Abstract
Objective
To examine whether delays in seeking care are associated with worse health outcomes or increased treatment costs in children, and then assess if insurance coverage reduces these delays.
Study design
We use data on 4070 children under 5 years from the Quality Improvement Demonstration Study (QIDS), a randomized controlled experiment assessing the effects of increasing insurance coverage. We examined if delay in care, defined as greater than two days between the onset of symptoms and admission to the study district hospitals, is associated with wasting or having positive C-Reactive Protein (CRP) levels upon discharge, and with total charge for hospital admission, and, evaluated whether increased benefit coverage and enrollment, reduced the likelihood of delay.
Results
Delay is associated with 4.2 and 11.2 percentage point increase in the likelihood of wasting (p=0.08) and having positive CRP levels (p=0.03), respectively, at discharge. On average hospitalization costs were 1.9% higher with delay (p=0.04). Insurance intervention results in 5 additional children in 100 to not delay going to the hospital (p =0.02).
Conclusions
In this population, delayed care is associated with worse health outcomes and higher costs. Access to insurance reduced delays, thus, insurance interventions may have positive effects on health outcomes.
Keywords: Insurance, child health, health policy, delay in care, health care utilization, health care costs, child health outcomes
Many studies conducted in developed countries have found that the uninsured have poorer access to health care services.1-3 Children, in particular, are vulnerable.4-6 If poor access is due to a delay in seeking care and starting treatment, children may not be able to recover or even survive.7 Thus, insurance expansions targeted at children have been advocated and implemented where coverage of children is limited, for example in the United States8. Initial evaluations in wealthier countries show that insurance programs have been able to improve access by reducing delays in health seeking for newly insured children.9-13 Initial evaluations show that these insurance expansions lead to better subjective health outcomes12, 14 and lowered costs.6 Reductions in delays can improve outcomes as children are brought to health facilities at less severe illness stages. These can partially mitigate the effects of other non-financial barriers to care, such as lack of education.
The finding that insurance reduces delays and improves health outcomes is especially important for low income countries where child health status is worse and relative out-of-pocket payments for care are high.15 The supposition is that delays in care contribute to worse health outcomes and higher costs. A related question is whether insurance coverage mitigates against these delays, and if children seek care earlier when out-of-pocket payments are reduced through insurance. If we can show the same results in a middle income country setting, then this suggests insurance can be a potent instrument with which to improve access and improve health outcomes.
The presence of a unique randomized experiment in the Philippines provided us with an opportunity to replicate these results in a developing country setting where the financial burden of care is high. Using the child patient exit data from the Quality Improvement Demonstration Study (QIDS), a large randomized controlled experiment assessing the effects of increasing insurance coverage, we perform three analyses in this paper: (1) examine whether children who delay have a worsening of their health status, (2) estimate the impact of delays in health seeking on costs of treatment, and (3) assess whether the QIDS Access Intervention reduces delays.
Methods
The children analyzed in this paper were part of the Philippine Child Health Insurance and Policy Experiment known locally as QIDS, a five year randomized controlled experiment that seeks to assess ongoing national health sector reforms, particularly the impacts of insurance interventions and quality of care bonuses on health outcomes of children under 5 years of age.16 The study has been implemented in 30 districts, each with a corresponding district hospital, throughout 11 provinces in the Visayas islands of the Philippines. As part of the experiment, hospitals were matched into blocks and randomly assigned to (1) Access Intervention, which expands access to care by increasing the insurance benefit package for children under 5 years old and increasing enrolment of households into the insurance program, and (2) Control, in which no interventions were introduced. Baseline, or pre-intervention, assessments were conducted in 2003-2004 and post-intervention in 2006 in all sites, allowing a difference-in-difference analysis of Interventions and Controls. QIDS was conducted and approved in accordance with Human Subject Review standards and institutional review boards of the University of the Philippines and the University of California, San Francisco. We examine here the impact of the Access Intervention on delays compared with the controls. (A full description of the study and sampling frame can be found in our previous publication. 16)
Data came from exit surveys obtained at the sample district hospitals starting in 2003 for the baseline round, and from the post-intervention round in 2006. At the time of discharge, children were sequentially identified at the facility following an acute illness. Exit surveys obtained information on services provided, health facility utilization, and total expenses incurred related to the episode of illness. Household socio-economic information was also collected as part of the instrument. Licensed medical technologists were trained to conduct the interviews and collect anthropometric measurements and blood samples. We obtained written consent from the parents and guardians before information was collected from patient charts and face-to-face interviews, and before blood samples were collected.
