Abstract
Background
Depressive symptoms above screening thresholds have been shown to predict functional decline in older adults. Less is known about the impact of subthreshold depression, and whether more symptoms confer significantly greater risk compared to fewer symptoms.
Methods
Using data from the Duke Established Populations for Epidemiologic Studies of the Elderly (EPESE) collected over ten years, we employed repeated measures mixed models to predict functional change by depression status at the prior (index) in-person interview. Depressive symptoms were measured using a modified version of the Center for Epidemiologic Studies-Depression (CES-D). Subthreshold depression was operationalized as 6–8 symptoms and CES-D defined depression as 9–20 symptoms the previous week. Three domains of functional status were assessed at the subsequent inperson interview: limitations in basic activities of daily living (ADLs), instrumental ADLs (IADLs) and mobility.
Results
Controlling for race, sex, age, education, marital status, cognitive status, health status, self-perceived health, perceived social support, and functional status at the index interview, having 6+ depressive symptoms predicted an increase of 0.12 IADL limitations 3–4 years later (p=0.03). The incremental effect of CES-D defined depression (9+ symptoms compared to 6–8 symptoms) was not significant, suggesting that the effect of more symptomatic depression did not add to that of subthreshold depression. CES-D score modeled as a continuous variable predicted functional change for all domains, but the relationship was not linear, supporting a possible threshold effect.
Conclusions
The relationship between depressive symptoms and functional change is complex, not necessarily linear, and may vary by tasks assessed.
Keywords: Subthreshold depression, functional status
Introduction
Depression is a leading cause of disability worldwide (Murray & Lopez, 1996). Among older adults, the relationship between depression and physical functioning has been documented in both cross-sectional and longitudinal studies, among patients with major depression and among adults with depressive symptoms (Lenze et al., 2001). Penninx et al. followed a cohort of 6247 community-dwelling adults 65 or older originally free from disability for six years, and found those who were depressed at baseline had an increased risk of incident self-reported disability in both activities of daily living (ADLs) and mobility, controlling for baseline chronic conditions and sociodemographic factors (Penninx et al., 1999). Depression was defined as a score of 20 or more on the Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, 1977) to examine outcomes associated with more severe depression. Depressive symptoms also predicted physical decline measured through objective tests of physical performance (Penninx et al., 1998). In a sample of high-functioning elders free of any disability, high levels of depressive symptoms predicted an increased risk of onset of disability in basic ADLs over a 2.5-year interval (Bruce et al., 1994). In this study, depressive symptoms were measured on a continuous scale, and an increased risk was associated with increased symptoms. Depression has also been shown to accelerate the disablement process in older adults (van Gool et al., 2005). The Italian Longitudinal Study on Aging recently reported baseline depressive symptoms were associated with higher rates of reported disability in men and women and performance based disability in men over 3.5 years (Carbonare et al., 2009). In a systematic review of variables predicting functional decline in community-dwelling older adults, depression was one of the key risk factors identified (Stuck et al., 1999).
Other studies, however, have found not found an association between depression and function. In a prospective study of low-functioning older adults, depressive symptoms did not predict change in self-reported basic ADL limitations over two years (Kempen et al., 1999a). In another study, functionally independent older adults with symptoms more similar to major depression did not experience functional decline in basic ADLs over a multi-year follow-up (Kivela & Pahkala, 2001). Depressed mood was not associated with functional decline or improvement in a sample of adults 75 or older when the outcome was a global measure that included basic ADLs, instrumental ADLs (IADLs), and mobility items (Hebert et al., 1999). Others have found a cross-sectional but not longitudinal relationship. For example, Everson-Rose et al. found a cross-sectional relationship between depressive symptoms and physical performance, but depressive symptoms at baseline were not associated with greater functional decline over time. These investigators modeled four levels of depressive symptoms and, while finding a graded relationship with physical performance, did not observe a threshold effect for depressive symptoms in relation to change in physical performance (Everson-Rose et al., 2005). In a longitudinal study of the effect of depressive symptoms on the recovery of IADL function after a fall-related injury, depressive symptoms at baseline were not predictive of recovery/disability (Kempen et al., 2003). Some researchers have suggested depressive symptoms can predict functional decline, but most likely through changes in physical health (Geerlings et al., 2001; Ormel et al., 2002). For example, in a study from the Netherlands, depression at the index measurement was associated with functional limitations at the next measurement only in the presence of chronic physical disease (Geerlings et al., 2001). In another study using structural equation models, the investigators found a one-year lagged effect of depressive symptoms on disability, but a stronger effect of disability on depressive symptoms (Ormel et al., 2002).
In a discussion of this complex relationship between depression and disability, Bruce identified some challenges raised by differing definitions of both constructs (Bruce, 2001). Expanding the definition of depression has been informative. Gallo et al. reported that older adults who reported depressive symptoms but no sadness or dysphoria were at increased risk for impairments in ADLs and IADLs after a 13-year interval compared to those without symptoms (Gallo et al., 1997). Cronin-Stubbs et al. reported the likelihood of becoming disabled over six years increased with each additional symptom of depression at baseline, and this association was observed for basic ADL tasks, mobility, upper and lower body strength and basic motor functions (Cronin-Stubbs et al., 2000). These findings are consistent with others suggesting a dose-response relationship. Using a sample of primary care patients, for example, Lyness et al. reported functional outcomes associated with subsyndromal or minor depression were not as poor as for those among patients with major depression but poorer than observed for those who were nondepressed (Lyness et al., 2006).
While the term 'depression' is primarily reserved for a clinical diagnosis of depression, there has been much focus over the past decade on predictors, correlates and outcomes associated with depressive symptoms not meeting criteria for major depression or dysthymia. In previous work, we examined the cross-sectional relationship between subthreshold depression and variables known to be associated with more symptomatic depression in older adults, and reported that subthreshold depression was significantly associated with impairment in physical functioning. We defined subthreshold depression as clinically significant depressive symptoms below the threshold used in depression screening (Hybels et al., 2001). This syndrome has been variously called subthreshold, subsyndromal or minor depression (Pincus et al., 1999), and has been defined in a number of ways. Although not categorized by the current nomenclature, these depressive symptoms are thought to be of clinical relevance to older adults (Judd & Akiskal, 2002), and have also been shown to be related to functional status in primary care patients (Lyness et al., 1999).
Studies examining functional outcomes related to depressive symptoms in community studies have tended to focus on depressive symptoms as a continuous variable (Bruce et al., 1994; Cronin-Stubbs et al., 2000), at an identified threshold indicating more severe depression (Penninx et al., 1999), or at levels comparable to major depression (Kivela & Pahkala, 2001). Findings differ whether the outcome is incident disability or change in one or more of the domains among those with or without functional impairment. Although in cross-sectional studies both major and minor depression are associated with disability (Beekman et al., 1997), less is known about longitudinal outcomes associated with subthreshold depression in community samples of older adults, and particularly whether outcomes differ by the type of functional limitation.
The purpose of our research was to examine the impact of subthreshold depression on change in functional status in a sample of community-dwelling older adults followed for ten years. Using a cutpoint for subthreshold depression established in our prior work, we hypothesized subthreshold depression would be a predictor of decline in three domains of function: basic ADLs, IADLs and mobility. We employed an innovative approach to examine the impact of subthreshold depression. Specifically, our aim was to determine the importance of subthreshold depression by exploring the incremental effect of more symptomatic depression over the effects of lower levels of depressive symptomatology predicting functional change.
