Abstract
The states of Oregon and Washington both provide methadone maintenance treatment (MMT) services though a modest number of clinics. More than 10,000 clients in each state were followed for 3 years after an initial admission for opiate use between 1993 and 2000. Medicaid clients in both states had far greater access to MMT than their non-Medicaid counterparts, controlling for differences in client characteristics using propensity scores. Months in MMT were associated with much lower arrest rates than time not in treatment, but unexpectedly this was only true for clients participating in MMT for many months. Despite differences in the treatment systems for opiate addiction in these two states observed in previous studies, the current findings generalized across both states.
Keywords: Methadone, Substance Abuse, Arrests, Opiate Treatment
INTRODUCTION
Numerous studies have shown a persistent link between opiate use and criminal behavior.1-3 Importantly, much of this research has also indicated that treatment for opiate addiction can reduce criminal activity. Methadone maintenance treatment (MMT) programs in particular have been shown to be effective in reducing arrests among opiate users. However, gaining access to methadone treatment and managing the fees associated with the treatment may be difficult for many clients. Indeed, many rely on public funding to pay for treatment and in many states Medicaid is the primary payer for publicly funded opiate treatment. The role of Medicaid coverage in promoting access to treatment and treatment outcomes, however, has been minimally addressed in the substance abuse treatment literature. In the current paper we examine the role of Medicaid in providing for MMT services and the subsequent relationship of arrests to sustained MMT episodes in two states.
Background and Prior Studies
Oregon is one of only 25 states that include methadone maintenance in the Medicaid benefit.4 Medicaid eligibility was expanded in Oregon in 1994 through a section 1115 waiver. A prioritized list of covered services and a shift to managed care were used to help pay for the expansion. This series of changes became known as the Oregon Health Plan. The Medicaid eligible population more than doubled as a result. Moreover, the combined effect of the expansion and managed care led to a dramatic increase in the number of opiate users enrolled in methadone maintenance programs after 19945 and was associated with increases in retention rates.6,7
Unfortunately, an unprecedented budget deficit in 2002 prompted the state legislature to remove substance abuse and mental health treatment from the Medicaid benefit for this expansion group effective March, 2003. Furthermore, the state strengthened cost sharing measures by stepping up enforcement of premium payments, dropping the no-income waivers that had exempted many from the premiums, and adding modest co-payments. The immediate impact of these changes was strongly felt by the 100,000 adults enrolled in the OHP expansion group and by the community treatment systems for substance abuse and mental health that rely heavily on public funding. While a significant number of those who were enrolled in opiate treatment when the benefit cut took effect elected to continue their treatment by paying out of pocket, methadone admissions dropped precipitously; admissions in 2003 were only 26% of those in 2002. While disenrollment from Medicaid accounted for some of this drop, the extent of the decline was much greater than can be explained by disenrollment alone. Moreover, opiate users presenting for publicly funded treatment after the change were less than half as likely to be placed in an opiate treatment program compared to the prior year. In addition, those with a recent treatment history were more likely to present for treatment after the benefit change than those who had not been in treatment recently.7 Although research on the impact of Oregon's Health Plan has shown effects on both access to MMT programs and retention in MMT, treatment outcomes among this population have not been examined.
The state of Washington is geographically and demographically very similar to Oregon. Washington, however, provides state administered substance abuse services and reimburses providers for treatment services to Medicaid recipients on a fee-for-service basis. Although Washington provides full coverage for MMT, matching funds are scarce and legislation has limited the size and location of methadone clinics.
Arrests as a Treatment Outcome
Addiction to heroin is usually associated with an increase in criminal activity. The costs associated with criminal behavior among opiate users are a major concern to society. Deschenes, Anglin, and Speckart,1 for instance, analyzed data on a sample of 279 heroin addicts enrolled in methadone maintenance programs between 1978 and 1980 and found over 250,000 property crime-days and 6,251 arrests. The aggregate societal cost, including criminal justice and treatment costs was conservatively estimated at $85 million. In an earlier study, Ball and colleagues8 examined crime among 243 heroin addicts finding an accumulated average of 2,000 crime days each over 11 years, the most common crime being theft, followed by drug related offenses. Other research has indicated that criminal activity among opiate addicts varies with higher rates of property crime during periods of addiction9 and more arrests during periods of use than during periods of non-use.10 Similarly, research has shown that the percent of time committing crimes, the number of crime days per month, and income from crime all vary directly as a function of more or less narcotic use.2,11
Numerous studies have indicated that substance abuse treatment is effective in decreasing both substance use and criminal activities.12,13 National evaluations of treatment, including the Drug Abuse Reporting Program,14 the Treatment Outcome Prospective Study15 (TOPS), the National Treatment Improvement Evaluation Study16 (NTIES), and the Drug Abuse Treatment Outcome Study12 (DATOS) have documented decreases in opiate use and criminal involvement after treatment.12,17,18 Furthermore, longer retention in treatment is associated with more favorable outcomes.14,15,19 Compared to other modalities, methadone maintenance treatment (MMT) has been found to be an effective mode of treatment for reducing heroin use and criminal behaviors.18-22 These findings are echoed in DATOS where follow-up measures indicated a 69% decline in the number of weekly heroin users and a 52% decline in illegal activity.12
Methadone treatment is not only effective in reducing substance use and criminal behaviors, but is also a cost-effective form of treatment for opiate addiction,23 costing approximately $13 per day.24,25 Flynn and colleagues26 conducted a cost-benefit analysis using data on 394 methadone patients collected as part of the DATOS study. Their findings indicated that longer retention in treatment is associated with greater reductions in crime costs, providing evidence of significant returns on treatment investments. Other cost-benefit analyses have shown that every $1 spent on treatment reduces the costs of drug-related crime, criminal justice costs, and theft by $4 to $7.27
Nonetheless, an NIH expert panel noted that less than 20% of the estimated 600,000 opiate addicts were participating in methadone maintenance treatment programs. Individuals with more severe substance abuse problems tend not to have either private or public insurance.28,29 In the DATOS study, for instance, only 10% of the clients admitted to methadone treatment had private insurance.12 The lack of insurance to cover treatment may impact treatment retention. Garcia and colleagues,30 for instance, found that uninsured clients enrolled in a non-profit drug treatment program were 3.4 times less likely than others to complete treatment. These findings suggest that a majority of individuals seeking treatment must rely on either public funding or find a way to manage the fees on their own.
