Abstract
PURPOSE
AP-1 has been proposed as a key intermediate linking exposure to light and photoreceptor cell death in rodent light damage models. Inhibition of AP-1 associated with steroid administration also prevents light damage. In this study the role of steroids in inhibiting AP-1 activation and/or in preventing photoreceptor degeneration was examined in the rhodopsin mutant dog model.
METHODS
The dogs were dark adapted overnight, eyes dilated with mydriatics; the right eye was light occluded and the fundus of the left eye photographed (∼15-17 overlapping frames) with a fundus camera. For biochemical studies, the dogs remained in the dark for 1 to 3 hours after exposure. Twenty-four hours before exposure to light, some dogs were treated with systemic dexamethasone or intravitreal/subconjunctival triamcinolone. AP-1 DNA-binding activity was determined by electrophoresis mobility shift assay (EMSA) and phosphorylation of c-Fos and activation of ERK1/2 were determined by immunoblot analyses. The eyes were collected 1 hour and 2 weeks after exposure to light, for histopathology and immunocytochemistry.
RESULTS
Inhibition of AP-1 activation, and phosphorylation of ERK1/2 and c-Fos were found after dexamethasone treatment in light-exposed T4R RHO mutant dog retinas. In contrast, increased AP-1 activity and phosphorylation of c-Fos and ERK1/2 were found in triamcinolone-treated mutant retinas. Similar extensive rod degeneration was found after exposure to light with or without treatment, and areas with surviving photoreceptor nuclei consisted primarily of cones. Only with systemic dexamethasone did the RPE cell layer remain.
CONCLUSIONS
Intraocular or systemic steroids fail to prevent light-induced photoreceptor degeneration in the T4R RHO dog retina. Finding that systemic dexamethasone prevents AP-1 activation, yet does not prevent retinal light damage, further supports the hypothesis that AP-1 is not the critical player in the cell-death signal that occurs in rods.
The differentiated photoreceptor is elegantly organized to have an external light-capturing outer segment optimized for efficient quantal absorption. Internally, the inner segment has the protein synthetic and energy-generating organelles, and on the vitreal aspect is the synaptic terminal that connects to the second-order neurons that ultimately transfer information to higher visual centers. Each rod photoreceptor can be 120 μm or longer, and such exquisite compartmentalization efficiently separates multiple specialized functions. Not surprisingly, the photoreceptors' complexity, together with the specific signal transduction and “housekeeping” functions performed, renders them susceptible to degenerative diseases, either genetic or acquired, that result from damage to genes or pathways critical for their function or viability. Of the 190 retinal disease loci mapped to date, the genes and mutations have been identified for ∼135 (RetNet available at http://www.sph.uth.tmc.edu/RetNet/ provided in the public domain by the University of Texas Health Science Center, Houston, TX). In many cases, different mutations in the same gene result in a broad range of differing phenotypes, thus emphasizing the broad genetic and allelic heterogeneity of these degenerative retinal disorders.
Of particular interest has been the interaction between light and the death of photoreceptors. After Noell et al.1,2 made the seminal finding that visible light may damage mammalian photoreceptors at intensities that are ordinarily encountered, many investigators in subsequent studies have examined this interaction, especially in normal albino rodents, and have begun to identify the pathways and molecular events that link exposure to light to photoreceptor degeneration.3,4 Two different pathways, the bright- and low-light pathways, mediate light-induced visual cell death, but only the bright-light pathway is accompanied by activation of the AP-1 transcription factor.5 This critical intermediary has been proposed to link damaging exposure to lights with photoreceptor apoptosis by activation of the c-Fos/AP-1 molecular pathway.5
Photoreceptor degeneration also results from exposure to light in retinas having mutations in the rhodopsin gene (RHO) that renders them especially sensitive to light. The naturally occurring T4R6 and transgenic T17M7 RHO mutations in dogs and mice, respectively, represent models for homologous diseases in humans with autosomal dominant retinitis pigmentosa (adRP).8,9 Although these mutations affect the first- and second-consensus glycosylation sequences,10 a possible indication of the enhanced light-damage susceptibility, other RHO mutations in humans also show marked delays in visual pigment regeneration with bleaching,11-13 a feature that raises concern as to the possible modulatory effect that exposure to light can have on the disease process.6,14 Although light-induced damage in both normal mice, and RHO mutant dogs or mice is mediated by RHO, the major difference between normal and mutant subjects is that, in the latter, photoreceptors degenerate with light intensities that cause no damage to normal retinas. Very short exposures to light, such as those used in routine clinical eye examinations of humans, result in severe outer retinal degeneration.14,15
Previous studies in albino rodents using genetic or pharmacologic approaches have demonstrated an association between AP-1 inhibition and prevention of photoreceptor degeneration.16-18 Although there are some questions as to the specificity of this inhibition and the role of AP-1 as a cell death or cell survival signal,19 it is clear that high-dose administration of corticosteroids before exposure to light is associated with no photoreceptor degeneration.18 In this study, we examined the effect of systemic or ocular corticosteroid administration on AP-1 induction and photoreceptor degeneration. We found that only systemic steroids inhibit AP-1 activation, but in neither case do steroids prevent or modulate photoreceptor damage. This supports prior findings that, at least in the T4R RHO mutant canine retina, AP-1 is not the critical player in the cell death signaling pathway that links exposure to light and photoreceptor degeneration.19
MATERIALS AND METHODS
Animals
Dogs were maintained at the Retinal Disease Studies (RDS) facility in Kennett Square (PA), and all procedures were in adherence to the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research. The dogs represent an outbred population with a common genetic background.20 The animal identification, genotype, ages studied, and procedures performed are detailed in Table 1. At the ages studied and under the ambient light conditions used in the kennels and procedure rooms (described later), the RHO mutants (T4R/+; T4R/ T4R) have no photoreceptor degeneration as long as ophthalmic examination procedures are not performed.6,14
Table 1.
Summary of the Experimental Dogs and Studies Performed
| Treatment |
Analysis and PE Interval |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Animal ID* | T4R Status | Age (wk) | Light Exposure | Systemic | Local | AP-1 | p-c-Fos | p-ERK1/2 | Morph/IHC |
| Controls | |||||||||
| N164 | +/+ | 41 | L | No Rx | No Rx | 3 h | 3 h | — | — |
| EM60 | −/− | 40 | L | No Rx | No Rx | 1 h | 1 h | 1 h | — |
| EM61 | −/+ | 26 | L | No Rx | No Rx | 1 h | 1 h | 1 h | — |
| EM66 | −/+ | 16 | L | No Rx | No Rx | 1 h | 1 h | 1 h | — |
| EM72 | −/− | 23 | L | No Rx | No Rx | 1 h | — | 1 h | — |
| EM141 | −/+ | 23 | L | No Rx | No Rx | — | — | 1 h-OCT | |
| EM142 | −/+ | 23 | No | No Rx | No Rx | — | — | 1 h-OCT | |
| EMB29* | −/+ | 14 | L | No Rx | No Rx | 1.5 h | — | 1.5 h | — |
| EMB30* | −/+ | 14 | L | No Rx | No Rx | 1.5 h | — | 1.5 h | — |
| EMB34* | −/+ | 14 | L | No Rx | No Rx | 1.5 h | — | 1.5 h | — |
| EM109 | −/+ | 19 | L | No Rx | No Rx | — | — | — | 2 w-PB |
| EMB37* | −/+ | 16 | L | No Rx | No Rx | 2 w-PB | |||
| EMB38* | −/+ | 16 | L | No Rx | No Rx | 2 w-PB | |||
| EM112 | −/+ | 19 | L | No Rx | No Rx | 2 w-OCT | |||
| Systemic DEX | |||||||||
| EM57 | −/+ | 40 | L | DEX | — | 1 h | 1 h | 1 h | — |
| EM59 | −/− | 40 | L | DEX | — | 1 h | 1 h | 1 h | — |
| EM67 | −/+ | 16 | L | DEX | — | 1 h | 1 h | 1 h | — |
| EM108 | −/+ | 19 | L | DEX | — | — | — | — | 2 w-OCT |
| EM110 | −/+ | 19 | L | DEX | — | — | — | — | 2 w-PB |
| EM227 | −/− | 19 | L | DEX | — | — | — | 1 h-OCT | |
| IVit and Sconj TRIAM to Exposed Eye | |||||||||
| EM65 | −/− | 23 | L | — | TRIAM-L | 1 h | — | 1 h | — |
| EM71 | −/+ | 23 | L | — | TRIAM-L | 1 h | — | 1 h | — |
| EM73 | −/− | 20 | L | — | TRIAM-L | 1 h | — | 1 h | — |
| EM74 | −/+ | 20 | L | — | TRIAM-L | 1 h | — | 1 h | — |
| EM226 | −/− | 19 | L | — | TRIAM-L | — | — | 1 h-OCT | |
| IVit and Sconj TRIAM to Shielded Eye | |||||||||
| EM68 | −/− | 23 | L | — | TRIAM-R | 1 h | — | 1 h | — |
| EM70 | −/− | 23 | L | — | TRIAM-R | 1 h | — | 1 h | — |
| EM75 | −/+ | 20 | L | — | TRIAM-R | 1 h | — | 1 h | — |
| EM77 | −/+ | 20 | L | — | TRIAM-R | 1 h | — | 1 h | — |
| IVit and Sconj TRIAM to Exposed and Shielded Eyes | |||||||||
| EMB18* | −/+ | 46 | L | — | TRIAM-B | 2 h | 2 h | — | — |
| EM101 | −/+ | 13 | R | — | TRIAM-B | 2 h | — | 2 h | — |
| EM102 | +/+ | 13 | L | — | TRIAM-B | 2 h | — | 2 h | — |
| EM98 | −/+ | 15 | L | — | TRIAM-B | — | — | — | 2 w-PB |
| EM104 | −/+ | 13 | L | — | TRIAM-B | — | — | — | 2 w-PB |
| EM103 | −/− | 13 | L | — | TRIAM-B | — | — | — | 2 w-PB |
| EM105 | −/− | 13 | L | — | TRIAM-B | — | — | — | 2 w-PB |
| EM99 | +/+ | 15 | L | — | TRIAM-B | — | — | — | 2 w-PB/L |
| EM100 | +/+ | 15 | L | — | TRIAM-B | — | — | — | 2 w-PB |
Control dogs highlighted in bold were included in a prior study that characterized retinal AP-1 and the signaling pathways that were activated after clinical exposure to light.19 PE, postexposure interval; L, left eye; R, right eye; B, both eyes; No Rx, no treatment; DEX, systemic (SC, IV) treatment with DEX beginning the day before light exposure; TRIAM, IVit and Sconj TRIAM administered the day before exposure to light; Morph/IHC, morphology/immunohistochemistry; PB, plastic embedding medium (PolyBed; Polysciences); OCT, optimal cutting temperature embedding medium.
