Abstract
Aims
To examine the impact of depressive symptoms on rehospitalisation for heart failure exacerbation in patients with preserved systolic function.
Background
Depressive symptoms associated with higher risk of rehospitalisation have been primarily demonstrated in heart failure patients with systolic dysfunction (ejection fraction < 40%) and the factors influencing rehospitalisation of patients with preserved systolic function (ejection fraction ≥40%) remain unclear.
Design
A prospective, descriptive study design was used.
Methods
The following baseline data were collected from 165 patients with preserved systolic function during an index hospitalisation for heart failure in South Korea: age, gender, body mass index, New York Heart Association functional class, the ratio of mitral velocity to early diastolic velocity of the mitral annulus, comorbidities, history of prior admission and depressive symptoms. Patients were followed monthly for six months after discharge to collect date on all rehospitalisation for heart failure exacerbation. Hierarchical Cox proportional hazards regression was used to identify independent predictors of rehospitalisation. Kaplan–Meier survival curves with log-rank test were used to determine differences in time to rehospitalisation according to severity of depressive symptoms.
Results
Almost half of the patients (48%) had moderate to severe depressive symptoms. The ratio of mitral velocity to early diastolic velocity of the mitral annulus (hazard ratio = 1·06, 95% confidence interval = 1·02–1·10) and depressive symptoms (hazard ratio = 1·05, 95% confidence interval = 1·02–1·08) independently predicted rehospitalisation after controlling for other risk factors. Moderate and severe depressive symptoms were associated with both a higher rate and shorter time to rehospitalisation.
Conclusions
Moderate to severe depressive symptoms predict early rehospitalisation for heart failure exacerbations in patients with preserved systolic function.
Relevance to clinical practice
Nurses should assess for depressive symptoms in patients with heart failure and refer those with depressive symptoms for treatment to improve outcomes.
Keywords: depression, heart disease, nurses, nursing, outcomes
Introduction
Heart failure is the most common reason for hospitalisation and readmission of individuals over 65 years of age world-wide (Proctor et al. 2000). In South Korea, approximately 500,000 people have heart failure (Korean Society of Heart Failure 2004) and the prevalence and mortality from heart failure have significantly increased over the last 10 years (Ha 2003). According to data from two multicentre studies of Korean patients with heart failure (Lee et al. 2003, Han et al. 2005), 20% of patients die and 50% are rehospitalised due to worsening heart failure within one year of hospital discharge for decompensated heart failure.
There has been a growing interest in heart failure with ‘preserved’ left ventricular systolic function in which left ventricular ejection fraction (LVEF) is ≥40% (Vasan et al. 1999, Vasan & Levy 2000, Senni & Redfield 2001). Patients with PSF represent up to 58% of the total population of patients with heart failure, but this group has been excluded from most clinical trials (Vasan et al. 1999, Petrie & McMurray 2001). Patients with preserved systolic function (PSF) may differ from heart failure patients with systolic dysfunction (LVEF < 40%) with regard to epidemiology, treatment options and clinical outcomes (Hogg et al. 2004). Although recent cross-sectional, population-based studies have shown that heart failure patients with PSF are less symptomatic and receive different pharmacological therapy than patients with systolic dysfunction (Judge et al. 1991, McDermott et al. 1995, Moller et al. 2003, Hogg et al. 2004), the factors influencing rehospitalisation of heart failure patients with PSF remain unclear.
Approximately 25% of patients with heart failure experience depressive symptoms including sadness, loss of interest, decreased energy, changes in appetite and sleeping difficulties (Havranek et al. 2004). The presence of depressive symptoms is associated with increased risk for morbidity or death (Murberg et al. 1999, Jiang et al. 2001, 2004, Vaccarino et al. 2001, Havranek et al. 2004, Parissis et al. 2008, Redwine et al. 2007). The higher risk for hospitalisation and mortality associated with depressive symptoms, however, has been primarily demonstrated in heart failure patients with systolic dysfunction (Bennett et al. 1997, Moser & Worster 2000, Jiang et al. 2004, Murberg 2004). Thus, the relationship of depressive symptoms with risk for hospitalisation and mortality in patients with PSF has received considerably less attention. Previous studies from South Korea have noted that hypertension and diabetes mellitus confer increased risk for mortality and hospitalisation of patients with heart failure (Lee et al. 2003, Han et al. 2005). No research has been conducted among Korean patients examining psychological factors associated with rehospitalisation and mortality in heart failure patients with PSF.
