Abstract
Acute decompensated heart failure (ADHF) is a common and highly morbid cardiovascular disorder. Most hospitalizations for ADHF are related to symptoms of congestion, and the vast majority of ADHF patients are treated with intravenous loop diuretics. Despite this nearly ubiquitous use, data supporting the safety and efficacy of loop diuretics in ADHF are limited, and controversy exists about the best way to use loop diuretics with regard to both dosing and means of administration (continuous infusion vs. intermittent boluses). We reviewed the data supporting the safety and efficacy of loop diuretics in patients with ADHF. A large body of observational literature suggests that loop diuretics, especially at higher doses, may be associated with increased mortality in patients with heart failure even after detailed adjustment for other measures of disease severity. Additionally, multiple small underpowered trials suggest that continuous infusion may be equivalent or superior to intermittent bolus dosing. In summary, there is a critical need to develop more robust data on the use of loop diuretics in ADHF. In that context, the NIH Heart Failure Clinical Research Network has begun the Diuretics Optimization Strategies Evaluation (DOSE) study, a multi-center, double-blind, randomized controlled trial that will enroll 300 patients with ADHF. The DOSE study will randomize patients using a 2 × 2 factorial design to low dose vs. high dose furosemide, and intermittent bolus vs. continuous infusion. Successful completion of the DOSE study will provide important data on the optimal clinical use of loop diuretics in ADHF.
Keywords: diuretics, acute decompensated heart failure, clinical trials
“In times of great danger, you are permitted to walk with the devil until you have crossed the bridge”.
Bulgarian proverb
Acute decompensated heart failure (ADHF) is the most common cause of hospital admission in patients over age 65, accounting for over 1 million hospitalizations, 6 million hospital days, and $12 billion in costs annually in the United States alone1, 2. The prognosis of patients admitted with AHF is dismal, with rates of rehospitalization or death approaching 50% within 6 months 3, 4. Despite these alarming and oft-cited statistics, the development of new therapies in ADHF has changed little over recent decades5, and short and intermediate-term outcomes have remained poor6. In addition to spurring the development of new therapies for ADHF, these data suggest the need for an active reappraisal of current therapy. This review will focus on the data (or lack thereof) supporting the efficacy and safety of loop diuretics in ADHF, discuss the challenges in performing clinical trials of diuretics in ADHF, and describe an ongoing clinical trial designed to rigorously evaluate optimal diuretic use in this syndrome.
Loop diuretics are the foundation of current ADHF therapy. Data from the Acute Decompensated Heart Failure National Registry (ADHERE) demonstrate that approximately 90% of patients hospitalized with ADHF in the United Sates receive intravenous (IV) loop diuretics during the hospitalization7. This nearly ubiquitous use of loop diuretics in ADHF is understandable given that the vast majority of ADHF hospitalizations are related to volume overload and congestion8, and decades of clinical observation has shown that intravenous administration of loop diuretics results in prompt diuresis and relief of symptoms in most patients. Despite this breadth of clinical experience, however, high quality data supporting the safety and efficacy of loop diuretics in ADHF are sparse. Accordingly, the most recent practice guidelines for ADHF from the Heart Failure Society of America recommend loop diuretics at “doses needed to produce a rate of diuresis sufficient to achieve an optimal volume status”9. Notably, this guideline has the strongest level of recommendation (“is recommended”) but the lowest level of evidence (C, based on expert opinion only). Current guidelines from the American College of Cardiology and the American Heart Association do not address the treatment of acute decompensated heart failure.10 Although modern phase II development programs for new drugs go to great lengths to identify the range of doses that best balance safety and efficacy, these fundamental clinical questions have not been rigorously investigated for loop diuretics. Given the lack of available evidence to guide diuretic therapy, it is not surprising that practice patterns vary widely between physicians and centers. In a study identifying unanswered questions in heart failure management, over 50% of the questions were related to the most appropriate use of diuretics11.
Safety of Loop Diuretics in ADHF
Several mechanistic considerations suggest the possibility that loop diuretics may have detrimental effects in patients with heart failure. Administration of loop diuretics to patients with heart failure has been shown to activate the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system (SNS), both of which are known to play a fundamental role in heart failure progression12–14. Although decreases in intravascular volume from diuretic therapy contribute to RAAS and SNS activation, volume independent mechanisms also play a role, including the direct stimulation of renin release by blocking sodium chloride uptake at the macula densa and upregulation of renin gene expression in the kidney15. These mechanisms may underlie the clinical observation that loop diuretics are associated with increases in systemic vascular resistance and may initially raise ventricular filling pressures13.
Administration of loop diuretics to patients with heart failure may result in a significant decrease in glomerular filtration rate in some patients with heart failure, presumably due to RAAS and SNS activation with related changes in renal blood flow and glomerular filtration pressure16. Paradoxically, some patients with ADHF may have improvement in renal function with diuretic therapy, potentially due to improvements in functional mitral regurgitation with unloading or changes in venous or intra-abdominal pressure17. Administration of loop diuretics may lead to electrolyte imbalances (such hypokalemia, hyponatremia, and hypomagnesemia) that may exacerbate cardiac arrhythmias and increase the risk of sudden cardiac death18, 19. Although placebo controlled studies of diuretics in human with heart failure have not been performed, an animal study using a porcine heart failure model showed that treatment with furosemide resulted in an increased progression of left ventricular systolic dysfunction, increases in circulating aldosterone levels, and a greater down regulation of beta-adrenergic responsiveness compared to placebo20.