Researchers examining the consequences of terminating clients from methadone maintenance programs, either due to loss of funding for a clinic or loss of coverage for a client's treatment, have found that a majority of the clients are unable to pay out of pocket for methadone treatment.31 Most notably, when clients were forced to discontinue methadone treatment because of clinic closures, they were likely to return to heroin use and to be involved in criminal activities.31-33 These studies suggested that financial concerns played a major role in a client's ability to continue treatment. For instance, Rosenbaum, Murphy and Beck32 reported that implementing a client fee was associated with an increase in criminal activities, incarcerations, heroin use, and hospitalizations. Similarly, Anglin and colleagues33 found that among clients who were terminated from a publicly funded MMT program, only 43% were able to continue their treatment by transferring to a private methadone clinic. Another study examining the effects of closing publicly funded methadone clinics found that within 24 months 54% of the clients were using heroin and 73% had been rearrested.34
Current Study
The objective of the current study was to examine the role of Medicaid in promoting sustained MMT and the subsequent impact of sustained MMT on the likelihood of arrests. Administrative data sets from Oregon and Washington covering a 10 year period were utilized to address this issue. We hypothesized that Medicaid coverage significantly improves access to MMT and that months in MMT significantly reduces the likelihood of felony arrests.
METHODS
Design
This observational study takes a longitudinal perspective to examine how an individual's health coverage influences utilization of appropriate treatment services and how that treatment experience influences a desired outcome, namely a reduction in the likelihood of felony arrests. By restructuring administrative data sets into monthly records and linking client identifiers across data sets, the results reflect the presence or absence of Medicaid eligibility, treatment enrollment, and felony arrests for each individual at each time interval. By treating both the independent and dependent measures as time-varying, we can model the complexity of the naturally occurring patterns of coverage and treatment participation with some precision. Because individuals were not be randomly assigned to Medicaid or to a treatment modality, however, it was necessary to make adjustments for the pre-existing differences among the groups compared. Adjustment was feasible due to the availability of a rich description of client treatment admission characteristics and large sample sizes. The study addresses generalizability by replicating the analysis in samples from both Oregon and Washington, two neighboring states with similar demographics but differences in the financing of substance abuse treatment, especially for opiate addiction.
Sample
All adults presenting for publicly funded treatment for opiate problems between 1993 and 2000 in two neighboring states, were identified using state treatment databases. Parallel samples were drawn from Oregon's Client Process Monitoring System (CPMS) and Washington's Treatment and Assessment Report Generation Tool (TARGET). Institutional review board approval for the study was obtained in each state. There was no contact with clients.
Table 1 summarizes the admission characteristics for both state samples. Although Oregon is much less populous than its neighbor, the state was aggressive in expanding Medicaid eligibility and in funding opiate treatment5,6 so the sample sizes were more similar than might be expected. The two samples were very similar except that the Washington state sample was somewhat more diverse ethnically, more likely to be unemployed, and more likely to have cocaine or alcohol as a secondary drug problem. These modest differences were expected as Washington was more varied ethnically and implemented a special treatment program for the indigent.
TABLE 1.
Characteristics of Oregon and Washington adults presenting for publicly funded opiate treatment between 1993 and 2000.
| Characteristic | Oregon | Washington |
|---|---|---|
| Number | 11,356 | 15,577 |
| Mean age | 36 years | 36 years |
| Gender | ||
| Male | 58% | 58% |
| Female | 42% | 42% |
| Ethnicity | ||
| White, not Hispanic | 83% | 76% |
| Black, not Hispanic | 7% | 11% |
| Hispanic | 5% | 7% |
| Native American | 4% | 4% |
| Other | 1% | 2% |
| Not employed | 79% | 87% |
| Never married | 40% | 42% |
| Needle user at intake | 84% | 84% |
| Secondary drug problem reported | ||
| Cocaine | 27% | 44% |
| Alcohol | 31% | 41% |
| Mean years of opiate use | 13 years | 13 years |
Data Linkages
To match records across multiple data sets in this study, we developed Link King35 implemented in SAS. This software package was used to match client records linking on name, social security number, gender, and birth date. The software incorporated both probabilistic and deterministic linkage algorithms36 and provided for manual review of cases where the algorithms did not agree. The combined algorithms performed better than either alone.37 Special adaptations were made to handle a coded version of names in Oregon's treatment database. Within each state, the software was first used to unduplicate the substance abuse treatment records defining the sample and generate a unique study identifier. All other data sets were then matched to this data set. To protect confidentiality, state staff conducted the linkages and delivered de-identified data sets for analysis.
In addition to the substance abuse treatment data sets, we linked Medicaid eligibility records, mental health treatment records, quarterly employment records, death records, and welfare benefits. To determine if a client was lost to the study prior to the end of the 3 year observation period, the last observed date was derived from all available data sets. No monthly records were generated after the last date observed across all the listed data sets.
Measures
Time
Time was measured in months from the client's initial admission for opiate treatment during the observation period. To obtain parameter estimates at 12 months rather than at admission, time was centered at 12.
Period
Periods of implementation of the Oregon Health Plan were represented by binary indicators for early implementation (May, 1995, through May, 1998) and mature implementation (after May, 1998).
Medicaid
Medicaid eligibility status each month was determined from each state's Medicaid Management Information System (MMIS). A client was considered eligible in any month if enrolled 15 or more days.