All dogs were +/+ at the RPE65 locus unless an * is placed after their number, which indicates heterozygous status (RPE65−/+).
Treatment Protocols
Four different treatment protocols were performed to examine the effect of corticosteroids on AP-1 activation and/or prevention of photoreceptor degeneration after clinical light exposures; the steroids were administered either by systemic or direct ocular routes. All animals used and procedures performed are listed in Table 1. As controls, we used 1 normal and 13 untreated RHO mutants for biochemical (n = 8) and morphologic (n = 6) analyses; some of these dogs were included in a previous study which characterized AP-1 and other signaling pathways that were activated by exposure to light and are identified in the table.19
Study 1 consisted of six affected dogs used for biochemical (n = 3) and morphologic (n = 3) analyses. The dogs were placed in constant darkness on the day before clinical exposure to light, and received systemic dexamethasone (DEX) on the following schedule: Approximately 18 to 19 hours and again 4 to 5 hours before exposure to light, the dogs received subcutaneous (SC) DEX (dexamethasone 2 mg/mL; Phoenix Pharmaceuticals, St. Joseph, MO) at an ∼dose of 0.18 mg/kg. Two to 3 hours before exposure, a 10-fold higher dose of DEX (1.8 mg/kg) was administered intravenously (IV).
Studies 2, 3 and 4 involved the ocular administration of corticosteroids before exposure to light. Treatment was given to the light-exposed (n = 2), shielded (n = 3), or both the exposed and shielded eyes (n = 4; Table 1). If a treatment effect was observed, this paradigm was designed to determine whether it resulted from a direct or an indirect effect of the steroid in the light-exposed eye. On the day before the clinical light exposure, the dogs were dark adapted. Under dim red light illumination, the pupils were dilated with topical mydriatic solutions (1% atropine, 10% phenylephrine, 1% tropicamide). The dogs were sedated with a combination of intramuscular acetylpromazine/atropine and then anesthetized with IV ketamine. The treated eyes had 150 μL of aqueous fluid removed by anterior chamber paracentesis and then were injected with subconjunctival (Sconj) and intravitreal (IVit) triamcinolone acetonide (TRIAM; Kenalog-40; Bristol-Meyers Squibb, Princeton, NJ). Each treated eye received ∼6 to 10 mg Sconj and 6 mg IVit. At the ages studied, the vitreous volume of the treated dogs is ∼1.75 to 2.5 mL,21 and the IVit doses administered were in the range of 2.4 to 3.4 mg/mL of vitreous.
Exposure to Light and Tissue Collection
The animal housing and light-exposure conditions used in this study have been described in detail previously,19 and are briefly summarized. Dogs were maintained in kennel runs in a cyclic light environment (7 AM lights on/7 PM lights off) with light intensities that varied between 175 and 350 lux at the level of the “standard” dog eye. For the clinical light exposures, the dark-adapted dogs had the pupils dilated (1% tropicamide, 1% atropine, 10% phenylephrine) in both eyes, and one eye was completely shielded from light (shielded). Under dim red illumination, the other eye was exposed to a series of overlapping retinal photographs (exposed) obtained with a hand-held, manual advance fundus camera (model RC-2; Kowa Company Ltd., Nagoya, Japan) within 4 to 5 hours of light onset (7 AM). With one exception, the right eye was shielded, and the left eye was exposed (Table 1). Because the dog retina has regions where the pigment epithelium is (inferior, nontapetal region) and is not (superior, tapetal region) pigmented, different light intensities were used for viewing and photographing these two regions. These adjustments were made with neutral density or gray polarizing film filters and/or adjusting the settings of the photographic flash. For viewing, the approximate retinal illuminances produced by the tungsten bulb were 0.95 and 3.8 mW · cm−2 respectively, for the tapetal and nontapetal regions. For photography, microsecond duration flashes of a xenon lamp produced approximate retinal doses/flash of 0.6 and 11 mJ · cm−2, respectively, for the tapetal and nontapetal regions. Fifteen to 17 pictures were taken of the eye during an ∼5-minute period, and these were equally distributed between the tapetal and nontapetal zones.
Based on the light intensities used and activation of AP-1 by the exposure to light,19 we propose that the light exposure paradigm used causes photoreceptor degeneration via the bright-light pathway, although the genetic tools for testing independence from transducin signaling presently are not available for such studies in the dog model.3,5 The use of multiple microsecond-duration, bright-light flashes suggests damage by intermittent exposure to light, which has been shown to be more damaging to the retina.1 However, the short interflash interval used in our studies (∼17-20 seconds) differed from the 1-hour dark-adapted intervals used by Noell et al.1 in their study of intermittent exposure to light1; thus a direct translation of those studies is not possible.
After exposure to light, the dogs were returned to the dark and killed 1 to 3 hours later for biochemical studies. For immunohistochemistry and conventional morphology, samples were collected at 1 hour and 2 weeks, or at 2 weeks, respectively, after exposure. For the longer postexposure time point, the dogs were returned to the regular kennel environment and maintained under cyclic light conditions until they were killed 2 weeks after exposure.
For collections of retinas from exposed and shielded eyes, the dogs were anesthetized with intravenous pentobarbital sodium in a dark room with dim red illumination, the eyes were enucleated, and the dogs were euthanatized with a barbiturate overdose. The globes were opened with a razor-blade cut anterior to the ora serrata, the posterior segment isolated, and the vitreous removed. The retina was then manually separated from the pigment epithelium and frozen at −80°C until use. For immunohistochemistry, the eyes were processed by using standard techniques previously described.22
Preparation of Nuclear Protein Extracts
Nuclear protein extracts were prepared as described elsewhere.19,23 Briefly, single retina tissue samples were homogenized in homogenization buffer (0.25 M sucrose, 15 mM Tris-HCl [pH 8.0], 60 mM KCl, 15 mM NaCl, 5 mM EDTA [pH 8.0], 1 mM EGTA [pH 8.0], 0.15 mM spermine, 0.15 mM spermidine, 1 mM DTT, 0.5 mM PMSF, 5 μg/mL aprotinin, 2 μg/mL leupeptin, and 2 μg/mL pepstatin), and after low-speed centrifugation, the supernatant was saved as the postnuclear fraction. The pellet (crude nuclear fraction) was washed and extracted with the extraction solution (20 mM HEPES [pH 7.3], 400 mM NaCl, 1 mM EDTA [pH 8.0], 1 mM EGTA [pH 8.0], 1 mM DTT, 0.5 mM PMSF, 5 μg/mL aprotinin, 2 μg/mL leupeptin, and 2 μg/mL pepstatin), and the supernatant was collected by centrifugation and saved as the nuclear protein extract. All postnuclear supernatant and nuclear extracts were stored at −80°C until used; protein concentrations were determined with a DC protein assay kit (Bio-Rad Laboratories, Hercules, CA) and normalized by silver staining of the gels that were analyzed with a scanner and workstation (Storm 860 scanner; Amersham Biosciences, Pittsburgh, PA, and ImageQuant workstation; Molecular Devices, Sunnyvale, CA) to determine protein concentration.
Probe Labeling
The probe for the electrophoresis mobility shift assay (EMSA) was a 21-bp double-stranded AP-1 consensus oligonucleotide (5′-CGC TTG ATG AGT CAG CCG GAA-3′, 1.75 pM; Promega, Madison, WI) labeled with γ-[32P]ATP (10 mCi/mL, 3000 Ci/mmol; Amersham Biosciences) according to the phosphorylation reaction protocol in the gel shift assay system manual (Promega). Unincorporated γ-[32P]ATP was removed by a spin column (Sephadex G-25; Roche Diagnostics, Indianapolis, IN), and radioactivity was determined with a scintillation counter (model LS6500; Beckman Coulter, Fullerton, CA).