To be eligible for the study a child had to be aged 6 months to 5 years and 11 months from families residing in the geographic catchment of the facility. A total of 4070 children, 1997 from the baseline and 2073 sample patients from the post intervention round, were surveyed in the 20 control and Access sites. Overall, 2027 sampled patients were from the Access sites, of which 985 were from those surveyed at baseline and 1042 were sampled post intervention.
In determining the impact of delays on health outcomes and total hospital charges we used data from the baseline sample to establish the no intervention scenario. This avoids problems brought about by the possible correlation of elapsed time before admission and interventions in the second round sample (which increases the estimates of standard errors).
We defined delay as the total number of days between the onset of symptoms and admission to the district hospital. Total cost is defined as the actual charges associated with a confinement. Drug charges in particular can be incurred outside of the hospital in the Philippines. Costs thus included total hospital charges, physician charges and out of pocket charges.
For our health outcome variables, we used both biologic and anthropometric assays to measure health status. Blood samples were collected at the point of discharge to measure whether a child had an elevated C reactive protein (CRP). CRP is an acute inflammatory marker that reliably indicates infection or other types of inflammation, as a general marker or indicator of response to treatment (not as a patient-specific test for disease or clinical care). We used established clinical procedures with established quality control methods for obtaining venous samples for the laboratory testing. CRP levels were tested using a rapid latex agglutination test manufactured by Teco Diagnostics (http://www.tecodiag.com/). Wasting, our anthropometric measures, is commonly used to indicate, illness, or poor nutritional status. Wasting was also constructed as a binary variable and was defined as whether the child had a ratio of weight to age below the normal range standardized for age and sex. 20
Data analysis
We developed a logit model to determine if health outcomes worsened when delays increased, controlling for other factors that may affect these outcomes such as any utilization or treatment obtained at another facility before the confinement, the age and sex of the child, the diagnoses (pneumonia or diarrhea), length of stay and prior hospitalization for the same illness condition as indicators of illness severity. Services and treatment intensity was modeled by the use of oral medications, the number of oral medications taken, whether intravenous drugs were administered to the patient, whether the child was visited by a specialist and whether the child had any laboratory tests done in the facility.
We used ordinary least squares to determine if delays in care resulted in higher costs. In addition to the same control variables used on the health outcomes model, we included whether a child was a PhilHealth beneficiary to control for possible mark-ups imposed on insured patients. Father's education and type of room accommodation were also introduced to control for other potential sources of price mark-ups or discounts.
We estimated the likelihood that a delay, defined as more than two days before admission, would be less likely if the child were in the insurance intervention group in the logit model. We used our before and after data and compared control versus intervention groups in a difference in difference estimation to evaluate our hypothesis that insurance decreased utilization barriers imposed by resource constraints. We included the diagnoses variables to control for differences in symptoms that influence the likelihood to delay across illnesses, and treatment sought at another facility to partially control for physician decisions to admit patients. To compute for the differences in predicted probabilities of delay, we utilized the sample means for the control variables and imputed a value of one for the intervention variable. We used Stata 10 to estimate the three models and perform tests of significance for our variables (Copyright 1984-2007, StataCorp, College Station, Texas, USA).
Results
The age of our sampled children ranged from 5 to 59 months with an average of 23.1 months and their parents had finished about 8 years of education, with some parents reporting no schooling at all. Nearly two-thirds of children were diagnosed with either pneumonia or diarrhea. Slightly more than one in four children were initially brought to another facility before admission to the hospital and, for around half of our sample, this hospitalization episode was not the first time that they were admitted for the same condition.
