Abstract
National attention to the effects of interpersonal trauma has led mental health systems to adopt policies on trauma-related services; however, there is a lack of clarity regarding targeting of these services. Data from the Women, Co-occurring Disorders and Violence Study (WCDVS) were reanalyzed by grouping women on their baseline PTSD and substance abuse presentation and assessing the differential response to an integrated mental health/substance abuse intervention. Treatment effects were largest for subgroups characterized by high levels of PTSD, whereas the effects for those in the low symptom group were near zero. These findings underscore the need for clinicians to conduct careful assessments of trauma-related symptoms and to target the most intensive trauma-related interventions to individuals with PTSD symptoms.
Keywords: PTSD, Interventions, Substance abuse
Interpersonal trauma such as physical or sexual abuse is a serious and common public health issue, as highlighted in the U.S. Surgeon General’s report on mental health (United States Department of Health and Human Services [DHHS] 1999). Indeed, epidemiological studies indicate that 38–59% of the U.S. population has experienced some form of interpersonal trauma (Breslau et al. 1998; Kessler et al. 1995; Tjaden and Thoennes 2000). Among women with serious mental illness (SMI) seeking services, lifetime rates of exposure to interpersonal violence are much higher, with estimates ranging between 43% and 97% (Carmen et al. 1984; Cascardi et al. 1996; Goodman et al. 1995). Data also suggest that women are at greater risk than men for more serious and/or chronic forms of victimization (e.g., sexual assault, domestic violence) (Pimlott-Kubiak and Cortina 2003).
A wealth of research demonstrates the pervasive negative consequences of interpersonal trauma (Kessler et al. 1995; Breslau et al. 2000; Kilpatrick et al. 1998). These outcomes include posttraumatic stress disorder (PTSD), substance abuse, somatic complaints, and general psychological distress. Among women with SMI, sexual and physical abuse are related to more severe symptoms of mental illness such as psychotic symptoms, depression, suicidality, anxiety and dissociation (Carmen et al. 1984; Beck and van der Kolk 1987; Briere et al. 1997; Craine et al. 1988; Muenzenmaier et al. 1993; Surrey et al. 1990). Studies have also found the experience of trauma to be related to greater use of high cost, acute care services (Carmen et al. 1984; Briere et al. 1997; Elhai et al. 2005).
Following depression, substance abuse is the second most common disorder co-occurring with PTSD for women (Kessler et al. 1995; Jacobsen et al. 2001). A number of causal explanations exist which posit a central role for PTSD in the relationship between trauma and substance abuse (Chilcoat and Breslau 1998; Mueser et al. 2002). Studies indicate that the comorbidity of substance abuse with PTSD is associated with more severe PTSD symptoms, significantly higher rates of other comorbid Axis I and II disorders, psychosocial and medical problems, inpatient hospital admissions, and relapse compared to substance abuse patients without comorbid PTSD (Jacobsen et al. 2001).
Expert opinion combined with research over the past 10 years (including emerging research on the simultaneous treatment of PTSD and substance abuse) indicates that treatment outcomes are best when mental health and substance abuse disorders are treated simultaneously (Brady et al. 2004; Drake and Mueser 2001; Najavits et al. 1997). However, services for people with mental illness and substance abuse are often fragmented, and these individuals often end up being bounced back and forth between service systems (Mueser et al. 2003). Furthermore, few individuals receive appropriate PTSD related services, as trauma history tends not to be assessed and PTSD is often overlooked as a result (Cusack et al. 2006; Mueser et al. 1998). In recent years, greater national attention to this issue, including position statements from the National Association of State Mental Health Program Directors (NASMHPD) and the National Association of Consumer/Survivor Mental Health Administrators (NAC/SMA), has led to increased efforts to incorporate trauma services into all aspects of mental health and substance abuse services, including the formation of statewide Trauma Initiatives (e.g., Maine, Connecticut, South Carolina) (Frueh et al. 2001) and national-level groups focused on raising awareness about the prevalence of trauma and promoting effective, integrated, trauma-informed, and trauma-specific services (e.g., the National Trauma Consortium; http://www.nationaltraumaconsortium.org).
Despite these efforts, clear guidelines regarding the appropriate targeting of trauma-related interventions do not exist. While most trauma experts emphasize PTSD symptoms as the appropriate target (Foa et al. 2000), others have argued for a much broader view of trauma sequelae, and consequently, a much wider range of symptoms targeted for trauma-related intervention. (Fallot and Harris 2002). As a result, state mental health systems use widely varying definitions of target populations for trauma-related services, ranging from individuals with a history of abuse to those presenting with PTSD (Jennings 2004).
The question of how to target trauma-related services can be assessed empirically by an intervention study with a large, regionally diverse sample of individuals with trauma histories. The Women, Co-occurring Disorders and Violence Study (WCDVS) provides the best available data in these regards. WCDVS was a federally-funded, multi-site quasi-experimental evaluation of integrated services for women with co-occurring mental illness and substance abuse who were victims of trauma. The study was conducted from 1998 to 2003 across nine sites in the United States. This study was the largest to date (N = 2,729) to evaluate services for women with complex presentations of trauma history, mental health and substance abuse needs (for full description see McHugo et al. 2005b; Morrissey et al. 2005a).
The primary analysis of 6-month and 12-month outcomes of the WCDVS revealed small yet positive overall effects of the intervention relative to a comparison treatment-as-usual on general mental health, PTSD symptoms, and substance abuse severity at 6 months (Morrissey et al. 2005a, b; Cocozza et al. 2005). However, the inclusion criteria of the WCDVS stipulated only that the women have a history of interpersonal trauma and comorbid mental health and substance abuse disorders of any type. As a consequence, sites had some leeway in who was enrolled and the resultant sample of 2,729 women represented a wide range of lifetime traumatic experiences, PTSD severity, and substance abuse problems (Becker et al. 2005).
The main analyses of WCDVS outcomes employed an experimental logic and focused on average effects for the overall sample that was followed-up at 6 and 12 months. In contrast, the present study disaggregates the sample and asks whether outcomes varied for several empirically-derived subgroups of women who had different symptom presentations prior to study enrollment. Consistent with the existing trauma literature, we expected considerable variation in the type and degree of trauma-related comorbidity in this sample. Further, we expected that these subgroups of women would have distinct profiles across mental and physical health indicators.
Specifically, we expected subgroups with higher levels of PTSD symptom severity at baseline would have higher rates of both child and adult abuse and would report a greater lifetime frequency of traumatic events. We also expected that subgroups with high levels of PTSD severity at baseline would demonstrate worse mental health functioning in additional areas (e.g., psychosis, paranoia, general mental health), earlier onset of mental health problems, and worse physical health. Finally, we expected women with active high levels of PTSD to have a greater treatment response to the integrated intervention on measures of PTSD, general mental health, and substance abuse (when indicated) than women with other symptom characteristics.
