Abstract
Objective:
The purpose of this study was to test a conceptual model predicting children's anxiety/depression in middle childhood in a community sample of children with parents who had alcohol problems (n = 112) and those without alcohol problems (n = 101). The conceptual model examined the role of parents' alcohol diagnoses, depression, and antisocial behavior among parents of children ages 12 months to kindergarten age in predicting marital aggression and parental aggravation. Higher levels of marital aggression and parental aggravation were hypothesized to predict children's depression/anxiety within time (18 months to kindergarten age and, prospectively, to age during fourth grade).
Method:
The sample was recruited from New York State birth records when the children were 12 months old. Assessments were conducted at 12, 18, 24, and 36 months; at kindergarten age; and during fourth grade.
Results:
Children with alcoholic fathers had higher depression/anxiety scores according to parental reports but not self-reports. Structural equations modeling was largely supportive of the conceptual model. Fathers' alcoholism was associated with higher child anxiety via greater levels of marital aggression among families with alcohol problems. Results also indicated that there was a significant indirect association between parents' depression symptoms and child anxiety via marital aggression.
Conclusions:
The results highlight the nested nature of risk characteristics in alcoholic families and the important role of marital aggression in predicting children's anxiety/depression. Interventions targeting both parents' alcohol problems and associated marital aggression are likely to provide the dual benefits of improving family interactions and lowering risk of children's internalizing behavior problems.
Theories of the emergence of alcohol problems indicate that alcohol abuse may be a coping mechanism for negative affect such as depression and anxiety (Colder and Chassin, 1997; Swendsen et al., 2000). Children of alcoholics are thought to be at increased risk for such in ternalizing problems (Hussong et al., 2008; Puttler et al., 1998), although this risk is generally lower than that for externalizing problems (Puttler et al., 1998). However, little is known about the processes involved in the association between parents' alcohol problems and children's internalizing symptoms. The purpose of this study was to test a process model of the association between parents' alcoholism and symptoms of child depression and anxiety. We hypothesized parenting and marital aggression as two key intervening variables in this process.
Most studies on children of alcoholics have focused on externalizing behavior problems, with just a few studies examining internalizing behaviors. The results from these studies indicate a greater risk of internalizing symptoms among children of alcoholics across the developmental period from toddlers (Edwards et al., 2001), preschoolers, and early-school-age children (Puttler et al., 1998) to adolescents (Chassin et al., 1999; Hussong et al., 2008). Parental depression and antisocial behavior, often comorbid with alcohol problems, are known to increase risk of children's internalizing behavior problems, either via increased genetic vulnerability or because of greater exposure to a negative caregiving environment.
Studies of alcoholism subtypes have reported the highest rates of internalizing behavior problems among children of depressed alcoholics, followed by a marginally higher risk in children of antisocial alcoholics compared with those without a comorbid diagnosis (Hussong et al., 2008; Puttler et al., 1998). Thus, it is important to consider the role of parental psychopathology when examining internalizing behavior problems among children of alcoholics.
Two proximal processes that may play an etiological role in predicting child depression and anxiety among children of alcoholics are (1) marital aggression and (2) parents' negative affect or aggravation with the child. There is a robust association between alcohol problems and higher marital aggression (see Leonard and Eiden, 2007). Several developmental theories, such as family systems theory (Minuchin, 1985) and emotional security theory (Davies and Cummings, 1994), implicate the marital or intimate partner relationship as a key contextual influence on children's adjustment. Children's exposure to and awareness of the marital relationship in general—and to verbal or physical aggression among parents in particular—may lead to higher anxiety or depression as a result of increased stress. There may also be an indirect effect of marital aggression on children's adjustment through a “spillover” effect on parenting behavior, perhaps because of boundary dissolution between the parental and child subsystems (see Grych, 2002).
Aspects of parenting reflective of negative affect or rejection of the child may be most strongly associated with both higher marital aggression as well as parental risk characteristics such as alcoholism and depression. For instance, alcoholic parents have been reported to be more aggravated with their children, and this association was mediated by parental depression (Eiden and Leonard, 2000). Thus, in addition to marital aggression, parental alcohol problems may be indirectly predictive of child anxiety via parental aggravation.
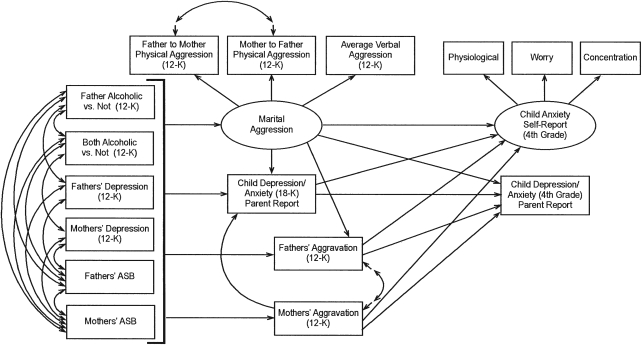
The major purpose of this study was to test a conceptual process model of the association between parents' alcoholism and symptoms of child depression and anxiety using a long-term, prospective design that spanned infancy to fourth grade. The model is displayed in Figure 1 and incorporates the following hypotheses. As indicated in the model, parental alcohol problems, depression, and antisocial behavior were conceptualized as predictors of marital aggression and parental aggravation. We hypothesized that parents' alcohol diagnoses, depression, and antisocial behavior would be associated with higher levels of marital aggression and higher parental aggravation. Higher marital aggression and aggravation over the first 5 years of the child's life were expected to be longitudinally predictive of increases in child anxiety and depression from early childhood to fourth grade. We chose to focus on the fourth-grade assessment rather than earlier ages because the children have had the opportunity to settle into the elementary school routine and are able to reliably report on their own symptoms.
