Abstract
Purpose
Historically, informed consent forms have been developed for the purpose of educating patients. However, informed consent forms can be very difficult to understand. Our hypothesis is that a method utilizing diagrams will improve patient-physician communication without increasing the time required to obtain informed consent over the teach-the-teacher method as well as over our current standard informed consent protocol.
Methods
This was a prospective, randomized, controlled study. Institutional review board approval and informed consent was obtained. The investigators were in compliance with HIPAA. Ninety-nine of 109 patients undergoing a spine injection agreed to participate and completed the study. The patients were randomly assigned to the control group (informed consent obtained in the customary manner at our institution with twelve key points of consent and home-care discussed conversationally); the teach-the-teacher group (patients had to repeat the twelve key points to the physician before informed consent was complete); and the diagram group (patients viewed a set of diagrams illustrating the twelve key points before signing the informed consent form). After the procedure, the patients finished a survey to test knowledge recall, anxiety, and pain during the procedure.
Results
Statistically significant results included: a lower survey score for the control group; longer time required for the teach-the-teacher group in comparison to the control group; a negative correlation between age and survey score in the teach-the-teacher group.
Conclusions
The diagram method required less time than the teach-the-teacher method, had no negative correlation in survey score results with age, and had improved patient-physician communication over the control group.
Keywords: Education, Communication, Efficacy Studies, Health Policy and Practice, Safety
Purpose
Unencumbered patient-physician communication is the central core to a sound, viable patient-physician relationship. However, patients can have difficulty understanding many aspects of medical care [1]. With only 12% of the American adult population having health literacy rated at a proficient level, it is imperative that physicians work to provide information in understandable terms [2]. Furthermore, the Institute of Medicine’s report Crossing the Quality Chasm: A New Health System for the 21st Century stresses the paramount importance of improved communication for improved delivery of care [3]. Therefore, the fundamental concepts of communication and patient education are essential to providing patients with information so that they may make sense of medical issues and make informed healthcare decisions. Research that studies ways to improve patient-physician communication directly addresses at least two of the ten “Rules for Redesign” proposed by the Institute of Medicine. Verbatim, these two rules are: A. The patient is the source of control. Patients should be given the necessary information and opportunity to exercise the degree of control they choose over health care decisions that affect them. The system should be able to accommodate differences in patient preferences and encourage shared decision making. B. Knowledge is shared and information flows freely. Patients should have unfettered access to their own medical information and to clinical knowledge. Clinicians and patients should communicate effectively and share information. [3]
In the field of radiology, a significant portion of patient-physician communication is committed to the informed consent process for procedures. Standard informed consent protocols typically involve physicians conversationally listing steps of the procedure and possible complications as well as providing an information pamphlet or form describing the procedure. Previous attempts have been made to improve the informed consent process by utilizing different means of communication, although few studies have focused on improving patient-physician communication in informed consent for invasive radiological procedures. One studied method, in which patients were asked to recite material back to the radiologist as part of the informed consent protocol, has shown improved comprehension [4]. However, additional time was required for this “teach-the-teacher” method. Developing an alternative informed consent protocol that would improve patient education with a minimal increase in time needed would be beneficial. Diagrams have been utilized for enhancing patient education and have been tested with improved comprehension in the setting of home care instructions [5]. However, evaluating teach-the-teacher and diagram methods has not been done in a head-to-head comparison while using a control group. Therefore, evaluating both the “teach-the-teacher” and “diagram” methods head-to-head as well as in comparison to a standard informed consent process in a single study would provide valuable comparative information on patient-physician communication and time requirements for all three methods. This information is not currently available in the medical imaging literature.
Therefore, this study was designed to evaluate and compare methods for improving patient informed consent for a radiological procedure in order to aid in the approach to a population with health literacy issues. Our hypothesis is that a method utilizing diagrams will improve patient knowledge recall (with recall being tested by a multiple choice survey) without increasing the time required to obtain informed consent over the teach-the-teacher method as well as over our current standard informed consent protocol.
