Abstract
Aims
To describe the effects of tolvaptan therapy on dyspnoea relief based on timing of delivery, influence of concomitant therapies, and baseline patient and clinical characteristics. Also, the influence of clinical trial design on dyspnoea measurement, from the Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) trials.
Methods and results
Post hoc analysis was performed based on the endpoint of patient-assessed dyspnoea. Changes from baseline at inpatient Day 1 were compared between treatment groups by the van Elteren test. Pre-determined subgroup analyses were also performed. Tolvaptan's effects are greatest within 12 h after first dose with an additional, but modest dyspnoea improvement benefit irrespective of time after admission. Overall, patients continue to report dyspnoea improvement up to 60 h after admission. The window of enrolment, up to 48 h after admission, combined with measurement on ‘Day 1’ led to a wide range over when dyspnoea was assessed.
Conclusion
Post hoc analysis suggests that tolvaptan modestly improves dyspnoea compared with standard therapy alone, regardless if given early or relatively late after hospitalization, and also across major pre-specified subgroups, despite ongoing background therapy aimed at relieving signs and symptoms. Significant variability around when dyspnoea was assessed, in addition to the persistence of dyspnoea despite ongoing background therapy, may influence how future clinical trials assess dyspnoea in acute heart failure syndromes.
Keywords: Acute heart failure syndromes, Heart failure, Dyspnoea, Vasopressin antagonists, Clinical trials
Introduction
The sensation of breathlessness, or dyspnoea, is nearly universal in patients who present with acute heart failure syndromes (AHFS).1,2 Relief from this symptom prompts patients to seek medical care. Given the prevalence of dyspnoea in AHFS, its relief is important to both patients and clinicians, and its role in regulatory approval has resulted in this symptom being targeted in clinical trials.3–12
Only two Phase III randomized controlled trial programmes have demonstrated statistically significant improvement in dyspnoea, the Vasodilation in the Management of Acute CHF (VMAC) trial and the Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) short-term clinical status trials. VMAC improved dyspnoea with nesiritide vs. placebo (but not vs. nitroglycerin) at 3 h (∼73 vs. ∼63%).5 No statistically significant improvement was seen at 24 h vs. nitroglycerin and the mild benefit over nitroglycerin was seen primarily in those patients who received invasive haemodynamic monitoring.13 In EVEREST, tolvaptan plus standard therapy demonstrated statistically significant improvement in patient-assessed dyspnoea at Day 1 in both short-term trials; however, the absolute benefit was modest.3 Neither VMAC nor EVEREST demonstrated a long-term benefit in either morbidity or mortality.5,14
Despite the lack of long-term mortality benefit, dyspnoea relief remains an important goal. The influence of clinical trial design on dyspnoea measurement, as well as the effects of the timing of therapy, concomitant therapies, and baseline patient and clinical characteristics, has not been previously well described from a large clinical trial database. Post hoc analysis of the EVEREST database was performed to answer the following questions: (i) how soon is an effect seen and what is its duration in relation to first dose? (ii) does tolvaptan's effect diminish with increased duration of standard therapy as determined by time of dose post-admission? (iii) what is tolvaptan's effect on dyspnoea across multiple pre-defined subgroups? (iv) what is the relationship between tolvaptan's effect on dyspnoea and other standard measures of heart failure (HF) status (e.g. oedema and NYHA class)? and (v) What is the influence of protocol design on dyspnoea measurement and assessment irrespective of treatment arm?
Methods
The study design and overall findings from the EVEREST trials have been described previously.3,14,15 Briefly, this prospective, international, randomized, double-blind, placebo-controlled trial examined the short- and long-term efficacy and safety of tolvaptan when added to optimal medical therapy including loop diuretics in adults ≥18 years of age with chronic HF [left ventricular ejection fraction (EF) ≤ 40%], who were hospitalized for worsening HF, with two or more signs of fluid overload [dyspnoea, oedema and/or jugular venous distention (JVD)] who were randomized within 48 h of hospitalization to oral tolvaptan (30 mg/day) or matching placebo. Two identical short-term trials took place during the inpatient period, with one long-term outcome study combining all 4133 randomized patients. The secondary endpoints in the two short-term trials focused on improvements in signs and symptoms of heart failure, including patient-assessed dyspnoea at Day 1 following initiation of study therapy in patients with either frequent or continuous dyspnoea at rest or with minimal exertion at time of enrolment as assessed by the investigator.