Figure 1.
Conceptual model predicting child anxiety at fourth grade. 12-K = child ages 12 months to age at kindergarten; ASB = antisocial behavior.
Method
Participants
The sample consisted of 213 families with 12-month-old infants at recruitment (105 girls and 108 boys). Families were classified as being in one of two major groups: a group consisting of families with no or few alcohol problems since the child's birth (the no-alcoholic [NA] group; n = 101) and a group consisting of families with alcoholic fathers (the father-alcoholic [FA] group; n = 112). Within the FA group, 82 families had alcoholic fathers with nonalcoholic partners, and 30 families had two alcoholic parents. These classifications were based on parental responses at six time points: child ages of 12, 18, 24, 36, and 48 months and during kindergarten.
The majority of the parents in the study were white (94% of mothers and 87% of fathers), with a smaller percentage of black parents (5% of mothers and 7% of fathers). Although parental education ranged from less than a high school degree to master's degree, about half the mothers (57%) and fathers (55%) had received some education beyond high school or had a college degree. Annual family income ranged from $4,000 to $95,000 (mean [SD] = $41,824 [$19,423]). At the first assessment, mothers were residing with the biological father of the infant in the study. Most of the parents were married to each other (88%). At recruitment, mothers' ages ranged from 19 to 40 years (mean = 30.4 [4.58] years). Fathers' ages ranged from 21 to 58 years (mean = 32.9 [6.06] years). About 61% of the mothers and 91% of the fathers were working outside the home at the initial assessment. About 68% of the families had one to two children, including the target child. Thus, the majority of the families were middle-income, white families with one to two children in the household at recruitment.
Procedure
The names and addresses of these families were obtained from the New York State birth records for Erie County (see Eiden et al., 2007, for procedural details). Families meeting basic eligibility criteria were sent an introductory letter, and those who returned the enclosed form indicating interest in hearing more about the study were screened over the telephone. The phone screens ascertained additional inclusion criteria. Mothers could not have used drugs during pregnancy or in the past year (except for less than two instances of marijuana use), mothers' average drinking was less than one drink a day during pregnancy, and mothers did not drink five or more drinks on a single occasion during pregnancy. During the phone screen, mothers were administered the Family History Research Diagnostic Criteria for alcoholism with regard to their partners' drinking (Andreasen et al., 1986), and fathers were screened with regard to their alco hol use, problems, and treatment. Because we had a large pool of families potentially eligible for the nonalcoholic group, alcoholic and nonalcoholic families were matched on race/ethnicity, maternal education, child gender, parity, and marital status.
Families visited the Institute at six different child ages (12, 18, 24, and 36 months, during kindergarten, and in fourth grade). A parental questionnaire assessment was also conducted at 48 months. Informed written consents were obtained from both parents, and child assents were obtained from kindergarten-age and older children. This article focuses on data from children ages 12 months to fourth grade. The predictors (parental risk characteristics) and mediators (marital aggression and parental aggravation) were aggregated over the 12-month to kindergarten time points to reflect the levels of these variables over the first 5 years of the child's life, predicting anxiety in fourth grade.
Measures
Parental alcohol use.
The University of Michigan Composite International Diagnostic Interview (UM-CIDI; Anthony et al., 1994; Kessler et al., 1994) was used to assess alcohol abuse and dependence at each assessment. Several questions of the instrument were reworded to inquire as to “how many times” a problem had been experienced, as opposed to whether it happened “very often.”
In addition to the screening criteria, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994), criteria for alcohol abuse and dependence diagnoses for current alcohol problems (in past 6 months at the 18- and 24-month assessments and in the past year at other time points) were used to assign families to the FA or NA groups. For abuse criteria, recurrent alcohol problems were described as those occurring at least three to five times in the past year or one to two times in three or more problem areas. Parents who met diagnostic criteria at any time point between 12 months and kindergarten were assigned to the FA group. The UM-CIDI is a widely used diagnostic interview designed to assess substance abuse and dependence with high inter-rater, test-retest reliability and good validity with regard to concordance with clinical diagnoses (see Kessler, 1995).
Parents' depression.
Parents' depression was assessed at each assessment point with the Center for Epidemiological Studies Depression Inventory (CES-D; Radloff, 1977), a scale designed to measure depressive symptoms in community populations. To create an index of maternal and paternal depression from 12 months to kindergarten, the CES-D scores at each age were averaged, and a composite index of depression was created for each parent. The depression scores were moderately stable over time for both parents, with Pearson correlations ranging from .52 to .73 for fathers and from .56 to .68 for mothers. The internal consistencies of the scale ranged from .84 to .89 for fathers and from .87 to .90 for mothers in this sample.
Parents' antisocial behavior.
A modified 28-item version of the Antisocial Behavior Checklist (Ham et al., 1993; Zucker and Noll, 1980) was used in this study at child age of 12 months (see Eiden et al., 2007). The measure was not re-administered because it is a measure of lifetime antisocial behavior. The internal consistency was quite high for both parents (Cronbach's α = .90 for fathers and .82 for mothers). The antisocial behavior scores for both mothers and fathers were skewed and were transformed using square root transformations.
Parental aggravation.
The 51-item Parental Attitudes toward Child Rearing (Easterbrooks and Goldberg, 1984, 1990) tool was used to measure parental aggravation. Parental aggravation was measured at each time point from child age of 12 months to kindergarten. The scores at each time point were highly correlated with each other, with Pearson correlations ranging from .58 to .77 for mothers and from .59 to .73 for fathers. These subscale scores were averaged across time to compute the average parental aggravation score from 12 months to kindergarten. This subscale had high internal consistency, with coefficient α's ranging from .68 to .77 for mothers and from .70 to .75 for fathers.
