Abstract
Here we confirm that intranasal (IN) dry powder anthrax vaccine formulations are able to protect rabbits against aerosol challenge 9 weeks after a single immunization. The optimum dose of rPA in our dry powder anthrax vaccine formulation in rabbits was experimentally determined to be 150 μg and therefore was chosen as the target dose for all subsequent experiments. Rabbits received a single dose of either 150 μg rPA, 150 μg rPA + 150 μg of a conjugated 10-mer peptide representing the B. anthracis capsule (conj), or 150 μg of conj alone. All dry powder formulations contained MPL and chitosan (ChiSys®). Significant anti-rPA titers and anthrax lethal toxin neutralizing antibody (TNA) levels were seen with both rPA containing vaccines, although rPA-specific IgG and TNA levels were reduced in rabbits immunized with rPA plus conj. Nine weeks after immunization, rabbits were exposed to a mean aerosol challenge dose of 278 LD50 of Ames spores. Groups immunized with rPA or with rPA + conj had significant increases in survivor proportions compared to the negative control group by Logrank test (p = 0.0001 and 0.003, respectively), and survival was not statistically different for the rPA and rPA + conj immunized groups (p = 0.63). These data demonstrate that a single immunization with our dry powder anthrax vaccine can protect against a lethal aerosol spore challenge 9 weeks later.
1. Introduction
Bacillus anthracis is a gram-positive, spore forming, facultative anaerobic bacterium and the causative agent of anthrax. An anthrax infection can manifest in three ways depending on the route of transmission; cutaneous, inhalation and gastrointestinal anthrax [1]. Inhalation anthrax, the most likely form that will result from a bioterrorist attack, is relatively rare and usually fatal even with aggressive treatment [2]. Since the earliest symptoms of disease are non-specific [3–6] recognition of exposure and initiation of appropriate treatment may not occur soon enough to be effective. The only licensed vaccine, Anthrax Vaccine Adsorbed (BioThrax®), is probably effective and safe according to the Institute of Medicine. However, the Institute also recommended development of an improved vaccine that has a less daunting immunization schedule and reduced reactogenicity [7]. “Second-generation” anthrax vaccines that have undergone clinical trials in the U.S. are parenterally delivered, and the primary mechanism of protection is through development of anti-protective antigen (PA) immune responses. The considerable reduction in antigenic complexity of the new vaccines from that of the currently licensed vaccine is expected to minimize reactogenicity while eliciting systemic anti-PA humoral responses that correlate with protection. However, these next-generation vaccines may have several shortcomings. For instance, they require needles to be administered, and thus are inappropriate for administration in the field by untrained personnel. The vaccines currently under clinical examination also require a cold chain until the time of administration, which is expensive and considered impractical under field conditions.
We have specifically designed our anthrax vaccine to address those characteristics identified by the Institutes of Medicine in 2002 as desirable for an advanced vaccine. Our dry powder anthrax vaccine was formulated with recombinant protective antigen (rPA) and two immune enhancing additives. One was a toll-like receptor-4 (TLR-4) agonist, monophosphoryl lipid A (MPL) to increase the adaptive immune response, and the other was chitosan, a mucoadhesive to maximize the exposure of the vaccine in the host nasal passages to immune effector cells [8].
Our nasally delivered anthrax vaccine may have numerous advantages over parenteral immunization. Needle-free delivery has high potential for self-administration, and a dry powder formulation is expected to have excellent stability characteristics in the absence of a continuous cold chain. In a recent publication, a similar dry powder formulation had greatly improved rPA stability over liquid formulations [9,10]. The dry powder formulations maintained rPA integrity under both ambient and elevated temperatures for approximately 1 month, while the liquid formulations showed rapid degradation. This anticipated enhanced stability of our dry powder anthrax vaccine will increase shelf life and decrease replacement costs, which are important considerations for a stockpiled vaccine. Having no requirement for continuous cold chain will also greatly ease the logistics of transport and storage in case of the need for rapid mass distribution. All of these qualities will be particularly valuable in a vaccine that also quickly stimulates broadly protective responses.
One of the most desirable qualities would be the ability to protect a recipient soon after immunization with a single dose. Based on observations that a single intramuscular (IM) immunization was shown to protect against a low dose aerosol challenge [11] and observations from preliminary studies (unpublished data, [12]), we sought to determine if protective immunity could be achieved with a single IN dose of our dry powdered anthrax vaccine.
The data presented herein describe results of immunizing rabbits IN with a single dose of dry powder anthrax vaccine and then challenging with aerosolized Bacillus anthracis spores. We describe the optimum dose of rPA in our vaccine regimen to induce anti-rPA antibody levels that are protective in rabbits. The data also demonstrate that the vaccinated rabbits not only survived challenge, but were able to limit active infection as indicated by modest post-challenge titers against lethal factor (LF) which would only be present in animals that had experienced an active B. anthracis infection. It has been reported that rPA-specific serum IgG levels as low as 20μg/mL have shown to be protective [13]. In this report we measured antigen-specific immune responses in this range following a single dose of vaccine as early as 21 days after immunization. The combination of rapid, protective immune responses resulting from a single dose vaccine, the ability to be self-administered and reduced storage requirements could facilitate rapid protection of the greatest number of potential victims. Our dry powder anthrax vaccine seeks to address these desirable attributes.
2. Methods and Materials
2.1 Materials and reagents
Recombinant anthrax protective antigen (rPA) was obtained in frozen form from VaxGen, Inc. (South San Francisco, CA). Anthrax lethal factor (LF) was obtained in lyophilized form from List Biological Laboratories (Campbell, CA) and MPL (administered 50μg per animal) from GlaxoSmithKline (Philadelphia, Pennsylvania). The ChiSys®- based formulations were provided by Archimedes Development Limited (Nottingham, UK) and utilized chitosan glutamate (Protasan UPG 213). Mannitol (Mannitol 60) was obtained from Roquette (Lestrem, France) and all other reagents were acquired from Sigma (St. Louis, MO or Poole, UK), except where indicated. The 10-mer capsule peptide was synthesized by AnaSpec, Inc. (San Jose, CA) as previously described [14].
2.2 Peptide conjugation to rPA
A 10-mer peptide representing the B. anthracis capsule (Ac-CGGG-[g-D-glu]9-g-D-glu) was conjugated to BSA, which functioned as a carrier protein, as follows. Five milligrams of BSA (Vector Laboratories, Burlingame, CA) was dissolved in 1mL 0.1M potassium phosphate (pH 7.4); 200 μL of 2 M potassium phosphate and 5 mg of SBAP (Succinimidyl 3-[bromoacetamido] propionate, Pierce, Rockford, IL), dissolved in 50 μL dimethyl sulfoxide (DMSO), were mixed on a rotator end-over-end at room temperature for 2 hours. The SBAP-treated BSA was dialyzed against 10 mM sodium phosphate, pH 7.4 at 4°C overnight then incubated with an additional 200 μL of 2 M potassium phosphate and 5 mg of 10-mer capsule peptide at pH 7.6 on the rotator overnight at 4°C. The10-mer capsule peptide-BSA conjugate was dialyzed exhaustively against phosphate buffered saline (PBS; 137 mM NaCl, 2.7 mM potassium chloride, 10 mM phosphate buffer Na2HPO4/KH2PO4, pH 7.4). The resulting capsule-conjugate was analyzed by SDS-PAGE and Coomassie blue stained gels revealing an upward shift in molecular weight compared to unconjugated BSA, confirming the crosslinking of the capsule peptide to BSA (data not shown). The resulting capsule peptide-BSA conjugate is referred to as “conj”.