Treatment
Enrollment in MMT and in outpatient drug-free treatment each month was derived from state treatment databases. Both Oregon's Client Process Monitoring System (CPMS) and Washington's Treatment and Assessment Report Generation Tool (TARGET) report the start and end dates and modality for each episode of publicly funded treatment. A client was considered in treatment if enrolled at least 14 days. Months enrolled in residential treatment were excluded from the data set because the opportunity to commit crime would be minimal in this controlled setting.
Felony arrests
Arrest data were obtained from the state police records in both states. Only felonies and gross misdemeanors were preserved in the analysis data because misdemeanors are not consistently reported across jurisdictions.
Propensity Score Adjustment
Propensity score analysis38-40 was used to control for selective factors that may have created a different client mix when comparing Medicaid and non-Medicaid groups or clients placed in MMT compared to other placement. The technique models treatment assignment with all observed covariates and generates a score that can be used for matching, stratification, or as a covariate where random assignment is not possible. At any propensity score, the treated and untreated groups will be well balanced on the observed covariates. The method has been widely used but only recently in addictions research.41,42
For this study, the initial treatment admission record provided a detailed description of client characteristics. Separate logistic regressions were run to predict initial Medicaid eligibility and placement in MMT. A conceptual model utilized in previous studies5,6 served to guide the selection of predictors that reflected predisposing, need, or enabling characteristics regarding treatment using a framework promoted by Andersen.43 The scores from these analyses were saved to serve as covariates in the subsequent analysis. However, the MMT propensity score was recoded into deciles and a squared term added due to the strongly curvilinear relationship with MMT enrollment.
Analysis
We applied generalized linear mixed models44,45 for the analysis. HLM 646 was used to estimate the effects of coverage and treatment using multilevel longitudinal regression models. A first model predicted the probability in a given month that the client would be enrolled in a MMT program. A second model predicted the probability that the client would have a felony arrest during the month. Parallel analyses were conducted with the Oregon and Washington samples. Because both outcome measures were binary, the logit link function and Laplace estimation were used.
To predict use of methadone services, the Level 1 model (Time) included the number of months since the initial admission centered at one year (T12 = Months - 12), enrollment in Medicaid that month (coded 0 or 1), and a time by Medicaid interaction. Periods of implementation of the Oregon Health Plan were represented by binary indicators for early implementation (May, 1995, through May, 1998) and mature implementation (after May, 1998). A piecewise term was added to model the greater enrollment in MMT during the first few months following the initial admission.
The Level 2 model (Person) included propensity scores predicting Medicaid eligibility and placement in MMT. Past history was represented by binary indicators of both MMT enrollment and felony arrests in the year prior to the index treatment admission. Stability of Medicaid enrollment was represented by the proportion of months that were Medicaid eligible.
To predict arrests, the Level 1 model substituted binary indicators of monthly participation in MMT and outpatient treatment plus their interaction with time for the Medicaid variable and interaction. The Level 2 model substituted the proportion of months in MMT and outpatient treatment for the Medicaid stability measure. An interaction term between the MMT propensity and proportion of months enrolled in MMT was added.
Predictors were added to an initial unconditional base model until no significant improvement in Akaike information criterion (AIC) was observed, maximizing the explained variance with the most parsimonious model. Insignificant predictors and cross-level interactions were dropped unless central to the hypotheses. Plots of predicted probabilities were compared to plots of the observed probabilities to check for overall model fit.
RESULTS
Propensity Scores
A propensity score analysis predicting initial eligibility for Medicaid was conducted for both the Oregon (χ2 = 886, df = 22, p < .001) and Washington (χ2 = 4481, df = 26, p < .001) samples. Oregon clients who were old, female, pregnant, or unemployed were more likely to be Medicaid eligible. Clients who were Hispanic, self referred or referred by the legal system, or had prior treatment experience were less likely to be Medicaid eligible. The pattern was similar for Washington clients but those with prior treatment experience were also more likely to be Medicaid eligible. Washington clients with a longer history or greater frequency of opiate use were less likely to be eligible.
A second propensity score analysis predicting initial placement into methadone maintenance was also conducted for the Oregon (χ2 = 3963, df = 28, p < .001) and Washington (χ2 = 4369, df = 30, p < .001) samples. In Oregon, a methadone placement was more likely for clients who were pregnant, needle users, long term opiate users, or prior methadone users. A methadone placement was less likely for clients who were young, Hispanic, living too far from the nearest clinic, unable to work, or homeless. Washington clients referred by a treatment agency, having co-occurring mental disorders, or presenting with alcohol problems were less likely to be placed in methadone. See Deck and Carlson5 for an extended discussion of factors predicting access to methadone in these two states.
Each propensity model was examined for overlap between the two groups across all quintiles of the propensity score. Balance of covariates was assessed by comparing the individual covariates and the mean propensity score within each quintile. Missing data was reduced by rerunning each model without the variables that contributed most to missing data. The predicted scores from both analyses were saved and later applied as person level covariates in the multilevel analyses.
Utilization of Methadone Maintenance
Table 2 summarizes multilevel analyses predicting the monthly probability of enrollment in a methadone maintenance program for Oregon and Washington while controlling for the propensity for Medicaid eligibility, propensity for methadone maintenance, and prior history of methadone enrollment. The odds of methadone enrollment at 12 months from initial admission were greater for clients with a high propensity for methadone placement, with a prior history of methadone, and with a high proportion of months in Medicaid.
TABLE 2.
