Abstract
Context:
The relationship between lower extremity alignment and lower extremity injury risk remains poorly understood, perhaps because most authors have examined only individual or a select group of alignment variables. Examining the relationships among alignment variables may allow us to more accurately describe lower extremity posture and clarify the relationship between lower extremity alignment and injury risk in future studies.
Objective:
To measure lower extremity alignment variables and examine whether relationships could be identified among these variables.
Design:
Observational study.
Setting:
Laboratory.
Patients or Other Participants:
Two hundred eighteen (102 males: age = 23.1 ± 3.2 years, height = 177.3 ± 8.4 cm, mass = 80.8 ± 13.0 kg; 116 females: age = 21.8 ± 2.7 years, height = 163.5 ± 7.4 cm, mass = 63.4 ± 12.4 kg) healthy, college-aged participants.
Main Outcome Measure(s):
We measured pelvic angle, femoral anteversion, quadriceps angle, tibiofemoral angle, genu recurvatum, and tibial torsion to the nearest degree and navicular drop to the nearest millimeter on the right and left lower extremities. Separate principal components factor analyses were performed for each sex and side (left, right).
Results:
A distinct lower extremity factor was identified, with relationships observed among increased pelvic angle, increased quadriceps angle, and increased tibiofemoral angle. A second distinct lower extremity factor was identified, with relationships observed among increased supine genu recurvatum, decreased tibial torsion, and increased navicular drop. Femoral anteversion loaded as an independent third factor. These distinct lower extremity alignment factors were consistent across side and sex.
Conclusions:
Factor analysis identified 3 distinct lower extremity alignment factors that describe the potential interactions among lower extremity alignment variables. Future authors should examine how these collective alignment variables, both independently and in combination, influence dynamic knee function and risk for lower extremity injuries.
Keywords: postural relationships, risk factor assessment
Key Points
In healthy, college-aged participants, using a factor analysis approach, the measured alignment variables yielded 3 lower extremity alignment factors: valgus alignment (greater anterior pelvic, quadriceps, and tibiofemoral angles), pronated alignment (greater genu recurvatum and navicular drop and less outward tibial torsion), and femoral anteversion.
The observed factors accounted for only approximately 60% of the total variance in lower extremity alignment variables. Therefore, more research is needed to examine other anatomical and alignment factors (eg, joint surface geometry, differences in soft tissue structures) that may account for the remaining variance.
Lower extremity alignment has been proposed as a risk factor for acute and chronic lower extremity injuries, including patellofemoral syndrome,1–3 anterior cruciate ligament injuries,4–7 medial tibial stress syndrome,8 stress fractures, and plantar fasciitis.8 It has been suggested that biomechanical changes resulting from abnormal alignment may influence joint loads, mechanical efficiency of muscles, and proprioceptive orientation and feedback from the hip and knee, resulting in altered neuromuscular function and control of the lower extremities.4,9,10 However, the relationship between anatomical alignment and injury risk remains poorly understood. Most investigators have examined only one alignment factor or a small number of alignment factors. Given the potential interdependence of various alignment faults along the lower kinetic chain,4–7,11 examining only one or a limited number of alignment factors may not adequately describe the position of the lower extremity, providing insufficient information to identify clinically meaningful relationships.
Accounting for the alignment of the entire lower extremity, rather than a single segment, may more accurately describe the relationship between anatomic alignment and the risk of lower extremity injury, because one alignment characteristic may interact with or cause compensations at other bony segments.4,12 The potential for an interactive effect among alignment characteristics is illustrated by a study10 evaluating the independent and combined effects of excessive quadriceps angle and navicular drop on neuromuscular timing and amplitude of the lower extremity muscles in response to postural perturbations. Participants classified as having above-average navicular drop and quadriceps angles exhibited very different neuromuscular responses (ie, amplitude and reflex time of the thigh musculature), depending on whether one or both of these alignment characteristics was present. The potential for the interaction of alignment variables to affect dynamic knee function10 and predict the likelihood of suffering lower extremity injuries4–6 reinforces the need to take a more comprehensive approach if we are to fully understand the relationships among lower extremity alignment, dynamic lower extremity function, and risk of injury.
The potential interactions among lower extremity alignment variables have been previously described as either “correlated” or “compensatory” postures by Riegger-Krugh and Keysor.13 These postures were suggested to result from several factors, such as deviations in skeletal alignment (eg, when the position of one segment depends on the position of an adjacent segment) and changes toward efficient dynamic function (eg, when positioning of the limb is altered to improve neuromechanical efficiency). In an effort to account for the potential interactions among lower extremity alignment variables in future studies, our purpose was to measure several lower extremity alignment variables and determine whether distinct relationships among the variables could be identified. Using a factor analysis approach, our expectation was that many of the alignment characteristics would be associated with one another and would collectively describe one or more lower extremity alignment factors.