The purpose of this study was to determine whether the presence of depressive symptoms is an independent predictor of rehospitalisation for exacerbation of heart failure or mortality in patients with PSF from South Korea. The specific aims were: (1) to describe the prevalence of depressive symptoms in heart failure patients with PSF; (2) to determine differences in time to rehospitalisation or death according to severity of depressive symptoms among heart failure patients with PSF; (3) to determine whether presence of depressive symptoms is an independent predictor of rehospitalisation or mortality after controlling for other risk factors.
Methods
Research design
This study was a prospective, descriptive study of heart failure patients with PSF admitted to six cardiology units between 1 October 2005–31 December 2005.
Participants and Setting
Patients were recruited from six cardiology wards at two large (more than 1500 beds) university hospitals that serve as tertiary medical centres located in Seoul, South Korea. Patients were included who (1) were older than 18 years of age; (2) were diagnosed with heart failure by a cardiologist; (3) were New York Heart Association (NYHA) functional classification ≥II and 4) had a LVEF ≥40%. Cardiologists confirmed diagnosis of heart failure using the Framingham criteria (Ho et al. 1993), which included the presence of at least two major criteria or one major criterion in combination with two minor criteria. Major criteria are paroxysmal nocturnal dyspnoea, neck vein distension, rales, cardiomegaly on chest X-ray, S3 gallop, pulmonary oedema and increased central venous pressure. Minor criteria are bilateral ankle oedema, nocturnal cough, dyspnoea on ordinary exertion, hepatomegaly, pleural effusion and tachycardia (rate ≥ 120/minutes). Minor criteria were not accepted if they could be attributed to another medical condition such as pulmonary hypertension, chronic lung disease, liver cirrhosis, ascites or renal disease.
A total of 170 patients met inclusion criteria for this study and were approached for participants in this study. Three patients refused to participate in this study and two patients were lost to follow-up. Thus, data from 165 patients were included in the study.
Measurement of variables
Depressive symptoms
The Beck Depression Inventory (BDI) was used to measure depressive symptoms (Beck 1967, Beck et al. 1979). The BDI is a widely used, self-reported, 21-item instrument consisting of statements about symptoms of depression. Statements are rated on a four-point scale ranging from 0 (not at all)–3 (very much so) in terms of severity. The total score range is 0–63 with higher scores indicating higher levels of depressive symptoms. All patients were categorised into four groups of depressive symptoms based on standard clinical categories for the BDI. A score of 0–9 was categorised as no depressive symptoms, 10−6 as mild, 17–29 as moderate and 30–63 as severe depressive symptoms (Beck 1967). The reliability of the BDI was previously supported by Cronbach’s alpha coefficient of 0·81 (Beck 1967). The Cronbach’s alpha coefficient for the Korean version of the BDI was 0·86 (Rhee et al. 1995). In this study, the Cronbach’s alpha coefficient for the total 21 items was 0·90.
Other risk factors
The following factors were collected from medical chart review and self-report during the index hospitalisation: age, gender, body mass index (BMI), NYHA functional class, underlying aetiology of heart failure, history of hypertension or diabetes, prior admission for heart failure, left ventricular ejection fraction (LVEF) and the ratio of mitral velocity to early diastolic velocity of the mitral annulus (E/E′) from echocardiography. LVEF from echocardiography reflected left ventricular systolic function and E/E′ reflected left ventricular filling pressure, which is elevated in patients with diastolic dysfunction. These risk factors were chosen as potential predictors based on their known associations with outcomes (Ahmed et al. 2006, Huang et al. 2006, Fonarow et al. 2007a,b, Sanderson 2007, Terzi et al. 2007).
Outcome variable
The outcome variable for this study was the combined end-point of rehospitalisation for heart failure exacerbation or death. All rehospitalisation and mortality data were collected for six months after discharge from index hospitalisation and were confirmed by hospital record review by a nurse with expertise in heart failure. The following information was obtained: time and date of death, cause of death and time and date of rehospitalisation due to an exacerbation of heart failure.
Procedure
Approval was obtained from the Institutional Review Boards at the two university hospitals to conduct the study. The primary investigator presented the study and outlined the participation requirements to interested patients. Patients were informed that their responses would be kept confidential. Written informed consent was obtained from each patient. Permission was obtained at the time of informed consent to review patient hospital records for any subsequent hospitalisation.