Marital aggression.
Three measures of marital aggression were obtained at each time point from 12 months to kindergarten. Mother and father reports of physical aggression were obtained from a modified version of the Conflict Tactics Scale (CTS; Straus, 1979). Parents were asked to report the frequency of their own and their partners' aggression toward each other on a seven-item scale. Indicators of each variable were created by taking the maximum of the mother and father reports. Data were converted using square root transformations because of the skewed distribution of scores.
Verbal aggression was assessed using the verbal aggression subscale of the Index of Spouse Abuse scale (Hudson and McIntosh, 1981). Parents were asked to report on the frequency of their partners' verbal aggression toward them on the resulting 15-item measure. A composite verbal aggression measure was created by averaging the total scores for father-to-mother and mother-to-father aggression (α = .94).
The composite scales of mothers' physical aggression, fathers' physical aggression, and verbal aggression averaged over time were used as measured indicators of the latent construct reflecting marital aggression. Confirmatory factor analysis indicated that the three scales loaded on one factor, with factor loadings ranging from .73 to .81.
Child depression and anxiety.
Maternal and paternal reports of child depression and anxiety were measured from child ages of 18 months to fourth grade using the anxious/depressed subscale of the Child Behavior Checklist (Achenbach, 1992). Maternal and paternal reports on the anxious/depressed subscale were significantly correlated across time, with Pearson correlations ranging from .30 to .65 for fathers and from .30 to .60 for mothers. Maternal and paternal reports were averaged to yield a composite index of anxiety/depression from 18 months to kindergarten and at fourth grade. The internal consistency of this measure was adequate, with coefficient α's ranging from .66 to .72 for mothers and from .66 to .86 for fathers.
The Revised Child Manifest Anxiety Scale (RCMAS; Reynolds and Richmond, 1978) and the Child Depression Inventory (Kovacs, 1992) were used to measure self-reported anxiety and depression, respectively, at fourth grade. The Child Depression Inventory is the most widely used measure of childhood depression (Kazdin, 1990). The RCMAS consists of 37 items, which are divided into four subscales: physiological anxiety, worry/oversensitivity, concentration/ social concerns, and the lie scale. The child responds to each question with a “yes” or “no” answer. The total number of “yes” items for each subscale were counted and converted into a scale score to provide a total score for each subscale. For the purposes of the present study, child anxiety was assessed as a latent variable with physiological anxiety (α = .72), concentration/social concerns (α = .85), and worry/ oversensitivity (α = .71) as its measured indicators. Although the RCMAS had adequate variability, there was low variability on the Child Depression Inventory measure among fourth graders in this sample. Thus, the final model focused on self-reports of anxiety alone. The internal consistency of the RCMAS was .90 at fourth grade.
Results
Data analytic approach
Structural equation modeling was used to test the conceptual model displayed in Figure 1. All structural equation modeling analyses were conducted using Mplus, Version 4.0 software (Muthén and Muthén, 1998–2006) using full-information maximum likelihood (Arbuckle, 1996) estimation procedures. Indirect effects were tested using the biased-corrected bootstrap method. This method has been found to provide a more accurate balance between Type 1 and Type 2 errors compared with other methods used to test indirect effects (MacKinnon et al., 2004). Five hundred bootstrap samples and the 95% bias-corrected confidence intervals (CIs) were used to test the significance of indirect effects.
Missing data
As expected in any longitudinal study, there were some incomplete data for some of the participants at one or more of the six assessment points included in this study. Of the 213 families included in the analyses,1 all provided data at 12 and 18 months; 208 mothers and 204 fathers provided data at 24 months; 193 mothers and 183 fathers provided data at 36 months; 177 mothers and 167 fathers provided data at kindergarten; and 159 mothers, 153 fathers, and 166 children provided data at the fourth-grade assessment.
Overall, 71% of the participants had complete data, with participants missing information on 1 (1.93) variable on average. There were no group differences between families with missing data versus complete data on any of the model variables, with one exception. Parents with missing data reported higher levels of verbal aggression than parents with complete data (t = −2.14, 89.63 df, p < .05; d = −0.45). As noted earlier, full-information maximum likelihood was used to estimate model parameters.
Descriptive information
Descriptive and demographic information were first examined for each group of families. By the fourth-grade assessment, 16% of the biological fathers were not living with their families. Of these, 7% were in the FA group, 5% were in the both-alcoholic (BA) group, and 4% were in the NA group. Chi-square analyses revealed that this difference was not statistically significant (χ2 = 4.93, 2 df, p > .05; n = 151). All of the children who completed assessments at fourth grade had regular contact (at least once a week) with their biological fathers, and there were no group differences regarding how much time fathers (F = 0.98, 2/140 df, p > .05) or mothers (F = 1.39, 2/149 df, p > .05) spent with their children. Overall, 27 fathers (13%) and 23 mothers (11%) had been in treatment for alcohol problems at some point since recruitment and the fourth-grade assessment, 14 fathers (7%) and 11 mothers (5%) had been in treatment for drug-related problems, and 24 fathers (11%) and 38 mothers (18%) had been in treatment for psychological problems.
One-way analysis of variance tests revealed that there were no significant group differences in mothers' education (F = 0.09, 2/210 df, p > .05), total family income (F = 0.86, 2/204 df, p > .05), fathers' work hours (F = 2.91, 2/143 df, p > .05), or mothers' work hours (F = 2.21, 2/118 df, p > .05). However, there were significant group differences in terms of fathers' education (F = 3.75, 2/210 df, p < .05), such that fathers who met diagnostic criteria for alcoholism and who had partners who also met diagnostic criteria for alcoholism (i.e., the BA group) had less education than fathers who did not meet diagnostic criteria for alcoholism and who did not have partners who met those criteria (i.e., the NA group).