METHODS
Seven anatomic alignment characteristics were measured on the right and left pelvis and lower extremities of 218 volunteers (102 males: age = 23.1 ± 3.2 years, height = 177.3 ± 8.4 cm, mass = 80.8 ± 13.0 kg; 116 females: age = 21.8 ± 2.7 years, height = 163.5 ± 7.4 cm, mass = 63.4 ± 12.4 kg). Participants were predominantly college-aged students and had no current injury to the lower extremities or any previous history that would affect the alignment or motion of the lower extremity joints (eg, fractures or surgery). The population reflected a combined sample of 100 volunteers (50 males, 50 females) from previous studies14,15 in which we examined sex differences and bilateral asymmetries in lower extremity alignment and current volunteers in an ongoing project examining the effects of hormone-mediated knee laxity on knee stability (52 males, 76 females). Participants read and signed a consent form approved by the university's Institutional Review Board for protection of human subjects before data collection began.
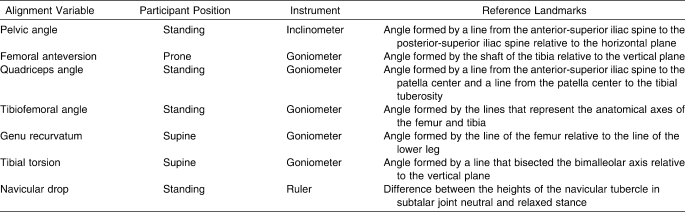
Demographics of age, height, and mass were recorded for each volunteer. With the exception of genu recurvatum (see description below), all variables were measured using identical measurement techniques across the 2 samples and have been previously described in detail.14,16,17 These lower extremity alignment characteristics were based on commonly identified variables suggested to potentially influence dynamic motion and the risk of lower extremity injuries. Pelvic angle was measured in bilateral stance and represented the angle formed by a line from the anterior-superior iliac spine to the posterior-superior iliac spine relative to the horizontal plane using an inclinometer. Femoral anteversion was measured using the Craig test with the participant prone and the knee flexed to 90°; the angle between the true vertical and the shaft of the tibia was measured using a standard goniometer. Quadriceps angle was measured in bilateral stance and represented the angle formed by a line from the anterior-superior iliac spine to the patella center and a line from the patella center to the tibial tuberosity using a standard goniometer. Tibiofemoral angle was measured in bilateral stance and represented the angle formed by the anatomical axis of the femur and tibia in the frontal plane using a standard goniometer. Genu recurvatum represented the sagittal-plane alignment of the femur and tibia, measured in a non–weight-bearing, supine position with a bolster under the distal tibia. In the first 100 participants, the measurement was recorded while the examiner applied a posteriorly directed force to the anterior knee until passive resistance was noted.14 In the later 118 volunteers, the measurement was recorded while the individual actively and maximally extended the knee. We have previously reported that this change in procedure resulted in no systematic differences in the measure (4.6° ± 5.6° versus 4.5° ± 5.7°, intraclass correlation coefficient [2,3] = 0.97, SEM = 1.0°).18 Tibial torsion was measured supine with the femur positioned so that a line between the epicondyles was parallel to the horizontal plane. The angle between the true vertical and a line bisecting the bimalleolar axis was measured using a standard goniometer and represented the magnitude of torsion of the distal tibia. Navicular drop was measured in bilateral stance and recorded as the difference between the height of the navicular in subtalar joint neutral (position in which the medial and lateral aspects of the talar head were equally palpable on both sides) and a relaxed stance measured with a ruler. A summary of these measurement methods is provided in Table 1. All measurement procedures were performed by a single examiner who had previously established good to excellent measurement consistency on all measures (intraclass correlation coefficient [2,3] ≥ 0.87) based on repeated measures taken on 15 to 16 participants on 2 separate days using identical equipment and measurement methods.14,16,18 All standing measures were taken in a standardized stance, with the left and right feet spaced equal to the width of the left and right acromial processes and toes facing forward. The stance was achieved by instructing participants to march in place and then take a step forward. They were instructed to look straight ahead during all standing measures with equal weight over both feet. Each measure was repeated 3 times.
Table 1.