Patient-assessed dyspnoea was measured on the first calendar day (Day 1) following the first dose of study therapy by asking the patient to answer the following question: ‘Compared to how much difficulty you were having with your breathing just before study drug was started, how is your breathing now?’ Answers were provided using a seven-point Likert scale (markedly better, moderately better, minimally better, no change, minimally worse, moderately worse, and markedly worse). The patient was instructed to read the question and answer it by marking the appropriate box using an ink pen, and then to initial and date the form. To avoid potential bias, neither the study staff nor the healthcare team was allowed to discuss or assist the subject in completing the patient-assessed dyspnoea status with the exception that if the patient was illiterate, the scale could be read to the patient.
Timing of the Day 1 study visit in EVEREST (the time to perform patient-assessed dyspnoea) was specified by protocol to be anytime on the calendar day after the first dose of study drug. As the time of day of randomization to study drug and first dose of study drug was not specified by protocol, first dose could occur at any hour on Day 0 of the study. For these reasons, the timing of patient-assessed dyspnoea in relation to first dose of study medication varied by patient, resulting in patient-assessed dyspnoea assessments being performed over a range of times from a few hours post-dose to over 24 h. Additionally, as patients were randomized to study drug up to 48 h following hospital admission, patient-assessed dyspnoea assessment was performed within 1 day to over 3 days after hospitalization.
Statistical analysis
Secondary endpoints in the short-term EVEREST trials were ordered in a tiered analysis, such that at least one of the endpoints in each of the tiers were required to demonstrate significance at a value of P < 0.05 prior to analysis of the next tier. Both pre-specified and post hoc subgroup analyses were performed on the pooled population from the EVEREST short-term clinical status trials A and B to further explore the effects of tolvaptan on patient-assessed dyspnoea.
Of the pre-specified subgroups, the following are reported:
Demographic: sex, race, and age < and >65.
Co-morbidities: ischaemic vs. non-ischaemic aetiology.
Baseline status: severe oedema (++ and +++) vs. no or minimal oedema (<++), >9 cm H2O JVD vs. <10 cm H2O, and ‘frequent/continuous’ vs. ‘no/seldom’ dyspnoea, EF by median, and blood pressure comparison by quartile.
Chemistry and neurohormones by quartile: blood urea nitrogen (BUN), serum creatinine, and B-type natriuretic peptide.
Baseline (prior to randomization) concomitant therapy use: in-hospital median daily furosemide dose.
Additional post hoc subgroup analyses were performed on the following subgroups with these baseline variables: creatinine ≥2 or <2, BUN ≥ 40 or <40, and sodium ≥135 or <135 mEq/L.
Patient-assessed dyspnoea was a pre-specified secondary endpoint and was evaluated in 3664 of the 4133 total subjects in the EVEREST trial using a patient-assessed, seven-point Likert scale administered on Day 1 after randomization. Separately, physician-assessed dyspnoea, orthopnoea, oedema, and JVD were evaluated using a four-level rating at the time of randomization and subsequently at each inpatient day, and also at each outpatient visit. Body weight was also assessed at each patient visit. To establish the convergent validity of the patient-assessed Likert scale for dyspnoea, correlations were sought with each of these direct and indirect measures of congestion. Spearman's correlation coefficient, rather than Pearson's, was used to describe this more general relationship rather than a strict linear one.
In order to explore the effects of tolvaptan on patient-assessed dyspnoea relative to time after administration of first dose, post hoc analysis was conducted by the following times following first dose: <12, >12 to ≤16, >16 to ≤20, >20 to ≤24, and >24 h. These groups were chosen based on visual inspection of apparent groupings, which emerged secondary to the analysis.
Further analyses to determine tolvaptan's effects on dyspnoea relative to time after hospital admission were performed. Patient-assessed dyspnoea was compared between tolvaptan- and placebo-treated patients by time from hospital admission: ≤36, >36 to ≤60, and >60 h after hospitalization. Of note, these times did not include time spent in the emergency department or pre-hospital care. Categories were selected based on visual inspection of the time distribution of assessment.
Patient-assessed dyspnoea for all pre-specified and post hoc subgroups were compared between treatment groups by the non-parametric van Elteren test,16 to allow for more robust distribution assumptions with centre as the stratification factor, in patients with frequent or continuous dyspnoea at baseline. The overall per cent improved by category was analysed for each subgroup.
