Abstract
Aims
The purpose of the study was to examine whether patients with borderline personality disorder (BPD) have a higher rate of new onsets of substance use disorders (SUD) than do patients with other personality disorders (OPD).
Design
This study uses data from the Collaborative Longitudinal Personality Disorder Study (CLPS), a prospective naturalistic study with reliable repeated measures over 7 years of follow-up.
Setting
Multiple clinical sites in four northeastern US cities.
Participants
175 patients with BPD and 396 patients with OPD (mean age 32.5 years), were assessed at baseline and at 6, 12, 24, 36, 48, 60, 72, and 84 months.
Measurements
The Structured Clinical Interview for DSM-IV Axis I Disorders and the Diagnostic Interview for DSM-IV Personality Disorders were used at baseline, the Follow-Along Version of the DIPD-IV and the Longitudinal Interval Follow-Up Evaluation at the follow-up evaluations. Kaplan-Meier analyses were calculated to generate the time to new onsets.
Findings
BPD patients showed a shorter time to new onsets of SUD. Thirteen percent of BPD patients developed a new alcohol use disorder, and 11% developed a new drug use disorder, as compared to rates of 6% and 4% respectively for OPD. Non-remitted BPD and remitted BPD patients did not differ significantly in rates of new onsets of SUD.
Conclusions
BPD patients have a high vulnerability for new onsets of SUDs even when their psychopathology improves. These findings indicate some shared etiological factors between BPD and SUD and underscore the clinical significance of treating SUD when it co-occurs in BPD patients.
Keywords: Borderline personality disorder, substance use disorder, alcohol use disorder, drug use disorder, new onset, CLPS
Introduction
While it is well known that the psychiatric comorbidity rates in BPD patients include elevated rates of mood disorders, anxiety disorders, eating disorders, and posttraumatic stress disorder (PTSD), BPD has shown a particularly strong association with substance use disorders (SUD) (1-10). Prior studies have shown that half or more of patients with BPD have co-occurring alcohol use disorder (AUD) or drug use disorder (DUD) (11-14), and that co-occurrence of these substance use disorders (SUD) is associated with a greater severity of suicidality in BPD patients (15).
The standard explanation as to why BPD has increased rates of SUDs is a shared genetically-based disposition to poor impulse control (16-18); i.e. that both are impulse spectrum disorders (19-21). This association of BPD with high impulsivity would link it to antisocial personality disorder (ASPD), a disorder linked epidemiologically and genetically to SUD (22-28). However, although the markedly increased prevalence of both SUD and ASPD in relatives of BPD subjects (29-32) supports a likely spectrum relationship between these disorders, the genetic evidence currently available for the link between BPD and SUD is limited (33).
Environmental issues that predispose patients with either BPD or SUD to relapse may be as important. BPD subjects show significantly higher responses to psychosocial stressors than healthy control subjects (34, 35) and specifically to interpersonal stressors than do patients with other personality disorders (36). In SUD patients, taking drugs is frequently driven by cravings from drug-conditioned stimuli and stress (37, 38) which also play a critical role in relapse after prolonged abstinence (39, 40). Thus, the psychosocial stressors may add vulnerability to both BPD and SUD and make BPD patients more vulnerable to new onsets of SUD.
The study reported here will examine whether the hypothesized spectrum relationship between BPD and SUD is demonstrated using longitudinal data. At this time there are no prior studies having examined the vulnerability to new onsets of SUDs in BPD patients. This report takes place within a new context, insofar as longitudinal studies have recently shown that most BPD patients remit (41, 42). However, based on the hypothesis that both disorders share etiological factors, BPD patients might still retain a risk for developing a SUD in the long-term course. This study uses prospectively collected data from the Collaborative Longitudinal Personality Disorder Study (CLPS) (42) to investigate the risk of development a SUD in BPD versus other personality disorders (OPD). We will also examine whether non-remitted BPD have higher rates of new onsets of SUD.
Methods
Participants
Participants for this study were enrolled in CLPS, an ongoing National Institute of Mental Health-funded, multi-site, prospective naturalistic study. Detailed descriptions of aims, design, assessment methods, and sample characteristics and major findings of the Collaborative Longitudinal Personality Disorders Study (CLPS) project have been reported separately (42, 43). Briefly, the CLPS included treatment-seeking patients aged 18 to 45 years with one of four study personality disorders (schizotypal personality disorder, STPD; borderline personality disorder, BPD; avoidant personality disorder, AVPD; obsessive-compulsive disorder, OCPD) for whom follow-up data were collected over seven years (6, 12, 24, 36, 48, 60, 72 and 84 months). The four personality disorders selected for the study represent those which are the most prototypic and prevalent within the three DSM personality clusters: i.e, STPD for cluster A, BPD for cluster B, AVPD for cluster C (36). OCPD was added because factor analytic studies had shown that it is distinctive from the three DSM clusters (44). Each of the four personality disorders derive from different theoretical frameworks. By focusing on these four personality disorders, only about 15% of treatment-seeking patients meeting the criteria for any axis II disorder were excluded (43).