Results of HLM models predicting monthly enrollment in methadone maintenance in Oregon and Washington.
| Oregon |
Washington |
|||||
|---|---|---|---|---|---|---|
| Coefficient | SE | OR | Coefficient | SE | OR | |
| Intercept | ||||||
| Intercept | -5.378*** | 0.018 | 0.00 | -7.853*** | 0.014 | 0.00 |
| Medicaid propensity | -2.711*** | 0.011 | 0.07 | -0.608*** | 0.013 | 0.54 |
| MMT propensity | 1.357*** | 0.005 | 3.88 | 0.828*** | 0.003 | 2.29 |
| Prior MMT history | 2.279*** | 0.059 | 9.76 | 2.254*** | 0.179 | 9.53 |
| Prior Arrest history | -0.633*** | 0.003 | 0.53 | -0.153*** | 0.002 | 0.86 |
| Stability (centered at 50%) | -0.327*** | 0.004 | 0.72 | 0.465*** | 0.028 | 1.59 |
| MMT propensity by Stability | 1.485*** | 0.021 | 4.42 | |||
| Medicaid slope | ||||||
| Intercept | 2.529*** | 0.017 | 12.55 | 2.384*** | 0.016 | 10.84 |
| MMT propensity | -0.295*** | 0.007 | 0.74 | |||
| Stability (centered at 50%) | 3.232 | 0.021 | 25.33 | 0.755 | 0.028 | 2.13 |
| T12 slope | ||||||
| Intercept | 0.047*** | 0.001 | 1.05 | 0.013*** | 0.001 | 1.01 |
| Medicaid propensity | 0.029 | 0.001 | 1.03 | |||
| MMT propensity | -0.024*** | 0.000 | 0.98 | -0.017*** | 0.000 | 0.98 |
| T12 by Medicaid | ||||||
| Intercept | -0.034*** | 0.001 | 0.97 | -0.005*** | 0.001 | 1.00 |
| MMT propensity | 0.004*** | 0.000 | 1.00 | -0.023*** | 0.001 | 0.98 |
| Period 1 slope | ||||||
| Intercept | -0.683*** | 0.011 | 0.51 | 0.250*** | 0.018 | 1.28 |
| Medicaid propensity | -1.571 | 0.018 | 0.21 | |||
| MMT propensity | -0.031*** | 0.005 | 0.97 | 0.030*** | 0.002 | 1.03 |
| Stability (centered at 50%) | 1.922 | 0.038 | 6.84 | |||
| Period 2 slope | ||||||
| Intercept | -0.065*** | 0.010 | 0.94 | 0.623*** | 0.018 | 1.86 |
| Medicaid propensity | -2.459 | 0.015 | 0.09 | |||
| MMT propensity | 0.117*** | 0.005 | 1.12 | 0.090*** | 0.002 | 1.09 |
| Stability (centered at 50%) | 2.730 | 0.038 | 15.34 | |||
| Period 1 by Medicaid | ||||||
| Intercept | 0.179*** | 0.014 | 1.20 | -0.442*** | 0.019 | 0.64 |
| MMT propensity | 0.108*** | 0.007 | 1.11 | |||
| Stability (centered at 50%) | -0.282 | 0.037 | 0.75 | |||
| Period 2 by Medicaid | ||||||
| Intercept | 0.356*** | 0.012 | 1.43 | -0.867*** | 0.020 | 0.42 |
| MMT propensity | 0.056*** | 0.006 | 1.06 | |||
| Stability (centered at 50%) | -0.406 | 0.035 | 0.67 | |||
| T12A slope | ||||||
| Intercept | -0.088*** | 0.002 | 0.92 | -0.150*** | 0.001 | 0.86 |
| T12A by Medicaid | ||||||
| Intercept | 0.060*** | 0.002 | 1.06 | 0.049*** | 0.002 | 1.05 |
The effect of Medicaid eligibility on methadone enrollment was strong in both states, with an odds ratio of nearly 13 in Oregon and over 10 in Washington. As expected, the odds of methadone enrollment was lower in Oregon during period 1 and period 2 relative to the baseline period as an influx of new clients under the Oregon Health Plan quickly filled available capacity. In contrast, the odds of enrollment increased slightly during period 1 and period 2 in the Washington sample. The interactions with Medicaid in period 1 and period 2 were significant for both states though in opposite directions.
The piecewise term T12a and its interaction with Medicaid were included to model the decline in the odds of methadone enrollment during the first year following the index treatment admission. This decline was primarily an artifact of the way the sample was selected and is of little substantive interest here.
The probability of methadone enrollment was significantly associated with many temporal and client factors and interactions, making it inappropriate to use any single point estimate as representative of the overall effect of Medicaid eligibility. Plotting the predicted probabilities for key effects, while holding less important effects constant, provided a useful illustration of the model. Figure 1 shows the cross-level interaction for proportion of months Medicaid eligible and the time-varying effect of months Medicaid eligible (solid lines) compared to months not eligible (dashed lines) for Oregon. The relationship is plotted separately for clients with high (75%, red lines) or low (25%, blue lines) proportion of months in Medicaid.
Figure 1.
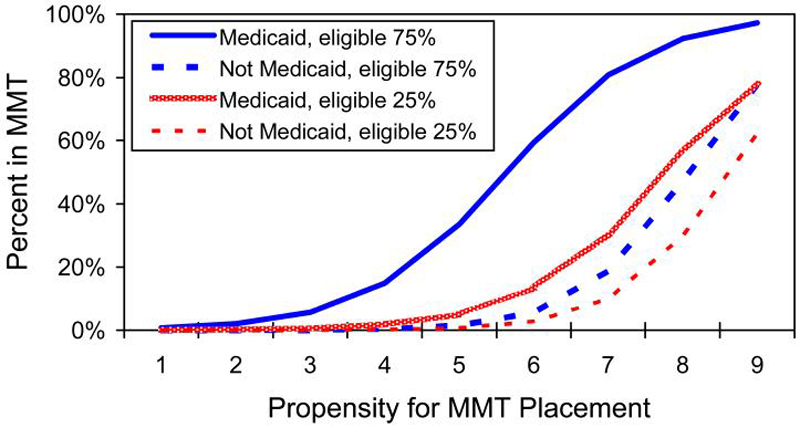
Predicted probability of methadone enrollment for Oregon clients during months Medicaid eligible (solid line) or not eligible (dashed line) for clients with high (blue lines) or low (red lines) proportion of months Medicaid eligible. Utilization is much higher in months of Medicaid eligibility as long as there is stable eligibility. However, low propensity clients are unlikely to get methadone regardless of Medicaid eligibility.
