Abstract
We prospectively examined whether the relationship between skeletal fragility and fracture risk in children 9.9 ± 0.3 (SD) yr is affected by trauma level. Bone size relative to body size and humeral vBMD showed similar inverse relationships with fracture risk, irrespective of whether fractures followed slight or moderate/severe trauma.
Introduction
Fracture risk in childhood is related to underlying skeletal fragility. However, whether this relationship is confined to low-trauma fractures or whether skeletal fragility also contributes to the risk of fracture caused by higher levels of trauma is currently unknown.
Materials and Methods
Total body DXA scan results obtained at 9.9 yr of age were linked to reported fractures over the following 2 yr in children from the Avon Longitudinal Study of Parents and Children. DXA scan results that were subsequently derived included total body less head (TBLH) bone size relative to body size (calculated from TBLH area adjusted for height and weight) and humeral volumetric BMD (vBMD; derived from subregional analysis at this site). Trauma level was assigned using the Landin classification based on a questionnaire asking about precipitating causes.
Results
Of the 6204 children with available data, 549 (8.9%) reported at least one fracture over the follow-up period, and trauma level was assigned in 280 as follows: slight trauma, 56.1%; moderate trauma, 41.0%; severe trauma, 2.9%. Compared with children without fractures, after adjustment for age, sex, socioeconomic status, and ethnicity, children with fractures from both slight and moderate/severe trauma had a reduced bone size relative to body size (1133 cm2 in nonfractured children versus 1112 cm2 for slight trauma fractures, p < 0.001; 1112 cm2 for moderate/severe trauma fractures, p = 0.001) and reduced humeral vBMD (0.494 g/cm3 in nonfractured children versus 0.484 g/cm3 for slight trauma fractures, p = 0.036; and 0.482g/cm3 for moderate/severe trauma fractures, p = 0.016).
Conclusions
Skeletal fragility contributes to fracture risk in children, not only in fractures caused by slight trauma but also in those that result from moderate or severe trauma.
Keywords: fractures, children, trauma levels, epidemiology, BMD, Avon Longitudinal Study of Parents and Children
INTRODUCTION
IN ADULTS, IT is well established that the occurrence of a fracture is associated with an increased risk of future fractures.(1) In individual people with low BMD, eliciting a history of fracture provides information about future fracture risk that can be helpful in informing decisions about osteoporosis management.(2) It is thought that the association between fracture history and risk of subsequent fracture is strongest for fractures that occur after relatively low levels of trauma, such as a fall from standing height. Conversely, bone fragility is generally assumed not to contribute toward the risk of fracture after high-energy injuries, such as road traffic injuries. In evaluating risk factors for osteoporosis, a history of fracture in childhood is often ignored on the assumption that such fractures are generally caused by relatively high levels of trauma. However, there is emerging evidence that fractures in childhood are related to underlying skeletal fragility.
In our recent prospective study based on the Avon longitudinal Study of Parents and Children (ALSPAC), fracture risk was inversely related to estimates of volumetric BMD (vBMD) derived from DXA-based measurements at the total body less head (TBLH) and humerus, as well as to bone size relative to body size as reflected by TBLH bone area adjusted for height and weight.(3) These findings are in line with results of a meta-analysis of 10 previous case control studies indicating an inverse association between BMD and fracture risk in childhood.(4) Taken together, these results suggest that fractures in childhood are related to underlying skeletal fragility. However, it is currently unclear whether this applies to all fractures or whether a subgroup of fractures associated with lower levels of trauma exists which explains this association.
A seminal paper on childhood injury epidemiology by Landin defined different levels of trauma in children based on analysis of 8682 fractures in Swedish children between 1950 and 1979. A classification method was developed based on descriptions of the events that surrounded these injuries.(5) Key features included height of fall, type of activity engaged in, and the use of equipment, and these features were used to classify fractures as after slight, moderate, or severe injury. To our knowledge, no previous study has investigated interrelationships between fracture risk, measures of skeletal fragility, and trauma level in children based on this or any other classification.
In our previous work on the ALSPAC cohort, we explored the association between skeletal fragility and fracture risk. As reported in our recent prospective study, we related DXA-based measures obtained at 9.9 yr of age to the risk of fracture over the following 2 yr.(3) In this paper, we studied whether the associations we observed depended on the level of trauma preceding the injury, as defined by a modified Landin classification. Our a priori hypothesis was that, whereas skeletal fragility would contribute to the risk of fracture after slight trauma in children, there is little or no association with skeletal fragility in the case of fractures that occur after moderate or severe trauma.