Alignment Measurement Methods
Data Reduction and Statistical Analysis
For each measurement variable and side, 3 measurements were taken and averaged for analysis. Independent-samples t tests were performed for the right and left alignment characteristics to examine sex differences. Although we have previously reported on these sex differences in a smaller sample,14 we felt it was important to confirm these sex differences in the current sample to support our rationale for examining these relationships in males and females separately. Separate exploratory principal components factor analyses with an orthogonal (varimax) rotation were performed for the right and left lower extremities of both males and females and used to reduce the static alignment variables into unique lower extremity factors. Factor analysis is a type of multivariate analysis that allows us to effectively examine the relationships among individual items (eg, lower extremity alignment variables) and effectively group them to describe a reduced number of independent factors.19 This process allows us to account for the maximum possible amount of the variance of the variables while still maximizing the retention of each variable's unique information.19 The strength of the relationship among variables for each factor is known as the factor loading (α) and represents the correlation between the variables and the factor. The number of meaningful factors was determined by accepting factors for which the calculated eigenvalues (characteristic roots that represent the sum of the squared loadings on the principal factor represented by λ) are equal to or greater than 1.19 An orthogonal rotation was performed to establish a simpler relationship between the factors and the variables to achieve simple structure, parsimony, and meaningful clinical interpretation.19
RESULTS
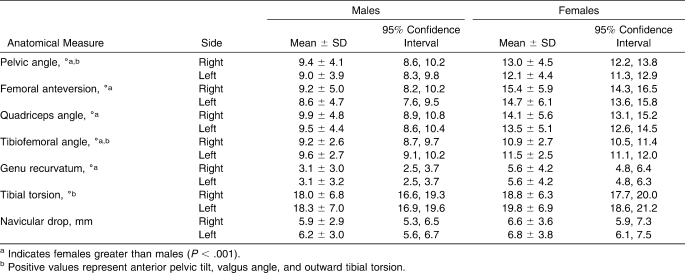
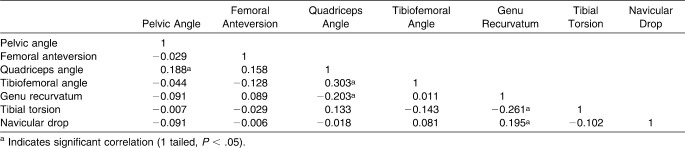
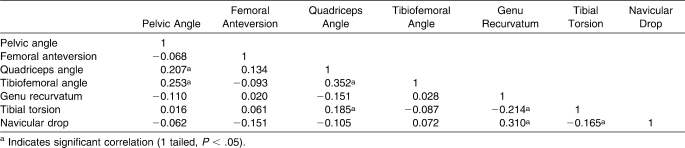
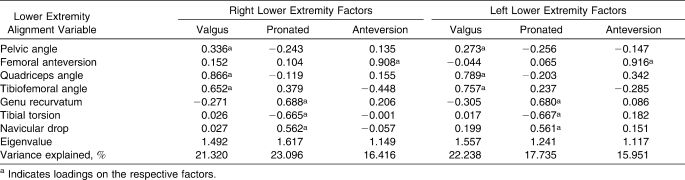
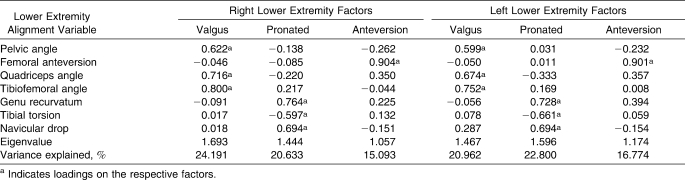
For both the right and left lower extremities, females had greater mean values than males for pelvic angle, femoral anteversion, quadriceps angle, tibiofemoral angle, and genu recurvatum (P < .001; Table 2). Males and females were not different on navicular drop (P ≥ .100) or tibial torsion (P ≥ .117). Thus, the sex differences observed in pelvis, hip, and knee alignment in a subsample of these data14 still hold with the addition of 118 more participants (100 versus 218 participants). Correlation matrices used for the analyses of the right lower extremity (which were similar to the left lower extremity) for males and females are presented in Tables 3 and 4, respectively. Rotated factor loadings for each factor by sex and side are presented in Tables 5 and 6. Three distinct factors with eigenvalues of λ = 1.1 to 1.7 were identified and were consistent for both the right and left extremities and between the sexes. Pelvic angle, quadriceps angle, and tibiofemoral angle positively loaded (greater anterior pelvic tilt, quadriceps angle, and knee valgus angles) on 1 factor and accounted for 21.0% to 24.2% of the total variance in lower extremity alignment variables. Genu recurvatum, tibial torsion, and navicular drop loaded on a second factor and accounted for 17.7% to 22.8% of the total variance in lower extremity alignment variables (positive loadings indicating greater genu recurvatum and navicular drop, negative loading indicating decreased outward torsion). Femoral anteversion was not related to the other anatomic alignment characteristics and loaded as an independent third factor, accounting for 15.1% to 16.8% of the variance in lower extremity alignment. Together, these 3 factors accounted for 59.9% and 60.5% of the total variance in lower extremity alignment variables for males and 56.6% and 55.9% for females, for the right and left sides, respectively.
Table 2.
Lower Extremity Alignment Characteristics
Table 3.
Correlation Matrix for Right Lower Extremity Alignment in Males
Table 4.
Correlation Matrix for Right Lower Extremity Alignment in Females
Table 5.
Male Rotated Factor Loadings (α) Following Principal Components Analysis
Table 6.
