Abstract
Purpose
To provide population-based normative data for monocular visual acuity (VA) and interocular differences in VA (IOD), in African-American and Hispanic children 30–72 months of age without visually significant refractive errors or ophthalmic abnormalities.
Methods
In a population-based cohort of children in the Multi-Ethnic Pediatric Eye Disease Study, monocular HOTV VA measurements using the Amblyopia Treatment Study protocol were analyzed using continuous and dichotomous outcomes for VA and IOD, after excluding subjects with ophthalmic abnormalities or refractive error.
Results
The analysis cohort consisted of 1722 African-American and Hispanic children aged 30 to 72 months. Mean logMAR VA improved with age (P<0.0001) and male gender (p=0.0008). The proportion of children achieving VA 20/40 or better was associated with age (p<0.0001), but not ethnicity or gender, and was 81%, 94%, 99% and virtually 100% in children aged 30–35, 36–47, 48–59, and 60–72 months of age, respectively. The most stringent VA threshold that excluded <5% of normal children was 20/63, 20/50, 20/32, and 20/32 for children aged 30–35, 36–47, 48–59, and 60–72 months, respectively. Children attending preschool or daycare achieved VA 20/32 more often than those not attending, after age adjustment (P=0.01), as did children from higher-income families (p=0.04). There was no association between mean absolute IOD and age (P=0.45), ethnicity (P=0.12), or gender (P=0.19). The proportion of children achieving an IOD of 0–1 lines was higher in males than females (P=0.02); it did not vary by age (P=0.06) or ethnicity (P=0.17). IOD of two or more lines occurred in 6% of normal children.
Conclusions
Visual acuity test performance in normal preschool children improves with age. We propose new age-specific thresholds for defining abnormal monocular VA using HOTV optotypes in children between 2 and 5 years of age, for use in screening, clinical practice and research.
Keywords: visual acuity, normal, interocular difference, preschool, HOTV
The diagnosis and management of amblyopia, strabismus, refractive error, and other vision disorders in children are dependent upon an accurate and reliable determination of visual acuity (VA). VA is also the most common measure used in vision screening to identify children who may require comprehensive eye examinations. While VA of 20/20 or better is widely considered to be “normal” for most adult patients,1 VA worse than 20/20 is common in preschool children, even in the absence of refractive error or other vision disorders.2 For this reason, vision screening referral criteria and definitions of amblyopia are often based on acuity values in the range of 20/30 to 20/50 or worse. However, there are no published VA norms derived from population-based samples of preschool children. Thus, it remains imperative to define normal VA test performance in healthy preschool children, including its dependence on age.
The Amblyopia Treatment Study (ATS) HOTV visual acuity testing protocol was specifically developed for young children. It is currently used by the pediatric vision research community and increasingly used in clinical practice by pediatric eye care providers. Testability rates are high for preschool children3,4 and measurements can sometimes be obtained in children as young as 2 years of age.5,6 As is the case for other optotype acuity tests, existing studies of HOTV protocols in young children are not population-based,7 and/or do not report data for normal children (i.e., children without visually significant refractive error or ocular abnormalities).4,8,9,10
The Multi-Ethnic Pediatric Eye Disease Study (MEPEDS) is an ongoing cross-sectional, population-based study, with the specific aims of providing prevalence estimates for amblyopia, strabismus, and refractive error in a multi-ethnic cohort of children between the ages of 6 and 72 months. The purpose of this report is to provide population-based, age-specific visual acuity normative data for monocular VA and interocular VA differences in African-American and Hispanic children between the ages of 30 and 72 months who have no significant refractive error or other ophthalmic abnormalities.
METHODS
This study was supported by the National Eye Institute of the National Institutes of Health. The protocol and informed consent forms were approved by the Institutional Review Board (IRB)/Ethics Committee of the Los Angeles County University of Southern California Medical Center. A parent or guardian (henceforth referred to as “parent”) of each study participant gave written informed consent. An independent data monitoring and oversight committee (DMOC) provided study oversight.
