Abstract
Context:
Patellofemoral pain syndrome (PFPS) is a common knee condition in athletes. Recently, researchers have indicated that factors proximal to the knee, including hip muscle weakness and motor control impairment, contribute to the development of PFPS. However, no investigators have evaluated eccentric hip muscle function in people with PFPS.
Objective:
To compare the eccentric hip muscle function between females with PFPS and a female control group.
Design:
Cross-sectional study.
Setting:
Musculoskeletal laboratory.
Patients or Other Participants:
Two groups of females were studied: a group with PFPS (n = 10) and a group with no history of lower extremity injury or surgery (n = 10).
Intervention(s):
Eccentric torque of the hip musculature was evaluated on an isokinetic dynamometer.
Main Outcome Measure(s):
Eccentric hip abduction, adduction, and external and internal rotation peak torque were measured and expressed as a percentage of body mass (Nm/kg × 100). We also evaluated eccentric hip adduction to abduction and internal to external rotation torque ratios. The peak torque value of 5 maximal eccentric contractions was used for calculation. Two-tailed, independent-samples t tests were used to compare torque results between groups.
Results:
Participants with PFPS exhibited much lower eccentric hip abduction (t18 = −2.917, P = .008) and adduction (t18 = −2.764, P = .009) peak torque values than did their healthy counterparts. No differences in eccentric hip external (t18 = 0.45, P = .96) or internal (t18 = −0.742, P = .47) rotation peak torque values were detected between the groups. The eccentric hip adduction to abduction torque ratio was much higher in the PFPS group than in the control group (t18 = 2.113, P = .04), but we found no difference in the eccentric hip internal to external rotation torque ratios between the 2 groups (t18 = −0.932, P = .36).
Conclusions:
Participants with PFPS demonstrated lower eccentric hip abduction and adduction peak torque and higher eccentric adduction to abduction torque ratios when compared with control participants. Thus, clinicians should consider eccentric hip abduction strengthening exercises when developing rehabilitation programs for females with PFPS.
Keywords: hip abduction, hip external rotation, torque
Key Points
Females with patellofemoral pain syndrome had a diminished capacity to generate eccentric hip abduction torque compared with healthy females.
External and internal eccentric hip rotator mean peak torque values and the internal to external hip torque ratios were not different between the 2 groups.
Patellofemoral pain syndrome (PFPS) is one of the most common orthopaedic knee conditions encountered in athletes and is more prevalent in female athletes than in male athletes.1,2 The symptom most frequently reported is diffuse peripatellar and retropatellar pain associated with activities that load the patellofemoral joint, such as ascending and descending stairs and squatting and sitting with flexed knees for prolonged periods.3,4 One of the most commonly accepted causes of PFPS is abnormal tracking of the patella within the femoral trochlea. Potential contributing factors that have been studied include vastus medialis oblique insufficiency4; decreased quadriceps,5,6 hamstrings,6 and iliotibial band flexibility7; femoral anteversion3; increased quadriceps angle8,9; and patellar hypermobility.3
Recently, Powers10 suggested that poor hip adduction and internal rotation control during weight-bearing activities is related to PFPS in female athletes. Excessive femoral adduction and internal rotation may increase the dynamic quadriceps angle and lead to greater lateral patellar contact pressure.10 Repetitive movements during functional activities with this misalignment can overload the patellar retinaculum and retropatellar articular cartilage and cause pain.9,11 Powers et al12 demonstrated that during a weight-bearing task, the femur internally rotated underneath the patella in female participants with patellofemoral pain and lateral subluxation of the patella. Increased hip adduction during functional activities has also been reported13,14 in female participants with PFPS. Conversely, greater hip external rotation during walking, squatting, running, and jumping has also been reported13,15 as a possible compensatory mechanism to decrease the quadriceps angle among individuals with PFPS when compared with healthy control participants.
