |
|
| ||
| Pre-Injury Function – FSQ Instrumental Activities of Daily Living Scale | 89.5 (20.7) | |
|
| ||
| Pre-Injury Mental Health - FSQ Wellbeing Scale | 79.4 (17.1) | |
|
| ||
| Pre-Injury Social Activity - FSQ Social Activity Scale | 91.5 (20.8) | |
|
| ||
| Pre-Injury Quality of Interaction – FSQ Quality of Interaction Scale | 83.2 (16.8) | |
|
| ||
| # of Days Spent in Bed in the Month prior to Injury | 0.66 (2.03) | |
|
| ||
| # of Days with Reduced Activities due to Health in the Month Prior to Injury | 1.13 (3.20) | |
|
| ||
| Number Injuries Treated over Lifetime in ED | 3.14 (3.69) | |
|
| ||
| Size of Social Network | 22.1 (12.4) | |
|
| ||
| Satisfaction with Social Network | 5.73 (0.56) | |
|
| ||
| Categorical Variables | % | |
| Gender | Male | 51.6% |
| Female | 48.4% | |
|
| ||
| Injury Type | Extremity Injury involving fracture | 63.3% |
| No fractured extremity | 36.7 | |
|
| ||
| Marital Status | Not married | 74.2% |
| Married | 25.8% | |
|
| ||
| Feelings About Health at Intake | Satisfied | 89.8% |
| Dissatisfied | 10.2% | |
|
| ||
| Frequency Getting Together With Friends/Relatives - Month Prior to Injury | Not at All | 3.3% |
| Once a Month | 8.4% | |
| 2 or 3 Times a Month | 12% | |
| Once a week | 13.5% | |
| Several Times a Week | 40.4% | |
| Every Day | 22.5% | |
|
| ||
| Satisfaction With Sexual Relationships (n=202), PreInjury | Satisfied | 95.6% |
| Dissatisfied | 4.4% | |
|
| ||
| Pre-injury Work Status | Working Part or Full time | 69.8% |
| Unemployed | 30.2% | |
|
| ||
| Pre-Injury Health Rating Compared with prior 12 months | Better | 16.7% |
| Worse | 12.7% | |
| About the Same | 70.5% | |
|
| ||
| Anticipates Problems after Injury | No | 56% |
| Yes | 44% | |
|
| ||
| Location of Injury | Home | 20.4% |
| Workplace | 14.9% | |
| School | 2.2% | |
| On Street | 53.8% | |
| Other | 8.7% | |
|
| ||
| Injury Intent | Intentional Injury | 9.1% |
| Unintentional Injury | 90.9% | |
|
| ||
| DSM-IV Disorder at Intake | No Disorder | 84.4% |
| DSM-IV Disorder | 15.6% | |
|
| ||
| History of DSM-IV Disorder | No History | 70.9% |
| History of Disorder | 29.1% | |
|
| ||
| Admitted to Hospital from ED | Yes | 10.5% |
| No | 89.5% | |
Significance was set at p<0.05 for the final multivariate models. The mood disorder indicator was forced to be in the model regardless of the significance level. Other non-significant variables were removed from the models to obtain final odds ratios. To guard against the potential inflated Type 1 error, we verified significance by performing a longitudinal analysis using Generalized Estimating Equations (Liang & Zeeker, 1986).
Results
Participants
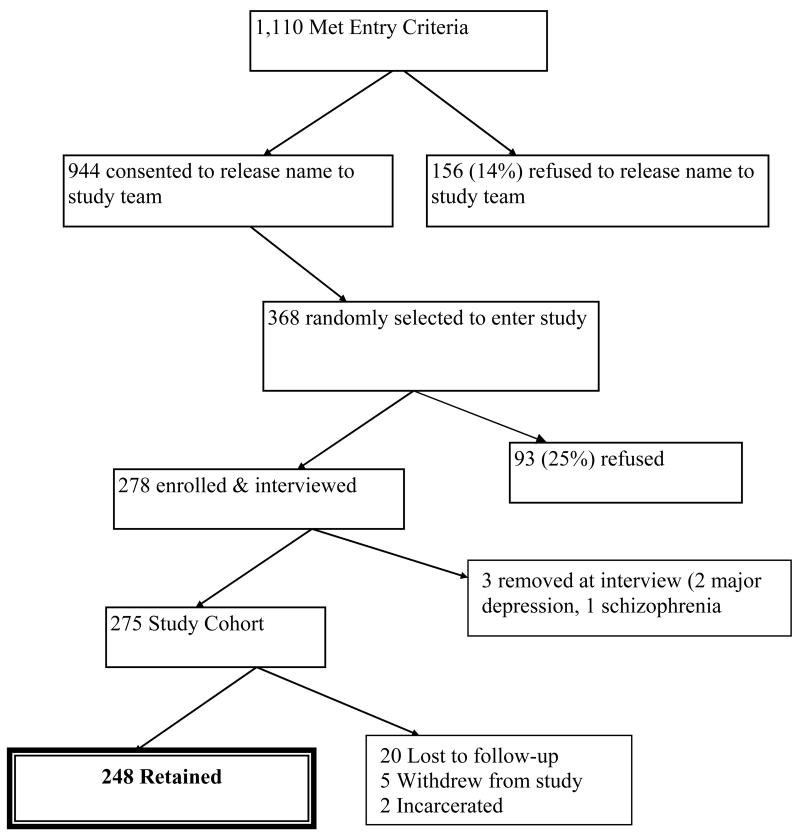
Three hundred and sixty-eight patients were randomly selected for study entry. (see Figure 1) Of these, 278 agreed to participate in the study. Three were excluded from the study at the intake diagnostic interview (1 for major depression; 2 for schizophrenia). The final sample of 275 consisted of 142 men (52%) and 133 women (48%). The majority was single (53%) and employed (71%) with only 10% of the sample unemployed. Over half of the sample was Black (57%), then Caucasian (40%) and Asian (3%). The mean education level was 13.7 years (sd = 2.7). Income level was evenly distributed: 32.1% earning less than $20,000 per year, 22.8% earning >$60,000 per year, and 45.1% falling in between. The dominant injury cause was a slip or fall (48%) followed by motor vehicle/pedestrian/bike crash (28.7%), sports (8.4%) and assaults (8%). The mean ISS was 4.1 (sd=1.1). Twenty-nine of the participants (11.7%) were admitted to the hospital from the ED.