Female Rotated Factor Loadings (α) Following Principal Components Analysis
DISCUSSION
Using a factor analysis approach, our primary finding was that the measured alignment variables yielded 3 distinct lower extremity alignment factors. One factor identified a relative valgus alignment characterized by positive relationships among greater anterior pelvic angle, quadriceps angle, and tibiofemoral angle. This factor was independent of a pronated alignment factor characterized by relationships among greater genu recurvatum, navicular drop, and decreased outward torsion of the tibia. Clinical measures of femoral anteversion were not related to the other anatomic alignment characteristics and loaded as a separate third factor. Females had greater values than males in the alignment characteristics of the pelvis, hip, and knees, confirming our previous findings.14 This would suggest that the identified valgus alignment factor and femoral anteversion were more pronounced in females than in males. As previously described by Riegger-Krugh and Keysor,13 the relationships among alignment characteristics can be structural or functional in nature, with the position of one segment depending on alignment deviations of an adjacent segment or resulting from compensatory changes toward more efficient dynamic function. As all individuals are known to be different in structure, the positioning of adjacent segments in response to a specific alignment difference would also be unique to that individual, likely explaining the somewhat low correlation values presented in Tables 3 and 4. The following discussion will explore the potential relationships among the alignment characteristics respective to the identified factors and consider their clinical implications on dynamic lower extremity motion.
Valgus Alignment Factor
Clinical expertise and observation suggest that excessive anterior tilt of the pelvis is associated with alignment changes in the lower kinetic chain, specifically hip internal rotation, genu valgus, and genu recurvatum.20,21 Our findings partially support this collective posture at the pelvis and knees, identifying a factor by which participants who had greater pelvic angles also had greater quadriceps and tibiofemoral angles. The relationship between pelvic angle and frontal-plane knee angles (ie, quadriceps and tibiofemoral angles) may reflect an interaction between the pelvis and femur. When measured in a weight-bearing position (as is the case with the current study), increased pelvic tilt has been associated with internal rotation at the hip.22 This associated hip internal rotation could be further related to transverse-plane and frontal-plane knee angles by changing the spatial orientation of the anatomical landmarks used for these measurements. For example, this resultant hip internal rotation would effectively displace the anatomical axes of the femur into adduction and the tibia into abduction, thereby increasing the tibiofemoral angle. Further, abnormal gait patterns resulting from increased hip internal rotation can also indirectly lead to compensations in other parts of the lower extremity, such as a compensatory external rotation of the tibia on the femur,23 which in turn would position the tibial tuberosity more laterally, resulting in an increased quadriceps angle. Finally, a combination of greater pelvic angle (with associated hip internal rotation), knee valgus (movement of the patella medially relative to the anterior-superior iliac spine and tibial tubercle), and external rotation of the tibia on the femur (movement of the tibial tubercle laterally) would result in an increase in quadriceps angle.21,24,25
Although excessive quadriceps angle has been proposed to increase the risk of lower extremity injuries, particularly those at the knee, few researchers have directly examined this relationship.1–7 As previously mentioned, greater quadriceps angle may result from movement of the patella medially or movement of the tibial tuberosity laterally (or both) with greater tibiofemoral angle and femoral internal rotation21,24 (which may result from an increased pelvic angle, changing the orientation of the acetabulum22). Given the identified relationships between these variables and the potential for any one of these variables to differentially influence the quadriceps angle, independently examining the quadriceps angle for its effects on lower extremity motion may not be sufficient to identify individuals at risk for lower extremity injury. This concept further supports the need to consider the collective influence of lower extremity alignment variables, rather than examining alignment variables in isolation.
Pronated Alignment Factor
When considering the potential relationship between lower extremity alignment and lower extremity injuries, we cannot ignore the fact that subtalar joint pronation is the lower extremity alignment variable most commonly linked to lower extremity injuries. It is also important to understand that the predictive strength of this variable on knee injuries is notably greater when examined in combination with genu recurvatum,4 suggesting an association between these alignment characteristics. Our findings support an interactive effect between the knee and foot pronation, as we observed that volunteers with greater genu recurvatum also had greater navicular drop. Greater genu recurvatum is often considered a postural deviation in the sagittal plane, but evidence from a magnetic resonance imaging study suggests that rotational motion also occurs at the tibiofemoral joint as the knee moves from hyperextension to flexion.26 Specifically, genu recurvatum results in medial femoral rotation relative to the tibia as the lateral femoral condyle moves anteriorly relative to the tibia to a greater extent than the medial femoral condyle. This associated medially rotated posture at the knee may increase medial rotational stress at the foot, resulting in greater pronation, a triplanar deviation described as eversion of the calcaneus, adduction, and plantar flexion of the talus and abduction of the forefoot.27 These known kinematics of the tibiofemoral joint may explain the positive relationships we noted between greater genu recurvatum (with the associated medial rotation of the femur) and navicular drop.