MATERIALS AND METHODS
Study population
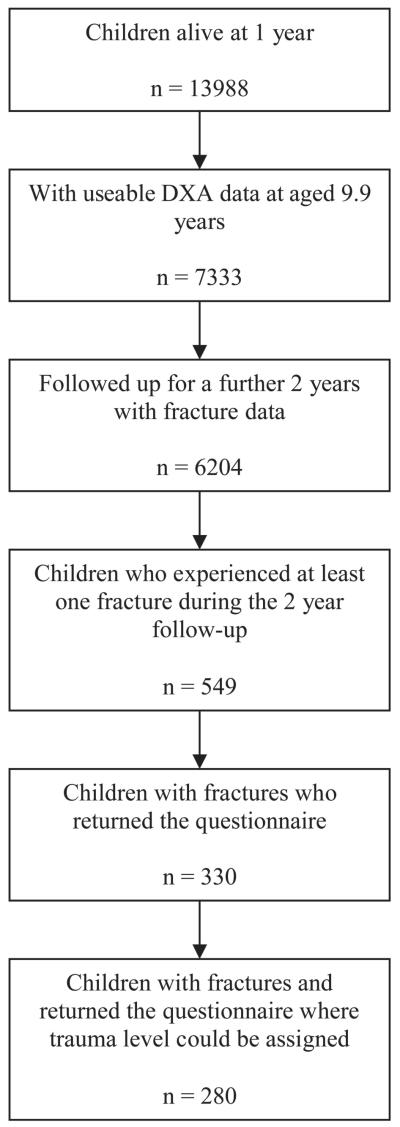
The ALSPAC is a geographically based UK cohort that recruited pregnant women residing in Avon (southwest England) with an expected date of delivery between April 1, 1991 and December 31, 1992. A total of 14,541 pregnancies were enrolled, with 14,062 children born (see www.alspac.bris.ac.uk for more information). Of these births, 13,988 children were alive at 12 mo (Fig. 1). This study is based on total body DXA scans performed at a research clinic to which the whole cohort were invited at a mean age of 9.8 yr, and 7725 children attended. Ethical approval was obtained from the ALSPAC Law and Ethics committees and the Central Office for Research Ethics Committees (COREC). Parental consent and child’s assent was obtained for all measurements made.
FIG. 1.
Flow diagram showing the children from ALSPAC included in this analysis.
Measure of height, weight, and DXA-derived parameters
At the research clinic, height was measured to the last complete millimeter using a Harpenden stadiometer. Weight was measured to the nearest 50 g using a Tanita Body Fat Analyzer (model TBF 305). TBLH bone area (TBLH BA) and TBLH BMC were measured using a Lunar Prodigy DXA in 7444 of the 7725 children. Total body DXA scans were not used because the head is not responsive to environmental stimuli such as exercise.(6) A total of 111 DXA scans were not interpretable because of the presence of large movement artifacts or other anomalies, yielding 7333 (98.5%) usable scans. The CV for TBLH BMC was 0.8% based on 120 repeat scans. To estimate TBLH vBMD, TBLH BMC was adjusted for height, weight, and TBLH BA. To estimate TBLH bone size relative to body size, TBLH BA was adjusted for height and weight. Regional DXA measurements at the right humerus were derived in a sample of 1385 children as previously described.(7) Humeral vBMD was estimated assuming the humerus was cylindrical by dividing humeral BMC by humeral volume derived from the product of humeral length and humeral cross-sectional area.
Fracture incidence and descriptions of events surrounding the injury
DXA results were linked to results of a questionnaire administered on subsequent attendance at research clinics ~12 and 24 mo later, where children were asked if they had broken a bone since they visited for their DXA scan. Children who indicated they had sustained a fracture were sent a further questionnaire to collect information on the nature and circumstances of the injury and for consent to obtain a copy of their X-ray report. There was an interval of up to 24 mo between the injury and return of the questionnaire. In those where radiology reports were available (~40%), 87% confirmed a fracture. For the rest of this study, it is reported fracture, not verified fracture, that is used as the outcome.