Given the complexity of the relationship between depressive symptoms and functional status, we had as a second objective to model the functional form of the relationship between depressive symptoms and functional change across the three outcomes. Specifically, as summarized above, the literature suggests as depressive symptoms increase, the likelihood of functional limitations increases in a linear manner. Our previous work in the area of subthreshold depression, using cutpoints that were arbitrarily defined, suggested there may be a threshold effect lower than the traditional screening point on the CES-D which may indicate a level of depressive symptomatology which shared similar correlates with more symptomatic depression and differed from little or no depressive symptomatology. Our aim therefore was to assess the linearity of the relationship between the number of depressive symptoms and functional change, and whether there was support for our defined threshold and/or if there were naturally occurring thresholds in this longitudinal association that may be more suitable for modeling this relationship.
In cross-sectional studies, the prevalence of depressive symptoms have been shown to be associated with a number of demographic, health and social variables (Beekman et al., 1995; Blazer et al., 1991; Hybels et al., 2001), and some of these variables have also been shown to predict functional decline in older adults. For example, functional decline has been shown to be associated with older age and fewer years of education (Ho et al., 1997; Ishizaki et al., 2000; Kempen et al., 2006). Some studies have shown functional decline to be more prevalent in women and blacks (Dunlop et al., 2002; Dunlop et al., 2005) (Mendes de Leon et al., 1997). Being married has been shown in a sample of nursing home residents to predict worsening ADL dependencies (McConnell et al., 2002). Chronic medical conditions and poorer self-rated health have been shown to put older adults at risk for poor functional outcomes (Stuck et al., 1999; Wang et al., 2002). In a study from the Netherlands, poor self-perceived health was not a risk factor for functional decline, but good perceived health predicted healthy functional trajectories (Kempen et al., 2006). Low cognitive function has also been shown to predict decline in physical functioning in older adults (Dodge et al., 2006; Stuck et al., 1999; Wang et al., 2002), and this association has been observed among older adults both with and without dependence at baseline (Mehta et al., 2002). Having poor social roles and fewer social contacts has also been shown to be associated with functional decline (Ishizaki et al., 2000; Stuck et al., 1999). To address our objective examining the direct effects of depressive symptoms on change in functional status, we therefore hypothesized we would find an association controlling for these potential confounders.
Methods
Sample Design and Data Collection
The data derive from the Duke Established Populations for Epidemiologic Studies of the Elderly (EPESE), a multi-site National Institute on Aging (NIA) sponsored longitudinal study of community-dwelling older adults. The study design has been described in detail elsewhere (Blazer et al., 1991; Cornoni-Huntley et al., 1990). The Duke site utilized a multi-staged area probability sample representative of a five-county area in central North Carolina. One county was predominantly urban, and four were rural. Blacks were oversampled, and comprised 54% of the baseline sample. A total of 4,162 adults age 65+ were selected in 1986–87, an interview response rate of 80%, and followed for up to ten years. In-person surveys were conducted at three, six, and ten years post baseline. Proxy interviews were conducted for those who were physically or cognitively unable to participate. Approximately 50% of the sample was deceased at ten years, but attrition for reasons other than death was minimal. Participants provided written consent each round of data collection, and the study protocol was reviewed and approved annually by the Duke Institutional Review Board (IRB).
Measures
Depressive symptomatology
was measured using the CES-D (Radloff, 1977). The original 20-item scale ascertains the degree to which a symptom was present in the previous week. Each symptom is scored from 0–3, for a total scale range of 0–60, with a score of 16+ considered the threshold for clinically significant depression (Radloff & Locke, 2000). For the Duke EPESE, we used a modified version that coded whether each symptom was present the previous week (Y/N), with a possible range of scores 0–20. Our modified scale showed good internal consistency in our baseline data (Cronbach’s coefficient alpha=0.82). To model the functional form of depressive symptoms as they impact functional change, we used the total score from the modified CES-D as a continuous variable. To assess subthreshold depression we created three levels of depressive symptoms (0–5, 6–8, and 9+ symptoms). We previously reported a score of 9+ on our modified scale corresponded to a score of 16+ on the original scale (Blazer et al., 1991), and in earlier work defined subthreshold depression as a score of 6–8 on the modified scale (Hybels et al., 2001). For the analyses presented in this current paper, we conducted a sensitivity analysis using data from the Yale EPESE (Cornoni-Huntley et al., 1986), where the CES-D was used in its traditional format, to identify a corresponding cutpoint on the full scale that corresponded to our coding of subthreshold depression. Within the Yale data, we recoded the Yale responses to Yes/No, and confirmed a code of 9 on the modified scale was comparable to a score of 16 on the traditional scale (sensitivity=92%, specificity=93%, c-index=0.98). Our cutpoint of 6 best corresponded to a score of 8 on the traditional scale (sensitivity=94%, specificity=92%, c-index=0.98). Our definition of subthreshold depression, therefore, corresponds to a score of 8–15 on the traditional CES-D scale.
Sociodemographic variables
included age as a continuous variable, race, years of education as a continuous variable, marital status (1=not married, 0=married), and sex (1=female, 0=male). We classified sample members as African American (coded 0) or White/Other (coded 1), with less than 1% of our sample classified as Other.
Physical functioning
was measured using three scales. Basic ADL tasks were measured as needing help with five items identified by Katz et al. (Katz et al., 1970): bathing, dressing, eating, getting from the bed to a chair, and toileting (scale range 0–5). IADL tasks were measured using five items from the OARS survey (Duke University Center for the Study of Aging and Human Development, 1978): driving car/travel alone, shopping for groceries/clothes alone, preparing own meals, doing own housework and handling own money (scale range 0–5). Mobility was measured using three of the six items used by Rosow and Breslau (Rosow & Breslau, 1966): doing heavy work, ability to walk up and down stairs, and ability to walk ½ mile (scale range 0–3). Missing items within a scale did not contribute toward the count of limitations. Overall, the mean number of limitations at baseline was somewhat low - 76% of the participants did not have any IADL limitations, 92% did not have any ADL limitations, and 57% did not have any mobility limitations. For the regression models, the number of limitations was used as a continuous variable, with higher values corresponding to more limitations.
Cognitive functioning
was measured using the Short Portable Mental Status Questionnaire (SPMSQ) (Pfeiffer, 1975). For our analyses, we used a continuous variable indicating the number of errors, with a possible range of 0 to 10.
Health status
was measured using a summary measure of chronic disease that recorded the number and impact of conditions present (heart problems, hypertension, diabetes, stroke, and cancer) (Fillenbaum et al., 1998). We used the health index score as a continuous variable with a possible range of 0 (no health conditions) to 189 (multiple conditions with high impact). We also included a measure of self-rated health modeled as an ordinal variable with excellent (coded 1) to poor (coded 4).
Perceived social support
was measured by asking sample members how much they felt they could count on or talk about their deepest problems with family members and friends. The range of responses was 2 to 6, with higher levels indicating stronger perceived support (Hybels et al., 2001).
Data Analysis
We first ran a repeated measures mixed model using depression score at the index wave as a predictor of functional change 3–4 years later. CES-D score was modeled as a continuous variable and each of the three outcomes was modeled separately. Functional status at the index interview for the appropriate measure was entered for each interval (e.g., baseline mobility status was included in the interval predicting three-year mobility status), resulting in residualized change models. Some participants improved in function over the interval, others declined in function, while the majority stayed primarily at the same level of function. We plotted the residuals for the three mixed models, and the residuals appeared to follow a normal distribution. We evaluated three possible error structures to adjust for the correlated measures over time, and based on Bayesian Information Criteria (BIC) fit statistics, an unstructured covariance structure provided the best fit to these data.
Three intervals 3–4 years apart were incorporated into each model: baseline depressive symptoms predicting function at the three year follow-up, three-year status predicting function at the six year follow-up, and six-year status predicting function at the 10 year follow-up. Marital status, cognitive status, chronic health conditions, self-perceived health, and perceived social support were entered as time varying covariates; that is, their status at the index interview was entered for each interval. To contribute data for a particular interval, sample members had to have complete depression data at the index interview and complete function data at the index and subsequent interview. Depression data were not collected from proxy respondents, but proxy information for functional status was accepted.