Methods
This was a prospective, randomized, controlled study. Institutional review board (IRB) approval was obtained before commencement of the study and the investigators were in compliance with HIPAA. The two alternate methods of informed consent were developed before commencement of the study. Twelve key points were developed before commencement of the study and were included in all three methods of informed consent (Figure 1). The twelve key points were developed by consensus opinion among three radiologists who each had at least 10 years of experience in performing imaging guided spinal injection procedures at our institution. The physicians (eight radiologists) involved in performing the procedures in this study were instructed to include the same twelve key points during the informed consent process for all patients in order to assure uniformity and to cover the information that would be tested on the written examination. However, the physicians were not limited to these twelve points in their discussions with the patients.
Figure 1.
The twelve key points of spine injection procedures.
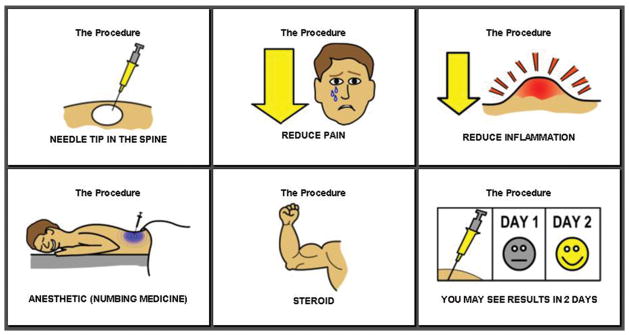
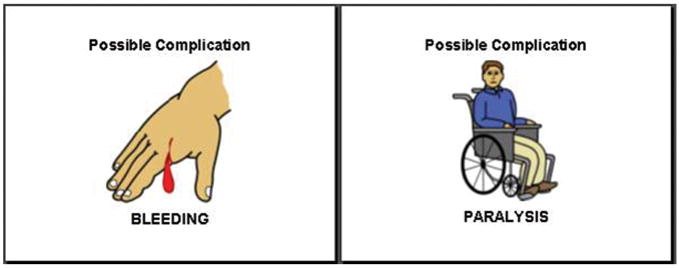
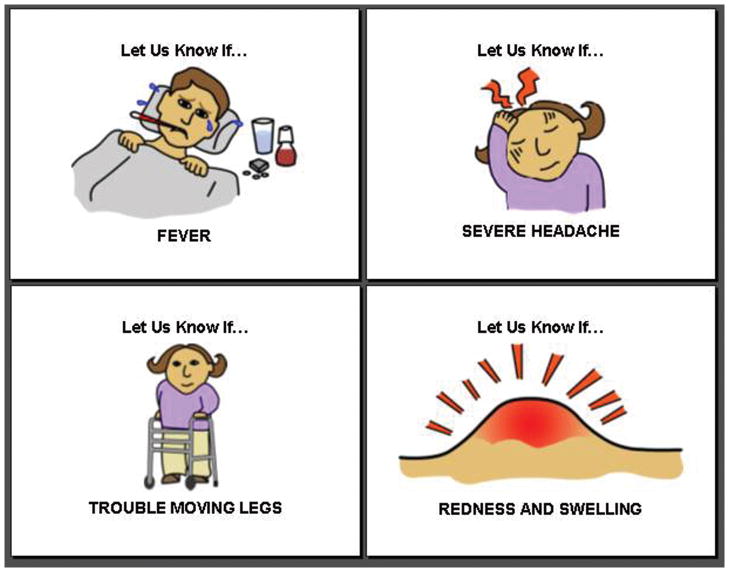
109 patients undergoing spine injections (epidural steroid, nerve root, and facet joint injections) in musculoskeletal radiology were invited to take part in the study when they arrived in the department for their procedure, of which 99 agreed to participate and completed the study. Patient research informed consent was obtained prior to the procedure (by a research assistant trained and approved by the IRB) from those who agreed to participate using research informed consent forms approved by our IRB. A research assistant randomly assigned patients to the control group (informed consent obtained in the customary manner at our institution, which is a conversational description of the twelve key points of consent and home-care with the patients given the opportunity to read and sign the printed procedure informed consent document); the teach-the-teacher group (patients had to verbally repeat the twelve key points without error to the physician before the patient could sign the informed consent form); and the diagram group (patients viewed a set of diagrams illustrating the twelve key points before signing the informed consent form) (Figure 2). The eight radiologists participating in the study received no specialized formal education in the teach-the-teacher method or diagrams method. However, the eight radiologists were formally instructed on the definition of each group, and that the patients had to verbally repeat the twelve key points without error to the physician in the teach-the-teacher group, and that the diagrams must be shown to the patients in the diagram group.