Close to 26% of the children took more than 2 days before seeking care. The average out-of-pocket cost was US$ 32.77 per child (using the 2003 average exchange rate of PhP 54.203 to US$ 1), with a maximum reported of US$ 436.14. In the baseline sample, we observed that about 35% of the sampled children were wasted and around 27% had a positive CRP at the time they were discharged (Table I).
Table 1.
Descriptive Statistics, Baseline Sample (N=1997)
| Variable | Mean | SD |
|---|---|---|
| Delay of more than two days | 0.27 | 0.44 |
| Child was wasted upon discharge | 0.35 | 0.48 |
| CRP positive upon discharge | 0.27 | 0.45 |
| Total charges inside and outside the facility (PhP) | 1776.44 | 1447.45 |
| Male child | 0.56 | 0.50 |
| Age in months | 23.10 | 14.07 |
| Child has Pneumonia | 0.26 | 0.44 |
| Child has Diarrhea | 0.28 | 0.45 |
| Length of stay | 3.35 | 1.85 |
| Delay of more than 2 days*Length of stay | 1.01 | 2.07 |
| Number of oral medicines | 2.16 | 2.01 |
| Child used IV meds in the facility | 0.69 | 0.46 |
| Child was visited by a specialist | 0.09 | 0.29 |
| Child received oral medicines in the facility | 0.44 | 0.50 |
| Child underwent laboratory tests in facility | 0.90 | 0.30 |
| Child was hospitalized before for same condition | 0.46 | 0.50 |
| Child was initially brought to another facility | 0.27 | 0.44 |
| Initial treatment prior to hospitalization | 0.21 | 0.41 |
| Years of mother's education | 8.86 | 3.36 |
| Years of father's education | 8.41 | 3.66 |
| PhilHealth beneficiary | 0.32 | 0.47 |
| Child stayed in charity ward | 0.35 | 0.48 |
| Household belongs to lowest income quintile | 0.21 | 0.41 |
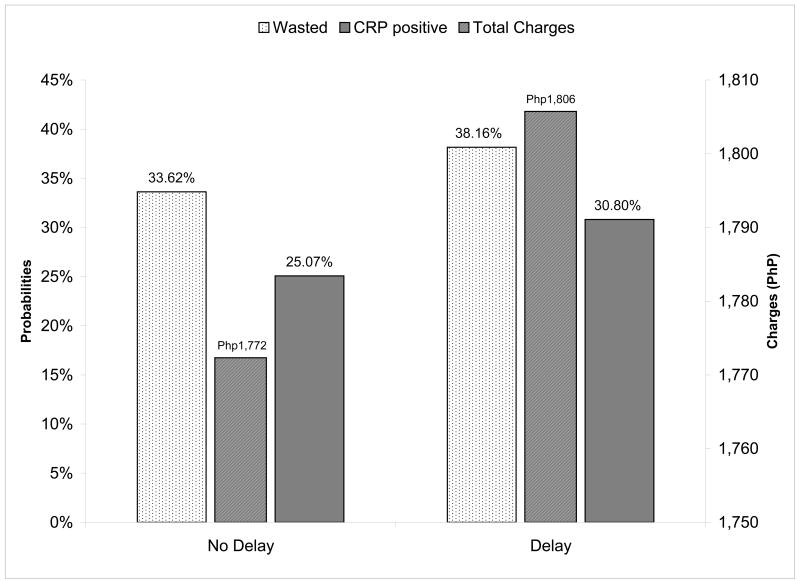
When more than two days elapsed between the onset of symptoms and the hospital admission, we found that a child was 11.2 % more likely to be CRP positive and thus more likely to have worse health status at the time of discharge relative to a child who was promptly admitted (p=0.03). Diarrhea decreased the likelihood of being CRP positive, and those who required specialist visits, an indicator of illness severity, were more likely to be CRP positive (Table II; available at www.jpeds.com). Similarly, there was a 4.6% increase in the likelihood that a child would be wasted if their admission was delayed than if it were not (p=0.08). Wasting was also associated with longer lengths of stay with either diarrhea (p<0.001) or pneumonia (p=.04) compared with children with other illness. In summary, if the delay is minimized to less than two days for an ‘average’ child, the predicted probability of having a positive CRP levels at discharge is reduced by at least 5.7 percentage points, and the predicted probability of wasting is reduced by about 4.5 percentage points (Figure 1).