Factors proximal to the knee, including hip muscle weakness, have been shown to contribute to the development of PFPS. Indeed, investigators16–18 have tested hip muscle strength using handheld dynamometers and have demonstrated weaker hip abductor and external rotator muscles in female participants with PFPS than in a control group. One study18 revealed global hip muscle weakness, including weakness in hip flexor, extensor, abductor, and external and internal rotator muscles, in the participants with PFPS. However, the findings of Piva et al6 did not support these results.
Few researchers have focused on the role of hip muscle function in the development of PFPS, and the results of their studies have been inconsistent. In addition, although the hip abductor and external rotator muscles must act eccentrically to control or resist excessive femoral adduction and internal rotation during functional weight-bearing activities,19 no researchers have evaluated eccentric hip muscle function in individuals with PFPS. Furthermore, only Cichanowski et al18 have evaluated the isometric hip adductor and internal rotator muscle function in individuals with PFPS, and no one has evaluated the hip abductor to adductor and external to internal rotator torque ratios in females with PFPS, which could influence control of hip movement during weight-bearing activities.10 Therefore, the purpose of our study was to test for differences between females with PFPS and age-matched female control participants with regard to eccentric hip abduction, adduction, and external and internal rotation torque. We hypothesized that altered external hip muscle rotation function could contribute to internal rotation of the femur underneath the patella, leading to lateral stress on the retropatellar cartilage.
METHODS
Design and Setting
We used a cross-sectional study design to assess differences in eccentric hip muscle function in females with PFPS compared with a control group. Testing was performed at the São Carlos Federal University's musculoskeletal laboratory.
Participants
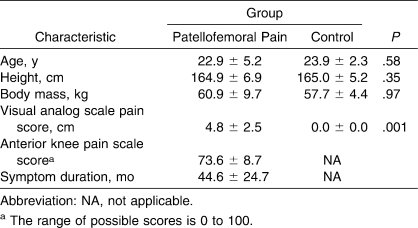
We recruited 10 consecutive female patients with physician-diagnosed PFPS and referral to the physical therapy clinic from the University (Table 1). Ten age-matched, height-matched, and body mass–matched females from the university were recruited to participate in a control group. The females in this control group had no history of knee injury or pain. The participants were aged 17 to 35 years.
Table 1.
Comparisons Between the Patellofemoral Pain Group and the Control Group for Demographic and Clinical Characteristics (Mean ± SD)
The inclusion criteria for the PFPS group were (1) presence of anterior or retropatellar knee pain during at least 3 of the following activities: ascending and descending stairs, squatting, running, kneeling, hopping and jumping, and prolonged sitting; (2) insidious onset of symptoms unrelated to trauma and persistence of symptoms for at least 4 weeks; and (3) presence of pain on palpation of the patellar facets with stepping down from a 25-cm step or during a double-legged squat.4,20
The exclusion criteria for both groups included history of patellar dislocation; surgery involving the patellofemoral joint; or signs or symptoms of meniscal or other intra-articular pathologic conditions, cruciate or collateral ligament involvement, tenderness of the patellar tendon, tenderness of the iliotibial band, tenderness of the pes anserinus tendon, patellar apprehension sign, Osgood-Schlatter or Sinding-Larsen-Johansson syndrome, hip pain, back pain, sacroiliac joint pain, or knee joint effusion.18,20
For each participant, 1 limb was used for comparison between the groups. Measurements of the injured limb were recorded for participants with unilateral pain. The patient's self-reported most-affected side was considered to be the involved side for participants with bilateral symptoms.6 The most-affected side was defined as the side that the patient perceived as being the most painful and limiting during functional activities. The corresponding limb of the matched control participant was tested.6
All participants provided informed consent, and all testing procedures were approved by the São Carlos Federal University Ethics Committee for Human Investigations.
Instruments
Participants rated their usual pain in the week before the study on a 10-cm visual analog scale, with 0 indicating no pain and 10 indicating extremely intense pain. Crossley et al21 demonstrated this procedure to be reliable, valid, and responsive in assessing the outcome in individuals with PFPS.