Figure 2.
Cartoons used for the Diagram Method. (A) Cartoons used to describe the procedure. (B) Cartoons used to describe possible complications. (C) Cartoons used to describe the post-procedure instructions.
The randomization was done on a rotating basis; that is, the first patient enrolled in the study was assigned to the control group, the second to the teach-the-teach group, the third to the diagram group, the fourth to the control group, etc. The subjects were educated about the procedure and the possible risks by one of eight radiologists (that perform image guided spine injections at our institution) before the procedure to achieve informed consent. After the procedure the radiologist who performed the procedure educated the subjects about home care instructions. These radiologists were blind as to the study hypothesis. However, these radiologists were aware that the enrolled patients would be taking a survey, but the radiologists did not have access to the survey or its questions. Each radiologist worked one week and saw approximately twelve enrolled patients, therefore, approximately three patients from each group. That is, all imaging guided spine injections were performed by the same radiologist for a week. The first patient the radiologist saw was assigned to the control group, the second patient to the teach-the-teacher group, the third patient to the diagrams group, the fourth patient to the control group, etc. All patients, regardless of group, were given the opportunity to ask questions and have them answered before the informed consent process was deemed finished. Information on the time required for the informed consent process and the length of the procedure was recorded for each patient by one of the researchers. This same researcher also made sure the twelve key points were communicated to the patient by the radiologist. Patients were also asked if they had received prior spinal injection procedures.
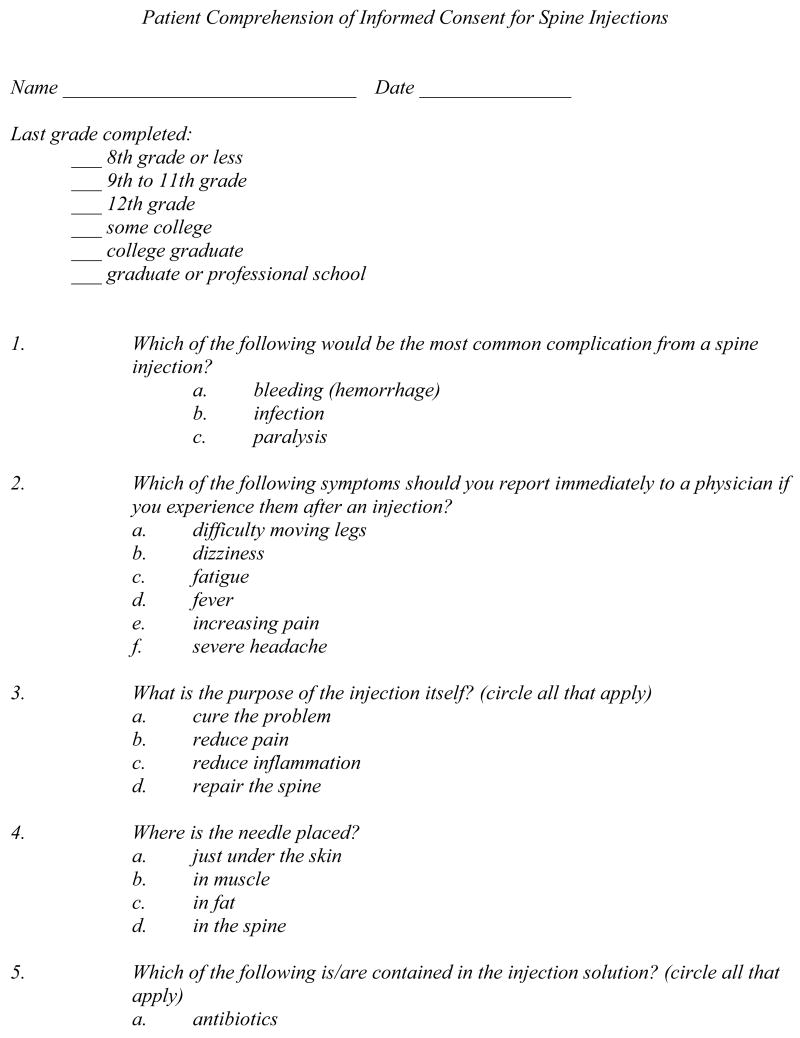
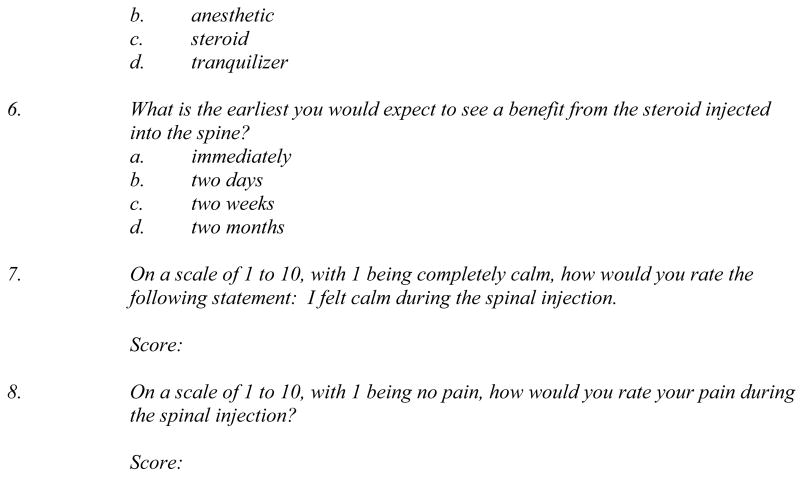