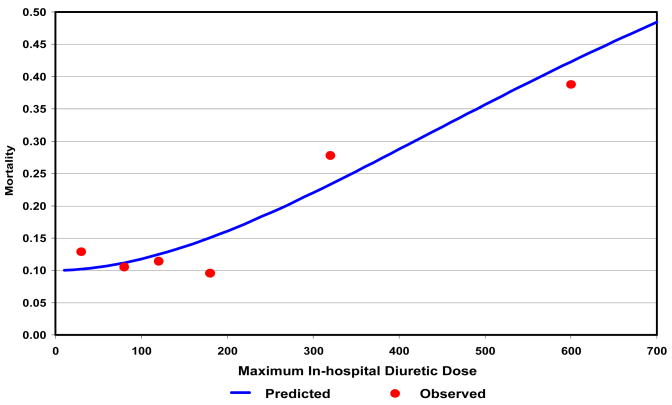
Clinically, multiple observations have suggested an association between diuretic use and worsening outcomes in patients with heart failure (Table 1)19, 21–27. In the Studies of Left Ventricular Function (SOLVD) Trial, use of a diuretic was associated with a 37% increase in the risk of arrhythmic death after controlling for multiple other measures of disease severity19. Several other studies have identified an association between higher doses of diuretics in patients and adverse outcomes in with ADHF26, 28 and advanced heart failure outpatients24, 25, 27 and inpatients23. An analysis of data from the Digitalis Investigation Group (DIG) study used sophisticated propensity matching to control for baseline differences in patients taking diuretics compared to those who were not, and still found a 31% increased risk of death associated with diuretic use.21 Most recently, analysis of the data from the Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness (ESCAPE) study demonstrated a nearly linear relationship between loop diuretic dose and mortality over 6 months of follow up in patients hospitalized with advanced heart failure (Figure 1)23.
Table 1.
Observational Studies of Diuretics and Outcomes in Heart Failure
| Study | Population | N | Comparison | Endpoint | Risk | 95% CI |
|---|---|---|---|---|---|---|
| SOLVD19 | LV dysfunction with or without HF | 6797 | Oral diuretics vs. none | Mortality | 1.37 | 1.08–1.73 |
| DIG21 | chronic HF | 2782 | Oral diuretics vs. none | Mortality | 1.31 | 1.11–1.55 |
| Butler22 | ADHF | 382 | Dose of IV loop diuretics | worsening renal function (Δ 0.3mg/dl) | 1.04 per 20 mg increment of furosemide | 1.004–1.076 |
| ESCAPE23 | Advanced HF inpts | 395 | Dose of IV loop diuretics | Mortality | 1.15 per doubling of dose | 1.025–1.28 |
| Eshaghian24 | Advanced HF outpts | 1354 | Dose of oral diuretics | Mortality | 3.4 per quartile of dose | 2.4–4.7 |
| Neuberg25 | chronic HF | 1153 | Diuretic oral dose (<> 80 mg furosemide) | Mortality | 1.37 for dose above median | not provided, p=0.004 |
| Philbin26 | ADHF | 1150 | # of IV diuretic doses | In-hospital mortality | 1.11 per # of doses | 1.06–1.17 |
| Mielniczuk27 | chronic HF | 183 | oral diuretic dose | HF events | 1.53 for dose > 80mg | 0.58–4.03 |
Figure 1.
Relationship between maximum in-hospital diuretic dose and mortality in the ESCAPE study (Reprinted from reference 23, with permission from Elsevier).
Although these observational data demonstrate an association between higher doses of diuretics and worse outcomes, all such data are highly confounded by indication, i.e., patients who receive higher doses of diuretics may do so because of greater disease severity compared to patients who can be successfully treated with lower doses of diuretics. Although most (but not all) prior studies have found a persistent adverse effect of loop diuretics even after multi-variable adjustment for other known predictors of mortality, such adjustment may be insufficient to completely eliminate confounding. Prospective, carefully controlled studies will be required to clarify whether there is a causal relationship between diuretic use and adverse outcomes, or alternatively if diuretic dosage is just a surrogate for disease severity.
Efficacy of Loop Diuretics in ADHF
Administration of intravenous furosemide to patients with ADHF typically results in a prompt diuretic effect (within 30 minutes) that peaks at 1.5 hours. This effect leads to a decrease in ventricular filling pressures and improvement in symptoms in the majority of patients with ADHF. This observation has been confirmed in the placebo groups of the Value of Endothelin Receptor Inhibition with Tezosentan in Acute Heart Failure Studies (VERITAS) and Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST), in which treatment based primarily on loop diuretics was associated with rapid and substantial improvement of dyspnea29, 30.