2.3 Dry powder vaccine formulations
Solutions used in the production of the dry powder formulations were prepared by combining the appropriate amounts of rPA, BSA-conj, and 50μg MPL (solubilized in ethanol), water and 100 mg/mL mannitol/HEPES (1 g mannitol dissolved in 10 mL of 5 mM, pH 7.5 HEPES buffer). The solutions were frozen in liquid nitrogen followed by lyophilization in a ThermoSavant ModulyoD Freeze Drier (GMI, Ramsey MN) for 36 to 48 hours. To produce a uniform powder, freeze-dried solid samples were transferred to a small glass mortar, mixed carefully with chitosan using a pestle and then passed through a 250 μm sieve. Powders were then transferred into 20 mL glass vials which were sealed and further mixed using a Turbula T2C mixer (Glen Mills, Clifton, NJ) at speed 2 for 30 minutes. Vials were then stored at 4°C in a desiccator until loading into Valois Monopowder devices (Valois Pharmaceutical Division, Le Vaudreuil, France; nominal fill weight 11 mg). The loaded devices and injection vials were stored in polyethylene bags with silica gel sachets at 0–4°C until use. The emitted powder dose was predetermined to be 10 mg when the device was actuated. One-half dosage of vaccine was delivered in 10 mg of powder, requiring two nasal administration devices for each rabbit that received the dry powder formulations (one for each nostril). Negative control formulations contained MPL and chitosan only.
2.4 Liquid vaccine formulations
Recombinant PA formulated in alum (aluminum hydroxide) was thawed on ice just prior to use, and diluted with appropriate amounts of alum in buffer (1.5 mg/mL alum in 20 mM Tris, 0.9% NaCl, 0.01% Polysorbate 80, pH 7.4) to a final dosage of either 100 μg or 150 μg of rPA and 750 μg alum. The liquid vaccine formulations were compounded immediately prior to use and kept on ice until administration.
2.5 Immunization of rabbits
Groups of female New Zealand White rabbits (Myrtle’s Rabbitry, Thompson Station, TN) approximately 10–12 weeks of age were immunized on day 0 with the vaccine formulations shown in each figure legend. Immunizations were administered to animals on days 0 under firm restraint, but without anesthesia. All dry powder vaccine formulations were administered via the IN route. The positive control rabbits were vaccinated by IM injection into in the lumbar region with 100 μL of the liquid formulation.
2.6 Sample collection and analysis by ELISA
Serum samples were collected prior to the first immunization (day 0), and again on day 21 (week 3) and on day 42 (week 6). Serum was analyzed by Enzyme-Linked ImmunoSorbent Assay (ELISA) for antigen-specific antibody responses. All wells of 96-well plates (Nunc, Rochester, NY) were coated with 100 ng/well rPA in PBS, pH 7.2 for 2 hours at room temperature. Wells were then blocked 1 hour at room temperature with PBS/0.05% Tween-20 (PBST) + 10% normal goat serum (GS). Serum samples were serially diluted four-fold in PBST/GS beginning at 1:600 and continuing down to 1:614,400. Calibrated rabbit anti-rPA serum, which served as a standard curve, was serially diluted in duplicate on all plates and used to calculate the quantity of anti-rPA antibody present in the test sera. The test and standard serum dilutions were incubated on plates at room temperature for 2 hours and then wells were washed three times with PBST. The rabbit antibodies binding to rPA were then detected via 1.5 hour incubation at room temperature with HRP-conjugate goat anti-rabbit IgG (Southern Biotech, Birmingham, AL) diluted 1/2000 into PBST/GS. Wells were washed again three times with PBST, and the plate developed with 2,2′-azino-bis(3-ethylbenzthiazoline-6-sulphonic acid) (ABTS) (Pierce, Rockford, IL) for 45 minutes at room temperature. Optical density readings at 405 nm for the test samples and standard curves were plotted against their respective dilution (reciprocal) using SoftMax® Pro software (Molecular Devices Corporation, Sunnyvale, CA). Anti-capsule and anti-lethal factor (LF) IgG ELISAs were conducted in the same manner using dilutions of rabbit IgG (Southern Biotech, Birmingham, AL) to prepare the standard curve. Standard curves consisted of four-fold serial dilutions of from 100 ng/well to 0.097 ng/well in duplicate wells. Anti-10-mer capsule antibodies were detected by coating plates with 200 ng/well of unconjugated 10-mer capsule peptide and plates were coated with 100 ng/well of rLF was used for anti-LF antibody detection. Anti-rLF concentrations were expressed as units per mL (U/mL), with each unit equating to approximating 1 μg of IgG.
ELISA results are expressed as geometric mean values (GMN) and were statistically analyzed by non-parametric ANOVA (Kruskal-Wallis test) followed by Dunn’s Multiple Comparison test of treatment means using Prism 4 software (GraphPad Software, Inc., San Diego, CA). Differences between treatment group means were considered significant at p < 0.05.
2.7 Lethal toxin (LeTx) neutralization assays (TNA)
Murine macrophage-like J774A.1 cells were seeded in 96 well plates (Corning™ COSTAR™, Acton, MA) at a density of 3 ×104 cells/well in 75 μL Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% fetal bovine serum (FBS), and then cultured overnight at 37°C in 5% CO2. Sera were diluted three to five-fold beginning at 1:100 in DMEM/10% FBS. Dilutions of sera were then incubated with an equal volume of rPA (0.8 μg/mL) and rLF (8 μg/mL) in DMEM/10% FBS for 1 hour at 37°C. Twenty five μL of the toxin/serum solutions were then added to the J774.1 cell and plates incubated at 37°C and 5% CO2 for three to four hours. Cell viability was measured using the fluorescence-based Promega CellTiter-Blue™ assay as per the manufacturer’s protocol (Promega, Madison, WI). Twenty μL of the CellTiter-Blue™ substrate was added to each well and incubation continued at 37°C and 5% CO2 for two hours. Fluorescence was then measured at 590 nm after excitation at 560 nm. Rabbit serum previously determined to protect 50% of the cells at a dilution > 5000 was included in assays as a positive control, and wells that received toxin mixed with normal rabbit serum served as negative controls for toxin killing. All sera were analyzed in triplicate, and the coefficient of variation between wells was consistently less than 15% (data not shown). The ED50 (the dilution of serum that will inhibit death of 50% of the cells) was calculated for each serum sample, where 50% survival equaled the fluorescence midway between that measured for the highest and lowest cell viabilities on the plate, including controls. This value was obtained by extrapolation from a four-parameter curve (SoftMax® Pro software) fitted to a graph of the dilution factor (X axis) and the resulting fluorescence (Y axis). Mean ED50 values by immunization group are expressed as geometric mean values (GMN) and were compared by non-parametric ANOVA (Kruskal-Wallis test) followed by Dunn’s Multiple Comparison test of treatment means as described above. Again, differences were considered significant if p < 0.05.