Patients completed the questionnaires within three to four days of hospital admission. A research assistant was available to help patients complete their questionnaires, if needed. The status of all patients was followed by outpatient contact or by telephone contact for a six-month period after discharge from January 2006–July 2006. If a patient was hospitalised, a trained research assistant reviewed the hospital record to confirm admission diagnosis and verify date of admission.
Statistical analysis
Statistical analyses were performed using spss for Windows 12·0. Frequencies and percents were calculated for categorical variables and means and standard deviations were calculated for continuous variables. Survival analyses included Kaplan–Meier survival curves and a Cox regression model. Standard Kaplan–Meier survival curves were constructed to estimate cumulative risk of rehospitalisation or death. The log-rank test was conducted to compare differences in time to rehospitalisation or death for patients grouped by severity of depressive symptoms. Hierarchical Cox proportional hazards regression was used to determine independent predictors associated with rehospitalisation for exacerbation of heart failure or death after controlling for other risk factors. Cox regression allows determining independent predictors of clinical outcomes such as mortality and rehospitalisation that occur at varying time points during follow-up. A hazard ratio (HR) for rehospitalisation was obtained for all independent variables along with 95% confidence intervals (CIs). There was no violation with normality, independence and multicollinearity.
Results
Patient characteristics
The majority of the patients were over 60 years old, with a range of 22–92 years. The sample was evenly split by gender. As a group, patients had normal BMIs and were primarily in NYHA functional class III. Nearly half of the sample had ischemic heart disease as the underlying aetiology of heart failure. The common comorbidities were hypertension and diabetes mellitus. Approximately one third had a prior history of admission for exacerbation of heart failure (Table 1).
Table 1.
Patients’ characteristics with heart failure and preserved systolic function (n = 165)
| Characteristics | n (%) | Mean (±SD) |
|---|---|---|
| Age (year) | 62·2 (±12·5) | |
| Gender | ||
| Male | 84 (50·9) | |
| Female | 81 (49·1) | |
| Body mass index (kg/m2) | 23·8 (±3·3) | |
| Underweight (<18·5) | 9 (5·5) | |
| Normal weight (18·5–24·9) | 106 (64·2) | |
| Overweight (25·0–29·9) | 42 (25·5) | |
| Obesity (≥30·0) | 8 (4·8) | |
| NYHA functional class | ||
| II | 70 (42·4) | |
| III | 77 (46·7) | |
| IV | 18 (10·9) | |
| Underlying aetiology of heart failure | ||
| Valvular heart disease | 24 (14·5) | |
| Idiopathic heart failure | 61 (37·0) | |
| Ischaemic heart disease | 80 (48·5) | |
| Hypertension | 68 (41·2) | |
| Diabetes mellitus | 50 (30·3) | |
| Prior admission for heart failure | 51 (30·9) | |
| Left ventricular ejection fraction (%) | 58·10 (±9·97) | |
| E/E′ | 16·46 (±7·88) |
NYHA: New York Heart Association, E/E′: the ratio of mitral velocity to early diastolic velocity of the mitral annulus.
Rates of rehospitalisation and death
During the six month follow-up period, 53 patients (32%) were rehospitalised for decompensated heart failure and seven (4%) died. The seven deaths were all identified as being caused by sudden cardiac death. Thirteen patients (8%) were rehospitalised more than once. In these cases, only the first hospitalisation was considered for analysis. Because all seven patients who died during the course of this study were rehospitalised for heart failure exacerbation before their death, only time and date of rehospitalisation were used in analysis. Therefore, survival analyses as performed in this study included only the first event.
Prevalence of depressive symptoms in heart failure patients with PSF
Only 20% of the patients had no depressive symptoms and almost half of the patients had moderate to severe depressive symptoms (Table 2).
Table 2.
Prevalence of depressive symptoms in heart failure patients with preserved systolic function (n = 165)
| Characteristics | n (%) | Mean (±SD) |
|---|---|---|
| Depressive symptoms (in BDI scores) | 18·7 (±10·6) | |
| No (0–9) | 34 (20·6) | |
| Mild (10–16) | 52 (31·5) | |
| Moderate (17–29) | 58 (35·2) | |
| Severe (30–63) | 21 (12·7) |
BDI: Beck Depression Inventory.