Despite this clinical efficacy, substantial questions remain about how to best use diuretics to treat volume overload in patients with heart failure. One major unanswered issue is the most appropriate dosing strategy for loop diuretics in ADHF. There are almost no data evaluating the relationship between diuretic dose and diuretic efficacy in ADHF. In the ESCAPE study, higher doses of intravenous loop diuretics were not associated with greater weight loss during the index hospitalization after adjustment for other measures23. Doses in published studies of intravenous furosemide in heart failure have ranged over 200 fold, from as low as 20 mg to as high as 4000 mg daily31, 32.
Several aspects of the pharmacology of loop diuretics may account in part for the observed variability in diuretic dosing for ADHF. Heart failure shifts the dose response curve for loop diuretics downward and the right, necessitating a higher starting dose in order to achieve the same level of sodium excretion. Additionally, the “braking phenomenon”, characterized by a progressively diminishing response to diuretic therapy with ongoing treatment, is well recognized in heart failure patients and appears to be related to several underlying mechanisms. As described above, loop diuretics activate both the RAAS and SNS, both of which tend to reduce renal blood flow and increase resorbtion of sodium in the proximal and distal tubule. Absolute or relative decreases in intravascular volume with ongoing diuretic therapy leads to a decrease in the amount of sodium filtered at the glomerulus and an increase in the amount of sodium reabsorbed33. Chronic loop diuretic therapy also leads to structural changes in the kidney itself, particularly hypertrophy of the epithelial cells in the distal tubules, which enhance distal reabsorbtion of sodium and limit sodium excretion and diuresis.34 The combined effects of heart failure, frequent concomitant renal insufficiency, and physiologic braking all contribute to the clinical phenomenon of diuretic resistance, in which patient have persistent evidence of volume overload but are progressively resistant to the effects of loop diuretics. When accompanied by worsening renal function, this has been termed the “cardio-renal syndrome”, and represents a major clinical challenge in the management of acute decompensated heart failure.35.
Do higher doses of loop diuretics contribute to the development of the cardio-renal syndrome? In a retrospective analysis, Butler and colleagues identified higher loop diuretic dosage as an independent predictor of worsening renal function in ADHF even after controlling for disease severity and the degree of diuresis 22. As with the relation between diuretic dose and mortality described above, however, it may be impossible to completely adjust for other confounders of disease severity that could effect both diuretics requirements and the risk of worsening renal function. Thus it remains unknown whether higher diuretic requirement are simply a marker for higher risk or whether higher doses of loop diuretics contribute directly to the development of the cardio-renal syndrome in patients with ADHF.
Are there Safer Ways to Use Diuretics? Bolus vs. Infusion
The concerns about safety and efficacy described above suggest the need to identify the better strategies for using loop diuretics in ADHF. In addition to the questions about dosing described above, ongoing uncertainty exists about the optimal route of administration of intravenous loop diuretics (bolus dosing or continuous infusion). From a pharmacokinetic and pharmacodynamic perspective, there are potential benefits of continuous infusion as compared to intermittent bolus dosing. Bolus diuretic dosing may be associated with a higher rate of diuretic resistance due to prolonged periods of sub-therapeutic drug levels in the kidney. For example, giving an IV bolus of furosemide twice daily results in a 4–6 hour period of diuretic effect, followed by a 6–8 hour period of sub-therapeutic diuretic concentration during which sodium reabsorbtion in the kidney may rebound, especially in the face of inadequate dietary sodium restriction33. Continuous infusion results in a more constant delivery of diuretic to the tubule, potentially reducing this phenomenon. Additionally, continuous infusion is associated with lower peak plasma concentrations, which may be associated with a lower incidence of other side effects such as ototoxicity, especially at higher doses.
Multiple small studies have evaluated the role of continuous infusion of loop diuretics in patients with heart failure 36–41. These studies have been underpowered to address clinical questions and have generally lacked methodologic rigor. A recent meta-analysis from the Cochrane Collaboration comprehensively evaluated the available literature to address this question31 and identified studies including a total of 254 patients who met rigorous analytical standards (Table 2)42–48. In general, continuous infusion was associated with greater urine output, shorter length of hospital stay, less impairment of renal function, and lower mortality when compared to intermittent bolus dosing. Notably, however, almost all the conclusions of this meta-analysis were driven by a single study by Licata and colleagues, which was substantially confounded by the use of hypertonic saline infusion in the continuous infusion group 48. In their conclusions, the authors of the Cochrane analysis strongly emphasized the overall poor quality of the available data and the need for methodologically sound and adequately powered randomized trials to definitively address this question31.
Table 2.