Following the procedure, the patients completed a multiple choice survey to test recall of information included in the twelve key points given by the doctor (Figure 3). The survey was developed based on the twelve key points. The diagrams were developed based on the twelve key points as well, without access to the survey questions. The diagrams were designed by one of the authors (who has a special interest in graphic arts). This author developed the cartoons with the idea of them being as simple as possible and conveying mild humor (when possible and appropriate). Several of the multiple choice questions required the patient to circle all that apply. The survey was read aloud to any patient with difficulty reading. The subjects were also asked to rate their pain and anxiety during the procedure on a scale of 1 to 10, with 1 being a completely painless procedure or completely calm during the procedure, respectively. The survey asked for the level of formal education completed by the patient. Only the patient’s age, gender, and assigned study group were used on the survey form. The patient’s were allowed to take as long as they wished to complete the survey.
Figure 3.
The post-procedure survey.
The scores for the questions addressing patient comprehension were obtained by adding one point for every correct answer and subtracting one point for every incorrect answer. Therefore, the patients were not penalized for failing to answer a question, but they were penalized for incorrectly answering a question. This scoring system was used to discourage patients from guessing the correct answer and to improve test reliability [6]. The maximum score possible was 10. The scores were adjusted for the patients undergoing epidural steroid injections who answered that the injection solution contained steroid, but no anesthetic. The adjustment consisted of regrading question five on the surveys done by patients who received an epidural steroid injection because this was initially graded incorrectly. The time required for the process was obtained by summing the time needed for the informed consent process and the take home instructions. The collected data was analyzed using SAS® software. Statistical methods used included: factorial analysis of variation and Pearson correlation for interval data; Mantel-Haensel chi-square for nominal data. P ≤ 0.05 was considered significant.