Descriptive information regarding group differences on risk variables and model variables is presented in Table 1. As expected, fathers in the FA and BA groups and mothers in the BA group had higher scores on all the alcohol variables. Fathers in the FA and BA groups were more antisocial than fathers in the NA group. Mothers in the BA group were more antisocial than mothers in both the FA and NA groups and more depressed than mothers in the NA group. Mothers in the FA group were more antisocial than those in the NA group. In general, by the fourth-grade assessment, 18 fathers (12%) and 20 mothers (13%) exhibited scores on the CES-D indicative of clinical depression.
Table 1.
Group differences in alcohol consumption and other variables in the model
| Variable | Total Mean (SD) | Father-alcoholic group |
No-alcoholic group (n = 101) Mean (SD) | η2 | |
| Father alcoholic (n = 82) Mean (SD) | Both alcoholic (n = 30) Mean (SD) | ||||
| Maternal QFI | 0.12 (0.20) | 0.12 (0.21) | 0.35a (0.41) | 0.06b (0.07) | .17 |
| Maternal HED T1 | 0.27 (0.50) | 0.30a (0.47) | 0.84a (0.94) | 0.12b (0.21) | .20 |
| Maternal freq. intox. T1 | 0.35 (0.48) | 0.37a (0.37) | 1.05b (0.82) | 0.17c(0.27) | .31 |
| Maternal alc. symp. T1 | 0.77 (4.55) | 0.28a (0.67) | 6.09b (13.85) | 0.07a (0.18) | .14 |
| Paternal QFI T1 | 0.75 (0.98) | 1.18a (1.07) | 1.34a (1.46) | 0.21b(0.30) | .25 |
| Paternal HED T1 | 1.61 (1.75) | 2.51a (1.57) | 3.15a (2.28) | 0.35b (0.52) | .44 |
| Paternal freq. intox. T1 | 1.12 (1.30) | 1.68a (1.03) | 2.45a (1.96) | 0.25b (0.32) | .42 |
| Paternal alc. symp. T1 | 5.74 (15.38) | 7.91a (9.18) | 15.81b (30.36) | 0.09c (0.29) | .17 |
| Maternal depression T1 | 7.48 (6.07) | 7.45 (6.15) | 10.40a (6.44) | 6.01b(5.38) | .06 |
| Paternal depression T1 | 6.86 (5.32) | 7.37 (5.12) | 8.54 (5.49) | 5.64 (5.35) | .04 |
| Maternal ASB: T1 | 35.84 (5.36) | 35.80a (4.55) | 39.33b (6.76) | 33.62c(4.14) | .14 |
| Paternal ASB: T1 | 39.76 (8.39) | 41.67a (8.11) | 44.20a (9.93) | 35.38b (5.99) | .18 |
| PR child anxiety: T1 | 3.38 (1.61) | 3.65a (1.57) | 3.96a (1.92) | 2.93b(1.30) | .07 |
| Father to mother aggr. T1 | 0.70 (0.86) | 0.69 (0.85) | 1.26a (0.94) | 0.43b (0.59) | .11 |
| Mother to father aggr. T1 | 1.14 (1.11) | 1.23 (1.02) | 1.79a (1.12) | 0.75b (0.92) | .11 |
| Mean verbal aggr. T1 | 0.59 (0.49) | 0.63a (0.46) | 0.61 (0.33) | 0.39b (0.37) | .08 |
| Maternal aggravation: T1 | 2.72 (0.53) | 2.76 (0.53) | 2.80 (0.51) | 2.60 (0.55) | .03 |
| Paternal aggravation: T1 | 2.68 (0.52) | 2.75a (0.56) | 2.64 (0.55) | 2.53b (0.48) | .04 |
| PR child anxiety: T2 | 1.97 (2.02) | 2.17 (2.15) | 2.58 (2.47) | 1.61 (1.71) | .03 |
| SR child anxiety: T2 | 35.51 (6.14) | 35.70 (6.63) | 36.00 (5.77) | 35.39 (6.04) | .00 |
Notes: QFI = quantity-frequency index; HED = heavy episodic drinking; T1 = Time 1 (12/18 months to kindergarten); freq. intox. = frequent intoxication; alc. symp. = alcohol symptoms; ASB = antisocial behavior; PR = parental report; aggr. = aggression; SR = self-report; T2 = Time 2 (fourth grade).
In each row, statistics with different superscripts are significantly different from one another at p < .05.
Although no group differences were apparent with regard to children's self-reports of anxiety or parental reports of child depression/anxiety at the fourth-grade assessment, there were significant group differences in parents' reports of child depression/anxiety at Time 1 (average of 18- to 60-month scores). Parents in the FA and BA groups reported higher levels of child depression/anxiety than parents in the NA group. Parents in the BA group also reported signifi cantly higher levels of family aggression than parents in the NA group. Finally, fathers in the FA group reported higher levels of aggravation with their children than fathers in the NA group.
Correlational analyses
At the level of correlations, higher levels of maternal and paternal depression were each associated with higher levels of maternal and paternal antisocial behavior, higher levels of maternal and paternal aggravation with their children, and higher levels of each of the indices of marital aggression. Moreover, higher levels of maternal and paternal depression were each positively associated with parental reports of child depression/anxiety at Time 1 and Time 2.
