Abstract
Objective
This aim of this study was to examine the influence of grandparental (G1) and parental (G2) major depressive disorder (MDD) and other forms of psychopathology on behavior problems in very young offspring (G3).
Method
Oregon Adolescent Depression Project (OADP) participants who had children over a 3-year period were invited to participate in a study of infant and child development. We attempted to collect diagnostic history from the original OADP (G2) participants, their coparents, the parents of the original OADP participants (G1), and the parents of the coparents. Child (G3) outcomes at 24 months of age were based on parent reports of behavior problems.
Results
Univariate correlations indicated that G1 and G2 familial loadings for MDD were associated with higher levels of G3 internalizing and externalizing behavior problems. Multiple regression analyses revealed a significant interaction between G1 and G2 MDD on G3 internalizing (but not externalizing) behavior problems. A higher familial loading for MDD in either the parental or grandparental generation was associated with elevated grandchild internalizing problems, but higher loadings for MDD in both generations did not convey additional risk.
Conclusions
Parental MDD and grandparental MDD are both associated with elevated levels of internalizing problems in young grandchildren, but MDD in both the G1 and G2 generations does not confer additional risk. One important implication is that MDD in the grandparental generation is associated with increased risk to grandchildren even in the absence of parental MDD. Future studies should examine the mechanisms through which grandparental psychopathology influences behavior problems in grandchildren.
Keywords: internalizing behavior problems, familial transmission, preschool, mood disorder
Intergenerational transmission of major depressive disorder (MDD) is well documented.1,2 Many of the studies in the literature have focused on the transmission of MDD across two generations.3–5 However, investigators have recently expanded this work to three generations. Although there are a number of three-generation studies of the familial transmission of externalizing disorders,6–8 we are aware of only two published9,10 studies of depressive disorders that examine three generations within the same families.
Weissman and colleagues10,11 prospectively followed the offspring (parents [G2]) of patients with MDD and individuals with no history of mood disorders (grandparents [G1]). Diagnostic information was collected on both the G1 parent probands and G1 coparents. Subsequently, these investigators assessed G3 (child) offspring older than the age of 5 years of the G2 parents. Weissman et al.10 reported a significant interaction between grandparental (G1) MDD and parental (G2) MDD on both anxiety disorders and psychopathology in general in the grandchildren (G3). This interaction suggested that grandchildren with a family history of MDD in both the parental and grandparental generations were at greatest risk of psychopathology. There was also a heightened risk of psychopathology in grandchildren if there was a history of MDD in the grandparents, but not in the parents. However, in the absence of grandparental MDD, the risk of psychopathology in grandchildren did not differ as a function of whether their parents had MDD. Thus, although the combination of grandparental and parental MDD was associated with the highest rates of psychopathology in grandchildren, grandparental MDD had a greater effect than parental MDD on psychopathology in the third generation.
Hammen et al.9 examined the transmission of MDD in a large community sample. They focused on the influence of MDD in maternal grandmothers (G1) and mothers (G2) on MDD in adolescent grandchildren (G3). In bivariate analyses, the authors found that G1 MDD and G2 MDD were both associated with MDD in grandchildren (G3). However, the effect of maternal grandmother MDD on granddaughter MDD was mediated by maternal MDD; that is, no direct association remained between G1 MDD and G3 MDD when G2 MDD was taken into account.
These pioneering studies have begun to elucidate the patterns of intergenerational transmission of internalizing disorders across three generations. These studies have two important limitations: First, neither study assessed psychopathology in complete G1 and G2 pedigrees. Weissman et al.10 did not have access to data on psychopathology for half of the pedigree in the G1 generation (the parents of the G2 spouses). Hammen et al.9 did not include data on psychopathology in fathers, maternal grandfathers, and either paternal grandparent. The absence of data on portions of pedigrees is important because it may lead to misclassifying some families as being free of MDD in the G1 and/or G2 generations when, in fact, MDD may be present in members of the nonassessed part of the pedigree.
Second, previous studies have not examined the effects of nonmood disorders in parents and grandparents on grandchildren (although an earlier, preliminary report by Warner and colleagues11 included G1 and G2 anxiety and substance use disorders). Hence, it is unclear whether the associations between parental and grandparental psychopathology and grandchild outcomes are specific to MDD or whether they reflect the effects of G1 and G2 psychopathology in general.
In addition, in both the Weissman et al.10 and Hammen et al.9 studies, most of the G3 grandchildren were older children or adolescents. Connell and Goodman12 found that associations between parental depression and child behavior problems were stronger when children were younger. Hence, it is also important to examine the effects of parental and grandparental psychopathology on younger children who may have greater exposure to G2 and G3 family members.