Results
The data collected for all patients are given in Table 1. There were 33 patients in the control group, 34 patients in the teach-the-teacher Group, and 32 patients in the diagram group.
Table 1.
Summary of Survey Results.
| Control | Teach | Diagram | |
|---|---|---|---|
| Mean Score (Standard Deviation) | 5.5 (+/−2.5) * | 7.4 (+/−2.0) | 7.3 (+/−2.2) |
| Minimum Score | 0 | 1 | 1 |
| Maximum Score | 10 | 10 | 10 |
| Median Score | 6 | 8 | 8 |
| 70+ Mean Score (Standard Deviation) | 5.3 (+/−2.4) | 6.3 (+/−2.5) | 7.5 (+/−2.8) |
|
| |||
| Average Time in Minutes (Standard Deviation) | 5.8 (+/−2.5) | 8.1 (+/−3.4) † | 6.8 (+/−2.7) |
|
| |||
| Median Anxiety Score | 2 | 3 | 2 |
|
| |||
| Median Pain Score | 2 | 2 | 3 |
LEGEND: Control (heading of column 1) refers to the control group; Teach (heading of column 2) refers to the teach-the-teacher method group; Diagram (heading of column 3) refers to the diagram method group; Mean Score refers to the mean survey score obtained from questions 1 through 6 from the survey; 70+ Mean Score refers to the mean survey score of patients ≥70 years of age obtained from questions 1 through 6 from the survey; Average Time refers to the mean time (in minutes) required by the physician to obtain informed consent and give post-procedure instructions;
means this result is statistically significant from the Teach and Diagram Groups results in this row;
means this result is statistically significant from the Control Group result in this row.
In order to verify that the groups were indeed comparable, the data pertaining to the demographics were analyzed. No statistically significant difference was found among the three groups with respect to age, gender, level of formal education, and history of prior spinal procedures.
The average survey score (out of 10) was 5.5 for the control group, 7.4 for the teach-the-teacher group, and 7.3 for the diagram group. An analysis of variance (F test) for the scores, controlling for multiple comparisons, revealed statistically significant differences in the teach-the-teacher group compared to the control group and the diagram group compared to the control group (p ≤0.05). Therefore, the control group score was statistically significant from and lower than the other groups.
There was no statistically significant difference between the survey scores based on gender, level of formal education, history of prior spinal procedures, or length of time the procedure took. Interestingly, there was a statistically significant (p ≤0.05) negative correlation between age and score in the teach-the-teacher group.
The average time needed was analyzed to determine whether the alternate methods required additional time over the control group. The average length of time needed for each method of educating the patients was 5.8 minutes for the control group, 8.1 minutes for the teach-the-teacher group, and 6.8 minutes for the diagram group. The increased time required for the teach-the-teacher group was statistically significant from the time required for the control group.
None of the patients required that the survey be read to them. Some patients asked only one or two clarifying questions about the survey; however, this was not recorded as part of the study. One patient left two questions unanswered (questions four and six). Nine patients left one question unanswered. Of these nine, eight did not answer question one and one did not answer question four.
The study was also designed to evaluate the patients’ ratings of pain and anxiety. There was no statistically significant difference in the pain and anxiety ratings among the three groups.
Discussion
The diagram method was the most successful in this study. The diagram method required less time than the teach-the-teacher method, had no negative correlation with age, and had improved survey scores (improved patient recall/recognition) over the control group.
It is important for physicians to communicate information to patients in a manner that allows the patients to understand the information. Therefore, this study investigated two alternative methods for improving patient-physician communication during the informed consent process.