Methods
Study Design Overview
The WCDVS sought to determine whether integrated trauma care would lead to better outcomes for women than receiving usual care in the form of separate and uncoordinated mental health and substance abuse services. The study set out to recruit a population of women who were difficult to treat and who were high utilizers of services (McHugo et al. 2005b). The criteria specified that participants be age 18 or older, have a chart-documented DSM-IV Axis I or II psychiatric disorder and a DSM-IV substance use disorder (at least one of which was symptomatic in the past 30 days and the other in the past 5 years), have a history of physical and/or sexual abuse, have two or more previous service episodes, and speak English or Spanish as their primary language.
Trained interviewers administered the cross-site protocol to each participant. The protocol assessed demographic characteristics, traumatic life events, mental health symptoms, and substance use. Each intervention site provided services that were comprehensive, used one of several trauma-specific intervention models in a group format (TREM, Seeking Safety, Atrium, TRIAD; more details of the sites and interventions can be found in McHugo et al. 2005b), integrated mental health and substance abuse services, and involved consumers in advisory and service provision roles. In the absence of evidence that any one comprehensive, integrated, trauma/substance abuse intervention was more effective, sites were encouraged to be creative in adapting existing service models to their site. Each model was relatively brief, ranging from 12 to 33 sessions. Women recruited into the control condition received treatment-as-usual at a local service setting comparable to the intervention site but without integrated trauma care.
Participants
The women were enrolled in the study through local projects in California (two sites), Colorado, Florida, Massachusetts (three sites), New York City, and Washington, DC. The average age was 36 years (range 18–76). The women were from diverse racial and ethnic backgrounds (17% Hispanic, 50% White non-Hispanic, 25% Black non-Hispanic, 7% other non-Hispanic). The median number of years of education was 12. About a third (38%) of the sample was married or partnered (28% never married). Most (70%) had experienced homelessness and half (51%) reported a current serious physical illness or disability. As a group, the women reported long-term mental health, substance use, and trauma experiences as indicated by first mental health problem by age 12 (50%), regular use of alcohol to intoxication for at least 5 years (50%), regular use of drugs for at least 10 years (50%), and childhood sexual or physical abuse (79%).
Measures
Measures of PTSD symptoms and drug and alcohol use severity prior to study enrollment were used to cluster the participants into subgroups. Drug use and alcohol use problem severity were assessed using the Addiction Severity Index (ASI) (McLellan et al. 1980). The Drug Composite Score (ASI-D) and Alcohol Composite Score (ASI-A) measure problem severity during the prior 30 days. Possible scores range from 0 to 1, with higher scores indicating greater substance use problem severity. The ASI-A score was modified slightly in consultation with its author, but was scored on the original scale (for details, see McHugo et al. 2005b). At baseline, average scores for the total sample were .20 on the ASI-D and .16 on the ASI-A, indicating a moderate level of severity. Among women reporting any use, the mean scores were .23 and .38 respectively.
PTSD symptoms were assessed by the PTSD Symptom Scale (PSS) of the Post-traumatic Stress Diagnostic Scale (Foa et al. 1993). This 17-item scale asks respondents to indicate how often in the past month (on a scale of 0 [not at all or only once] to 3 [5 or more times or almost always]) they experienced a list of problems sometimes experienced after a traumatic event. Possible scores range from 0 to 51, with higher scores indicating more severe PTSD symptoms. The PSS has high internal consistency and test–retest reliability and is highly correlated with structured diagnostic interviews (Foa et al.). At baseline the average score for the total sample was 23.7, indicating a moderate-to-severe level of symptom severity. For women who reported any PTSD symptoms, the average score was 24.3.
In addition, the subgroups of women at baseline were profiled with three additional sets of variables—demographic characteristics, trauma history, and mental health symptoms—in order to test hypotheses related to the subgroups. Demographic variables were recorded at baseline including age, race, education, employment, and homeless status.
Traumatic Events History was assessed with a version of the LSC-R (Wolfe and Kimerling 1997) that was modified for the WCDVS (McHugo et al. 2005a). The LSC-R is a 30-item instrument that uses behaviorally specific language and includes probes to assess age at the time of the first event and chronicity. The LSC-R has demonstrated good criterion-related validity for PTSD in diverse populations of women and in several languages. Based on the recommendations of the multidisciplinary WCDVS workgroup, the LSC-R was modified to be more gender specific and culturally sensitive and to use greater caution in the wording of questions related to abuse. The modified version of the LSC-R was found to have good test–retest reliability (McHugo et al. 2005a).
Mental health symptoms were assessed using the Brief Symptom Inventory (BSI) (Derogatis 1993). The BSI is a 53-item self-report scale that measures nine symptom dimensions including somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoia, and psychoticism, and also includes a global severity index (GSI) based on all nine symptom dimensions. Internal consistency and test–retest reliability range from moderate to high for the various subscales. Respondents were asked how much a problem distressed them in the past 7 days (ranging from 0 to 4, “not at all” to “extremely”). Possible scores range from 0 to 4, with higher scores indicating more severe symptomatology. At baseline, the average GSI raw score was 1.35 (T-score = 69) indicating a moderately elevated level of symptom severity.
Finally, the effects of the intervention were examined for PTSD symptoms (PSS), Substance abuse (ASI-A, ASID), and global mental health problems (GSI).
Statistical Analyses
Analyses were performed in SPSS version 15.0 and in R version 1.9.1 (R Development Core Team 2004). First, participants were grouped into empirically-derived clusters based on self-reported symptoms on the PSS, ASI-alcohol, and ASI-drug measures. Baseline scores on the three measures were standardized and then submitted to k-means cluster analysis (Hartigan 1975). The k-means approach was selected due to its ability to handle large samples and because it is preferred in situations like the current study when the number of clusters in the data can be inferred a priori from theory and extant literature (Hair et al. 1998). The technique uses an algorithm to partition individual cases into a pre-specified number (k) of clusters, based on their scores on the three measures, in a manner that maximizes between-cluster differences and minimizes within-cluster variance. The cluster centers are iteratively updated until the optimal groupings are achieved based on Euclidean distance. Based on expected profile combinations of the presence or absence of PTSD, along with possible comorbid drug, alcohol, or neither we requested six-, seven-, and eight-cluster solutions. The six-cluster solution was retained based on overall fit of the data. We evaluated the validity of the resulting solution in two ways. First, we examined the robustness of the solution by splitting the sample into two random halves, conducted the cluster analysis on the first random half of the sample and replicated it with the second half, and then compared the two solutions. We also examined whether the clusters differed on external measures that were not part of the clustering but which were expected to differ among clusters.