Independent predictors of rehospitalisation in heart failure patients with PSF
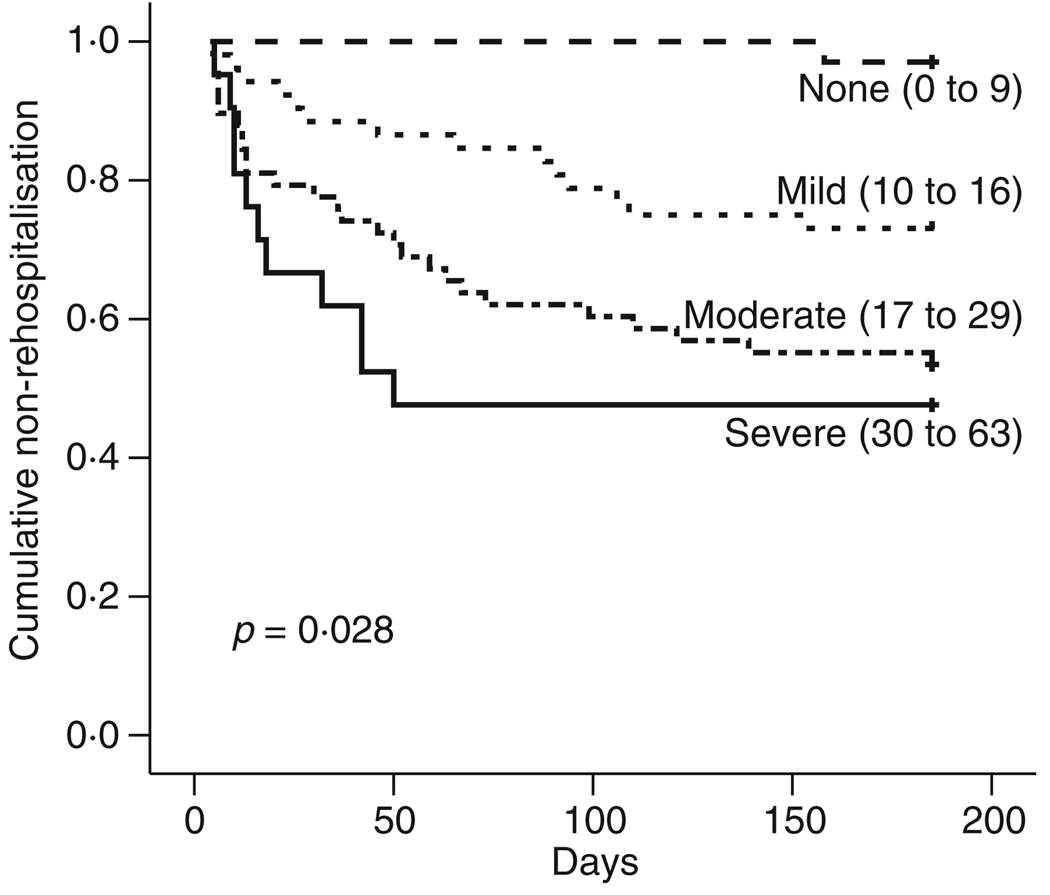
The Kaplan–Meier survival curves demonstrated a dose–response for depressive symptoms with respect to time to rehospitalisation. The log-rank test demonstrated that moderate and severe depressive symptoms were associated with both a higher rate and shorter time to rehospitalisation for heart failure exacerbation after adjusting for all variables (Fig. 1). Only two factors were significantly associated with rehospitalisation in Hierarchical Cox proportional hazard model (Table 3): higher E/E′ and severe depressive symptoms. The risk of rehospitalisation increased by 6% for each one unit increase in the E/E′ and by 5% for each one unit increase in the BDI score. Depressive symptoms remained an independent predictor of rehospitalisation (HR = 1·05, 95% CI = 1·02–1·08) after controlling for other risk factors.
Figure 1.
Time to rehospitalisation for heart failure exacerbation among patients with heart failure and preserved systolic function grouped by severity of depressive symptoms.
Table 3.