Exclusion criteria were schizophrenia, schizoaffective disorders, psychotic disorder due to medical conditions, and current substance intoxication or withdrawal. The study is based on 571 personality disorder participants with follow-up data over seven years. Of the participants, 65% were women, and 35% were men. The mean age was 32.5 (SD = 8.1) years.
For the purpose of the study, patients were divided into the following two groups: those diagnosed with borderline personality disorder (BPD) (n = 175) and a comparison group of those diagnosed with STPD, AVPD, and OCPD (other personality disorder, OPD) (n = 396). The BPD group consisted of 75% women and 25% men, the OPD group of 60% women and 40% men. The mean ages were 32.1 (SD = 7.8) for the BPD group and 32.7 (SD = 8.3) for the OPD group.
New onset was defined as a new diagnosis of alcohol or drug use disorder for one month or longer in the follow-up, with no current or lifetime SUD at baseline. To investigate the influence of remission from BPD upon the occurrence of new onsets of SUD, we divided the BPD subgroup into stably remitted and non-remitted patients after 2 years of follow-up. Stable remission from BPD was defined as less than 2 BPD criteria for a period of at least 12 months in the second year of follow-up.
Procedures
All participants signed or written informed consent, following a full explanation of the study. Clinically experienced interviewers trained to pay particular attention to distinguishing Axis I mental state conditions from Axis II personality trait phenomena interviewed subjects who screened positive for the four targeted personality disorders with the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P) (45) and the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) (46). The participants were evaluated again at 6, 12, 24, 36, 48, 60, 72 and 84 months with a follow-along version of the DIPD (DIPD-FAV) that records monthly variations in BPD criteria (47), and the Longitudinal Interval Follow-up Evaluation (LIFE) (48) that records weekly variations in DSM-IV SUD criteria.
The DIPD-FAV (47) was used to determine criteria-based outcome. It provided a record of the presence of BPD crieria for each month of the follow-up period. The follow-along reliability showed that the correlations between new raters for the number of borderline criteria (mean range 0.71-0.92), and the correlation of new raters with original raters (mean range 0.75-0.94), was similar. Reliability for retrospective reporting on the DIPD-FAV was found to be good, with kappa scores ranging from 0.68 to 0.78 (42).
The LIFE (48) is a semistructured interview rating system which assesses the longitudinal course of Axis I disorders. Good to excellent reliability has consistently been demonstrated for the LIFE (49).
Analyses
All statistical analyses were performed with SPSS/15.0 for Windows. The Kaplan-Meier product-limit technique (50) was used to generate time to new onset curves. A probability of p < 0.05 was defined as the level of significance.
Results
SUD at baseline
Table 1 shows the frequency of current and lifetime substance use disorders (SUD) for BPD and the other personality disorders (OPD) at baseline. The rate for alcohol use disorder and drug use disorder was 52.0% and 54.9% respectively in the BPD group, and 38.4% and 30.6% in the OPD group. Whereas BPD patients had a significantly higher rate of both alcohol dependence and drug dependence than OPD patients, they were not more apt to have alcohol and drug abuse.
Table 1.
