Abstract
We analyzed the trends in product regimens used to treat depression to investigate whether there has been a shift in treatment patterns following the May 2008 launch of desvenalfaxine in the United States and the approval of an atypical antipsychotic as add-on therapy to antidepressants. Our analysis suggests that antidepressant monotherapy continues to be the most widely used drug treatment approach, accounting for 84 percent of depression treatment regimens. Antidepressant monotherapy is more prevalent among primary care physician-prescribed treatment regimens (92%) than psychiatry-prescribed regimens (73%). Combination treatment regimens have become increasingly more common as physician perception of disease severity increases, with antidepressant combination therapy accounting for eight percent, 17 percent, and 27 percent of treatment regimens for mild, moderate, and severe depression, respectively. The most commonly used agents in addition to an antidepressant in combination treatment regimens include another antidepressant (40% of combination regimens), an anxiety agent (40%), and/or atypical antipsychotics (18%). A trend analysis suggests that combination regimens that include an antidepressant plus an atypical antipsychotic, anxiety agent, or a prescription sleep aid comprise a greater share of combination regimens in 12 months ending May 2009 than they did in 12 months ending June 2008.
Keywords: depression, antidepressant, monotherapy, combination therapy, desvenalfaxine, antipsychotic
Introduction
A previous Trend Watch published in November 20071 presented trends in depression treatment regimens to uncover how clinicians were using antidepressants in the treatment of depression over a 12-month period, ending August 2007. Since that analysis was completed, the United States Food and Drug Administration (FDA) approved desvenlafaxine, a new serotonin and norepinephrine reuptake inhibitor (SNRI), for the treatment of depression in adults. Additionally, an atypical antipsychotic, aripiprazole, was approved as an add-on agent to antidepressant therapy. Given the new approvals in the area of depression treatment, we reanalyzed depression product regimens to understand if the use of antidepressants has changed over time and whether the use of atypical antipsychotics in depression has increased with the new indication approvals.
Methods
We obtained product regimen data from SDI Health’s Physician Drug and Diagnosis Audit (PDDA) from July 2007 through May 2009 for depression (ICD-9 code 311). PDDA provides data on disease states and associated treatment from a panel of approximately 3,100 office-based physicians across 29 specialties. Depression treatment regimens were analyzed overall and by both specialty and physician-reported disease severity. Trend data was analyzed on moving 12-month increments, so as to maintain a robust sample size.
Results
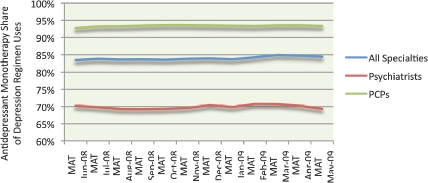
As seen in Figure 1, antidepressant monotherapy represented 84 percent of depression drug regimens in the 12-month period ending May 2009. Antidepressant monotherapy regimens represent a growing share of primary care physician (PCP)-prescribed regimens, representing 93 percent of PCP depression regimens in 12 months ending May 2009. Conversely, at 69 percent of all psychiatry-prescribed depression regimens in 12 months ending May 2009, antidepressant monotherapy regimens comprised a shrinking share of psychiatrist-prescribed depression regimens, meaning that combination therapy comprised a growing share of regimens prescribed by psychiatrists.
FIGURE 1.
Share of antidepressant monotherapy across all depression regimens by specialty.
Source: SDI Health PDDA, ICD-9 Diagnosis Code 311, July 2007–May 2009.
Key:
- MAT
- moving annual total
Similar to previous findings, the proportion of antidepressant monotherapy regimen uses also varied by physician-perceived disease severity (Figure 2). In 12 months ending May 2009, antidepressant monotherapy comprised a larger share of regimen uses in mild depression (92%) than for moderate depression (83%) or severe depression (73%). There was a slight uptick in the share of monotherapy regimens in mild depression, while monotherapy rates remained relatively constant in moderate- and severe-depression.
FIGURE 2.
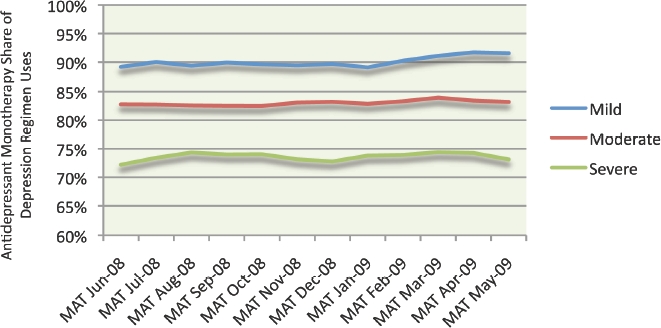
Share of antidepressant monotherapy across all depression regimens by physician-reported disease severity.
Source: SDI Health PDDA, ICD-9 Diagnosis Code 311, July 2007–May 2009.
Key:
- MAT
- moving annual total
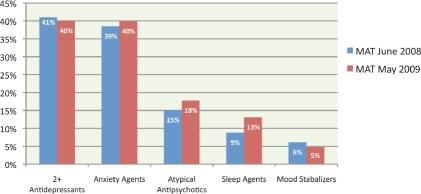
While antidepressant monotherapy continues to dominate depression regimens, we isolated combination regimens over time to understand if and how combination therapy is evolving. In Figure 3, we compared antidepressant combination therapy regimens prescribed in 12 months ending June 2008 with those prescribed in 12 months ending May 2009. Within antidepressant combination regimens, we found that the agents physicians most often prescribed with an antidepressant in 12 months ending May 2009 included an anxiety agent, such as a benzodiazepine (40% of combination regimens), or another antidepressant (40%), such as a selective serotonin reuptake inhibitor (SSRI) plus buproprion combination. Other therapeutic classes found in antidepressant combination regimens included atypical antipsychotics (18% of combination regimens), prescription sleep aids (13%), and/or mood stabilizers (5%). A comparison of the combination regimens prescribed in 12 months ending June 2008 with those prescribed in 12 months ending May 2009 revealed that combination regimens including atypical antipsychotics, anxiety agents, and prescription sleep aids, represented larger shares of the combination regimen mixes than they did in the past, while combinations involving a mood stabilizer or an additional antidepressant were less likely.
FIGURE 3.
Therapies used in combination with antidepressants for the treatment of depression. Combination regimens represent 16.6% of depression regimens in MAT June 2008 and 15.6% of depression regimens in MAT May 2009. Shares do not total 100% due to combinations that could include multiple classes. Anxiety agents include benzodiazepines and Buspar (buspirone). Mood stabilizers include antiepileptics and lithium. Trazodone classified as an antidepressant.
Source: SDI Health PDDA, ICD-9 Diagnosis Code 311, MAT June 2008 and MAT May 2009.
Key:
- MAT
- moving annual total
Contributor Information
Susan Lenderts, Ms. Lenderts is Manager, Strategic Analytics, Quintiles, Inc.,/Innovex, Falls Church, Virginia.
Amir Kalali, Dr. Kalali is Vice President, Global Therapeutic Group Leader CNS, Quintiles Inc., San Diego, California, and Professor of Psychiatry, University of California, San Diego.
References
- 1.Cascade E, Kalali A, Blier P. Treatment of depression: antidepressant monotherapy and combination therapy. Psychiatry (Edgemont) 2007;4(11):21–23. [PMC free article] [PubMed] [Google Scholar]