Randomized Trials of bolus vs. continuous infusion of diuretics in heart failure
| Study | N | Design | Intervention | Duration | Endpoint(s) | Findings |
|---|---|---|---|---|---|---|
| Aaser42 | 8 | randomized, cross-over, unblinded | Continuous infusion vs. BID IV bolus | 24 hrs | Urine output | bolus better |
| Dormans44 | 20 | randomized, cross-over, unblinded | continuous infusion vs. single IV bolus | 24 hrs | Urine output | infusion better |
| Kramer45 | 8 | randomized, cross-over, unblinded | continuous infusion vs. single IV bolus | 24 hrs | Urine output | no difference |
| Lahav46 | 9 | randomized, cross-over, unblinded | Continuous infusion vs. q8 hr bolus | 48 hrs | Urine output | infusion better (trend) |
| Licata48 | 107 | randomized, single blind | Continuous infusion + hypertonic saline vs. Q12 bolus | 6–12 days | Urine output at 24 hours LOS Mortality | infusion better on all endpoints |
| Pivac43 | 20 | randomized, single blind, crossover | Q12 4 hour “infusion” vs. Q12 bolus | 24 hrs | Urine output | infusion better |
| Schuller47 | 33 | randomized, unblinded | continuous infusion vs. bolus | 72 hrs | mortality | No difference |
In sum, almost all patients with ADHF are treated with a therapy (intravenous loop diuretics) about which there is substantial uncertainty regarding the best dosing strategy and route of administration, and for which observational data raise concerns about the overall safety. This suggests the need for an adequately powered, carefully controlled clinical study to address the balance between safety and efficacy of various dosing and mode of administration strategies for loop diuretics in ADHF —a “phase II development program” for furosemide.
Is it Possible to Study Diuretics in ADHF? Design of the DOSE Study
Despite the meager data on which current clinical practice is based, diuretics are seen as so fundamental to ADHF management that careful, evidence based investigation of their use is challenging. Placebo controlled trials of diuretics in highly symptomatic patients with ADHF have been appropriately deemed unethical. One strategy for investigating optimal diuretic therapy is to evaluate differing doses or combinations with other agents. Cotter et al compared a vasodilator focused strategy (high dose nitrates with low dose diuretics) to a diuretic focused strategy (high dose diuretics and low dose nitrates) in patients with ADHF and acute pulmonary edema, and found that the vasodilator focused strategy led to significantly lower incidence of the need for mechanical ventilation and of myocardial infarction49.
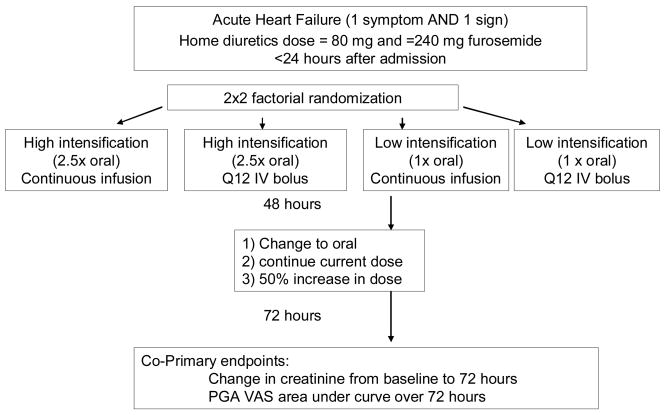
In light of the uncertainty about loop diuretics, the optimal dosing strategy, and the best route of administration, the National Heart, Lung and Blood Institute Heart Failure Clinical Research Network (HFCRN) has undertaken a multicenter, randomized, controlled trial of loop diuretic strategies in ADHF, the Diuretic Optimization Strategies Evaluation (DOSE) study (clinicaltrials.gov, NCT00577135). DOSE will randomize 300 patients hospitalized with ADHF and signs and/or symptoms of congestion in a 2 × 2 factorial design, in order to test the following hypotheses:
That “low intensification” furosemide therapy (1 × the chronic oral dose) will be more efficacious (with regard to relief of symptoms) and safer (with regard to changes in renal function), as compared to “high intensification” furosemide therapy (2.5 × the chronic oral dose) in patients with ADHF
That continuous infusion diuretic therapy will be more efficacious (with regard to relief of symptoms) and safer (with regard to renal function), as compared to twice daily bolus therapy in patients with ADHF
The co-primary endpoints will be improvement in symptoms (based on the area under the curve of the patient global assessment using a visual analog scale) from randomization to 72 hours, and the change in serum creatinine between randomization and 72 hours. Given the subjective nature of the evaluation of clinical symptoms, the DOSE study will use a double-blind, double dummy design to minimize bias. All patients will receive both a continuous infusion and intermittent IV boluses, one of which will contain furosemide and the other a saline placebo. A flow chart of treatment assignment and study timeline for the DOSE study is shown in Figure 2.
Figure 2.