Frequency and percentage of co-occurrence of current and lifetime substance use disorder (SUD) in patients with personality disorder at baseline
| SUD | BPD
(n=175) |
OPD
(n=396) |
p |
|---|---|---|---|
| n (%) | n (%) | ||
| Alcohol use disorder | 91 (52.0) | 152 (38.4) | χ2 = 9.20, df = 1, p = 0.002 |
| Alcohol Abuse | 30 (17.1) | 52 (13.1) | χ2 = 1.59, df = 1, n.s. |
| - Current alcohol abuse | 6 (3.4) | 7 (1.8) | χ2 = 1.51, df = 1, n.s. |
| - Lifetime alcohol abuse | 24 (13.7) | 45 (11.4) | χ2 = 0.63, df = 1, n.s. |
| Alcohol Dependence | 61 (34.9) | 100 (25.3) | χ2 = 5.53, df = 1, p = 0.013 |
| Drug use disorder | 96 (54.9) | 121 (30.6) | χ2 = 30.42, df = 1, p < 0.0001 |
| Drug Abuse | 18 (10.3) | 29 (7.3) | χ2 = 1.41, df = 1, n.s. |
| - Current drug abuse | 4 (2.3) | 6 (1.5) | χ2 = 0.42, df = 1, n.s. |
| - Lifetime drug abuse | 14 (8.0) | 23 (5.8) | χ2 = 0.96, df = 1, n.s. |
| Drug Dependence | 78 (44.6) | 92 (23.2) | χ2 = 26.43, df = 1, p < 0.0001 |
BPD=Borderline Personality Disorder, OPD= Other Personality Disorder
New onsets of SUD
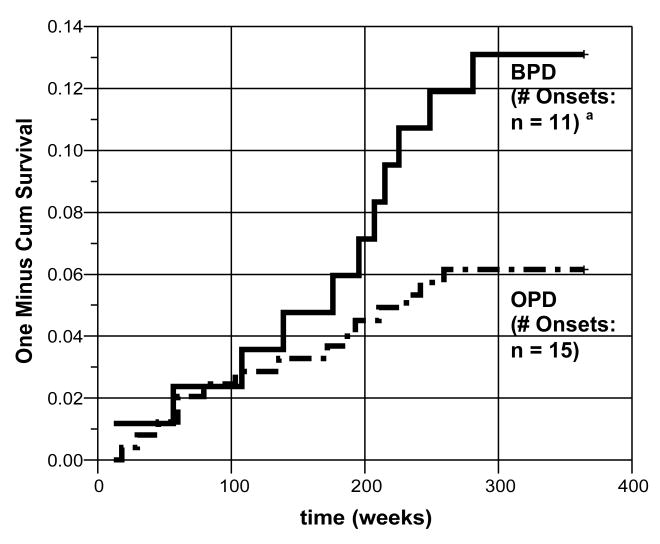
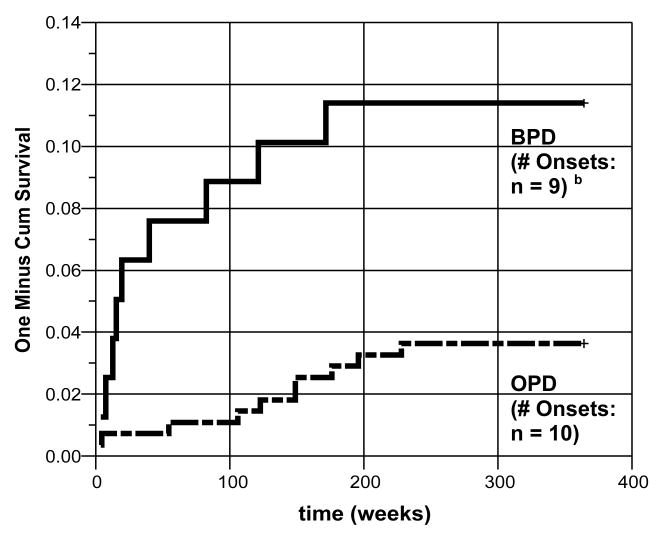
The 84 patients with BPD and 244 patients with OPD without a current or lifetime alcohol use disorder at baseline, and the 79 BPD patients and 275 OPD patients without a current or lifetime drug use disorder at baseline were investigated for new onsets of SUD during the 7 years of follow-up. New onsets of alcohol use disorder were 13% for BPD, and 6% for OPD patients. Omnibus chi-square analysis revealed that the groups differed significantly in time to new onsets of alcohol abuse/dependence (log-rank χ2 = 4.04, df = 1, p = 0.044) (Figure 1). As shown in Figure 2, the groups (BPD, OPD) also differed significantly in their time to new onset of drug use disorder (log-rank χ2 = 7.64, df = 1, p = 0.006): 11% (BPD), and 4% (OPD).
Figure 1. Time to new onsets of alcohol use disorder.
BPD = Borderline personality Disorder (n = 84). OPD = Other Personality Disorder (n = 244). a Significance difference between test conditions (log-rank χ2 = 4.04, df = 1, p = 0.044)
Figure 2. Time to new onsets of drug use disorder.
BPD = Borderline personality Disorder (n = 79). OPD = Other Personality Disorder (n = 275). b Significance difference between test conditions (log-rank χ2 = 7.64, df = 1, p = 0.006)
New onsets of SUD in remitted vs. non-remitted BPD
After two years of follow-up, 85 BPD patients (48.6%) showed a stable remission from their BPD diagnosis, whereas 90 BPD patients (51.4%) did not. The co-occurring SUDs for the two groups at baseline are shown in Table 2. The remitted BPD patients had a significantly higher frequency of drug use disorder at baseline than the BPD patients who do not have remissions. The frequency of alcohol use disorder and any SUD at baseline in remitted and non-remitted BPD patients did not differ. As shown in Table 2, there were no significant differences in the new onset rates of SUD between remitted and non-remitted BPD groups.
Table 2.