A self-administered anterior knee pain scale (AKPS) was completed by the participants with PFPS to better describe their knee function. The AKPS is a 13-item questionnaire with a maximum total score of 100, which indicates no disability. This tool is a validated and responsive outcome measure of PFPS treatment.21,22
Eccentric hip abduction, adduction, and external and internal rotation mean peak torque were measured using an isokinetic dynamometer (Biodex Multi-Joint System 2; Biodex Medical Systems, Shirley, NY). The dynamometer was calibrated each day of testing.
Procedures
Before testing, we collected the demographic information, including age, height, body mass, duration of symptoms, and level of physical activity, for each participant. To assess the level of physical activity, we used a standardized questionnaire with items about the frequency, duration, and intensity of any participation in exercises, sports, or physically active hobbies. A physical therapist (T.H.N.) used a standardized physical examination to screen the participants based on the inclusion and exclusion criteria. Next, the participants completed the self-reported measures of pain and function.
Each participant completed a 5-minute submaximal warm-up on a cycle ergometer (Ergo 167 Cycle; Ergo-Fit, Pirmasens, Germany). Next, the familiarization procedures of eccentric hip abduction and adduction and hip external and internal rotation torque tests were conducted in a random order among the participants. If the test began with the eccentric hip abduction and adduction torque test, the participant assumed the side-lying position23 with the nontested hip and knee flexed and fixed with straps. The dynamometer's rotation axis was aligned with a point on the participant representing the intersection of 2 straight lines. One line was directed inferiorly from the posterior-superior iliac spine toward the knee, and the other line was medially directed from the greater trochanter of the femur toward the midline of the body. The lever arm of the dynamometer was attached with straps 5 cm above the superior border of the patella. The hip was placed in a position that was neutrally aligned in all 3 planes. The participants were instructed to keep their toes pointed forward and not to bend their knees to help prevent alterations in muscle recruitment and compensation during testing (Figure 1). The range of motion of the test was from 0° (neutral position) to 30° of hip abduction.
Figure 1.
Participant position for hip abduction and adduction torque measurement.
The participants performed 2 series of 5 submaximal and 1 series of 5 maximal reciprocal eccentric hip adduction and abduction familiarization contractions with a 1-minute rest interval between the 2 series. After a 3-minute rest interval, participants performed 2 sets of 5 repetitions at their maximal eccentric voluntary effort with 3-minute rest intervals between sets. Next, the eccentric hip external and internal rotation familiarization procedures and torque tests were performed. External and internal hip rotation isokinetic eccentric peak torque were measured with the participant seated and the hip and knee flexed to 90°.24 The axis of the dynamometer was aligned with the long axis of the femur (Figure 2). The range of motion of the test was from 0° (neutral position) to 30° of external hip rotation. Oral encouragement was provided during all maximal eccentric hip torque tests. The movements were performed at an angular speed of 30°/s.25 To correct the influence of gravity effect torque on the data, the limb was weighed following the instructions from the dynamometer's operations manual. Test results were automatically corrected in the software for gravity effect torque.
Figure 2.
Participant position for the hip external and internal rotation torque measurement.
We visually analyzed all the repetitions to identify and exclude potential repetitions that could have influenced the mean value. The repetition was excluded if the participant was not able to initiate the movement or to execute the movement through the total range of movement during the eccentric torque test or if the torque value was inferior to 80% of the peak torque values of the last 5 repetitions. We excluded 2 repetitions from the hip abduction torque test, 3 repetitions from the hip external rotation torque test, and 1 repetition from the hip internal rotation torque test based on the criteria described. We used the peak torque value of the last 5 maximal eccentric contractions to calculate the mean peak torque value, but if we excluded a repetition, the mean peak torque value was calculated using the peak torque value from the last 4 repetitions of the test.