Study Schema for DOSE Study. ADHF=acute decompensated heart failure. PGA=patient global assessment, VAS=visual analog scale, AUC=area under the curve
The design of the DOSE study has several notable challenges that are worthy of comment. With regard to dosage, the investigators recognized that what constitutes a high dose or low dose of diuretics for an individual patient differs based on patient specific factors such as baseline renal function and chronic diuretic dose. Therefore, assigned diuretic dosing will be based on the chronic oral diuretic dosage (1 × oral dose for “low intensification”, and 2.5 × oral dose for “high intensification”). In clinical practice, diuretic strategies are continually reassessed and adjusted based on the clinical condition of the patient and the response to therapy. This creates a substantial tension between the desire to adjust the diuretic dose frequently and the need to have patients continue on their assigned treatment in order to evaluate the differences between therapies. To provide an opportunity to adjust diuretic dosing within the context of the study protocol, an adjustment in diuretic dosing is permitted by the study protocol at 48 hours from the time of randomization. Based on the clinical assessment of the patient at that time, the treating physician may chose to:
Maintain current strategy without change
Increase dose by 50% (while remaining blinded)
Change to oral diuretics (dose at physician discretion)
Patients requiring additional open label diuretics, IV vasoactive agents, or mechanical support during the randomization period will meet the secondary endpoint of “worsening or persistent heart failure”. Conversely, patients may develop signs or symptoms of excessive diuresis (such as hypotension or worsening azotemia) that necessitate holding or discontinuing diuretics before completion of the randomization period. This will be captured as a “treatment failure” only if it requires specific intervention beyond simply holding diuretics. As this is a randomized trial comparing initial diuretic strategies, in all cases the interpretation of the primary endpoints with regard to both symptom relief and renal function will be on an “intention to treat” basis. All subjects will undergo serial measurement of cardiac and renal biomarkers throughout the index hospitalization and during follow-up. The DOSE study is currently enrolling patients at 9 regional clinical centers in the United States and Canada.
Conclusions
ADHF has emerged as one of the most important clinical syndromes in cardiovascular medicine in terms of incidence, morbidity, and costs. Although loop diuretics are the mainstay of therapy for ADHF, much uncertainty remains about the safety and efficacy of various doses as well as means of administration. While observational data can provide clues to the safety and efficacy of therapies, a true assessment of the risks and benefits can only be achieved with an appropriately powered, prospective randomized clinical trial. Despite the challenges of performing rigorous randomized trials of diuretic therapy, we suggest that a therapy provided routinely to almost all patients with ADHF should be held to a higher level of evidence than expert opinion only9. The DOSE study is attempting to address the critical question of how best to use loop diuretics in patients with ADHF and signs and symptoms of volume overload. Successful completion of the DOSE study will identify the optimal initial strategy of loop diuretics in this patient population, which will be broadly representative of the roughly 1 million yearly hospitalizations for ADHF in the United States annually.
In addition to the obvious clinical benefit of defining the best strategy for diuretic therapy, data from the DOSE study will help establish a standard for optimal background therapy against which future ADHF therapies can be compared. Defining the optimal strategy for diuretic administration will therefore not only impact current clinical care, but will aid in the development and evaluation of new ADHF therapies moving forward.
Acknowledgments
Funding Source: The Heart Failure Clinical Research Network is funded by the National Heart, Lung and Blood Institute (NHLBI).
APPENDIX
Clinical sites and investigators participating in the Heart Failure Clinical Research Network:
Network Chair: Eugene Braunwald, MD
NHLBI Project Officers: Alice Mascette, MD
Robin Boineau, MD
Data Coordinating Center: Kerry Lee, PhD
Duke Clinical Research Institute, Durham, NC
Principle Investigators and Clinical Centers:
David Bull, MD
University of Utah Health Sciences Center
Salt Lake City, UT
Steven Goldsmith, MD
University of Minnesota
Minneapolis, MN
Martin LeWinter, MD
University of Vermont
Burlington, VT
Douglas Mann, MD
Baylor College of Medicine
Houston, TX
Christopher O’Connor, MD
Duke University
Durham, NC
Elizabeth Ofili, MD
Morehouse School of Medicine
Atlanta, GA
Margaret Redfield, MD
Mayo Clinic
Rochester, MN
Jean-Lucien Rouleau, MD
University of Montreal
Montreal, Quebec, Canada
Lynne Stevenson, MD
Harvard University
Boston, MA
Footnotes
Conflict of Interest Disclosures: None
References
- 1.Members of the Statistics C, Stroke Statistics S, Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, Zheng ZJ, Flegal K, O’Donnell C, Kittner S, Lloyd-Jones D, Goff DC, Jr, Hong Y, Adams R, Friday G, Furie K, Gorelick P, Kissela B, Marler J, Meigs J, Roger V, Sidney S, Sorlie P, Steinberger J, Wasserthiel-Smoller S, Wilson M, Wolf P. Heart Disease and Stroke Statistics--2006 Update: A Report From the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85–151. doi: 10.1161/CIRCULATIONAHA.105.171600.