Independent predictors of rehospitalisation for heart failure patients with preserved systolic function (n = 165)
| Characteristics | Adjusted hazard ratio |
95% CI | P |
|---|---|---|---|
| Age (year) | 1·02 | 0·99–1·05 | 0·122 |
| Female gender | 0·70 | 0·38–1·26 | 0·232 |
| Body mass index (kg/m2) | 1·01 | 0·93–1·10 | 0·787 |
| NYHA functional class | |||
| III | 0·98 | 0·49–1·96 | 0·956 |
| IV | 1·30 | 0·53–3·24 | 0·566 |
| Underlying aetiology of heart failure | |||
| Idiopathic heart failure | 1·04 | 0·42–2·58 | 0·937 |
| Ischemic heart disease | 0·51 | 0·19–1·33 | 0·166 |
| Hypertension | 1·52 | 0·81–2·85 | 0·189 |
| Diabetes mellitus | 1·09 | 0·58–2·06 | 0·782 |
| Prior admission for heart failure | 1·35 | 0·75–2·43 | 0·324 |
| Left ventricular ejection fraction (%) | 0·99 | 0·96–1·02 | 0·387 |
| E/E′ | 1·06 | 1·02–1·10 | 0·004 |
| Depressive symptoms | 1·05 | 1·02–1·08 | < 0·001 |
NYHA: New York Heart Association, E/E′: the ratio of mitral velocity to early diastolic velocity of the mitral annulus.
Discussion
This is the first study to demonstrate that moderate to severe depressive symptoms are associated with early rehospitalisation for heart failure exacerbations in patients with PSF. Moreover, it is the first study to show that depressive symptoms play a role in increasing risk for rehospitalisation in a Korean population of patients with heart failure. Consistent with the findings of other studies, approximately 33% of heart failure patients with PSF were rehospitalised during six month the follow-up period (Proctor et al. 2000, Schwarz & Elman 2003). This high rehospitalisation rate compares with that seen in heart failure patients with systolic dysfunction (Fonarow et al. 2007b). Thus, the patients with PSF in this sample had risk for rehospitalisation similar to that seen in patients with systolic dysfunction.
Several previous investigators have identified predictors associated with an increased likelihood of being rehospitalised for decompensated heart failure in patients with systolic dysfunction. These predictors included advanced age, prior hospital admission, increased severity of heart failure and an increased number of medical comorbidities (Chin & Goldman 1997, Hogg et al. 2004, Goldberg et al. 2005). However, the ratio of mitral velocity to early diastolic velocity of the mitral annulus (E/E′) was a significant predictor of rehospitalisation for heart failure exacerbation with heart failure patients with PSF. Left ventricular end diastolic pressure is a good marker of diastolic function measured by invasive catheterisation. Nagueh et al. (1997) assessment of mitral inflow and mitral annular velocity suggested that E/E′ can predict left ventricular filling pressure. This result was also supported by Ommen et al. (2000) and other researchers who demonstrated that higher E/E′ identified increased diastolic filling pressure, non-invasively (Taylor et al. 2006). In addition, because NT-pro B type natriuretic peptide (BNP) is lower despite higher left ventricular end-diastolic pressure (LVEDP) (Taylor et al. 2006), E/E′ may be a better biomarker of diastolic dysfunction in heart failure patients with PSF.
Depressive symptoms remained an independent predictor of rehospitalisation in patients with PSF even after controlling for all other risk factors. This finding is similar to studies in patients with systolic dysfunction (Jiang et al. 2001, 2004, Parissis et al. 2008, Redwine et al. 2007). Jiang et al. (2001) reported the risk of mortality increased by 4% for each one unit increase in the BDI score of hospitalised heart failure patients with systolic dysfunction. In addition, depression is associated with poor follow-up and poor postdischarge professional support (Goldberg et al. 2005), a higher risk of non-compliance and lower levels of social support (Joynt et al. 2004), which have been shown to worsen prognosis in heart failure. More importantly, the present study had shown a higher predictive value of depressive symptoms in patients with PSF and patients with severe depressive symptoms had less time to rehospitalisation for heart failure exacerbation.
Comparison of the levels of depressive symptoms in hospitalised heart failure patients in present study with those reported in a study of hospitalised heart failure patients in the USA reveals that Korean patients reported strikingly higher levels. In the study of American patients, the mean depression scores were 8·7 (SD 7·6) (Jiang et al. 2004, Westlake et al. 2005), whereas in the present study the average depression score was 18·7 (SD 10·6). The high levels of depressive symptoms in Korean patients warrant further investigation particularly because the importance of psychosocial factors has been underestimated in South Korea. It is also important to determine whether those results indicate a greater severity of depressive symptoms in Korean patients or differences in the way the BDI performs in these populations.