Data were collected using the additional questionnaire on height of any fall, landing surface, physical activity engaged in, and whether any equipment was being used. Children were assigned a trauma level category based on a modified Landin’s description (Table 1). Landin’s original description was altered by changing the categories of some sporting activities (e.g., skiing was moved to moderate trauma), by including landing surfaces, and by including falls down stairs or off beds. Some activities resulted in different injuries that could be classified in different categories. For example, in an injury occurring during gymnastics, if it involved a fall from >0.5 m or from equipment such as a balance beam it was categorized in the moderate trauma category. If the injury occurring during gymnastics involved a fall from <0.5 m, it was classified in the slight trauma category.
Table 1.
Three Descriptive Categories of Landin’s Modified Trauma Levels Used in This Study
| Descriptives indicating slight trauma |
| Falling to the ground from <0.5 m (standing height) |
| Falling to a resilient surface (rubber or sand) from 0.5 to 3 m |
| Falling from a bed or cot |
| Playing injuries including playground scuffles |
| Low-energy sporting injuries such as ball sports, wrestling, judo, karate, and gymnastics |
| Descriptives indicating moderate trauma |
| Falling to concrete or other nonresilient surface from 0.5 to 3 m |
| Flling from a bunkbed |
| Baby being dropped to the floor by an adult |
| Falling downstairs |
| Falling from a bicycle or horseback |
| Falling from swings or slides or similar playing equipment |
| Child being hit by a bicycle |
| Falls while moving on skateboards, skis, rollerblades, or skates |
| Descriptives indicating severe trauma |
| Falling from a height exceeding 3 m |
| All traffic accidents not already mentioned |
| Being hit by a moving heavy object |
Other methods
The mother’s, partner’s, and grandparent’s race and ethnic group were recorded by the mother on self-reported questionnaires sent out at ~32 wk of gestation. Sex was obtained from birth notifications. Mothers highest educational qualifications were also assessed at 32 wk of gestation and were coded on a five-point ascending scale where levels 1, 2, and 3 refer to educational qualifications generally gained at school by 16 yr of age, level 4 to qualifications gained at school at 18 yr of age, and level 5 to university degrees. Paternal social class was derived using the Office of Population Censuses and Surveys (OPCS) 1991 occupation-based classification, based on the fathers/partners current or last job at 32 wk of gestation.
Puberty was assessed by self-completion questionnaires using diagrams based on Tanner staging of pubic hair distribution for boys and girls and breast development for girls. At the time of the DXA scan and measurement of the anthropometric variables, the child’s baseline age was calculated from the date of birth and date of attendance at the research clinic. The amount of weekly vigorous physical activity was assessed by a self-completion questionnaire at 9.0 yr of age, asking how many times a week the child participated in a range of activities including running, dance, gymnastics, netball, swimming, and aerobics.
Statistical analyses
All statistical analyses were performed using STATA 8.0. A two-tailed unpaired t-test was used to test the null hypothesis of no difference between the children with and without fractures. Linear regression was used to assess the mean ± 95% CIs for the bone variables in children without fractures and in those with fractures caused by slight, moderate, or severe trauma. Models were initially run separately for boys and girls, but because no difference was seen, results are presented for both sexes combined. Models were run unadjusted and then adjusted for age, sex, ethnicity, and socioeconomic status (maternal education and paternal social class). Models were further adjusted for pubertal status and reported vigorous physical activity.
RESULTS
Of the 6204 children followed up for 2 yr, 549 (8.9%) experienced at least one fracture (Fig. 1). As previously reported,(3) 71.4% of fractures occurred in the upper limb; boys had a higher risk of fracture compared with girls; white children had a higher risk of fracture compared with non-white children; and children with fractures had a lower estimated humeral vBMD compared with children without fractures (Tables 2 and 3). Of these 549 who fractured, trauma level could be assigned in 280 (51%). The latter group was slightly younger than those with fractures where trauma level was not assigned and had a slightly lower TBLH BMD. Further analyses were based on these 280 children with fractures where trauma level could be assigned and the 5655 children without fractures: 56.1% of children fractured from slight trauma based on the descriptions in Table 1, 41.0% from moderate trauma, and 2.9% from severe trauma. Because only eight children had fractures associated with severe trauma, the categories for moderate and severe trauma were combined.