- 2.Felker GM, Adams KF, Konstam MA, O’Connor CM, Gheorghiade M. The problem of decompensated heart failure: Nomenclature, classification, and risk stratification. Am Heart J. 2003;145:S18–S25. doi: 10.1067/mhj.2003.150. [DOI] [PubMed] [Google Scholar]
- 3.Felker GM, Leimberger JD, Califf RM, Cuffe MS, Massie BM, Adams KF, Jr, Gheorghiade M, O’Connor CM. Risk stratification after hospitalization for decompensated heart failure. J Card Fail. 2004;10:460–466. doi: 10.1016/j.cardfail.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Lee DS, Austin PC, Rouleau JL, Liu PP, Naimark D, Tu JV. Predicting Mortality Among Patients Hospitalized for Heart Failure: Derivation and Validation of a Clinical Model. JAMA: The Journal of the American Medical Association. 2003;290:2581–2587. doi: 10.1001/jama.290.19.2581. [DOI] [PubMed] [Google Scholar]
- 5.Ramirez A, Abelmann WH. Cardiac decompensation. New Eng J Med. 1974;290:499–501. doi: 10.1056/NEJM197402282900906. [DOI] [PubMed] [Google Scholar]
- 6.Lee DS, Mamdani MM, Austin PC, Gong Y, Liu PP, Rouleau JL, Tu JV. Trends in heart failure outcomes and pharmacotherapy: 1992 to 2000. Am J Med. 2004;116:581–589. doi: 10.1016/j.amjmed.2003.11.025. [DOI] [PubMed] [Google Scholar]
- 7.Emerman CL, Marco TD, Costanzo MR, Peacock WF for the ASAC. Impact of intravenous diuretics on the outcomes of patients hospitalized with acute decompensated heart failure: insights from the ADHERE(R) Registry. J Card Fail. 2004;10:S116–S117. [Google Scholar]
- 8.Adams, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, Berkowitz RL, Galvao M, Horton DP. Characteristics and outcomes of patients hospitalized for heart failure in the United States: Rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE) Am Heart J. 2005;149:209–216. doi: 10.1016/j.ahj.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Adams KF, Lindenfeld J, Arnold JM, Baker D, Barnhard DH, Baughman KL, Boehmer JP, Deedwania P, Dunbar SB, Elkayam U, Gheorghiade M, Howlett J, Konstam MA, Kronenberg MW, Massie BM, Mehra MR, Miller AB, Moser DK, Patterson JK, Rodeheffer RJ, Sackner-Bernstein JD, Silver MA, Starling MR, Stevenson LW, Wagoner LE. HFSA 2006 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2006;12:1–119. [Google Scholar]
- 10.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult--Summary Article: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): Developed in Collaboration With the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: Endorsed by the Heart Rhythm Society. Circulation. 2005;112:1825–1852. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 11.Shah MR, Stevenson LW. Searching for evidence: Refractory questions in advanced heart failure. J Card Fail. 2004;10:210–218. doi: 10.1016/j.cardfail.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Francis GS, Benedict C, Johnstone DE, Kirlin PC, Nicklas J, Liang CS, Kubo SH, Rudintoretsky E, Yusuf S. Comparison of Neuroendocrine Activation in Patients with Left-Ventricular Dysfunction with and Without Congestive-Heart-Failure - A Substudy of the Studies of Left-Ventricular Dysfunction (SOLVD) Circulation. 1990;82:1724–1729. doi: 10.1161/01.cir.82.5.1724. [DOI] [PubMed] [Google Scholar]
- 13.Francis GS, Siegel RM, Goldsmith SR, Olivari MT, Levine TB, Cohn JN. Acute Vasoconstrictor Response to Intravenous Furosemide in Patients with Chronic Congestive Heart-Failure - Activation of the Neurohumoral Axis. Ann Intern Med. 1985;103:1–6. doi: 10.7326/0003-4819-103-1-1. [DOI] [PubMed] [Google Scholar]
- 14.Bayliss J, Norell M, Canepaanson R, Sutton G, Poolewilson P. Untreated Heart-Failure - Clinical and Neuroendocrine Effects of Introducing Diuretics. British Heart Journal. 1987;57:17–22. doi: 10.1136/hrt.57.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellison DH. Diuretic therapy and resistance in congestive heart failure. Cardiology. 2001;96:132–143. doi: 10.1159/000047397. [DOI] [PubMed] [Google Scholar]
- 16.Gottlieb SS, Brater DC, Thomas I, Havranek E, Bourge R, Goldman S, Dyer F, Gomez M, Bennett D, Ticho B, Beckman E, Abraham WT. BG9719 (CVT-124), an A(1) adenosine receptor antagonist, protects against the decline in renal function observed with diuretic therapy. Circulation. 2002;105:1348–1353. doi: 10.1161/hc1102.105264. [DOI] [PubMed] [Google Scholar]