Study Population
The study population consisted of African-American and Hispanic children aged 30 to 72 months in 44 census tracts in the city of Inglewood and adjacent communities in Los Angeles County, California. The study design has been previously published.11 In brief, a trained interview team conducted a door-to-door census of all dwelling units within targeted census tracts to identify eligible children (aged 6–72 months). After parental consent and an in-home interview, children were scheduled for a comprehensive eye examination at the local MEPEDS examination center, performed by MEPEDS optometrists or ophthalmologists trained and certified using standardized protocols. Ethnicity was determined by parental self-report.
Examination and Determination of Visual Acuity
In the clinic, a detailed parental interview was conducted, including questions regarding family income and preschool or daycare enrollment.11 The examination, described in detail elsewhere,11,12 included VA testing, evaluation of ocular alignment, cycloplegic refractive error measurement, and anterior segment and dilated fundus evaluations. Cycloplegic refraction was performed with the Retinomax Autorefractor (Right Manufacturing, Virginia Beach, VA) at least 30 minutes after instilling the second of 2 drops of 1% cyclopentolate given 5 minutes apart. Cycloplegic retinoscopy was performed if Retinomax readings with confidence ratings of ≥8 were not obtained in both eyes after 3 attempts per eye. If parents refused cycloplegic eyedrops, non-cycloplegic retinoscopy was performed.
Presenting monocular distance VA measurement was attempted using an electronic visual acuity (EVA) tester6 with the ATS protocol.5 The EVA system uses a handheld device programmed with the protocol algorithm to control the presentation of high-contrast black-and-white single HOTV optotypes framed by crowding bars spaced a half-letter width from the letter on a 17-inch monitor. The ATS testing algorithm has been described previously;5,6 an initial screening phase obtaining an approximate VA threshold is followed by a first threshold determination phase, a reinforcement phase, and a second threshold determination phase. The VA score, measured in 0.1 logMAR increments from 20/800 to 20/16, is the smallest logMAR level passed in either of the two threshold phases.
The VA testing protocol specific to MEPEDS has been reported in detail.3 Children were seated 3 meters from the monitor with a lap card containing the single-surround HOTV letters. Children who had difficulty comprehending the task underwent a binocular pretest at near, which if passed was followed by a binocular pretest at 3 meters, and monocular threshold testing for those able to complete the pretests. Children were instructed to identify the letter on the monitor verbally or by pointing to the matching optotype on the hand-held card; those who knew their letters were still encouraged to refer to the card. The right eye was tested first, followed by the left, with the fellow eye occluded with an adhesive patch or, rarely, occluding glasses. Testing was attempted on all children, including those with developmental delay or disability.
Inclusion/Exclusion Criteria
Only Hispanic and African-American children able to complete monocular threshold VA testing in both eyes were included in the analysis. The following were excluded: children presenting with glasses; those whose examination resulted in a diagnosis of amblyopia,12 strabismus,12 nystagmus, visual axis occlusion, or other anterior segment or fundus abnormalities capable of causing visual impairment; and those with potentially visually significant refractive error in either eye, defined as ≥2.00 D spherical equivalent (SE) hyperopia, ≥ 0.50 D SE myopia, ≥ 1.00 D astigmatism at any axis, ≥1.00 D SE hyperopic anisometropia, or antimetropia with ≥1.00 D SE in the hyperopic eye.
Statistical Analysis
Visual acuity outcomes were defined continuously as mean logMAR VA or mean logMAR interocular difference (IOD) in VA, and dichotomously as the proportion of children achieving a particular threshold level of VA or IOD. The estimated cutoff for the lowest fifth percentile of normal children was derived from the mean and standard deviation (s.d.) of logMAR VA for each age group, assuming a normal distribution of logMAR VA (limit = mean + 1.645 * s.d.). The actual percentages of children in the study cohort with VA worse than the two protocol-tested threshold levels nearest to the estimated cutoff were determined for each age group. Multiple linear regression was used to assess associations of logMAR VA and logMAR IOD with age, gender, and ethnicity. Multiple logistic regression was used to assess associations between the proportion of children meeting a threshold VA or IOD criterion, and age, gender, ethnicity, family income, or preschool or daycare attendance. T-tests were used to determine whether mean IOD was significantly different from zero. All analyses were conducted using SAS software 9.1 (SAS Institute Inc, Cary, NC) and a 0.05 significance level.