Electrophoresis Mobility Shift Assay
EMSA was performed according to the manufacturer's instructions (Promega), as described previously.19 All binding reactions between nuclear proteins (∼1.5 μg of protein/reaction) and labeled probe (0.07 picomoles, ∼10,000 cpm/reaction), including the positive control HeLa nuclear extract (>2.4 mg/mL; Promega), were examined by nondenaturing, gradient polyacrylamide gels (2%-20%). Gels were dried and exposed to either of two phosphorescence imagers (model BAS-IP 2040; Fujifilm Life Science, Stamford, CT, or PhosphorImager, Amersham Biosciences) and/or x-ray films (Fujifilm Life Science). The images were scanned and analyzed by a scanner with commercial software (BAS 1000, Image Gauge software; Fujifilm Life Science), or the scanner and workstation described in the Probe Labeling section. The relative AP-1 activity was determined based on the intensity of shifted bands measured on a workstation normalized for equal protein loading by silver staining of the gels (Image Gauge software, Fujifilm Life Science; or ImageQuant; Molecular Devices). Binding specificity was confirmed by blocking reactions using unlabeled specific AP-1. The intensity measurements obtained with the phosphorescence imager or x-ray films were comparable and also with the radiation dose displayed in terms of units of photostimulated luminescence (PSL).
Immunoblot Assay
All immunoblot procedures were performed as previously described.19 One-dimensional protein electrophoresis and immunoblot analysis was performed with nitrocellulose membranes (Trans-Blot Transfer Medium, Bio-Rad Laboratories). The primary antibodies used are listed in Table 2; HRP rabbit anti-mouse IgG and HRP goat anti-rabbit IgG (ZyMax, San Francisco, CA) were used as the secondary antibodies. The immunoreacted bands were detected by the enhanced chemiluminescence (ECL) system (Amersham Biosciences), scanned, measured, and analyzed (ImageQuant; Molecular Devices).
Table 2.
Antibodies
| Antigen | Host | Source* | IB | IHC |
|---|---|---|---|---|
| c-Fos (4) | Rabbit pc | Santa Cruz Biotech, Santa Cruz, CA; sc-52 (0.2 μg/μL) | 1:500 | |
| P-c-Fos (Ser374) | Mouse mc | Assay Designs; 905–640 | 1:10 | |
| P-ERK (E-4) | Mouse mc | Santa Cruz Biotech; sc-7383 (0.2 μg/μL) | 1:1,000 | |
| P-ERK1/2 | Mouse mc | Cell Signaling, Beverly, MA; 9106 | 1:30 | |
| β/3-Actin | Mouse mc | Chemicon, Temecula, CA; MAB1501 | 1:1,000 | |
| Tubulin | Mouse mc | Santa Cruz Biotech; sc-23950 (0.2 μg/μL) | 1:5,000 | |
| CRALBP | Rabbit pc | Jack Saari (University of Washington, Seattle, WA) | 1:1,500 | |
| GFAP | Rabbit pc | DakoCytomation, Carpinteria, CA; Z0334 | 1:1,000 | |
| RPE65 | Mouse mc | Novus Biologicals; NB-100-355 | 1:500 | |
| Rod opsin | Mouse mc | Chemicon; MAB5316 | 1:1,000 | |
| Human cone arrestin | Rabbit pc | Cheryl Craft, LUMIF (University of Southern California, Los Angeles, CA) | 1:10,000 | |
| AF488 2ary anti-mouse | Goat | Invitrogen, Carlsbad, CA; A-11029 | 1:200 | |
| AF568 2ary anti-rabbit | Goat | Invitrogen; A-11036 | 1:200 |
P, phosphorylated; pc, polyclonal; mc, monoclonal; IB, immunoblot analysis; IHC, immunohistochemistry; 2ary, secondary.
Catalog numbers for commercially available antibodies are listed as a reference to their specificity.
Immunohistochemistry
A slit was made through the enucleated globe at the level of the ora serrata, and the entire globe was fixed for 1 hour in 4% paraformaldehyde in 0.1 M phosphate-buffered saline at 4°C. The posterior segment then was isolated, the vitreous gently removed, and the eye cup fixed for an additional 2 hours at 4°C in 2% paraformaldehyde in 0.1 M phosphate-buffered saline. The eye cup was then transferred to 2% paraformaldehyde in 0.1 M phosphate-buffered saline for 24 hours. The tissue was trimmed, cryoprotected sequentially for 24 hours in a solution of 15% and 30% sucrose in 0.1 M sodium phosphate and 0.15 M sodium chloride, pH 7.2 (BupH phosphate-buffered saline; Pierce, Rockford, IL), at 4°C, and embedded in optimal cutting temperature (OCT) medium. Retinal cryosections along the superior and inferior retinal meridians of both the light-exposed and shielded eyes from RHO mutant dogs were cut at 7-μm thickness and used to examine the cellular localization of the AP-1 complex component phosphorylated c-Fos, and phosphorylated ERK1/2 (Table 2) using standard immunofluorescence protocols.24 Double-immunofluorescence with CRALBP was performed to determine colocalization in Müller cells. Labeling with GFAP and RPE65 determined the reactivity of Müller cells, and the integrity of the RPE in exposed mutant retinas. Double-labeling with human cone arrestin and rod opsin identified the remaining photoreceptor cells in the areas of retinal atrophy.
Conventional Retinal Morphology
Immediately after enucleation, the posterior segments were isolated and fixed in a triple-fixative protocol (3% glutaraldehyde-2% formalde-hyde 2% glutaraldehyde-1% osmium tetroxide, and 2% osmium tetroxide), as previously reported.25 The posterior segments were trimmed into segments that extended from the optic nerve to the ora serrata along the superior and inferior meridians, dehydrated, and embedded in epoxy resin (PolyBed 812; Polysciences, Warrington, PA). Full-length 1-μm sections were cut with glass knives, stained with azure II-methylene blue, with or without a paraphenylenediamine counter stain. The sections were examined in contiguous fields from the optic disc to the ora serrata, and representative images from the same retinal location photographed (Spot 4.0 camera; Diagnostic Instruments, Inc., Sterling Heights, MI).
RESULTS
Effect of Systemic DEX on AP-1 DNA Binding Activity in Exposed RHOMutant Retina
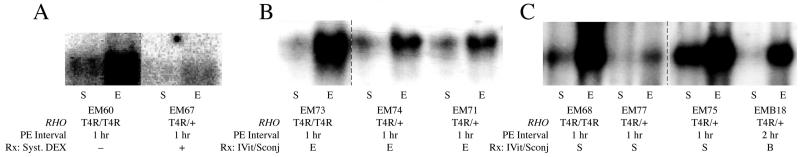
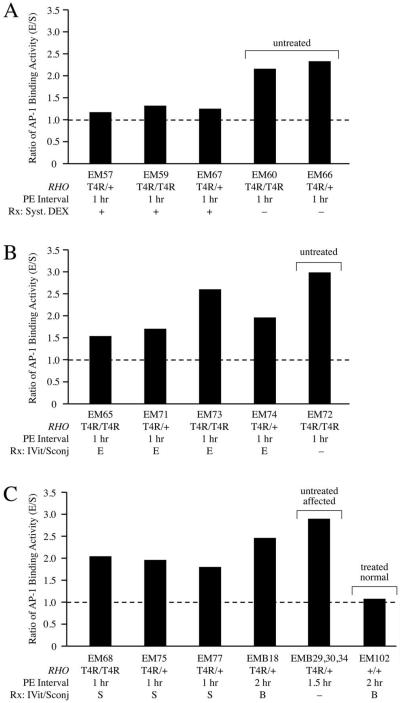
We have described that clinical light exposure of the T4R RHO mutant retina results in an ∼2.5- to 3.5-fold increase in AP-1 DNA-binding activity. Increased binding occurred within 1 hour of exposure, remained elevated for 6 hours, and decreased to normal (pre-exposure or shielded levels) by 24 hours. Activation of AP-1 by light was specific to the RHO mutant retina and did not occur either in normal controls or animals with prcd, a nonallelic retinal disease.19,20 After systemic DEX, there was a marked inhibition of AP-1 activation after exposure to light of the RHO mutant retina (Figs. 1A, 2A). In comparison to untreated animals that showed increases in retinal AP-1 binding of ∼2.6-fold (Figs. 1A-C), the levels increased 1.2- to 1.3-fold with DEX treatment (Fig. 2A).
FIGURE 1.
EMSA of AP-1 DNA-binding activity in retinal nuclear proteins from T4R RHO mutant dogs 1 hour after light exposure. The dogs were untreated or treated with systemic DEX (A) or were treated locally with TRIAM in the exposed (E) eye (B), the shielded (S) eye, or both (B) eyes (C). The exposed retina of the untreated dog (EM60) showed a marked increase in AP-1 binding, but it was suppressed by DEX treatment (EM67). Retinas receiving TRIAM in the E, S, or B eyes showed increased AP-1 binding in the exposed eye. The description below the gels represent the genotype at the RHO locus, the postexposure (PE) interval, and the treatment. The dashed lines in the gels indicate that the images represent lanes from the same gel that were not adjoining.
FIGURE 2.