There are a few limitations to be acknowledged in this study. Firstly, the sample for this study included patients admitted to two university hospitals in South Korea and therefore may not be characteristic of all heart failure patients with PSF. Subsequently, caution should be used in generalising the findings before they are confirmed in other settings. Secondly, depressive symptoms were measured during hospitalisation, thus patients’ psychological status prior to admission was unknown. Longitudinal studies may understand pattern or changing in depressive symptoms from Korean patients with heart failure between hospital and home.
The results of this study have clinical implications. Firstly, the results indicate that rehospitalisation may be related to depressive symptoms. Accordingly, to prevent early rehospitalisation, a continual program for treating depressive symptoms from hospital to home should be implemented in heart failure patients with PSF. Close monitoring for severity of depressive symptoms in heart failure patients with PSF should also be emphasised in clinical practice. This emphasis is particularly important, because the focus has traditionally been on treatment of physical symptoms in hospitalised patients with heart failure (Koenig 1998).
Conclusion
Heart failure patients with PSF from South Korea with depressive symptoms are at increased risk for rehospitalisation. This is similar to the relationship of depressive symptoms to hospitalisation risk in patients with systolic dysfunction. This indicates that depressive symptoms of heart failure patients with PSF are equally at risk in those with systolic dysfunction. Interventions that begin in the hospital and continue to home settings may decrease high six-month rehospitalisation rate of heart failure patients with PSF.
Acknowledgement
The authors acknowledge with gratitude the editorial suggestions of Dr Magaret Storey, the most competent consultant of Professor Cho-ja Kim, and the cooperation of Dr Jae-joong Kim, MD.
Contributor Information
Eun Kyeung Song, College of Nursing, University of Kentucky, Lexington, KY, USA.
Terry A Lennie, College of Nursing, University of Kentucky, Lexington, KY, USA.
Debra K Moser, College of Nursing, University of Kentucky, Lexington, KY, USA.
References
- Ahmed A, Aronow WS, Fleg JL. Higher New York Heart Association classes and increased mortality and hospitalization in patients with heart failure and preserved left ventricular function. American Heart Journal. 2006;151:444–450. doi: 10.1016/j.ahj.2005.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT. Depression: Causes and treatments. Philadelphia, PA, USA: University of Pennsylvania Press; 1967. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York: Guilford Press; 1979. [Google Scholar]
- Bennett SJ, Pressler ML, Hays L, Firestine LA, Huster GA. Psychosocial variables and hospitalization in persons with chronic heart failure. Progress in Cardiovascular Nursing. 1997;12:4–11. [PubMed] [Google Scholar]
- Chin M, Goldman L. Correlates of early hospital readmission or death in patients with congestive heart failure. American Journal of Cardiology. 1997;79:1640–1644. doi: 10.1016/s0002-9149(97)00214-2. [DOI] [PubMed] [Google Scholar]
- Fonarow GC, Srikanthan P, Costanzo MR, Cintron GB, Lopatin M. An obesity paradox in acute heart failure: analysis of body mass index and inhospital mortality for 108,927 patients in the Acute Decompensated Heart Failure National Registry. American Heart Journal. 2007a;153:74–81. doi: 10.1016/j.ahj.2006.09.007. [DOI] [PubMed] [Google Scholar]
- Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, O’Connor CM, Sun JL, Yancy CW, Young JB. Characteristics, treatments and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. Journal of the American College of Cardiology. 2007b;50:768–777. doi: 10.1016/j.jacc.2007.04.064. [DOI] [PubMed] [Google Scholar]
- Goldberg R, Spencer F, Farmer C, Meyer T, Pezzella S. Incidence and hospital death rates associated with heart failure: a community-wide perspective. The American Journal of Medicine. 2005;118:728–734. doi: 10.1016/j.amjmed.2005.04.013. [DOI] [PubMed] [Google Scholar]