Higher levels of maternal and paternal antisocial behavior were each associated with higher levels of maternal and paternal aggravation, higher levels of marital aggression, and higher levels of parent-reported child depression/anxiety at Time 1 and Time 2. Maternal and paternal aggravation with their children were each positively associated with each of the indicators of marital aggression and with parental reports of child depression/anxiety at Time 1 and Time 2. Each of the indicators of marital aggression were positively related to one another and were related to parental reports of child depression/anxiety at Time 1 and Time 2.
Moreover, each of the indices of marital aggression was positively associated with self-reported child anxiety assessed at fourth grade. Interestingly, although parental reports of child depression/anxiety at Time 1 and Time 2 were positively related to one another, parental reports of child depression/anxiety at Time 1 and Time 2 were not related to self-reported child anxiety assessed at fourth grade.
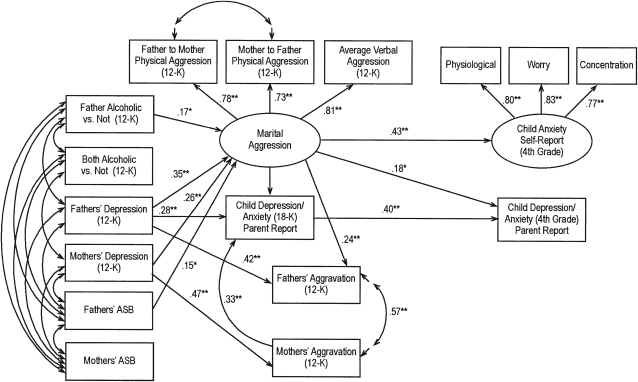
Structural equation model analyses
The conceptual model tested is depicted in Figure 1. Goodness of fit indices revealed that the structure of our hypothesized model was an adequate explanation of the data (i.e., χ2 = 84.69, 59 df, p < .05; χ2/df = 1.44; comparative fit index = .98; root mean square error of approximation = .05). The significant parameter coefficients for this model are depicted in Figure 2. Overall, the maternal and paternal risk factors (i.e., alcohol diagnosis, depression, and antisocial behavior) were generally associated with one another (see Tables 1 and 2). Maternal and paternal symptoms of depression were positively associated with each other, as were maternal and paternal antisocial behavior. Finally, paternal aggravation was positively associated with maternal aggravation. As might be expected from the correlational analyses, at fourth grade, parent-reported child depression/anxiety was not related to self-reported child anxiety.
Figure 2.
Results of structural equations modeling. The numbers represent standardized path coefficients. Nonsignificant paths are not depicted in the figure for ease of presentation. Covariances between exogenous variables were included in model testing but not depicted in figure; these are reported in Table 1. The error terms for the measured indicator are not depicted in figure. 12-K = child ages 12 months to age at kindergarten; ASB = antisocial behavior.
*p < .05; **p < .01.
Table 2.
Correlations among measured variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
| 1. Child gender | — | ||||||||||||||
| 2. FA vs not | .01 | — | |||||||||||||
| 3. BA vs not | −.02 | −.32* | — | ||||||||||||
| 4. Maternal depression | −.07 | .11 | .13 | — | |||||||||||
| 5. Paternal depression | .02 | .15* | .08 | .19* | — | ||||||||||
| 6. Maternal ASB | −.05 | .14* | .29* | .37* | .25* | — | |||||||||
| 7. Paternal ASB | −.01 | .24* | .29* | .30* | .31* | .48* | — | ||||||||
| 8. Maternal aggravation | −.06 | .10 | .06 | .54* | .23* | .24* | .23* | — | |||||||
| 9. Paternal aggravation | −.05 | .17* | .03 | .16* | .56* | .23* | .30* | .38* | — | ||||||
| 10. Verbal aggression | −.09 | .27* | .07 | .40* | .41* | .30* | .33* | .33* | .39* | — | |||||
| 11. FM aggression | .00 | .12 | .21* | .32* | .38* | .35* | .41* | .30* | .38* | .63* | — | ||||
| 12. MF aggression | .03 | .23* | .14* | .29* | .36* | .34* | .32* | .24* | .31* | .59* | .74* | — | |||
| 13. PR anxiety (18-K) | .07 | .13* | .09 | 38* | .43* | .28* | .29* | .49* | .38* | .29* | .31* | .27* | — | ||
| 14. PR anxiety (4th gr.) | .05 | .05 | .14 | 17* | .30* | .20* | .25* | .30* | .19* | .26* | .25* | .27* | 47* | — | |
| 15. SR anxiety (4th gr.) | −.02 | −.02 | −.01 | .06 | .11 | .09 | .09 | .03 | −.02 | .20* | .22* | .32* | .06 | .13 | — |
Notes: FA = father alcoholic; BA = both alcoholic; ASB = antisocial behavior; FM = father to mother; MF = mother to father; PR = parental report; 18-K = 18 months to kindergarten; gr. = grade; SR = self-report.
p < .05.
The structural paths indicated that fathers' alcohol diagnosis (i.e., whether fathers met diagnostic criteria for alcoholism), maternal and paternal depression, and paternal antisocial behavior were associated with higher levels of marital aggression. Moreover, after controlling for prior levels of child depression/anxiety, marital aggression was predictive of higher levels of child anxiety at fourth grade, as reported by both parents and the children themselves. That is, higher levels of marital aggression at Time 1 predicted higher levels of child anxiety at fourth grade, after accounting for child depression/anxiety at Time 1.
Paternal depression was related to higher levels of fathers' aggravation with their children. Correspondingly, maternal depression was associated with higher levels of mothers' aggravation with their children. However, neither maternal aggravation nor paternal aggravation was predictive of child anxiety as reported by parents or children at the fourth grade. Within time, marital aggression was positively associated with fathers' aggravation with their children, such that fathers in relationships characterized by greater marital aggression were more likely to report greater aggravation with their children.