Table 2.
Regression Models Estimating Effect of Delay on Health Outcomes
| Variables | CRP Positive | Wasted | ||
|---|---|---|---|---|
| Logit, N=1945 | Logit, N=1872 | |||
| Marginal effects | P>z | Marginal effects | P>z | |
| Delay of more than two days | 0.112 | 0.032 | 0.046 | 0.078 |
| Length of stay | 0.006 | 0.378 | 0.020 | 0.002 |
| Delay of more than two days*Length of stay | -0.016 | 0.149 | ||
| Age in months | 0.004 | 0.183 | 0.001 | 0.436 |
| Age in months squared | 0.000 | 0.296 | ||
| Child is male | -0.025 | 0.203 | -0.029 | 0.189 |
| Chils has Pneumonia | -0.001 | 0.971 | 0.058 | 0.045 |
| Child has Diarrhea | -0.081 | 0.000 | 0.110 | 0.000 |
| Child received oral meds in the facility | 0.102 | 0.000 | ||
| Child received IV Meds in the Facility | 0.011 | 0.642 | -0.002 | 0.926 |
| Child was initially brought to another facility | 0.000 | 0.986 | ||
| Child was visited by a specialist | 0.170 | 0.000 | ||
| Child underwent laboratory tests in the facility | 0.075 | 0.013 | ||
| Number of oral meds | -0.004 | 0.486 | ||
| Child was hospitalized before for same condition | 0.004 | 0.866 | ||
| Child received initial treatment prior to hospitalization | -0.036 | 0.179 | ||
Figure 1.
Predictions: Total Charges and Probabilities of CRP and Wasting, Delay vs. No Delay
We estimated the incremental effect of the delays on total charges to be about PhP 270 or US$ 4.98. This is the equivalent of 5 times the daily poverty threshold utilized by the World Bank (p=0.04) (Table III; available at www.jpeds.com). As expected, the increased costs were also associated with length of stay, insurance status, father's education, IV medication and specialist visit use and whether this was pneumonia. However, the interaction of delay and length of stay indicates that the cost reduction with early care seeking diminishes as the patient is more severely ill. Thus, for an average length of stay, the net effect of more than two days delay in admission was to increase costs by about 1.9 % of mean total charges (Figure 2).
Table 3.
Regression Model Estimating Effect of Delay on Total Charges
| Variables | Total Charges | |
|---|---|---|
| OLS, N=1841 | ||
| Coefficient | P>t | |
| Delay of more than two days | 270.325 | 0.037 |
| Length of stay | 386.694 | 0.000 |
| Delay of more than two days*Length of stay | -70.712 | 0.025 |
| Child has Pneumonia | 191.429 | 0.006 |
| Child has Diarrhea | -228.701 | 0.001 |
| Child received oral meds in the facility | -215.781 | 0.001 |
| Child received IV Meds in the Facility | 191.963 | 0.005 |
| Child was visited by a specialist | 225.025 | 0.022 |
| Child stayed in charity ward | -382.542 | 0.000 |
| Years of father's education | 22.181 | 0.004 |
| PhilHealth beneficiary | 665.100 | 0.000 |
| Constant | 164.715 | 0.153 |
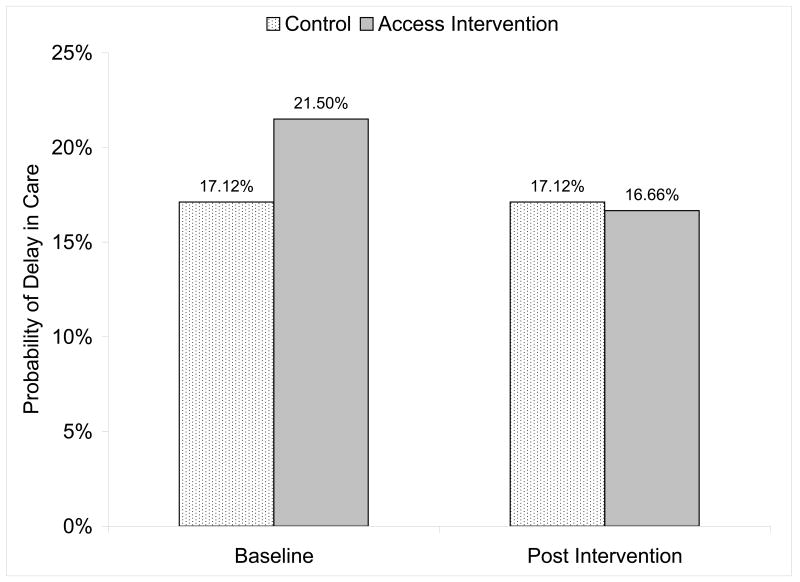