Frequency and percentage of SUD in stably-remitted vs. non-remitted BPD
| SUD | Remitted BPD
(n=85) |
Non-Remitted BPD
(n=90) |
p |
|---|---|---|---|
| n (%) | n (%) | ||
| Baseline: | |||
| Alcohol use disorder | 36 (42.4) | 31 (34.4) | χ2 = 1.16, df = 1, n.s. |
| Drug use disorder | 48 (56.5) | 36 (40.0) | χ2 = 6.13, df = 1, p = 0.013 |
| Follow-up: | |||
| New onsets of SUD | 3 (13.0) | 13 (24.2) | log-rank χ2 = 0.97, df = 1, n.s. |
BPD=Borderline Personality Disorder
Discussion
This is the first study, to our knowledge, to examine the new onsets of alcohol use disorder (AUD) and drug use disorder (DUD) in patients with borderline personality disorder (BPD). Consistent with previous findings (5), we found that the prevalence rates of AUD and DUD in BPD at baseline was significantly higher than in OPD -- a result that was biased by the absence of the other cluster B disorder, antisocial personality disorder, that has even higher rates of SUD (51, 52). This report notes, in addition, that the BPD patients showed a higher prevalence rate in alcohol and drug dependence than the OPD patients, but not in alcohol and drug abuse, suggesting that SUD in BPD patients is more severe than in OPDs. This conclusion is consistent with prior reports where severe substance use problems has been associated with BPD and ASPD more than with any other personality disorder (53-55).
The main finding that the rates of new onsets of AUD is more than two times higher and of DUD is more than three times higher in BPD than in OPD. This confirms that BPD patients have particularly high vulnerability for the development of SUDs over the course of time. Our finding that new onsets of SUD does not differ significantly between remitted and non-remitted BPD patients adds to the impression of shared etiological factors between BPD and SUD. This conclusion is consistent other studies which have shown that adolescents with a Cluster B personality disorder have an increased risk of SUD in adulthood (56, 57), and that a higher BPD criterion count is associated with early-onset of SUD (58).
Although these findings suggest that SUDs share underlying pathologies with BPD, (i.e., have a spectrum relationship), we could not rule out the possibility that other comorbid Axis I disorders -- most notably, mood disorders -- may have influenced the new onsets of SUD. However, the baseline comorbidity of major depressive disorder (MDD) and bipolar disorder were only moderately higher for BPD than for OPD (59, 60). Moreover, in other CLPS reports, we found that BPD patients fail to have higher rates of new onsets for MDD (61), and they have only a slightly higher rates of new onsets of bipolar disorders than do CLPS patients with OPD (60). It is also possible that these BPD patients with higher rates of new onsets of SUD are a BPD subgroup whose vulnerability reflects a higher level of impulsivity (62) than other BPD patients. Use of neurobiological measures for impulsivity that could shed light on whether that mechanism is present could add to future studies. Because our samples was restricted to four personality disorders, we could not examine rates of new onsets of SUDs in other personality disorders, particularly ASPD. Furthermore our findings are limited by a lack of information as to which specific substances were used, no information of stressful life events during the follow-up period which could influence the onsets of SUD and because of the limited sample sizes for assessing the role of remission in later years. Each of these limitations identify important questions that future studies will need to answer.
These limitations notwithstanding, we think our results retain some significant clinical implications. Continued substance dependence is a formidable resistance to treatment of BPD and is associated with a poor outcome (63-65). Remission of SUD sometimes is followed by remission of BPD (66). For these reasons from a clinical point of view we believe that when substance abuse is comorbid with BPD, it should become a priority in treatment planning (1). Our finding that remitted BPD patients have a rate of new onsets of SUD as high as non-remitted patients points out the clinical importance of sustained attention to this risk. Clinicians should recognize that specific psychotherapeutic strategies have been developed to treat the interrelated symptoms of substance abuse and co-occurring personality disorders (67, 68) and specifically for treating BPD patients with comorbid substance abuse (69, 70).
This is the first examination of new onsets of alcohol use disorder and drug use disorder in BPD patients in a prospective longitudinal design with adequate sample size. It establishes that BPD patients -- even when remitted -- seem to have a higher vulnerability than patients with other personality disorders -- with the likely exception of ASPD -- for the development of a SUD. This conclusion is consistent with both the concept of a spectrum relationship and with the clinical wisdom that substance abuse is a particularly hazardous form of comorbidity for patients with BPD.
Acknowledgments
This work was funded by the National Institute of Mental Health (NIMH)
Award sites include Brown University Department of Psychiatry and Human Behavior (MH50837), Columbia University College of Physicians and Surgeons and New York State Psychiatric Institute (MH50839), Harvard Medical School and McLean Hospital (MH50840), Texas A&M University (MH50838), Yale University School of Medicine (MH50850) and MH073708 (Dr. Sanislow). This manuscript has been reviewed and approved by the Publications Committee of the Collaborative Longitudinal Personality Disorders Study.