Statistical analyses were performed with SAS software, version 8.2 (SAS Institute Inc., Cary, NC, USA) and were conducted by the study sponsor.
Results
Baseline characteristics of the population sample related to dyspnoea assessments
Table 1 illustrates the baseline characteristics of the population and outlines in detail the absolute numbers represented graphically in Figures 2–4. The majority of patients were NYHA class III with significant signs of congestion at baseline, without significant variation between subgroups defined by timing of Day 1 assessments.
Table 1.
Baseline characteristics by dyspnoea subgroup defined by timing of patient-assessed dyspnoea
| Baseline characteristic | Overall |
Time post-hospital admission (h) |
Time post-first dose (h) |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤36 |
36–60 |
>60 |
≤12 |
12–16 |
16–20 |
20–24 |
>24 |
|||||||||||
| TLV | PLC | TLV | PLC | TLV | PLC | TLV | PLC | TLV | PLC | TLV | PLC | TLV | PLC | TLV | PLC | TLV | PLC | |
| Number of patientsa | 2072 | 2061 | 453 | 430 | 993 | 979 | 412 | 423 | 33 | 38 | 190 | 197 | 658 | 655 | 850 | 831 | 124 | 109 |
| Number of patients with baseline dyspnoea | 1835 | 1829 | 431 | 406 | 921 | 905 | 361 | 376 | 29 | 36 | 175 | 185 | 636 | 605 | 771 | 781 | 112 | 91 |
| NYHA class III/IV (%) | 59/39 | 58/40 | 55/45 | 57/43 | 62/38 | 57/42 | 61/38 | 65/35 | 67/33 | 55/45 | 54/46 | 60/39 | 59/41 | 56/43 | 61/39 | 60/40 | 68/31 | 65/33 |
| Dyspnoea | ||||||||||||||||||
| Frequent (%) | 60 | 61 | 57 | 60 | 66 | 63 | 59 | 63 | 58 | 63 | 56 | 60 | 60 | 57 | 65 | 67 | 63 | 55 |
| Continuous (%) | 29 | 28 | 38 | 34 | 26 | 29 | 28 | 25 | 30 | 32 | 37 | 29 | 33 | 34 | 25 | 26 | 23 | 24 |
| JVD ≥10 cm, no. (%) | 27 | 27 | 32 | 33 | 25 | 27 | 25 | 19 | 18 | 27 | 32 | 31 | 28 | 27 | 24 | 27 | 23 | 18 |
| Rales, no. (%) | 81 | 82 | 84 | 81 | 82 | 84 | 77 | 80 | 91 | 100 | 79 | 86 | 82 | 82 | 81 | 82 | 81 | 79 |
| Pedal oedema, no. (%) | 79 | 79 | 81 | 80 | 80 | 81 | 77 | 79 | 69 | 76 | 84 | 83 | 80 | 80 | 80 | 81 | 70 | 72 |
aOne hundred and seven-three tolvaptan/192 placebo patients were excluded from analyses for time post-first dose and 170 tolvaptan/190 placebo were excluded from time post-admission analyses due to missing data variables necessary to calculate timing.
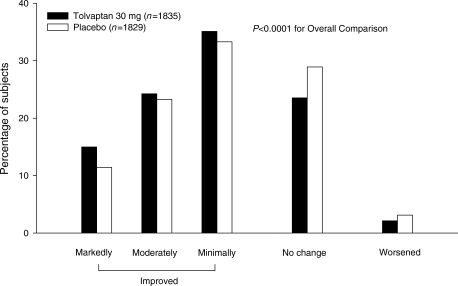
Figure 1.
Patient-assessed dyspnoea status at inpatient Day 1 in the combined EVEREST trial population. Note. Patients with continuous or frequent dyspnoea at baseline; Patients were asked ‘Compared to how much difficulty you were having with your breathing just before trial drug was started, how is your breathing now?’; Worsened includes minimally worse, moderately worse, and markedly worse. Reproduced with permission from Gheorghiade et al.3 Copyright © (2007), American Medical Association. All Rights reserved.