Second, a propensity scoring approach was used to reduce the biases inherent in nonrandom assignment of participants to intervention and comparison conditions in the WCDVS (Rosenbaum and Rubin 1984). The propensity score reduces the pretreatment differences between the groups to a single score that appropriately summarizes those differences. Weighting the outcomes by propensity score statistically balances the two groups with respect to observed covariates.
Propensity scores are often estimated using logistic regression. McCaffrey et al. (2004) compared two logistic regression methods of propensity score estimation to generalized boosted modeling (GBM), an iterative algorithm that uses regression trees to develop increasingly accurate estimates of the log-odds of assignment to treatment. They found that relative to the logistic regression methods, GBM reduced prediction error, improved the balance between groups on the means of the covariates, and resulted in estimated average treatment effects with substantially smaller standard errors. Therefore, in the current analysis, propensity scores were calculated using the GBM package developed by McCaffrey et al., along with R software, version 1.9.1 (R Development Core Team 2004). The propensity score included 33 covariates in the following domains: demographic characteristics, traumatic events history, ratings of physical and mental health, and previous mental health and substance abuse treatment.
We assessed the success of the propensity scoring procedure in balancing the intervention and comparison groups with respect to baseline covariates by comparing results of unweighted intervention-versus-comparison t-tests on covariates and compared these to propensity score weighted t-tests. Results indicated that the procedure was successful in balancing the intervention and comparison groups on all selected baseline covariates. The unweighted tests on covariates found that nine of the 33 variables were significantly different between conditions. The propensity score weighted tests indicated that only two of these variables were significantly different between conditions. Balance was also checked within each cluster, where 17% of the unweighted tests were significant, and 6% of weighted tests were significant (close to what would be expected by chance alone).
We also compared effect sizes of covariate differences before and after propensity score weighting as an additional check for balance between the conditions. The average effect size of the unweighted tests was .06. Following weighting, the average effect size was .01, indicating that the propensity score reduced the magnitude of difference between conditions. Effect size analyses were also repeated within each cluster, with the same pattern of decreased effect sizes after propensity score adjustment. (Details of these analyses are available from the first author.)
Finally, propensity score weighted t-tests were used to examine the effects of the intervention on the primary and secondary measures (PSS, ASI-D, ASI-A, and GSI) for each of the six clusters. The dependent variable was change score from baseline to 12-months for all weighted t-tests.
Results
Description of Empirically Derived Clusters
Figure 1 profiles the six groups based on mean z-scores computed for the sample as a whole on PTSD symptoms and alcohol and drug use severity. Participants in Group 1: Low Symptoms (n = 817) reported the lowest level of symptoms across PTSD, alcohol and drug use severity. Group 2: Polysubstance Users (n = 162) contains participants who reported problems primarily with drug and alcohol use. Group 3: PTSD/Alcohol (n = 272) is characterized by high levels of PTSD symptoms and alcohol use problems. Group 4: PTSD/Drug (n = 488) is characterized by high levels of PTSD symptoms and drug use problems. Group 5: Severe Comorbid (n = 214) is characterized by high levels of all three PTSD, alcohol, and drug problems. Group 6: PTSD (n = 672) is characterized primarily by high levels of PTSD symptoms.
Fig. 1.
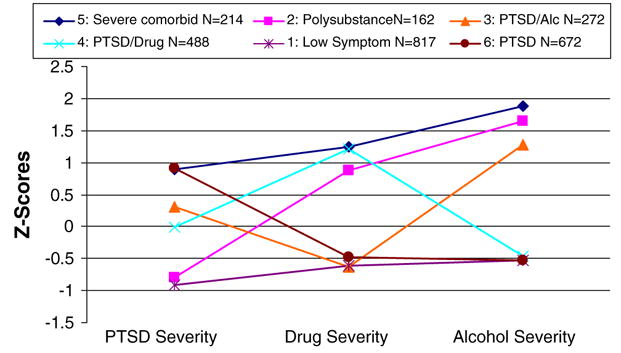
Profiles of mean symptom levels for each group. Note: PTSD severity is measured with the PSS; Drug use severity is measured with the ASI-D; Alcohol use severity is measured with the ASI-A
Characteristics of Subgroups
Demographic Characteristics
Table 1 presents a demographic profile of each of the six subgroups. Using chi-square and ANOVA tests, we found significant relationships between group membership and several demographic variables. In particular, groups differed on age F(5, 2589) = 6.58, P < .001, current employment (X2 = 13.75, df = 5, P < .01), and whether they had ever been homeless (X2 = 33.37, df = 5, P < .001). Groups also differed in the proportion of Blacks (X2 = 41.59, df = 5, P < .001) and Whites (X2 = 32.85, df = 5, P < .001). Specifically, Black women were disproportionately likely to appear in the Polysubstance group. White women appeared disproportionately in the PTSD/Drug and the PTSD/Alcohol groups. Women in the PTSD/Alcohol group were somewhat older than the rest of the women. Women in the Low Symptom group and PTSD/Alcohol group were the most likely to be employed (22.1%), while women in the PTSD group were least likely to be employed (15.2%). The greatest proportion of women who were ever homeless was found among women in the Severe Comorbid group (79.3%). There were no differences among the groups on marital status or education.
Table 1.
Full sample and subgroup demographic profile
| Demo | Full sample N = 2,729 | Grp 1 low symptom N = 817 | Grp 2 poly-substance N = 162 | Grp 3 PTSD/Alcohol N = 272 | Grp 4 PTSD/Drug N = 488 | Grp 5 severe comorbid N = 214 | Grp 6 PTSD N = 672 |
|---|---|---|---|---|---|---|---|
| Race (%) | |||||||
| Black** | 29.1 | 35.3 | 38.2 | 23.9 | 17.1 | 32.7 | 33.0 |
| White** | 54.1 | 48.7 | 44.6 | 62.8 | 61.2 | 50.0 | 53.7 |
| Hispanic | 18.1 | 19.9 | 22.8 | 15.2 | 13.8 | 16.6 | 21.8 |
| Age**—M (SD) | 35.7 (12.1) | 35.9 (9.1) | 36.4 (7.6) | 38.5 (8.7) | 33.5 (8.8) | 34.8 (8.5) | 36.3 (8.7) |
| Employment* (%) | 19.3% | 22.1% | 21.6% | 22.1% | 18.2% | 18.7% | 15.2% |
| Ever homeless** (%) | 71.6% | 65.9% | 77.2% | 65.4% | 75% | 79.3% | 74.9% |
P < .01,
P < .001
Traumatic Experiences
Differences among groups were observed on several indicators of traumatic experience (see Table 2). The proportion of women who reported childhood physical, (X2 = 70.33, df = 5, P < .001) and sexual abuse (X2 = 86.58, df = 5, P < .001) varied significantly by subgroup. The proportion who had experienced adult sexual (X2 = 74.69, df = 5, P < .001) and physical abuse (X2 = 50.35, df = 5, P < .001) also varied by subgroup. Specifically, women in the Severe Comorbid group followed by the PTSD group had the highest rates of childhood and adult physical and sexual abuse experiences. The cumulative number of lifetime experiences of interpersonal abuse also varied by subgroup F(5, 2583) = 61.99, P < .001. Post hoc pairwise comparisons indicated that the Severe Comorbid and PTSD groups reported the greatest number of lifetime abuse experiences.