2.8 Aerosolized spore challenge
The efficacy of the dry powder vaccine formulations were tested using rabbits vaccinated with formulations containing MPL, chitosan and either 150 μg rPA, 150 μg rPA + 150 μg conj, or 150 μg conj. An additional group of rabbits that received 150 μg BSA was included in the challenge to serve as a negative control. The rabbits were transported to the Battelle Medical Research & Evaluation Facility (West Jefferson, OH) eight weeks after the initial immunization. After one week of quarantine, rabbits were aerosol challenge with a mean dose of 278 LD50 of Ames B. anthracis spores based on a benchmark LD50 of 105,000 cfu [15] delivered via a muzzle-only inhalation exposure chamber. Animals were monitored twice daily during the quarantine period as well as for 14 days following challenge for clinical signs including, but not limited to diarrhea, respiratory distress, decreased appetite, weight loss and activity. Deaths were recorded at the time of observation. Rabbits that survived the post-challenge period were anesthetized with Acepromazine (0.7 mL), and terminal serum samples collected. Following serum collection, the rabbits were euthanized. Serum samples collected from survivors were analyzed for IgG responses specific to rPA and LF. All surviving rabbits were negative for post challenge bacteremia (data not shown).
3. Results
3.1 Determination of the optimum rPA dose in a single intranasal powder immunization to maximize PA-specific antibody responses in rabbits
Two identical experiments were conducted to initially determine and then confirm the most effective rPA dose for eliciting anti-rPA IgG and lethal toxin neutralizing antibodies in rabbits immunized IN once with our dry powder vaccine formulation. Results of the two experiments were statistically indistinguishable, therefore all data were combined for presentation herein. Rabbits were vaccinated either IN with dry powders formulations containing either 50 μg, 100 μg or 150 μg of rPA or IM with 100 μg of rPA formulated with alum. Serum antibody responses were measured by ELISA pre-immunization and at 0, 3 and 6-weeks. No serum rPA-specific IgG response was detected in animals prior to immunization (data not shown). Serum levels of rPA-specific IgG three and six weeks after immunization are shown in Figure 1. Three weeks post-immunization, the powder formulation that contained the highest dose of rPA (150 μg) elicited statistically significant increased serum anti-rPA IgG (GMN = 14.8 μg/mL, p < 0.05) compared to the negative control. The group that received the IM immunization of 100 μg rPA + alum mounted a robust anti-rPA serum antibody response (40.4 μg/mL, p < 0.001) compared to the other groups at three weeks. However, the rPA-specific response waned in the IM immunized rabbits by 6 weeks post immunization (6.6 μg/mL), and became statistically indistinguishable from that of the negative control group (p > 0.05). The most robust serum rPA-specific antibody responses six weeks after immunization were measured in rabbits immunized IN with 150 μg of rPA (18.8 μg/mL) (p < 0.001).
Figure 1.
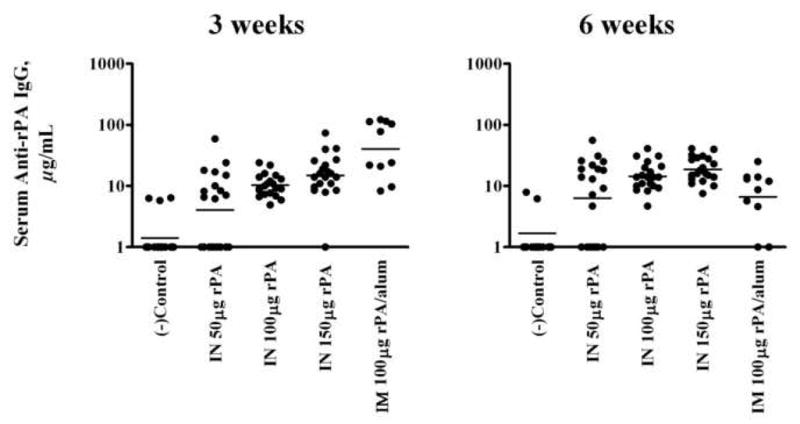
rPA-specific IgG concentrations in rabbits 3 weeks and 6 weeks post immunization. Serum samples were collected 3 and 6 weeks following a single IN vaccination with dry powder vaccine formulations containing 0, 50, 100 or 150 μg rPA. rPA combined with alum was injected IM served as a control. Horizontal bars indicate geometric means. Twenty rabbits were used in each group with the exception of the IM group, which consisted of 10 rabbits. Means were compared by non-parametric ANOVA.
The ability to neutralize anthrax LeTx cytotoxicity was also measured in the serum of the immunized rabbits. The titer was expressed as the reciprocal of the dilution required to inhibit 50% of the cytotoxic effects on J774A.1 cells and is referred to as the ED50. The results are shown in Figure 2. The 150 μg rPA dry powder formulation induced the highest geometric mean TNA titers, with mean ED50 values at 3 and 6 weeks post-immunization of 105.2 and 33.4, respectively, which were both statistically different from the negative control (p < 0.001). This mean response was significantly greater (p < 0.05) than all other groups at week 3 except for the IM immunized groups that received rPA + alum. The IM formulation also induced a significant mean neutralizing titer at 3 weeks (83.5, p < 0.001), but not at 6 weeks post immunization (12.8, p > 0.05) from the negative control. Although measurable, the mean neutralizing titers of the remaining groups at 3 and 6 weeks were not statistically different from that of the negative control group, including the dry powder formulation containing 100 μg of rPA.
Figure 2.
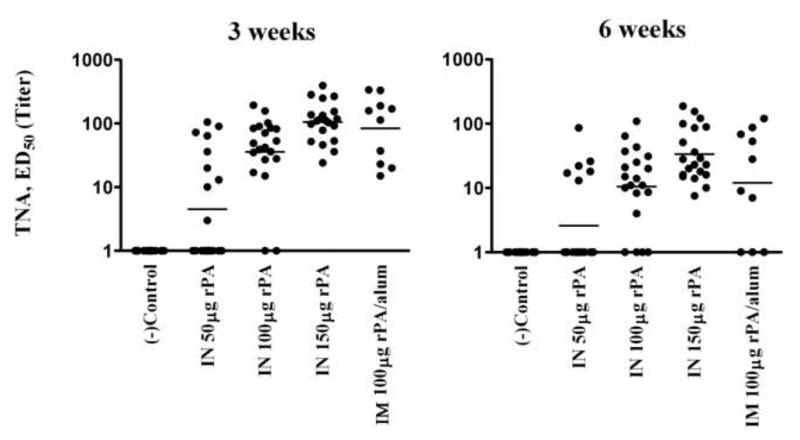
TNA titers after a single immunization. Serum samples were collected 3 and 6 weeks following a single IN vaccination with dry powder vaccine formulations containing 0, 50, 100 or 150 μg of rPA. rPA combined with alum was injected IM served as a control. Horizontal bars indicate geometric means. Twenty rabbits were used in each group with the exception of the IM group, which consisted of 10 rabbits. Means were compared by non-parametric ANOVA.
3.2 Dry powder vaccine formulations protect rabbits against challenge following a single IN immunization
The main objective of this experiment was to test the efficacy of a single IN dry powder formulation immunization using the dose of rPA determined most effective in the previous experiments. Another objective was to determine if a single IN vaccination with a formulation containing a 10-mer capsule peptide could stimulate anti-capsule immune responses that would be protective. Rabbits were vaccinated either IN once with either 150 μg rPA with or without 150 μg conj or IM with 150 μg of rPA precipitated with alum. All dry powder formulations contained MPL and chitosan. Serum antibody levels were monitored at 3 and 6 weeks post-vaccination for rPA-specific IgG and TNA titers (Figure 3). Rabbits that were vaccinated IN with 150 μg of rPA mounted a robust antibody response by 3 weeks (31.6 μg/mL) with levels dropping only slightly at 6 weeks post-immunization (20.4 μg/mL). These levels were significantly greater than those measured as compared to the negative control (p < 0.001 for both 3 and 6 weeks). The TNA results from this treatment group were also greater at 3 (127.2, p < 0.01) and 6 weeks (56.7, p < 0.01) as compared to the negative control. Serum from rabbits vaccinated IN with vaccine formulations containing capsule-conj were negative for capsule-specific antibodies (data not shown) indicating that a measurable antibody response was not mounted against the capsule antigen after a single immunization with the capsule conjugate containing formulations.