Figure 2.
Predicted probabilities of delay, differences across intervention sites
When we examined whether insurance mitigated against delays in seeking care, we found that higher insurance coverage reduced the delays in health seeking. Delays were 5.29% lower in the intervention sites after the experimental introduction of the Access intervention compared with the control sites (p=0.02), controlling for secular trends and differences across the sites at baseline. Thus, if a child was insured there were at least 5 fewer children in 100 with more than two days elapsing before hospital admission (Table IV).
Table 4.
Regression Model Estimating Effect of the Access Intervention on Delay
| Delay of more than two days | ||
|---|---|---|
| Logit, N=3963 | ||
| Marginal Effects | P>z | |
| Difference in Difference | -0.0529 | 0.024 |
| Male Child | 0.0117 | 0.380 |
| Mother's Education | -0.0079 | 0.000 |
| Child has Pneumonia | 0.1040 | 0.000 |
| Child has Diarrhea | -0.0575 | 0.000 |
| Lowest Income Quintile | 0.0490 | 0.005 |
| Age of child in months | -0.0036 | 0.071 |
| Age of child in months squared | 0.0001 | 0.057 |
| Child initially brought to another facility | 0.0511 | 0.001 |
| Baseline Access vs Baseline Control | 0.0438 | 0.031 |
| Post-intervention Control vs Baseline Control | 0.0304 | 0.121 |
| Post-intervention Access vs Baseline Access | -0.0224 | 0.197 |
Mother's education reduced the likelihood of delay but increased by 4.9 % if the child belongs to a household in the bottom income quintile. Interestingly, children with diarrhea were more likely to be brought to the hospital without delay than those with pneumonia but if the child was brought to another facility before the hospital, this increased the likelihood of more than two days elapsing before admission by about 5.1 %.
The presence of insurance reduces the proportion with delays from about 21.5% to about 16.7% (Figure 2). This translates to about 50 less children seeking admission more than two days after the onset of symptoms.
Discussion
Using a unique longitudinal dataset from a randomized experiment, we tested whether experimentally introduced higher insurance coverage improved health outcomes and reduced costs of care. Our estimates show that a delay of more than two days before admission is associated with 4.2% higher likelihood of wasting and an 11.2% higher likelihood of positive CRP levels upon discharge. Costs of hospitalization also increase by about 1.9 % of average total costs with delay of more than two days. We find that reducing out-of-pocket payments through higher insurance coverage would result in about 5 more children in 100 going to hospitals less than three days after the onset of symptoms. The reductions were significant and could therefore translate into improved health status and reduced costs in general.