We conducted a pilot study following the same protocol to establish intrarater reliability related to the isokinetic eccentric mean peak torque measurements. We also used the peak torque values of the last 5 maximal eccentric contractions to calculate the mean peak torque value. Nine participants were tested on 2 occasions, which were separated by 1 week. The random order of the tests was matched between day 1 and day 2. We used an intraclass correlation coefficient (3,1) [ICC (3,1)] to evaluate intrarater reliability and the SEM to describe the precision of the measurement. The results expressed as ICC (3,1) (SEM) were 0.97 (0.07 Nm/kg) for abduction, 0.78 (0.16 Nm/kg) for adduction, 0.87 (0.07 Nm/kg) for external rotation, and 0.92 (0.11 Nm/kg) for internal rotation.
Statistical Analysis
After the data collection, we determined peak torque values using the Biodex software (Biodex Medical Inc). We compiled the peak torque value of the last 5 maximal eccentric contractions in a Microsoft Excel (version 2003; Microsoft Inc, Redmond, WA) spreadsheet to calculate the eccentric hip abduction, adduction, and internal and external rotation mean peak torque values, which were used in the data analysis and which were normalized against body mass ([Nm/kg] × 100). The eccentric hip adduction to abduction and internal to external rotation torque ratios were calculated using the mean peak torque values.
We used SPSS (version 10.0; SPSS Inc, Chicago, IL) to calculate the 2-tailed, independent-samples t tests for comparing differences in the results of the demographic variables, pain symptoms, eccentric hip mean peak torque normalized to body mass, and eccentric hip torque ratios between the injured (in case of unilateral pain) or the most-affected lower extremity (in case of bilateral pain symptoms) from the PFPS group and the corresponding limb from the control group. The α level was set a priori at .05.
RESULTS
Demographic and clinical characteristics at baseline of the PFPS group and control group are reported in Table 1. The evaluated groups did not differ in their levels of physical activity. Only 5 participants were involved in sports activities or performed regular physical activities: 3 participants from the PFPS group and 2 participants from the control group walked for 30 to 40 minutes, 3 times each week.
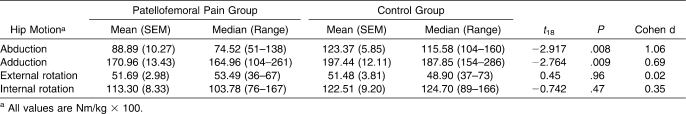
Results of isokinetic eccentric hip torque tests are summarized in Table 2. Participants with PFPS exhibited lower eccentric hip abduction (t18 = −2.917, P = .008) and adduction (t18 = −2.764, P = .009) mean peak torque normalized to body mass values than did their healthy, age-matched counterparts. On average, the PFPS group showed 28% lower eccentric hip abduction torque (88.89 Nm/kg × 100 in the PFPS group versus 123.37 Nm/kg × 100 in the control group) and 14% lower eccentric hip adduction torque (170.96 Nm/kg × 100 in the PFPS group versus 197.44 Nm/kg × 100 in the control group). No difference in the normalized eccentric hip external (t18 = 0.45, P = .96) or internal (t18 = −0.742, P = .47) rotation peak torque was detected between the groups.
Table 2.
Descriptive Data and Comparisons Between the Patellofemoral Pain Group and the Control Group for Eccentric Hip Abduction, Adduction, External Rotation, and Internal Rotation Isokinetic Peak Torque per Body Mass (Nm/kg × 100)
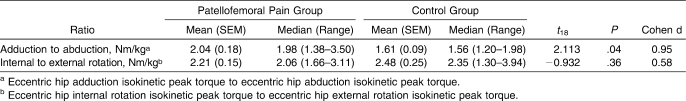
The results of the comparisons between groups for eccentric hip adduction to abduction and internal to external rotation torque ratios are summarized in Table 3. The eccentric hip adduction to abduction torque ratio was higher in the PFPS group (t18 = 2.113, P = .04), but we found no difference in the eccentric hip internal to external rotation torque ratios between the groups (t18 = −0.932, P = .36).
Table 3.