RESULTS
An in-home interview and clinical examination were completed by 3835 African-American and Hispanic children aged 30 to 72 months. In 3.0% of participants, parents refused cycloplegic eyedrops, and non-cycloplegic retinoscopy was performed. In children aged 30–35 months, 36–47 months, 48–59 months and 60–72 months, respectively, 34%, 81%, 98% and 99% of children were testable in both eyes; after excluding children with ophthalmic abnormalities and refractive errors, 1722 children remained (50%, 53%, 53% and 55% of testable children, respectively, in each age group). Overall, 49.3% of participants were Hispanic and 50.7% were African-American, while 49.1% were male.
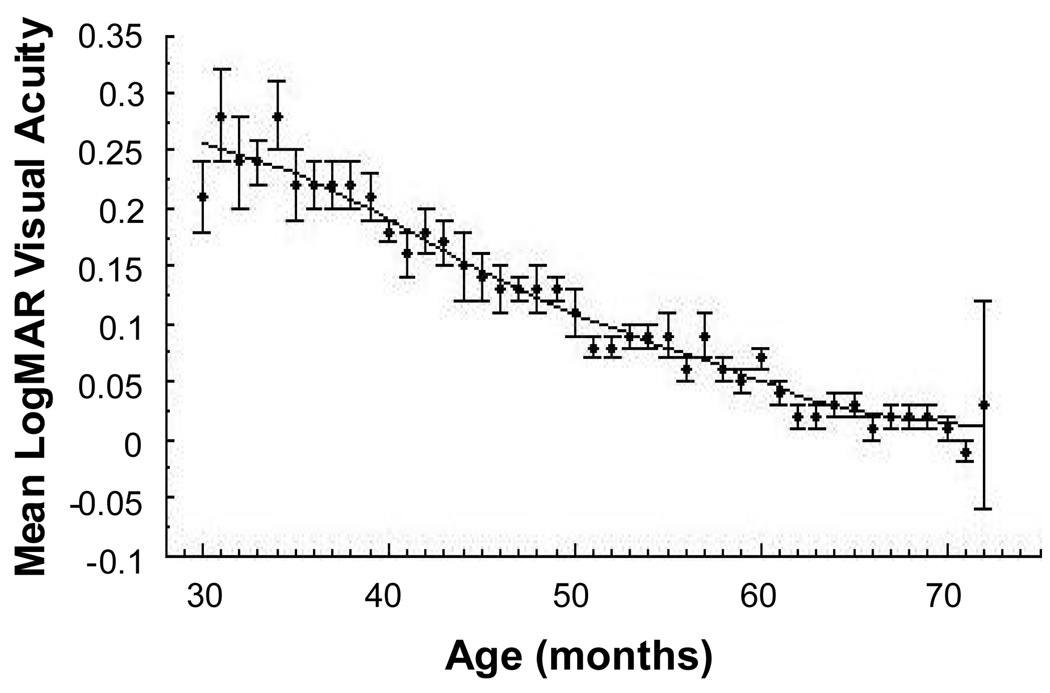
Age- and gender-specific mean logMAR VA levels for the right eye are shown in Table 1. A multivariate linear regression model including age group, ethnicity, and gender showed no association of VA with ethnicity (P=0.07), but significant associations with age (P<0.0001) and gender (P=0.0008). Males performed slightly better than females with an overall mean logMAR VA difference of 0.01. In stratified analyses, males performed significantly better than females in the 48–59 and 60–72 month age groups (P=0.0007 and P=0.005, respectively). Mean logMAR VA decreased steadily with increasing age, as shown in the Lowess plot of mean VA by months of age (Figure 1).
Table 1.
Mean Logmar visual acuity and thresholds for lowest fifth percentile.
| Age (mos) | Mean VA(Male) | Mean VA (Fem.) | Mean (s.d.) VA | 5th %ile(Snellen equiv.)* | Snellen equiv. threshold† | % children with worse acuity | Alternate‡ threshold | % children with worse acuity |
|---|---|---|---|---|---|---|---|---|
| 30–35 (N=100) | 0.24 | 0.22 | 0.23 (0.14) | 0.46 (20/58) | 20/63 | 3.0% | 20/50 | 6.0% |
| 36–47 (N=460) | 0.16 | 0.18 | 0.17 (0.13) | 0.38 (20/48) | 20/50 | 3.0% | 20/40 | 6.3% |
| 48–59 (N=567) | 0.07 | 0.10 | 0.08 (0.11) | 0.26 (20/36) | 20/40 | 1.1% | 20/32 | 4.1% |
| 60–72 (N=595) | 0.01 | 0.03 | 0.02 (0.09) | 0.17 (20/30) | 20/32 | 0.5% | 20/25 | 7.9% |
mos.= months
N = number of participants
VA = logMAR visual acuity
Fem.= female
s.d. = standard deviation
equiv.= equivalent
Estimated VA limit of lowest fifth percentile (%ile), assuming a normal distribution.