Figure 3.
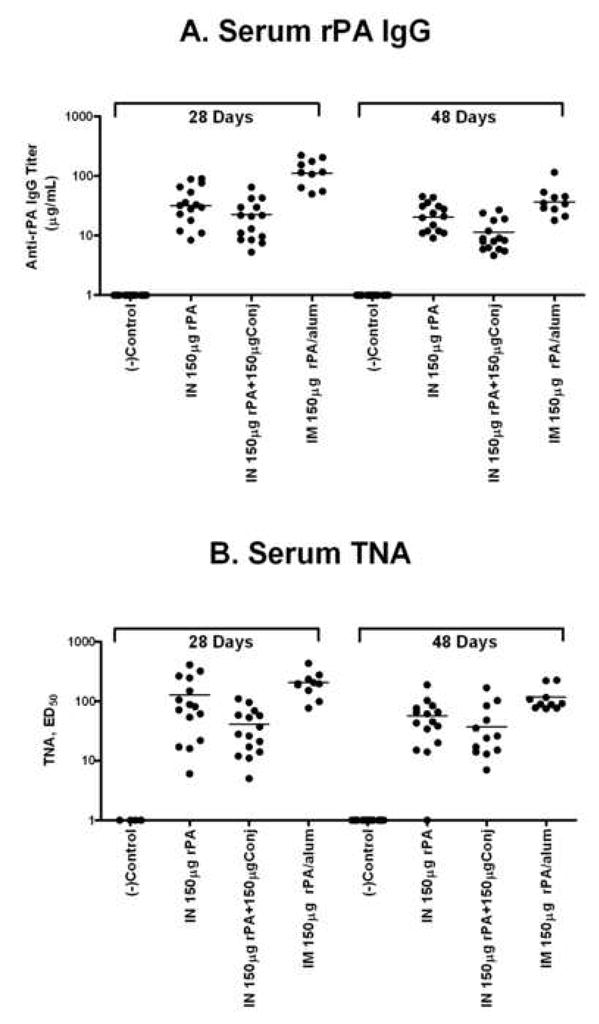
ELISA and TNA titers of rabbits vaccinated either IN with a single dose of 150 μg rPA with or without 150 μg conj, or 150 μg conj alone or IM with 75 μg rPA. Fifteen rabbits were used in each treatment group with the exception of the IM group, which only contained 10 rabbits. Serum was collected 28 and 48 days following a single vaccination and PA-specific IgG (Panel A) and TNA (Panel B) were measured. Horizontal bars indicate geometric means. Means were compared by non-parametric ANOVA.
Vaccinated rabbits were subjected to aerosol challenge with virulent Ames spores (mean challenge dose 278 LD50) 9 weeks after immunization. The results of that challenge are summarized in Table 1. As expected, all rabbits immunized with the negative control vaccine formulation succumbed to infection. However, eight of the ten animals immunized with 150 μg rPA survived the challenge (Logrank test, p < 0.0001), while only six of the ten rabbits that received the same dose of rPA with the addition of the capsule conjugate survived the 14 day post-challenge period (Logrank test, p = 0.003). Survival was not statistically different for the rPA only and rPA + conj immunized groups (p = 0.63). The rabbits vaccinated with the IM formulation were not sent to challenge because we expected approximately 100% survival based on reports in the literature [13,16]. To further examine the extent of protection afforded by vaccination, we measured anti-lethal factor (LF) IgG levels in those rabbits that survived challenge. LF is especially immunogenic in rabbits [our observations, [17] and thus we reasoned that if the challenged animals experienced an actual anthrax infection, they would mount a measurable serum response against the secreted LF. Since none of the surviving rabbits had measurable levels of anti-LF IgG in their serum two weeks prior to challenge (data not shown), LF antibodies detected in convalescent serum 14 days after challenge must have arisen as the result of an active infection. A total of four rabbits in the rPA-immunized groups had measurable anti-rLF responses following challenge (range of 39 to 700 U/mL), suggesting they suffered active infections (Fig. 4, Panel B). The anti-LF IgG titers measured for these individuals were substantially lower than what was observed in a non-immune survivor of a previous aerosol challenge experiment (5700 U/mL), [12] suggesting that the level of infection was greatly limited by the single immunizations.
Table 1.
Immunogenicity results of anthrax aerosol challenge.
| Vaccine | a LD50 | Post-Challenge Anorexia or other Clinical Signsa | Survival Rate | Pre-challenge serum Anti-rPAb | Pre-challenge serum TNA | Post-challenge serum TNA | Post-challenge IgG serumb | |||
|---|---|---|---|---|---|---|---|---|---|---|
| 3-week (μg/ml) | 6-week (μg /ml) | 3-week (ED50) | 6-week (ED50) | (ED50) | anti-PA, μg/mL | anti-LF, U/mL | ||||
| Negative Control | 259 ± 59 | Day 1 | 0/8 | 1.0 | 1.0 | 1.0 | 1.0 | - | - | - |
| IN 150μg rPA | 295 ± 50 | Day 2, normal by Day 3 | 8/10 | 31.6* | 20.4* | 127.2* | 56.7* | 983 | 1348 | 5.1 |
| IN 150μg conj. | 286 ± 85 | Day 1 | 0/10 | 1.0 | 1.2 | 1.0 | 1.0 | - | - | - |
| IN 150μg rPA + 150μg conj. | 285 ± 54 | Day 1, normal by Day 4 | 6/10 | 17.5* | 9.7 | 40.9 | 36.8 | 995 | 606 | 2.9 |
| IM150μg rPA + Alum | - | - | - | 112.7* | 42.4* | 205.3* | 116.5* | - | - | - |
Clinical signs: diarrhea, lethargy, etc.
Geometric means are reported
Indicates statistical significance compared to negative control group (maximum p < 0.05) as determined by non-parametric ANOVA
Differences were also noted between the surviving groups in post-challenge behavior as evidenced by the failure of some rabbits to eat normally during the convalescent period (data not shown). The surviving rabbits immunized with 150 μg rPA showed less weight loss on average (mean 4.3% loss) than the surviving members of the group immunized with 150 μg rPA + conj (mean 10% loss, p < 0.05). Moreover, there were fewer animals showing signs of illness (i.e., not eating, lethargy) from the group immunized with 150 μg rPA than the group immunized with 150 μg rPA + conj (data not shown).
4. Discussion
4.1 Optimization of rPA dose in a single immunization IN vaccination using a dry powder formulation
In order for a single dose vaccination to be effective, the dose of antigen must be optimized. The rPA dose range tested here for a single dose regimen was chosen based on our previous observations, [unpublished data, [12]. Anti-rPA and anti-capsule immune responses were measured in order to evaluate the effects of the different vaccine formulations. Serum antibody responses indicated that the optimum dose for a single immunization regimen was 150 μg of rPA, which is greater than what is typically used in other anthrax vaccines [11]. PA-specific immune responses can be elicited using a much lower dose of rPA [9,18–21], but more than one vaccination is required. Moreover, an additional immunization is also required for the development of measurable antibody responses against the capsule [unpublished observations, 11]. Nonetheless, the anti-rPA serum antibody levels in this study were comparable to what has been reported previously for multiple dose regimens in terms of antibody production and protective efficacy [9,18,22]. In the end, the levels of anthrax lethal toxin neutralizing antibody obtained and the substantial protection afforded by single immunization of our dry powder anthrax vaccine containing 150 μg rPA supported the use of this large antigen dose in rabbits.