We modeled the functional form of the relationship between CES-D score and functional change in ADLs, IADLs, and mobility in several ways: 1) We checked for any naturally occurring thresholds or inflection points in the CES-D score. Specifically, using PROC MIXED, we output the residuals from a model which included all the covariates but not the CES-D score for each of the three outcomes. To examine the impact of CES-D score on the error, we applied a smoothing algorithm using PROC LOESS; 2) We checked for the presence and location of steps or thresholds using a mixed model that included the CES-D score as a continuous variable and all possible cutpoints (e.g., score of 1 or less vs. 2 or more, 2 or less vs. 3 or more, etc.) to identify any statistically significant thresholds above and beyond the linear score for each outcome, removing nonsignificant CES-D terms through backward elimination; 3) We assessed the impact of spline effects at the two cutpoints we defined in our previous work (6 and 9); and 4) We assessed the impact of higher order polynomials of the CES-D score on functional change.
To address our key research question, the impact of subthreshold depression on functional change, we used the CES-D thresholds defined as we had done in previous work. We were interested in this analysis in examining the importance of subthreshold depression (a score of 6–8) by measuring the incremental effect of more symptomatic or CES-D defined depression (a score of 9 or more). Specifically, we were interested in comparing functional outcomes in those with either subthreshold or CES-D defined depression compared to those who were nondepressed, and comparing outcomes among those with more symptomatic or CES-D defined depression to those with subthreshold depression. This type of analysis is slightly different to what is often seen, and can be further explained as follows.
In a traditional model, we would look at the effect of both groups by creating two dummy variables:
Dummy 1 - coded 1 if the score was 6–8 and 0 if the score was <6 or 9+
Dummy 2 - coded 1 if the score was 9+ and 0 if the score was <6 or 6–8
By including both dummy variables in the model, the estimated effects for both groups would be compared to those who were nondepressed (score <6 - the lowest group).
In this regression analysis, we are modeling the incremental effect of more symptomatic depression, similar to the effect modeled using ordinal variables. Here, each effect is the incremental effect relative to the next lower group. We created two dummy variables:
Dummy 1 – coded 1 if the score is 6+ and 0 if the score is <6.
Dummy 2 – coded 1 if the score is 9+ and 0 if the score is <9
By including both these dummy variables in the regression model, the group with scores 6+ would be compared to the nondepressed, and the group with scores 9+ would be compared to the next lower group (those with scores 6–8).
There were at total of 4162 participants at baseline and 618 died during the first interval. A total of 3052 had complete depression and function data for the first interval. There were 3337 participants at the second in-person survey three years after baseline, and a total of 663 died during the second interval. A total of 2209 had complete depression and function data for the second interval. There were 2569 participants in the third in-person survey six years after baseline, and a total of 867 died during the third interval. A total of 1408 had complete data for the third interval. Among the participants, 1% or less were missing data for marital status, cognitive status, health status, self-perceived health, or perceived social support. A total of 237 (3.6%) observations were dropped from the analysis because of missing data on one or more of these variables, resulting in an analysis sample of 6432 observations (1–3 per participant) for the mixed models.
All analyses were run using SAS software (SAS Institute, 2004). Significance thresholds were set at p<.05, and all tests were two-tailed. We did not adjust for the unequal probabilities of selection in the sample design, but variables used in the stratification process were included in the regression models (Korn & Graubard, 1991).
Results
Table 1 shows the characteristics of the sample members who participated in the first two in-person interviews. While the mean depression score was quite low, a total of 19.9% of the sample had a number of depressive symptoms - 11.1% of the sample had subthreshold depression (a score of 6–8), while 8.8% had a CES-D score of 9 or greater. These prevalence estimates are slightly different from those reported earlier from the baseline sample alone (Hybels et al., 2001). Limitations in mobility and IADLs were more common than limitations in basic ADL function.
Table 1.
Characteristics of the respondents who participated in the first interval (n=3052)
| Characteristic | Mean (SD) | Number (%) |
|---|---|---|
| CES-D Score 6+ at BL (%) | 607 (19.9%) | |
| CES-D Score 9+ at BL (%) | 267 (8.8%) | |
| Mean CES-D Score at BL (SD) | 3.1 (3.32) | |
| Mean Age at BL (SD) | 72.8 (6.2) | |
| Mean # Yrs Education (SD) | 8.6 (4.1) | |
| Mean # ADL Limitations at BL (SD) | 0.15 (0.61) | |
| Mean # ADL Limitations at P2 (SD) | 0.43 (1.09) | |
| Mean # IADL Limitations at BL (SD) | 0.50 (1.11) | |
| Mean # IADL Limitations at P2 (SD) | 0.88 (1.54) | |
| Mean # Mobility Limitations at BL (SD) | 0.79 (1.07) | |
| Mean # Mobility Limitations at P2 (SD) | 1.03 (1.15) | |
| Black Race (%) | 1654 (54.2%) | |
| Male Sex (%) | 1017 (33.3%) | |
| Not Married at BL (%) | 1842 (60.1%) | |
| Mean Number Errors SPMSQ at BL (SD) | 1.6 (1.5) | |
| Mean Health Conditions Score at BL (SD) | 36.0 (29.9) | |
| Mean Self-Rated Health at BL (SD) | 2.4 (0.9) | |
| Mean Perceived Social Support at BL (SD) | 5.5 (0.9) |
Prior to running the mixed models, we checked for collinearity among the predictors including depression. The variable with the lowest tolerance in each of the three models was marital status (.74), suggesting there was not extreme correlation among the variables that could impact the results.
The results of our models assessing the functional form of the relationship between depressive symptoms and functional change were inconclusive. In our first assessment, there were no visibly apparent thresholds identified through the smoothing algorithm for any of the three outcomes. In our second assessment examining all possible cutpoints, we found differences across the three outcomes. For the IADL model, significant thresholds remaining in the model were at CES-D scores 1, 4 and 8. For ADL, the only significant threshold was 15, and for mobility, the only significant threshold was a score of 1 or more vs. 0. These results suggest that some score or scores less than our cutpoint of 9 may be a significant threshold for depressive symptoms as they predict change in IADL function. The cutpoints of 1 and 15 for change in mobility and ADL were less meaningful in defining a threshold for subthreshold depression. In our third assessment, the two spline effects at the cutpoints defined in our previous work were not significant for any of the three outcomes. Finally, for each of the three models where we assessed the impact of linear and higher order polynomials of CES-D score on the outcomes, the squared term was significant (the cubic term was not and was subsequently removed). These results of these models are provided in Table 2. We plotted the quadratic terms and found for each of the three outcomes, an increase in CES-D score was associated with an increase in limitations until a score of around 8–10 and then an increase in CES-D score was associated with a decrease in limitations, suggesting a possible threshold effect.
Table 2.