References
- 1.Gunderson JG, Links PS. Borderline personality disorder. A clinical guide. Second. Washington DC: American Psychiatric Press; 2008. [Google Scholar]
- 2.Akiskal HS, Chen SE, Davis GC, Puzantian VR, Kashgarian M, Bolinger JM. Borderline: An adjective in search for a noun. J Clin Psychiatry. 1985;46:41–48. [PubMed] [Google Scholar]
- 3.Akiskal HS. The temperament borders of affective disorders. Acta Psychiatr Scand. 1994;89:S32–S37. doi: 10.1111/j.1600-0447.1994.tb05815.x. [DOI] [PubMed] [Google Scholar]
- 4.Oldham JM, Skodol AE, Kellman HD, Hyler SE, Doidge N, Rosnick L, et al. Comorbidity of Axis I and Axis II disorders. Am J Psychiatry. 1995;152:571–578. doi: 10.1176/ajp.152.4.571. [DOI] [PubMed] [Google Scholar]
- 5.McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, et al. The Collaborative Longitudinal Personality Disorder Study: baseline axis I/II and II/II diagnosis co-occurrence. Acta Psychiatr Scand. 2000;102:256–264. doi: 10.1034/j.1600-0447.2000.102004256.x. [DOI] [PubMed] [Google Scholar]
- 6.Dolan-Sewell RT, Krueger RF, Shea MT. Co-occurrence with syndrome disorders. In: Livelsey WJ, editor. Handbook of personality disorders. New York: Guilford Press; 2001. pp. 84–104. [Google Scholar]
- 7.Shea MT, Stout RL, Yen S, Pagano M, Skodol A, Morey LC, et al. Associations in the course of personality disorders and Axis I disorders over time. J Abnorm Psychol. 2004;113:499–508. doi: 10.1037/0021-843X.113.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tyrer P, Gunderson J, Lyons M, Tohen M. Special feature: Extent of comorbidity between mental state and personality disorders. J Personal Disord. 1997;11:242–259. doi: 10.1521/pedi.1997.11.3.242. [DOI] [PubMed] [Google Scholar]
- 9.Skodol AE, Oldham JM, Gallaher PE. Axis II comorbidity of substance use disorders among patients referred for treatment of personality disorders. Am J Psychiatry. 1999;156:733–738. doi: 10.1176/ajp.156.5.733. [DOI] [PubMed] [Google Scholar]
- 10.Trull TJ, Sher KJ, Minks-Brown C, Durbin J, Burr R. Borderline personality disorder and substance use disorders. Clin Psychol Rev. 2000;20:235–253. doi: 10.1016/s0272-7358(99)00028-8. [DOI] [PubMed] [Google Scholar]
- 11.Grilo CM, Martino S, Walker ML, Becker DF, Edell WS, McGlashan TH. Controlled study of psychiatric comorbidity in psychiatrically hospitalized young adults with substance use disorders. Am J Psychiatry. 1997;154:305–1307. doi: 10.1176/ajp.154.9.1305. [DOI] [PubMed] [Google Scholar]
- 12.Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry. 1998;155:1733–1739. doi: 10.1176/ajp.155.12.1733. [DOI] [PubMed] [Google Scholar]
- 13.Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6 year follow-up and prediction of time to remission. Am J Psychiatry. 2004;161:2108–2114. doi: 10.1176/appi.ajp.161.11.2108. [DOI] [PubMed] [Google Scholar]
- 14.Links PS, Heslegrave RJ, Mitton JE, Van Reekum R, Patrick J. Characteristics of borderline personality disorder: A Canadian study. Can J Psychiatry. 1995;33:336–354. doi: 10.1177/070674379504000105. [DOI] [PubMed] [Google Scholar]
- 15.Yen S, Shea MT, Pagano M, Sanislow CA, Grilo CM, McGlashan TH, et al. Axis I and axis II disorders as predictors of prospective suicide attemps: findings from the collaborative longitudinal personality disorders study. J Abnorm Psychol. 2003;112:375–381. doi: 10.1037/0021-843x.112.3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merikangas KR, Stolar M, Stevens DE, Goulet J, Preisig MA, Fenton B, et al. Familial transmission of substance use disorders. Arch Gen Psychiatry. 1998;55:973–979. doi: 10.1001/archpsyc.55.11.973. [DOI] [PubMed] [Google Scholar]
- 17.Miles DR, Stallings MC, Young SE, Hewitt JK, Crowley TJ, Fulker DW. A family history and direct interview study of familial aggregation of substance abuse. Drug Alcohol Depend. 1998;49:105–114. doi: 10.1016/s0376-8716(97)00156-7. [DOI] [PubMed] [Google Scholar]
- 18.White CN, Gunderson JG, Zanarini MC, Hudson JI. Family studies of borderline personality disorder: a review. Harv Rev Psychiatry. 2003;11:8–19. doi: 10.1080/10673220303937. [DOI] [PubMed] [Google Scholar]