- 17.Mullens W, Abrahams Z, Skouri HN, Francis GS, Taylor DO, Starling RC, Paganini E, Tang WHW. Elevated intra-abdominal pressure in acute decompensated heart failure. J Am Coll Cardiol. 2008;51:300–306. doi: 10.1016/j.jacc.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 18.Klein L, O’Connor CM, Leimberger JD, Gattis-Stough W, Pina IL, Felker GM, Adams KF, Jr, Califf RM, Gheorghiade M for the O-CHFI. Lower Serum Sodium Is Associated With Increased Short-Term Mortality in Hospitalized Patients With Worsening Heart Failure: Results From the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) Study. Circulation. 2005;111:2454–2460. doi: 10.1161/01.CIR.0000165065.82609.3D. [DOI] [PubMed] [Google Scholar]
- 19.Cooper HA, Dries DL, Davis CE, Shen YL, Domanski MJ. Diuretics and risk of arrhythmic death in patients with left ventricular dysfunction. Circulation. 1999;100:1311–1315. doi: 10.1161/01.cir.100.12.1311. [DOI] [PubMed] [Google Scholar]
- 20.McCurley JM, Hanlon SU, Wei Sk, Wedam EF, Michalski M, Haigney MC. Furosemide and the progression of left ventricular dysfunction in experimental heart failure. J Am Coll Cardiol. 2004;44:1301–1307. doi: 10.1016/j.jacc.2004.04.059. [DOI] [PubMed] [Google Scholar]
- 21.Ahmed A, Husain A, Love TE, Gambassi G, Dell’Italia LJ, Francis GS, Gheorghiade M, Allman RM, Meleth S, Bourge RC. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 2006;27:1431–1439. doi: 10.1093/eurheartj/ehi890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Butler J, Forman DE, Abraham WT, Gottlieb SS, Loh E, Massie BM, O’Connor CM, Rich MW, Stevenson LW, Wang Y. Relationship between heart failure treatment and development of worsening renal function among hospitalized patients. Am Heart J. 2004;147:331–338. doi: 10.1016/j.ahj.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 23.Hasselblad V, Stough WG, Shah MR, Lokhnygina Y, O’Connor CM, Califf RM, Adams KF., Jr Relation between dose of loop diuretics and outcomes in a heart failure population: Results of the ESCAPE Trial. Eur J Heart Fail. 2007;9:1064–1069. doi: 10.1016/j.ejheart.2007.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eshaghian S, Horwich TB, Fonarow GC. Relation of Loop Diuretic Dose to Mortality in Advanced Heart Failure. Am J Cardiol. 2006;97:1759–1764. doi: 10.1016/j.amjcard.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 25.Neuberg GW, Miller AB, O’Connor CM, Belkin RN, Carson PE, Cropp AB, Frid DJ, Nye RG, Pressler ML, Wertheimer JH, Packer M. Diuretic resistance predicts mortality in patients with advanced heart failure. Am Heart J. 2002;144:31–38. doi: 10.1067/mhj.2002.123144. [DOI] [PubMed] [Google Scholar]
- 26.Philbin EF, Cotto M, Rocco TA, Jr, Jenkins PL. Association between diuretic use, clinical response, and death in acute heart failure. Am J Cardiol. 1997;80:519–522. doi: 10.1016/s0002-9149(97)00409-8. [DOI] [PubMed] [Google Scholar]
- 27.Mielniczuk LM, Tsang SW, Desai AS, Nohria A, Lewis EF, Fang JC, Baughman KL, Stevenson LW, Givertz MM. The Association Between High-Dose Diuretics and Clinical Stability in Ambulatory Chronic Heart Failure Patients. J Card Fail. 2008;14:388–393. doi: 10.1016/j.cardfail.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 28.Forman DE, Butler J, Wang Y, Abraham WT, O’Connor CM, Gottlieb SS, Loh E, Massie BM, Rich MW, Stevenson LW. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J Am Coll Cardiol. 2004;43:61–67. doi: 10.1016/j.jacc.2003.07.031. [DOI] [PubMed] [Google Scholar]
- 29.McMurray JJ, Teerlink JR, Cotter G, Bourge RC, Cleland JG, Jondeau G, Krum H, Metra M, O’Connor CM, Parker JD, Torre-Amione G, van Veldhuisen DJ, Lewsey J, Frey A, Rainisio M, Kobrin I. Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials. JAMA. 2007;298:2009–2019. doi: 10.1001/jama.298.17.2009. [DOI] [PubMed] [Google Scholar]
- 30.Gheorghiade M, Konstam MA, Burnett JC, Jr, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C for the Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan I. Short-term Clinical Effects of Tolvaptan, an Oral Vasopressin Antagonist, in Patients Hospitalized for Heart Failure: The EVEREST Clinical Status Trials. JAMA: The Journal of the American Medical Association. 2007;297:1332–1343. doi: 10.1001/jama.297.12.1332. [DOI] [PubMed] [Google Scholar]
- 31.Salvator DR, Rey NR, Ramos GC, Punzalan FE. Continuous infusion versus bolus injection of loop diuretics in congestive heart failure. Cochrane Database of Systemic Reviews. 2005;3 doi: 10.1002/14651858.CD003178.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gerlag PG, van Meijel JJ. High-dose furosemide in the treatment of refractory congestive heart failure. Arch Intern Med. 1988;148:286–291. [PubMed] [Google Scholar]
- 33.Wilcox CS, Mitch WE, Kelly RA, Skorecki K, Meyer TW, Friedman PA, Souney PF. Response of the Kidney to Furosemide .1. Effects of Salt Intake and Renal Compensation. Journal of Laboratory and Clinical Medicine. 1983;102:450–458. [PubMed] [Google Scholar]