The results reported here demonstrate that our dry powder anthrax vaccine elicits PA-specific immune responses following a single dose vaccination in as little as 21 days and these responses exceed those previously shown to be protective against aerosol spore challenge[13]. This rapid production of protective antibody levels suggests that a single dose of our anthrax vaccine formulation could prove to be a successful post-exposure treatment when combined with antibiotic therapy. It has been reported that although inhalation anthrax can develop in as little as 7–10 days post exposure, symptoms can take as long as 58 days to emerge [23]. This observation has led to the standard recommendation of 60 day prophylactic antimicrobial therapy following suspected exposure. Patient compliance with this type of long term therapy can be relatively poor. The full compliance rate of the Washington D.C. postal workers in 2001 was only 40%, with the remaining 60% modifying their antibiotic regimen in some way [24,25]. The addition of a single dose vaccine to the standard prophylactic therapy could stimulate the immune system to mount an effective response before antibiotic compliance wanes and while the bactericidal properties of the antibiotic keep the organism within manageable levels.
4.2 Single dose vaccines
Single dose vaccinations have successfully protected against a variety of diseases [26–28]. If protective immunity can be similarly established against pulmonary anthrax after a single dose of vaccine, then the logistical issues of an emergency or third world vaccine program would be far less complicated. For instance, there is a higher probability that a health worker in a third world country may have contact with patients for a single visit due to great travel distances to health clinics; potential vaccinees may only show for a single appointment or the time between the primary and boosting immunizations may be extended. In case of an emergency or the threat of imminent exposure to B. anthracis spores, rapid acquisition of immunity, with or without a boost may save lives. For these reasons, we sought to test the protective abilities of a single dose vaccine regimen in rabbits as a first step.
Here we demonstrated the significant findings of immune responses and protection against lethal aerosol B. anthracis spore challenge following a single dose IN vaccination with a dry powder anthrax vaccine. The key to eliciting an effective immune response in these studies appeared to be dependent on the dose of the antigen given. We tested several doses of rPA, but found the 150 μg dose resulted in the highest sustainable immune responses. Using our previous observations (unpublished results) as precedence (i.e., protection against infection is afforded with a minimum anti-rPA titer of ~20 μg/mL) it was plausible that rabbits would be protected from a lethal challenge. We then demonstrated that our vaccine formulation conferred significant protection (up to 80% survival) against aerosol spore challenge in rabbits after a single dose.
4.3 Advantages of a Dry Powder Anthrax Vaccine
In addition to the potential protective efficacy, LigoCyte’s anthrax vaccine has several probable advantages over the more traditional parenteral vaccines, primarily IN administration. This simple, non-invasive mode of administration may be particularly important in case of bioterrorist attack with anthrax spores, as the route of exposure would likely be inhalation, and development of antibodies on the respiratory mucosal surfaces might enhance the overall systemic immunity. Immunization by the IN route against a variety of pathogens has gained considerable interest in recent years [9,29–34] due to the stimulation of local mucosal immune responses, while eliminating the need for needles and the associated discomfort with their use [35–37]. IN immunization is also an effective method of eliciting systemic antigen-specific antibodies [38–40]. In a separate experiment, we performed a prime/boost IN vaccine regimen in rabbits using the same 150 μg rPA dry powder formulation and measured rPA-specific IgG (21.8μg/mL) levels at 12 months post immunization (our unpublished results), which are similar to what has been reported for prime/boost IM immunizations with rPA/alum (19.88μg/mL) [13]. Several laboratories, including our own, have demonstrated that IN immunization of animals with rPA protects against lethal aerosol spore challenge [9,12,29,41–43].
Our dry powder anthrax vaccine formulation is composed of several elements that have the potential to enhance immune responsiveness. MPL has been widely used as an adjuvant in parenteral vaccine regimens but, has also been shown to be effective when administered IN [44]. MPL is currently being evaluated in several clinical trials and has thus far shown to be safe for use in humans. Chitosan is another component of our formulation that was chosen based on its ability to enhance the efficacy of several vaccines[36,45] as well as increase the time required to clear antigen from the nasal cavity [46]. We are currently addressing the possibility of the allergen potential of chitosan.
Another important advantage of our vaccine is that it is a dry powder formulation. Dry powders may have the distinct advantage of not requiring a cold chain for transport or storage. Due to their inherent stability and ease of handling, costs of distribution and storage could be reduced. Probably the most important advantage of a dry powder IN vaccine is that it has potential for self-administration because there is nothing to mix or measure, which could minimize the need for trained medical personnel. These characteristics would be especially advantageous in third-world countries or emergency situations where access to trained personnel is limited.
4.4 The role of a capsule antigen in a single dose regimen with dry powder anthrax vaccine
The inclusion of capsule antigens in anthrax vaccines has become of great interest in recent years [14,19,47,48], and the potential role that immune responses against the capsule may play in protection are now being defined [19,49,50]. In this report, we sought to determine if immunizing with a capsule antigen would enhance the protective immune responses after only one dose. We chose BSA as a carrier for the conjugate peptide to delineate any protective responses seen due to the presence of capsule antigen alone from those resulting from immunization with rPA + conj. BSA is commonly used as a carrier protein and was chosen for this study because it has similar properties in terms of size and composition as compared to rPA. The most important factor in our decision was the fact that BSA has 60 mols of lysine per mol of protein and rPA has 58 mols of lysine per mol of protein allowing for comparable peptide-loading capacity [14]. Interestingly, the anti-rPA titers of rabbits immunized with 150 μg rPA + 150 μg conj were lower than those of the rabbits immunized with 150 μg rPA alone (p < 0.05), although TNA titers and survival were not statistically different for the two groups (p > 0.05). We are not able to explain these unexpected results at this time.
We did not detect any capsule-specific serum antibody responses resulting from a single vaccination, which is consistent with our previous observation that anti-capsule antibody responses were not observable until after a boosting immunization [12]. Similarly, immunizing rhesus macaques with rPA + conj has not been shown to elicit significant levels of capsule-specific antibodies until after a second boost (our unpublished results). These results suggest that the capsule conjugate may not be as immunogenic as rPA, and in order to establish titers against the capsule, several immunizations must be given, which is similar to other reports [19,49,50]. It is possible that immunizing with a higher dose of capsule would be sufficient to elicit capsule-specific antibodies after a single dose, but we have not formally tested this hypothesis. While it is conceivable that this particular capsule peptide may not represent conformational epitopes of the polyglutamate antigen 2 IN doses of the decamer peptide conjugated to BSA were able to protect mice against lethal challenge (our unpublished results). Clearly, immune responses are elicited to this particular capsule peptide when conjugated to a carrier protein [12,14,51], but unless given at least twice, antibody responses remain below detection. Therefore, the inclusion of the capsule peptide at the dose used here would not be expected to enhance the effectiveness of our anthrax vaccine formulation in a single dose regimen.