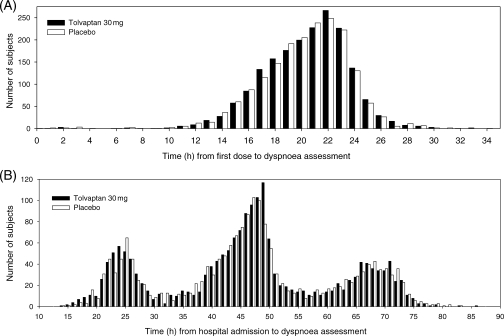
Figure 2.
Timing of patient-assessed dyspnoea measurement relative to first dose or hospital admission. (A) Timing of patient assessment of dyspnoea relative to dosing by treatment group. (B) Timing of patient assessment of dyspnoea relative to time of hospital admission by treatment group.
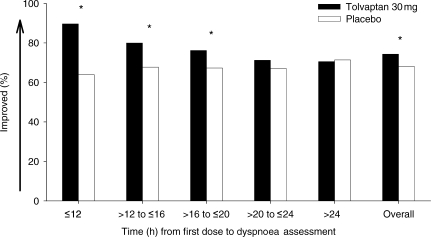
Figure 3.
Patient-assessed dyspnoea as a function of time from first dose of study drug. *P < 0.05 van Elteren test.
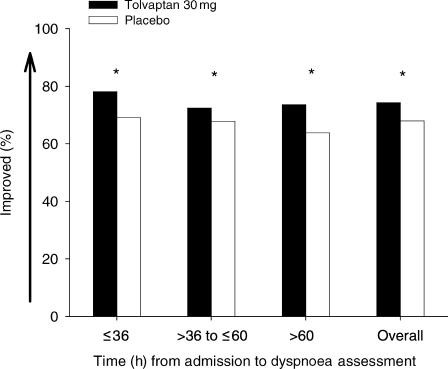
Figure 4.
Patient-assessed dyspnoea as a function of time from hospital admission. *P < 0.05 van Elteren test.
As reported in the primary EVEREST analysis, in subjects with physician-assessed dyspnoea at baseline (88.6% of tolvaptan and 88.7% of placebo patients), tolvaptan, compared with placebo, was associated with improved patient-assessed dyspnoea on inpatient Day 1 [1364/1835 (74.3%) vs. 1243/1829 (68.0%), P < 0.0001].3 For those subjects with frequent or continuous dyspnoea as initially determined by the physician, self-reported dyspnoea is shown graphically in Figure 1. Dyspnoea improved regardless of the severity of the subjects' baseline dyspnoea status; however, the greatest treatment differences were seen in subjects with continuous dyspnoea at baseline (Table 2).
Table 2.
Patient-assessed dyspnoea treatment response by severity of dyspnoea at baseline
| Baseline dyspnoea status | TLV/PLC, n | % improved |
Treatment group difference (%) | P-value | |
|---|---|---|---|---|---|
| Tolvaptan | Placebo | ||||
| Seldoma | 153/164 | 71.89 | 70.12 | 1.77 | 0.6934 |
| Frequent | 1247/1244 | 73.62 | 69.05 | 4.57 | 0.0013 |
| Continuous | 588/585 | 75.95 | 65.65 | 10.30 | 0.0021 |
Note: baseline dyspnoea status determined by investigator. Per cent improved based on patient self-assessment.
aNot included in overall analyses.
Assessment of dyspnoea as a function of time from first dose
Figure 2 depicts the timing of patient-assessed dyspnoea in EVEREST. The timing of dyspnoea assessment was tri-modal relative to initial hospitalization, with each mode separated by ∼24 h. This suggests that most dyspnoea assessments and trial enrolments were performed during daytime hours, as expected for a clinical trial. Patients were divided post hoc into five groups, based on time (in hours) of dyspnoea assessment after the first dose of tolvaptan. Figure 3 represents the percentage of patients reporting improvement in dyspnoea overall, as well as any improvement at different time points. The percentage improvement with placebo in addition to standard medical therapy stays relatively constant, whereas improvement with tolvaptan in addition to standard medical therapy appears greatest when measured early (P < 0.05, van Elteren test, Figure 3). The majority of patients in the study had an improvement in dyspnoea at all time points relative to hospital admission, with a statistically higher rate with tolvaptan compared with placebo in addition to standard medical therapy (P < 0.05, van Elteren test, Figure 4).