- 19.Zanarini MC. BPD as an impulsive spectrum disorder. In: Paris J, editor. Borderline personality disorder: Etiology and treatment. Washington, DC: American Psychiatric Press; 1993. pp. 67–85. [Google Scholar]
- 20.Links PS, Heslegrave R, van Reekum R. Impulsivity: Core aspect of borderline personality disorder. J Personal Disord. 1999;12:1–9. doi: 10.1521/pedi.1999.13.1.1. [DOI] [PubMed] [Google Scholar]
- 21.Siever LJ, Davis KL. A psychobiological perspective on the personality disorder. Am J Psychiatry. 1991;148:1647–1658. doi: 10.1176/ajp.148.12.1647. [DOI] [PubMed] [Google Scholar]
- 22.Pickens RW, Svikis DS, McGue M, LaBudaa MC. Common genetic mechanism in alcohol, drug, and mental disorder comorbidity. Drug Alcohol Depend. 1995;39:129–138. doi: 10.1016/0376-8716(95)01151-n. [DOI] [PubMed] [Google Scholar]
- 23.Grove WM, Eckert ED, Heston L, Bouchard TJ, Jr, Segal N, Lykken DT. Heritability of substance abuse and antisocial behavior: A study of monozygotic twins reared apart. Biol Psychiatry. 1990;27:1293–1304. doi: 10.1016/0006-3223(90)90500-2. [DOI] [PubMed] [Google Scholar]
- 24.Health AC, Cloninger CR, Martin NG. Testing a model for the genetic structure of personality: a comparison of the personality systems of Cloninger and Eysenck. J Pers Soc Psychol. 1994;66:762–775. doi: 10.1037//0022-3514.66.4.762. [DOI] [PubMed] [Google Scholar]
- 25.Howard MO, Kivlahan D, Walker RD. Cloninger's tridemensional theory of personality and psychopathology: applications to substance use disorder. J Stud Alcohol. 1997;58:48–66. doi: 10.15288/jsa.1997.58.48. [DOI] [PubMed] [Google Scholar]
- 26.Slutske WS, Heath AC, Dinwiddie SH, Madden PA, Buchholz KK, Dunne MP, et al. Common genetic risk factors for conduct disorder and alcohol dependence. J Abnorm Psychol. 1998;107:363–374. doi: 10.1037//0021-843x.107.3.363. [DOI] [PubMed] [Google Scholar]
- 27.Krueger RF. The structure of common mental disorder. Arch Gen Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 28.Johnson BA, Brent DA, Connolly J, Bridge J, Matta J, Constantine D, et al. Familial aggregation of adolescent personality disorders. J Am Acad Adol Psychiatry. 1995;34:798–804. doi: 10.1097/00004583-199506000-00021. [DOI] [PubMed] [Google Scholar]
- 29.Pope HG, Jr, Jonas HM, Hudson JI, Cohen BM, Gunderson JG. The validity of DSM-III borderline personality disorder. A phenomenologic, family history, treatment response, and long-term follow-up study. Arch Gen Psychiatry. 1983;40:23–30. doi: 10.1001/archpsyc.1983.01790010025003. [DOI] [PubMed] [Google Scholar]
- 30.Loranger AW, Tulis EH. Family history of alcoholism in borderline personality disorder. Arch Gen Psychiatry. 1985;42:153–157. doi: 10.1001/archpsyc.1985.01790250047006. [DOI] [PubMed] [Google Scholar]
- 31.Silverman JM, Pinkham L, Horvarth TB, Coccaro EF, Klar H, Schear S, et al. Affective and impulsive personality disorder traits in the relatives of patients with borderline personality disorder. Am J Psychiatry. 1991;148:378–1385. doi: 10.1176/ajp.148.10.1378. [DOI] [PubMed] [Google Scholar]
- 32.Riso LP, Klein DN, Anderson RL, Ouimette PC. A family study of outpatients with borderline personality disorder and no history of mood disorder. J Personal Disord. 2000;14:208–217. doi: 10.1521/pedi.2000.14.3.208. [DOI] [PubMed] [Google Scholar]
- 33.Jang KL, Vernon PA, Livesley WJ. Personality disorder traits, family environment, and alcohol misuse: a multivariate behavioural genetic analysis. Addiction. 2000;95:873–888. doi: 10.1046/j.1360-0443.2000.9568735.x. [DOI] [PubMed] [Google Scholar]