- Ha JW. Diastolic dysfunction and heart failure: a new paradigm. Korean Journal of Internal Medicine. 2003;65:631–637. [Google Scholar]
- Han SW, Ryu KH, Chae SC, Yang DH, Shin MS, Lee SH, Jeon ES, Oh BH, Choi D, Kim JJ, Shin DG, Ryu BS, Ahn YG. Multicenter analysis of clinical characteristics and prognostic factor of patients with congestive heart failure in Korea. Korean Circulation Journal. 2005;35:357–361. [Google Scholar]
- Havranek E, Spertus J, Masoudi F, Jones P, Rumsfeld J. Predictors of the onset of depressive symptoms in patients with heart failure. Journal of the American College of Cardiology. 2004;44:2333–2338. doi: 10.1016/j.jacc.2004.09.034. [DOI] [PubMed] [Google Scholar]
- Ho K, Anderson K, Kannel W, Grossman W, Levy D. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation. 1993;88:107–115. doi: 10.1161/01.cir.88.1.107. [DOI] [PubMed] [Google Scholar]
- Hogg K, Swedberg K, McMurray J. Heart failure with preserved left ventricular systolic function: epidemiology, clinical characteristic and prognosis. Journal of the American College of Cardiology. 2004;43:317–327. doi: 10.1016/j.jacc.2003.07.046. [DOI] [PubMed] [Google Scholar]
- Huang CH, Tsai MS, Hsieh CC, Wang TD, Chang WT, Chen WJ. Diagnostic accuracy of tissue Doppler echocardiography for patients with acute heart failure. Heart. 2006;92:1790–1794. doi: 10.1136/hrt.2006.089516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS, Blazing MA, Davenport C, Califf RM, Krishnan RR, O’Connor CM. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Archives of Internal Medicine. 2001;161:1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- Jiang W, Kuchibhatla M, Cuffe M, Christopher E, Alexander J, Clary G, Blazing M, Gaulden L, Califf R, Krishnan R, O’Connor C. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004;110:3452–3456. doi: 10.1161/01.CIR.0000148138.25157.F9. [DOI] [PubMed] [Google Scholar]
- Joynt KE, Whellan DJ, O’Connor CM. Why is depression bad for the failing heart? A review of the mechanistic relationship between depression and heart failure. Journal of Cardiac Failure. 2004;10:258–271. doi: 10.1016/j.cardfail.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Judge KW, Pawitan Y, Caldwell J, Gersh BJ, Kennedy JW. Congestive heart failure symptoms in patients with preserved left ventricular systolic function: analysis of the CASS registry. Journal of the American College of Cardiology. 1991;18:377–382. doi: 10.1016/0735-1097(91)90589-2. [DOI] [PubMed] [Google Scholar]
- Koenig HG. Depression in elderly hospitalized patients with medical illness. General Hospital Psychiatry. 1998;20:29–43. doi: 10.1016/s0163-8343(98)80001-7. [DOI] [PubMed] [Google Scholar]
- Korean Society of Heart Failure. Stem cell therapy in heart failure altered calcium handling in heart failure. South Korea: Seoul; 2004. [Google Scholar]
- Lee MM, Oh BH, Park HS, Chae SC, Lee SH, Kim JJ, Ahn YG, Jung MH, Han SW, Ryu KH. Multicenter analysis of clinical characteristics of the patients with congestive heart failure in Korea. Korean Circulation Journal. 2003;33:533–541. [Google Scholar]
- McDermott M, Feinglass J, Sy J, Gheorghiade M. Hospitalized congestive heart failure patients with preserved versus abnormal left ventricular systolic function: clinical characteristics and drug therapy. The American Journal of Medicine. 1995;99:629–635. doi: 10.1016/s0002-9343(99)80250-2. [DOI] [PubMed] [Google Scholar]
- Moller J, Brendorp B, Ottesen M, Kober L, Egstrup K, Poulsen S, Torp-Pedersen C Group BEiAMIT. Congestive heart failure with preserved left ventricular systolic function after acute myocardial infarction: clinical and prognostic implications. European Journal of Heart Failure. 2003;5:811–819. doi: 10.1016/s1388-9842(03)00159-4. [DOI] [PubMed] [Google Scholar]
- Moser DK, Worster PL. Effect of psychosocial factors on physiologic outcomes in patients with heart failure. The Journal of Cardiovascular Nursing. 2000;14:106–115. doi: 10.1097/00005082-200007000-00008. [DOI] [PubMed] [Google Scholar]
- Murberg TA. Long-term effect of social relationship on mortality in patients with congestive heart failure. International Journal of Psychiatry Medicine. 2004;34:207–217. doi: 10.2190/GKJ2-P8BD-V59X-MJNQ. [DOI] [PubMed] [Google Scholar]