There are only a few rigorous studies that have analyzed the effects of insurance on access to and utilization of care for either adults or children, or the effects of insurance on health outcomes whether measured by specific health conditions or by more general measures of morbidity and mortality.1 Studies focused on children, however, have largely come from quasi experimental settings without a control group (i.e., special insurance programs for children,12,21 expansion of Medicare and Medicaid and other private insurance,6,13-14,22 and more recently, the implementation of various State Children's Health Insurance Programs in the United States.9-11, 23-24). The unique experimental nature of our dataset allowed us to more rigorously assess the impact of a randomized insurance intervention on a large number of children in a developing country setting where the financial burden of care is high.
Prior studies found insurance coverage improves self-reported perceived health status and reduce activity limitations in children.12,14 We differ from these studies in two aspects. Firstly, we use health status measures that are based on objective biologic and anthropometric measures that are less prone to subjective differences in health perceptions over time. Secondly, we are able to investigate specific mechanisms through which insurance affects outcomes. We find that insurance coverage affects outcomes by influencing the characteristics of utilization, in particular delay in utilization.
Studies that have assessed the cost implications of providing insurance coverage have focused on the increases brought about by moral hazard in the form of increased utilization of care.25 Other studies support the finding that insurance may reduce costs of care only by implication, i.e., that costs can be mitigated by more appropriate utilization, for instance by the utilization of ambulatory care vs. emergency department utilization,10,26 and by utilizing a usual source of care or primary care.11,14 We substantiate these findings by directly estimating differences in total charges owing to delays in utilization of hospital care and showing that insurance coverage can reduce the proportions of children with delayed hospital admission.
Our finding that insurance coverage improves access by reducing delays in health seeking is consistent with other studies that show reductions in the proportions of children that delayed care after enrolling in children's health insurance programs. These studies have reported changes in utilization at both the national9 and state levels.10-12 They also point to the importance in the continuity in insurance coverage, which in our population was accounted for by looking at access across the three year study period.13 Our findings extend these studies in that our measure of delay is associated with hospitalization, rather than ambulatory visits as is typically used. Among the advantages, we expect the impact to be higher on costs and health status and recall bias to be less because we obtained data from the parent or guardian at the point of discharge.
Controlling for diagnosis and services received by child patients, we found those who were admitted more than two days after the onset of symptoms are discharged with worse health status, which is consistent with the literature.27-29 Delays in utilization likely result in children being brought to facilities at later stages of diseases, requiring more intensive treatment. From a family perspective, a delay in utilization inflates the resource requirements related to an illness episode, as more medical interventions and household resources outside of the hospital setting are needed to restore the child to full health. This intuition is supported by our finding that reductions in the number of days from the onset of symptoms to the hospitalization reduce total charges, especially for those with shorter lengths of stay. Because the length of stay of the patient is one of our indicators for illness severity, the effects of delay on charges will be felt more on less ill patients.
Our study has some limitations. We did not have the data to link the introduction of insurance, which clearly decreased care delays, to longer term improvements in health status although we infer this from the association of delays and poor health outcomes at baseline. We also did not have anthropometric measures upon admission that would allow us to definitively rule out wasting as a pre-existing condition; however we were able to control for expected predictors of wasting: parental socioeconomic status and insurance. We cannot distinguish how much of the delay is due to delay in health seeking versus delay in recognizing serious illness by either the parent or the providers. Similarly, we are unable to determine how quality of care at intake or the route of admission impacts the delay. It is possible that some providers systematically fail to recognize whether the condition requires hospitalization, albeit this would be primarily a concern in borderline cases. We further note that due to the unavailability of some supplies and medicines in primary care facilities, some patients are referred to the district hospitals not because of their illness but because more supplies are available at the hospital than the clinic. If this were the case, this would partly explain the reductions in costs observed for reducing delays in admissions for relatively shorter lengths of stay or less severe illnesses.
Lastly, further studies would help establish causal links between delays and adverse outcomes taking into account poor nutritional status, an important co-factor in illness in developing countries. Benefits in terms of health outcomes should also be placed in relation to costs of interventional changes, which we have begun to explore in a forthcoming publication.30
Acknowledgments
This study is funded by the U.S. National Institute of Child Health and Development (NICHD) through an R01 grant (HD042117). Operational support of the interventions was provided by the Philippine Health Insurance Corporation (PHIC).