Finally, mothers' aggravation with their children was positively associated with higher levels of parent-reported child depression/anxiety at Time 1. Thus, mothers who were more aggravated with their children had children with higher levels of depression/anxiety, as reported by parents.
Our model included hypotheses about several indirect effects. Thus, the bias-corrected bootstrap method was employed to determine whether the implied indirect effects within our hypothesized model were statistically significant. The association between fathers' alcoholism and children's anxiety symptoms was expected to be indirect, via higher marital aggression. Results demonstrated that the indirect effect of fathers' alcohol diagnosis on children's self-reported anxiety in fourth grade was statistically significant (B = 0.27, 95% confidence interval [CI]: 0.04–0.77).
Because there were unique associations between parents' depression and marital aggression, we also tested the significance of the indirect paths from parents' depression to child anxiety in fourth grade via higher marital aggression. Both the indirect effects of father's depression (B = 0.05, 95% CI: 0.01–0.12) and mother's depression (B = 0.03, 95% CI: 0.01–0.07) on children's self-reports of anxiety in fourth grade via marital aggression were statistically significant. However, the indirect association from fathers' antisocial behavior to child self-reports of anxiety in fourth grade via marital aggression was nonsignificant.
We next tested the significance of the indirect effects on parental reports of child depression/anxiety at fourth grade. Results indicated that there was a significant indirect path from fathers' alcohol diagnosis to parental reports of child depression/anxiety through marital aggression (B = 0.13, 95% CI: 0.01–0.35). In addition to fathers' alcoholism, there was a significant indirect association between fathers' depression and parental reports of child depression/anxiety at fourth grade via parental reports of child depression/anxiety at Time 1 (B = 0.04, 95% CI: 0.02–0.09), such that higher levels of paternal depression were related to higher levels of parent-reported anxiety at Time 1, which in turn predicted increases in parent-reported child depression/anxiety at fourth grade.
Discussion
The major purpose of this study was to examine whether parents' alcoholism was associated with children's internalizing symptoms via marital aggression or parental aggravation. Results were supportive of the hypothesis that fathers' alcoholism would be associated with higher child internalizing symptoms via greater levels of marital aggression among alcoholic families. Results also indicated that there was a significant indirect association between parents' depression symptoms and child-reported anxiety via marital aggression.
The association between alcoholism and greater marital aggression has been well documented (see Leonard and Eiden, 2007). As indicated in this review, men's heavy drinking and alcohol problems are robust correlates of greater aggression toward women. This association has been noted across different high-risk and community samples, including health care settings such as emergency rooms, primary care clinics, family practice clinics, prenatal clinics, and rural health care clinics. It has also been noted in large community studies of newlywed couples (Quigley and Leonard, 2000) and nationally representative samples (O'Leary and Schumacher, 2003).
Higher average marital aggression over the first 5 years of the child's life was predictive of higher child anxiety at fourth grade. Results regarding this prospective association between marital aggression and child anxiety are supportive of previous studies with older cohorts. For instance, Jekielek (1998) reported that after controlling for initial levels of anxiety among 6- to 14-year-old children, marital conflict and divorce were predictive of anxiety 6 years later. Indeed, the effect of divorce on children's anxiety was time limited, but the effect of marital conflict was not.
Emery (1989) suggested several processes through which marital aggression may affect child outcomes. These include social learning processes by which children may model ineffective conflict resolution behaviors such as withdrawal, one symptom of internalizing disorders. Higher marital conflict may also be related to inconsistent parenting, which may be related to lack of predictability for the child, leading to higher levels of anxiety. Finally, exposure to marital aggression may serve as a general source of stress, threatening the child's sense of security and leading to higher anxiety symptoms. This hypothesis has received much attention from proponents of the emotional security theory (Davies and Cummings, 1994) and has been supported by empirical evidence examining the processes explaining the association between marital aggression and child functioning (Keller et al., 2008).
Contrary to expectations, parental aggravation was not predictive of child anxiety over time, although higher maternal aggravation was associated with higher parental reports of child depression/anxiety within time. It is also worth noting that both maternal and paternal aggravation variables were associated with parental reports of child depression/anxiety at Time 1 and Time 2 at the level of correlations.
However, parental aggravation did not predict changes in parental reports of child depression/anxiety. The lack of association between these parenting variables and child anxiety may be, in part, a result of their association with marital aggression. It is important not to reach the conclusion that parenting is unimportant. Other aspects of parenting may be predictive of child anxiety. For instance, reviews of the literature between dimensions of parenting and child anxiety have concluded that there is converging evidence of the association between over-controlling parenting behavior and child anxiety (Bogels and Brechman-Toussaint, 2006; Rapee, 1997; Wood et al., 2003). These reviews also concluded that there was less consistent association between low parental warmth or high negativity and child anxiety. Future longi tudinal studies with measures of parental warmth and over-control may test this hypothesis among children of alcoholic and nonalcoholic families.
Contrary to expectations, there were few direct associations between parental depression and child anxiety symptoms as evident from the correlational analyses. Instead, associations between parental depression and child anxiety were indirect, via marital aggression. Few studies have examined the role of marital aggression when examining the role of paternal depression and child anxiety. However, several have examined the potential role of the broader concept of contextual risk including marital discord when examining the association between maternal depression and internalizing behavior problems. These studies have generally yielded mixed results.
For instance, Cicchetti et al. (1998) reported that maternal depression was associated with child internalizing problems, but contextual risk did not account for additional variance. Duggal et al., (2001) indicated that contextual risk factors did account for additional variance in predicting child depression in middle childhood. Others indicated that contextual risk mediated the association between maternal depression and behavior problems in the preschool (Dawson et al., 2003) and early school (Ashman et al., 2008) years. The current results are supportive of these latter findings indicating that the association between paternal and maternal depression and child anxiety is indirect, via higher marital aggression.