Table 2.
Full sample and subgroup history of interpersonal trauma profile
| Full sample N = 2,729 | Grp 1 low symptom N = 817 | Grp 2 poly-substance N = 162 | Grp 3 PTSD/Alcohol N = 272 | Grp 4 PTSD/Drug N = 488 | Grp 5 severe comorbid N = 214 | Grp 6 PTSD N = 672 | |
|---|---|---|---|---|---|---|---|
| Child sex abuse** (%) | 62.0 | 53.1 | 49.4 | 62 | 62.2 | 70.1 | 74.2 |
| Child phys. abuse** (%) | 62.2 | 53 | 57.4 | 61 | 63 | 75.2 | 71.3 |
| Adult sex abuse** (%) | 60.3 | 49.1 | 66 | 62.2 | 59.7 | 73.4 | 67.5 |
| Adult phys. abuse** (%) | 80.4 | 72.6 | 81.5 | 85.7 | 80.9 | 87.4 | 84.5 |
| LFIAa,** M (sd) | 15.8 (7.4) | 12.8 (6.7) | 14.5 (6.6) | 16.3 (7.2) | 15.9 (7.2) | 19.5 (6.7) | 18.4 (7.1) |
Lifetime frequency of interpersonal abuse;
P < .001
Mental and Physical Health
Symptom severity related to depression F(5, 2617) = 181.39, P < .001, anxiety F(5, 2618) = 217.02, P < .001, paranoia F(5, 2617) = 129.25, P < .001, psychoticism F(5, 2617) = 175.97, P < .001, and PTSD F(5, 2619) = 731.14, P < .001, varied by symptom profile (see Table 3). Specifically, women in the Severe Comorbid group reported the highest levels of psychoticism and women in the Severe Comorbid and PTSD groups reported the highest levels of depression, anxiety, paranoia, and PTSD. Self-reported age when first emotional or mental health problems began differed by symptom profile F(5, 2559) = 10.31, P < .001. Women in the Severe Comorbid, PTSD, and PTSD/Drug groups reported a significantly younger age than women in the Polysubstance, Low Symptom, or PTSD/Alcohol groups. Ratings for overall physical health differed by subgroup F(5, 2619) = 26.36, P < .001 and were poorest for women in the Severe Comorbid, PTSD, and PTSD/Alcohol groups. The proportion of women reporting a serious physical illness differed by profile (X2 = 35.99, df = 5, P < .001). Specifically, the PTSD group had the highest rate and the Polysubstance and Low Symptom subgroups had the lowest rate.
Table 3.
Full sample and subgroup clinical profile
| Full sample N = 2,729 | Grp 1 low symptom N = 817 | Grp 2 poly-substance N = 162 | Grp 3 PTSD/Alcohol N = 272 | Grp 4 PTSD/Drug N = 488 | Grp 5 severe comorbid N = 214 | Grp 6 PTSD N = 672 | |
|---|---|---|---|---|---|---|---|
| BSI subscales | |||||||
| Depression** | 1.52 (1.01) | .88 (.75) | .95 (.70) | 1.67 (.87) | 1.62 (.96) | 2.15 (.97) | 2.07 (.94) |
| Anxiety** | 1.43 (1.0) | .76 (.67) | .96 (.68) | 1.61 (.88) | 1.44 (.94) | 2.15 (.90) | 2.03 (.94) |
| Paranoia** | 1.54 (.95) | 1.04 (.79) | 1.16 (.75) | 1.61 (.88) | 1.54 (.90) | 2.07 (.86) | 2.05 (.90) |
| Psychoticism** | 1.37 (.94) | .78 (.68) | .92 (.67) | 1.51 (.82) | 1.48 (.90) | 2.03 (.85) | 1.86 (.89) |
| GSI** | 1.35 (.78) | .80 (.52) | .92 (.51) | 1.47 (.64) | 1.38 (.72) | 1.95 (.70) | 1.90 (.70) |
| PSS** | 23.95 (11.86) | 13.12 (6.82) | 14.51 (6.91) | 27.67 (8.68) | 23.74 (9.82) | 34.56 (7.18) | 34.64 (6.68) |
| PSS > 20** | 63.4% | 22.4% | 27.8% | 84.2% | 65.6% | 100% | 100% |
| Age mental health problems began** | 13.7 (8.9) | 15.1 (9.5) | 15.5 (8.7) | 14.1 (10.0) | 13.2 (8.2) | 11.9 (7.3) | 12.4 (8.3) |
| Overall health** | 3.28 (1.08) | 3.04 (1.08) | 2.84 (1.03) | 3.41 (.98) | 3.28 (1.01) | 3.41 (1.04) | 3.58 (1.07) |
| Physical disability** | 49.1% | 44.2% | 35.8% | 50% | 50.1% | 50% | 56.9% |
P < .001
Differential Intervention Effects by Cluster
PSS Symptoms
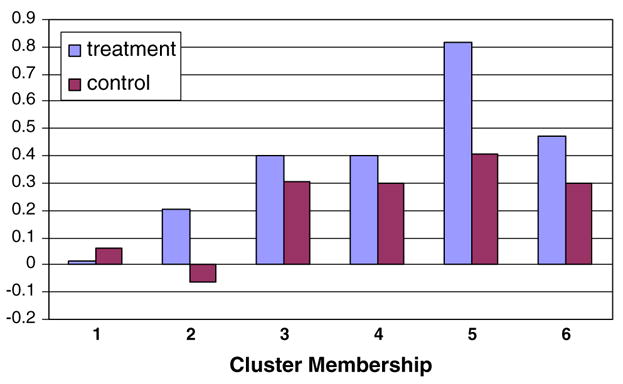
The results of propensity score weighted t-tests indicated significant improvement for the PTSD/Drug t(365) = −2.53, P < .01, the Severe Cormorbid t(140) = −3.05, P < .01, and the PTSD cluster t(480) = −2.63, P < .01. The adjusted mean change in PTSD symptoms from baseline to 12 months is shown in Fig. 2 for each group. The largest effect was found for the Severe Comorbid group, in which women in the intervention had an average decrease of 14.1 points on the PSS, compared to a decrease of 8 points for the comparison group (Cohen’s d effect size = .38), followed by the PTSD/Drug group (Cohen’s d effect size = .27), and the PTSD group (Cohen’s d effect size = .24). To put these numbers in perspective, a decrease of 14 points might indicate, for example, a change from a rating of “almost always” to “once in a while” for seven of the 17 PTSD symptoms.