Descriptive Data and Comparisons Between the Patellofemoral Pain Group and the Control Group for Eccentric Hip Adduction to Abduction and Internal to External Rotation Isokinetic Peak Torque Ratios (Nm/kg)
DISCUSSION
The role of hip muscle function in the cause and treatment of patellofemoral pain has received increasing attention in recent years.6,7,13,14,16–18 Although researchers19 have reported that the eccentric demand on hip muscles is greater in women than in men during functional activities, we are not aware of any study in which the investigators have evaluated eccentric hip torque in female patients with PFPS. Therefore, our purpose was to evaluate eccentric hip abduction, adduction, external rotation, and internal rotation isokinetic mean peak torque to compare female participants with PFPS with female control participants.
Our results indicated that eccentric hip abduction mean peak torque was 28% lower in the PFPS group than in the control group. We could not find a study with which to compare our results, but our results are in accordance with the results of previous studies in which investigators evaluated the use of a handheld dynamometer and compared the isometric hip abduction strength between participants with PFPS and control participants. Ireland et al,16 Robinson and Nee,17 and Cichanowski et al18 reported reductions of 26% (23% body mass in the PFPS group versus 31% body mass in the control group), 27% (16% body mass in the PFPS group versus 22% body mass in the control group), and 27% (37% body mass in the PFPS group versus 29% body mass in the control group), respectively, in hip abduction strength in female participants with PFPS compared with sex-matched control participants. In addition, few researchers have evaluated the eccentric hip torque in healthy participants. Claiborne et al26 demonstrated that young, healthy women presented eccentric hip abduction and adduction torque at 60°/s (128% and 143% of body mass, respectively) that was similar to our results. Although we and previous authors have demonstrated a relationship between diminished hip abduction muscle strength and PFPS, it is still unclear if this deficit in hip muscle strength is related to alterations in the lower extremity kinematics leading to increased hip adduction during functional weight-bearing activities and increased lateral patellar tracking, as previously suggested.27 Dierks et al28 compared hip abduction and external rotation isometric strength measurements and lower extremity kinematic data before and after recreational runners with PFPS and matched uninjured runners completed a prolonged run. The authors concluded that runners with PFPS displayed weaker hip abductor muscles that were associated with increased hip adduction during running, especially at the end of the run. Conversely, Bolgla et al29 evaluated isometric hip abductor and external rotator muscle strength and hip and knee kinematics during a stair-stepping task in female participants with PFPS and matched control participants. The authors reported a diminished capacity to generate hip abductor and external rotator torque in the female participants with PFPS, but they reported no between-groups differences for the hip and knee transverse-plane and frontal-plane angles during stair descent. In addition, recent evidence30,31 has not shown a relationship between hip muscle weakness and lower extremity kinematics in healthy populations. Thus, our findings demonstrated a diminished capacity to generate eccentric hip abduction torque in females with PFPS, but more studies are needed to investigate the role of this deficit in participants with PFPS.
In our study, the patients with PFPS also showed a 14% lower eccentric hip adduction mean peak torque compared with the control participants (170.96 Nm/kg × 100 in the PFPS group versus 197.44 Nm/kg × 100 in the control group). The diminished eccentric hip abduction and adduction mean peak torque values reported for the PFPS group could not be considered to be an effect of a low level of physical activity associated with a prolonged duration of the symptoms (42 months), because in our study, both groups had similar levels of physical activity, and the relative hip abductor torque deficit was greater than the hip adductor torque deficit in the PFPS group, with a 21% greater eccentric adduction to abduction torque ratio in the PFPS group (mean = 2.04) than in the control group (mean = 1.61). Cichanowski et al18 reported that collegiate female athletes with patellofemoral pain exhibited global weakness in the hip muscle groups, except for the hip adductor muscles, when compared with a control group. They also showed that only the hip abductor and external rotator muscles were much weaker when the injured and uninjured legs in athletes with PFPS were compared. Tyler et al7 related that patients with unilateral PFPS demonstrated weakness on the involved side in hip flexion and hip abduction but not in hip adduction. Thus, we believe that although participants with PFPS may present a generalized deficit in hip muscle function, hip abduction torque deficit may play a more important role in PFPS than current research has indicated.