Nearest Snellen-equivalent line tested by the ATS HOTV protocol.
Alternate threshold is the next closest acuity level tested by the ATS HOTV protocol.
Figure 1.
Mean logMAR visual acuity for children for every month of age, with LOWESS fit line. The error bars correspond to +/− one standard error of the mean.
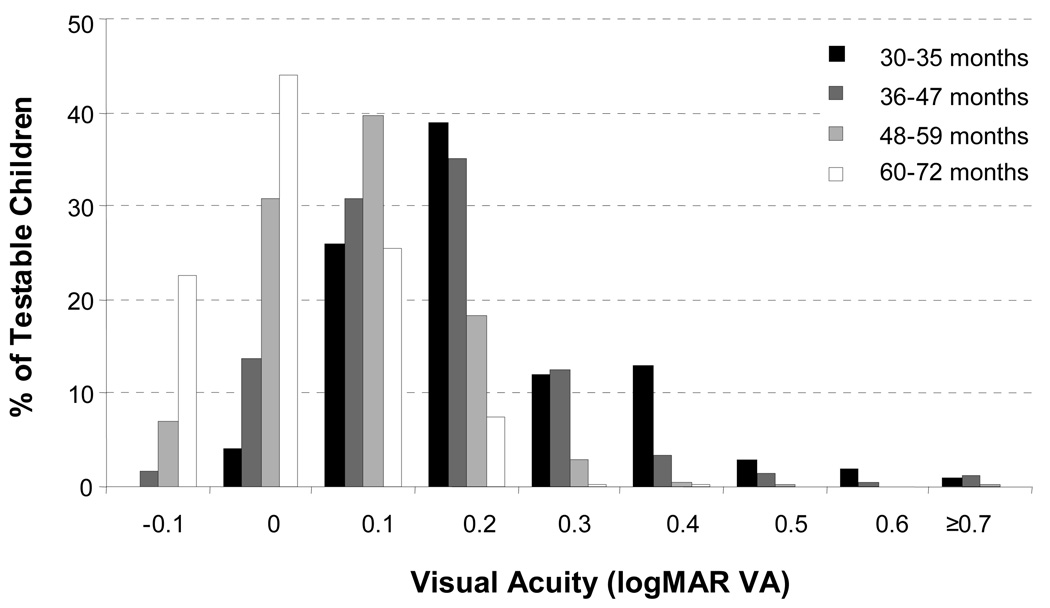
Figure 2 shows the distribution of logMAR VA for children in four age groups. The proportion of children with VA 20/40 or better was 81%, 94%, 99% and virtually 100% in children 30–35 months, 36–47 months, 48–59 months, and 60–72 months of age, respectively. In multivariate logistic regression adjusting for age, ethnicity, and gender, the proportion of children attaining VA of 20/40 or better was significantly associated with age (P<0.0001), but not ethnicity (P=0.82) or gender (P=0.88).
Figure 2.
Frequency histogram of distribution of logMAR visual acuity by age group.
To explore age-specific threshold levels of VA that were met by at least 95% of normal eyes, the logMAR VA cutoff for the worst fifth percentile was estimated from the mean and s.d. of logMAR VA for each age group, assuming a normal distribution of VA values. The lowest fifth percentile acuity limit and its Snellen equivalent are shown in Table 1. For each of the two nearest Snellen-equivalent VA thresholds employed by the ATS HOTV protocol, the observed proportion of children having VA worse than the threshold in question was determined (Table 1).