Depressive symptoms as a predictor of functional limitations using a mixed model repeated measures design and CES-D score as a continuous variables
| IADL Limita | ADL Limitations | Mobility Limitations | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Parameter Estimate |
Standard Error |
p-value | Parameter Estimate |
Standard Error |
p-value | Parameter Estimate |
Standard Error |
p-value | |
| Intercept | −4.0887 | 0.2470 | <.0001 | −2.4966 | 0.1805 | <.0001 | −2.2502 | 0.1692 | <.0001 |
| CES-D Score | 0.0373 | 0.0082 | <.0001 | 0.0219 | 0.0062 | 0.0004 | 0.0229 | 0.0056 | <.0001 |
| CES-D Score Squared** | −0.0036 | 0.0011 | 0.0011 | −0.0017 | 0.0008 | 0.0395 | −0.0024 | 0.0007 | 0.0013 |
| Black Race | −0.0936 | 0.0335 | 0.0053 | −0.0614 | 0.0242 | 0.0113 | 0.0060 | 0.0229 | 0.7945 |
| Male Sex | −0.0391 | 0.0378 | 0.3012 | 0.0172 | 0.0274 | 0.5288 | −0.1064 | 0.0260 | <.0001 |
| Age | 0.0545 | 0.0029 | <.0001 | 0.0316 | 0.0021 | <.0001 | 0.0324 | 0.0020 | <.0001 |
| Yrs of Education | 0.0019 | 0.0045 | 0.6726 | 0.0068 | 0.0033 | 0.0394 | −0.0064 | 0.0031 | 0.0377 |
| Not Married | 0.0615 | 0.0371 | 0.0979 | 0.0398 | 0.0270 | 0.1407 | 0.0995 | 0.0254 | <.0001 |
| SPMSQ Errors | 0.1925 | 0.0126 | <.0001 | 0.1062 | 0.0094 | <.0001 | 0.0544 | 0.0084 | <.0001 |
| Chronic Health | 0.0029 | 0.0005 | <.0001 | 0.0007 | 0.0004 | 0.0766 | 0.0024 | 0.0004 | <.0001 |
| Conditions Score | |||||||||
| Self-Rated Health | 0.1182 | 0.0207 | <.0001 | 0.1053 | 0.0155 | <.0001 | 0.1409 | 0.0145 | <.0001 |
| Perceived Social Support | −0.0307 | 0.0182 | .0921 | −0.0236 | 0.0139 | 0.0895 | −0.0279 | 0.0124 | 0.0245 |
| Function Score at Index | 0.6364 | 0.0157 | <.0001 | 0.7631 | 0.0190 | <.0001 | 0.5601 | 0.0120 | <.0001 |
| Interview* | |||||||||
| Year | 0.1024 | 0.0226 | <.0001 | 0.0598 | 0.0190 | .0017 | 0.0852 | 0.0148 | <.0001 |
For model predicting IADL limitations, we controlled for IADL score at index interview, etc.
Quadratic term is difference between CES-D score and the mean squared.
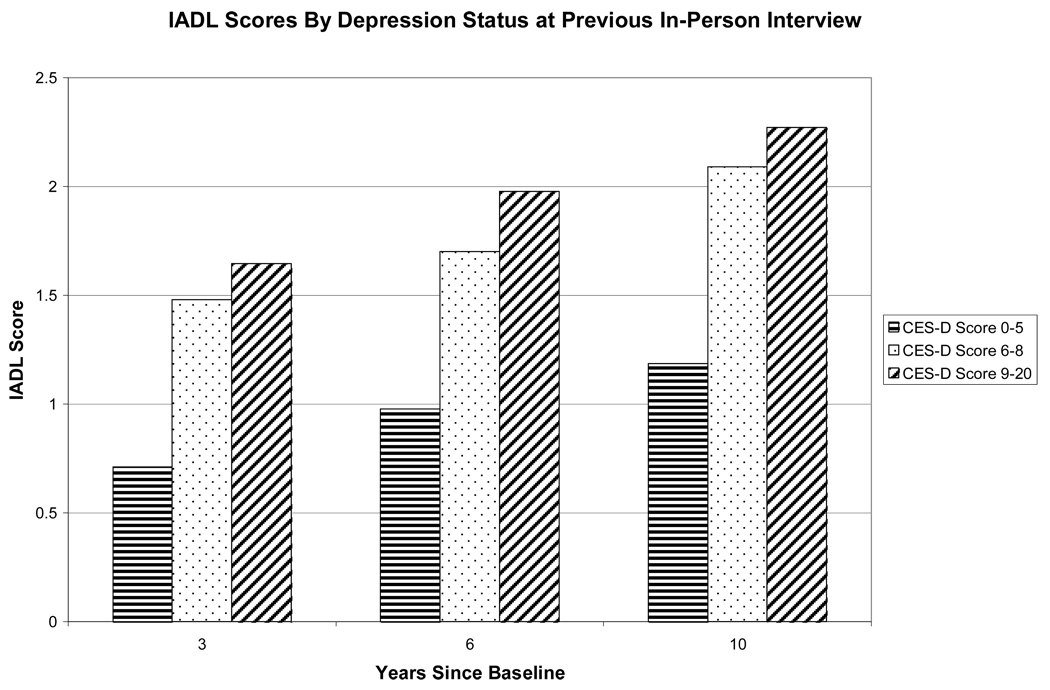
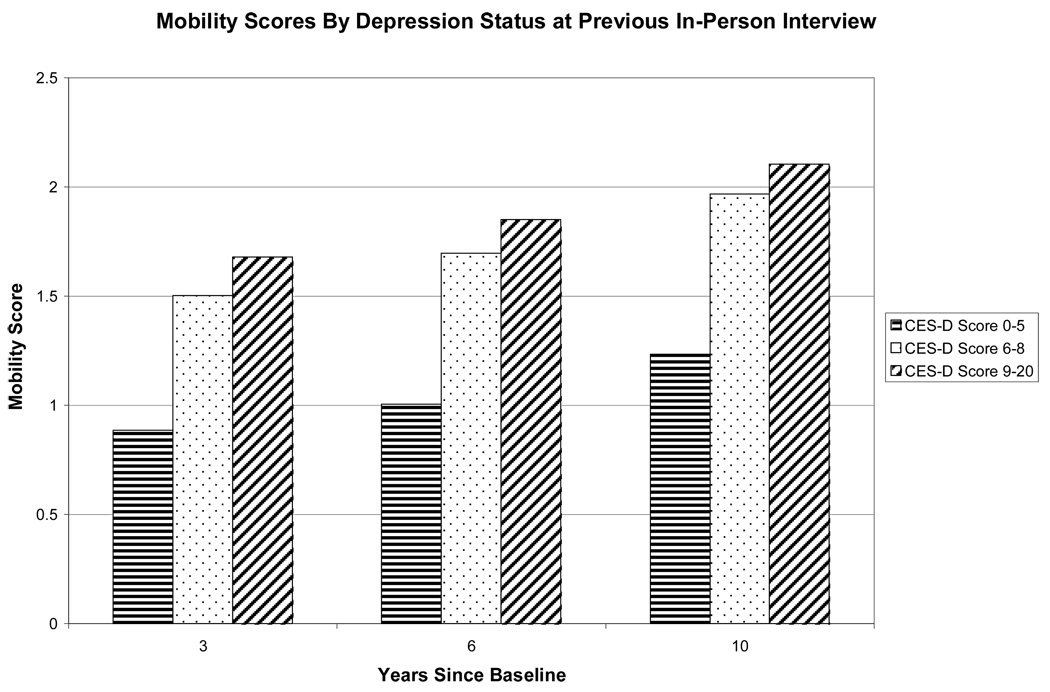
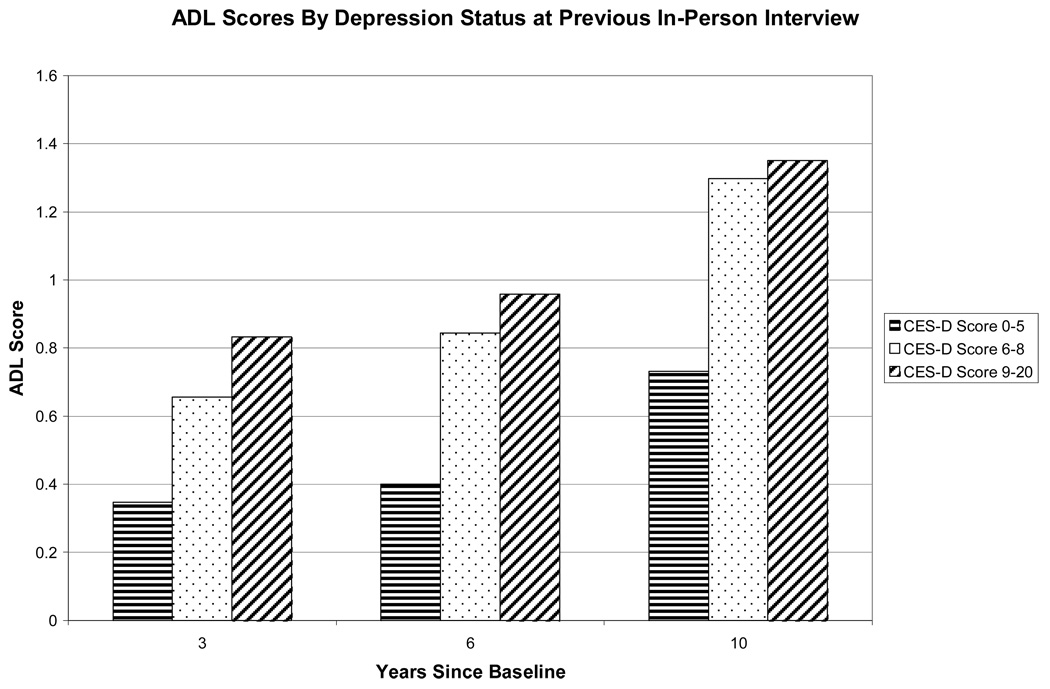
In the absence of consistently defined thresholds, we turned to our main objective of examining the impact of subthreshold depression on functional change using the cutpoints defined in our earlier research. In Figure 1, we show the uncontrolled mean scores for IADL, ADL and mobility limitations by depression status (scores <6, scores 6–8, and scores 9+) at the previous in-person interview. It is important to note those who were nondepressed at baseline may or may not be part of the group that was nondepressed at three years predicting six-year outcome. While there appears to be an expected overall increase in limitations over time, the figures suggest there is no differential effect of depressive symptoms over time. The effect of 6–8 symptoms appears to be similar to the effect of 9 or more symptoms.