Not surprising, Medicaid coverage was a strong predictor of methadone enrollment, at least for clients with stable Medicaid eligibility. As Figure 1 shows, individuals in Oregon with highly stable eligibility (eligible 75% of months) were far more likely to be enrolled in methadone maintenance treatment (MMT) during months Medicaid eligible (blue solid line) than months not eligible (blue dashed line). Clients with low stability (eligible 25% of months), were somewhat more likely to be enrolled in MMT during months of Medicaid eligible (red solid line) than when not Medicaid eligible (red dashed line) but the differences was modest. The relationship held for most subgroups (1-9) defined by propensity for placement in methadone (an index derived from client demographics, severity of need, proximity to clinic, and other characteristics that predict the likelihood of placement in methadone apart from coverage). However, as expected, low propensity clients were unlikely to be placed in methadone regardless of coverage.
These relationships also generally held in the Washington data, though there were fewer clients with stable eligibility and less use of methadone overall. Even middle propensity clients were rarely placed in methadone when Medicaid eligible, though high propensity clients had greater utilization when Medicaid eligible.
Felony Arrests
Table 3 presents the results of multilevel model predicting the likelihood of a felony arrest in Oregon and Washington. The model was grand mean centered on the propensity for Medicaid eligibility and methadone enrollment. Prior arrest history was included as a covariate.
TABLE 3.
Results of HLM models predicting monthly probability of arrest in Oregon and Washington.
| Oregon |
Washington |
|||||
|---|---|---|---|---|---|---|
| Coefficient | SE | OR | Coefficient | SE | OR | |
| Intercept | ||||||
| Intercept | -4.215*** | 0.053 | 0.01 | -3.967*** | 0.051 | 0.02 |
| Medicaid propensity | -1.064*** | 0.136 | 0.35 | -0.603*** | 0.057 | 0.55 |
| MMT propensity | -0.003 | 0.007 | 1.00 | -0.015** | 0.005 | 0.98 |
| Prior arrest | 0.901*** | 0.043 | 2.46 | 0.886*** | 0.031 | 2.43 |
| Months MMT | -0.482*** | 0.105 | 0.62 | -0.099 | 0.102 | 0.91 |
| Months Outpatient | 0.293* | 0.145 | 1.34 | 0.015 | 0.102 | 1.02 |
| MMT slope | ||||||
| Intercept | -0.601*** | 0.086 | 0.95 | -0.777*** | 0.097 | 0.46 |
| Medicaid propensity | 0.066 | 0.307 | 1.07 | -0.007 | 0.181 | 0.99 |
| MMT propensity | -0.023 | 0.018 | 0.98 | |||
| Prior arrest | 0.074 | 0.091 | 1.08 | 0.403*** | 0.087 | 1.50 |
| Months MMT* | -1.177*** | 0.164 | 0.31 | -1.517*** | 0.163 | 0.22 |
| Outpatient slope | ||||||
| Intercept | -0.140 | 0.116 | 0.55 | -0.503*** | 0.101 | 0.60 |
| Medicaid propensity | 0.841** | 0.314 | 2.32 | 0.381** | 0.139 | 1.46 |
| MMT propensity | 0.022 | 0.015 | 1.02 | |||
| Prior arrest | -0.315** | 0.093 | 0.73 | -0.047 | 0.078 | 0.95 |
| Months Outpatient | -0.883** | 0.253 | 0.41 | -0.602** | 0.167 | 0.55 |
| T12 slope | ||||||
| Intercept | -0.007* | 0.003 | 1.00 | -0.004 | 0.003 | 1.00 |
| Medicaid propensity | -0.026** | 0.009 | 0.97 | 0.003 | 0.004 | 1.00 |
| MMT propensity* | 0.000 | 0.000 | 1.00 | |||
| Prior arrest | -0.021*** | 0.003 | 0.98 | -0.019*** | 0.002 | 0.98 |
| Months MMT | 0.008 | 0.005 | 1.01 | -0.00829 | 0.006 | 0.99 |
| Months Outpatient | -0.03169** | 0.009481 | 0.97 | -0.02243** | 0.006 | 0.98 |
At one year from the initial admission (T12 = 0), the likelihood of methadone enrollment was strongly associated with the methadone propensity score, prior history of methadone enrollment, and living in a county with no clinic. However, Medicaid eligibility in a particular month was associated with a much lower likelihood of arrest compared to non-Medicaid adults with similar characteristics in both states.
The log odds of methadone enrollment is significantly associated with many temporal and client factors and interactions, making it misleading to use any single point estimate as representative of the overall effect of Medicaid eligibility. However, plotting the predicted probabilities for key effects while holding less important effects constant provides a useful illustration of the model. Figure 2 illustrates the probability of arrest for the cross-level interaction of months in methadone maintenance (solid lines) and months untreated (dashed lines) and the proportion of months in methadone for clients with a prior arrest history (red lines) or no prior arrests (blue lines). For Oregon clients enrolled in methadone only a few months, the difference in probability of arrest was minimal. However, for clients enrolled in methadone for a majority of the observation period, the predicted probability of arrest was very low, even for clients with a prior arrest history.
Figure 2.