This article presents data from the Infant Development Study (IDS) of the Oregon Adolescent Depression Project (OADP),13 in which a subsample of the G2 probands and families in the larger OADP were selected for more intensive assessments. The first aim of this report is to examine the relationships between grandparental (G1) and parental (G2) psychopathology and internalizing and externalizing behavior problems in grandchildren (G3). The grandchildren were assessed at 24 months of age. This is an important developmental period to investigate given evidence that the precursors, and sometimes full syndromal cases, of internalizing psychopathology can be observed in toddlers and preschoolers.14–16 Moreover, two generation studies have reported differences in developmentally important behaviors between offspring of depressed and non-depressed parents using children of similar17,18 and younger ages.19 The second aim is examine whether the effects of G1 and G2 psychopathology is specific to MDD or whether G1 and G2 anxiety or substance use disorders are also associated with G3 behavior problems.
METHOD
The initial pool of participants was randomly selected from nine high schools and participated in three assessments (T1–T3) from 1987 to 1999 as part of the OADP. Detailed descriptions of recruitment, sampling, and participation rates at each assessment have been documented elsewhere.13
Around the time of the T3 assessment, when original participants were approximately 24 years of age, OADP participants who had a newborn infant, became pregnant, or whose partner became pregnant over a 3-year recruitment period, lived in Oregon, and wished to participate were recruited into the IDS. The participation rate for eligible families was 83%. Those who chose to participate in the IDS were less likely to have obtained a bachelor’s degree or higher when compared to the full sample of OADP T3 participants (17% versus 33%; χ2 [1, n = 930] = 12.8; p < .001). Differences in IDS participation as a function of other demographic variables at T3 were nonsignificant. Assessments were conducted when the children were 3, 6, 12, and 24 months old. At the first assessment, a total of 166 mothers, 152 fathers, and 166 infants participated. There were roughly equal numbers of male and female G3 offspring (48% male). The G2 mothers were mainly white (87.5%), the average age was 28.04 years (SD 2.43), and 41.0% had received at least a 2-year college degree. The G2 fathers were mainly white (88.6%), the average age was 29.7 years (3.2), and 36.4% had received at least a 2-year college degree. Attrition across the four assessment periods was minimal: 162 (97.6%) mothers, 147 (96.7%) fathers, and 162 (97.6%) children participated in the fourth assessment.
Assessment of Psychopathology
Diagnostic Interviews
The Structured Clinical Interview for DSM-IV Disorders–Non-Patient Edition20 was used to assess psychopathology in the G1 and G2 participants. Interviews were conducted by telephone, which generally yield results comparable to those of face-to-face interviews.21,22 Diagnostic interviewers generally had master’s degrees in a mental health field and received extensive training, as described elsewhere.13 Based on a randomly selected subsample (25%), interrater reliability was moderate to excellent: MDD (κ = .71), anxiety disorders (κ = .69), alcohol abuse/dependence (κ = .86), and drug abuse/dependence (κ = .85).
To ensure that some diagnostic data were available even for relatives who were not personally interviewed and to supplement the direct interviews, family history data on all first-degree relatives were collected from all of the G2 probands and spouses and at least one first-degree relative from each family. Because the sensitivity of the family history method varies as a function of the number of informants,23 we conducted additional family history interviews with all of the available family members regarding relatives who could not be directly interviewed.
Family history data were collected using a modified version of the Family Informant Schedule and Criteria.24 Best estimate DSM-IV diagnoses25 were derived for all relatives using all available data by the two senior diagnosticians (P.M.L. and D.N.K.). Data were collected on 162 mothers (99 probands and 63 spouses of the proband), 148 fathers (63 probands and 85 spouses of the proband), 152 mothers of probands, 152 fathers of probands, 127 mothers of spouses of probands, and 123 fathers of spouses of probands. Direct interviews were conducted with 67.5% of the mothers of the proband, 41.0% of the fathers of the proband, 67.5% of the mothers of the proband’s spouse, and 27.7% of the fathers of the proband’s spouse.
G3 Behavior Problems
G2 mothers and fathers completed the Child Behavior Checklist (CBCL) 2/326 when their G3 offspring were 24 months old. The CBCL 2/3 consists of 99 items that are rated on a 3-point scale (not true, somewhat or sometimes true, or very true or often true) that are used to score six narrow-band problem scales and two broadband scales, Internalizing Problems and Externalizing Problems. CBCL T scores are based on an extensive normative sample and substantial support exists for their reliability and validity.27 For the present study, we examined dimensional T scores averaged across mothers and fathers on the two broadband scales. This was done to increase reliability by aggregating data from multiple informants. Data were available for 162 G3 children; 128 (77.8%) of the children had both maternal and paternal reports.