Figure 1.
IADL Score By Depression Status at Previous In-Person Interview
In Table 3, we present the results of the three mixed models measuring the effect of subthreshold depression and the incremental effect of CES-D defined depression. We show both uncontrolled models (with only the two depression variables, functional status at the index wave, and time as predictors) and models examining the effect of depressive symptoms controlling for other identified potential confounders as well. In uncontrolled analyses, a score of 6+ on the modified CES-D was a significant predictor of IADL, ADL, and mobility limitations 3–4 years later, while the incremental effect of CES-D defined depression was not significant. The parameter estimates changed when potential confounders were included in the models. In controlled analyses, having six or more depressive symptoms predicted an increase of 0.12 IADL limitations at the subsequent interview (p=0.0298). A score of 6 or greater was not a significant predictor of change in mobility or ADL function. The incremental effect of more symptomatic depression (a score of 9 or greater) compared to a score of 6–8 symptoms was not significant for any of the three outcomes when potential confounders were controlled.
Table 3.
Depressive symptoms as a predictor of functional limitations using a mixed model repeated measures design and three levels of depressive symptoms as predictors
| IADL Limitations | ADL Limitations | Mobility Limitations | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Parameter Estimate |
Standard Error |
p-value | Parameter Estimate |
Standard Error |
p-value | Parameter Estimate |
Standard Error |
p-value | |
| Uncontrolled analyses** | |||||||||
| Intercept | 0.2194 | 0.0418 | <.0001 | 0.1315 | 0.0342 | 0.0001 | 0.2635 | 0.0292 | <.0001 |
| CES-D Score 6+ | 0.3048 | 0.0590 | <.0001 | 0.2297 | 0.0441 | <.0001 | 0.2007 | 0.0398 | <.0001 |
| CES-D Score 9+ | 0.0641 | 0.0806 | 0.4264 | 0.0252 | 0.0610 | 0.6793 | 0.0043 | 0.0540 | 0.9368 |
| Function Score at Index | 0.8254 | 0.0153 | <.0001 | 0.8831 | 0.0191 | <.0001 | 0.7295 | 0.0108 | <.0001 |
| Interview* | |||||||||
| Year | 0.1827 | 0.0226 | <.0001 | 0.0858 | 0.0191 | <.0001 | 0.1297 | 0.0147 | <.0001 |
| Controlled analyses | |||||||||
| Intercept | −4.0570 | 0.2464 | <.0001 | −2.4690 | 0.1801 | <.0001 | −2.2223 | 0.1687 | <.0001 |
| CES-D Score 6+ | 0.1234 | 0.0568 | 0.0298 | 0.0722 | 0.0437 | 0.0989 | 0.0672 | 0.0387 | 0.0826 |
| CES-D Score 9+ | 0.0074 | 0.0761 | 0.9226 | −0.0134 | 0.0589 | 0.8201 | −0.0186 | 0.0518 | 0.7190 |
| Black Race | −0.0885 | 0.0334 | 0.0082 | −0.0599 | 0.0241 | 0.0132 | 0.0086 | 0.0228 | 0.7080 |
| Male Sex | −0.0503 | 0.0376 | 0.1814 | 0.0093 | 0.0273 | 0.7335 | −0.1127 | 0.0259 | <.0001 |
| Age | 0.0548 | 0.0029 | <.0001 | 0.0318 | 0.0021 | <.0001 | 0.0325 | 0.0020 | <.0001 |
| Yrs of Education | 0.0010 | 0.0045 | 0.8274 | 0.0062 | 0.0033 | 0.0604 | −0.0070 | 0.0031 | 0.0228 |
| Not Married | 0.0647 | 0.0371 | 0.0813 | 0.0428 | 0.0270 | 0.1130 | 0.1014 | 0.0254 | <.0001 |
| SPMSQ Errors | 0.1926 | 0.0126 | <.0001 | 0.1071 | 0.0094 | <.0001 | 0.0546 | 0.0084 | <.0001 |
| Chronic Health | 0.0029 | 0.0005 | <.0001 | 0.0007 | 0.0004 | 0.0637 | 0.0024 | 0.0004 | <.0001 |
| Conditions Score | |||||||||
| Self-Rated Health | 0.1307 | 0.0203 | <.0001 | 0.1161 | 0.0152 | <.0001 | 0.1485 | 0.0143 | <.0001 |
| Perceived Social Support | −0.0349 | 0.0181 | .0541 | −0.0280 | 0.0138 | 0.0426 | −0.0311 | 0.0123 | 0.0116 |
| Function Score at Index | 0.6399 | 0.0157 | <.0001 | 0.7666 | 0.0190 | <.0001 | 0.5658 | 0.0119 | <.0001 |
| Interview* | |||||||||
| Year | 0.0933 | 0.0226 | <.0001 | 0.0546 | 0.0189 | .0039 | 0.0798 | 0.0147 | <.0001 |
For model predicting IADL limitations, we controlled for IADL score at index interview, etc.
The uncontrolled model includes the two variables measuring depression and time as predictors in the same model. Including the 9+ variable in the model as well as the 6+ allows us to measure the incremental effect of CES-D defined depression compared to the effect of subthreshold depression.
For each of the three models, we also included two interaction terms, each of the two depression terms *year, to see if the effect was consistent over time. The interaction terms were not significant in any of the three models, and were subsequently removed.
Discussion
We present new findings in this work. First, we conclude the effect of depression on decline in IADL abilities occurs at low levels of depressive symptomatology, and that more symptoms may not confer significantly greater risk of decline. Second, we conclude the relationship between depressive symptoms and functional change is complex, may differ by domain of function assessed, and may not necessarily be linear. That is, as the number of depressive symptoms increases, the degree of functional decline may not correspondingly increase.