Table 2.
Number (%) of the Children With No Fractures and With Fractures Caused by Slight or Medium/Severe Trauma According to Sex, Ethnicity, and Maternal Education
| Children without fractures (N = 5655) [N (%)] |
Children with fractures (all) (N = 549) [N (%), p value*] |
Children with fractures and trauma levels (N = 280) [N (%)] |
Children with fractures caused by slight trauma (N = 157) [N (%), p value†] |
Children with fractures caused by moderate or severe trauma (N = 123) [N (%), p value‡] |
|
|---|---|---|---|---|---|
| Sex | |||||
| Male | 2745 (48.5) | 292 (53.2), 0.038 | 151 (53.9) | 81 (51.6), 0.451 | 70 (56.9), 0.066 |
| Female | 2910 (51.5) | 257 (46.8) | 129 (46.1) | 76 (48.4) | 53 (43.1) |
| Ethnicity | |||||
| White | 4965 (96.2) | 472 (98.1), 0.033 | 247 (99.2) | 140 (98.6), 0.143 | 107 (100), 0.041 |
| Non-white | 194 (3.8) | 9 (1.9) | 2 (0.8) | 2 (1.4) | 0 |
| Maternal education | |||||
| Level 1 | 645 (12.4) | 67 (13.6), 0.455 | 27 (10.6) | 16 (11.1), 0.727 | 11 (10.0), 0.288 |
| Level 2 | 420 (8.0) | 47 (9.5) | 27 (10.6) | 16 (11.1) | 11 (10.0) |
| Level 3 | 1842 (35.2) | 180 (36.5) | 92 (36.2) | 49 (34.0) | 43 (39.1) |
| Level 4 | 1451 (27.8) | 124 (25.2) | 63 (24.8) | 41 (28.5) | 22 (20.0) |
| Level 5 | 869 (16.6) | 75 (15.2) | 45 (17.7) | 22 (15.3) | 23 (20.9) |
p values are for the difference between all children with fractures compared with children without fractures.
p values are for the difference between children with fractures caused by slight trauma compared with those children without fractures.
p values are for the difference between children with fractures caused by moderate or severe trauma compared with children without fractures.
Table 3.
Mean (SD) Age, Height, Weight, TBLH BMC, TBLH BA, TBLH BMD, and Estimated Humeral vBMD of the Children With No Fractures and With Fractures Caused by Slight, Medium, or Severe Trauma
| Children with fractures (N = 5655) [mean (SD)] |
Children with fractures (all) (N = 549) [mean (SD), p value*] |
Children with fractures and trauma levels (N = 280) [mean (SD)] |
Children with fractures caused by slight trauma (N = 157) [mean (SD), p value†] |
Children with fractures caused by moderate or severe trauma (N = 123) [mean (SD), p value‡] |
|
|---|---|---|---|---|---|
| Age (yr) | 9.9 (0.3) | 9.9 (0.3), 0.276 | 9.8 (0.3)§ | 9.8 (0.3), 0.384 | 9.9 (0.3), 0.930 |
| Height (cm) | 139.6 (6.4) | 139.7 (5.9), 0.764 | 139.7 (6.0) | 139.1 (5.8), 0.404 | 140.5 (6.2), 0.117 |
| Weight (kg) | 34.6 (7.4) | 35.0 (7.3), 0.279 | 34.8 (7.4) | 33.6 (6.1), 0.072 | 36.4 (8.6), 0.010 |
| TBLH BMC (g) | 891 (185) | 884 (172), 0.392 | 872 (168) | 847 (152), 0.003 | 903 (182), 0.500 |
| TBLH BA (cm2) | 1137 (165) | 1136 (154), 0.861 | 1127 (152) | 1105 (138), 0.018 | 1154 (163), 0.264 |
| TBLH BMD (g/cm2) | 0.778 (0.055) | 0.773 (0.054), 0.053 | 0.768 (0.053) | 0.761 (0.051), <0.001 | 0.777 (0.055), 0.822 |
| Humeral vol density (cm3) | 0.495 (0.05) | 0.484 (0.05), <0.001 | 0.482 (0.05) | 0.483 (0.05), 0.005 | 0.481 (0.05), 0.004 |
Results are unadjusted.
p values are for the difference between all children with fractures compared with children without fractures.
p values are for the difference between children with fractures caused by slight trauma compared with those children without fractures.
p values are for the difference between children with fractures caused by moderate or severe trauma compared with children without fractures.
p value of 0.045 for difference between all children with fractures compared with those children with fractures who had a trauma level assigned.
p value of 0.037 for difference between all children with fractures compared with those children with fractures who had a trauma level assigned.