The AP-1 binding activity ratio (E/S, exposed/shielded) in retinas after exposure to light. (A) Without treatment, AP-1 levels increased significantly 1 hour after light exposure, but DEX pretreatment inhibited AP-1 activation. (B) Pretreatment with TRIAM in the exposed (E), or (C) shielded (S) or both (B) eyes resulted in minimal to no AP-1 inhibition. (C) The exposed, normal retina (EM102) did not show any increase in AP-1-binding activity. Note that the AP-1 binding ratio for untreated affected dogs in (C) (EMB29, -30, -34) represents the average of the three ratios. The description below the histograms represent the genotype at the RHO locus, the postexposure (PE) interval, and the treatment.
Effect of Ocular TRIAM on AP-1 DNA Binding Activity in Exposed RHO Mutant Retina
In contrast, we found minimal inhibition of AP-1 activation in mutant retinas that were treated by direct ocular injection of TRIAM. Exposure to light after treatment of the exposed eye showed distinct AP-1 activation (Fig. 1B), with increases ranging from 1.5- to 2.6-fold (Fig. 2B). Similar increases were observed whether the TRIAM was administered to the shielded eye or to both exposed and shielded eyes (Figs. 1C, 2C). Treatment with ocular TRIAM of a normal control dog in both eyes showed the expected lack of AP-1 activation by clinical light exposure (Fig. 2C).
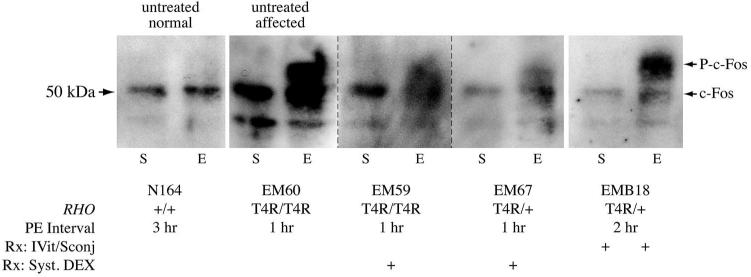
Effect of Ocular TRIAM or Systemic DEX on Phosphorylation of c-Fos
A distinct 50-kDa c-Fos band was found by immunoblot analysis in the untreated, shielded mutant retina that was the same as in the light-exposed or shielded normal retina (N164). A second immunoreactive band of ∼56 kDa, indicative of phosphorylated c-Fos,19 was observed in the exposed mutant retina (Fig. 3, EM60, compare lanes from shielded and exposed retinas). The same is observed in the exposed TRIAM treated, but not the shielded retina (Fig. 3, EMB18). In contrast, exposed retinas of DEX-treated dogs showed a smear at the p-c-Fos position (Fig. 3; EM59, EM67). This result suggests that systemic DEX partially inhibits c-Fos phosphorylation at some residues. In all cases, a lower molecular mass band, ∼ 45 kDa, of variable intensity was present in all samples and was assumed to represent nonspecific binding of the antibody or a lower molecular mass isoform of c-Fos.
FIGURE 3.
c-Fos immunoreactive pattern in nuclear proteins of light-exposed (E) or shielded (S) retinas. The normal retina (N164) showed a distinct c-Fos band of ∼50 kDa, and there were no differences between E and S eyes. The untreated, affected mutant retina (EM60) also showed a pattern similar to normal in S eye, but exposure to light (E) resulted in the appearance of a higher molecular mass band at ∼56 kDa, which represents phosphorylated c-Fos.19 Direct ocular treatment with TRIAM did not prevent c-Fos phosphorylation (EMB18). Exposure to light after systemic DEX resulted in a smear in the p-c-Fos position, an indication of slight and partial c-Fos phosphorylation (EM59, EM67). The description below the gels represents the genotype at the RHO locus, the postexposure (PE) interval, and the treatment. The dashed lines in the gels indicate that the images represent lanes from the same gel that were not adjoining.
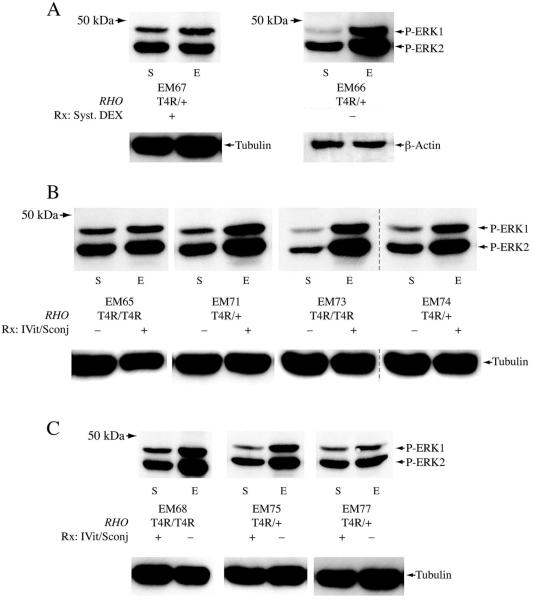
Steroids, Exposure to Light, and ERK1/2 Phosphorylation
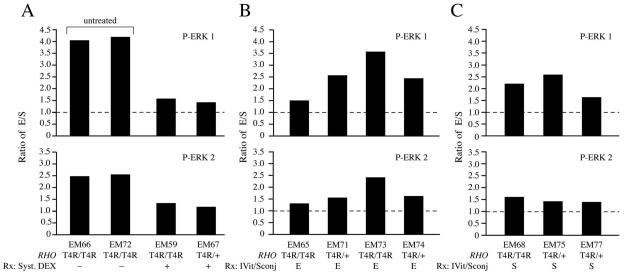
We previously demonstrated that extracellular regulated kinase (ERK), an upstream activator of AP-1,26 is phosphorylated in the RHO mutant retina after exposure to light, and the activation time course is similar to that of AP-1.19 In the present study, we examined the effect of systemic or ocular steroids on ERK1/2 phosphorylation after exposure to light. In the untreated, exposed mutant retina, ERK1/2 phosphorylation occurred by 1 hour after exposure to light, and levels were ∼4 (p-ERK1)- and ∼2.5 (p-ERK2)-fold higher than in the contralateral shielded retina (Figs. 4A, 5A). Systemic DEX markedly inhibited ERK1 (1.4- to 1.6-fold) and -2 (1.2- to 1.4-fold) phosphorylation (Figs. 4A, 5A). Direct application of ocular TRIAM to the exposed eye resulted in a variable ERK1/2 phosphorylation response (Figs. 4B, 5B). One retina showed minimal ERK phosphorylation (EM65), but the rest showed ERK1 phosphorylation levels that ranged from 2.5- to 3.6-fold higher than the untreated shielded eye (Fig. 5B). Similar results were observed in the exposed retinas when the direct ocular TRIAM treatment was applied to the shielded eye (Figs. 4C, 5C). With direct ocular steroid treatment, either to the exposed or to the shielded eye, the effect on ERK phosphorylation, although variable, appeared to be more pronounced on ERK2 than on ERK1.
FIGURE 4.
Phosphorylated ERK1/2 in retinal postnuclear Rernatant fractions from T4R RHO mutant dogs 1 hour after exposure to light. (A) Comparable levels of phosphorylated ERK1/2 were detected by immuno-blot analysis in both light-exposed (E) and shielded (S) retinas of a dog treated with systemic DEX (EM67), but a significantly increased level of p-ERK1/2 was found in the exposed retina of untreated mutant (EM66). (B, C) Increased p-ERK1/2 levels in the E retinas were found in animals in which the TRIAM was administered to the exposed (B) or shielded (C) eyes. There was some degree of variability in the level of p-ERK1/2 phosphorylation in the exposed retinas of TRIAM-treated eyes, but all showed increased p-ERK1/2 levels with exposure to light. Tubulin or β-actin immunoblots were used as a loading control for normalization. The lines below the p-ERK1/2 gels represent the genotype at the RHO locus, and the treatment. The dashed lines in the gels indicate that the images represent lanes from the same gel that were not adjoining.
FIGURE 5.
Ratios of phosphorylated ERK1/2 (E/S, exposed/shielded) in T4R RHO mutant retinas 1 hour after light exposure. (A) Untreated, exposed mutant retinas showed a marked increase in p-ERK1/2, but it was inhibited by systemic DEX. The exposed retinas showed light-dependent increases in p-ERK1 and p-ERK2 after treatment with TRIAM, which was administered to the exposed (B) or shielded (C) eyes. In general, p-ERK1/2 levels were variable between animals, and increases were more marked in p-ERK1 than for p-ERK2. The lines below the histograms represent the genotype at the RHO locus, and the treatment.
Effect of Ocular or Systemic Steroids on Retinal Degeneration after Exposure to Light
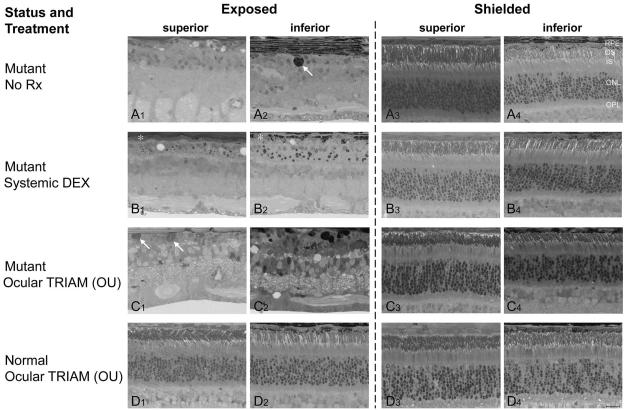
Two weeks after clinical light exposure, the untreated, exposed RHO mutant retina showed advanced outer retinal degeneration, and the findings were similar for both the central tapetal (Rerior) and nontapetal (inferior) regions—areas where the RPE, respectively, is not or is pigmented. There was a nearly complete loss of all photoreceptors and their nuclei. As the RPE layer had degenerated and disappeared as an anatomically distinct cell layer, the external limiting membrane now rested on a markedly attenuated choriocapillaris. Although these abnormalities were quite uniform in the exposed regions, it is important to note than some localized regions retained one to two incomplete rows of outer nuclear layer (ONL) nuclei and degenerating photoreceptor inner segments. In addition, the nontapetal layer showed hypertrophied and detached RPE cells that had migrated intraretinally (Figs. 6A1, 6A2). The shielded retina, on the other hand, was morphologically normal (Figs. 6A3, 6A4).