- Murberg TA, Bru E, Svebak S, Tveteras R, Aarsland T. Depressed mood and subjective health symptoms as predictors of mortality in patients with congestive heart failure: a two-years follow-up study. International Journal of Psychiatry Medicine. 1999;29:311–326. doi: 10.2190/0C1C-A63U-V5XQ-1DAL. [DOI] [PubMed] [Google Scholar]
- Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA. Doppler tissue imaging: anoninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. Journal of the American College of Cardiology. 1997;30:760–768. doi: 10.1016/s0735-1097(97)00344-6. [DOI] [PubMed] [Google Scholar]
- Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ. Clinical utility of Doppler chocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures. Circulation. 2000;102:1788–1793. doi: 10.1161/01.cir.102.15.1788. [DOI] [PubMed] [Google Scholar]
- Parissis JT, Nikolaou M, Farmakis D, Bistola V, Paraskevaidis IA, Adamopoulos S, Filippatos G, Kremastinos DT. Clinical and prognostic implications of self-rating depression scales and plasma B-type natriuretic peptide in hospitalized patients with chronic heart failure. Heart. 2008;94:585–589. doi: 10.1136/hrt.2007.117390. [DOI] [PubMed] [Google Scholar]
- Petrie M, McMurray J. Changes in notions about heart failure. Lancet. 2001;358:432–434. doi: 10.1016/S0140-6736(01)05664-1. [DOI] [PubMed] [Google Scholar]
- Proctor E, Morrow-Howell N, Li H, Dore P. Adequacy of home care and hospital readmission for elderly congestive heart failure patients. Health & Social Work. 2000;25:87–96. doi: 10.1093/hsw/25.2.87. [DOI] [PubMed] [Google Scholar]
- Redwine LS, Mills PJ, Hong S, Rutledge T, Reis V, Maisel A, Irwin MR. Cardiac-related hospitalization and/or death associated with immune dysregulation and symptoms of depression in heart failure patients. Psychosomatic Medicine. 2007;69:23–29. doi: 10.1097/PSY.0b013e31802e2f35. [DOI] [PubMed] [Google Scholar]
- Rhee MK, Lee YH, Park SH, Sohn CH, Chung YC, Hong SK, Lee BK, Chang P, Yoon AR. A standardization study of Beck Depression Inventory 1-Korean version (K-BDI): reliability and factor analysis. The Korean Journal of Psychopathology. 1995;4:77–95. [Google Scholar]
- Sanderson JE. Heart failure with a normal ejection fraction. Heart. 2007;93:155–158. doi: 10.1136/hrt.2005.074187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz K, Elman C. Identification of factors predictive of hospital readmissions for patients with heart failure. Heart and Lung. 2003;32:88–99. doi: 10.1067/mhl.2003.15. [DOI] [PubMed] [Google Scholar]
- Senni M, Redfield M. Heart failure with preserved systolic function. A different natural history? Journal of the American College of Cardiology. 2001;38:1277–1282. doi: 10.1016/s0735-1097(01)01567-4. [DOI] [PubMed] [Google Scholar]
- Taylor JA, Christenson RH, Rao K, Jorge M, Gottlieb SS. B-type natriuretic peptide and N-terminal pro B-type natriuretic peptide are depressed in obesity despite higher left ventricular end diastolic pressures. American Heart Journal. 2006;152:1071–1076. doi: 10.1016/j.ahj.2006.07.010. [DOI] [PubMed] [Google Scholar]
- Terzi S, Sayar N, Bilsel T, Enc Y, Yildirim A, Ciloglu F, Yesilcimen K. Tissue Doppler imaging adds incremental value in predicting exercise capacity in patients with congestive heart failure. Heart and Vessels. 2007;22:237–244. doi: 10.1007/s00380-006-0961-x. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Kasl SV, Abramson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. Journal of the American College of Cardiology. 2001;38:199–205. doi: 10.1016/s0735-1097(01)01334-1. [DOI] [PubMed] [Google Scholar]
- Vasan R, Levy D. Defining diastolic heart failure: a call for standardized diagnostic criteria. Circulation. 2000;101:2118–2121. doi: 10.1161/01.cir.101.17.2118. [DOI] [PubMed] [Google Scholar]
- Vasan R, Larson E, Benjamin E, Evans J, Reiss C, Levt D. Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. Journal of the American College of Cardiology. 1999;33:1948–1955. doi: 10.1016/s0735-1097(99)00118-7. [DOI] [PubMed] [Google Scholar]
- Westlake C, Dracup K, Fonarow G, Hamilton M. Depression in patients with heart failure. Journal of Cardiac Failure. 2005;11:30–46. doi: 10.1016/j.cardfail.2004.03.007. [DOI] [PubMed] [Google Scholar]