Fig. 2.
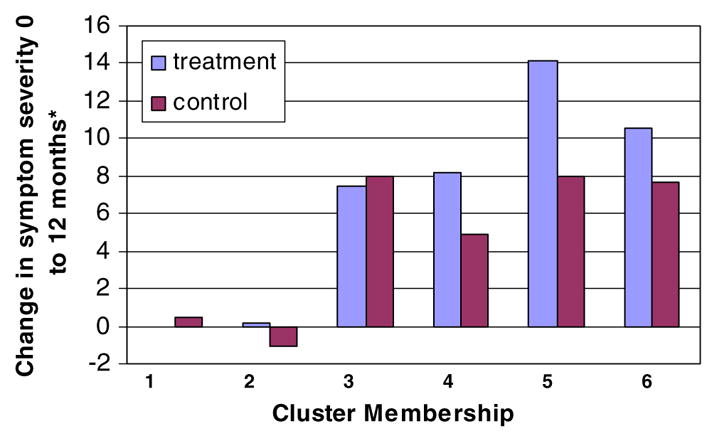
Propensity-weighted PTSD symptom change by cluster and study condition. Cluster 1 = Low symptom group; Cluster 2 = Substance abuse group; Cluster 3 = PTSD/Alcohol group; Cluster 4 = PTSD/Drug group; Cluster 5 = Severe comorbid group; Cluster 6 = PTSD group. * Higher scores correspond to greater improvement
ASI-A Symptoms
The results of propensity score weighted t-tests indicated significant improvement for the Polysubstance group t(122) = −2.72, P < .01. The mean change from baseline to 12 months on the ASI-A for each cluster is shown in Fig. 3. The largest effect was found for the Polysubstance cluster in which women in the intervention had an average decrease of .59 on the 0–1 scale compared to .44 for the comparison group (Cohen’s d effect size = .37).
Fig. 3.
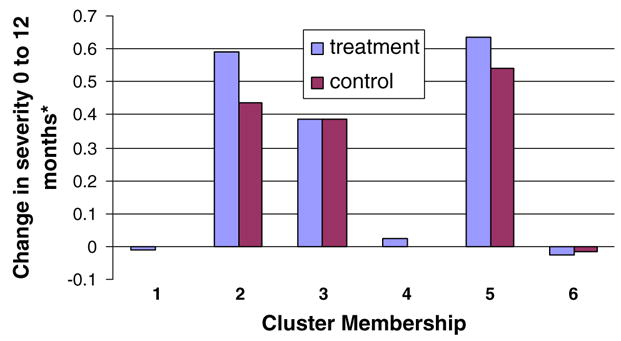
Propensity-weighted change in alcohol use severity by cluster and study condition. Cluster 1 = Low symptom group; Cluster 2 = Substance abuse group; Cluster 3 = PTSD/Alcohol group; Cluster 4 = PTSD/Drug group; Cluster 5 = Severe comorbid group; Cluster 6 = PTSD group. * Higher scores correspond to greater improvement
ASI-D Symptoms
The results of propensity score-weighted t-tests indicated significant improvement for the Polysubstance t(122) = −2.19, P < .05 and PTSD/Drug clusters t(374) = −2.84, P < .01. The mean change from baseline to 12 months on the ASI-D for each subgroup is shown in Fig. 4. The largest effect was found for the Polysubstance group in which intervention women had an average decrease of .25 compared to .19 for the comparison (Cohen’s d effect size = .29), followed by the PTSD/Drug group in which intervention women had an average decrease of .27 compared to .24 for the comparison (Cohen’s d effect size = .20).
Fig. 4.
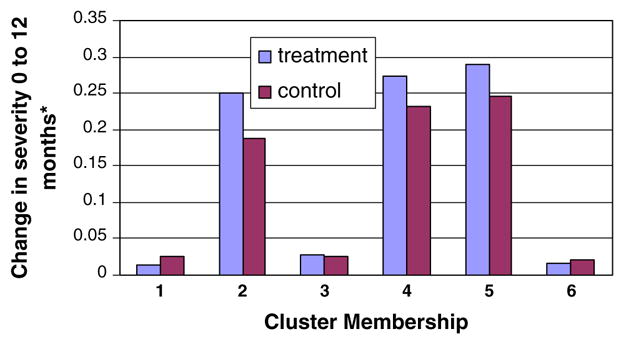
Propensity-weighted change in drug use severity by cluster and study condition. Cluster 1 = Low symptom group; Cluster 2 = Substance abuse group; Cluster 3 = PTSD/Alcohol group; Cluster 4 = PTSD/Drug group; Cluster 5 = Severe comorbid group; Cluster 6 = PTSD group. * Higher scores correspond to greater improvement
GSI Symptoms
The results of propensity score-weighted t-tests indicated significant improvement for the Polysubstance group t(122) = −2.37, P < .05, Severe Comorbid group t(146) = −2.93, P < .01, and the PTSD group, t(489) = −2.36, P < .05. The mean change from baseline to 12 months on the GSI for each subgroup is shown in Fig. 5. The largest effect was found for the Severe Comorbid cluster in which intervention women had an average decrease of .82 compared to .41 for the comparison (Cohen’s d effect size = .36) followed by the Polysubstance group in which intervention women had an average decrease of .21 compared to an increase of .06 for the comparison (Cohen’s d effect size = .33).
Fig. 5.
Propensity-weighted change in GSI by cluster and study condition. Cluster 1 = Low symptom group; Cluster 2 = Substance abuse group; Cluster 3 = PTSD/Alcohol group; Cluster 4 = PTSD/Drug group; Cluster 5 = Severe comorbid group; Cluster 6 = PTSD group. * Higher scores correspond to greater improvement
Clinical Significance
We examined the clinical significance of the PTSD outcomes based on cutoff scores as well as indicators of reliable change (see Table 4). The proportion of women who were considered “cases” before treatment who would no longer be considered “cases” following treatment was approximately 50% of all intervention participants among the four PTSD clusters. Women who were above the cutoff at baseline (“cases”) yet below the cutoff at the 12-month follow-up (“non-cases”) ranged from 37% to 47% among the four PTSD clusters. The proportion who met the Jacobson and Truax (1991) criteria for reliable change—which goes beyond the magnitude of the effect by also considering the reliability of the measurement—ranged from 38% to 60% across the four PTSD clusters.
Table 4.