Figure 1.
Sampling Tree
Follow-up data were obtained from 248 (90%) individuals, although some of these participants may have missed one of the three follow-up visits (240 at 3mo., 235 at 6mo., 238 at 12mo.). T-tests, analysis of variance, chi square and Fisher’s exact tests were used to compare participants who completed the study and those who were lost to follow-up. Individuals lost to follow-up were more likely (p<.05) to be male, injured via motor vehicle crash, have a less severe injury, and have a mean of 1.5 years less education than those who completed the study.
Descriptive Data
Fifty-seven participants (23%; 95% CI 17.7, 28.2%) were diagnosed with a post-injury DSM IV-TR Axis 1 disorder (see table 2). These diagnoses included mood (78.9%), substance abuse (3.6%), anxiety (2.8%), and adjustment disorders (0.4%). Among the sample for whom there were follow-up data, 18.1% (45/248; 95% CI 13.3, 22.9%) had a depression. Of those diagnosed with mood disorders (n=45), 26.7% had major depressive disorder (MDD), 40% Depression NOS, and 33.3% dysthymia. Four participants had an Axis 1 disorder co-morbid with depression: 2 with posttraumatic stress disorder, 1 with generalized anxiety disorder, and 1 with alcohol abuse.
Table 2.
Frequency of Axis I Disorders Present in the Year after Injury
| Disorder | Proportion of total sample (n = 248) N (%) | Diagnosed Disorder as Proportion of those with Axis 1 Disorders (n = 57) N (%) |
|---|---|---|
| Mood | 45 (18.1) | 45 (78.9) |
| Mood Disorders | ||
| Major Depression Disorder | 12/45 (26.7) | |
| Depression, NOS | 18/45 (40.0) | |
| Dysthymia | 15/45 (33.3) | |
|
| ||
| Anxiety | 7 (2.8) | 7 (12.3) |
| Anxiety Disorders | ||
| PTSD | 6/7 (85.7) | |
| Generalized anxiety | 1/7 (14.3) | |
|
| ||
| Substance Abuse | 9 (3.6) | 9 (15.8) |
| Substance Abuse Disorders | ||
| Alcohol | 6/9 (66.7) | |
| Drug | 3/9 (33.3) | |
|
| ||
| Adjustment Disorder | 1 (0.4) | 1 (1.8) |
| Anxious Mood | 1/1 (100) | |
Four persons had co-morbid diagnoses (MDD & anxiety; MDD & PTSD; Dep NOS & PTSD; Dysthymia, alcohol, substance)
The depressed and non-depressed groups were compared at each time point (see table 3). There were no differences in any pre-injury function subscales between the two groups. Post-injury function was significantly lower at all post-injury time points for the depressed group, with the exception of work status at 6 months.
Table 3.
Comparison of Depressed and Non-Depressed Patients on Function at 3, 6 and 12 months
| Variable | Depressed | Not Depressed |
|---|---|---|
| Time point | Mean (SD) | Mean (SD) |
| Pre-injury N = 45 | Pre-injury N = 203 | |
| 3mo N = 30 | 3mo N = 210 | |
| 6mo N = 42 | 6 mo N = 189 | |
| 12mo N = 45 | 12 mo N = 190 | |
|
| ||
| Function (FSQ)-Activities of Daily Living Scale | ||
| Pre-injury | 95.6 (14.1) | 97.3 (9.44) |
| 3 mo | 84.6 (21.4)* | 92.9 (15.3) |
| 6 mo | 86.0 (21.4)* | 95.2 (14.4) |
| 12 mo | 89.1 (15.4)* | 96.2 (13.9) |
|
| ||
| Function (FSQ)- Instrumental Activities of Daily Living Scale | ||
| Pre-injury | 85.7 (24.6) | 90.1 (20.6) |
| 3 mo | 62.3 (29.3)* | 77.0 (26.3) |
| 6 mo | 65.5 (31.8)** | 84.2 (22.7) |
| 12 mo | 73.0 (31.2)** | 85.9 (21.7) |
|
| ||
| Function (FSQ) - Mental Health Scale | ||
| Pre-injury | 67.3 (22.3) | 82.5 (14.2) |
| 3 mo | 56.6 (20.4)** | 81.0 (15.5) |
| 6 mo | 56.6 (19.0)** | 84.6 (14.1) |
| 12 mo | 60.2 (16.5)** | 82.3 (16.8) |
|
| ||
| Function (FSQ) - Social Activity Scale | ||
| Pre-injury | 86.2 (26.9) | 92.0 (20.1) |
| 3 mo | 64.4 (31.7)* | 79.2 (29.5) |
| 6 mo | 65.3 (36.3)** | 84.6 (28.0) |
| 12 mo | 68.7 (35.6)** | 86.3 (26.6) |
|
| ||
| Function (FSQ) - Social Interaction Scale | ||
| Pre-injury | 74.5 (20.5) | 86.1 (14.6) |
| 3 mo | 63.2 (16.6)** | 82.4 (14.2) |
| 6 mo | 64.0 (18.5)** | 84.7 (14.5) |
| 12 mo | 66.1 (19.7)** | 83.3 (15.6) |
|
| ||
| Function (FSQ) - Work Status Scale | ||
| Pre-injury | 91.7 (13.9) | 94.5 (10.0) |
| 3mo | 73.5 (20.7)** | 88.6 (14.5) |
| 6mo | 88.1 (11.7) | 92.3 (12.2) |
| 12mo | 87.9 (15.7)* | 94.3 (8.8) |
To determine if those diagnosed as depressed in the post-injury year differed in pre-injury function, all 45 diagnosed as depressed at any time in the post-injury year were compared to those who were never depressed at any time in the post-injury year.