Concurrent G2 Depressive Symptomatology
As parents’ mood state has been found to influence ratings of their children,28 we controlled for the influence of concurrent depressive symptomatology on parents’ ratings of child behavior problems. G2 probands and spouses completed the Center for Epidemiological Studies Depression Scale (CESD)29 in the same session as the CBCL 2/3. The CESD is a 20-item measure that has been widely used in epidemiological studies and demonstrates high levels of internal consistency and test-retest stability.28
Data Analysis
We computed familial loading in the grandparental (G1) and parental (G2) generations as the percentage of participants in each generation with a lifetime history of each disorder. We did not use age corrections because the ranges of ages of both G1 and G2 participants were fairly narrow owing to the fact that all of the G2 probands entered the study as high school students. To examine the associations between grandparental and parental psychopathology and grandchildren’s behavior problems, we conducted a series of four multiple regression models separately for grandchildren’s internalizing and externalizing behavior problems. The first model included grandchild sex and grandparental and parental MDD, the second model added grandparental and parental anxiety and substance use disorders, the third model added concurrent parental depressive symptoms, and the fourth model added the interaction between grandparental and parental MDD. Concurrent parental depressive symptoms were computed as the average of maternal and paternal CESD scores to be consistent with the averaging of the ratings of parents’ reports of child behavior problems.
Analyses were also conducted using multilevel regression models. In these models, maternal and paternal reports of child behavior problems both served as level 1–dependent variables. Maternal and paternal depressive symptomatology were both level 1 predictor variables, and all of the G1 and G2 diagnostic variables were entered as level 2 predictors. Results of the multilevel and traditional regression analyses were substantively identical. Hence, in the interest of simplicity, we present the results of the traditional regression models.
RESULTS
Descriptive statistics and intercorrelations between G3 behavior problems and G1 and G2 psychopathology are displayed in Table 1.
TABLE 1.
Descriptive Statistics for and Correlations Between Predictors and CBCL Scores
| Internalizing | Externalizing | Mean (SD) or 5 | |
|---|---|---|---|
| G3 | |||
| Internalizing | 41.70 (7.07) | ||
| Externalizing | 0.73*** | 45.24 (6.91) | |
| Male sex | 0.08 | 0.22** | 48.8% |
| G2 | |||
| MDD | 0.26** | 0.22** | 0.26 (0.34) |
| Anxiety | 0.11 | 0.21** | 0.16 (0.28) |
| SUD | 0.09 | 0.01 | 0.40 (0.39) |
| G1 | |||
| MDD | 0.22** | 0.18* | 0.30 (0.29) |
| Anxiety | 0.14 | −0.09 | 0.13 (0.20) |
| SUD | 0.04 | −0.09 | 0.32 (0.27) |
Note: CBCL = Child Behavior Checklist; G3 = grandchildren; G2 = parental generation; G1 = grandparental generation; Internalizing = CBCL Internalizing Behavior Problem T score; Externalizing = CBCL Externalizing Behavior Problem T score; MDD = familial loading for major depressive disorder; anxiety = familial loading for anxiety disorder; SUD = familial loading for substance use disorder. Means for G2 and G1 psychopathology refer to the mean proportion of individuals, within G1 and G2, respectively, with the disorder.
p < .05;
p < .01;
p < .001.
Grandchildren’s Internalizing Behavior Problems
In the first multiple regression model, grandparental MDD and parental MDD were each associated with grand children’s internalizing behavior problems (Table 2). When grandparental and parental anxiety and substance use disorders were included in the second model, grandparental and parental MDD remained significantly associated with grandchildren’s internalizing problems; however, no other associations between G1 and G2 psychopathology and G3 internalizing behavior were significant. G2 concurrent depressive symptoms were included in the third model, and this was the only variable that remained significantly associated with G3 internalizing problems. In the final model, the interaction between grandparental MDD and parental MDD was included. In this model, G2 concurrent depressive symptoms, the main effects of G1 MDD and G2 MDD, and the interaction between G1 MDD and G2 MDD was significantly associated with G3 internalizing problems.
TABLE 2.