4.5 Post challenge immune responses
As another measure of protection against anthrax challenge, we evaluated rLF-and rPA-specific serum antibody levels at 14 days following aerosol challenge in surviving rabbits. Our rationale for measuring LF responses was that since the rabbits had not been immunized against LF, the presence of anti-LF antibodies following challenge could only result from active anthrax infection and toxin secretion. It has been our experience that the LF titers from a non-protected animal would be >5000 U/mL following infection. [12]. However, most of the surviving immunized rabbits had low levels of serum anti-rLF antibody (< 100 U/mL) post-challenge which implied that little or no toxin (LF) was secreted in those animals and that an active infection was minimal. Moreover, these animals were negative for B. anthracis cfu. We also measured significant increases in the anti-rPA titers of surviving rabbits (Table 1), which is in contrast to previously reported data that suggested there is no increase in anti-rPA or anti-rLF titers following challenge [52]. Possible contributing factors to the difference in post-challenge PA responses between the study by Hermanson and ours may be the routes of immunization (IM versus IN), the form of antigen (DNA vs. protein), and the mean spore dose (110 LD50 for Hermanson et al. versus approximately 278 LD50 for this study). These significantly different vaccine regimens may target immune cell populations that differ either phenotypically or in physical location. It has also been shown that Ames anthrax spores can have PA epitopes on their surfaces [53–55] and the reintroduction of those PA epitopes into the site of the original immunization (i.e., the nasal tract at the time of aerosol challenge) may act as an antigen boost even if the spores do not go on to establish an active infection.
4.6 Immune correlates
The search for immune correlates of protection (defined as protection from death) has focused on anti-PA antibodies in animals parenterally immunized with rPA-based vaccines. In these cases, serum levels of lethal toxin neutralizing antibody [56,57] and total serum anti-rPA IgG [11,56] correlated with protection against challenge with virulent spores. However, these studies are not necessarily in agreement as to the level of antibody required to protect animals against anthrax challenge. Correlations have proven informative within studies, but no consensus requirement for minimum levels of anti-rPA serum or toxin neutralizing antibody has emerged, even within a single species such as the rabbit. For instance, one report suggested good correlation between both total serum PA-specific antibody and toxin neutralizing antibody when animals were immunized twice with AVA [56]. Mean serum levels of anti-rPA IgG of ≥ 122 μg/mL two weeks before challenge were required to see greater than 70% survival. In contrast, another report suggested that anti-PA serum levels as low as 16 μg/mL protected 66% of rabbits immunized with rPA against lethal challenge [11]. The differences in results of these two studies do not appear to be attributable to inhaled spore dose, and both authors utilized Ames strain spores, but each study used very different antigens (AVA versus rPA). Our study used the same type of antigen and a similar immunization schedule as described in Little et al. and, therefore, it is not surprising that our results are similar. As Little et al. found, our studies suggest that an anti-rPA titer as low as 20 μg/mL can offer some degree of protection against lethal challenge.
4.7 Conclusions
The results presented in this study demonstrate that our dry powder anthrax vaccine formulation, an IN dry powder vaccine formulated with rPA, MPL and the mucoadhesive chitosan, significantly protected rabbits against lethal challenge nine weeks after a single immunization. Single dose immunization with our dry powder anthrax vaccine formulation could prove to be particularly advantageous in an emergency situation where there is limited time to protect citizens against an anthrax infection where vaccine storage, distribution and administration resources are strained.
Acknowledgments
This work is supported by the U.S. Army Medical Research and Material Command under Contract No. DAMD17-01-C-0040. The views, opinions and/or findings contained in this report are those of the author(s) and should not be construed as an official Department of the Army position, policy or decision unless so designated by other documentation. In conducting research using animals, the investigator(s) adhered to the “Guide for the Care and Use of Laboratory Animals,” prepared by the Committee on Care and Use of Laboratory Animals of the Institute of Laboratory Animal Resources, National Research Council (NIH Publication No. 86-23, Revised 1985).
This publication was made possible by NIH grant number 1 VC1 AI067156-02 from the National Institute of Allergy and Infectious Diseases. Its contents are solely the responsibility of the authors and do not represent the official views of NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
ChiSys® is a trade mark of Archimedes Development Ltd and is registered as a CTM, and as a US Registered Trademark and in certain other jurisdictions.
Reference List
- 1.Pile JC, Malone JD, Eitzen EM, Friedlander AM. Anthrax as a potential biological warfare agent. Arch Intern Med. 1998 Mar 9;158(5):429–34. doi: 10.1001/archinte.158.5.429. [DOI] [PubMed] [Google Scholar]
- 2.Dixon TC, Meselson M, Guillemin J, Hanna PC. Anthrax. N Engl J Med. 1999;341(11):815–26. doi: 10.1056/NEJM199909093411107. [DOI] [PubMed] [Google Scholar]
- 3.Demicheli V, Rivetti D, Deeks JJ, Jefferson T, Pratt M. The effectiveness and safety of vaccines against human anthrax: a systematic review. Vaccine. 1998;16(9–10):880–4. doi: 10.1016/s0264-410x(98)00023-1. [DOI] [PubMed] [Google Scholar]
- 4.Friedlander AM. Clinical aspects, diagnosis and treatment of anthrax. J Appl Microbiol. 1999;87(2):303. doi: 10.1046/j.1365-2672.1999.00896.x. [DOI] [PubMed] [Google Scholar]
- 5.Hambleton P, Carman JA, Melling J. Anthrax: the disease in relation to vaccines. Vaccine. 1984;2(2):125–32. doi: 10.1016/0264-410x(84)90003-3. [DOI] [PubMed] [Google Scholar]
- 6.Jernigan JA, Stephens DS, Ashford DA, Omenaca C, Topiel MS, Galbraith M, et al. Bioterrorism-related inhalational anthrax: the first 10 cases reported in the United States. Emerg Infect Dis. 2001;7(6):933–44. doi: 10.3201/eid0706.010604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine. Is It safe? Does It Work? Washington, D.C: National Academy Press; 2002. The Anthrax Vaccine. [Google Scholar]
- 8.van der Lubben IM, Verhoef JC, Borchard G, Junginger HE. Chitosan for mucosal vaccination. Adv Drug Deliv Rev. 2001;52(2):139–44. doi: 10.1016/s0169-409x(01)00197-1. [DOI] [PubMed] [Google Scholar]
- 9.Huang J, Mikszta JA, Ferriter MS, Jiang G, Harvey NG, Dyas B, et al. Intranasal administration of dry powder anthrax vaccine provides protection against lethal aerosol spore challenge. Hum Vaccin. 2007;3(3):64–7. doi: 10.4161/hv.3.3.4011. [DOI] [PubMed] [Google Scholar]