FSQ– higher scores reflect higher levels of function and QOL respectively.
Significance
p <0.01;
p<0.001
Participants diagnosed with depression were only included in the depressed group if the depression was diagnosed prior to the assessment of function, After adjusting for co-variates, depression was found to significantly and consistently increase the odds of not returning to pre-injury baseline levels of function in all functional domains (see table 4). The impact of depression on return to function was negative, sustained, and significant.
Table 4.
Post-Injury Effect of Depression Diagnosis on the Primary Outcome of Return to Pre-injury Level of Function Logistic Regression Analysis, Adjusting for Key Pre-injury & Injury Related Factors
| Outcome | Variable | Adjusted Odds Ratios (95% Confidence Intervals) | ||
|---|---|---|---|---|
| 3 months | 6 months | 12 months | ||
| Activities of Daily Living lower than pre-injury | Depressed Y/N | 3.17 (1.25 – 8.01)*/Ref | 4.09 (1.80 – 9.27)***/Ref | 8.37 (3.78 – 18.53)****/Ref |
| Extremity injury Y/N | 4.129 (1.87 – 9.05)****/Ref | -- | -- | |
| Anticipate problem Y//N | 2.06 (1.10 – 3.88)*/Ref | 3.52 (1.57 – 7.88)** | -- | |
| Hospitalized Y/N | 3.92 (1.65 – 9.32)**/Ref | -- | -- | |
| # Activity days cut down pre-injury | 1.14 (1.02 – 1.28)*/Ref | -- | -- | |
| Social Network Size | -- | 0.96 (0.93 –0.99)* | -- | |
| Age in years | -- | 1.04 (1.02 – 1.06)***/Ref | -- | |
| Pre-injury IADL | -- | -- | 0.98 (0.96 – 0.99)** | |
| Pre-injury time with friends | -- | -- | 0.73 (0.54 – 0.92)* | |
|
| ||||
| Instrumental Activities of Daily Living lower than pre-injury | Depressed Y/N | 1.56 (0.64 – 3.81)/Ref | 3.20 (1.48 – 6.93)**/Ref | 3.25 (1.44 – 7.31)**/Ref |
| Hospitalized Y/N | 5.56 (1.88 – 16.45)***/Ref | -- | -- | |
| Pre-injury IADL | 1.04 (1.02 – 1.05)**** | 1.05 (1.03 – 1.07)**** | 1.06 (1.03 – 1.08)**** | |
| Anticipate problem Y//N | 2.07 (1.17 – 3.65)* | -- | -- | |
| Age in years | -- | 1.04 (1.02 – 1.05)**** | 1.05 (1.03 – 1.07)**** | |
| Years of Education | -- | -.84 (0.75 – 0.94)*** | 0.81 (0.71 – 0.91)*** | |
| Gender Female/Male-Ref | -- | -- | 2.94 (1.55 – 5.58)*** | |
| # times met with friends pre-injury | -- | -- | 0.73 (0.57 – 0.94)* | |
|
| ||||
| Fewer social activities than pre-injury | Depressed Y/N | 1.98 (0.83 – 4.75)/Ref | 3.98 (1.89 – 8.38)****/Ref | 3.08 (1.42 – 6.70)**/Ref |
| Hospitalized Y/N | 3.60 (1.43 – 9.04)**/Ref | -- | -- | |
| Extremity injury Y/N | 2.72 (1.47 – 5.02)***/Ref | -- | -- | |
| Social activities pre-injury | 1.03 (1.01 – 1.04)** | 1.03 (1.01 – 1.05)** | 1.04 (1.01 – 1.07)** | |
| Years of Education | 0.87 (0.78 – 0.97)** | -- | 0.77 (0.67 – 0.88)**** | |
| # ED visits for injury over lifetime | -- | 1.10 (1.02 – 1.19)* | -- | |
| # Activity days cut down pre-injury | -- | -- | 1.15 (1.03 – 1.28)* | |
|
| ||||
| Quality of Social interaction lower than pre-injury | Depressed Y/N | 9.34 (2.26 – 38.62)**/Ref | 3.41 (1.29 – 9.02)*/Ref | 6.48 (2.35 – 17.89)****/Ref |
| Intentional Injury Y/N | 11.91 (2.10 – 67.72)**/Ref | 5.19 (1.30 – 20.78)*/Ref | 11.02 (2.39 = 50.87)**/Ref | |
| Anticipate problem Y//N | 4.06 (1.99 – 8.26)****/Ref | 2.11 (1.13 – 3.95)*/Ref | -- | |
| Quality of social interaction pre-injury | 1.11 (1.08 – 1.14)****/Ref | 1.08 (1.05 – 1.11)****/Ref | 1.10 (1.07 – 1.13)*** | |
| Social activities pre-injury | -- | -- | -- | |