Family income and daycare/preschool enrollment status were reported for 89% and 98% of children, respectively: 70% of children attended daycare or preschool and 65% of parents reported annual household income under $20,000. Overall, 96% of children attending daycare or preschool achieved a VA of 20/32 or better, compared to 82% of children who did not; 91% of children in lower-income families had VA of 20/32 or better, compared to 94% of children in higher-income families. In a model adjusting for age as a continuous variable (months of age), ethnicity, gender, preschool/daycare attendance, and income, the percentage of children with VA 20/32 or better was significantly higher among those attending daycare or preschool than among those who did not attend daycare or preschool (P=0.01; odds ratio: 1.76, 95% CI: 1.12, 2.76). The percentage was significantly lower among those with low family income than among those with higher income (P=0.04; odds ratio: 0.62, 95% CI: 0.39, 0.98).
In contrast to monocular VA, IOD showed little variation with age. The mean absolute IOD in logMAR VA was 0.05 (sd 0.07), 0.06 (sd 0.07), 0.06 (sd 0.07), and 0.06 (sd 0.06), for children aged 30–35 months, 36–47 months, 48–59 months, 60 to 72 months, respectively. Multivariate linear regression of IOD in VA showed no significant association with age (P=0.45), ethnicity (P=0.12), or gender (P=0.19). Table 2 shows the proportion of children achieving logMAR IOD of 0.1 or less (Snellen equivalent one line or less) as a function of age, stratified by gender. In multivariate logistic regression adjusting for age, ethnicity and gender, the proportion of children with an IOD of ≤0.1 showed a significant association with gender (P=0.02), but no association with ethnicity (P= 0.17) or age (P=0.06). Males were more likely to have ≤0.1 IOD in VA than females (odds ratio 1.6; 95% CI: 1.08, 2.44).
Table 2.
Proportion of children with interocular LogMAR VA difference ≤ 0.1.
| Age (months) | Male | Female | Total |
|---|---|---|---|
| 30–35 | 51/54 (94.4%) |
45/46 (97.8%) |
96/100 (96%) |
| 36–47 | 218/234 (93.2%) |
206/226 (91.2%) |
424/460 (92.2%) |
| 48–59 | 273/285 (95.8%) |
254/282 (90.1%) |
527/567 (92.9) |
| 60–72 | 263/272 (96.7%) |
308/323 (95.4%) |
571/595 (96.0) |
| Total | 805/845 (95.3%) |
813/877 (92.7%) |
1618/1722 (94.0) |
To evaluate for any systematic effect of the order in which the eyes were tested, the mean IOD (right eye minus left eye logMAR VA, with the sign of the difference preserved) was calculated for each age group. The mean logMAR VA IOD in children aged 30 to 35 months was 0.02, significantly different from zero (P=0.01, two tailed t-test), indicating better VA on average in the second eye tested than the first. The mean IOD was 0.00 in all other age groups.
DISCUSSION
This study is, to our knowledge, the first to provide population-based normative data on optotype VA test performance in a cohort of preschool children without significant refractive error or other ophthalmic abnormalities. The strong age-dependence of monocular VA between 30 and 72 months of age indicates a need for new, age-specific thresholds for defining abnormal VA in preschool children. Interocular differences in VA did not show a clear dependence on age, but 6% of normal children showed an apparently spurious IOD in presenting VA of two or more lines.
Mean right eye logMAR VA using HOTV optotypes with the ATS protocol improved by the equivalent of more than two lines between the 30–35 month-old age group and the 60–72 month-old age group. This could be related to maturation of attention and general cognitive abilities, or to maturation of visual function itself. Because improving test performance parallels an increase in overall testability with increasing age using the same testing method,3, 10 it is likely that older age leads to improved cooperation and comprehension rather than true physiological improvement in vision over the age range studied; however, a component of physiological maturation cannot be ruled out.
Drover et al 7 assessed a non-population-based sample of 384 children between the ages of 3 and 10 years using the ATS protocol with HOTV optotypes on the EVA testing system, excluding children with known eye disease, and similarly found improvement in VA with increasing age. LogMAR VA averaged 0.03 and 0.08 among 5- and 4-year-old children, respectively; this is similar to the means of 0.02 and 0.09 in 60–72 month-old children and 48–59 month-old children, respectively, in the present study. However, the 3-year-old group of Drover et al had a mean VA of 0.08, compared to 0.17 in 36–47 month-old children in the present study. Since Drover et al did not specify age in months, their 3-years-olds may have been older on average than those in the present study. Participation bias in their non-population-based sample may have led to over-representation of more mature or cooperative children. Finally, population differences in socioeconomic status or preschool attendance (see below) may have contributed to study differences in test performance.