As noted, Powers et al12 demonstrated that during a weight-bearing task, the femur rotated internally underneath the patella in female participants with PFPS and lateral subluxation of the patella. Thus, we hypothesized that an altered external hip muscle rotation function could contribute to internal rotation of the femur underneath the patella, leading to lateral stress on the retropatellar cartilage. We found no difference in the external and internal eccentric hip rotator mean peak torque or the internal to external hip torque ratios between the PFPS group and the control group. Our results correspond with those of Piva et al,6 who reported no differences in isometric hip external rotation strength, but they do not correspond with the results of other authors16–18 who reported diminished isometric external hip muscle strength in participants with PFPS. According to Crossley et al,21 a score of 70 on the AKPS and a rating of 6 cm on a visual analogue scale imply a moderate amount of pain and disability. Based on this information, our PFPS group experienced a mild amount of pain and disability, which may explain the lack of difference in the hip rotation torque between the evaluated groups in our study. Although we did not assess kinematic variables, it is relevant to highlight the research of Powers et al,15 who evaluated 3-dimensional kinematics of the foot, tibia, and femur during self-selected free-walking trials in female participants with PFPS and in female participants without PFPS. Their PFPS group demonstrated less internal femoral rotation compared with the control group. In addition, Wilson and Davis13 evaluated the 3-dimensional lower extremity mechanics of female participants with PFPS and of healthy female control participants during single-leg squats, running, and repetitive single-leg jumps. The PFPS group performed all 3 activities with 4.3° greater knee external rotation, 3.5° greater hip adduction, and 3.9° less hip internal rotation than the control group. The finding of decreased internal rotation in the PFPS group in these studies13,15 indicates that this motion may be a compensatory strategy to reduce the quadriceps angle during the weight-bearing functional tasks. Thus, our results did not support the hypothesis that hip external rotation muscle weakness contributes to PFPS. Future researchers need to investigate if the capacity to generate eccentric hip external or internal torque is associated with the kinematic and kinetic variables during functional activities in individuals with PFPS.
Because we used a cross-sectional design, we do not know whether PFPS caused the reduced eccentric hip abduction and adduction torque, or vice versa. Leetun et al27 prospectively evaluated hip muscle strength as a risk factor for lower extremity injury in athletes. The authors reported that athletes who sustained no injuries during the athletic season had much stronger hip abduction and external rotation and stated that hip external rotator strength was a predictor of lower extremity injuries in collegiate athletes. The difference between our results and the results of Leetun et al27 may reflect our use of a nonathletic sample, or this difference may be due to methodologic differences in assessing hip musculature, as we evaluated the eccentric hip muscle torque using an isokinetic dynamometer and Leetun et al27 evaluated isometric contraction using a handheld dynamometer. Thus, future study with an athletic population is needed to determine if females with PFPS have a diminished capacity to generate eccentric hip torque compared with healthy females.
Future investigation is also needed to study the relationship between eccentric hip torque and hip and knee kinematics in individuals with PFPS and to better understand if adding exercises that address the eccentric hip mean peak torque deficits in female participants with PFPS improves pain symptoms and functional level. Researchers7,14 who have included hip muscle strengthening in the treatment of PFPS have obtained successful results; however, more clinical studies are necessary to determine which muscle group should be addressed and whether eccentric, concentric, isometric strengthening, or endurance exercises would be more efficient for improving pain symptoms, especially during functional activities, in the rehabilitation program for patients with PFPS.
CONCLUSIONS
Female participants with PFPS showed reduced maximal eccentric hip abduction and adduction torque and an increased eccentric adduction to abduction torque ratio compared with control participants. The diminished capacity to generate eccentric hip abduction torque may lead to an impaired capacity to prevent excessive femoral adduction during repetitive functional activities, causing excessive lateral stress on the patellofemoral joint. Thus, clinicians should assess the strength of hip muscles, preferably using eccentric isokinetic testing, and should include eccentric strengthening exercises for the hip as part of PFPS rehabilitation programs for females.