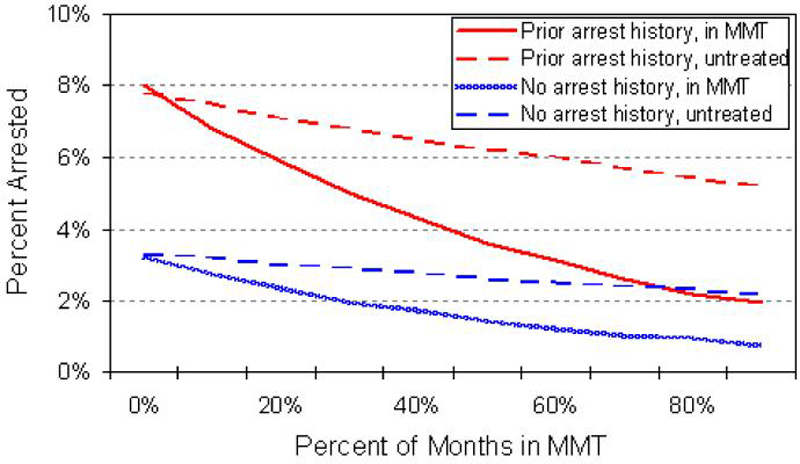
Predicted probability of a felony arrest in Oregon during months in methadone maintenance treatment (MMT, solid lines) compared to months untreated (dashed lines) by prior arrest history (red lines) or no history (blue lines). Arrests are much less likely as long as there is stable methadone enrollment.
To illustrate important implications of the model, Figure 2 shows the observed probability of felony or gross misdemeanor arrests in a given month for Oregon clients by treatment status for individuals with or without a prior history of arrest. Clients with at least one arrest in the year prior to the target treatment admission were about twice as likely to be arrested in a given month during the observation period. The probability of arrests was much lower during months in methadone maintenance treatment (solid line) compared to months untreated (dashed line). The red lines show results for individuals with a prior history of arrest (arrested at least once in the year prior to the initial opiate admission) and the blue lines show results for individuals with no arrests in the prior year.
The Washington model produced very similar results. Figure 3 shows a similar pattern in arrest rates. The probability of arrest is much lower during months in MMT than in months untreated, but again this relationship held only for clients with relatively stable MMT enrollment. A prior paper with a different sample in Washington also showed similar patterns.47
Figure 3.
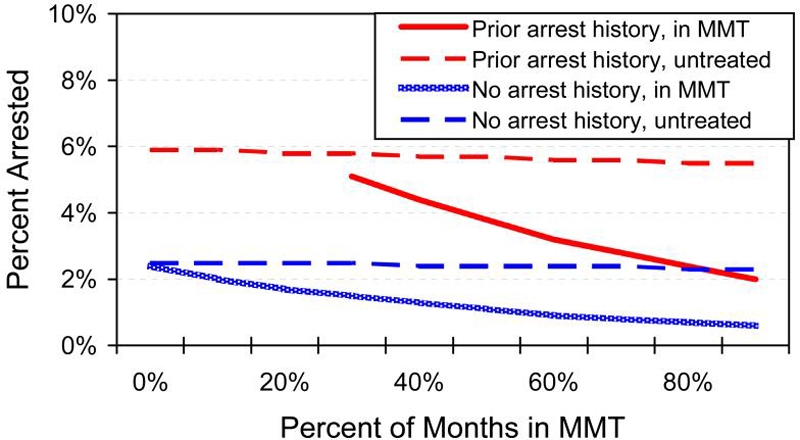
Predicted probability of a felony arrest in Washington during months in methadone maintenance treatment (MMT, solid line) compared to months untreated (dashed line) for clients with a prior arrest history (red lines) or no history (blue lines). As with Oregon, arrests are much less likely when enrolled in MMT as long as there is stable enrollment over time.
There were, however, a few minor differences in the two models. For example, in Oregon a higher proportion of months in MMT was associated with a lower probability of arrest. Outpatient clients with prior arrests had a smaller decline in arrests than their counterparts with no prior arrests. In Washington, MMT clients with a prior arrest history had a higher arrest rate than their counterparts with no prior arrest. These reflect some minor differences between the states, but do not change the overall findings.
DISCUSSION
This study examines the dramatic impact of Medicaid coverage on access to methadone maintenance services and the effect of methadone maintenance treatment in reducing felony arrests in 2 states. Despite state differences in the financing of substance abuse treatment explored in prior studies,5-7 the impact of methadone maintenance was very similar in these two states. From a client perspective, the results of this study suggest that Medicaid coverage had a dramatic impact on access to care for individuals addicted to opiates. Future research should pay more attention to Medicaid coverage, both as a vehicle for promoting access to publicly funded treatment and as an individual covariate.
Importance of Coverage
In both states, Medicaid eligibility was strongly associated with enrollment in methadone maintenance treatment programs. The results of this study are consistent with prior studies that focused on a single episode of care,6 but in this study we could also examine the additive effect of stable coverage.
Medicaid coverage in a given month was a strong predictor of enrollment in a methadone program in both states. Because we took a longitudinal approach, we can estimate arrest rates for months that the same client is in and out of opiate treatment. Although high propensity clients were much more likely to enroll in methadone than low propensity clients, clients were more likely to enroll at all levels of methadone propensity when Medicaid eligible.
Like other chronic medical conditions, stable medical coverage was critical to ensure that low income clients had access to the most appropriate form of treatment was critical for poor individuals. These individuals generally have little means to pay for continued treatment out of pocket. While both Oregon and Washington states offer some opiate treatment paid by other funding streams, Medicaid continues to be the largest payer for methadone services.
Impact on Arrest
As expected, during months in which individuals were enrolled in treatment, the odds of a felony arrest was much lower than in months when untreated. While the effectiveness of treatment was to be expected based on clinical trials that have been conducted, this was the first observational study to confirm the expected outcome across two large statewide populations over a 10 year period. Such similar results from two different states after merging multiple administrative data sets (treatment, Medicaid, and state police) over a 10 year period gives us greater confidence in our findings.
An unexpected finding was an interaction with the proportion of months in treatment. Our a priori hypothesis was that this was a simple additive effect—for any month treated we expected an average impact on arrests. Instead, the findings suggest that long term retention leads to a greater reduction in arrests than originally expected while short term retention is associated with little or no observable impact. Stable enrollment in methadone treatment was a critical factor in achieving the expected effect on arrests. We observed little difference in arrest rates by treatment status for clients who were enrolled in methadone only a few months. Thus long term retention is important, yet many prior studies have focused on rather brief and fixed lengths of stay. This lends support to the often cited guideline that more than 12 months of MMT should be provided.