The present study provides guidelines for age-specific thresholds for normal presenting VA, derived from preschool children without significant refractive error or other ophthalmic abnormalities. Particularly stringent and uncontroversial criteria were chosen, excluding even moderate hyperopia and astigmatism, to ensure a cohort of children without any conceivable ophthalmic reason to have subnormal VA. Among children aged 60 to 72 months, VA worse than 20/32 had less than a 1% chance of occurring in a normal child. By contrast, 20/63 may be a more appropriate threshold in testable 2-year-olds; VA was worse than 20/50 in more than 5% of normal children less than 36 months of age. The data suggest that normal presenting HOTV acuity using the ATS protocol may be defined as follows: 20/63 or better for 30 to 35 month-old children; 20/50 or better for 36 to 47 month-old children; either 20/40 or better, or 20/32 or better, for 48 to 59 month-old children; and 20/32 or better for 60 to 72 month-old children. The American Academy of Pediatrics, American Association for Pediatric Ophthalmology and Strabismus, and American Academy of Ophthalmology have recommended referral by pediatricians to eye-care providers of those children between 3 and 5 years of age who have a 2-line or greater IOD or VA worse than 20/40.13 This VA threshold may be too stringent for 3 year-olds, and be overly lenient for 5 year-olds.
It should be noted that variability of test performance in younger children leads to overlap of the VA distributions for normal children and children with visual pathology. Providers must be cognizant that 20/63 VA in a 2-year-old could well result from pathology, even though it is observed in 3% of normal children aged 30–35 months. Even in older children, a VA of 20/32 in both eyes in a 5-year-old child must not be interpreted as ruling out the possibility of visually significant ophthalmic conditions. Rather, the implications of this study are that failure to achieve this level of VA indicates a very low likelihood that the child has a completely normal ophthalmic exam. Furthermore, cooperation and environmental factors such as school attendance and prior exposure to similar tasks must be considered when interpreting VA results.
In this study, children attending preschool or daycare were more likely to attain VA of 20/32 or better than those who did not, as were those from higher-income families, echoing findings for preschool stereoacuity testability.14 Children attending preschool/daycare may learn to follow instructions and perform cognitive tasks better than those without such experience. Family income and daycare attendance may be correlated with increased parental education and teaching received in the home, contributing to better VA test performance. It is also possible that less behaviorally mature children are less likely to be placed in preschool or daycare, and also less likely to do well on testing, rather than children's exposure to educational activities improving test performance. The association between preschool/daycare attendance and VA, whether direct or indirect, suggests that improved performance on VA testing with age is related to behavioral maturation rather than physiological maturation of the visual system, although some degree of visual maturation cannot be ruled out.
No ethnicity-related differences in VA were seen. Males were no more likely to have VA of 20/40 or better than females, but did have slightly better mean logMAR VA, and were less likely to show two or more lines of IOD. Robaei and coworkers found Australian boys had slightly better right eye VA than girls,8 but included children with ocular abnormalities and refractive error. MEPEDS3 and the Baltimore Pediatric Eye Disease Study,10 using identical methodology,3,11,10 found that young girls were more often able to complete VA testing than young boys; boys who would have performed badly may have been less likely to complete testing than female counterparts, accounting for better performance by testable boys than testable girls. Alternatively, the results may reflect a genuine, albeit clinically insignificant, gender disparity in vision.
In contrast to monocular VA, IOD was not associated with age, ethnicity, or gender, and was, on average, less than one line at all ages, similar to the findings of Drover and colleagues.7 A small practice effect was identified in the 30 to 35 month-old children, with the left eye on average performing slightly better than the right, but no effect of testing order was observed in any other age group.