Acknowledgments
Financial support of this study was received from the National Council for Scientific and Technological Development, Brasília, Brazil, and the São Paulo State Research Foundation, São Paulo, Brazil.
Footnotes
Rodrigo de Marche Baldon, PT; Theresa Helissa Nakagawa, PT; and Thiago Batista Muniz, PT, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. César Ferreira Amorim, PhD, and Carlos Dias Maciel, PhD, contributed to analysis and interpretation of the data and critical revision and final approval of the article. Fábio Viadanna Serrão, PhD, contributed to conception and design; acquisition and analysis and interpretation of the data; and critical revision and final approval of the article.
REFERENCES
- 1.Taunton J. E., Ryan M. B., Clement D. B., McKenzie D. C., Lloyd-Smith D. R., Zumbo B. D. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36(2):95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tumia N., Maffulli N. Patellofemoral pain in female athletes. Sports Med Arthrosc Rev. 2002;10(10):69–75. [Google Scholar]
- 3.Fulkerson J. P. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30(3):447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 4.Cowan S. M., Bennell K. L., Crossley K. M., Hodges P. W., McConnell J. Physical therapy alters recruitment of the vasti in patellofemoral pain syndrome. Med Sci Sports Exerc. 2002;34(12):1879–1885. doi: 10.1097/00005768-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Witvrouw E., Lysens R., Bellemans J., Cambier D., Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population: a two-year prospective study. Am J Sports Med. 2000;28(4):480–489. doi: 10.1177/03635465000280040701. [DOI] [PubMed] [Google Scholar]
- 6.Piva S. R., Goodnite E. A., Childs J. D. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35(12):793–801. doi: 10.2519/jospt.2005.35.12.793. [DOI] [PubMed] [Google Scholar]
- 7.Tyler T. F., Nicholas S. J., Mullaney M. J., McHugh M. P. The role of hip muscle function in the treatment of patellofemoral pain syndrome. Am J Sports Med. 2006;34(4):630–636. doi: 10.1177/0363546505281808. [DOI] [PubMed] [Google Scholar]
- 8.Mizuno Y., Kumagai M., Mattessich S. M., et al. Q-angle influences tibiofemoral and patellofemoral kinematics. J Orthop Res. 2001;19(5):834–840. doi: 10.1016/S0736-0266(01)00008-0. [DOI] [PubMed] [Google Scholar]
- 9.Huberti H. H., Hayes W. C. Patellofemoral contact pressures: the influence of Q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66(5):715–724. [PubMed] [Google Scholar]
- 10.Powers C. M. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- 11.Lee T. Q., Morris G. M., Csintalan R. P. The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports Phys Ther. 2003;33(11):686–693. doi: 10.2519/jospt.2003.33.11.686. [DOI] [PubMed] [Google Scholar]
- 12.Powers C. M., Ward S. R., Fredericson M., Guillet M., Shellock F. G. Patellofemoral kinematics during weight-bearing and non–weight-bearing knee extension in persons with lateral subluxation of the patella: a preliminary study. J Orthop Sports Phys Ther. 2003;33(11):677–685. doi: 10.2519/jospt.2003.33.11.677. [DOI] [PubMed] [Google Scholar]
- 13.Wilson J. D., Davis I. S. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech (Bristol, Avon) 2008;23(2):203–211. doi: 10.1016/j.clinbiomech.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 14.Mascal C. L., Landel R., Powers C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J Orthop Sports Phys Ther. 2003;33(11):647–660. doi: 10.2519/jospt.2003.33.11.647. [DOI] [PubMed] [Google Scholar]