Another plausible explanation for the association between greater genu recurvatum and greater navicular drop is that these measures may represent joint hypermobility. To examine whether a relationship exists between these variables and hypermobility, we ran an exploratory analysis on a subset of these data in which we had also assessed general joint laxity using the Beighton and Horan Joint Mobility Index28 (n = 103: 45 males, 58 females). This model scores the laxity at 5 joints (fifth finger, thumb, elbow, knee, and forward flexion of the trunk) and has been used to indicate the magnitude of general joint laxity as a measure of joint hypermobility. In females, the correlations with generalized joint laxity were low for both genu recurvatum (Pearson product moment correlation coefficient [r] [left, right]: 0.175, 0.251, P > .05) and navicular drop (−0.31, −0.044, P > .05). These low correlations were also consistent in males for measures of genu recurvatum (0.166, 0.252, P > .05) and navicular drop (0.073, 0.078, P > .05). Therefore, the relationship between greater genu recurvatum and greater navicular drop does not appear to be simply an issue of joint hypermobility.
A limitation of the study was that genu recurvatum was measured in a non–weight-bearing position, whereas navicular drop was measured in bilateral stance. However, we believe that the observed relationship between these alignment characteristics would likely be similar if genu recurvatum were measured in a weight-bearing position. Using similar measurement techniques to ours (active maximal knee extension) but with the limb in a weight-bearing position, Trimble et al29 obtained very similar mean values of genu recurvatum (in both males and females). It is not known, however, whether the interaction at the tibiofemoral joint would be similar in a weight-bearing versus a non–weight-bearing position. Further work is needed to confirm that measures and tibiofemoral joint motions are indeed consistent across non–weight-bearing and weight-bearing conditions.
Along with the observed relationship between greater genu recurvatum and greater navicular drop, this pronated alignment factor was also characterized by decreased tibial torsion. Tibial torsion is considered a bony alignment defined as the twist of the tibia around the longitudinal axis in the transverse plane and often describes the magnitude of outward (external) torsion.30 It has been reported31 that inward (internal) torsion is present at birth and gradually transitions toward outward torsion throughout adolescence. Consistent with our findings, the lack of transition to outward torsion has been suggested to be associated with subtalar joint pronation.32,33 Specifically, a lack of outward torsion of the tibia is thought to cause an “in-toeing” gait, which the individual compensates for by abducting the foot at the subtalar joint (pronated position) to achieve a more normal, straight-ahead position.32
The association observed among these 3 variables (greater genu recurvatum, decreased outward torsion of the tibia, and greater navicular drop) could potentially combine in weight bearing to define a pronated posture. The association among these variables in weight bearing has been previously described by Kendall et al34 as knee hyperextension occurring with medial rotation of the femur and pronation of the feet. Although the orientation of the tibia was not specifically identified, the illustrations describing this lower extremity posture suggest an inward torsion (or rotation) of the tibia. This relationship is largely based on clinical observation; the current study is the first, to our knowledge, to examine the relationship among genu recurvatum, torsion of the tibia, and measures of pronation. Further work is needed to understand the association in full weight bearing between rotational alignment of the tibia and alignment at the foot and ankle and whether these associations are influenced by differences in knee hyperextension. Further work is also needed to examine the relationship among measures of pronation and other alignment characteristics during dynamic motion, as we assessed navicular drop in a bilateral, static position.
Femoral Anteversion
We observed that clinical measures of femoral anteversion were not related to the other alignment characteristics and loaded as a separate third factor. A relationship between greater femoral anteversion and other lower extremity alignment variables has not been reported, yet the most common problem associated with increased anteversion is an in-toeing gait.35 However, an in-toeing gait would result only if no compensatory postural changes occurred at the other joints of the lower extremity, in particular at the knee. In fact, it has been suggested that a postural consequence of femoral anteversion is external rotation of the tibia on the femur, potentially contributing to an increased quadriceps angle.24 Our results did not indicate a relationship between femoral anteversion and quadriceps angle, but evidence suggests that greater femoral anteversion may alter hip muscle function in a way that leads to reduced hip control and increased dynamic lower extremity malalignments during functional activities.36,37 Using a simulated hip model, an increase in gluteus medius muscle force was necessary to maintain a level pelvis when the femur was internally rotated (where the distal attachment site of the muscle [greater trochanter] is more anterior, as in the case with femoral anteversion) compared with a neutral alignment.36 Further, decreased activation of the gluteus medius, as measured by surface electromyography amplitude, has been demonstrated in those with increased relative femoral anteversion.37 Collectively, these findings suggest that individuals with increased femoral anteversion require increased force production to control the hip and pelvis, yet they demonstrate decreased activation, which together may severely reduce frontal-plane and transverse-plane hip control during functional activities.