Multiple Regression of G1 and G2 Psychopathology on G3 Internalizing Problems
|
B (SE) |
||||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| G3 male | 1.87 (1.12) | 1.89 (1.13) | 1.70 (1.07) | 1.38 (1.07) |
| G1 MDD | 4.50 (1.93)* | 4.79 (2.08)* | 3.07 (2.02) | 6.29 (2.46)* |
| G2 MDD | 5.09 (1.69)** | 4.44 (1.77)* | 3.19 (1.70) | 7.71 (2.63)** |
| G1 anxiety | 2.43 (3.18) | 2.29 (3.02) | 3.00 (2.99) | |
| G2 anxiety | 1.84 (2.03) | −0.63 (2.01) | −1.03 (1.99) | |
| G1 SUD | −2.57 (2.39) | −1.20 (2.29) | −1.36 (2.27) | |
| G2 SUD | 1.39 (1.48) | 1.23 (1.41) | 1.07 (1.39) | |
| G2 concurrent depression | 0.37 (0.09)*** | 0.36 (0.09)*** | ||
| G1 MDD × G2 MDD | −13.25 (5.93)* | |||
| F3,148 = 6.18, p < .001 | ΔF4,144 = .73, p = 058 | ΔF1,143 = 16.87, p < .001 | ΔF1,142 = 4.99, p < .05 | |
Note: G1 = grandparental generation; G2 = parental generation; G3 = grandchildren; MDD = major depressive disorder; Anxiety = anxiety disorder; SUD = substance use disorder.
p < .05;
p < .01;
p < .001.
To better understand this interaction, we examined the final regression model stratified by the percentage of parents (G2) with MDD. Thus, we estimated three separate regression models that included all other predictors in the final model except the cross-product term for the interaction. When G2 MDD was absent, G1 MDD was significantly associated with G3 internalizing behavior problems (B = 6.55, SE = 2.85, p < .05; pr = .23); when either one or both of the G2 parents had MDD, G1 MDD was not significantly associated with G3 internalizing behavior problems.
For descriptive purposes, Figure 1 presents mean child internalizing problem scores as a function of grandparental MDD and parental MDD. G1 MDD was dichotomized according to whether 50% or more grandparents had a history of MDD and G2 MDD was coded as present if at least one parent had a history of MDD. As the figure illustrates, when parental MDD was absent, a greater loading of MDD in grandparents was associated with higher levels of internalizing problems in grandchildren. However, when parental MDD was present, grandchild internalizing problems were elevated regardless of the loading of MDD in grandparents.
Fig. 1.
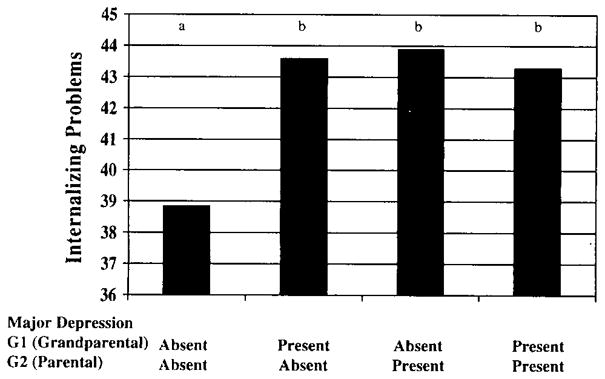
Means of grandchildren (G3) internalizing behavior as a function of G1 (grandparental) and G2 (parental) MDD. Presence of G1 MDD indicates that 50% or more G1 family members had MDD. Different letters indicate significant differences at p < .05. MDD = major depressive disorder.
Grandchildren’s Externalizing Behavior Problems
We conducted the same series of regression models for grandchildren’s externalizing problems. In the first model, grandchild male sex and parental MDD, but not grandparental MDD, were associated with grandchildren’s externalizing problems. When grandparental and parental anxiety and substance use disorders were included in the model, grandchild male sex, grandparental MDD, parental MDD, and parental anxiety disorder were significantly associated with greater grandchild externalizing problems. Parental concurrent depressive symptoms were included in the third model. Grandchild male sex, grandparental MDD, parental anxiety disorder, and parental concurrent depressive symptoms were significantly associated with greater grandchild externalizing behavior. In addition, grandparental anxiety disorder was associated with fewer externalizing problems. In the final model, the interaction between grandparent MDD and parent MDD was entered in the regression. Because this interaction was nonsignificant, we do not interpret the results of this model.