Abbreviations
- QIDS
Quality Improvement Demonstration Study
- PHIC or PhilHealth
Philippine Health Insurance Corporation
- CRP
C-reactive protein
- SCHIP
State Children's Health Insurance Programs
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Aleli D. Kraft, University of the Philippines School of Economics.
Stella A. Quimbo, University of the Philippines School of Economics.
Orville Solon, University of the Philippines School of Economics.
Riti Shimkhada, Institute for Global Health, University of California San Francisco.
Jhiedon Florentino, University of the Philippines School of Economics.
John W. Peabody, Institute for Global Health, University of California San Francisco.
References
- 1.Hadley J. Sicker and poorer: the consequences of being uninsured: a review of the research on the relationship between health insurance, medical care use, health, work and income. Medical Care Research and Review. 2003;60:3S–75S. doi: 10.1177/1077558703254101. [DOI] [PubMed] [Google Scholar]
- 2.Zuvekas SH, Mulnick RM. Changes in access to care, 1977-1996: the role of health insurance. Health Services Research. 1999;34:271–279. [PMC free article] [PubMed] [Google Scholar]
- 3.Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Services Research. 2003;38:809–827. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holl JL, Szilagyi PG, Rodewald LE, et al. Profile of uninsured children in the United States. Archives of pediatrics and adolescent medicine. 1995;149:398–406. doi: 10.1001/archpedi.1995.02170160052008. [DOI] [PubMed] [Google Scholar]
- 5.Newacheck PW, Hughes DC, Stoddard JJ. Children's access to primary care: differences by race, income, and insurance status. Pediatrics. 1996;97:26–32. [PubMed] [Google Scholar]
- 6.Todd JM, Armon C, Griggs A, Poole S, Berman S. Increased rates of morbidity, mortality, and charges for hospitalized children with public or no health insurance as compared with children with private insurance in Colorado and the United States. Pediatrics. 2006;118:577–585. doi: 10.1542/peds.2006-0162. [DOI] [PubMed] [Google Scholar]
- 7.Kallander K, Hildenwall H, Waiswa P, et al. Delayed care seeking for fatal pneumonia in children aged under five years in Uganda: a case-study series. Bulletin of the World Health Organization. 2008;86:332–338. doi: 10.2471/BLT.07.049353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenbaum S, Johnson K, Sonosky C, Markus A, DeGraw C. The children's hour: the state children's health insurance program. Health Affairs. 1998;17:75–89. doi: 10.1377/hlthaff.17.1.75. [DOI] [PubMed] [Google Scholar]
- 9.Duderstadt KG, Hughes DC, Soobader M, Newachek PV. The impact of public insurance expansions on children's access and use of care. Pediatrics. 2006;118:1676–1682. doi: 10.1542/peds.2006-0004. [DOI] [PubMed] [Google Scholar]
- 10.Lave JR, Keane CR, Lin CJ, Ricci E, Amersbach G, LaVallee C. Impact of a children's health insurance program on newly enrolled children. JAMA. 1998;279:1820–1825. doi: 10.1001/jama.279.22.1820. [DOI] [PubMed] [Google Scholar]
- 11.Szilagyi PG, Dick AW, Klein JD, Shone LP, Zwanziger J, McInerny T. Improved access and quality of care after enrolment in the New York State Children's Health Insurance Program (SCHIP) Pediatrics. 2004;113:e395–e404. doi: 10.1542/peds.113.5.e395. [DOI] [PubMed] [Google Scholar]
- 12.Howell E, Trenholm C. The effect of new insurance coverage on the health status of low-income children in Santa Clara County. Health Services Research. 2006;42:867–889. doi: 10.1111/j.1475-6773.2006.00625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olson LM, Tang SS, Newacheck P. Children in the United States with discontinuous health insurance coverage. New England Journal of Medicine. 2005;353:382–391. doi: 10.1056/NEJMsa043878. [DOI] [PubMed] [Google Scholar]