A possible reason why femoral anteversion did not correlate well and, thus, did not load on one of the other factors, is the potential for inconsistent measurements due to poor measurement reliability. However, although the reliability and validity of hip anteversion measurement have come into question,38,39 the measurement technique of Ruwe et al40 that we used had good reliability between testers and high correlations with intraoperative measurements. Consistent with previous authors who have reported high intratester16,41 and intertester reliability,41 the tester in this study had more than 10 years of clinical experience and had established a high level of reliability on this measure. Therefore, we believe that our findings of femoral anteversion as an independent factor from the valgus and pronated alignment factors are more likely because of the structural factors previously described.
Implications for Lower Extremity Injury
The relationship among static alignment, dynamic lower extremity function, and injury risk remains largely theoretical. We specifically labeled the collective relationship among the pelvis and knee variables (pelvic angle, quadriceps angle, tibiofemoral angle) as a valgus alignment factor because the combination of these variables suggests the potential for inward collapse of the knee. The clinical implications of the increased pelvis and knee angles, as measured statically, are relatively unknown, but females appear to be more prone to this valgus posture, as our current findings and previous research suggest that females have greater anterior pelvic tilt,5,14 quadriceps angle,5,14,25,42–45 and tibiofemoral angle14,45 than males. Whether this static valgus posture may, in part, explain why females have been consistently found to land and cut with greater dynamic knee valgus angles and moments compared with males or whether this is due to anatomical versus neuromuscular differences, or both, is unknown and deserves further study.
Although the valgus alignment factor, pronated alignment factor, and measures of femoral anteversion are considered independent of one another, it may be that the interaction of these factors in some way influences the lower extremity injury equation. Specifically, individuals who demonstrate increased values for each of these factors may further increase “at-risk” lower extremity positions during functional activities common to lower extremity injuries. Work is ongoing to determine the extent to which these alignment factors in combination may influence dynamic knee function.
The relationships identified in the current study are limited to the specific alignment characteristics measured by a single examiner with known measurement reliability. Future authors should continue to examine the validity of these clinical measures as they relate to lower extremity function. In addition, we acknowledge that other anatomical and postural measures are assessed during clinical evaluations (eg, measures of foot structure, joint laxity, range of motion) and may also contribute to these static postures and their ultimate effect on dynamic motion and injury risk. These findings are also limited to alignment characteristics measured in a static stance or in a non–weight-bearing position (genu recurvatum, tibial torsion, and hip anteversion). More work is clearly needed in this area, but we hope our findings lead to more integrated examinations of lower extremity alignment when considering anatomical contributions to dynamic lower extremity motion and injury risk.
CONCLUSIONS
Relationships among lower extremity alignment variables identified a distinct valgus alignment factor characterized by the alignment of the pelvis and knees (pelvic tilt, quadriceps angle, and tibiofemoral angle), which was independent of a pronated alignment factor (genu recurvatum, navicular drop, and inward tibial torsion) and femoral anteversion. These observed relationships are limited to healthy, college-aged individuals with no current lower extremity injury and cannot be generalized to an injured population. The results should also be interpreted as a descriptive relationship among the variables, not as a cause-and-effect relationship. In addition, the observed alignment factors accounted for only approximately 56% to 60% of the total variance in lower extremity alignment variables. More work is needed to examine other anatomical and alignment factors that may account for the remaining unexplained variance. Such factors may include geometry of the joint surfaces and differences in soft tissue structures (ie, laxity or stiffness of ligaments and joint capsules and surrounding muscle mass).
Acknowledgments
This study was funded in part by the National Institute of Arthritis and Musculoskeletaland Skin Diseases, National Institutes of Health, #R01 AR053172.
Footnotes
Anh-Dung Nguyen, PhD, ATC, and Sandra J. Shultz, PhD, ATC, CSCS, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article.