Because a two-line IOD is a standard criterion for the diagnosis of amblyopia in the presence of risk factors,15 it is important to note that 6% of normal preschool children without amblyopia risk factors showed two or more lines of IOD in presenting VA. In younger children, an IOD associated with an amblyopia risk factor is thus not necessarily attributable to that risk factor. The threshold for defining amblyopia can not be increased to three lines without excluding mild amblyopia, but levels of IOD intermediate between two and three lines can not be discerned using line-based acuity tests. Letter-based acuity measurement, which permits finer classification of IOD than line-based measurement, may have a valuable role in the assessment of IOD in VA in preschool children.16 In practice, when using a line-based measure, repeated testing can help to distinguish between "real" IODs and those resulting from variable test performance.
Several limitations of the present study should be noted. VA testing could not be completed in 66% of 2-year-old children. While this is comparable to the proportion of untestable 2-year-olds in the Baltimore Pediatric Eye Disease study (57%),10 it results in a smaller sample size for this age group, and raises the possibility of under-representation of children who would have performed poorly had they been able testable. Visual acuity in 2-year-old children might prove to be even worse than reported here, if all of them could be tested. With regard to IOD, the use of a discontinuous measure of VA (line-based rather than letter-based) leads to a coarse measure of IOD, relative to the narrow distribution of IOD in the cohort.16 However, line-based IOD in VA is the measure most commonly used in clinical practice to make the diagnosis of conditions such as amblyopia, so our findings using this measure remain pertinent to routine clinical practice. Because this study analyzes presenting VA, the specific normative values reported may not apply to children having prior testing experience. Finally, the results may not be applicable to VA testing methods other than HOTV optotypes using the ATS protocol.
Our findings can be generalized at least to African-American and Hispanic children aged 30 to 72 months throughout the United States. They are likely applicable to other ethnic groups as well, although socioeconomic factors that may vary by ethnicity might impact testing via environmental factors such as preschool and daycare attendance.
In conclusion, thresholds for defining normal monocular VA in preschool children should be age-specific over the 2 to 5 year-old age range. This study provides specific suggestions for re-defining normal presenting VA test performance at different ages using the HOTV ATS protocol, for use in screening, clinical practice, and clinical research. The study also highlights the occurrence of apparently spurious interocular differences in line-based presenting visual acuity in normal preschool children. The validity of the findings is strengthened by the use of population-based data, a highly standardized protocol, a large overall sample size permitting age-stratified analysis, and the rigorous exclusion of all children with refractive errors or other ophthalmic conditions with potential to affect VA. As the use of crowded isolated HOTV optotypes is increasing in pediatric eye care, these results provide much-needed normative data and guidelines for interpreting VA test results in young children.
ACKNOWLEDGMENTS
This study was supported by Grants Nos.EY14472 and EY03040 from the National Eye Institute, Bethesda, Maryland, and an unrestricted Grant from the Research to Prevent Blindness, Inc., New York, New York.
The Multi-Ethnic Pediatric Eye Disease Study Group
Rohit Varma, MD, MPH (Principal Investigator); LaVina Abbott (2002–2005);George Ayala (2005–2006); Stanley P. Azen, PhD; Tal Barak, OD; Mark Borchert, MD; Jessica Chang, OD (2005–2008); Felicia K. Chen, OD (2005–2007); Rose Chon (2008); Susan Cotter, OD, MS (Co-Principal Investigator); Jennifer Deneen, MPH; Jackie Diaz; Anne DiLauro, MPH (2005–2007);Jill Donofrio, MPH (2003–2005); Claudia Dozal (2003–2004); Athena W. Foong; James Gardner; Regina Garriott, OD (2003–2005), Jackson Lau, OD (2006–2007); Jesse Lin, MS; George Martinez; Roberta McKean-Cowdin, PhD; Kisha Milo; Carlos Moya; Ying Pan, MD; Sylvia Paz, MS (2002–2005); Ana Penate; Amanda Reiner, MPH (2007); Claudia Salazar (2006–2008); Erin Song, OD (2003–2008); Kristina Tarczy-Hornoch, MD, DPhil; Mina Torres, MS; Natalia Uribe, OD (2003–2007); Ivania Verrico (2005–2007); Ying Wang, MS (2006–2007); Ge Wen; Peng Zhao, MS (2003–2007); Amy Zhu.
Footnotes
The authors have no financial conflicts of interest.