Clinical significance of intervention group improvement on the PSS
| Grp 1 low symptom N = 817 (%) | Grp 2 poly-substance N = 162 (%) | Grp 3 PTSD/Alcohol N = 272 (%) | Grp 4 PTSD/Drug N = 488 (%) | Grp 5 severe comorbid N = 214 (%) | Grp 6 PTSD N = 672 (%) | |
|---|---|---|---|---|---|---|
| Above PTSD cutoff at baseline* | 21 | 24.2 | 85.9 | 66.4 | 100 | 100 |
| Above PTSD cutoff at follow up | 24.3 | 30.6 | 49 | 37.7 | 52.6 | 63.3 |
| % Changed from case to non-casea | 11.7 | 10.2 | 39.8 | 37.1 | 47.4 | 36.7 |
| % Meeting RCIb | 13.8 | 8.2 | 45.9 | 37.7 | 60.3 | 47 |
PSS score of ≥20,
Caseness is defined as being at or above the cutoff score,
RCI = reliable change index (Jacobson and Truax 1991)
Discussion
The main finding emerging from the current study was that women with the most severe PTSD and substance abuse presentation (Severe Comorbid Group) who received the integrated intervention had the greatest amount of symptom reduction in PTSD symptoms relative to the comparison condition, followed by women with the PTSD/Drug profile and those with the PTSD profile. The PTSD effect size achieved by the Severe Comorbid subgroup (.38) is considerably larger than that reported in the initial WCDVS outcomes paper (effect size = .16; Morrissey, et al. 2005a, b) and consistent with effect sizes (.33–.61) found in studies of non-exposure based PTSD interventions (Bisson et al. 2007).
These three subgroups of women represent a population of difficult to treat individuals and are arguably the most in need of an integrated trauma-specific intervention. The fact that these women obtained statistically significant and clinically meaningful change following the integrated intervention is highly encouraging. Women in the PTSD/Alcohol profile were the only subgroup characterized by PTSD symptoms whose PTSD outcomes were no better for women in the integrated intervention than in the comparison condition (although both groups achieved a moderate reduction of approximately 8 points on the PSS).
Our findings indicate that women in the WCDVS had a variety of outcomes associated with interpersonal victimization. The findings regarding the heterogeneous symptom patterns are consistent with studies examining rates of psychiatric disorder stemming from childhood and adult victimization (Kendall-Tackett et al. 1993; Hanson et al. 2001), which indicate a full range of outcomes associated with trauma—including no negative psychological outcomes (Binder et al. 1996). The diversity of outcomes associated with trauma suggests that not all persons with a trauma history and other mental health/substance abuse problems should need the same intervention addressing traumatic experiences. In addition, the literature on psychological interventions in the immediate aftermath of a traumatic event suggests that since the majority of individuals do not develop psychological problems following trauma, trauma-focused interventions broadly targeting a trauma-exposed group may disrupt the normal recovery process and may even be harmful (Rauch et al. 2001; Gray and Litz 2005). As the mental health and substance abuse fields have begun to recognize the role of traumatic victimization in the needs of their clients, it is critical that a distinction between traumatic victimization and trauma-related symptoms remain clear.
While the lack of treatment effect for the PTSD/Alcohol group is somewhat surprising, this finding is in part consistent with literature examining differences in women with PTSD who abuse drugs versus alcohol (Back et al. 2003; Saladin et al. 1995). The extant literature suggests that women with PTSD who abuse alcohol are likely to be older, have chronic PTSD, and have higher levels of avoidance and arousal. This is exactly what was found in the current study. Although chronicity was not addressed in the WCDVS, women with PTSD/Alcohol were older than any other profile and had significantly higher avoidance and arousal symptoms than women with the PTSD/Drug profile. In light of this, the finding of no improvement for women with PTSD/Alcohol may speak to a more treatment-resistant form of PTSD. Future research is needed to further explore these differential patterns of comorbidity.
In order to address concerns that symptoms other than PTSD are important treatment targets, we also looked at the GSI as an indicator of treatment outcome. Similar to their PTSD outcomes, the subgroups with the highest levels of PTSD symptoms (Severe Comorbid and PTSD) improved significantly on the GSI. The two other clusters characterized by PTSD and substance abuse (PTSD/Alcohol, PTSD/Drug) did not improve significantly on the GSI relative to the comparison condition. One possible explanation is that it takes greater reductions in PTSD symptoms—of the magnitude experienced by the Severe Comorbid and PTSD clusters—to impact symptoms that may be secondary to PTSD.
Contrary to hypotheses, we found overall little differential improvement in substance abuse outcomes for the three PTSD groups with comorbid drug or alcohol problems. It is possible that the duration and/or intensity of the substance abuse component of the intervention was insufficient for these dually disordered groups. More research is needed on interventions that simultaneously address PTSD and substance abuse to determine the optimal balance of efficiency and effectiveness.
One benefit of analyzing treatment outcome by subgroup is that we were able to examine the impact of the integrated intervention in the two subgroups without significant levels of current PTSD symptoms (Group 1: Low Symptom and Group 2: Polysubstance). Of equal importance to the above findings is that there was no positive effect of the integrated intervention for women in the Low Symptom cluster on either PTSD symptoms or other mental health domains frequently mentioned as trauma-related problems. In contrast, women in the Polysubstance cluster did have significantly greater improvement on the alcohol and drug measures. These women also improved on the GSI relative to women in the comparison condition. However, the magnitude of change was small, corresponding to a change of 2 T-score points.
While some form of mental health service (e.g., careful assessment/PTSD screening) may be appropriate for all trauma victims, and other specific interventions may be appropriate for many trauma victims (e.g., safety planning, assertiveness skills), the current findings suggest that integrated trauma-specific interventions are not necessarily helpful for women with any mental health and substance abuse presentation simply on the basis of their history of interpersonal abuse. As in other areas of life, one size does not fit all; trauma interventions must be tailored to the presenting problems and experiences of each individual. Further, integrated interventions are demanding, time consuming, and costly—not only for the women recipients, but for clinicians and payers as well (Domino et al. 2005a, b). Public mental health systems in the U.S. have constrained resources and individuals with PTSD are particularly highly underserved (Cusack et al. 2006; Mueser et al. 1998; Switzer et al. 1999). Therefore, the scant resources available in mental health systems should be prioritized for those clearly in need of intervention.
Limitations
The findings are based on secondary analyses that are largely exploratory and hypothesis generating. While k-means cluster analysis is a useful technique for describing subgroups, it is an exploratory technique that does not yield definitive results. Women in the study were recruited to take part in the intervention. Therefore, the results may not be representative of the population of women with co-occurring disorders who are victims of interpersonal abuse and high-end users of substance abuse and mental health services. However, the large sample size, range of urban/rural sites, and diversity of service settings in the study increase the confidence that the women in the WCDVS are representative of this group. On the other hand, a drawback of analyzing large samples is that the analyses may produce statistically significant results that have little clinical significance. Based on indicators of clinical significance in the present study, our findings are indicative of meaningful effects. Although the use of propensity score adjustment can be a useful method for reducing bias associated with non-random assignment to conditions, the propensity score incorporates only measured covariates and therefore cannot account for bias resulting from unmeasured variables. To the extent that the measured covariates in this study do not capture all pretreatment differences between the two conditions, bias may still exist. Further research with randomized designs is needed for more rigorous tests of the relationship between trauma symptom profiles and differential responses to integrated interventions.