FIGURE 6.
Photomicrographs of plastic-embedded retinal sections from eyes collected 2 weeks after clinical exposure to light. Images were taken approximately 1250 μm from the optic disc along both the superior (A1, A3; B1, B3; C1, C3; D1, D3) and inferior (A2, A4; B2, B4; C2, C4; D2, D4) meridians from the exposed (A1, A2; B1, B2; C1, C2; D1, D2) and shielded (A3, A4; B3, B4; C3, C4; D3, D4) eyes. (A) The untreated mutant (EM109) showed extensive outer retinal degeneration and loss of RPE in the exposed retina, but the shielded retina was normal; (A2, arrow) intraretinal pigmented cell. (B) Systemic DEX (EM110) the photoreceptors and outer retinal layers degenerated in the exposed eye, but the shielded retina was normal. An incomplete, and structurally compromised RPE layer remained (B1, B2, *), and the ONL consisted of one to two incomplete rows of nuclei. (C) Sconj and IVit TRIAM administered to both eyes (OU) of a mutant dog (EM103) before exposure to light did not prevent RPE, photoreceptor, and outer retinal degeneration. Note presence of hypertrophied cells external to the inner nuclear layer (INL) with cytoplasmic inclusions that have cytologic characteristics of macrophages (C1, arrows). The TRIAM-treated shielded, mutant retina remained normal (C3, C4). (D) Intravitreal TRIAM administered to both eyes (OU) of a normal dog (EM100) before exposure to light caused no adverse effects in the exposed or shielded retinas. OS, outer segment layer; IS, inner segment layer; OPL, outer plexiform layer. Scale bar, 20 μm.
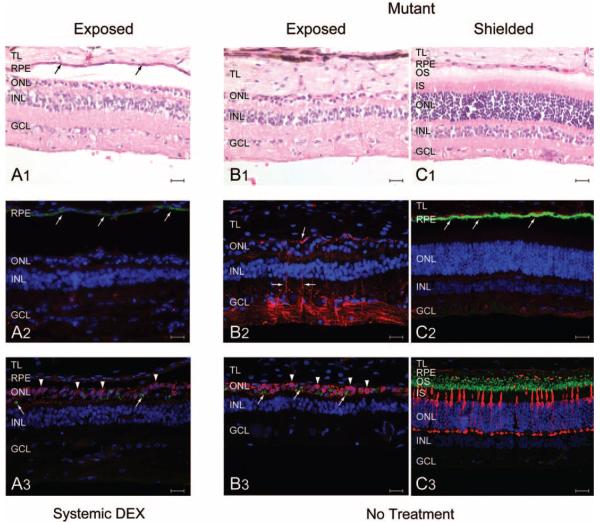
Treatment with systemic DEX before light exposure did not prevent outer retinal degeneration in the exposed eyes. The pathologic abnormalities were similar to that observed in untreated mutant retinas, although more areas in the treated eye retained one to two incomplete rows of ONL nuclei and degenerating photoreceptor inner segments (Figs. 6B1, 6B2). Moreover, in both the DEX-treated and untreated mutant retinas, cone nuclei comprised most of the surviving photoreceptor nuclei in the ONL (Figs. 7A3-C3). Systemic DEX did not cause any adverse retinal effects, and the shielded mutant retina remained normal (Figs. 6B3,6B4). However, the exposed retina of the DEX-treated animals had two salient differences from untreated, exposed retinas (Figs. 6B1, 6B2, 7). First, there was preservation of an RPE monolayer that, although structurally compromised and slightly attenuated, still expressed low levels of RPE65 protein (compare Figs. 7A1, 7A2 with 7C1, 7C2). Second, there was Rpression of activation of Müller cells, and glial processes did not extend into the subretinal space. (Figs. 7A2-C2).
FIGURE 7.
Morphologic and immunohistochemical characterization of the retina from light-exposed (EM108, OS; EM112, OS) and shielded (EM112, OD) T4R RHO mutant dogs; dog EM108 was treated with systemic DEX, and dog EM112 was not treated. All sections from an individual eye were from a series of serial sections taken from the same region. (A1) Marked thinning of the ONL, and loss of photoreceptor inner and outer segments in the DEX-treated, light-exposed mutant retina. Note the preservation of the RPE (arrows). (B1) Similar loss of photoreceptors in the untreated, light-exposed retina. Note, however, the absence of the RPE. (C1) Normal retinal structure and lamination in the shielded eye. (A2) Weak RPE65 labeling (arrows; green) and absence of GFAP labeling (red) in the DEX-treated light-exposed mutant retina. (B2) Strong GFAP labeling in the untreated, light-exposed retina; the absence of RPE65 labeling resulted from RPE loss. (C2) The shielded mutant retina was normal, and RPE labeling was intense and distinct. (A3) The majority of the remaining cell somata in the ONL of the DEX-treated, light-exposed mutant retina were human cone arrestin (hCAR) positive (arrowheads; red); punctate labeling of some cells with the rod opsin antibody is also present (arrows; green). (B3) Similar findings in the untreated, light-exposed retina. (C3) Normal pattern of rod opsin (green) and hCAR (red) labeling in the shielded mutant retina. TL, tapetum lucidum; OS, outer segments; IS, inner segments; INL, inner nuclear layer; GCL, ganglion cell layer. Scale bar, 20 μm.
Direct ocular administration of TRIAM also did not modify the light-induced retinal degeneration that was observed in mutant retinas 2 weeks after exposure to light. In contrast to systemic DEX, there was no preservation of RPE cells (Figs. 6C1, 6C2). In some areas, cells with the cytologic characteristics of macrophages were located adjacent to Bruch's membrane or intraretinally, and contained multiple cytoplasmic inclusions characteristic of undegraded susbtrate in lysosomes (Fig. 6C1; data not shown). Significantly, direct ocular administration of TRIAM did not have an adverse effect in the shielded mutant retina (Figs. 6C3, 6C4), or the normal retina, whether shielded or exposed (Figs. 6D1-D4).
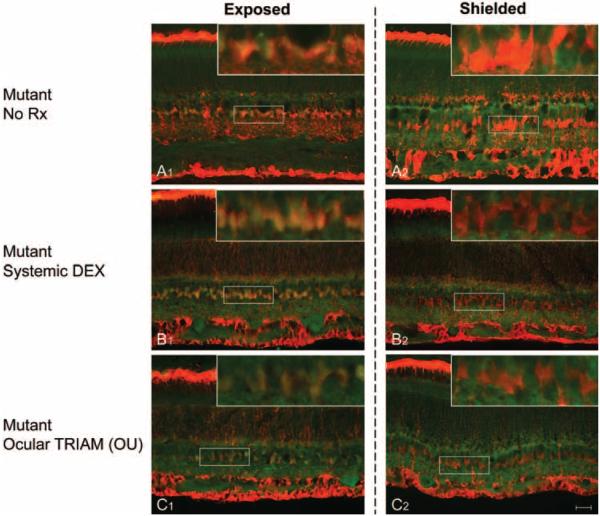
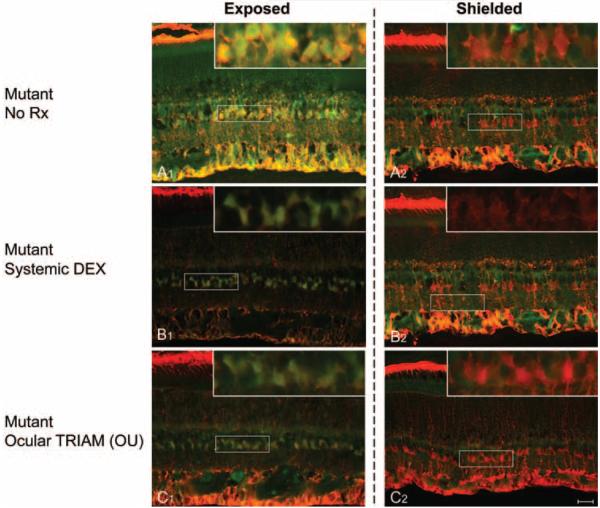
Light-Induced c-Fos and ERK1/2 Phosphorylation in Müller Cells Despite Steroid Treatment
One hour after exposure to light, c-Fos and ERK1/2 phosphorylation was observed in the somata of Müller cells (Figs. 8A1, 8A2; 9A1, 9A2), as previously reported19. Steroid treatment (systemic DEX, or ocular TRIAM) did not prevent phosphorylation of c-Fos (Figs. 8B1, 8C1) in Müller cells after exposure to light. Since the antibody we used is directed against c-Fos phosphorylated on Ser374, our results suggest that steroids do not prevent phosphorylation at this residue.