Finally, we examined models that incorporated intergenerational homotypic interactions between anxiety and substance use disorders (grandparent anxiety × parent anxiety and grandparent substance abuse × parent substance abuse). Neither of these interactions was significantly associated with grandchildren’s internalizing or externalizing problems. All of the analyses were repeated controlling for the percentage of G1 who received direct interviews. The results of these analyses were identical to the results presented.
DISCUSSION
We examined the associations of psychopathology in the grandparental (G1) and parental (G2) generations with behavior problems in the grandchild (G3) generation. Our findings are difficult to compare to previous three-generation studies of MDD9–11 because the age of the grandchild generation was much younger and the children had not yet entered the period of risk of depressive and anxiety disorders. In addition, unlike previous studies, we had access to information on psychopathology for the entire G1 and G2 pedigrees. Finally, in addition to examining the relationships between parental and grandparental depressive disorders and internalizing problems in grandchildren, we also included grandparental and parental anxiety and substance use disorders and children’s externalizing problems in order to explore the specificity of the associations.
We found a significant interaction between grandparental MDD and parental MDD on young children’s internalizing symptoms after adjusting for grandchild sex, grandparental and parental anxiety and substance use disorders, and parents’ concurrent depressive symptomatology. This interaction indicated that a higher familial loading for MDD in either the G1 or G2 generations was associated with elevated grandchild internalizing problems, but that higher loadings for MDD in both generations did not convey additional risk. These findings are noteworthy given the young age of the grandchildren (24 months) and indicate that both parental and grandparental MDD are significantly associated with child adjustment at an early age.
Using an older sample, Weissman et al.10 also reported an interaction between G1 MDD and G2 MDD on G3 psychopathology. However, the nature of the interactions in the two studies differed. Weissman et al. found that when parental MDD was present but grandparental MDD was absent, the rates of anxiety disorders and any psychopathology in grandchildren did not differ from the rates in grandchildren with no history of MDD in parents and grandparents. However, rates of psychopathology in grandchildren were elevated when grandparental MDD was present, regardless of the presence or absence of parental MDD. Several methodological differences could account for the divergent findings. First, as noted above, the ages of the grandchildren differed substantially across studies. Second, Weissman et al.10 assessed psychiatric diagnoses in the grandchildren using semistructured interviews, whereas we used parent reports on a symptom checklist. Third, they used a clinical sample, whereas we used a community sample. Finally, Weissman et al.10 had access to diagnostic information on only half of the grandparental generation, whereas we conducted diagnostic assessments on the entire parental and grandparental generations.
It is important to note that despite these substantial methodological differences, both studies found that MDD in the grandparental generation is associated with elevated internalizing symptoms in grandchildren, even in the absence of parental MDD. This is intriguing and could be due to a number of mechanisms. For example, it could reflect incomplete penetrance in the G2 generation, with unaffected parents transmitting susceptibility genes from grandparents to grandchildren. Alternatively, grandparental (G1) MDD could influence the development of characteristics in the parental (G2) generation, such as maladaptive parenting, familial dysfunction, and a tendency to generate stressful family environments30,31 that, in turn, increase risk of internalizing problems in the next (G3) generation. Such processes could be important targets for intervention to disrupt the intergenerational transmission of psychopathology. Indeed, studying the transmission of psychopathology from G1 to G3 in the absence of G2 psychopathology is potentially one of the more important contributions of three-generation studies and may provide a unique window for elucidating risk mechanisms. Regardless of the mechanism, however, the results of Weissman et al. 10 and our study strongly suggest that MDD can have effects that persist for multiple generations and that clinicians and researchers obtain extended family pedigrees to evaluate risk in children. It is especially important not to assume that just because neither parent has a history of MDD, the child has a negative family history, as grandparental depression appears to be associated with increased risk even in the absence of parental depression.
In addition, it is common to investigate offspring of depressed parents (especially mothers) because they are considered a high-risk group. The results here suggest that at least among very young children, offspring of depressed grandparents may be included in such high-risk research designs, regardless of parental history.