REFERENCES
- 1.Powers C. M., Maffucci R., Hampton S. Rearfoot posture in subjects with patellofemoral pain. J Orthop Sports Phys Ther. 1995;22(4):155–160. doi: 10.2519/jospt.1995.22.4.155. [DOI] [PubMed] [Google Scholar]
- 2.Powers C. M., Chen P. Y., Reischl S. F., Perry J. Comparison of foot pronation and lower extremity rotation in persons with and without patellofemoral pain. Foot Ankle Int. 2002;23(7):634–640. doi: 10.1177/107110070202300709. [DOI] [PubMed] [Google Scholar]
- 3.Tiberio D. The effect of excessive subtalar joint pronation on patellofemoral mechanics: a theoretical model. J Orthop Sports Phys Ther. 1987;9(4):160–165. doi: 10.2519/jospt.1987.9.4.160. [DOI] [PubMed] [Google Scholar]
- 4.Loudon J. K., Jenkins W., Loudon K. L. The relationship between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther. 1996;24(2):91–97. doi: 10.2519/jospt.1996.24.2.91. [DOI] [PubMed] [Google Scholar]
- 5.Hertel J., Dorfman J. H., Braham R. A. Lower extremity malalignments and anterior cruciate ligament injury history. J Sports Sci Med. 2004;3(4):220–225. [PMC free article] [PubMed] [Google Scholar]
- 6.Woodford-Rogers B., Cyphert L., Denegar C. R. Risk factors for anterior cruciate ligament injury in high school and college athletes. J Athl Train. 1994;29(4):343–346. [PMC free article] [PubMed] [Google Scholar]
- 7.Beckett M. E., Massie D. L., Bowers K. D., Stoll D. A. Incidence of hyperpronation in the ACL injured knee: a clinical perspective. J Athl Train. 1992;27(1):58–62. [PMC free article] [PubMed] [Google Scholar]
- 8.Hintermann B., Nigg B. M. Pronation in runners: implications for injuries. Sports Med. 1998;26(3):169–176. doi: 10.2165/00007256-199826030-00003. [DOI] [PubMed] [Google Scholar]
- 9.Coplan J. A. Rotational motion of the knee: a comparison of normal and pronating subjects. J Orthop Sports Phys Ther. 1989;10(3):366–369. doi: 10.2519/jospt.1989.10.9.366. [DOI] [PubMed] [Google Scholar]
- 10.Shultz S. J., Carcia C. R., Gansneder B. M., Perrin D. H. The independent and interactive effects of navicular drop and quadriceps angle on neuromuscular responses to a weight-bearing perturbation. J Athl Train. 2006;41(3):251–259. [PMC free article] [PubMed] [Google Scholar]
- 11.Uhorchak J. M., Scoville C. R., Williams G. N., Arciero R. A., St. Pierre P., Taylor D. C. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31(6):831–842. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 12.Gross M. T. Lower quarter screening for skeletal malalignment: suggestions for orthotics and shoewear. J Orthop Sports Phys Ther. 1995;21(6):389–405. doi: 10.2519/jospt.1995.21.6.389. [DOI] [PubMed] [Google Scholar]
- 13.Riegger-Krugh C., Keysor J. J. Skeletal malalignments of the lower quarter: correlated and compensatory motions and postures. J Orthop Sports Phys Ther. 1996;23(2):164–170. doi: 10.2519/jospt.1996.23.2.164. [DOI] [PubMed] [Google Scholar]
- 14.Nguyen A. D., Shultz S. J. Sex differences in clinical measures of lower extremity alignment. J Orthop Sports Phys Ther. 2007;37(7):389–398. doi: 10.2519/jospt.2007.2487. [DOI] [PubMed] [Google Scholar]
- 15.Shultz S. J., Nguyen A. D. Bilateral asymmetries in clinical measures of lower-extremity anatomic characteristics. Clin J Sport Med. 2007;17(5):357–361. doi: 10.1097/JSM.0b013e31811df950. [DOI] [PubMed] [Google Scholar]
- 16.Shultz S. J., Nguyen A., Windley T. C., Kulas A. S., Botic T. L., Beynnon B. D. Intratester and intertester reliability of clinical measures of lower extremity anatomic characteristics: implications for multicenter studies. Clin J Sport Med. 2006;16(2):155–161. doi: 10.1097/00042752-200603000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Shultz S. J., Nguyen A. D., Schmitz R. J. Differences in lower extremity anatomical and postural characteristics in males and females between maturation groups. J Orthop Sports Phys Ther. 2008;38(3):137–149. doi: 10.2519/jospt.2008.2645. [DOI] [PubMed] [Google Scholar]
- 18.Shultz S. J., Levine B., Nguyen A. D. The relationship among lower extremity alignment characteristics and anterior knee joint laxity. Sports Health. 2009;1(1):966–972. doi: 10.1177/1941738108326702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gorsuch R. L. Factor Analysis. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Assoc; 1983. pp. 94–109. [Google Scholar]
- 20.Ireland M. L., Gaudette M., Crook S. ACL injuries in the female athlete. J Sport Rehabil. 1997;6(2):97–110. [Google Scholar]
- 21.Powers C. M. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- 22.Khamis S., Yizhar Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture. 2007;25(1):127–134. doi: 10.1016/j.gaitpost.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Fabry G., MacEwen G. D., Shands A. R., Jr Torsion of the femur: a follow-up study in normal and abnormal conditions. J Bone Joint Surg Am. 1973;55(8):1726–1738. [PubMed] [Google Scholar]