Although these findings fill an important gap in the literature, there are several limitations as well. For instance, although recruiting a community sample of alcoholic and nonalcoholic families is an obvious strength with regard to generalizability compared with treatment samples, there are also limitations. The response rate to our recruitment letter was around 25%. This raises the possibility that responders may be biased compared with the larger population.
In addition, we did not have a group of alcoholic mothers with nonalcoholic partners. Thus, the role of maternal alcohol problems independent of paternal problems could not be examined in this study. However, it is worth noting that women with alcohol problems are more likely to have partners with alcohol problems than vice versa (Roberts and Leonard, 1997), making this a difficult group to recruit.
Finally, associations among parental reports of parenting, marital aggression, and parental reports of child depression/anxiety may be partly the result of shared method variance. Although this is a limitation for parental reports, there was a significant indirect association between fathers' alcoholism and child reports of anxiety via marital aggression as well.
Despite these limitations, the study makes an important and unique contribution to the literature in a number of ways. First, it uses a longitudinal design beginning in infancy compared with the majority of studies on children of alcoholics that begin in early adolescence (with one exception: the Michigan Longitudinal study beginning in the preschool period). Second, we examine risk pathways to childhood anxiety using a high-risk sample of alcoholic families. Third, marital context and parenting for both mothers and fathers are included as key etiological constructs. Few previous studies of children of alcoholics have examined process models of anxiety, and few studies of child anxiety have included both parents.
In conclusion, although most of the literature has focused on externalizing problems, we found that children of alcoholics are also at higher risk for depression/anxiety, at least according to parental reports. Importantly, our study began to flesh out early risk pathways that account for this association. Namely, levels of marital discord are high among alcoholic families, and this has a deleterious effect on children's internalizing problems at a relatively young age. Treatment for alcohol problems that address the dual issues of alcoholism and marital discord may be particularly beneficial for children of alcoholic families.
The results also highlight the importance of including family-level variables in the study of risk for internalizing behavior problems among children of alcoholics. Further elaboration of family-level mediators will likely inform more effective interventions.
Acknowledgment
We thank the parents and children who participated in the study and the research staff who were responsible for conducting the parent-child assessments with these families.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism grant R01 AA 10042.
The original sample consisted of 227 families. Of these, 14 families consisted of mothers with alcohol problems and partners who did not have alcohol problems by the time children reached kindergarten age. These families were not included in the current analyses.
References
- Achenbach TM. Manual for the Child Behavior Checklist/2-3 and 1992 Profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1992. [Google Scholar]
- Andreasen NC, Rice J, Endicott J, Reich T, Coryell W. The family history approach to diagnosis: How useful is it? Arch. Gen. Psychiat. 1986;43:421–429. doi: 10.1001/archpsyc.1986.01800050019002. [DOI] [PubMed] [Google Scholar]
- Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: Basic findings from the National Comorbidity Survey. Exp. Clin. Psychopharmacol. 1994;2:244–268. [Google Scholar]
- Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced Structural Equation Modeling: Issues and Techniques. Mahwah, NJ: Lawrence Erlbaum; 1996. pp. 243–277. [Google Scholar]
- Ashman SB, Dawson G, Panagiotides H. Trajectories of maternal depression over 7 years: Relations with child psychophysiology and behavior and role of contextual risks. Devel. Psychopathol. 2008;20:55–77. doi: 10.1017/S0954579408000035. [DOI] [PubMed] [Google Scholar]
- Bogels SM, Brechman-Toussaint ML. Family issues in child anxiety: Attachment, family functioning, parental rearing and beliefs. Clin. Psychol. Rev. 2006;26:834–856. doi: 10.1016/j.cpr.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: Predicting young adult substance use disorders, anxiety, and depression. J. Abnorm. Psychol. 1999;108:106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. Maternal depressive disorder and contextual risk: Contributions to the development of attachment insecurity and behavior problems in toddlerhood. Devel. Psychopathol. 1998;10:283–300. doi: 10.1017/s0954579498001618. [DOI] [PubMed] [Google Scholar]
- Colder CR, Chassin L. Affectivity and impulsivity: Temperament risk for adolescent alcohol involvement. Psychol. Addict. Behav. 1997;11:83–97. [Google Scholar]
- Davies PT, Cummings EM. Marital conflict and child adjustment: An emotional security hypothesis. Psychol. Bull. 1994;116:387–411. doi: 10.1037/0033-2909.116.3.387. [DOI] [PubMed] [Google Scholar]
- Dawson G, Ashman SB, Panagiotides H, Hessl D, Self J, Yamada E, Embry L. Preschool outcomes of children of depressed mothers: Role of maternal behavior, contextual risk, and children's brain activity. Child Devel. 2003;74:1158–1175. doi: 10.1111/1467-8624.00599. [DOI] [PubMed] [Google Scholar]
- Duggal S, Carlson EA, Sroufe LA, Egeland B. Depressive symptomatology in childhood and adolescence. Devel. Psychopathol. 2001;13:143–164. doi: 10.1017/s0954579401001109. [DOI] [PubMed] [Google Scholar]