Long term treatment raises issues about costs. In general, studies have found that long term MMT is quite cost effective. For example, an unpublished study48 in Washington state showed lower costs among MMT patients due primarily to reduced medical costs, especially among those in treatment longer than a year. A New York study49 reported a $4 benefit for every $1 spent on MMT.
Overall, the arrest results from these two states was quite similar. This outcome was reassuring given that we acquired multiple administrative data sets from parallel, but not identical data systems, in both states. Furthermore, the findings were robust despite state differences in the financing of substance abuse services.
Policy Implications
Reduction in the number of arrests is but one of the expected outcomes of methadone maintenance therapy. But it is a particularly important outcome because opiate addiction is highly associated with criminal activity and arrests account for a significant portion of the costs generated by untreated care. The cost of opiate related crime has been estimated at about 3 times the cost of treatment.16 In our sample, nearly every untreated client was arrested at least once during the observation period and some had many arrests.
Opiate addiction is considered a chronic condition like diabetes and enrollment in methadone maintenance is considered a long term investment. However, studies have shown that treatment is a relative bargain. The annual cost of treating a client in a methadone maintenance program was approximately $4,600,50 though unpublished studies in Washington state suggest the cost may be as low as $3,500 in some areas.
Longitudinal Approach
McClellan51,52 has argued that addiction is a chronic condition and should be studied from a longitudinal perspective. Such a perspective is particularly important for opiate addiction. It is apparent from Figure 1 that our findings about the role of Medicaid coverage on access to MMT would have been much less dramatic had we only looked at the start of a single index treatment episode. A study that only examined access to methadone at the start of an index episode would underestimate the longer term effect of coverage. As expected, the longitudinal, multilevel design proved to be a powerful analytic approach.
Reductions in criminal behavior or arrest rates have long been shown to be important outcomes of opiate treatment, often in relatively short term clinical trials. However, our work is the first to demonstrate this longitudinally, on large statewide populations, using independent indicators (arrests) rather than self report. Thus legislators and policymakers should find our results policy relevant.
Limitations
This was a natural experiment so assignment to Medicaid and to treatment was not random. Propensity score analysis was used to adjust for selective factors but this technique can only adjust for the observed covariates. There may have been important unmeasured covariates, though a rich set of variables was available for this purpose.
The study relied on linked records from multiple administrative data sets that were developed for purposes other than research. While the same state-of-the-art matching algorithms were used in both states, the Oregon records were matched using an encoded form of name.
Oregon's Medicaid expansion population may be somewhat unique, perhaps limiting generalizations to other states. However, we have no reason to expect that individuals eligible through the mandatory eligibility categories would respond differently than Oregon's expansion category to loss of coverage for treatment.
This study did not measure substance use as an outcome. While the treatment data sets from both states included a measure of use, the way that the data was collected minimized the utility of the data. The cost of continued substance use can be high, especially among the most severe clients or those who do not have stable employment.
There was little data on residential care from either state for clients presenting for opiate use and the length of stay was generally short. It was necessary to exclude these data from the analysis.
ACKNOWLEDGEMENTS
This study was supported in part by grant R01 DA015060 from the National Institute for Drug Abuse. The authors would like to thank officials from Oregon's Department of Human Services and Washington's Department of Social and Health Services for their assistance in acquiring and linking the data sets used in this study.
Biography
Author Bio: Dennis D. Deck , RMC Research Corporation, 111 S.W. Columbia St., Suite 1200, Portland, OR 97201 (503) 223-8248 (E-mail ddeck@rmccorp.com)
REFERENCES
- 1.Deschenes EP, Anglin MD, Speckart GR. Narcotics addiction: Related criminal careers, social and economic costs. Journal of Drug Issues. 1991;21(2):383–411. [Google Scholar]
- 2.Anglin MD, Speckart GR. Narcotics use and crime: A multisample, multimethod analysis. Criminology. 1988;26(2):197–233. [Google Scholar]
- 3.Chaiken JM, Chaiken MR, Peterson JE. Varieties of criminal behavior. Rand; Santa Monica: 1982. [Google Scholar]
- 4.McCarty D, Frank RG, Denmead GC. Methadone maintenance and state Medicaid managed care programs. Milbank Quarterly. 1999;77(3):341–362. doi: 10.1111/1468-0009.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deck DD, Carlson MJ. Access to publicly funded methadone maintenance treatment in two western states. Journal of Behavioral Health Services Research. 2004;31(2):164–177. doi: 10.1007/BF02287379. [DOI] [PubMed] [Google Scholar]
- 6.Deck DD, Carlson MJ. Retention in publicly funded methadone maintenance treatment in two western states. Journal of Behavioral Health Services & Research. 2005;32(1):43–60. doi: 10.1007/BF02287327. [DOI] [PubMed] [Google Scholar]