Using the cutpoints we identified in previous research, older adults with six or more depressive symptoms had an increased risk of IADL limitations 3–4 years later, controlling for functional status at the index wave and the effects of other known predictors of change in functional status. Our key finding was that the incremental effect of more symptomatic depression was not significant in this model, suggesting the effect of more symptomatic depression did not add to that of subthreshold depression. Our findings were consistent with those of other investigators who reported depressive symptoms not meeting criteria for major depression predicted functional decline in older adults (Gallo et al., 1997; Penninx et al., 1999), and support those of Cronin-Stubbs et al. that mild depressive symptoms can increase the likelihood of becoming disabled (Cronin-Stubbs et al., 2000).
To the best of our knowledge, the incremental effect of more symptomatic depression compared to fewer symptoms has not been previously examined in community populations. We were able to show in these results that the effect of depressive symptoms predicting decline in IADL can be seen at symptom levels far below those captured by traditional threshold scores on the CES-D. These findings are intriguing, and add to a growing body of evidence supporting the importance of subthreshold depression in older adults.
There has been a considerable amount of research looking at depressive symptoms on a continuous scale or above a designated screening threshold predicting functional decline, but we were interested in looking at the risk of functional decline below a particular threshold. Cutpoints can be informative to both clinicians and researchers. These cutpoints are often chosen theoretically (e.g., systolic blood pressure >160) and then tested empirically to see if they have clinical meaning. Our intent was to choose a cutpoint below the usual screening threshold and explore outcomes associated with this level of symptomatology to see if this particular threshold had a meaningful clinical outcome. Specific guidelines are also often important for clinical interventions and prevention. Clinicians should be observant for functional decline even when depressive symptoms don't meet the severity of DSM-IV criteria or even screening thresholds.
We believe this is the first study to explore the functional form of depressive symptoms as they relate to functional change in older adults. We modeled the functional form of the modified version of the CES-D, and were unable to identify naturally occurring inflection points in the curves or provide quantitative support for the cutpoints we had previously used. We conducted several analyses to identify thresholds in the continuous scale, but the findings were inconsistent and varied somewhat across the three outcomes. The cutpoint of 6+ symptoms therefore was selected more on theoretical than statistical grounds. Our finding that depressive symptoms and functional change were not linearly related is particularly interesting, and suggests a greater number of symptoms is not necessarily associated with a significantly greater risk of decline. Both the quadratic model and the cutpoint model supported a nonlinear relationship.
Our findings also suggest the relationship between depressive symptoms and functional status may differ by domains of function assessed. The analyses exploring optimal or naturally occurring thresholds indicated a possible step for changes in IADL function that would be consistent with our categorization of subthreshold depression. Similarly, using our previously established thresholds, we found a significant effect of subthreshold depression for IADL change but not change in mobility or basic ADLs. IADL tasks may have a stronger cognitive component than basic ADLs or mobility, and this component may play a role in this association. Research by other investigators has shown through structural equation modeling in fact that depressive symptoms may affect IADL abilities through cognition (Gallo et al., 2003). We also found some similarities. In our repeated measures mixed models, we report a similar nonlinear effect for each of the three outcomes, with an increased risk of decline with fewer symptoms but then a similar or decreased risk with more symptoms.
Subthreshold depression may be a prodrome to a more serious form of depression or be indicative of a chronic condition which could eventually lead to functional change. Subthreshold depression may reflect an overall awareness that one’s health is not optimal. Our findings suggest that more symptomatic levels of depressive symptoms may indeed confer greater risk for future impairment, but that the incremental difference above the risk conferred by subthreshold depression is not significant. These findings build on our earlier work that levels below the threshold typically used to screen for depression can be informative.
Our study has several limitations. Previous research has suggested the validity of the CES-D in older adults is not affected by physical disabilities (Berkman et al., 1986), and others have reported depressive symptoms were not associated with poorer self-report of functional status (Sinclair et al., 2001), but we cannot rule out this potential bias. That is, because depressive symptoms and functional status were simultaneously assessed at each of the index waves, there is a potential validity issue. Persons with depressive symptoms may be more likely to misrepresent self-reported functional status. We have relied on self-reported data to measure both depressive symptoms and functional status as is frequently done in community based epidemiologic surveys. Depression data was not available for those who participated by proxy, so a number of older adults in poorer health or with cognitive impairment may have been excluded from the analysis. If participants with cognitive impairment also had more depressive symptoms, we may have underestimated the true effect of depressive symptoms on functional change. If depressive symptoms predict mortality, then persons with depressive symptoms may have been less likely to participate in future waves. The Duke EPESE also did not capture data on psychiatric comorbidity which could contribute to the association between depressive symptoms and functional change. Similarly, we did not control for psychological attributes such as mastery which have been shown to be protective in older adults (Kempen et al., 1999b), and may interact with depressive symptoms.
We used a modified version of the CES-D, but conducted a sensitivity analysis comparing this version to the traditional version used in the Yale EPESE. Other investigators have successfully used modified versions of this instrument to address this association (Penninx et al., 1998). For each interval, we assessed physical function in three areas at only one time point 3–4 years after the index interview, but research has shown transitions from independence to disability as well as disability to independent mobility are dynamic (Gill et al., 2006). We used a measure of depressive symptoms at the index wave to predict change in functional status. By only inquiring about depressive symptoms in the previous week using intervals three to four years apart, we were unable to capture changes in depressive symptoms that occurred at other times. We also looked at functional change three to four years after the measure of depressive symptoms, but we are aware depressive symptoms may have their effect on functional status within a shorter interval.
To explore depressive symptoms as a predictor of functional status 3–4 years later, we used a residualized change model that looked at change in functional status from the index interview. Our sample at baseline and the other index waves included persons who already had one or more limitations, so we cannot separate incident and prevalent disability, only change in functional status. While these persons with limitations could improve in function, there were a number of participants who already had the maximum number of limitations. Across the three index waves, the proportion of participants who were not at risk for decline was 2.4% for IADL limitations, <1% for basic ADL limitations, and 12.8% for limitations in mobility. We cannot rule out the possibility of a Type I error in that we looked at three outcomes. In future work, we plan to explore the longitudinal relationship between these measures of depression and the three functional outcomes in a multivariate model that would allow us to control for Type I error and adjust for the correlations among the three outcomes in one model.
It is not known if interventions could reduce future functional disability. Meaningful reductions in depressive symptoms that may help reduce future disability are difficult to measure when so few symptoms are present at the index wave. Other investigators may wish to address the effectiveness of interventions in community-dwelling older adults.
Strengths of the study include a large representative sample of community-dwelling older adults followed for ten years. We had a low attrition rate for reasons other than death. By including functional status and associates covariates at the time of the index interview to predict functional status 3–4 years later, we were able to establish change in function from one point in time to 3–4 years later and therefore temporal ordering. This design is advantageous over studies examining changes in depressive symptoms as predictors of functional change during the same time period (Lenze et al., 2005; Penninx et al., 2000), which address the challenges of this dynamic relationship but make it somewhat difficult to establish an antecedent-consequent relationship. Also, by exploring three different measures of physical function separately, we allowed depressive symptoms to have differential relationships with each component of function, since previous research has suggested use of an aggregate measure may be misleading (Landerman & Fillenbaum, 1997).
In summary, these findings address an important problem regarding geriatric mental health and functional outcomes, as the prevalence of subthreshold depression in both community and clinical samples is high (Blazer, 2003).
Figure 2.
Mobility Score By Depression Status at Previous In-Person Interview
Figure 3.
ADL Score By Depression Status at Previous In-Person Interview
Acknowledgements
The preparation of this manuscript was supported by NIMH grant K01 MH066380 and the Claude D. Pepper Older Americans Independence Center P30 AG028716. The data were gathered under NIA contract number N01 AG12102 and grant R01 AG12765. The content of this publication does not necessarily reflect the views or policies of the US Department of Health and Human Services. Preliminary results were presented in a poster session at the 132nd Annual Meeting of the American Public Health Association in Washington, DC in November 2004. The authors report no competing interests. Finally, we acknowledge the helpful comments provided by the three anonymous reviewers.