Conclusions
Targeting trauma-related interventions is essential for optimal benefits. Clinicians working with women victims of interpersonal violence should conduct careful assessments of current symptoms to identify the need for intervention. We suggest that integrated trauma-related interventions should be reserved for women who are most in need and may be expected to benefit from such interventions. Our findings indicate that these are women with active PTSD symptoms. Women with other characteristics such as polysubstance use without PTSD may obtain some benefit from such an intervention, but choosing interventions specifically addressing their presenting symptoms may have more positive results.
Acknowledgments
This work was supported in part by MH019117 from the National Institute of Mental Health and the Guidance for Applicants (GFA) No. TI 00-003 entitled Cooperative Agreement to Study Women with Alcohol, Drug Abuse and Mental Health (ADM) Disorders who have Histories of Violence: Phase II from the Department of Health and Human Services, Public Health Service, Substance Abuse and Mental Health Administration’s three centers: Center for Substance Abuse Treatment, Center for Mental Health Services, and Center for Substance Abuse Prevention (March, 2000). Portions of this paper were previously presented at the annual meeting of the International Society for Traumatic Stress Studies in Hollywood (November, 2006).
References
- Back SE, Sonne SC, Killeen T, Dansky BS, Brady KT. Comparative profiles of women with PTSD and comorbid cocaine or alcohol dependence. The American Journal of Drug and Alcohol Abuse. 2003;29(1):169–189. doi: 10.1081/ada-120018845. [DOI] [PubMed] [Google Scholar]
- Beck JC, van der Kolk BA. Reports of childhood incest and current behavior of chronically hospitalized psychotic women. American Journal of Psychiatry. 1987;144:1474–1476. doi: 10.1176/ajp.144.11.1474. [DOI] [PubMed] [Google Scholar]
- Becker MA, Noether CD, Larson MJ, Gatz M, Brown V, Heckman JP, et al. Characteristics of women engaged in treatment for trauma and co-occurring disorders: Findings from a multisite study. Journal of Community Psychology. 2005;33(4):429–443. [Google Scholar]
- Binder RL, McNiel DE, Goldstone RL. Is adaptive coping possible for adult survivors of childhood sexual abuse? Psychiatric Services. 1996;47:186–188. doi: 10.1176/ps.47.2.186. [DOI] [PubMed] [Google Scholar]
- Bisson JI, Ehlers A, Mattews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post-traumatic stress disorder: Systematic review and meta-analysis. British Journal of Psychiatry. 2007;190:97–104. doi: 10.1192/bjp.bp.106.021402. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Current Directions in Psychological Science. 2004;13(5):206–209. [Google Scholar]
- Breslau N, Davis GC, Peterson EL, Schultz LR. A second look at comorbidity in victims of trauma: The posttraumatic stress disorder-major depression connection. Biological Psychiatry. 2000;48:902–909. doi: 10.1016/s0006-3223(00)00933-1. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Briere J, Woo R, McRae B, Foltz J, Sitzman R. Lifetime victimization history, demographics, and clinical status in female psychiatric emergency room patients. Journal of Nervous and Mental Disease. 1997;185:95–101. doi: 10.1097/00005053-199702000-00005. [DOI] [PubMed] [Google Scholar]
- Carmen E, Rieker PP, Mills T. Victims of violence and psychiatric illness. American Journal of Psychiatry. 1984;141:378–383. doi: 10.1176/ajp.141.3.378. [DOI] [PubMed] [Google Scholar]
- Cascardi M, Mueser KT, DeGirolomo J, Murrin M. Physical aggression against psychiatric inpatients by family members and partners: A descriptive study. Psychiatric Services. 1996;47:531–533. doi: 10.1176/ps.47.5.531. [DOI] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N. Posttraumatic stress disorder and drug disorders: Testing causal pathways. Archives of General Psychiatry. 1998;55:913–917. doi: 10.1001/archpsyc.55.10.913. [DOI] [PubMed] [Google Scholar]
- Cocozza JJ, Jackson EW, Hennigan K, Morrissey JP, Reed BG, Fallot R, et al. Outcomes for women with co-occurring disorders and trauma: Program-level effects. Journal of Substance Abuse Treatment. 2005;28:109–119. doi: 10.1016/j.jsat.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Craine LS, Henson CE, Colliver JA, MacLean DG. Prevalence of a history of sexual abuse among female psychiatric patients in a state hospital system. Hospital and Community Psychiatry. 1988;39:300–304. doi: 10.1176/ps.39.3.300. [DOI] [PubMed] [Google Scholar]
- Cusack KJ, Grubaugh AL, Knapp R, Frueh BC. Trauma and PTSD in public mental health consumers with serious mental illness. Community Mental Health Journal. 2006;42:487–500. doi: 10.1007/s10597-006-9049-4. [DOI] [PubMed] [Google Scholar]
- Derogatis L. A brief form of the SCL-90-R: A self-report symptom inventory designed to measure psychological stress: Brief Symptom Inventory (BSI) Minneapolis: National Computer Systems; 1993. [Google Scholar]
- Domino ME, Morrissey JP, Chung S, Huntington N, Larson MJ, Russel LA. Service use and costs for women with co-occurring mental and substance use disorders and a history of violence. Psychiatric Services. 2005a;56:1223–1232. doi: 10.1176/appi.ps.56.10.1223. [DOI] [PubMed] [Google Scholar]
- Domino M, Morrissey JP, Nadlicki-Patterson T, Chung S. Service costs for women with co-occurring disorders and trauma. Journal of Substance Abuse Treatment. 2005b;28(2):135–143. doi: 10.1016/j.jsat.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Drake RE, Mueser KT. Managing comorbid schizophrenia and substance abuse. Current Psychiatry Reports. 2001;3:418–422. doi: 10.1007/s11920-996-0037-8. [DOI] [PubMed] [Google Scholar]
- Elhai JD, North TC, Frueh BC. Health service use predictors among trauma survivors: A critical review. Psychological Services. 2005;2:3–19. [Google Scholar]
- Fallot RD, Harris M. The trauma recovery and empowerment model (TREM): Conceptual and practical issues in a group intervention for women. Community Mental Health Journal. 2002;38(6):475–485. doi: 10.1023/a:1020880101769. [DOI] [PubMed] [Google Scholar]
- Foa EB, Keane TM, Friedman MJ. Effective treatments for PTSD: Practice guidelines from the international society for traumatic stress studies. New York: Guilford; 2000. [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Frueh BC, Cusack KJ, Hiers TG, Monogan S, Cousins VC, Cavenaugh SD. Improving public mental health services for trauma victims in South Carolina. Psychiatric Services. 2001;52(6):812–814. doi: 10.1176/appi.ps.52.6.812. [DOI] [PubMed] [Google Scholar]