|
| ||||
| Did not return to pre-injury work status++ | Depressed Y/N | 1.33 (0.38 – 4.66)/Ref | 2.68 (1.07 – 6.70)*/Ref | 2.37 (1.04 – 5.38)*/Ref |
| Anticipate problem Y//N | 2.84 (1.37 – 5.88)**/Ref | -- | -- | |
| Years of education | 0.80 (0.70 – 0.92)*** | 0.78 (0.69 – 0.90)**** | 0.85 (0.75 – 0.97)* | |
| Past history of psychiatric disorder | -- | -- | 2.24 (1.10 – 4.50)*/Ref | |
|
| ||||
| More days spent in bed because of illness or injury, in the month prior to interview | Depressed Y/N | 2.66 (1.11 – 6.37)*/Ref | 3.59 (1.62 – 7.95)**/Ref | 2.41 (1.15 – 5.07)*/Ref |
|
| ||||
| More days with cut down on usual activities for one-half or more days in the month before interview | Depressed Y/N | 2.64 (1.16 – 6.02)*/Ref | 1.39 (0.64 –3.04)/Ref | 2.89 (1.30 – 6.45)**/Ref |
| Anticipate problem Y//N | 3.05 (1.71 – 5.44)****/Ref | 2.25 (1.16 – 4.37)*/Ref | 2.14 (1.08 – 4.27)*/Ref | |
| Hospitalized Y/N | 2.57 (1.12 – 5.91)*/Ref | -- | -- | |
| Years of education | -- | 0.86 (0.75 – 0.97)* | -- | |
| Pre-injury ADL | -- | -- | 0.96 (0.93 -0.99)* | |
| # Activity days cut down pre-injury | -- | -- | 0.80 (0.66 – 0.97)* | |
|
| ||||
| Feeling less healthful at the time of interview than pre-injury | Depressed Y/N | 2.60 (1.00 – 6.75)*/Ref | 1.44 (0.67 – 3.09)/Ref | 1.92 (0.87 - 4.25)/Ref |
| Anticipate problem Y//N | -- | 2.80 (1.54 – 5.08)***/Ref | 2.63 (1.42 – 4.85)**/Ref | |
| Gender Female/Male-ref | -- | 1.85 (1.04 – 3.30)*/Ref | -- | |
| # Activity days cut down pre-injury | -- | 0.86 (0.74 – 0.98)* | 0.81 (0.69 – 0.96)* | |
| # ED visits for injury over lifetime | -- | -- | 0.88 (0.79 – 0.98)* | |
|
| ||||
| Connects less frequently with friends or relatives in person or by telephone than pre-injury | Depressed Y/N | 2.43 (0.96 – 6.12)/Ref | 1.18 (0.53 – 2.63)/Ref | 2.36 (1.02 – 5.49)*\Ref |
| Pre-injury sexual dissatisfaction Y/N | 5.37 (1.05 – 27.48)*/Ref | -- | -- | |
| Pre-injury time with friends | 2.45 (1.79 – 3.34)*** | 2.23 (1.66 – 3.00)**** | 2.67 (1.90 – 3.76)**** | |
| Married Y/N | 1.97 (1.01 – 3.85)*/Ref | -- | -- | |
| Working pre-injury Y/N | 0.49 (0.25 – 0.95)* | -- | -- | |
| Years of education | -- | 0.89 (0.80 – 1.00)* | 0.81 (0.71 – 0.92)*** | |
| Pre-injury IADL | -- | -- | 1.04 (1.02 – 1.06)*** | |
Key for Abbreviations: IADL = Instrumental Activities of Daily Living Scale; ADL = Activities of Daily Living
Key for Non-Categorical Variable Scoring included in the models: Scales for Pre-Injury IADL, Pre-injury Quality of Social Activity, Pre-Injury Social Activities, Pre-injury ADL, and Pre-injury Work all range from 0 – 100 with higher scores reflecting higher levels of function. All other continuous variables are self-explanatory (i.e. age in years, educational level in years, # of people in the social network, # of activity days cut down, and # of days spent in bed)
Based on the 171 participants working at time of injury
p<0.05;
p<0.01;
p<0.001;
p<0.0001
As seen in table 4, depression affected many domains of function at 3 months, but other factors such as the presence of an extremity injury, a cause of injury that was intentional, or hospitalization exerted stronger effects on return to function. However, by 6 months, depression was the dominant contributor to the inability to return to pre-injury levels of function and this continued through the 12 months after injury.