Footnotes
Publisher's Disclaimer: This paper has been accepted for publication in Psychological Medicine and will appear in a revised form, subsequent to editorial input by Cambridge University Press. The copyright holder is Cambridge University Press. Please refer to http://journals.cambridge.org/.
Contributor Information
Celia F. Hybels, Department of Psychiatry and Behavioral Sciences, Center for the Study of Aging and Human Development, Box 3003, Duke University Medical Center, Phone: (919) 660-7546, FAX: (919) 668-0453, E-mail: cfh@geri.duke.edu.
Carl F. Pieper, Department of Biostatistics and Bioinformatics, Center for the Study of Aging and Human Development, Duke University Medical Center.
Dan G. Blazer, Department of Psychiatry and Behavioral Sciences, Center for the Study of Aging and Human Development, Duke University Medical Center.
References
- Beekman ATF, Deeg DJH, Braam AW, Smit JH, van Tilberg W. Consequences of major and minor depression in later life:A study of disability, well-being, and service utilization. Psychological Medicine. 1997;27:1397–1409. doi: 10.1017/s0033291797005734. [DOI] [PubMed] [Google Scholar]
- Beekman ATF, Deeg DJH, van Tilberg T, Smit JH, Hooijer C, van Tilberg W. Major and minor depression in later life: a study of prevalence and risk factors. Journal of Affective Disorders. 1995;36:65–75. doi: 10.1016/0165-0327(95)00061-5. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Berkman CS, Kasl S, Freeman DH, Leo L, Ostfeld AM, Cornoni-Huntley J, Brody JA. Depressive symptoms in relation to physical health and functioning in the elderly. American Journal of Epidemiology. 1986;124:372–288. doi: 10.1093/oxfordjournals.aje.a114408. [DOI] [PubMed] [Google Scholar]
- Blazer D, Burchett B, Service C, George LK. The association of age and depression among the elderly: An epidemiologic exploration. Journal of Gerontology A: Biological Sciences and Medical Sciences. 1991;46(6):M210–M215. doi: 10.1093/geronj/46.6.m210. [DOI] [PubMed] [Google Scholar]
- Blazer DG. Depression in late life: Review and commentary. Journal of Gerontology A: Biological Sciences and Medical Sciences. 2003;58A:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- Bruce ML. Depression and disability in late life: Directions for future research. American Journal of Geriatric Psychiatry. 2001;9(2):102–112. [PubMed] [Google Scholar]
- Bruce ML, Seeman TE, Merrill SS, Blazer DG. The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. American Journal of Public Health. 1994;84:1796–1799. doi: 10.2105/ajph.84.11.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonare LD, Maggi S, Noale M, Giannini S, Rozzini R, Cascio VL, Crepaldi G for the ILSA Working Group. Physical disability and depressive symptomatology in an elderly population: A complex relationship - The Italian Longitudinal Study on Aging (ILSA) American Journal of Geriatric Psychiatry. 2009;17:144–154. doi: 10.1097/jgp.0b013e31818af817. [DOI] [PubMed] [Google Scholar]
- Cornoni-Huntley J, Blazer DG, Lafferty ME, Everett DF, Brock DB, Farmer ME. Established Populations for Epidemiologic Studies of the Elderly: Resource Data Book. Volume II. Washington, D.C.: National Institutes of Health; 1990. pp. 90–495. NIH Publication No. [Google Scholar]
- Cornoni-Huntley J, Brock D, Ostfeld A, Taylor JO, Wallace RB. Established Populations for Epidemiologic Studies of the Elderly: Resource Data Book. Bethesda, MD: National Institutes of Health; 1986. pp. 86–2443. NIH Publication No. [Google Scholar]
- Cronin-Stubbs D, Mendes de Leon CF, Beckett LA, Field TS, Glynn RJ, Evans DA. Six-year effect of depressive symptoms on the course of physical disability in community-living older adults. Archives of Internal Medicine. 2000;160:3074–3080. doi: 10.1001/archinte.160.20.3074. [DOI] [PubMed] [Google Scholar]
- Dodge HH, Du Y, Saxton JA, Ganguli M. Cognitive domains and trajectories of functional independence in nondemented elderly persons. Journal of Gerontology: Medical Sciences. 2006;61A:1330–1337. doi: 10.1093/gerona/61.12.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duke University Center for the Study of Aging and Human Development. Multidimensional Functional Assessment: The OARS Methodology. 2nd Edition. Durham, NC: Duke University; 1978. [Google Scholar]
- Dunlop DD, Manheim LM, Sohn M, Liu X, Chang RW. Incidence of functional limitation in older adults: The impact of gender, race, and chronic conditions. Archives of Physical Medicine and Rehabilitation. 2002;83:964–971. doi: 10.1053/apmr.2002.32817. [DOI] [PubMed] [Google Scholar]
- Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis and Rheumatism. 2005;52:1274–1282. doi: 10.1002/art.20968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everson-Rose SA, Skarupski KA, Bienias JL, Wilson RS, Evans DA, Mendes de Leon CF. Do depressive symptoms predict declines in physical performance in an elderly, biracial population? Psychosomatic Medicine. 2005;67:609–615. doi: 10.1097/01.psy.0000170334.77508.35. [DOI] [PubMed] [Google Scholar]
- Fillenbaum GG, Leiss JK, Pieper CF, Cohen HJ. Developing a summary measure of medical status. Aging Clinical and Experimental Research. 1998;10:395–400. doi: 10.1007/BF03339886. [DOI] [PubMed] [Google Scholar]
- Gallo JJ, Rabins PV, Lyketsos CG, Tien AY, Anthony JC. Depression without sadness: Functional outcomes of nondysphoric depression in later life. Journal of the American Geriatrics Society. 1997;45:570–578. doi: 10.1111/j.1532-5415.1997.tb03089.x. [DOI] [PubMed] [Google Scholar]
- Gallo JJ, Rebok GW, Tennsted S, Wadley VG, Horgas A The Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) Study Investigators. Linking depressive symptoms and functional disability in late life. Aging and Mental Health. 2003;7:469–480. doi: 10.1080/13607860310001594736. [DOI] [PubMed] [Google Scholar]
- Geerlings SW, Beekman ATF, Deeg DJH, Twisk JWR, Van Tilberg W. The longitudinal effect of depression on functional limitations and disability in older adults: an eight-wave prospective community-based study. Psychological Medicine. 2001;31:1361–1371. doi: 10.1017/s0033291701004639. [DOI] [PubMed] [Google Scholar]
- Gill TM, Allore HG, Hardy SE, Guo Z. The dynamic nature of mobility disability in older persons. Journal of the American Geriatrics Society. 2006;54:248–254. doi: 10.1111/j.1532-5415.2005.00586.x. [DOI] [PubMed] [Google Scholar]
- Hebert R, Brayne C, Spiegelhalter D. Factors associated with functional decline and improvement in a very elderly community-dwelling population. American Journal of Epidemiology. 1999;150(5):501–510. doi: 10.1093/oxfordjournals.aje.a010039. [DOI] [PubMed] [Google Scholar]
- Ho SC, Woo J, Yuen YK, Sham A, Chan SG. Predictors of mobility decline: the Hong Kong old-old study. Journal of Gerontology: Medical Sciences. 1997;52A:M356–M362. doi: 10.1093/gerona/52a.6.m356. [DOI] [PubMed] [Google Scholar]
- Hybels CF, Blazer DG, Pieper CF. Toward a threshold for subthreshold depression: An analysis of correlates of depression by severity of symptoms using data from an elderly community sample. The Gerontologist. 2001;41:357–365. doi: 10.1093/geront/41.3.357. [DOI] [PubMed] [Google Scholar]