- 10.Jiang G, Joshi SB, Peek LJ, Brandau DT, Huang J, Ferriter MS, et al. Anthrax vaccine powder formulations for nasal mucosal delivery. Journal of Pharmaceutical Science. 2006;95(1):80–96. doi: 10.1002/jps.20484. [DOI] [PubMed] [Google Scholar]
- 11.Little SF, Ivins BE, Fellows PF, Pitt ML, Norris SL, Andrews GP. Defining a serological correlate of protection in rabbits for a recombinant anthrax vaccine. Vaccine. 2004;22(3–4):422–30. doi: 10.1016/j.vaccine.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Wimer-Mackin S, Hinchcliffe M, Petrie CR, Warwood SJ, Tino WT, Williams MS, et al. An intranasal vaccine targeting both the Bacillus anthracis toxin and bacterium provides protection against aerosol spore challenge in rabbits. Vaccine. 2006;24(18):3953–63. doi: 10.1016/j.vaccine.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 13.Little SF, Ivins BE, Webster WM, Fellows PF, Pitt ML, Norris SL, et al. Duration of protection of rabbits after vaccination with Bacillus anthracis recombinant protective antigen vaccine. Vaccine. 2006 Mar 24;24(14):2530–6. doi: 10.1016/j.vaccine.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 14.Schneerson R, Kubler-Kielb J, Liu TY, Dai ZD, Leppla SH, Yergey A, et al. Poly(gamma-D-glutamic acid) protein conjugates induce IgG antibodies in mice to the capsule of Bacillus anthracis: a potential addition to the anthrax vaccine. Proc Natl Acad Sci U S A. 2003;100(15):8945–50. doi: 10.1073/pnas.1633512100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zaucha GM, Pitt LM, Estep J, Ivins BE, Friedlander AM. The pathology of experimental anthrax in rabbits exposed by inhalation and subcutaneous inoculation. Arch Pathol Lab Med. 1998;122(11):982–92. [PubMed] [Google Scholar]
- 16.Little SF, Ivins BE, Webster WM, Norris SL, Andrews GP. Effect of aluminum hydroxide adjuvant and formaldehyde in the formulation of rPA anthrax vaccine. Vaccine. 2007 Apr 12;25(15):2771–7. doi: 10.1016/j.vaccine.2006.12.043. [DOI] [PubMed] [Google Scholar]
- 17.Price BM, Liner AL, Park S, Leppla SH, Mateczun A, Galloway DR. Protection against anthrax lethal toxin challenge by genetic immunization with a plasmid encoding the lethal factor protein. Infect Immun. 2001;69(7):4509–15. doi: 10.1128/IAI.69.7.4509-4515.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boyaka PN, Tafaro A, Fischer R, Leppla SH, Fujihashi K, McGhee JR. Effective mucosal immunity to anthrax: neutralizing antibodies and Th cell responses following nasal immunization with protective antigen. J Immunol. 2003;170(11):5636–43. doi: 10.4049/jimmunol.170.11.5636. [DOI] [PubMed] [Google Scholar]
- 19.Rhie GE, Roehrl MH, Mourez M, Collier RJ, Mekalanos JJ, Wang JY. A dually active anthrax vaccine that confers protection against both bacilli and toxins. Proc Natl Acad Sci U S A. 2003;100(19):10925–30. doi: 10.1073/pnas.1834478100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sloat BR, Cui Z. Evaluation of the immune response induced by a nasal anthrax vaccine based on the protective antigen protein in anaesthetized and non-anaesthetized mice. J Pharm Pharmacol. 2006;58(4):439–47. doi: 10.1211/jpp.58.4.0003. [DOI] [PubMed] [Google Scholar]
- 21.Sloat BR, Cui Z. Strong mucosal and systemic immunities induced by nasal immunization with anthrax protective antigen protein incorporated in liposome-protamine-DNA particles. Pharm Res. 2006;23(2):262–9. doi: 10.1007/s11095-005-9078-7. [DOI] [PubMed] [Google Scholar]
- 22.Kobiler D, Gozes Y, Rosenberg H, Marcus D, Reuveny S, Altboum Z. Efficiency of protection of guinea pigs against infection with Bacillus anthracis spores by passive immunization. Infect Immun. 2002;70(2):544–60. doi: 10.1128/IAI.70.2.544-550.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meselson M, Guillemin J, Hugh-Jones M, Langmuir A, Popova I, Shelokov A, et al. The Sverdlovsk anthrax outbreak of 1979. Science. 1994;266(5188):1202–8. doi: 10.1126/science.7973702. [DOI] [PubMed] [Google Scholar]
- 24.Jefferds MD, Laserson K, Fry AM, Roy S, Hayslett J, Grummer-Strawn L, et al. Adherence to antimicrobial inhalation anthrax prophylaxis among postal workers, Washington D.C. 2001. Emerg Infect Dis. 2002;8(10):1138–44. doi: 10.3201/eid0810.020331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shepard CW, Soriano-Gabarro M, Zell ER, Hayslett J, Lukacs S, Goldstein S, et al. Antimicrobial postexposure prophylaxis for anthrax: adverse events and adherence. Emerg Infect Dis. 2002;8(10):1124–32. doi: 10.3201/eid0810.020349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dastur FD, Awatramani VP, Chitre SK, D’Sa JA. A single dose vaccine to prevent neonatal tetnus. Journal of Associated Physicians of India. 1993;41(2):97–9. [PubMed] [Google Scholar]
- 27.Miecarek N, Debrie A, Raze D, Bertout J, Rouanet C, Younes A, et al. Live attenuated B. pertussis as a single-dose nasal vaccine against Whooping cough. PLos Pathogens. 2006;2(7):e65. doi: 10.1371/journal.ppat.0020065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schlereth B, Rose JK, Buonocore L, ter Meulen V, Niewiesk S. Successful vaccine-induced seroconversion by single-dose immunization in the presence of measles virus-specific maternal antibodies. J Virol. 2000;74(10):4652–7. doi: 10.1128/jvi.74.10.4652-4657.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang J, Garmise RJ, Crowder TM, Mar K, Hwang CR, Hickey AJ, et al. A novel dry powder influenza vaccine and intranasal delivery technology: induction of systemic and mucosal immune responses in rats. Vaccine. 2004;23(6):794–801. doi: 10.1016/j.vaccine.2004.06.049. [DOI] [PubMed] [Google Scholar]
- 30.LiCalsi C, Christensen T, Bennett JV, Phillips E, Witham C. Dry powder inhalation as a potential delivery method for vaccines. Vaccine. 1999;17(13–14):1796–803. doi: 10.1016/s0264-410x(98)00438-1. [DOI] [PubMed] [Google Scholar]
- 31.Mestecky J, Michalek SM, Moldoveanu Z, Russell MW. Routes of immunization and antigen delivery systems for optimal mucosal immune responses in humans. Behring Inst Mitt. 1997;(98):33–43. [PubMed] [Google Scholar]
- 32.Sullivan VJ, Mikszta JA, Laurent P, Huang J, Ford B. Noninvasive delivery technologies: respiratory delivery of vaccines. Expert Opin Drug Deliv. 2006;3(1):87–95. doi: 10.1517/17425247.3.1.87. [DOI] [PubMed] [Google Scholar]
- 33.Vajdy M, Singh M. Intranasal delivery of vaccines against HIV. Expert Opin Drug Deliv. 2006;3(2):247–59. doi: 10.1517/17425247.3.2.247. [DOI] [PubMed] [Google Scholar]
- 34.Wu HY, Nahm MH, Guo Y, Russell MW, Briles DE. Intranasal immunization of mice with PspA (pneumococcal surface protein A) can prevent intranasal carriage, pulmonary infection, and sepsis with Streptococcus pneumoniae. J Infect Dis. 1997;175(4):839–46. doi: 10.1086/513980. [DOI] [PubMed] [Google Scholar]
- 35.Li F, Michalek SM, Dasanayake AP, Li Y, Kirk K, Childers NK. Intranasal immunization of humans with Streptococcus mutans antigens. Oral Microbiol Immunol. 2003;18(5):271–7. doi: 10.1034/j.1399-302x.2003.00067.x. [DOI] [PubMed] [Google Scholar]