- 34.Simeon D, Knutelska M, Smith L, Baker BB, Hollander E. A preliminary study of cortisol and norepinephrine reactivity to psychosocial stress in borderline personality disorder with high and low dissociation. Psychiatry Res. 2007;149:177–184. doi: 10.1016/j.psychres.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 35.Walter M, Bureau JF, Holmes B, Bertha EA, Hollander M, Wheelis J, et al. Cortisol response to interpersonal stress in young adults with borderline personality disorder: a pilot study. Eur Psychiatry. 2008;23:201–204. doi: 10.1016/j.curpsy.2007.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pagano ME, Skodol AE, Stout RL, Shea MT, Yen S, Grilo CM, et al. Stressful life events as predictors of functioning: findings from the Collaborative Longitudinal Personality Disorders Study. Acta Psychiatr Scand. 2004;110:421–429. doi: 10.1111/j.1600-0447.2004.00398.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Le Moal M, Koob GF. Drug addiction: pathways to the disease and pathophysiological perspectives. Eur Neuropsychopharmacol. 2007;17:377–393. doi: 10.1016/j.euroneuro.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 38.Walter M, Wiesbeck GA, Bloch N, Aeschbach S, Olbrich HM, Seifritz E, et al. Psychobiological responses to drug cues before and after methadone intake in heroin-dependent patients: a pilot study. Eur Neuropsychopharmacol. 2008;18:390–393. doi: 10.1016/j.euroneuro.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 39.Brown SA, Vik PW, Patterson TL, Grant I, Schuckit MA. Stress, vulnerability and adult alcohol relapse. J Stud Alcohol. 1995;56:538–545. doi: 10.15288/jsa.1995.56.538. [DOI] [PubMed] [Google Scholar]
- 40.Vielva I, Iraurgi I. Cognitive and behavioural factors as predictors of abstinence following treatment for alcohol dependence. Addiction. 2001;96:297–303. doi: 10.1046/j.1360-0443.2001.96229713.x. [DOI] [PubMed] [Google Scholar]
- 41.Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Prediction of the 10-year course of borderline personality disorder. Am J Psychiatry. 2006;163:827–832. doi: 10.1176/ajp.2006.163.5.827. [DOI] [PubMed] [Google Scholar]
- 42.Skodol AE, Pagano ME, Bender DS, Shea MT, Gunderson JG, Yen S, et al. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder over two years. Psychol Med. 2005;35:443–451. doi: 10.1017/s003329170400354x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gunderson JG, Shea MT, Skodol EA, McGlashan TH, Morey LC, Stout RI, et al. The Collaborative Longitudinal Personality Disorders Study I: development, aims, design, and sample characteristics. J Personal Disord. 2000;14:300–315. doi: 10.1521/pedi.2000.14.4.300. [DOI] [PubMed] [Google Scholar]
- 44.Morey LC. A comparison of three personality assessment approaches. J Psychopathol Behav Assess. 1986;8:25–30. [Google Scholar]
- 45.First MB, Spitzer RL, Gibbon M, William JBW. Structered Clinical Interview for DSM-IV Axis I Disorders/Patient Edition (SCID-I/P) New York: New York State Psychiatric Institute, Biometrics Research Department; 1996. [Google Scholar]
- 46.Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) Belmont: McLean Hospital; 1996. [Google Scholar]
- 47.Zanarini MC, Shea MT. The Diagnostic Interview for DSM-IV Personality Disorders - Follow-along Version (DIPD-IV-FA) Belmont: McLean Hospital; 1996. [Google Scholar]
- 48.Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, et al. The Longitudinal Interval Follow-Up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 49.Warshaw M, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term psychiatric study: An ongoing interrater reliability monitoring program using the Longitudinal Interval Follow-up Evaluation. J Psychiatr Res. 2001;35:297–305. doi: 10.1016/s0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- 50.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 51.Goldstein RB, Dawson DA, Daha TD, Ruan J, Compton WM, Grant BF. Antisocial behavioral syndroms and DSM-IV alcohol use disorders: results from the national epidemiologic survey on alcohol and related conditions. Alc Clin Exp Res. 2007;31:814–828. doi: 10.1111/j.1530-0277.2007.00364.x. [DOI] [PubMed] [Google Scholar]
- 52.Goldstein RB, Compton WM, Pulay AJ, Ruan WJ, Pickering RP, Stinson FS, Grant BF. Antisocial behavioral syndroms and DSM-IV drug use disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Drug Alcohol Depend. 2007;90:145–158. doi: 10.1016/j.drugalcdep.2007.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morgenstern J, Labouvie E, McCrady BS, Kahler CW, Frey RM. Affiliation with Alcoholics Anonymous after treatment: a study of its therapeutic effects and mechanisms of action. J Consult Clin Psychol. 1997;65:768–777. doi: 10.1037//0022-006x.65.5.768. [DOI] [PubMed] [Google Scholar]