In the present study, the pattern of findings differed for internalizing and externalizing problems in grandchildren. This is noteworthy given the high correlation between the internalizing and externalizing scales (r = 0.73). Although there were some associations between grandparental MDD and parental MDD and externalizing behavior in grandchildren, these effects varied depending on which covariates were included in the models. In the final model (model 3 in Table 3), grandchild male sex, grandparental MDD, parental anxiety disorder, and parental concurrent depressive symptoms were positively associated, but grandparental anxiety disorder was negatively associated, with grandchildren’s externalizing behavior problems. Consistent with Weissman et al., 10 grandparental MDD appears to predict G3 behavior problems in general. The associations for grandchild male sex and parents’ concurrent depressive symptoms are consistent with the literature.32,33 However, finding associations for grandparental and parental anxiety disorders that were in opposite directions was surprising. These effects may reflect different pathways to externalizing problems. Parents with anxiety disorders exhibit more inconsistent and maladaptive parenting behavior than nonanxious parents, 34,35 which may account for the positive association between parental anxiety disorder and offspring externalizing problems. However, there is also evidence that anxiety disorders and anxiety-relevant temperament traits such as behavioral inhibition may have a protective effect on the development of disruptive behavior disorders. 36 Thus, it is possible that the negative association between grandparental anxiety disorders and externalizing behavior in grandchildren reflects the transmission of anxiety-related traits that modulate externalizing tendencies. However, this explanation must be tempered by the fact that we did not observe a significant bivariate association between G1 anxiety disorder and G3 externalizing problems.
TABLE 3.
Multiple Regression of G1 and G2 Psychopathology on G3 Externalizing Problems
|
B (SE) |
||||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| G3 male | 3.71 (1.07)** | 3.61 (1.04)** | 3.50 (1.02)** | 3.52 (1.04)** |
| G1 MDD | 3.49 (1.85) | 5.72 (1.92)** | 4.76 (1.93)* | 4.55 (2.39) |
| G2 MDD | 4.31 (1.62)** | 3.81 (1.63)* | 3.12 (1.63) | 2.82 (2.56) |
| G1 anxiety | −5.73 (2.93) | −5.81 (2.89)* | −5.85 (2.91)* | |
| G2 anxiety | 5.32 (1.87)** | 3.95 (1.92)* | 3.98 (1.94)* | |
| G1 SUD | −3.49 (2.21) | −2.73 (2.19) | −2.72 (2.20) | |
| G2 SUD | −0.17 (1.36) | −0.26 (1.34) | −0.25 (1.35) | |
| G2 concurrent depression | 0.21 (0.09)* | 0.21 (0.09)* | ||
| G1 MDD × G2 MDD | 0.88 (5.76) | |||
| F3,148= 7.34, p <.01 | ΔF4,144 = 3.89, p <.01 | ΔF1,143 = 5.69, p <.05 | ΔF1,142 = 0.02, p =.88 | |
Note: G1 = grandparental generation; G2 = parental generation; G3 = grandchildren; MDD = major depressive disorder; anxiety = anxiety disorder; SUD = substance use disorder.
p <.05;
p <.01.
Based on the association between G2 anxiety disorders and G3 externalizing behavior problems, it may be important to assess for parental anxiety disorders when intervening with children with externalizing problems. Behaviors related to anxiety (e.g., unassertiveness) may influence parenting practices that maintain child externalizing problems.
The lack of associations between parental and grandparental substance use disorders and externalizing problems in grandchildren was also surprising in light of the large literature documenting the familial transmission of externalizing behavior.8,37 It is possible that by restricting the study to substance use disorders and not including other forms of externalizing psychopathology, such as antisocial personality disorder, we limited our ability to detect these associations. Alternatively, our sample of grandchildren was only 2 years old. The effects of parental and grandparental substance use disorders on externalizing problems in grandchildren may be more difficult to detect in early childhood.
The present study has several significant strengths, including focusing on an earlier developmental period than has been examined in previous three-generation studies of depression, the availability of diagnostic information on the full G1 and G2 pedigree, and examining the effects of parental and grandparental anxiety and substance use disorders to determine the specificity of the associations with behavior problems in grandchildren. However, our findings should be considered in light of several limitations. First, we were unable to obtain diagnostic information on all G1 and G2 participants. Second, the diagnostic assessments were retrospective, so it is possible that some episodes of psychopathology were not recalled or reported. Third, to maximize power and make our findings as comparable as possible to those of previous studies, we aggregated diagnoses within the grandparental and parental generations. Thus, we could not examine the effects of maternal versus paternal psychopathology or the effects of maternal versus paternal grandmothers and grandfathers. Fourth, we did not examine whether the association between grandparental MDD and offspring behavior problems was mediated by parental MDD. That is, when using having grandparental and parental MDD predicting offspring behavior problems, the association between grandparental MDD and offspring behavior problems should be near zero. Instead, however, the data demonstrated that grandparental and parental MDD both simultaneously influenced grandchild internalizing problems, which argues against mediation. Fifth, the level of behavior problems in the grandchildren was generally in the nonclinical range (Table 1). Thus, it is unclear whether these results can be generalized to clinically significant psychopathology, although it is worth noting that even nonclinical levels of internalizing and externalizing symptomatology have been related to clinically significant outcomes later in life.38 Follow-up will be necessary to determine whether parental and grandparental psychopathology will predict the development of depressive and anxiety disorders in the grandchildren. Sixth, children’s behavior problems were assessed via parent report. Thus, it is possible that our results are influenced by reporting biases. Because one of the best documented sources of reporting bias is current mood state,28 we included parents’ concurrent depressive symptoms in the models. However, future studies should examine the relationship between parental and grandparental psychopathology and behavior problems in grandchildren using other informants and other methods, such as semistructured diagnostic interviews and home and laboratory observations. Last, this design cannot distinguish between genetic and environmental effects. More genetically informative designs are needed to provide information regarding the mechanism of transmission of behavior problems across three generations.