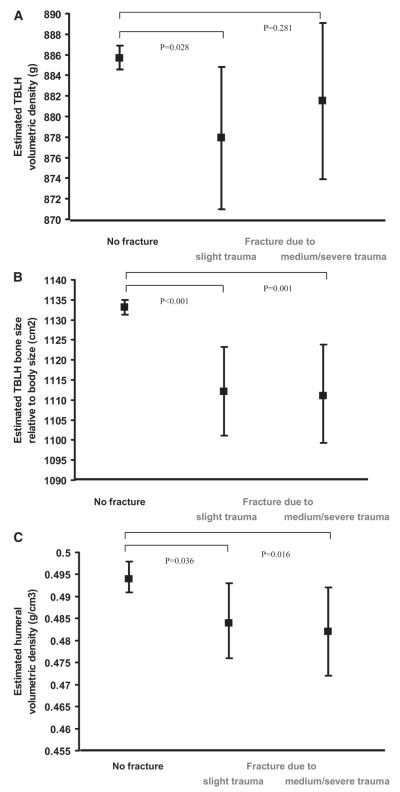
In unadjusted analyses, compared with children without fractures, children with fractures caused by slight trauma had lower TBLH BMC, BA, and BMD and humeral vBMD (Table 3). Children with fractures caused by moderate or severe trauma showed a similar reduction in humeral vBMD compared with children without fractures, whereas no reductions were seen in TBLH BMC, BA, and BMD. After adjustment for age, sex, socioeconomic status, and ethnicity, similar reductions in humeral vBMD relative to children without fractures were observed, irrespective of trauma level (Fig. 2C).
FIG. 2.
Box plots of mean (A) estimated TBLH vBMD, (B) TBLH bone size relative to body size, and (C) estimated humeral volumetric density with 95% CIs according to trauma level. Analyses were adjusted for age, sex, socioeconomic status, and ethnicity. p values are for the difference between means in those with fractures caused by slight or medium/severe trauma compared with those without fractures.
Further analyses were subsequently performed, based on our recent observation that fracture risk in childhood is inversely related to estimated TBLH vBMD (TBLH BMC adjusted for height, weight, and BA) and TBLH BA relative to body size (TBLH BA adjusted for height and weight).(3) Compared with children without fractures, estimated TBLH vBMD was reduced in those with fractures caused by slight trauma, whereas no decrease was seen in children with fractures caused by moderate or severe trauma (Fig. 2A). In contrast, TBLH bone size relative to body size showed similar reductions in children with fractures compared with those without, irrespective of trauma level (Fig. 2B). Similar results were obtained after adjustment for pubertal status or levels of physical activity (results not shown).
Finally, we explored differences between children reporting fractures related to slight compared with moderate or severe trauma. Interestingly, children reporting fractures caused by moderate or severe trauma were considerably (~8%) heavier than those with fractures caused by slight trauma (Table 3). In addition, children with fractures caused by moderate or severe trauma had a greater TBLH BMC, BA, and BMD compared with those with fractures caused by slight trauma. These differences in weight seemed to reflect in both higher fat and lean mass in children with moderate/severe trauma fractures, leading to a higher body mass index (BMI; Table 4). In terms of possible explanations for these differences, pubertal stage as reflected by Tanner stage and participation in physical activity were similar in children reporting fractures after light or moderate/severe trauma.
Table 4.