The results revealed that both the teach-the-teacher and diagram methods achieved better survey scores than the control group with no statistically significant difference between the scores of the teach-the-teacher group and the diagram group. The absence of a negative correlation (with regards to age) in the diagram group suggests that the elderly subpopulation may benefit from the use of diagrams during the informed consent process. The scores of the subjects 70 and older support this, with averages of 5.3 for the control group (n=11), 6.3 for the teach-the-teacher group (n=11), and 7.5 for the diagram group (n=10). However, a larger population size would be needed to confirm that these differences are statistically significant.
The additional time needed for the alternate methods (2.3 minutes for the teach-the-teacher group and 1.0 minute for the diagram group) suggests that improved educational techniques do not require considerably more time. This increase in time needed for the process may likely be due to increased interaction between the doctor and patient resulting in more questions asked by the patient about the procedure.
Our results were compared to a similar study that compared comprehension for informed consent between a control group and a teach-the-teacher group [4]. This prior study also found improved comprehension for the teach-the-teacher group. Additionally, the prior study reported an increase in time required for the teach-the-teacher method; however, the additional time to obtain consent was not quantified in this prior article.
We also compared our results with a prior study that compared recall for post-procedure instructions between a control group and a diagram group [5]. This prior study similarly found that there was improved recall of intructions in the diagram group with no difference between age, gender, or level of education. Also of interest is that the diagrams in our study and the prior study included elements of humor in the illustrations.
Why would humorous cartoons improve patient-physician communication (as measured by recall) across the general population? One reason would be the inclusion of humor in the communication or educational process. It has been shown that educating or communicating with humor improves recall on multiple choice examinations [7]. Another reason for improved recall from illustrations is the elimination of an illiteracy bias. One of the major forms of early (elementary or grade school) education is the use of illustrations. Since a some patients may have low healthy literacy level [2] that is comparable to early grade school training, perhaps cartoons are a method of communication with which a lower literacy patients feels more comfortable with and can relate better to information in this format [5].
Another benefit of diagrams may also be the ability to reduce the influence of anecdotal reasoning or bias in the way information is presented in text format or the way it is verbally presented. This has been the finding in somewhat recent research in health care decision making. Presenting information using pictographs can reduce the undue influence of anecdotal reasoning on treatment choices [8]. Therefore, perhaps simple pictures may also extend to improving the patient’s understanding of a procedure and post-procedure intructions as well as potential treatment choices.
There were some limitations to our study. While patients with a wide range of ages participated, the study population was relatively homogeneous in terms of race (given the local demographics), and no patients required the assistance of interpreters. Therefore, the patient participants may not be representative of the types of patients other institutions may serve. The study was also limited to spine injections; hence the results may not be generalizable to other imaging guided procedures.
A potential limitation of the diagram method is that some patients may have poor eyesight and not wear their glasses to the procedure. This would diminish the effectiveness of diagrams in reinforcing the information given to the patient.
A limitation in the method of measuring communication was that it tested recognition, which may not best simulate how the patient would utilize the recently learned information in real life situations. However, a patient certainly needs to have information retention (recognition or recall) in order to use that information in a real life situation, which may not be the case if a suboptimal educational method is used.
Another potential limitation is performance bias. The radiologists involved could deduce that informed consent was being evaluated. We enrolled all of the radiologists that routinely perform imaging-guided spine injections at our institution (eight radiologists). Certainly some of the radiologists would favor the new methods; however, some of the radiologists were also resistant to change. With the enrolled patients being spread over eight radiologists (with differing views on the best method of informed consent) and with each of the eight radiologists seeing patients enrolled in each group, it was felt that this would help lower the effect of any performance bias. Detection bias was avoided by grading the surveys without knowledge of the assigned patient group.
Additionally, one flaw in grading the survey was found after commencement of the study and a subgroup of surveys needed rescoring retrospectively. However, this adjustment was done prior to analysis of the data and without knowledge of the assigned group.