FIGURE 8.
Double fluorescence immunohistochemistry with p-c-Fos (green) and CRALBP (red) antibodies in T4R RHO mutant retinas 1 hour after exposure to light. Images were taken from the midperipheral region of the superior retinal meridian in light-exposed (A1, B1, C1) and shielded (A2, B2, C2) eyes of untreated animals (No Rx), or after steroid administration (systemic DEX or ocular TRIAM). Colocalization of p-cFos and CRALBP was seen in the Müller cell somata of the light-exposed retinas (A1: EM141 OS; B1: EM227 OS; and C1: EM226 OS) but not in the shielded eyes (A2: EM142 OD; B2: EM227 OD; and C2: EM226 OD). Scale bar: 20 μm.
FIGURE 9.
Double fluorescence immunohistochemistry with p-ERK1/2 (green) and CRALBP (red) antibodies in T4R RHO mutant retinas 1 hour after exposure to light. Images were taken from the midperipheral region of the superior retinal meridian in light-exposed (A1, B1, C1) and shielded eyes (A2, B2, C2) of untreated animals (No Rx) or after steroid administration (systemic DEX or ocular TRIAM). Colocalization of p-ERK1/2 and CRALBP was seen in the Müller cell somata of the light-exposed retinas (A1: EM141 OS; B1: EM227 OS; and C1: EM226 OS) but not in the shielded eyes (A2: EM142 OD; B2: EM227 OD; and C2: EM226 OD). p-ERK1/2 labeling was reduced in the exposed retinas treated with either systemic DEX (B1: EM227 OS), or ocular TRIAM (C1: EM226 OS) in comparison with that observed in the untreated exposed retina (A1: EM141 OS). Scale bar, 20 μm.
Phosphorylation of ERK1/2, on the other hand, was significantly reduced after steroid treatment and was predominantly restricted to the somata of Müller cells. No such colocalization of p-c-Fos and p-ERK1/2 with CRALBP was seen in shielded eyes (Figs. 8B2, 8C2; 9B2, 9C2). These findings support the immunoblot results and show that both steroids treatment (DEX and TRIAM) decrease the levels of pERK1/2 staining in Müller cells of the light-exposed eyes (Figs. 9B1, 9C1) in comparison to what is observed in the untreated retinas (Fig. 9A1). Although those levels are decreased, weak labeling persists, suggesting that steroids do not fully inhibit the light-induced ERK1/2 phosphorylation (compare Figs. 9B1, 9B2 with 9C1 9C2).
DISCUSSION
A critical intermediary identified in experimental retinal light damage is activation of the AP-1 transcription factor. It has been proposed that light induces photoreceptor apoptosis in wild-type mice by activation of the c-Fos/AP-1 molecular pathway.5 As a transcription factor, AP-1 has varied functions in many biological processes, among which are cell transformation, proliferation, differentiation, apoptosis, and survival.27-29 Such functions, which often appear to have opposite effects, most likely depend on the tissue, the stimulus, and the signaling pathway(s) involved.
In the T4R RHO mutant dog retina, we have found three early biochemical events associated with clinical exposure to lights that subsequently are associated with photoreceptor degeneration. Activation of ERK1/2, c-Fos phosphorylation and induction of AP-1 DNA binding activity occur within 1 hour of exposure to light, and all have a similar magnitude and time course.19 Phosphorylation of ERK1/2 in the mutant retina appears limited to the dog, as normal albino mice do not show retinal ERK1/2 activation with damaging exposure to lights.30 The downstream targets of this putative signaling pathway have not been identified yet, although our studies show that the biochemical events occur in Müller cells and not photoreceptors, a possible indication that the signaling pathway is a cell survival rather than cell death response.19
Inhibition of AP-1 by genetic manipulation (c-Fos knockout16) or activation of the glucocorticoid receptor by food deprivation or exogenous DEX18 is associated with prevention of light-induced retinal degeneration in wild-type mice. This is a compelling therapeutic target for translational studies in this mutant dog model, particularly because steroids are approved for human use by various routes of administration, and the potential for light damage is of concern for some human retinal degenerative disorders besides those caused by RHO mutations.14,31 We reasoned that if the protective effect of steroids on retinal light damage could be replicated in the canine model, then alternate delivery systems that lessen systemic and/or intraocular exposure and side effects, e.g., iontophoresis, could be tested experimentally before therapeutic use in humans. To date, only infrared imaging can be used for clinical examinations14 or surgical intervention32 in the highly light-sensitive RHO mutant canine retina.
To this end, we performed a series of studies examining the effect of systemic DEX or direct ocular administration of TRIAM on both the known components of the AP-1 signaling pathway in the mutant canine retina, and on the prevention of photoreceptor degeneration. The dose of DEX was more than 10-fold higher than that used in dogs in emergency situations to provide an acute anti-inflammatory effect (0.05- 0.1 mg/kg IV; Wadell L, School of Veterinary Medicine, University of Pennsylvania, Philadelphia, PA, written communication, June 2008). Similarly, the doses of TRIAM are comparable to or higher than those used clinically to suppress severe extraocular or intraocular inflammation. In humans, 2- to 4-mg doses of IVit TRIAM are used in the treatment of refractory, clinically significant diabetic macular edema,33 and 4 mg for most other intraocular diseases,34 although higher doses may be used.35 In dogs, IVit injections of 8 mg TRIAM in a 0.2-mL volume without anterior chamber paracentesis caused immediate, but transient elevations of intraocular pressure (IOP); thereafter, the IOP returned to baseline and remained normal.36 Thus, the single IVit TRIAM injection at the doses used in this study achieve immediate therapeutic levels that, based on clinical experience with dogs with intraocular inflammation, lasts 5 to 6 weeks and has no adverse effect.
We found that IV DEX, in contrast to IVit TRIAM, caused a profound inhibition of AP-1 activation. Although AP-1 DNA-binding activity with DEX was much lower than that in untreated light-exposed retinas, the DNA binding activity in TRIAM-treated eyes in most dogs was minimally inhibited. Because of the potential that an effect from IVit TRIAM could arise indirectly from systemic circulation rather than locally, we performed injections in the exposed eye, the shielded eye, or both eyes. In all cases, the results were comparable. Lack of systemic effect from TRIAM absorption is not unexpected given that in most patients there are no detectable levels of TRIAM in serum after IVit administration of 20 to 25 mg.37
In parallel with increased AP-1 DNA binding activity, there was a distinct c-Fos phosphorylation pattern in untreated mutant retinas exposed to light,19 and in exposed eyes treated with IVit TRIAM. The latter result was interpreted as no effect on c-Fos phosphorylation by locally administered steroids. In contrast, the exposed mutant retinas of dogs receiving IV DEX showed light labeling and a smear at the p-c-Fos position suggesting partial c-Fos phosphorylation. As there are multiple serine/threonine phosphorylation sites in the c-Fos protein structure,38,39 complete phosphorylation of c-Fos should form a clear phosphorylated c-Fos band in immunoblot images. However, if the phosphorylation process is interrupted, just some of these sites are phosphorylated. Such partially phosphorylated c-Fos proteins would form a smear in electrophoresis as seen in the mutant retinas from animals treated with IV DEX.
Similarly, administration of steroids by the systemic or ocular routes produced different outcomes in terms of ERK1 and -2 phosphorylation. In the untreated mutant retinas, ERK1/2 phosphorylation occurred by 1 hour after exposure to light, and the levels were approximately three- to fourfold higher than in the shielded retinas.19 Systemic DEX caused a marked inhibition of ERK1/2 phosphorylation, and this was much more pronounced than the more modest and slightly variable inhibition caused by locally administered TRIAM. With TRIAM, the results were the same whether the exposed or the shielded eyes were treated. If one assumes that dogs, like humans, show limited to no absorption of intravitreally administered TRIAM,37 then the results indicate lack of effect of locally administered TRIAM on ERK1/2 phosphorylation.
In summary, our biochemical results demonstrate that systemic DEX inhibited the principal components of the AP-1 molecular pathway after exposure to light of the T4R RHO mutant retina. In contrast, locally administered TRIAM had no to minimal effects on ERK1/2 activation and c-Fos phosphorylation; similarly, the effects on AP-1 DNA binding activity are equally modest.
Regardless of whether systemic or ocular steroids modify the AP-1 signaling pathway, an important question is whether they prevent or modify the retinal degeneration that results from clinical exposure to lights. Although there were some treatment-related differences in the response of the retina to light, it was clear that end-stage retinal degeneration was the common outcome of clinical light exposure regardless of treatment, and, in the degenerate retina, the predominant photo-receptor class that survived were cones. Preservation of RPE cells in retinas from animals treated with IV DEX was a prominent finding, even though the outer retinal degeneration was similar whether the RPE cell layer was present or absent. RPE damage and degeneration associated with exposure to light is a feature of the RHO mutant dog retina, and also occurs in normal albino rats with light-induced damage, although the timing of photoreceptor and RPE apoptosis is different between the two cell types.1,40 RPE degeneration secondary to light-induced damage is not a significant finding in wild-type mice4 or T17M RHO mutant mice (Lewin A, personal communication, June 2008), suggesting that the RPE response to similar light insults is species specific.