- 34.Kaissling B, Bachmann S, Kriz W. Structural adaptation of the distal convoluted tubule to prolonged furosemide treatment. American Journal of Physiology. 1985;248:F374–381. doi: 10.1152/ajprenal.1985.248.3.F374. [DOI] [PubMed] [Google Scholar]
- 35.Stevenson LW, Nohria A, Mielniczuk L. Torrent or Torment From the Tubules?: Challenge of the Cardiorenal Connections. J Am Coll Cardiol. 2005;45:2004–2007. doi: 10.1016/j.jacc.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 36.Vanmeyel JJM, Smits P, Dormans T, Gerlag PGG, Russel PGM, Gribnau PWJ. Continuous-Infusion of Furosemide in the Treatment of Patients with Congestive-Heart-Failure and Diuretic Resistance. Journal of Internal Medicine. 1994;235:329–334. doi: 10.1111/j.1365-2796.1994.tb01082.x. [DOI] [PubMed] [Google Scholar]
- 37.Vanmeyel JJM, Smits P, Russel FGM, Gerlag PGG, Tan Y, Gribnau FWJ. Diuretic Efficiency of Furosemide During Continuous Administration Versus Bolus Injection in Healthy-Volunteers. Clinical Pharmacology & Therapeutics. 1992;51:440–444. doi: 10.1038/clpt.1992.44. [DOI] [PubMed] [Google Scholar]
- 38.Rudy DW, Voelker JR, Greene PK, Esparza FA, Brater DC. Loop Diuretics for Chronic Renal-Insufficiency - A Continuous Infusion Is More Efficacious Than Bolus Therapy. Ann Intern Med. 1991;115:360–366. doi: 10.7326/0003-4819-115-5-360. [DOI] [PubMed] [Google Scholar]
- 39.Magovern JA, Magovern GJ. Diuresis in Hemodynamically Compromised Patients - Continuous Furosemide Infusion. Annals of Thoracic Surgery. 1990;50:482–484. doi: 10.1016/0003-4975(90)90505-z. [DOI] [PubMed] [Google Scholar]
- 40.Copeland JG, Campbell DW, Plachetka JR, Salomon NW, Larson DF. Diuresis with Continuous Infusion of Furosemide After Cardiac-Surgery. American Journal of Surgery. 1983;146:796–799. doi: 10.1016/0002-9610(83)90344-6. [DOI] [PubMed] [Google Scholar]
- 41.Lawson DH, Gray JMB, Henry DA, Tilstone WJ. Continuous Infusion of Frusemide in Refractory Edema. British Medical Journal. 1978;2:476–476. doi: 10.1136/bmj.2.6135.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aaser E, Gullestad L, Tollofsrud S, Lundberg J, Hall C, Djoseland O, Kjekshus J, Forfang K. Effect of bolus injection versus continuous infusion of furosemide on diuresis and neurohormonal activation in patients with severe congestive heart failure. Scandinavian Journal of Clinical & Laboratory Investigation. 1997;57:361–367. doi: 10.3109/00365519709099409. [DOI] [PubMed] [Google Scholar]
- 43.Pivac N, Rumboldt Z, Sardelic S, Bagatin J, Polic S, Ljutic D, Naranca M, Capkun V. Diuretic effects of furosemide infusion versus bolus injection in congestive heart failure. International Journal of Clinical Pharmacology Research. 1998;18:121–128. [PubMed] [Google Scholar]
- 44.Dormans TPJ, Vanmeyel JJM, Gerlag PGG, Tan Y, Russel FGM, Smits P. Diuretic efficacy of high dose furosemide in severe heart failure: Bolus injection versus continuous infusion. J Am Coll Cardiol. 1996;28:376–382. doi: 10.1016/0735-1097(96)00161-1. [DOI] [PubMed] [Google Scholar]
- 45.Kramer WG, Smith WB, Ferguson J, Serpas T, Grant AG, Black PK, Brater DC. Pharmacodynamics of torsemide administered as an intravenous injection and as a continuous infusion to patients with congestive heart failure. Journal of Clinical Pharmacology. 1996;36:265–270. doi: 10.1002/j.1552-4604.1996.tb04197.x. [DOI] [PubMed] [Google Scholar]
- 46.Lahav M, Regev A, Raanani P, Theodor E. Intermittent Administration of Furosemide Vs Continuous Infusion Preceded by A Loading Dose for Congestive-Heart-Failure. Chest. 1992;102:725–731. doi: 10.1378/chest.102.3.725. [DOI] [PubMed] [Google Scholar]
- 47.Schuller D, Lynch JP, Fine D. Protocol-guided diuretic management: Comparison of furosemide by continuous infusion and intermittent bolus. Critical Care Medicine. 1997;25:1969–1975. doi: 10.1097/00003246-199712000-00011. [DOI] [PubMed] [Google Scholar]
- 48.Licata G, Di Pasquale P, Parrinello G, Cardinale A, Scandurra A, Follone G, Argano C, Tuttolomondo A, Paterna S. Effects of high-dose furosemide and small-volume hypertonic saline solution infusion in comparison with a high dose of furosemide as bolus in refractory congestive heart failure: Long-term effects. Am Heart J. 2003;145:459–466. doi: 10.1067/mhj.2003.166. [DOI] [PubMed] [Google Scholar]
- 49.Cotter G, Metzkor E, Kaluski E, Faigenberg Z, Miller R, Simovitz A, Shaham O, Marghitay D, Koren M, Blatt A, Moshkovitz Y, Zaidenstein R, Golik A. Randomised trial of high-dose isosorbide dinitrate plus low-dose furosemide versus high-dose furosemide plus low-dose isosorbide dinitrate in severe pulmonary oedema. Lancet. 1998;351:389–393. doi: 10.1016/S0140-6736(97)08417-1. [DOI] [PubMed] [Google Scholar]