Number (%) of the Children Without Fractures and Those With Fractures Caused by Slight Trauma Compared With Those With Fractures Caused by Medium/Severe Trauma According to Tanner Stage of Puberty and Number of Episodes of Vigorous Physical Activity per Week
| Children with no fractures (N = 5655) |
Children with fractures caused by slight trauma (N = 157) [N (%), p value*] |
Children with fractures caused by moderate or severe trauma (N = 123) [N (%), p value†] |
p value for difference between children with fractures caused by slight trauma compared with moderate/severe trauma |
|
|---|---|---|---|---|
| Tanner stage | ||||
| 1 | 2950 (71.6) | 87 (74.4), 0.323 | 70 (74.5), 0.737 | 0.728 |
| 2 | 1034 (25.1) | 29 (24.8) | 22 (23.4) | |
| 3 or more | 137 (3.3) | 1 (0.8) | 2 (2.1) | |
| Physical activity episodes per week | ||||
| <3 | 1867 (56.5) | 34 (42.5), 0.036 | 36 (48.7), 0.347 | 0.554 |
| 4–6 | 965 (29.2) | 29 (36.3) | 27 (36.5) | |
| ≥7 | 473 (14.3) | 17 (21.3) | 11 (14.9) | |
|
| ||||
| Mean (SD) | Mean (SD) | |||
|
| ||||
| Fat mass (kg) | 8.5 (5.1) | 7.9 (5.3), 0.120 | 9.6 (5.3), 0.020 | 0.007 |
| Lean mass (kg) | 24.5 (3.2) | 24.1 (3.1), 0.129 | 25.1 (3.1), 0.039 | 0.007 |
| BMI (kg/m2) | 17.7 (2.9) | 17.3 (3.0), 0.099 | 18.3 (3.0), 0.015 | 0.005 |
Data are also presented as mean (SD) for fat mass, lean mass, and BMI of the children with fractures caused by slight trauma compared with those without fractures and those with fractures caused by medium/severe trauma.
p values are for the difference between children with no fractures and those with fractures caused by slight trauma.
p values are for the difference between children with no fractures and those with fractures caused by moderate/severe trauma.
DISCUSSION
In our recent prospective study, we found that fracture risk in childhood is related to parameters of skeletal fragility such as TBLH vBMD, TBLH bone size relative to body size, and humeral vBMD.(3) Here, we studied whether associations between these parameters and fracture risk are influenced by the level of trauma preceding the fracture. As expected, in those 157 children whose fracture followed slight trauma, the above parameters of skeletal fragility were inversely related to fracture risk compared with children without fractures. However, perhaps surprisingly, a similar inverse relationship between fracture risk and TBLH bone size relative to body size, and humeral vBMD, was observed in the 123 children with moderate or severe trauma preceding their fracture.
Based on these findings, we concluded that fracture risk in childhood is related to underlying skeletal fragility, even at relatively high trauma levels, although greater skeletal fragility is seen in children who fracture because of slight trauma. As far as we are aware, this is the first study to investigate the relationship between fracture risk in childhood and measures of skeletal fragility according to trauma level. Our conclusions may also apply to adults, in light of preliminary data suggesting that, in a population of 5995 older men, total hip and lumbar spine BMD measurements were equally predictive of low and high trauma fractures.(8)
Although our overall results suggested that underlying skeletal fragility contributes to the risk of fracture in children after moderate or severe trauma, contrary to this conclusion, TBLH BMC, BA, and TBLH vBMD were not reduced in this group compared with children without fractures. This apparent discrepancy may have reflected the fact that the majority of fractures over the follow-up period were of the upper limb, which may be only weakly related to measures of skeletal fragility as assessed at the whole body. Consistent with this conclusion, when vBMD was ascertained at the upper limb in children with fractures after moderate or severe trauma, as reflected by humeral vBMD, this was found to be reduced compared with children without fractures, to a similar extent to that in children with fractures after slight trauma.
One unexpected observation was that children with fractures caused by moderate or severe trauma were considerably heavier than those with fractures caused by slight trauma, because of a combination of greater fat and lean mass. Consistent with the strong associations we have previously found between both fat and lean mass with bone size and bone mass,(9) children with fractures caused by moderate or severe trauma also had a greater TBLH BA and BMC compared with those with slight trauma. Nevertheless, bone size relative to body size was reduced to a similar extent in both fracture groups, implying that, despite the higher TBLH BA and BMC in children with fractures caused by moderate or severe trauma, this is insufficient to compensate for their greater body weight. This apparent deficiency in bone size relative to body size in children with fractures caused by moderate or severe trauma, despite their relatively high body weight, is consistent with previous findings that increased weight is a risk factor for fracture in childhood.(10-12)
We are not aware of any previous reported weight differences in children with fractures according to trauma level. We recently found that fracture risk in this cohort is positively related to reported participation in vigorous physical activity,(13) consistent with previous observations that sports participation is associated with an increased risk of fractures in children.(14-17) To the extent that larger children are more likely to participate in vigorous team-based sporting activities, this may explain why children who fracture from moderate or severe trauma are relatively heavy. However, no differences in participation in physical activity were observed according to trauma level that might explain our results. Similarly, our findings were not explained by other possible confounding factors such as socioeconomic status as reflected by level of maternal education, or differences in pubertal development, although unmeasured confounding cannot be excluded in this observational study, particularly as the self-reported measures of Tanner stage of puberty used in ALSPAC have not been validated. After adjustment for potential confounders (age, sex, socioeconomic status, and ethnicity), the direction of association between humeral vBMD, for example, and fracture risk according to trauma level did not change, but the statistical strength of association decreased as would be expected with increasing the number of parameters in the regression equation.