Correlations between dyspnoea findings and other measures of congestion
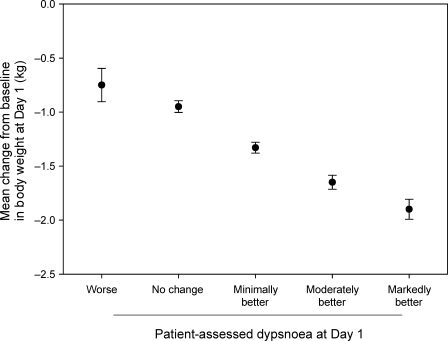
Physician-assessed measurements of congestion such as orthopnoea, JVD, oedema, and body weight demonstrate statistically significant associations with patient-assessed dyspnoea (Table 3). Although the correlation coefficients are <0.5, given this is a comparison of multiple different endpoints, there is a modest correlation. Physician-assessed dyspnoea and NYHA class was weakly correlated with patient-assessed dyspnoea. The association between patient-assessed dyspnoea status at inpatient Day 1 and change from baseline in body weight at Day 1 in the overall population is further represented in Figure 5, illustrating the linear association between reductions in body weight and improvements in patient-assessed dyspnoea.
Table 3.
Convergent validity of patient-assessed dyspnoea in the EVEREST trial at Day 1
| Reference measure (Day 1) | Patient-assessed dyspnoea | P-value |
|---|---|---|
| Spearman's correlationa | ||
| Physician-assessed dyspnoea | 0.289 | <0.0001 |
| Physician-assessed orthopnoea | 0.214 | <0.0001 |
| Physician-assessed JVD | 0.157 | <0.0001 |
| Physician-assessed oedema | 0.155 | <0.0001 |
| Body weight | 0.200 | <0.0001 |
|
χ2 associationb NYHA class |
198.17 | <0.0001 |
aSpearman's correlations between patient self-assessed dyspnoea and changes in physician-assessed signs/symptoms and body weight at Day 1 (all patients).
bχ2 test on association. For patient-assessed dyspnoea, improved = markedly/moderately better, unchanged = minimally better/no change/minimally worse, and worsened = moderately/markedly worse.
Figure 5.
Association between patient-assessed dyspnoea status and body weight change at inpatient Day 1. Note: worse includes minimally worse, moderately worse, and markedly worse. For association between weight change and treatment: P < 0.0001 for dyspnoea status adjusted for treatment; P < 0.0001 adjusted for dyspnoea status; and P = 0.3008 for dyspnoea–treatment interaction.
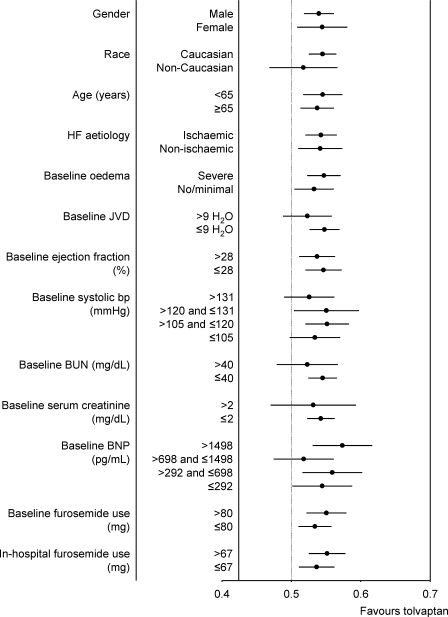
Subgroup analysis
Overall, effects on patient-assessed dyspnoea at Day 1 were consistent in all of the 67 pre-specified subgroups assessed in the EVEREST programme (Figure 6).
Figure 6.
Patient-assessed dyspnoea response by baseline subgroup represented as treatment effect (>0.5 favours tolvaptan) and 95% confidence interval.
Discussion
Tolvaptan, when added to standard therapy, is associated with a modest dyspnoea improvement compared with standard therapy alone within the first 12 h of first dose administration. This effect persists up to 20 h; however, the magnitude of benefit diminishes with time. Importantly, the first dose of tolvaptan may have occurred, per protocol, up to 60 h after admission. During this time, background therapy aimed at relieving signs and symptoms is ongoing. Irrespective of when patients were administered their first dose, early in their hospitalization or up to 60 h after hospitalization, an additional but modest improvement in dyspnoea is seen.