- Ishizaki T, Watanabe S, Suzuki T, Shibata H, Haga H. Predictors for functional decline among nondisabled older Japanese living in a community during a 3-year follow-up. Journal of the American Geriatrics Society. 2000;48:1424–1429. doi: 10.1111/j.1532-5415.2000.tb02632.x. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS. The clinical and public health relevance of current research on subthreshold depressive symptoms in elderly patients. American Journal of Geriatric Psychiatry. 2002;10:233–238. [PubMed] [Google Scholar]
- Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. The Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- Kempen GIJM, Ranchor AV, van Sonderen E, van Jaarsveld CHM, Sanderman R. Risk and protective factors of different functional trajectories in older persons: Are these the same? Journal of Gerontology Psychological Sciences. 2006;61B:P95–P101. doi: 10.1093/geronb/61.2.p95. [DOI] [PubMed] [Google Scholar]
- Kempen GIJM, Sanderman R, Scaf-Klomp W, Ormel J. The role of depressive symptoms in recovery from injuries to the extremities in older persons-A prospective study. International Journal of Geriatric Psychiatry. 2003;18:14–22. doi: 10.1002/gps.768. [DOI] [PubMed] [Google Scholar]
- Kempen GIJM, Sullivan M, van Sonderen E, Ormel J. Performance based and self-reported physical functioning in low-functioning older persons: Congruence of change and the impact of depressive symptoms. Journal of Gerontology B: Psychological Sciences and Social Sciences. 1999a;54B:P380–P386. doi: 10.1093/geronb/54b.6.p380. [DOI] [PubMed] [Google Scholar]
- Kempen GIJM, van Sonderen E, Ormel J. The impact of psychological attributes on changes in disability among low-functioning older persons. Journal of Gerontology Psychological Sciences. 1999b;54B:P23–P29. doi: 10.1093/geronb/54b.1.p23. [DOI] [PubMed] [Google Scholar]
- Kivela S-L, Pahkala K. Depressive disorder as a predictor of physical disability in old age. Journal of the American Geriatrics Society. 2001;49:290–296. doi: 10.1046/j.1532-5415.2001.4930290.x. [DOI] [PubMed] [Google Scholar]
- Korn E, Graubard B. Epidemiologic studies utilizing surveys: Accounting for sampling design. American Journal of Public Health. 1991;81:1166–1173. doi: 10.2105/ajph.81.9.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landerman LR, Fillenbaum GG. Differential relationships of risk factors to alternative measures of disability. Journal of Aging and Health. 1997;9(2):266–279. doi: 10.1177/089826439700900207. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, Schulz R, Reynolds CF. The association of late-life depression and anxiety with physical disability: A review of the literature and prospectus for future research. American Journal of Geriatric Psychiatry. 2001;9(2):113–135. [PubMed] [Google Scholar]
- Lenze EJ, Schulz R, Martire L, Zdaniuk B, Glass T, Kop WJ, Jackson SA, Reynolds CF. The course of functional decline in older people with persistently elevated depressive symptoms: Longitudinal findings from the Cardiovascular Health Study. Journal of the American Geriatrics Society. 2005;53:569–575. doi: 10.1111/j.1532-5415.2005.53202.x. [DOI] [PubMed] [Google Scholar]
- Lyness JM, Heo M, Datto CJ, Ten Have TR, Katz IR, Drayer R, Reynolds CF, Alexopoulos GS, Bruce ML. Outcomes of minor and subsyndromal depression among elderly patients in primary care settings. Annals of Internal Medicine. 2006;144:496–504. doi: 10.7326/0003-4819-144-7-200604040-00008. [DOI] [PubMed] [Google Scholar]
- Lyness JM, King DA, Cox C, Yoediono Z, Caine EC. The importance of subsyndromal depression in older primary care patients: Prevalence and associated functional disability. Journal of the American Geriatrics Society. 1999;47:647–652. doi: 10.1111/j.1532-5415.1999.tb01584.x. [DOI] [PubMed] [Google Scholar]
- McConnell ES, Pieper CF, Sloane RJ, Branch LG. Effects of cognitive performance on change in physical function in long-stay nursing home residents. Journal of Gerontology: Medical Sciences. 2002;57A:M778–M784. doi: 10.1093/gerona/57.12.m778. [DOI] [PubMed] [Google Scholar]
- Mehta KM, Yaffe K, Covinsky KE. Cognitive impairment, depressive symptoms, and functional decline in older people. Journal of the American Geriatrics Society. 2002;50:1045–1050. doi: 10.1046/j.1532-5415.2002.50259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes de Leon CF, Beckett LA, Fillenbaum GG, Brock DB, Branch LG, Evans DA, Berkman LF. Black-white differences in risk of becoming disabled and recovering from disability in old age: A longitudinal analysis of two EPESE populations. American Journal of Epidemiology. 1997;145(6):488–497. doi: 10.1093/oxfordjournals.aje.a009136. [DOI] [PubMed] [Google Scholar]
- Murray C, Lopez A. Summary: The Global Burden of Disease. Boston, MA: Harvard School of Public Health; 1996. [Google Scholar]
- Ormel J, Rijsdijk FV, Sullivan M, von Sonderen E, Kempen GIJM. Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. Journal of Gerontology B: Psychological Sciences and Social Sciences. 2002;57B:P338–P347. doi: 10.1093/geronb/57.4.p338. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, Deeg DJH, van Eijk JT, Beekman ATF, Guralnik JM. Changes in depression and physical decline in older adults: a longitudinal perspective. Journal of Affective Disorders. 2000;61:1–12. doi: 10.1016/s0165-0327(00)00152-x. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJH, Wallace RB. Depressive symptoms and physical decline in community-dwelling older persons. Journal of the American Medical Association. 1998;279(21):1720–1726. doi: 10.1001/jama.279.21.1720. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, Leveille S, Ferrucci L, van Eijk JTM, Guralnik JM. Exploring the effect of depression on physical disability: Longitudinal evidence from the Established Populations for Epidemiologic Studies of the Elderly. American Journal of Public Health. 1999;89:1346–1352. doi: 10.2105/ajph.89.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Pincus HA, Davis WW, McQueen LE. 'Subthreshold' mental disorders: A review and synthesis of studies on minor depression and other 'brand names'. British Journal of Psychiatry. 1999;174(4):288–296. doi: 10.1192/bjp.174.4.288. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Radloff LS, Locke BZ. Handbook of Psychiatric Measures. Washington DC: American Psychiatric Association; 2000. Center for Epidemiologic Studies Depression Scale (CES-D) [Google Scholar]
- Rosow I, Breslau N. A Guttman health scale for the aged. Journal of Gerontology. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- SAS Institute. Statistical Analysis System, Version 9. Cary NC: SAS Institute; 2004. [Google Scholar]
- Sinclair PA, Lyness JM, King DA, Cox C, Caine ED. Depression and self-reported functional status in older primary care patients. American Journal of Psychiatry. 2001;158:416–419. doi: 10.1176/appi.ajp.158.3.416. [DOI] [PubMed] [Google Scholar]
- Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Social Science and Medicine. 1999;48:445–469. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- van Gool CH, Kempen GIJM, Penninx BWJH, Deeg DJH, Beekman ATF, van Eijk JTM. Impact of depression on disablement in late middle aged and older persons: results from the Longitudinal Aging Study Amsterdam. Social Science and Medicine. 2005;60:25–36. doi: 10.1016/j.socscimed.2004.04.021. [DOI] [PubMed] [Google Scholar]
- Wang L, van Belle G, Kukull WB, Larson EB. Predictors of functional change: A longitudinal study of nondemented people aged 65 and older. Journal of the American Geriatrics Society. 2002;50:1525–1534. doi: 10.1046/j.1532-5415.2002.50408.x. [DOI] [PubMed] [Google Scholar]