In summary, this study evaluated different methods for enhancing patient-physician communication of informed consent and post-procedure home care instructions for spinal injection procedures. The measured improvement in the survey scores using the teach-the-teacher and diagram methods suggests that physicians may be able to better educate patients using these methods, and it has been reported that better patient education leads to fewer medical errors [3]. Therefore, the use of one of these alternative methods would be recommended over a conversational discussion of key procedural points with a printed informed consent informational document. The use of a combination of the two alternative methods was not investigated; however, this may be helpful in catering to different learning styles for the patient and could be an area of potential future study.
In conclusion, the diagram method was the most successful in this study. The diagram method required less time than the teach-the-teacher method, had no negative correlation with age, and had improved survey scores over the control group. Based on the results of this study and in comparison to the studies mentioned above, incorporating humorous simple diagrams into the informed consent process and take-home instructions process is a relatively easy way to improve patient-physician communication without increasing the time required for the communication of this important information (such as occurs with the teach-the-teacher method).
Acknowledgments
This research was supported in part by a NIH/Carver College of Medicine Educational Grant for training medical students in research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
D Lee Bennett, University of Iowa Roy J and Lucille A Carver College of Medicine Dept of Radiology 200 Hawkins Dr Iowa City, IA 52242-1077.
Chiraag V Dharia, University of Iowa Roy J and Lucille A Carver College of Medicine Student Affairs 100 College of Medicine Administration Building Iowa City, IA 52242-2600.
Kristi J Ferguson, University of Iowa Roy J and Lucille A Carver College of Medicine Office of Consultation and Research in Medical Education 1204 Medical Education Building Iowa City, IA 52242-1000.
Anietie E Okon, University of Iowa Roy J and Lucille A Carver College of Medicine Dept of Radiology 200 Hawkins Dr Iowa City, IA 52242-1077.
References
- 1.Hopper KD, TenHave TR, Hartzel J. Informed consent forms for clinical and research imaging procedures: how much do patients understand? AJR Am J Roentgenol. 1995;164:493–96. doi: 10.2214/ajr.164.2.7839996. [DOI] [PubMed] [Google Scholar]
- 2.Kutner M, Greenberg E, Jin Y, Paulsen C. Executive summary. The health literacy of America’s adults: results from the 2003 national assessment of adult literacy (NCES 2006-483) In: Kutner M, Greenberg E, Jin Y, Paulsen C, editors. US Department of Education. Washington, DC: National Center for Education Statistics; 2006. pp. iii–v. [Google Scholar]
- 3.Committee on Quality of Health Care in America, Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: The National Academies Press; 2001. Executive summary; pp. 1–22. [Google Scholar]
- 4.White CS, Mason AC, Feehan M, Templeton PA. Informed consent for percutaneous lung biopsy: comparison of two consent protocols based on patient recall after the procedure. AJR Am J Roentgenol. 1995;165:1139–1142. doi: 10.2214/ajr.165.5.7572491. [DOI] [PubMed] [Google Scholar]
- 5.Delp C, Jones J. Communicating information to patients: the use of cartoon illustrations to improve comprehension of instructions. Acad Emerg Med. 1996;3:264–270. doi: 10.1111/j.1553-2712.1996.tb03431.x. [DOI] [PubMed] [Google Scholar]
- 6.Muijtjens AM, van Mameren H, Hoogenboom RJ, Evers JL, van der Vleuten CO. The effect of a ‘don’t know’ option on test scores: number-right and formula scoring compared. Med Educ. 1999;33:267–275. doi: 10.1046/j.1365-2923.1999.00292.x. [DOI] [PubMed] [Google Scholar]
- 7.Ziv A. Teaching and learning with humor: experiment and replication. Journal of Experimental Education. 1988;57:5–15. [Google Scholar]
- 8.Fagerlin A, Wang C, Ubel PA. Reducing the influence of anecdotal reasoning on people’s health care decisions: is a picture worth a thousand statistics? Med Decis Making. 2005;25:398–405. doi: 10.1177/0272989X05278931. [DOI] [PubMed] [Google Scholar]