- 14.Stevens GD, Seid M, Halfon N. Enrolling vulnerable, uninsured but eligible children in public health insurance: association with health status and primary care access. Pediatrics. 2006;117:751–759. doi: 10.1542/peds.2005-1558. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. The World Health Report 2003: Shaping the Future. Geneva: World Health Organization; 2003. [Google Scholar]
- 16.Shimkhada R, Peabody JW, Quimbo SA, Solon O. The Quality Improvement Demonstration Study: An example of evidence-based policy-making in practice. Health Research Policy and Systems. 2008;6:5. doi: 10.1186/1478-4505-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jaye DL, Waites KB. Clinical applications of C-reactive protein in pediatrics. Pediatr Infect Dis J. 1997;16:735–46. doi: 10.1097/00006454-199708000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Smith RP, Lipworth BJ, Cree IA, Spiers EM, Winter JH. C-reactive protein: a clinical marker in community acquired pneumonia. Chest. 1995;108:1288–1291. doi: 10.1378/chest.108.5.1288. [DOI] [PubMed] [Google Scholar]
- 19.Clyne B, Olshaker JS. The C-reactive protein. J Emerg Med. 1999 Nov-Dec;17:1019–25. doi: 10.1016/s0736-4679(99)00135-3. [DOI] [PubMed] [Google Scholar]
- 20.Lohman T, Roche AF, Martorell R. Anthropometric Standardization Reference Manual. Champaign, IL: Human Kinetics Books; 1988. [Google Scholar]
- 21.Feinberg E, Swartz K, Zaslavsky A, Gardner J, Klein D. Family income and the impact of a children's health insurance program on reported need for health services and unmet health need. Pediatrics. 2002;109:e29. doi: 10.1542/peds.109.2.e29. [DOI] [PubMed] [Google Scholar]
- 22.Currie J, Gruber J. Health insurance eligibility, utilization of medical care, and child health. Quarterly Journal of Economics. 1996;111:431–455. [Google Scholar]
- 23.Keane CR, Lave JR, Ricci EM, Lavallee CP. The impact of a children's health insurance program by age. Pediatrics. 1999;104:1051–1058. doi: 10.1542/peds.104.5.1051. [DOI] [PubMed] [Google Scholar]
- 24.Kempe A, Beaty BL, Crane LA, Stokstad J, Barrow J, Belman S, Steiner JF. Changes in access, utilization and quality of care after enrollment into a state child health insurance plan. Pediatrics. 2005;115:364–371. doi: 10.1542/peds.2004-0475. [DOI] [PubMed] [Google Scholar]
- 25.Zwanziger J, Mukamel D, Szilagyi PG, et al. Evaluating child health plus in upstate New York: how much does providing health insurance to uninsured children increase health care costs. Pediatrics. 2000;105:728–732. [PubMed] [Google Scholar]
- 26.Lao X, Lui G, Frush K, Hey L. Children's health insurance status and emergency department utilization in the United States. Pediatrics. 2003;112:314–319. doi: 10.1542/peds.112.2.314. [DOI] [PubMed] [Google Scholar]
- 27.Berhman J. The impact of health and nutrition on education. World Bank Research Observer. 1996;11:23–37. [Google Scholar]
- 28.Grantham-McGregor S. A review of studies of the effect of severe malnutrition on mental development. Journal of Nutrition. 1995;125:2233S–2238S. doi: 10.1093/jn/125.suppl_8.2233S. [DOI] [PubMed] [Google Scholar]
- 29.Martorell R. The nature of child malnutrition and its long-term implications. Food and Nutrition Bulletin. 1999;20:288–292. [Google Scholar]
- 30.Solon O, Peabody JW, Woo K, Quimbo SA, Florentino J, Shimkhada R. A cost-effective approach to improving access to care using policy navigators. Health Policy. 2008 doi: 10.1016/j.healthpol.2008.10.010. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]