At one year post-injury, participants who had ever been diagnosed with depression were 8 times more likely to not return to baseline activities of daily living, 3 times more likely to not return to baseline instrumental activities of daily living, over 6 times more likely to not return to baseline quality of social interaction, 3 times more likely to have a lower level of social interaction, and were almost 3 times more likely to have cut down on activities usually performed. Of the 171 individuals working at the time of injury, the depressed group was 2.3 times more likely to not return to their pre-injury work status at 1 year post-injury.
Discussion
We examined the effect of post-injury depressive disorders on functional recovery after minor physical injury. Using structured diagnostic interview techniques, 18% of patients were diagnosed with a mood disorder (major depression, depression NOS, dysthymia) in the year after minor injury. Individuals with depression were less likely to return to pre-injury levels of function at one year post-injury. This finding expands the growing literature showing the impact of acute psychological responses to injury on subsequent levels of function (O’Donnell et al. 2005; Van Gool et al. 2005), and indicates that the impact of post-injury depression is not limited to patients with serious injury.
The use of a semi-structured interview to determine the presence or emergence of a DSM IV-TR Axis 1 diagnosis is a strength of this study and overcomes the limitations of earlier studies that assessed only psychiatric symptom severity (Mason et al. 2002). Using structured diagnostic interviews to establish all Axis 1 disorders allowed us to comprehensively assess the broad range of psychiatric consequences that may occur after injury. In contrast to the substantial body of research that has focused on posttraumatic stress disorder (Bisson et al. 2004; Hepp et al. 2005; Carty et al. 2006), our findings indicate that depression was the predominant diagnosis in the post-injury year. Further, in contrast to other studies that report high co-morbidity between depression and PTSD (O’Donnell et al. 2004; Shalev et al. 1998), only two participants were found to have this co-morbidity. The literature indicates that serious injury is not a pre-requisite for PTSD, and in fact, PTSD occurs in the absence of physical injury. However, it is likely that the mechanisms leading to injury in this study were insufficient to invoke a person’s response as one of intense fear, helplessness or horror (APA, 1994).
Depression that is co-morbid with chronic physical illness significantly increases functional disability (Stein et al. 2006). Our study adds to this literature in that it focuses on an acute event (injury) and demonstrates that even after controlling for important covariates, individuals diagnosed with depression are significantly less likely to return to pre-injury levels of function. Since injury is temporally grounded at a point of time, we were able to determine that the depression preceded subsequent assessments of return to function. Once coded as depressed, the case remained in the depressed group, and thus the value of the prospective follow-up design is that it allowed us to examine temporal patterns of the emergence of depression and its subsequent effect on function.
Previous studies have demonstrated an increase in health care costs in the two years following motor vehicle crashes in patients with PTSD, not through its independent contribution to costs, but perhaps by its effect on physical health (O’Donnell et al. 2005). Our study was not designed to assess the health care costs post-injury. However, our findings suggest that there is a potential and significant economic impact due to the sustained effect of depression on not returning to pre-injury work status and increased number of days spent in bed than pre-injury. Both of these findings indicate the economic impact of depression following injury and require further exploration.
This study was designed to be a naturalistic follow-up study and did not include an intervention arm. Participants who were diagnosed with a new or worsened disorder were formally notified of the diagnosis with the recommendation that they follow-up with their primary health care provider. In the absence of an existing health care provider a referral for treatment was offered.
Limitations
Previous research has been hampered by using outcomes measures with mental health scales embedded. In this study, the Functional Status Questionnaire was selected to measure the primary outcome, to allow us to remove the mental health/well-being scale from the analysis of outcomes, which would have potentially inflated the effect of depression. We did, however, include the pre-injury mental health/well-being subscale as a covariate in the multivariate models to more rigorously examine the effects of post-injury depression on return to function.
The directionality of effect can be argued: Does depression worsen function or does poor function increase depression (Scaf-Klomp et al. 2003)? In this prospective study, the use of repeated measures in the year following injury allowed us to verify the onset of depression prior to measuring outcomes. Finally, although this study controlled for many covariates, the presence of pain and its severity was not measured. Pain can possibly contribute to impaired function (Arinzon et al. 2007; Soberg et al. 2007;Read et al. 2007) either directly or indirectly (Fishbain et al. 2003), and future studies should explicitly examine the potential interaction between pain and depression.
Patients with a major depressive disorder at the time of injury were excluded from the study. Because we assessed patients using a structured interview at intake (within 2 weeks of injury), we were able to definitely exclude anyone with major depression. However, a few patients were included, who had not reported a current depression and were not receiving treatment were found to be dysthymic at the intake SCID interview. Because of this recruitment decision, we verified the robustness of the multivariate models and tested our models both with and without the small group of patients who had a dysthymia at the time of injury and found no substantial difference.
The absence of a general population comparison group was a study limitation. However, the use of a prospective, longitudinal cohort design with repeated measures and with a pre-injury measure of function was a very strong design for testing the hypothesis posed in this study. Our data demonstrate that there was no difference in pre-injury function in participants who did and did not become depressed.
This study had a robust retention (90%). Nonetheless, it is important to take into consideration that the group lost to follow-up was more likely to be male, injured via motor vehicle crash, have a less severe injury, and have 1.5 years less education than those who completed the study. Finally, minor injury accounts for millions of trips to ED annually; this sample was drawn from an urban ED, it is not yet known if these findings would extend to individuals in rural environments.