- Easterbrooks MA, Goldberg WA. Toddler development in the family: Impact of father involvement and parenting characteristics. Child Devel. 1984;55:740–752. [PubMed] [Google Scholar]
- Easterbrooks MA, Goldberg WA. Security of toddler-parent attachment: Relation to children's sociopersonality functioning during kindergarten. In: Greenberg MT, Cicchetti D, Cummings EM, editors. Attachment in the Preschool Years: Theory, Research, and Intervention. Chicago, IL: Univ. of Chicago Press; 1990. pp. 221–244. [Google Scholar]
- Edwards EP, Leonard KE, Eiden RD. Temperament and behavioral problems among infants in alcoholic families. Infant Ment. Health J. 2001;22:374–392. doi: 10.1002/imhj.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiden RD, Foote A, Schuetze P. Maternal cocaine use and caregiving status: Group differences in caregiver and infant risk variables. Addict. Behav. 2007;32:465–476. doi: 10.1016/j.addbeh.2006.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiden RD, Leonard KE. Paternal alcoholism, parental psychopathology, and aggravation with infants. J. Subst. Abuse. 2000;11:17–29. doi: 10.1016/s0899-3289(99)00016-4. [DOI] [PubMed] [Google Scholar]
- Emery RE. Family violence. Amer. Psychol. 1989;44:321–328. doi: 10.1037//0003-066x.44.2.321. [DOI] [PubMed] [Google Scholar]
- Grych JH. Marital relationships and parenting. In: Bornstein MH, editor. Handbook of Parenting, Vol. 4: Social Conditions and Applied Parenting. 2nd Edition. Mahwah, NJ: Lawrence Erlbaum Associates; 2002. pp. 203–225. [Google Scholar]
- Ham HP, Zucker RA, Fitzgerald HE. Assessing antisociality with the Antisocial Behavior Checklist: Reliability and validity studies; Poster presented at the annual meeting of the American Psychological Society; Chicago, IL. 1993. [Google Scholar]
- Hudson WW, McIntosh SR. The assessment of spouse abuse: Two quantifiable dimensions. J. Marr. Fam. 1981;43:873–885. [Google Scholar]
- Hussong AM, Cai L, Curran PJ, Flora DB, Chassin LA, Zucker RA. Disaggregating the distal, proximal, and time-varying effects of parent alcoholism on children's internalizing symptoms. J. Abnorm. Child Psychol. 2008;36:335–346. doi: 10.1007/s10802-007-9181-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jekielek SM. Parental conflict, marital disruption and children's emotional well-being. Social Forces. 1998;76:905–936. [Google Scholar]
- Kazdin AE. Assessment of childhood depression. In: LaGreca AM, editor. Through the Eyes of the Child: Obtaining Self-Reports From Children and Adolescents. Boston, MA: Allyn & Bacon; 1990. pp. 189–233. [Google Scholar]
- Keller PS, Cummings EM, Davies PT, Mitchell PM. Longitudinal relations between parental drinking problems, family functioning, and child adjustment. Devel. Psychopathol. 2008;20:195–212. doi: 10.1017/S0954579408000096. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The national comorbidity survey: Preliminary results and future directions. Int. J. Meth. Psychiat. Res. 1995;5:139–151. [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wiltchen H-U, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Arch. Gen. Psychiat. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kovacs M. The Children's Depression Inventory-Manual. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- Leonard KE, Eiden RD. Marital and family processes in the context of alcohol use and alcohol disorders. Annual Rev. Clin. Psychol. 2007;3:285–310. doi: 10.1146/annurev.clinpsy.3.022806.091424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivar. Behav. Res. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minuchin P. Families and individual development: Provocations from the field of family therapy. Child Devel. 1985;56:289–302. [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide, Version 4. Los Angeles, CA: Muthén & Muthén; 1998–2006. [Google Scholar]
- O'Leary KD, Schumacher JA. The association between alcohol use and intimate partner violence: Linear effect, threshold effect, or both? Addict. Behav. 2003;28:1575–1585. doi: 10.1016/j.addbeh.2003.08.034. [DOI] [PubMed] [Google Scholar]
- Puttler LI, Zucker RA, Fitzgerald HE, Bingham CR. Behavioral outcomes among children of alcoholics during the early and middle childhood years: Familial subtype variations. Alcsm Clin. Exp. Res. 1998;22:1962–1972. [PubMed] [Google Scholar]
- Quigley BM, Leonard KE. Alcohol and the continuation of early marital aggression. Alcsm Clin. Exp. Res. 2000;24:1003–1010. [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. [Google Scholar]
- Rapee RM. Potential role of childrearing practices in the development of anxiety and depression. Clin. Psychol. Rev. 1997;17:47–67. doi: 10.1016/s0272-7358(96)00040-2. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of children' manifest anxiety. J. Abnorm. Child Psychol. 1978;6:271–280. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- Roberts LJ, Leonard KE. Gender differences and similarities in the alcohol and marriage relationship. In: Wilsnack RW, Wilsnack SC, editors. Gender and Alcohol: Individual and Social Perspectives. New Brunswick, NJ: Rutgers Center of Alcohol Studies; 1997. pp. 289–311. [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics (CT) Scales. J. Marr. Fam. 1979;41:75–88. [Google Scholar]
- Swendsen JD, Tennen H, Carney MA, Affleck G, Willard A, Hromi A. Mood and alcohol consumption: An experience sampling test of the self-medication hypothesis. J. Abnorm. Psychol. 2000;109:198–204. [PubMed] [Google Scholar]
- Wood JJ, McLeod BD, Sigman M, Hwang W-C, Chu BC. Parenting and childhood anxiety: Theory, empirical findings, and future directions. J. Child Psychol. Psychiat. 2003;44:134–151. doi: 10.1111/1469-7610.00106. [DOI] [PubMed] [Google Scholar]
- Zucker RA, Noll RB. The Antisocial Behavior Checklist. East Lansing, MI: Department of Psychology, Michigan State University; 1980. unpublished instrument. [Google Scholar]