- Goodman LA, Dutton MA, Harris M. Physical and sexual assault prevalence among episodically homeless, seriously mentally ill women. Violence and Victims. 1995;11:159–174. [PubMed] [Google Scholar]
- Gray MJ, Litz BT. Behavioral interventions for recent trauma: Empirically informed practice guidelines. Behavior Modification. 2005;29(1):189–215. doi: 10.1177/0145445504270884. [DOI] [PubMed] [Google Scholar]
- Hair JF, Jr, Anderson RE, Tatham RL, Black WC. Multivariate data analysis. Upper Saddle River, NJ: Prentice-Hall; 1998. [Google Scholar]
- Hanson RF, Saunders B, Kilpatrick D, Resnick H, Crouch JA, Duncan R. Impact of childhood rape and aggravated assault on adult mental health. American Journal of Orthopsychiatry. 2001;71(1):108–119. [PubMed] [Google Scholar]
- Hartigan JA. Clustering algorithms. New York: Wiley; 1975. [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry. 2001;158:1184–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jennings A. Models for developing trauma-informed behavioral-health systems and trauma-specific services. National Association of Mental Health Program Directors, National Technical Assistance Center for State Mental Health Planning 2004 [Google Scholar]
- Kendall-Tackett KA, Williams LM, Finkelhor D. Impact of sexual abuse on children: A review and synthesis of recent empirical studies. Psychological Bulletin. 1993;13:164–180. doi: 10.1037/0033-2909.113.1.164. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Study. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Saunders BE, Best CL. Rape, other violence against women, and posttraumatic stress disorder. In: Dohrenwend BP, editor. Adversity, Stress, and Psychopathology. New York: Oxford Press; 1998. [Google Scholar]
- McCaffrey DF, Ridgeway G, Morral AR. Propensity score estimation with boosted regression for evaluating causal effects in observational studies. Psychological Methods. 2004;9(4):403–425. doi: 10.1037/1082-989X.9.4.403. [DOI] [PubMed] [Google Scholar]
- McHugo GJ, Caspi Y, Kammerer N, Mazelis R, Jackson EW, Russell L, et al. The assessment of trauma history in women with co-occurring substance abuse and mental disorders and a history of interpersonal violence. Journal of Behavioral Health Services & Research. 2005a;32(2):113–127. doi: 10.1007/BF02287261. [DOI] [PubMed] [Google Scholar]
- McHugo GJ, Kammerer N, Jackson EW, Markoff LS, Gatz M, Larson MJ, et al. Women, co-occurring disorders, and violence study: Evaluation design and study population. Journal of Substance Abuse Treatment. 2005b;28(2):91–107. doi: 10.1016/j.jsat.2004.08.009. [DOI] [PubMed] [Google Scholar]
- McLellan A, Luborsky L, O’Brien CP, Woody G. An improved diagnostic evaluation instrument for substance abuse patients: The addiction severity index. Journal of Nervous and Mental Disease. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Morrissey JP, Ellis AR, Gatz M, Amaro H, Reed BG, Savage A, et al. Outcomes for women with co-occurring disorders and trauma: Program and person-level effects. Journal of Substance Abuse Treatment. 2005a;28(2):121–134. doi: 10.1016/j.jsat.2004.08.012. [DOI] [PubMed] [Google Scholar]
- Morrissey JP, Jackson EW, Ellis AR, Amaro H, Brown VB, Najavits LM. Twelve-month outcomes of trauma-informed interventions for women with co-occurring disorders. Psychiatric Services. 2005b;56(10):1213–1222. doi: 10.1176/appi.ps.56.10.1213. [DOI] [PubMed] [Google Scholar]
- Muenzenmaier K, Meyer I, Struening E, Ferber J. Childhood abuse and neglect among women outpatients with chronic mental illness. Hospital and Community Psychiatry. 1993;44:666–670. doi: 10.1176/ps.44.7.666. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Goodman LB, Trumbetta SL, Rosenberg SD, Osher FC, Vidaver R, et al. Trauma and posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology. 1998;66:493–499. doi: 10.1037//0022-006x.66.3.493. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Noordsy DL, Drake RE, Fox L. Integrated treatment for dual disorders. New York: Guilford Press; 2003. [Google Scholar]
- Mueser KT, Rosenberg SD, Goodman LA, Trumbetta SL. Trauma, PTSD, and the course of severe mental illness: An interactive model. Schizophrenia Research. 2002;53:123–143. doi: 10.1016/s0920-9964(01)00173-6. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR. The link between substance abuse and posttraumatic stress disorder in women: A research review. American Journal of Addictions. 1997;6:273–283. [PubMed] [Google Scholar]
- Pimlott-Kubiak S, Cortina LM. Gender, victimization, and outcomes: Reconceptualizing risk. Journal of Consulting and Clinical Psychology. 2003;71(3):528–539. doi: 10.1037/0022-006x.71.3.528. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2004. [Google Scholar]
- Rauch SA, Hembree EA, Foa EB. Acute psychosocial preventive interventions for posttraumatic stress disorder. Advances in Mind-Body Medicine. 2001;17(3):187–190. doi: 10.1054/ambm.2000.0312. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. Journal of the American Statistical Association. 1984;79:516–524. [Google Scholar]
- Saladin ME, Brady KT, Kilpatrick DG. Understanding comorbidity between PTSD and substance use disorders: Two preliminary investigations. Addictive Behaviors. 1995;20(5):643–655. doi: 10.1016/0306-4603(95)00024-7. [DOI] [PubMed] [Google Scholar]
- Surrey J, Swett C, Jr, Michaels A, Levin S. Reported history of physical and sexual abuse and severity of symptomatology in women psychiatric outpatients. American Journal of Orthopsychiatry. 1990;60:412–417. doi: 10.1037/h0079172. [DOI] [PubMed] [Google Scholar]
- Switzer GE, Dew MA, Thompson K, Goycoolca JM, Derricott T, Mullins SD. Posttraumatic stress disorder and service utilization among urban mental health center clients. Journal of Traumatic Stress. 1999;12:25–39. doi: 10.1023/A:1024738114428. [DOI] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Prevalence and consequences of male-to-female and female-to-male intimate partner violence as measured by the National violence against women survey. Violence Against Women. 2000;6(2):142–161. [Google Scholar]
- U.S. Department of Health and Human Services. Mental health. A Report of the Surgeon General 1999 [Google Scholar]
- Wolfe J, Kimerling R. Gender issues in the assessment of posttraumatic stress disorder. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford; 1997. pp. 192–238. [Google Scholar]