Bias
The intensity of the psychiatric diagnostic interviews precluded the use of a consecutive sample. To avoid a potential bias inherent in a convenience sample, we randomly drew participants from the population of all minor injury patients in the ED. Race/ethnicity has been known to result in either over- or under-diagnosis of psychiatric disorders (Aklin & Turner, 2006; Flaskerud, 2001; Rosenthal & Berven, 1999). We used structured psychiatric interviews which are shown to minimize bias associated with race/ethnicity (Akpaffiong et al. 1999).
Interpretation
Emergency and trauma providers anticipate that serious, life-threatening injuries are associated with psychological consequences and risk for poor functional recovery. Individuals with minor injuries are primarily treated and released from the ED with the clear expectation that they will quickly and fully recovery with few if any residual effects. The findings of our study demonstrate that not all patients return to pre-injury function and that one of the etiologies of this poor recovery is post-injury depression. Subtypes of depression other than major depression are considered to exert less impact on function (Kessing, 2007), however, we elected to include all subtypes (major depressive disorder, depression NOS, dysthymia) and still found a statistically and clinically significant effect of depression on outcomes.
Depression is a diagnosable and treatable disorder, and as such it represents a modifiable factor that can be targeted to improve post-injury recovery. Collaborative interventions to address post-traumatic emotional disturbances have been tested in hospitalized injured survivors (Zatzick et al. 2001), and these interventions, when indicated, are more likely to be initiated in hospitalized patients. People who sustain minor injury receive care in an ED were classically ‘treated and streeted,’ with referrals for follow-up by specialty services as required by injury type (e.g., orthopedics for extremity fracture), who provide focused care. The silo nature of today’s health care coupled with the discharge of patients from the ED with follow-up by specialty care place minor injury patients at high risk for not having their depression recognized, diagnosed and treated. Given the findings of this study that indicate depression is a major risk for not returning to pre-injury levels of function, it is imperative for primary care providers to carefully assess their patients who have sustained injury and initiate treatment as needed in order to maximize functional recovery after injury.
Acknowledgments
Author Contributions: Dr. Richmond had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Richmond, Amsterdam, Gracias, Hollander, Robinson. Analysis and interpretation of data: Richmond, Guo, Ackerson.
Drafting of the manuscript: Richmond.
Critical revision of the manuscript for important intellectual content: Ackerson, Amsterdam, Gracias, Guo, Hollander, Robinson.
Statistical analysis: Guo, Ackerson.
Study supervision, Richmond, Ackerson.
Financial Disclosures: Dr. Amsterdam currently received research grant support from the NIMH, NIH/NCCAM, Lilly Research Laboratories, Novartis, Inc., and Sanofi-Aventis, Inc. He is on the speaker’s bureau of Wyeth and Bristol-Myers-Squibb.
Funding/Support: This study was funded by the National Institute of Mental Health grant RO1MH63818 (Dr. Richmond).
Role of the Sponsor: The National Institute of Mental Health had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
Funding Source: NIMH R01MH63818 to Dr. Richmond
Footnotes
Publisher's Disclaimer: Manuscript has been accepted for publication and will appear in final form subject to editorial input by Cambridge University Press in Psychological Medicine, which is published by Cambridge University Press, together with a copyright notice in the name of Cambridge University Press.
Contributor Information
Therese S. Richmond, School of Nursing, Biobehavioral & Health Sciences Division, University of Pennsylvania.
Jay D. Amsterdam, School of Medicine, Depression Research Unit, Department of Psychiatry, University of Pennsylvania.
Wensheng Guo, School of Medicine, Department of Clinical Epidemiology & Biostatistics, University of Pennsylvania.
Theimann Ackerson, School of Nursing, University of Pennsylvania.
Vicente Gracias, School of Medicine, Department of Surgery, University of Pennsylvania.
Keith M. Robinson, School of Medicine, Department of Physical Medicine & Rehabilitation, University of Pennsylvania.
Judd E. Hollander, School of Medicine, Department of Emergency Medicine, University of Pennsylvania.