- 15.Powers C. M., Chen P. Y., Reischl S. F., Perry J. Comparison of foot pronation and lower extremity rotation in persons with and without patellofemoral pain. Foot Ankle Int. 2002;23(7):634–640. doi: 10.1177/107110070202300709. [DOI] [PubMed] [Google Scholar]
- 16.Ireland M. L., Willson J. D., Ballantine B. T., Davis I. M. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33(11):671–676. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- 17.Robinson R. L., Nee R. J. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37(5):232–238. doi: 10.2519/jospt.2007.2439. [DOI] [PubMed] [Google Scholar]
- 18.Cichanowski H. R., Schmitt J. S., Johnson R. J., Niemuth P. E. Hip strength in collegiate female athletes with patellofemoral pain. Med Sci Sports Exerc. 2007;39(8):1227–1232. doi: 10.1249/mss.0b013e3180601109. [DOI] [PubMed] [Google Scholar]
- 19.Ferber R., Davis I. M., Williams D. S., III Gender differences in lower extremity mechanics during running. Clin Biomech (Bristol, Avon) 2003;18(4):350–357. doi: 10.1016/s0268-0033(03)00025-1. [DOI] [PubMed] [Google Scholar]
- 20.Crossley K., Bennell K., Green S., Cowan S., McConnell J. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med. 2002;30(6):857–865. doi: 10.1177/03635465020300061701. [DOI] [PubMed] [Google Scholar]
- 21.Crossley K. M., Bennell K. L., Cowan S. M., Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85(5):815–822. doi: 10.1016/s0003-9993(03)00613-0. [DOI] [PubMed] [Google Scholar]
- 22.Kujala U. M., Jaakkola L. H., Koskinen S. K., Taimela S., Hurme M., Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 23.Burnett C. N., Betts E. F., King W. M. Reliability of isokinetic measurements of hip muscle torque in young boys. Phys Ther. 1990;70(4):244–249. doi: 10.1093/ptj/70.4.244. [DOI] [PubMed] [Google Scholar]
- 24.Lindsay D. M., Maitland M. E., Lowe R. C., Kane T. J. Comparison of isokinetic internal and external rotation torque using different testing position. J Orthop Sports Phys Ther. 1992;16(1):43–50. doi: 10.2519/jospt.1992.16.1.43. [DOI] [PubMed] [Google Scholar]
- 25.Donatelli R., Catlin P. A., Backer G. S., Drane D. L., Slater S. M. Isokinetic hip abductor to adductor torque ratio in normals. Isokinet Exerc Sci. 1991;1(2):103–111. [Google Scholar]
- 26.Claiborne T. L., Armstrong C. W., Gandhi V., Pincivero D. M. Relationship between hip and knee strength and knee valgus during single leg squat. J Appl Biomech. 2006;22(1):41–50. doi: 10.1123/jab.22.1.41. [DOI] [PubMed] [Google Scholar]
- 27.Leetun D. T., Ireland M. L., Willson J. D., Ballantyne B. T., Davis I. M. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36(6):926–934. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- 28.Dierks T. A., Manal K. T., Hamill J., Davis I. S. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during a prolonged run. J Orthop Sports Phys Ther. 2008;38(8):448–456. doi: 10.2519/jospt.2008.2490. [DOI] [PubMed] [Google Scholar]
- 29.Bolgla L. A., Malone T. R., Umberger B. R., Uhl T. L. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38(1):12–18. doi: 10.2519/jospt.2008.2462. [DOI] [PubMed] [Google Scholar]
- 30.Lawrence R. K., III, Kernozek T. W., Miller E. J., Torry M. R., Reuteman P. Influences of hip external rotation strength on knee mechanics during single-leg drop landings in females. Clin Biomech (Bristol, Avon) 2008;23(6):806–813. doi: 10.1016/j.clinbiomech.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 31.Mizner R. L., Kawaguchi J. K., Chmielewski T. L. Muscle strength in the lower extremity does not predict postinstruction improvements in the landing patterns of female athletes. J Orthop Sports Phys Ther. 2008;38(6):353–361. doi: 10.2519/jospt.2008.2726. [DOI] [PubMed] [Google Scholar]