This latter finding complements the dyspnoea results seen in VMAC and the VERITAS trials.4,5 Both studies demonstrated large improvements in dyspnoea with both arms of the study. However, as time progressed (within 24 h), no further benefit over placebo plus standard therapy was seen. McMurray et al.4 noted the difficulty of demonstrating a significant effect beyond that of placebo alone due to the large improvements seen by placebo plus standard therapy. Although this analysis suggests a persistent benefit from time after hospital admission, with a more pronounced effect when measured earlier after first dose, additional studies with more frequent measurements would be required to determine whether an ‘optimal’ therapeutic window for improvement of dyspnoea exists. These findings should be considered within the overall context of the EVEREST trials, where tolvaptan did not demonstrate long-term mortality benefit, in spite of a sustained reduction in body weight and modest improvement in signs and symptoms during the first few days of hospitalization when compared with standard therapy.3,14,18
Given the heterogeneous baseline characteristics of the patient population, and precipitating factors leading to hospitalization, tailoring therapy in AHFS is often necessary. Pre-specified subgroup analysis of the EVEREST database was performed to determine whether certain subgroups responded better to tolvaptan than others in terms of patient-assessed dyspnoea. In most subgroups, tolvaptan plus standard therapy demonstrated statistically significant dyspnoea improvement (or trends towards improvement) vs. placebo plus standard therapy. This may reflect the common feature of congestion across AHFS patients despite their overall heterogeneity and is supported by the correlation between body weight decrease and dyspnoea improvement.
Although dyspnoea is the most frequent presenting symptom in patients with AHFS, the assessment of changes in this symptom has not been well studied.4,17 Although the consistency of improvements in patient-assessed dyspnoea across multiple subgroups is internally consistent, the correlation of improvement with other assessments of heart failure-related symptoms and signs provides external validation or convergent validity. Patient-assessed dyspnoea modestly correlated with physician assessments of heart failure-related symptoms, such as dyspnoea and orthopnoea, as well as the more objective physician-assessed changes in signs of heart failure, such as JVD and peripheral oedema. In addition, physician-assessed NYHA class, a well-established prognostic factor that integrates signs and symptoms in patients with heart failure, moderately correlated with improvements in patient-assessed dyspnoea.19
Overall, the methods by which dyspnoea was assessed has implications for future clinical trial design. Despite preliminary reports that dyspnoea improves rapidly,20 patients still report dyspnoea up to 60 h after admission. This may represent a unique subset of patients or, possibly, that early enrolment in terms of symptom improvement may not be mandatory in this patient population. The severity of this dyspnoea is not known however, only that patients report some form of continued improvement. Thus, future trial design should consider measuring the absolute severity of dyspnoea in addition to change from baseline. Finally, since ongoing therapy for AHFS affects the absolute severity of dyspnoea, the variability of timing of measurement seen after admission suggests that dyspnoea measurement should be pre-specified and timed according to drug administration.
Conclusion
Post hoc analyses from EVEREST demonstrate novel perspectives on dyspnoea from a large clinical trial database, an important target to patients and as an endpoint in clinical trials. Previous trials have not reported in detail the evolution of dyspnoea in general, or specifically in relation to timing of intervention or timing since hospital admission. Post hoc analysis suggests that tolvaptan's effects on dyspnoea are greatest within 12 h after first dose. This first dose may have been given early or up to 60 h after hospitalization. Despite ongoing background standard therapy aimed at relieving signs and symptoms throughout this time period, an additive but modest dyspnoea improvement benefit is seen. Further, dyspnoea relief with tolvaptan parallels initial severity of dyspnoea at presentation, with greatest relief in those with the worst dyspnoea. This is not conclusive but raises a hypothesis that requires further study. Finally, the variability seen in terms of timing of assessments in relation to both first dose and hospitalization, in addition to the persistence of dyspnoea despite ongoing therapy, may influence how future clinical trials assess dyspnoea in AHFS.
Funding
The EVEREST trials were sponsored by Otsuka Pharmaceuticals.