The descriptive categorization of trauma levels used in this study may have had limitations. For example, data on the injury producing a fracture was collected some time after the events, and so recall bias cannot be excluded. Although the original Landin classification had several drawbacks, we attempted to address these by developing a modified classification. In particular, we incorporated activities that are now more common (e.g., trampolining, use of microscooters) and revised the classification of injuries related to activities such as skiing, skateboarding, and rollerskating from the slight to moderate trauma category in view of the high speeds and forces involved in any subsequent fall. In addition, we included landing surfaces in the categorization, which are important in determining the outcome after a fall, with concrete being particularly unforgiving.(18,19) However, it was not possible to address other limitations, such as the inability to account for the degree of torque exerted on the upper limb after a fall, depending on how far the limb is outstretched.
Trauma levels could only be assigned in ~50% of children reporting fractures, because of a restricted number of children returning fracture questionnaires. Those who returned questionnaire data may not have been entirely representative of the childhood fracture population, because children with fractures in whom trauma levels could be assigned were slightly younger than those in whom it could not. This age difference may also have been responsible for the small differences in TBLH and humeral BMD that were present between these two groups. However, such differences were relatively small. Although self-selection of subjects may have contributed to the reduction in humeral BMD in children reporting fractures after moderate/severe trauma compared with children without fractures, self-selection is unlikely to be solely responsible, particularly because this reduction persisted after age adjustment.
Another limitation of this study is the drop-out rate. Only 44.4% of the original ALSPAC cohort were followed up for this 2-yr study, which may have introduced bias as there was a preferential loss of children from families of lower socioeconomic status (results not shown). Additionally, although 87% of participants in whom we were able to obtain copies of the X-ray reports were confirmed as having a fracture, we were not able to verify reported fractures in all cases. It is inevitable that a small number of children were wrongly classified as having a fracture, but this random misclassification is likely to have resulted in an underestimation of the true association between trauma level, BMD, and fracture risk, rather than produce a spurious result.
In conclusion, we studied whether underlying skeletal fragility, as assessed in a large cohort of 9-yr-old children, is related to subsequent risk of fracture after moderate or severe, as well as slight, trauma. Bone size relative to body size and humeral vBMD were reduced to a similar extent in children with fractures after moderate/severe or slight trauma compared with children without fractures. These findings indicate that at least in children, underlying skeletal fragility is a contributory factor even in fractures caused by moderate or severe trauma. Additionally, we observed that children with fractures caused by moderate or severe trauma were considerably heavier than those with fractures caused by slight trauma. Therefore, although skeletal fragility seems to affect the risk of fracture after slight and moderate/severe trauma to a similar extent, other important differences are likely to exist in the causation of fractures at high and low trauma levels.
ACKNOWLEDGMENTS
We are extremely grateful to all the families who took part in this study, the midwives for help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses. The UK Medical Research Council, the Wellcome Trust, and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors, and Emma Clark will serve as guarantor for the contents of this paper. This research was specifically funded by the Wellcome Trust.
Footnotes
The authors state that they have no conflicts of interest.