References
- Aklin WM, Turner SM. Towards understanding ethnic and cultural factors in the interviewing process. Psychotherapy: Theory, Research, Practice & Training. 2006;43:50–64. doi: 10.1037/0033-3204.43.1.50. [DOI] [PubMed] [Google Scholar]
- Akpaffiong M, Kunik ME, Hale D, Molinari V, Orengo C. Cross-cultural differences in demented geropsychiatric inpaitents with behavioral disturbances. International Journal of Geriatric Psychiatry. 1999;14:845–850. doi: 10.1002/(sici)1099-1166(199910)14:10<845::aid-gps34>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. DSM IV. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Arinzon Z, Gepstein R, Shabat S, Berner Y. Pain perception during the rehabilitation phase following traumatic hip fracture in elderly is an important prognostic factors and treatment tool. Disability & Rehabilitation. 2007;29:651–658. doi: 10.1080/09638280600926470. [DOI] [PubMed] [Google Scholar]
- Baker SP, O’Neill B, Haddon W, Long W. The Injury Severity Score: A method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- Baker SP, O’Neill B. The Injury Severity Score: An update. Journal of Trauma. 1976;16:882–885. doi: 10.1097/00005373-197611000-00006. [DOI] [PubMed] [Google Scholar]
- Bisson JI, Shepher JP, Joy D, Probert R, Newcombe RG. Early behavioural-cognitive therapy for post-traumatic stress symptoms after physical injury. British Journal of Psychiatry. 2004;184:63–69. doi: 10.1192/bjp.184.1.63. [DOI] [PubMed] [Google Scholar]
- Carty J, O’Donnell ML, Creamer M. Delayed-onset PTSD: A prospective study of injury survivors. Journal of Affective Disorders. 2006;90:257–261. doi: 10.1016/j.jad.2005.11.011. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. CDC Protecting Health for Life: The State of the CDC, Fiscal Year 2004. CDC; Atlanta, GA: 2005. [Google Scholar]
- Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the trauma score. Journal of Trauma. 1989;29:623–629. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- Cleary PD, Jette AM. Reliability and validity of the Functional Status Questionnaire. Qualityof Life Research. 2000;9:747–753. [Google Scholar]
- Committee on the Future of Emergency Care in the United States Health System. Hospital-based Emergency Care: At the Breaking Point. The National Academies Press; Washington DC: 2007. [Google Scholar]
- Davis RG, Ressler KJ, Schwartz AC, Stephens KJ, Bradley RG. Treatment barriers for low-income, urban African Americans with undiagnosed posttraumtic stress disorder. Journal of Traumatic Stress. 2008;21:218–222. doi: 10.1002/jts.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jonge P, Kempen GI, Sanderman R, Ranchor AV, van Jaarsveld CHM, van Sondern E, Scaf-Klomp W, Weening A, Slaets JPJ, Ormel J. Depressive symptoms in elderly patients after a somatic illness event. Psychosomatics. 2006;41:33–42. doi: 10.1176/appi.psy.47.1.33. [DOI] [PubMed] [Google Scholar]
- Diggle PJ, Liang KY, Zeger SL. Analysis of Longitudinal Data. Clarendon Press; Oxford: 1994. [Google Scholar]
- Elashoff JD. NQuery Advisor, Version 3.0 User’s Guide. Los Angeles, CA: 1999. [Google Scholar]
- Elklit A. Acute stress disorder in victims of robbery and victims of assault. Journal of Interpersonal Violence. 2002;17:872–887. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for Axis I DSM-IV Disorders--Patient Edition. Biometrics Research Department, New York State Psychiatric Institute; NY: 1994. [Google Scholar]
- Fishbain DA, Cole B, Cutler RB, Lewis J, Rosomoff HL, Rosomoff RS. Is pain fatiguing? A structured evidence-based review. Pain Medicine. 2003;4:51–62. doi: 10.1046/j.1526-4637.2003.03008.x. [DOI] [PubMed] [Google Scholar]
- Flaskerud JH. Ethnicity, culture, and neuropsychiatry. Issues in Mental Health Nursing. 2001;21:5–29. doi: 10.1080/016128400248248. [DOI] [PubMed] [Google Scholar]
- Hepp U, Moergeli H, Buchi S, Wittmann L, Schnyder U. Coping with serious accidental injury: A one-year follow-up study. Psychotherapy and Psychosomatics. 2005;74:379–386. doi: 10.1159/000087786. [DOI] [PubMed] [Google Scholar]
- Holbrook TL, Anderson JP, Sieber WJ, Drowner D, Hoyt DB. Outcome after major trauma: 12-month and 18-month follow-up results from the Trauma Recovery Project. Journal of Trauma. 1999;46:765–773. doi: 10.1097/00005373-199905000-00003. [DOI] [PubMed] [Google Scholar]
- Hollander JE, Sparano DM, Karounos M, Sites FD, Shofer FS. Studies in emergency department data collection: Shared versus split responsibility for patient enrollment. Academic Emergency Medicine. 2004;11:200–23. [PubMed] [Google Scholar]
- Jette AM, Davies AR, Cleary PD, Calteins DR, Rubenstein LV, Fink A, Kosekoff J, Young RT, Brook RH, Delbonco TL. The Functional Status Questionnaire: Reliability and validity when used in primary care. Journal of General Internal Medicine. 1986;1:143–149. doi: 10.1007/BF02602324. [DOI] [PubMed] [Google Scholar]
- Jette AM, Cleary PD. Functional disability assessment. Physical Assessment. 1987;67:1854–1858. doi: 10.1093/ptj/67.12.1854. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kempen GI, Sanderman R, Scaf-Klomp W, Ormel J. The role of depressive symptoms in recovery from injuries to the extremities in older persons: A prospective study. International Journal of Geriatric Psychiatry. 2003;18:14–22. doi: 10.1002/gps.768. [DOI] [PubMed] [Google Scholar]
- Kessing LV. Epidemiology of subtypes of depression. Acta Psychiatrica Scandinavica Supplement. 2007;115:85–89. doi: 10.1111/j.1600-0447.2007.00966.x. [DOI] [PubMed] [Google Scholar]