Conflict of interest: P.S.P. is or has been a consultant to Astellas, Bayer, the Medicines Company, Nile Therapeutics, Otsuka, PDL BioPharma, Pericor Therapeutics, and Solvay Pharmaceuticals, has received honoraria from BiogenIdec, Corthera, EKR Therapeutics, and Palatin Technologies, and research support from Merck and PDL BioPharma. M.A.K. has received research grants and contracts, honoraria, and consults for Otsuka. H.B.K. is an employee of Otsuka. K.S. has received research grants and/or honoraria from AstraZeneca, Servier, Amgen, and Otsuka and a consultant for Cytokinetics, Servier, and Novartis. F.Z. is a consultant for Servier, Johnson & Johnson, research grants from Bayer, and honoraria from AstraZeneca, Pfizer, Boehringer Ingelheim, Abbott, Sanofi-Aventis, and Otsuka. J.E.A.B. is a consultant to DebioPharm. C.Z. is an employee of Otsuka. J.R.T. reported that he has received research grants from Abbott Laboratories, Actelion Pharmaceuticals, Bristol–Myers Squibb, CardioDynamics, CHF Solutions, Cytokinetics, GlaxoSmithKline, Merck, Myogen, NovaCardia, Sanofi-Aventis, Scios, Inc., the National Institutes of Health and the Department of Veterans Affairs. In the past 5 years, he has received honoraria from and/or has been/is a consultant for Abbott Laboratories, Actelion Pharmaceuticals, Bristol–Myers Squibb, CardioDynamics, CHF Solutions, Cytokinetics, Duke Clinical Research Institute, Medtronic, Merck, Momentum Research, Myogen, NovaCardia, Protein Design Labs, Scios, Inc., and Wyeth. A.P.M. reported receiving research grants from the National Institutes of Health, Italian Ministry of Health, AstraZeneca, Novartis, Pfizer, Takeda, SPA, SigmaTau, Sanofi-Aventis, and GiennePharma; being a consultant for Novartis and Daiichi Sankyo; and receiving honoraria from AstraZeneca, Novartis, Takeda, SPA, SigmaTau, Sanofi-Aventis, Servier, and Otsuka. J.C.B. has received research grants from the National Institutes of Health, Microbia, and Theravance; a consultant for Abbott, Bayer, Otsuka, Wyeth, and Astellas, and has received honoraria from Scios, Otsuka, and Orqis. L.G. reported research grants and/or honoraria from GlaxoSmithKline, Otsuka, Amgen, Cordis, and Bristol; a consultant for Cordis. J.O. is an employee of Otsuka. J.E.U. has received research support, honoraria, and is a consultant for Otsuka. M.G. is or has been a consultant and/or received honoraria from Astellas, Bayer, Corthera, DebioPharm, ErreKappa Terapeutici, EKR Therapeutics, GlaxoSmithKline, Medtronic, Merck, Nile Therapeutics, Novartis, Otsuka, Palatin Technologies, Pericor Therapeutics, PDL BioPharma, Scios Inc., Solvay Pharmaceuticals, and SigmaTau.
References
- 1.ADHERE Scientific Advisory Committee. Acute Decompensated Heart Failure National Registry (ADHERE®) Core Module Q1 2006 Final Cumulative National Benchmark Report: Scios, Inc.; July 2006 [Google Scholar]
- 2.Adams KF, Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, Berkowitz RL, Galvao M, Horton DP. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE) Am Heart J. 2005;149:209–216. doi: 10.1016/j.ahj.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Gheorghiade M, Konstam MA, Burnett JC, Jr, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C. Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST Clinical Status Trials. JAMA. 2007;297:1332–1343. doi: 10.1001/jama.297.12.1332. [DOI] [PubMed] [Google Scholar]
- 4.McMurray JJ, Teerlink JR, Cotter G, Bourge RC, Cleland JG, Jondeau G, Krum H, Metra M, O'Connor CM, Parker JD, Torre-Amione G, van Veldhuisen DJ, Lewsey J, Frey A, Rainisio M, Kobrin I. Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials. JAMA. 2007;298:2009–2019. doi: 10.1001/jama.298.17.2009. [DOI] [PubMed] [Google Scholar]
- 5.VMAC Investigators. Intravenous nesiritide vs nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA. 2002;287:1531–1540. doi: 10.1001/jama.287.12.1531. [DOI] [PubMed] [Google Scholar]