REFERENCES
- 1.Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375–382. doi: 10.1016/j.bone.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 2.van Staa TP, Geusens P, Kanis JA, Leufkens HG, Gehlbach S, Cooper C. A simple clinical score for estimating the long-term risk of fracture in post-menopausal women. QJM. 2006;99:673–682. doi: 10.1093/qjmed/hcl094. [DOI] [PubMed] [Google Scholar]
- 3.Clark EM, Ness AR, Bishop NR, Tobias JH. The association between bone mass and fractures in children: A prospective cohort study. J Bone Miner Res. 2006;21:1489–1496. doi: 10.1359/jbmr.060601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clark EM, Tobias JH, Ness A. Association between bone density and fractures in children: A systematic review and meta-analysis. Pediatrics. 2005;117:e291–e297. doi: 10.1542/peds.2005-1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Landin LA. Fracture patterns in children. Acta Orthop Scand. 1983;202:1–109. [PubMed] [Google Scholar]
- 6.Taylor A, Konrad PT, Norman ME, Harcke HT. Total body BMD in young children: Influence of head BMD. J Bone Miner Res. 1997;12:625–655. doi: 10.1359/jbmr.1997.12.4.652. [DOI] [PubMed] [Google Scholar]
- 7.Clark EM, Ness AR, Tobias JH. Gender differences in the ratio between humerus width and length are established prior to puberty. Osteoporos Int. 2007;18:463–470. doi: 10.1007/s00198-006-0275-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mackey DC, Cummings SR, Bauer DC, Cawthon PM, Lewis C, Barrett-Connor E. High trauma fractures in men are associated with low bone mineral density. J Bone Miner Res. 2006;21:S1–S69. [Google Scholar]
- 9.Clark EM, Ness AR, Tobias JH, Study Team ALSPAC Adipose tissue stimulate bone growth in prepubertal children. J Clin Endocrinol Metab. 2006;91:2534–2541. doi: 10.1210/jc.2006-0332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skaggs DL, Loro ML, Pitukcheewanont P, Tolo V, Gilsanz V. Increased body weight and decreased radial cross-sectional dimensions in girls forearm fractures. J Bone Miner Res. 2001;16:1337–1342. doi: 10.1359/jbmr.2001.16.7.1337. [DOI] [PubMed] [Google Scholar]
- 11.Mobley SL, Ha E, Landoll JD, Badenhop-Stevens NE, Clairmont A, Goel P, Matkovic V. Children with bone fragility fractures have reduced bone mineral areal density at the forearm and hip and higher percent body fat. J Bone Miner Res. 2005;20:S34. [Google Scholar]
- 12.Goulding A, Jones IE, Taylor RW, Williams SM, Manning PJ. BMD and body composition in boys with distal forearm fractures: A DXA study. J Pediatr. 2001;139:509–515. doi: 10.1067/mpd.2001.116297. [DOI] [PubMed] [Google Scholar]
- 13.Clark EM, Ness AR, Tobias JH. Vigorous physical activity at age 9 increases the risk of childhood fractures, despite increasing bone mass. Rheumatol. 2007;46(suppl 1):i3. [Google Scholar]
- 14.Ma DQ, Jones G. Soft drink and milk consumption, physical activity, bone mass and upper limb fractures in children: A population-based case-control study. Calcif Tiss Int. 2004;75:286–291. doi: 10.1007/s00223-004-0274-y. [DOI] [PubMed] [Google Scholar]
- 15.Ma DQ, Jones G. TV, computer and video playing, physical activity and upper limb fracture risk in children: A population-based case-control study. J Bone Miner Res. 2003;18:1970–1977. doi: 10.1359/jbmr.2003.18.11.1970. [DOI] [PubMed] [Google Scholar]
- 16.Lyons RA, Delahunty AM, Krause D, Heaven M, McCabe M, Allen H, Nash P. Childrens fractures: A population-based study. Inj Prev. 1999;5:129–132. doi: 10.1136/ip.5.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loud KJ, Gordon CM, Micheli LJ, Field AE. Correlates of stress fractures among preadolescents and adolescent girls. Pediatrics. 2005;115:e399–e406. doi: 10.1542/peds.2004-1868. [DOI] [PubMed] [Google Scholar]
- 18.Cummins BH, Potter JM. Head injuries due to falls from heights. Injury. 1970;2:61–64. doi: 10.1016/s0020-1383(70)80120-6. [DOI] [PubMed] [Google Scholar]
- 19.Garretson LK, Gallagher SS. Falls in children and youth. Pediatr Clin North Am. 1985;32:153–162. doi: 10.1016/s0031-3955(16)34763-0. [DOI] [PubMed] [Google Scholar]