- 54.Bottlender M, Preuss UW, Soyka M. Association of personality disorder with type A and type B alcoholics. Eur Arch Psychiatry Clin Neurosci. 2006;265:55–61. doi: 10.1007/s00406-005-0601-y. [DOI] [PubMed] [Google Scholar]
- 55.Grilo CM, Becker DF, Fehon DF, Edell WS, McGlashan TH. Conduct disorder, substance use disorders, and co-existing conduct and substance use disorders in adolescent inpatients. Am J Psychiatry. 1996;153:914–920. doi: 10.1176/ajp.153.7.914. [DOI] [PubMed] [Google Scholar]
- 56.Johnson JG, Cohen P, Skodol AE, Oldham JM, Kasen S, Brook JS. Personality disorders in adolescence and risk of major mental disorders and suicidality during adulthood. Arch Gen Psychiatry. 1999;56:805–811. doi: 10.1001/archpsyc.56.9.805. [DOI] [PubMed] [Google Scholar]
- 57.Cohen P, Chen H, Crawford TN, Brook JS, Gordon K. Personality disorders in early adolescence and the development of later substance use disorders in the general population. Drug Alcohol Depend. 2007;88:S71–S84. doi: 10.1016/j.drugalcdep.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Franken IHA, Hendriks VM. Early-onset of illicit substance use is associated with greater axis-II comorbidity, not with axis-I comorbidity. Drug Alcohol Depend. 2000;59:305–308. doi: 10.1016/s0376-8716(99)00132-5. [DOI] [PubMed] [Google Scholar]
- 59.Verheul R, Kranzler HR, Poling J, Tenne H, Ball S, Rounsaville BJ. Co-occurrence of Axis I and Axis II disorders in substance abusers. Acta Psychiatr Scand. 2000;101:110–118. doi: 10.1034/j.1600-0447.2000.90050.x. [DOI] [PubMed] [Google Scholar]
- 60.Gunderson JG, Weinberg I, Daversa MT, Kueppenbender KD, Zanarini MC, Shea MT, et al. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163:1173–1178. doi: 10.1176/ajp.2006.163.7.1173. [DOI] [PubMed] [Google Scholar]
- 61.Gunderson JG, Stout RL, Sanislow CA, Shea MT, McGlashan TH, Zanarini MC, et al. New episodes and new onsets of major depression in borderline and other personality disorders. submitted, under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bornovalova MA, Lejuez CW, Daughters SB, Rosenthal MZ, Lynch TR. Impulsivity as a common process across borderline personality and substance use disorders. Clin Psychol Rev. 2005;25:790–812. doi: 10.1016/j.cpr.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 63.Dawson DA, Grant BF, Stinson FS, Chou PC, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001-2002. Addiction. 2005;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- 64.Verheul R. Co-morbidity of personality disorders in individuals with substance use disorders. Eur Psychiatry. 2001;16:274–282. doi: 10.1016/s0924-9338(01)00578-8. [DOI] [PubMed] [Google Scholar]
- 65.Galen LW, Brower KJ, Gillespie BW, Zucker RA. Sociopathy, gender, and treatment outcome among outpatient substance abusers. Drug Alcohol Depend. 2000;61:23–33. doi: 10.1016/s0376-8716(00)00125-3. [DOI] [PubMed] [Google Scholar]
- 66.Gunderson JG, Bender D, Sanislow C, Yen S, Rettew Bame J, Dolan-Sewell R, et al. Plausibility and possible determinants of sudden “remissions” in borderline patients. Psychiatry. 2003;66:111–119. doi: 10.1521/psyc.66.2.111.20614. [DOI] [PubMed] [Google Scholar]
- 67.Ball SA, Cobb-Richardson P, Connolly AJ, Bujosa CT, O'Neall TW. Substance abuse and personality disorders in homeless drop-in center clients: symptom severity and psychotherapy retention in a randomized clinical trail. Compr Psychiatry. 2005;46:371–379. doi: 10.1016/j.comppsych.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 68.Ball SA. Comparing individual theapies for personality disordered opioid dependent patients. J Personal Disord. 2007;21:305–321. doi: 10.1521/pedi.2007.21.3.305. [DOI] [PubMed] [Google Scholar]
- 69.Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, et al. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug Alcohol Depend. 2002;67:13–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- 70.Gregory RJ, Remen AL. A manual-based psychodynamic therapy for treatment-resistant borderline personality disorder. Psychother Theor Res Pract Train. 2008;45:15–27. doi: 10.1037/0033-3204.45.1.15. [DOI] [PubMed] [Google Scholar]