- 6.Teerlink JR, Massie B, Cleland J, Tzivoni D for the RITZ-1 Investigators. A double-blind, parallel-group, multi-center, placebo-controlled study to investigate the efficacy and safety of tezosentan in reducing symptoms in patients with acute decompensated heart failure (abstract) Circulation. 2001;104:II-526. [Google Scholar]
- 7.Coletta A, Cleland J. Clinical trials update: highlights of the scientific sessions of the XXIII Congress of the European Society of Cardiology—WARIS II, ESCAMI, PAFAC, RITZ-1 and TIME. Eur J Heart Fail. 2001;3:747–750. doi: 10.1016/s1388-9842(01)00210-0. [DOI] [PubMed] [Google Scholar]
- 8.Cuffe MS, Califf RM, Adams KF, Jr, Benza R, Bourge R, Colucci WS, Massie BM, O'Connor CM, Pina I, Quigg R, Silver MA, Gheorghiade M. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: a randomized controlled trial. JAMA. 2002;287:1541–1547. doi: 10.1001/jama.287.12.1541. [DOI] [PubMed] [Google Scholar]
- 9.Mebazaa A, Nieminen MS, Packer M, Cohen-Solal A, Kleber FX, Pocock SJ, Thakkar R, Padley RJ, Poder P, Kivikko M. Levosimendan vs dobutamine for patients with acute decompensated heart failure: the SURVIVE Randomized Trial. JAMA. 2007;297:1883–1891. doi: 10.1001/jama.297.17.1883. [DOI] [PubMed] [Google Scholar]
- 10.Packer M. REVIVE II: Multicenter placebo-controlled trial of levosimendan on clinical status in acutely decompensated heart failure (abstract) American Heart Association Scientific Sessions 2005 Late Breaking Clinical Trials II; 13–16 November 2005, Dallas, TX. 2005 [Google Scholar]
- 11.Committee for Proprietary Medicinal Products (CPMP) Note for Guidance on Clinical Investigation of Medicinal Products for the Treatment of Cardiac Failure, Addendum on Acute Cardiac Failure. London: EMEA, European Medicines Agency; 2004. [Google Scholar]
- 12.Teerlink JR. Dyspnea as an end point in clinical trials of therapies for acute decompensated heart failure. Am Heart J. 2003;145(Suppl. 2):S26–S33. doi: 10.1067/mhj.2003.151. [DOI] [PubMed] [Google Scholar]
- 13.US Food and Drug Administration. NDA 20-920 Natrecor (nesiritide) [Google Scholar]
- 14.Konstam MA, Gheorghiade M, Burnett JC, Jr, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C for the Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan I. Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST outcome trial. JAMA. 2007;297:1319–1331. doi: 10.1001/jama.297.12.1319. [DOI] [PubMed] [Google Scholar]
- 15.Gheorghiade M, Gattis WA, Barbagelata A, Adams KF, Jr, Elkayam U, Orlandi C, O'Connor CM. Rationale and study design for a multicenter, randomized, double-blind, placebo-controlled study of the effects of tolvaptan on the acute and chronic outcomes of patients hospitalized with worsening congestive heart failure. Am Heart J. 2003;145(Suppl. 2):S51–S54. doi: 10.1067/mhj.2003.154. [DOI] [PubMed] [Google Scholar]
- 16.Van Elteren P. On the combination of independent two-sample tests of Wilcoxin. Bull Int Stat Inst. 1960;37:351–361. [Google Scholar]
- 17.Pang PS, Cleland JG, Teerlink JR, Collins SP, Lindsell CJ, Sopko G, Peacock WF, Fonarow GC, Aldeen AZ, Kirk JD, Storrow AB, Tavares M, Mebazaa A, Roland E, Massie BM, Maisel AS, Komajda M, Filippatos G, Gheorghiade M. A proposal to standardize dyspnoea measurement in clinical trials of acute heart failure syndromes: the need for a uniform approach. Eur Heart J. 2008;29:816–824. doi: 10.1093/eurheartj/ehn048. [DOI] [PubMed] [Google Scholar]
- 18.Yancy CW. Climbing the mountain of acute decompensated heart failure: the EVEREST trials. JAMA. 2007;297:1374–1376. doi: 10.1001/jama.297.12.1374. [DOI] [PubMed] [Google Scholar]
- 19.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112:e154–e235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 20.Coletta AP, Cleland JG, Cullington D, Clark AL. Clinical trials update from Heart Rhythm 2008 and Heart Failure 2008: ATHENA, URGENT, INH study, HEART and CK-1827452. Eur J Heart Fail. 2008;10:917–920. doi: 10.1016/j.ejheart.2008.07.006. [DOI] [PubMed] [Google Scholar]