Systemic DEX also resulted in marked suppression of the GFAP activation of Müller cells. The untreated, exposed mutant retina showed GFAP expression extending throughout the radial fibers. The Müller processes projected into the subretinal space and coursed parallel to the external limiting membrane. Although this is a feature reported for many chronic photoreceptor degenerations,41 previously we have not observed such a Müller cell response in dogs.24 This effect may be related to the acute disruption of the external limiting membrane caused by exposure to light. A similar outgrowth of Müller cells into the subretinal space has been reported in animal models of retinal detachment as well as in human tissue samples.42
To localize the components of the AP-1 signaling pathway in the treated retinas and complement the biochemical analyses, we used immunohistochemistry to examine p-c-Fos and p-ERK1/2 expression. As in light-exposed untreated mutant retinas,19 these proteins were localized in Müller cells as evident by their colocalization with CRALBP. In both TRIAM- and DEX-treated animals, both p-c-Fos and p-ERK1/2 were expressed in Müller cells of light-exposed eyes. For p-c-Fos, there were no qualitative differences noted between light-exposed DEX- and TRIAM-treated mutant retinas. In contrast, immunohistochemistry confirmed the immunoblot analysis results by showing a decrease in ERK1/2 phosphorylation after steroid treatment.
Our results are not in agreement with those in published studies implicating the AP-1 molecular pathway in light-induced photoreceptor degeneration (see Refs. 4, 19 for review). This molecular pathway has been proposed, in part, by finding that photoreceptor degeneration is prevented through the inhibition of AP-1 by activation of the glucocorticoid receptor in wild-type mice.18 Although IV DEX markedly suppressed the known components of the AP-1 signaling pathway in the canine retina, photoreceptor degeneration was not prevented, even though systemic DEX appeared to protect the RPE and inhibit Müller cell reactivity. One could argue that the doses used are “subtherapeutic” as a dose-response curve was not calculated, and higher doses may have prevented the degeneration. Although that is true, we posit that the doses used either locally or systemically were quite high, particularly with IV DEX, of which we used doses 10- to 20-fold higher than that used in emergency situations. In contrast, AP-1 inhibition through activation of the glucocorticoid receptor in mice required a dose of 52 mg/kg of dexamethasone, and lower doses (e.g., 22 and 37 mg/kg), only offered partial protection.18 Such suprapharmacologic doses in mice may well have broader effects than those associated with AP-1 inhibition and are problematic to extrapolate to larger species such as dogs or humans.
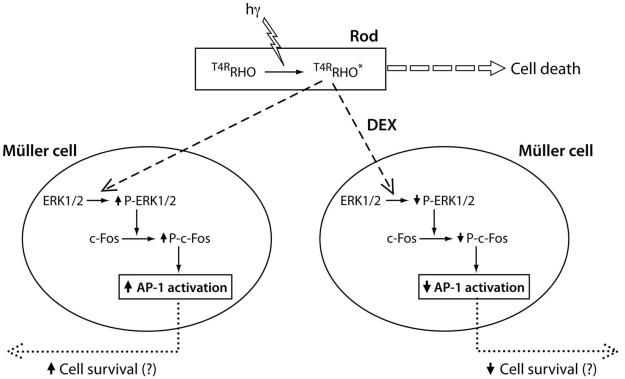
Our studies further support the hypothesis that the signaling components of the AP-1 molecular pathway are localized to Müller cells, not to the photoreceptors, and support a role for AP-1 in cell survival, rather than cell death.19 The localization of this pathway to Müller cells is not influenced by pretreatment with steroids (Fig. 10). Müller cell reactivity after a diverse array of retinal injuries is thought to promote an initial survival response through the release of neurotrophic factors and antioxidants43-45 after the early, nonspecific ERK activation and upregulation of GFAP expression.46 If these responses are survival rather than cell death signals, why then does the steroid-treated retina not show greater damage, especially with IV DEX, than the untreated mutant retinas? This may depend on the light intensity used, so that overwhelming damage occurs and modulation of degeneration, either worsening or ameliorated, cannot be recognized. Establishing threshold intensities for these lesions will allow these hypotheses to be tested experimentally.
FIGURE 10.
The events that occur after clinical light exposure that cause photoreceptor degeneration in the T4R RHO mutant retina in the presence or absence of systemic DEX. In the untreated mutant retina, exposure to light resulted in phosphorylation of ERK1/2 and c-Fos and increased DNA binding by AP-1 (AP-1 activation). Our previous results suggest that AP-1 activation results in a cell survival response initiated in Müller cells.19 Treatment with systemic DEX inhibits phosphorylation of ERK1/2 and c-Fos, and AP-1 DNA binding activity is not increased. This may result in a decreased cell survival response mediated by Müller cells. However, regardless of systemic DEX treatment, clinical light exposure of the T4R RHO mutant retina leads to photoreceptor cell death.
Last, although AP-1 has been ruled out as the critical player in the cell-death signal and studies are now in progress to identify other candidate molecules that play a role in cell death or survival, it is of equal importance to consider how the mutant opsin triggers disease, as this is informative regarding disease mechanisms that can be tested experimentally. Gaining this information will require examination of the interaction of ambient light versus exposure to bright light, the effect of serial graded bleachings that are not damaging after single exposure, and the effect of full rhodopsin bleaching in light-adapted versus dark-adapted retinas. These studies are now in progress.
Acknowledgments
The authors thank Julie Jordan for histology support; the RDS facility staff for technical assistance; Mary Leonard for the figure illustrations; Jack Saari and Cheryl Craft for the CRALBP and hCAR antibodies; and Artur Cideciyan for the light-intensity measurements and helpful comments on rhodopsin bleaching.
Supported by National Eye Institute Grants EY-06855, -13132, and -017549; The Foundation Fighting Blindness Center and individual investigator grants; the University of Pennsylvania Research Foundation; a Fight for Sight Nowak family grant; the Van Sloun Fund for Canine Genetic Research; Vision Research Center Grant P30 EY-001583; The ONCE International Prize for R&D in Biomedicine and New Technologies for the Blind; and Hope for Vision. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Eye Institute or the National Institutes of Health.
Footnotes
Disclosure: D. Gu, None; W.A. Beltran, None; S. Pearce-Kelling, None; Z. Li, None; G.M. Acland, None, G.D. Aguirre, None.
References
- 1.Noell WK, Walker VS, Kang BS, Berman S. Retinal damage by light in rats. Invest Ophthalmol. 1966;5:450–473. [PubMed] [Google Scholar]
- 2.Noell WK, Albrecht R. Irreversible effects of visible light on the retina: role of vitamin A. Science. 1971;172:76–80. doi: 10.1126/science.172.3978.76. [DOI] [PubMed] [Google Scholar]
- 3.Jacobson SG, McInnes RR. Blinded by the light. Nat Genet. 2002;32:215–216. doi: 10.1038/ng1002-215. [DOI] [PubMed] [Google Scholar]
- 4.Wenzel A, Grimm C, Samardzija M, Reme CE. Molecular mechanisms of light-induced photoreceptor apoptosis and neuroprotection for retinal degeneration. Prog Retin Eye Res. 2005;24:275–306. doi: 10.1016/j.preteyeres.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Hao W, Wenzel A, Obin MS, et al. Evidence for two apoptotic pathways in light-induced retinal degeneration. Nat Genet. 2002;32:254–260. doi: 10.1038/ng984. [DOI] [PubMed] [Google Scholar]
- 6.Kijas JW, Cideciyan AV, Aleman TS, et al. Naturally occurring rhodopsin mutation in the dog causes retinal dysfunction and degeneration mimicking human dominant retinitis pigmentosa. Proc Natl Acad Sci U S A. 2002;99:6328–6333. doi: 10.1073/pnas.082714499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li T, Sandberg MA, Pawlyk BS, et al. Effect of vitamin A supplementation on rhodopsin mutants threonine-17→methionine and proline-347→serine in transgenic mice and in cell cultures. Proc Natl Acad Sci U S A. 1998;95:11933–11938. doi: 10.1073/pnas.95.20.11933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van den Born LI, Vvan Schooneveld MJ, de Jong LAMS, et al. Thr4Lys rhodopsin mutation is associated with autosomal dominant retinitis pigmentosa of the cone-rod type in a small Dutch family. Ophthalmic Genet. 1994;15:51–60. doi: 10.3109/13816819409098864. [DOI] [PubMed] [Google Scholar]
- 9.Li Z-Y, Jacobson SG, Milam AH. Autosomal dominant retinitis pigmentosa caused by the threonine-17-methionine rhodopsin mutation: retinal histopathology and immunocytochemistry. Exp Eye Res. 1994;58:397–408. doi: 10.1006/exer.1994.1032. [DOI] [PubMed] [Google Scholar]