- 24.Hvid I., Andersen L. I. The quadriceps angle and its relation to femoral torsion. Acta Orthop Scand. 1982;53(4):577–579. doi: 10.3109/17453678208992261. [DOI] [PubMed] [Google Scholar]
- 25.Woodland L. H., Francis R. S. Parameters and comparisons of the quadriceps angle of college-aged men and women in the supine and standing positions. Am J Sports Med. 1992;20(2):208–211. doi: 10.1177/036354659202000220. [DOI] [PubMed] [Google Scholar]
- 26.Johal P., Williams A., Wragg P., Hunt D., Gedroyc W. Tibio-femoral movement in the living knee: a study of weight bearing and non-weight bearing knee kinematics using ‘interventional’ MRI. J Biomech. 2005;38(2):269–276. doi: 10.1016/j.jbiomech.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 27.Root M. L., Orien W. P., Weed J. H., Hughes R. J. Normal and Abnormal Function of the Foot. Los Angeles, CA: Clinical Biomechanics Corp; 1977. pp. 127–163. [Google Scholar]
- 28.Beighton P., Solomon L., Soskolne C. L. Articular mobility in an African population. Ann Rheum Dis. 1973;32(5):413–418. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trimble M. H., Bishop M. D., Buckley B. D., Fields L. C., Rozea G. D. The relationship between clinical measurements of lower extremity posture and tibial translation. Clin Biomech (Bristol, Avon) 2002;17(4):286–290. doi: 10.1016/s0268-0033(02)00010-4. [DOI] [PubMed] [Google Scholar]
- 30.Stuberg W., Temme J., Kaplan P., Clarke A., Fuchs R. Measurement of tibial torsion and thigh-foot angle using goniometry and computed tomography. Clin Orthop Relat Res. 1991;272:208–212. [PubMed] [Google Scholar]
- 31.Kristiansen L. P., Gunderson R. B., Steen H., Reikeras O. The normal development of tibial torsion. Skeletal Radiol. 2001;30(9):519–522. doi: 10.1007/s002560100388. [DOI] [PubMed] [Google Scholar]
- 32.Valmassy R., Stanton B. Tibial torsion: normal values in children. J Am Podiatr Med Assoc. 1989;79(9):432–435. doi: 10.7547/87507315-79-9-432. [DOI] [PubMed] [Google Scholar]
- 33.Mueller M. J., Host J. V., Norton B. J. Navicular drop as a composite measure of excessive pronation. J Am Podiatr Med Assoc. 1993;83(4):198–202. doi: 10.7547/87507315-83-4-198. [DOI] [PubMed] [Google Scholar]
- 34.Kendall F. P., McCreary E. K., Provance P. G., Rodgers M. M., Romani W. A. Muscles Testing and Function With Posture and Pain. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. pp. 82–83. [Google Scholar]
- 35.Gulan G., Matovinovic D., Nemec B., Rubinic D., Ravlic-Gulan J. Femoral neck anteversion: values, development, measurement, common problems. Coll Antropol. 2000;24(2):521–527. [PubMed] [Google Scholar]
- 36.Merchant A. C. Hip abductor muscle force; an experimental study of the influence of hip position with particular reference to rotation. J Bone Joint Surg Am. 1965;47:462–476. [PubMed] [Google Scholar]
- 37.Nyland J., Kuzemchek S., Parks M., Caborn D. N. Femoral anteversion influences vastus medialis and gluteus medius EMG amplitude: composite hip abductor EMG amplitude ratios during isometric combined hip abduction-external rotation. J Electromyogr Kinesiol. 2004;14(2):255–261. doi: 10.1016/S1050-6411(03)00078-6. [DOI] [PubMed] [Google Scholar]
- 38.Piva S. R., Fitzgerald K., Irrgang J. J., et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskelet Disord. 2006;7:33. doi: 10.1186/1471-2474-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sutlive T. G., Mitchell S. D., Maxfield S. N., et al. Identification of individuals with patellofemoral pain whose symptoms improved after a combined program of foot orthosis use and modified activity: a preliminary investigation. Phys Ther. 2004;84(1):49–61. [PubMed] [Google Scholar]
- 40.Ruwe P. A., Gage J. R., Ozonoff M. B., De Luca P. A. Clinical determination of femoral anteversion: a comparison with established techniques. J Bone Joint Surg Am. 1992;74A(6):820–830. [PubMed] [Google Scholar]
- 41.Jonson S. R., Gross M. T. Intraexaminer reliability, interexaminer reliability, and mean values for nine lower extremity skeletal measures in healthy naval midshipmen. J Orthop Sports Phys Ther. 1997;25(4):253–263. doi: 10.2519/jospt.1997.25.4.253. [DOI] [PubMed] [Google Scholar]
- 42.Guerra J. P., Arnold M. J., Gajdosik R. L. Q angle: effects of isometric quadriceps contraction and body position. J Orthop Sports Phys Ther. 1994;19(4):200–204. doi: 10.2519/jospt.1994.19.4.200. [DOI] [PubMed] [Google Scholar]
- 43.Aglietti P., Insall J. N., Cerulli G. Patellar pain and incongruence, I: measurements of incongruence. Clin Orthop Relat Res. 1983;176:217–224. [PubMed] [Google Scholar]
- 44.Horton M. G., Hall T. L. Quadriceps femoris muscle angle: normal values and relationships with gender and selected skeletal measures. Phys Ther. 1989;69(11):897–901. doi: 10.1093/ptj/69.11.897. [DOI] [PubMed] [Google Scholar]
- 45.Hsu R. W., Himeno S., Coventry M. B., Chao E. Y. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed] [Google Scholar]