- Kilgo PD, Meredith JW, Osler TM. Incorporating recent advances to make the TRISS approach universally available. Journal of Trauma. 2006;60:1002–1009. doi: 10.1097/01.ta.0000215827.54546.01. [DOI] [PubMed] [Google Scholar]
- Liang K, Zeeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- MacKenzie EJ, Shapiro S, Smith RT, Siegel JH, Moody M, Pitt A. Factors influencing return to work following hospitalization for traumatic injury. American Journal of Public Health. 1987;77:329–334. doi: 10.2105/ajph.77.3.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason S, Wardrope J, Turpin G, Rowlands A. The psychological burden of injury: An 18 month prospective cohort study. Emergency Medicine Journal. 2002;19:400–404. doi: 10.1136/emj.19.5.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney G, Speed J, Sheppard S. Factors related to recovery after mild traumatic brain injury. Brain Injury. 2005;19:975–987. doi: 10.1080/02699050500110264. [DOI] [PubMed] [Google Scholar]
- Murphy N, Confavreux C, Haas J, Konig N, Roullet E, Sailer M, Swash M, Young C. for the Cost of Multiple Sclerosis Study Group. Quality of life in multiple sclerosis in France, Germany, and the United Kingdom. Journal of Neurology, Neurosurgery, & Psychiatry. 1998;65:460–466. doi: 10.1136/jnnp.65.4.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell ML, Creamer M, Pattison P, Atkin C. Psychiatric morbidity following injury. American Journal of Psychiatry. 2004;161:507–514. doi: 10.1176/appi.ajp.161.3.507. [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Creamer M, Elliott P, Atkin C. Health costs following motor vehicle accidents: The role of posttraumatic stress disorder. Journal of Traumatic Stress. 2005;18:557–561. doi: 10.1002/jts.20064. [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Creamer M, Elliott P, Atkin C, Kossmann T. Determinants of quality of life and role-related disability after injury: Impact of acute psychological responses. Journal of Trauma. 2005;59:1328–1335. doi: 10.1097/01.ta.0000197621.94561.4e. [DOI] [PubMed] [Google Scholar]
- Rapoport MJ, Kiss A, Feinstein A. The impact of major depression on outcome following mild-to-moderate traumatic brain injury in older adults. Journal of Affective Disorders. 2006;92:273–276. doi: 10.1016/j.jad.2005.05.022. [DOI] [PubMed] [Google Scholar]
- Read KM, Kufera JA, Dischinger PC, Kerns TJ, Ho SM, Burgess AR, Burch CA. Life-altering outcomes after lower extremity injury sustained in motor vehicle crashes. Journal of Trauma. 2004;57:815–823. doi: 10.1097/01.ta.0000136289.15303.44. [DOI] [PubMed] [Google Scholar]
- Richmond TS. An Explanatory Model of Variables Influencing Post-Injury Disability. Nursing Research. 1997;46:262–269. doi: 10.1097/00006199-199709000-00004. [DOI] [PubMed] [Google Scholar]
- Richmond TS, Kauder D. Predictors of psychological distress following serious injury. Journal of Traumatic Stress. 2000;13:681–692. doi: 10.1023/A:1007866318207. [DOI] [PubMed] [Google Scholar]
- Rosenthal DA, Berven NL. Effects of client race on clinical judgment. Rehabilitation Counseling Bulletin. 1999;42:243–264. [Google Scholar]
- Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: Practical and theoretical implications. Journal of Social & Personal Relationships. 1987;4:497–510. [Google Scholar]
- Scaf-Klomp W, Sanderman R, Ormel J, Kempen GI. Depression in older people after fall-related injuries: A prospective study. Age and Ageing. 2003;32:88–94. doi: 10.1093/ageing/32.1.88. [DOI] [PubMed] [Google Scholar]
- Shalev AY, Freedman S, Peri T, Brandes D, Sahar T, Orr SP, Pitman RK. Prospective study of posttraumatic stress disorder and depression following trauma. American Journal of Psychiatry. 1998;155:630–637. doi: 10.1176/ajp.155.5.630. [DOI] [PubMed] [Google Scholar]
- Soberg HL, Bautz-Holter E, Roise O, Finset A. Long-term multidimensional functional consequences of severe multiple injuries two years after trauma: A prospective longitudinal cohort study. Journal of Trauma. 2007;62:461–470. doi: 10.1097/01.ta.0000222916.30253.ea. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software. Release 6.0. Stata Corporation; College Station, TX: 1999. [Google Scholar]
- Stein MB, Cox BJ, Afifi TO, Belik S, Sareen J. Does co-morbid depressive illness magnify the impact of chronic physical illness? A population-based perspective. Psychological Medicine. 2006;36:587–596. doi: 10.1017/S0033291706007239. [DOI] [PubMed] [Google Scholar]
- Van Gool CH, Kempen G, Penninx B, Deeg DJ, Beekman AT, van Eijk J. Impact of depression on disablement in late middle aged and older persons: Results from the Longitudinal Aging Study Amsterdam. Social Science & Medicine. 2005;60:25–36. doi: 10.1016/j.socscimed.2004.04.021. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Preventing injuries and violence: a guide for ministries of health. WHO; Geneva: 2007. [Google Scholar]
- Zatzick DF, Roy-Byrne P, Russo JE, Rivara FP, Koike A, Jurkovich GJ, Katon W. Collaborative interventions for physically injured trauma survivors: A pilot randomized effectiveness trial. General Hospital Psychiatry. 2001;23:114–123. doi: 10.1016/s0163-8343(01)00140-2. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Coryell W, Pfohl B, Stangl D. The validity of four definitions of endogenous depression: II. Clinical, demographic, familial, and psychosocial correlates. Archives of General Psychiatry. 1986;43:234–244. doi: 10.1001/archpsyc.1986.01800030052005. [DOI] [PubMed] [Google Scholar]