REFERENCES
- 1.Kniestedt C, Stamper RL. Visual acuity and its measurement. Ophthalmol Clin North Am. 2003;16:155–170. doi: 10.1016/s0896-1549(03)00013-0. [DOI] [PubMed] [Google Scholar]
- 2.Fern KD, Manny RE. Visual acuity of the preschool child: a review. Am J Optom Physiol Opt. 1986;63:319–345. doi: 10.1097/00006324-198605000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Cotter SA, Tarczy-Hornoch K, Wang Y, Azen SP, Dilauro A, Borchert M, Varma R. Visual acuity testability in African-American and Hispanic children: the multi-ethnic pediatric eye disease study. Am J Ophthalmol. 2007;144:663–667. doi: 10.1016/j.ajo.2007.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kulp MT, Dobson V, Peskin E, Quinn G, Schmidt P. The electronic visual acuity tester: testability in preschool children. Optom Vis Sci. 2004;81:238–244. doi: 10.1097/00006324-200404000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Holmes JM, Beck RW, Repka MX, Leske DA, Kraker RT, Blair RC, Moke PS, Birch EE, Saunders RA, Hertle RW, Quinn GE, Simons KA, Miller JM. The amblyopia treatment study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–1353. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 6.Moke PS, Turpin AH, Beck RW, Holmes JM, Repka MX, Birch EE, Hertle RW, Kraker RT, Miller JM, Johnson CA. Computerized method of visual acuity testing: adaptation of the amblyopia treatment study visual acuity testing protocol. Am J Ophthalmol. 2001;132:903–909. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 7.Drover JR, Felius J, Cheng CS, Morale SE, Wyatt L, Birch EE. Normative pediatric visual acuity using single surrounded HOTV optotypes on the Electronic Visual Acuity Tester following the Amblyopia Treatment Study protocol. J AAPOS. 2008;12:145–149. doi: 10.1016/j.jaapos.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robaei D, Rose K, Ojaimi E, Kifley A, Huynh S, Mitchell P. Visual acuity and the causes of visual loss in a population-based sample of 6-year-old Australian children. Ophthalmology. 2005;112:1275–1282. doi: 10.1016/j.ophtha.2005.01.052. [DOI] [PubMed] [Google Scholar]
- 9.Vision in Preschoolers Study Group. Preschool visual acuity screening with HOTV and Lea symbols: testability and between-test agreement. Optom Vis Sci. 2004;81:678–683. doi: 10.1097/01.opx.0000144746.80718.67. [DOI] [PubMed] [Google Scholar]
- 10.Friedman DS, Repka MX, Katz J, Giordano L, Ibironke J, Hawes P, Burkom D, Tielsch JM. Prevalence of decreased visual acuity among preschool-aged children in an American urban population: the Baltimore Pediatric Eye Disease Study, methods, and results. Ophthalmology. 2008;115:1786–1795. doi: 10.1016/j.ophtha.2008.04.006. 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varma R, Deneen J, Cotter S, Paz SH, Azen SP, Tarczy-Hornoch K, Zhao P. The multi-ethnic pediatric eye disease study: design and methods. Ophthalmic Epidemiol. 2006;13:253–262. doi: 10.1080/09286580600719055. [DOI] [PubMed] [Google Scholar]
- 12.Multi-Ethnic Pediatric Eye Disease Study Group. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months the multi-ethnic pediatric eye disease study. Ophthalmology. 2008;115:1229–1236. doi: 10.1016/j.ophtha.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Eye examination in infants, children, and young adults by pediatricians. Pediatrics. 2003;111:902–907. [PubMed] [Google Scholar]
- 14.Tarczy-Hornoch K, Lin J, Deneen J, Cotter SA, Azen SP, Borchert MS, Wang Y, Varma R. Stereoacuity testability in African-American and Hispanic pre-school children. Optom Vis Sci. 2008;85:158–163. doi: 10.1097/OPX.0b013e3181643ea7. [DOI] [PubMed] [Google Scholar]
- 15.Pediatric Eye Disease Investigator Group. patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120:268–278. doi: 10.1001/archopht.120.3.268. [DOI] [PubMed] [Google Scholar]
- 16.Simmers AJ, Gray LS, Spowart K. Screening for amblyopia: a comparison of paediatric letter tests. Br J Ophthalmol. 1997;81:465–469. doi: 10.1136/bjo.81.6.465. [DOI] [PMC free article] [PubMed] [Google Scholar]