- 36.McNeela EA, Jabbal-Gill I, Illum L, Pizza M, Rappuoli R, Podda A, et al. Intranasal immunization with genetically detoxified diphtheria toxin induces T cell responses in humans: enhancement of Th2 responses and toxin-neutralizing antibodies by formulation with chitosan. Vaccine. 2004;22(8):909–14. doi: 10.1016/j.vaccine.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 37.Muszkat M, Greenbaum E, Ben-Yehuda A, Oster M, Yeu’l E, Heimann S, et al. Local and systemic immune response in nursing-home elderly following intranasal or intramuscular immunization with inactivated influenza vaccine. Vaccine. 2003;21(11–12):1180–6. doi: 10.1016/s0264-410x(02)00481-4. [DOI] [PubMed] [Google Scholar]
- 38.Bielinska AU, Janczak KW, Landers JJ, Makidon P, Sower LE, Peterson JW, et al. Mucosal immunization with a novel nanoemulsion-based recombinant anthrax protective antigen vaccine protects against Bacillus anthracis spore challenge. Infect Immun. 2007 Aug;75(8):4020–9. doi: 10.1128/IAI.00070-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu WT, Hsu HL, Liang CC, Chuang CC, Lin HC, Liu YT. A comparison of immunogenicity and protective immunity against experimental plague by intranasal and/or combined with oral immunization of mice with attenuated Salmonella serovar Typhimurium expressing ssecreted Yersinia pestis F1 and V antigen. FEMS Immunol Med Microbiol. 2007 Oct;51(1):58–69. doi: 10.1111/j.1574-695X.2007.00280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Youn HJ, Ko SY, Lee KA, Ko HJ, Lee YS, Fujihashi K, et al. A single intranasal immunization with inactivated influenza virus and alpha-galactosylceramide induces long-term protective immunity without redirecting antigen to the central nervous system. Vaccine. 2007 Jul;25(28):5189–98. doi: 10.1016/j.vaccine.2007.04.081. [DOI] [PubMed] [Google Scholar]
- 41.Flick-Smith HC, Eyles JE, Hebdon R, Waters EL, Beedham RJ, Stagg TJ, et al. Mucosal or parenteral administration of microsphere-associated Bacillus anthracis protective antigen protects against anthrax infection in mice. Infect Immun. 2002;70(4):2022–8. doi: 10.1128/IAI.70.4.2022-2028.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Flick-Smith HC, Walker NJ, Gibson P, Bullifent H, Hayward S, Miller J, et al. A recombinant carboxy-terminal domain of the protective antigen of Bacillus anthracis protects mice against anthrax infection. Infect Immun. 2002;70(3):1653–6. doi: 10.1128/IAI.70.3.1653-1656.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mikszta JA, Sullivan VJ, Dean C, Waterston AM, Alarcon JB, Dekker JP, III, et al. Protective immunization against inhalational anthrax: a comparison of minimally invasive delivery platforms. J Infect Dis. 2005;191(2):278–88. doi: 10.1086/426865. [DOI] [PubMed] [Google Scholar]
- 44.Baldridge JR, Yorgensen Y, Ward JR, Ulrich JT. Monophosphoryl lipid A enhances mucosal and systemic immunity to vaccine antigens following intranasal administration. Vaccine. 2000;18(22):2416–25. doi: 10.1016/s0264-410x(99)00572-1. [DOI] [PubMed] [Google Scholar]
- 45.Huo Z, Sinha R, McNeela EA, Borrow R, Giemza R, Cosgrove C, et al. Induction of protective serum meningococcal bactericidal and diptheria-neutralizing antibodies and mucosal immunoglobulin A in volunteers by nasal insufflations of the Neisseria meningitidis serogroup C polysaccharide-CRM197 conjugate vaccine mixed with chitosan. Infection and Immunity. 2005 Dec;73(12):8256–65. doi: 10.1128/IAI.73.12.8256-8265.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Illum L, Jabbal-Gill I, Hinchcliffe M, Fisher AN, Davis SS. Chitosan as a novel nasal delivery system for vaccines. Adv Drug Deliv Rev. 2001;51(1–3):81–96. doi: 10.1016/s0169-409x(01)00171-5. [DOI] [PubMed] [Google Scholar]
- 47.Chabot DJ, Scorpio A, Tobery SA, Little SF, Norris SL, Friedlander AM. Anthrax capsule vaccine protects against experimental infection. Vaccine. 2004;23(1):43–7. doi: 10.1016/j.vaccine.2004.05.029. [DOI] [PubMed] [Google Scholar]
- 48.Wang JY, Roehrl MH. Anthrax vaccine design: strategies to achieve comprehensive protection against spore, bacillus, and toxin. Med Immunol. 2005;4(1):4. doi: 10.1186/1476-9433-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sloat BR, Cui Z. Nasal immunization with anthrax protective antigen protein adjuvanted with polyriboinosinic-polyribocytidylic acid induced strong mucosal and systemic immunities. Pharm Res. 2006;23(6):1217–26. doi: 10.1007/s11095-006-0206-9. [DOI] [PubMed] [Google Scholar]
- 50.Wang TT, Fellows PF, Leighton TJ, Lucas AH. Induction of opsonic antibodies to the gamma-D-glutamic acid capsule of Bacillus anthracis by immunization with a synthetic peptide-carrier protein conjugate. FEMS Immunol Med Microbiol. 2004;40(3):231–7. doi: 10.1016/S0928-8244(03)00366-3. [DOI] [PubMed] [Google Scholar]
- 51.Kubler-Kielb J, Liu TY, Mocca C, Majadly F, Robbins JB, Schneerson R. Additional conjugation methods and immunogenicity of Bacillus anthracis poly-G-D-glutamic acid-protein conjugates. Infection and Immunity. 2006 Aug;74(8):4744–9. doi: 10.1128/IAI.00315-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hermanson G, Whitlow V, Parker S, Tonsky K, Rusalov D, Ferrari M, et al. A cationic lipid-formulated plasmid DNA vaccine confers sustained antibody-mediated protection against aerosolized anthrax spores. Proc Natl Acad Sci U S A. 2004;101(37):13601–6. doi: 10.1073/pnas.0405557101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cote CK, Rossi CA, Kang AS, Morrow PR, Lee JS, Welkos SL. The detection of protective antigen (PA) associated with spores of Bacillus anthracis and the effects of anti-PA antibodies in spore germination and macrophage interactions. Microb Pathog. 2005 Apr;38:209–25. doi: 10.1016/j.micpath.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 54.Welkos S, Little S, Friedlander A, Fritz D, Fellows P. The role of antibodies to Bacillus anthracis and anthrax toxin components in inhibiting the early stages of infection by anthrax spores. Microbiology. 2001;147(Pt 6):1677–85. doi: 10.1099/00221287-147-6-1677. [DOI] [PubMed] [Google Scholar]
- 55.Welkos S, Friedlander A, Weeks S, Little S, Mendelson I. In-vitro characterization of the phagocytosis and fate of anthrax spores in macrophages and the effects of anti-PA antibody. J Med Microbiol. 2002;51(10):821–31. doi: 10.1099/0022-1317-51-10-821. [DOI] [PubMed] [Google Scholar]
- 56.Pitt ML, Little SF, Ivins BE, Fellows P, Barth J, Hewetson J, et al. In vitro correlate of immunity in a rabbit model of inhalational anthrax. Vaccine. 2001;19(32):4768–73. doi: 10.1016/s0264-410x(01)00234-1. [DOI] [PubMed] [Google Scholar]
- 57.Reuveny S, White MD, Adar YY, Kafri Y, Altboum Z, Gozes Y, et al. Search for correlates of protective immunity conferred by anthrax vaccine. Infection and Immunity. 2001;69(5):2888–93. doi: 10.1128/IAI.69.5.2888-2893.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]