- 10.Zhu L, Jang GF, Jastrzebska B, et al. A naturally occurring mutation of the opsin gene (T4R) in dogs affects glycosylation and stability of the G protein-coupled receptor. J Biol Chem. 2004;279:53828–53839. doi: 10.1074/jbc.M408472200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacobson S, Kemp CM, Sung CH, Nathans J. Retinal function and rhodopsin levels in autosomal dominant retinitis pigmentosa with rhodopsin mutations. Am J Ophthalmol. 1991;112:256–271. doi: 10.1016/s0002-9394(14)76726-1. [DOI] [PubMed] [Google Scholar]
- 12.Kemp CM, Jacobson SG, Roman AJ, Sung C-H, Nathans J. abnormal rod dark adaptation in autosomal dominant retinitis pigmentosa with proline-23-histidine rhodopsin mutation. Am J Ophthalmol. 1992;113:165–174. doi: 10.1016/s0002-9394(14)71529-6. [DOI] [PubMed] [Google Scholar]
- 13.Cideciyan AV, Hood DC, Huang Y, et al. Disease sequence from mutant rhodopsin allele to rod and cone photoreceptor degeneration in man. Proc Natl Acad Sci U S A. 1998;95:7103–7108. doi: 10.1073/pnas.95.12.7103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cideciyan AV, Jacobson SG, Aleman TS, et al. In vivo dynamics of retinal injury and repair in the rhodopsin mutant dog model of human retinitis pigmentosa. Proc Natl Acad Sci U S A. 2005;102:5233–5238. doi: 10.1073/pnas.0408892102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.White DA, Hauswirth WW, Kaushal S, Lewin AS. Increased sensitivity to light-induced damage in a mouse model of autosomal dominant retinal disease. Invest Ophthalmol Vis Sci. 2007;48:1942–1951. doi: 10.1167/iovs.06-1131. [DOI] [PubMed] [Google Scholar]
- 16.Hafezi F, Steinbach JP, Marti A, et al. The absence of c-fos prevents light-induced apoptotic cell death of photoreceptors in retinal degeneration in vivo. Nat Med. 1997;3:346–349. doi: 10.1038/nm0397-346. [DOI] [PubMed] [Google Scholar]
- 17.Wenzel A, Grimm C, Marti A, et al. c-fos controls the “private pathway” of light-induced apoptosis of retinal photoreceptors. J Neurosci. 2000;20:81–88. doi: 10.1523/JNEUROSCI.20-01-00081.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wenzel A, Grimm C, Seeliger MW, et al. Prevention of photoreceptor apoptosis by activation of the glucocorticoid receptor. Invest Ophthalmol Vis Sci. 2001;42:1653–1659. [PubMed] [Google Scholar]
- 19.Gu D, Beltran WA, Li Z, Acland GM, Aguirre GD. Clinical light exposure, photoreceptor degeneration, and AP-1 activation: a cell death or cell survival signal in the rhodopsin mutant retina? Invest Ophthalmol Vis Sci. 2007;48:4907–4918. doi: 10.1167/iovs.07-0428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aguirre GD, Acland GM. Models, mutants and man: searching for unique phenotypes and genes in the dog model of inherited retinal degeneration. In: Ostrander EA, Giger U, Lindblad-Toh K, editors. The Dog and Its Genome. Cold Spring Harbor Laboratory Press; Cold Spring Harbor, NY: 2006. pp. 291–325. [Google Scholar]
- 21.Buyukmihci N, Aguirre GD. Rod disc turnover in the dog. Invest Ophthalmol. 1976;15:579–584. [PubMed] [Google Scholar]
- 22.Beltran WA, Rohrer H, Aguirre GD. Immunolocalization of ciliary neurotrophic factor receptor alpha (CNTFRalpha) in mammalian photoreceptor cells. Mol Vis. 2005;11:232–244. [PubMed] [Google Scholar]
- 23.Gorski K, Carneiro M, Schibler U. Tissue-specific in vitro transcription from the mouse albumin promoter. Cell. 1986;47:767–776. doi: 10.1016/0092-8674(86)90519-2. [DOI] [PubMed] [Google Scholar]
- 24.Beltran WA, Hammond P, Acland GM, Aguirre GD. A frameshift mutation in RPGR exon ORF15 causes photoreceptor degeneration and inner retina remodeling in a model of X-linked retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2006;47:1669–1681. doi: 10.1167/iovs.05-0845. [DOI] [PubMed] [Google Scholar]
- 25.Acland GM, Aguirre GD. Retinal degenerations in the dog: IV. Early retinal degeneration (erd) in Norwegian elkhounds. Exp Eye Res. 1987;44:491–521. doi: 10.1016/s0014-4835(87)80160-4. [DOI] [PubMed] [Google Scholar]
- 26.Rubinfeld H, Seger R. The ERK cascade: a prototype of MAPK signaling. Mol Biotechnol. 2005;31:151–174. doi: 10.1385/MB:31:2:151. [DOI] [PubMed] [Google Scholar]
- 27.Angel P, Karin M. The role of Jun, Fos and the AP-1 complex in cell-proliferation and transformation. Biochim Biophys Acta. 1991;1072:129–157. doi: 10.1016/0304-419x(91)90011-9. [DOI] [PubMed] [Google Scholar]
- 28.Reddy SP, Mossman BT. Role and regulation of activator protein-1 in toxicant-induced responses of the lung. Am J Physiol Lung Cell Mol Physiol. 2002;283:L1161–L1178. doi: 10.1152/ajplung.00140.2002. [DOI] [PubMed] [Google Scholar]
- 29.Karin M, Liu Z, Zandi E. AP-1 function and regulation. Curr Opin Cell Biol. 1997;9:240–246. doi: 10.1016/s0955-0674(97)80068-3. [DOI] [PubMed] [Google Scholar]
- 30.Samardzija M, Wenzel A, Aufenberg S, Thiersch M, Reme C, Grimm C. Differential role of Jak-STAT signaling in retinal degenerations. FASEB J. 2006;20:2411–2413. doi: 10.1096/fj.06-5895fje. [DOI] [PubMed] [Google Scholar]
- 31.Paskowitz DM, LaVail MM, Duncan JL. Light and inherited retinal degeneration. Br J Ophthalmol. 2006;90:1060–1066. doi: 10.1136/bjo.2006.097436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Komaromy AM, Acland GM, Aguirre GD. Operating in the dark: a night-vision system for surgery in retinas susceptible to light damage. Arch Ophthalmol. 2008;126:714–717. doi: 10.1001/archopht.126.5.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim JE, Pollack JS, Miller DG, Mittra RA, Spaide RF. ISIS-DME: a prospective, randomized, dose-escalation intravitreal steroid injection study for refractory diabetic macular edema. Retina. 2008;28:735–740. doi: 10.1097/IAE.0b013e318163194c. [DOI] [PubMed] [Google Scholar]
- 34.Anijeet DR, Hanson RJ, Bhagey J, Bates RA. National survey of the technique of intravitreal triamcinolone injection in the United Kingdom. Eye. 2007;21:480–486. doi: 10.1038/sj.eye.6702232. [DOI] [PubMed] [Google Scholar]
- 35.Jonas JB, Schlichtenbrede F. Visual acuity and intraocular pressure after high-dose intravitreal triamcinolone acetonide in selected ocular diseases. Eye. 2008;22(7):869–73. doi: 10.1038/sj.eye.6702734. [DOI] [PubMed] [Google Scholar]
- 36.Molleda JM, Tardon RH, Gallardo JM, Martin-Suarez EM. The ocular effects of intravitreal triamcinolone acetonide in dogs. Vet J. 2008;176:326–332. doi: 10.1016/j.tvjl.2007.02.031. [DOI] [PubMed] [Google Scholar]
- 37.Degenring RF, Jonas JB. Serum levels of triamcinolone acetonide after intravitreal injection. Am J Ophthalmol. 2004;137:1142–1143. doi: 10.1016/j.ajo.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 38.Karin M. The regulation of AP-1 activity by mitogen-activated protein kinases. J Biol Chem. 1995;270:16483–16486. doi: 10.1074/jbc.270.28.16483. [DOI] [PubMed] [Google Scholar]
- 39.Murphy LO, Blenis J. MAPK signal specificity: the right place at the right time. Trends Biochem Sci. 2006;31:268–275. doi: 10.1016/j.tibs.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 40.Hafezi F, Marti A, Munz K, Reme CE. Light-induced apoptosis: differential timing in the retina and pigment epithelium. Exp Eye Res. 1997;64:963–970. doi: 10.1006/exer.1997.0288. [DOI] [PubMed] [Google Scholar]
- 41.Jones BW, Marc RE. Retinal remodeling during retinal degeneration. Exp Eye Res. 2005;81:123–137. doi: 10.1016/j.exer.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 42.Fisher SK, Lewis GP, Linberg KA, Verardo MR. Cellular remodeling in mammalian retina: results from studies of experimental retinal detachment. Prog Retin Eye Res. 2005;24:395–431. doi: 10.1016/j.preteyeres.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 43.Oku H, Ikeda T, Honma Y, et al. Gene expression of neurotrophins and their high-affinity Trk receptors in cultured human Müller cells. Ophthalmic Res. 2002;34:38–42. doi: 10.1159/000048323. [DOI] [PubMed] [Google Scholar]
- 44.Honjo M, Tanihara H, Kido N, Inatani M, Okazaki K, Honda Y. Expression of ciliary neurotrophic factor activated by retinal Muller cells in eyes with NMDA- and kainic acid-induced neuronal death. Invest Ophthalmol Vis Sci. 2000;41:552–560. [PubMed] [Google Scholar]
- 45.Schutte M, Werner P. Redistribution of glutathione in the ischemic rat retina. Neurosci Lett. 1998;246:53–56. doi: 10.1016/s0304-3940(98)00229-8. [DOI] [PubMed] [Google Scholar]
- 46.Bringmann A, Pannicke T, Grosche J, et al. Müller cells in the healthy and diseased retina. Prog Retin Eye Res. 2006;25:397–424. doi: 10.1016/j.preteyeres.2006.05.003. [DOI] [PubMed] [Google Scholar]