Acknowledgments
This work was supported by National Institute of Mental Health research grant RO1 MH-56604 (P.M.L.), RO1 MH-66023 (D.N.K), RO1 MH-75744 (J.W.P.).
Footnotes
Disclosure: The authors report no conflicts of interest.
References
- 1.Goodman SH, Gotlib IḢ. Children of Depressed Parents: Mechanisms of Risk and Implications for Treatment. Washington, DC: American Psychological Association; 2002. [Google Scholar]
- 2.Kane P, Garber J. The relations among depression in fathers, children’s psychopathology, and father-child conflict: a meta-analysis. Clin Psychol Rev. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Arch Gen Psychiatry. 2003;60:253–258. doi: 10.1001/archpsyc.60.3.253. [DOI] [PubMed] [Google Scholar]
- 4.Lieb R, Isensee B, Hofler M, et al. Parental major depression and the risk of depression and other mental disorders in offspring: a prospective-longitudinal community study. Arch Gen Psychiatry. 2002;59:365–374. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- 5.Klein DN, Lewinsohn PM, Rohde P, et al. Adolescent and young adult offspring of parents with major depression: effects of parental gender, diagnostic specificity, and moderating factors on psychopathology in offspring. Psychol Med. 2005;35:353–365. doi: 10.1017/s0033291704003587. [DOI] [PubMed] [Google Scholar]
- 6.Capaldi DM, Pears KC, Patterson GR, et al. Continuity of parenting practices across generations in an at-risk sample: a prospective comparison of direct and mediated associations. J Abnorm Child Psychol. 2003;31:127–142. doi: 10.1023/a:1022518123387. [DOI] [PubMed] [Google Scholar]
- 7.Conger RD, Neppl T, Kim KJ, et al. Angry and aggressive behavior across three generations: a prospective, longitudinal study of parents and children. J Abnorm Child Psychol. 2003;31:143–160. doi: 10.1023/a:1022570107457. [DOI] [PubMed] [Google Scholar]
- 8.Thornberry TP, Freeman-Gallant A, Lizotte AJ, et al. Linked lives: the intergenerational transmission of antisocial behavior. J Abnorm Child Psychol. 2003;31:174–184. doi: 10.1023/a:1022574208366. [DOI] [PubMed] [Google Scholar]
- 9.Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: test of an interpersonal stress model in a community sample. J Consult Clin Psychol. 2004;72:511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- 10.Weissman MM, Wickramaratne P, Nomura Y, et al. Families at high and low risk for depression: a three generation study. Arch Gen Psychiatry. 2005;62:29–36. doi: 10.1001/archpsyc.62.1.29. [DOI] [PubMed] [Google Scholar]
- 11.Warner V, Weissman MM, Mufson L, et al. Grandparents, parents, and grandchildren at high risk for depression: a three-generational study. J Am Acad Child Adolesc Psychiatry. 1999;38:289–296. doi: 10.1097/00004583-199903000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: a meta- analysis. Psychol Bull. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- 13.Lewinsohn PM, Hops H, Robert RE, et al. Adolescent psychopathology: I. prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- 14.Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. J Child Psychol Psychiatry. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- 15.Luby JL, Mrakotsky C, Heffelfinger A, et al. Modification of DSM-IV criteria for depressed preschool children. Am J Psychiatry. 2003;160:1169–1172. doi: 10.1176/appi.ajp.160.6.1169. [DOI] [PubMed] [Google Scholar]
- 16.Del Carmen-Wiggins R, Carter A. Handbook of Infant Toddler, and Preschool Mental Health Assessment. New York: Oxford University Press; 2004. [Google Scholar]
- 17.Kelley SA, Jennings KD. Putting the pieces together: maternal depression, maternal behavior, and toddler helplessness. Infant Ment Health J. 2003;24:74–90. [Google Scholar]
- 18.Kochanska G. Patterns of inhibition to the unfamiliar in children of normal and affectively ill mothers. Child Dev. 1991;62:250–263. doi: 10.1111/j.1467-8624.1991.tb01529.x. [DOI] [PubMed] [Google Scholar]
- 19.Hernandez-Reif M, Field T, Del Pino N, et al. Less exploring by mouth occurs in newborns of depressed mothers. Infant Ment Health J. 2003;21:204–210. [Google Scholar]
- 20.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders, Non-Patient Edition (SCID-NP, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 21.Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- 22.Sobin C, Weissman MM, Goldstein RB, et al. Diagnostic interviewing for family studies—comparing telephone and face-to-face methods for the diagnosis of lifetime psychiatric-disorders. Psychiatr Genet. 1993;3:227–233. [Google Scholar]
- 23.Cohen P. The effects of diagnostic instrumentation and informants on ascertainment. In: Robins L, Rutter M, editors. Relatives at risk for mental disorders. New York: Raven; 1988. pp. 31–52. [Google Scholar]
- 24.Mannuzza S, Fyer AJ. Family Informant Schedule and Criteria (FISC), July 1990 Revision. New York: Anxiety Disorders Clinic, New York State Psychiatric Institute; 1990. [Google Scholar]
- 25.Leckman JF, Sholomskas D, Thompson D, et al. Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry. 1982;39:879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- 26.Achenbach TM. Manual for the Child Behavior Checklist/2–3 and 1992 Profile. Burlington: University of Vermont, Department of Psychiatry; 1992. [Google Scholar]
- 27.Achenbach TM. Child Behavior Checklist: 4–18 Years (CBCL/4–18) Burlington: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 28.Chilcoat HD, Breslau N. Does psychiatric history bias mothers’ reports? an application of a new analytic approach. J Am Acad Child Adolesc Psychiatry. 1997;36:971–979. doi: 10.1097/00004583-199707000-00020. [DOI] [PubMed] [Google Scholar]
- 29.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 30.Lewinsohn PM, Olino TM, Klein DN. Impairments in offspring of depressed parents. Psychol Med. 2005;35:1493–1503. doi: 10.1017/S0033291705005350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hammen C. Stress generation in depression: reflections on origins, research, and future directions. J Clin Psychol. 2006;62:1065–1082. doi: 10.1002/jclp.20293. [DOI] [PubMed] [Google Scholar]
- 32.Fagot BI, Leve LD. Teacher ratings of externalizing behavior at school entry for boys and girls: similar early predictors and different correlates. J Child Psychol Psychiatry. 1998;39:555–566. [PubMed] [Google Scholar]
- 33.Spieker SJ, Larson NC, Lewis SM, et al. Developmental trajectories of disruptive behavior problems in preschool children of adolescent mothers. Child Dev. 1999;70:443–458. doi: 10.1111/1467-8624.00032. [DOI] [PubMed] [Google Scholar]
- 34.Turner SM, Beidel DC, Roberson-Nay R, et al. Parenting behaviors in parents with anxiety disorders. Behav Res Ther. 2003;41:541–554. doi: 10.1016/s0005-7967(02)00028-1. [DOI] [PubMed] [Google Scholar]
- 35.Woodruff-Borden J, Morrow C, Bourland S, et al. The behavior of anxious parents: examining mechanisms of transmission of anxiety from parent to child. J Clin Child Adolesc Psychol. 2002;31:364–374. doi: 10.1207/S15374424JCCP3103_08. [DOI] [PubMed] [Google Scholar]
- 36.Schwartz CE, Snidman N, Kagan J. Adolescent social anxiety as an outcome of inhibited temperament in childhood. J Am Acad Child Adolesc Psychiatry. 1999;38:1008–10015. doi: 10.1097/00004583-199908000-00017. [DOI] [PubMed] [Google Scholar]
- 37.Hicks BM, Krueger RF, Iocono WG, et al. Family transmission and heritability of externalizing disorders: a twin-family study. Arch Gen Psychiatry. 2004;61:922–928. doi: 10.1001/archpsyc.61.9.922. [DOI] [PubMed] [Google Scholar]
- 38.Mesman J, Koot HM. Early preschool predictors of preadolescent internalizing and externalizing DSM-IV diagnoses. J Am Acad Child Adolesc Psychiatry. 2001;40:1029–1036. doi: 10.1097/00004583-200109000-00011. [DOI] [PubMed] [Google Scholar]