- 7.Deck DD, Wiitala WL, Laws K. Medicaid coverage and access to publicly funded opiate treatment. The Journal of Behavioral Health Services & Research. 2006;33(3):1094–3412. doi: 10.1007/s11414-006-9018-2. (print); 1556-3308 (online) [DOI] [PubMed] [Google Scholar]
- 8.Ball JC, Rosen L, Flueck JA, Nurco DN. The criminality of heroin addicts: When addicted and when off opiates. In: Inciardi JA, editor. The drugs-crime connection. Vol. 5. Sage; Beverly Hills: 1981. Sage annual reviews of drug and alcohol abuse. [Google Scholar]
- 9.Anglin MD, Speckart GR. Narcotics use, property crime, and dealing: Structural dynamics across the addiction career. Journal of Quantitative Criminology. 1986;2(4):355–375. [Google Scholar]
- 10.Nurco DN, Hanlon TE, Balter MB, Kinlock TW, Slaght E. A classification of narcotic addicts based on type, amount, and severity of crime. J Drug Issues. 1991;21:429–448. [Google Scholar]
- 11.McGlothlin WH, Anglin MD, Wilson BD. An evaluation of the California Civil Addicts Program. National Institute on Drug Abuse; Rockville, MD: 1977. [Google Scholar]
- 12.Hubbard RL, Craddock SG, Flynn PM, Anderson J, Etheridge RM. Overview of 1-year follow-up outcomes in the drug abuse treatment outcome study (DATOS) Psychology of Addictive Behaviors. 1997;11(4):261–278. [Google Scholar]
- 13.Simpson DD, Joe GW, Broome KM, Hiller ML, Knight K, Rowan-Szal GA. Program diversity and treatment retention rates in the drug abuse treatment outcome study (DATOS) Psychology of Addictive Behaviors. 1997;11(4):261–278. [Google Scholar]
- 14.Sells SB, Simpson DD. A case for drug abuse treatment effectiveness based on the DARP research program. British Journal of Addiction. 1980;75(2):117–132. doi: 10.1111/j.1360-0443.1980.tb02437.x. [DOI] [PubMed] [Google Scholar]
- 15.Hubbard RL, Marsden ME, Rachal JV, Harwood HJ, Cavanaugh ER, Ginzburg HM. Drug abuse treatment: A national study of effectiveness. University of North Carolina Press; Chapel Hill, NC: 1989. [Google Scholar]
- 16.Center for Substance Abuse Treatment . Methadone treatment outcomes in the national treatment improvement studies(NTIES) Center for Substance Abuse Treatment, Department of Health and Human Services; Rockville, MD: 1995. [Google Scholar]
- 17.Hubbard RL, Marsden ME, Cavanaugh ER, Rachal JV, et al. The role of drug abuse treatment in limiting the spread of AIDS. Review of Infectious Diseases. 1988;10:377–384. doi: 10.1093/clinids/10.2.377. [DOI] [PubMed] [Google Scholar]
- 18.Simpson DD, Sells SB. Highlights of the DARP follow-up research on the evaluation of drug abuse treatment effectiveness (IBR Report 81-3) Institute of Behavioral Research, Texas Christian University; Fort Worth, TX: 1981. [Google Scholar]
- 19.Simpson DD, Sells SB. Effectiveness of treatment for drug abuse: An overview of the DARP Research Program. Advances in Alcohol and Substance Abuse. 1982;2(1):7–29. [Google Scholar]
- 20.Anglin MD, McGlothlin WH, Speckart GR, Ryan TM. Shutting off methadone: The closure of the San Diego Methadone Maintenance Program. National Institute on Drug Abuse; Rockville, MD: 1982. Final Report. [Google Scholar]
- 21.Anglin MD, McGlothlin WH. Outcome of narcotic addict treatment in California. In: Tims FM, Ludford JP, editors. Drug Abuse Treatment Evaluation: Strategies progress & prospects. National Institute on Drug Abuse; Rockville, MD: 1984. pp. 106–128. (NIDA Research Monograph Series, No. 51). [PubMed] [Google Scholar]
- 22.Marsch LA. The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: A meta-analysis. Addiction. 1998;93(4):515–532. doi: 10.1046/j.1360-0443.1998.9345157.x. [DOI] [PubMed] [Google Scholar]
- 23.Masson CL, Barnett PG, Sees KL, et al. Cost and cost-effectiveness of standard methadone maintenance treatment compared to enriched 180-day methadone detoxification. Addiction. 2004;99:718–726. doi: 10.1111/j.1360-0443.2004.00728.x. [DOI] [PubMed] [Google Scholar]
- 24.Office of National Drug Control Policy . Consultation Document on Methadone/LAAM. Author; Washington, DC: Sep 29, 1998. [Google Scholar]
- 25.French MT, Dunlop LJ, Calinis DN, et al. Health care reforms and managed care for substance abuse services: Findings from 11 case studies. Journal of Public Health Policy. 1996;17:181–203. [PubMed] [Google Scholar]
- 26.Flynn PM, Kristiansen PL, Porto JV. Costs and benefits of methadone treatment for women and men who left before or were still in treatment at follow-up. Paper presented at the College on Problems of Drug Dependence (CPDD) Annual Meeting; Acapulco. Jun, 1999. [Google Scholar]
- 27.Harwood HJ, Hubbard RL, Collins JJ, Rachal JV. The costs of crime and the benefits of drug abuse treatment: A cost benefit analysis using TOPS data. In: Leukefeld CG, Tims FM, editors. Compulsory Treatment of Drug Abuse: Research and Clinical Practice. U.S. Department of Health and Human Services; Rockville, MD: 1988. pp. 209–235. (NIDA Research Monograph 86). [PubMed] [Google Scholar]
- 28.Frank RG, McGuire TG. Estimating costs of mental health and substance abuse coverage. Health Affairs. 1995;14:102–115. doi: 10.1377/hlthaff.14.3.102. [DOI] [PubMed] [Google Scholar]
- 29.Oggins J. Changes in health insurance and payment for substance use treatment. American Journal of Drug and Alcohol Abuse. 2003;9(1):55–74. doi: 10.1081/ada-120018839. [DOI] [PubMed] [Google Scholar]
- 30.Garcia LM, McGeary KA, Shultz JM, et al. The impact of insurance status on drug abuse treatment completion. Journal of Health Care Finance. 1999;26:40–47. [PubMed] [Google Scholar]
- 31.Rosenbaum M, Washburn A, Knight K, et al. Treatment as harm reduction, defunding as harm maximization: The case of methadone maintenance. Journal of Psychoactive Drugs. 1996;28(3):241–249. doi: 10.1080/02791072.1996.10472485. [DOI] [PubMed] [Google Scholar]
- 32.Rosenbaum M, Murphy S, Beck J. Money for methadone: Preliminary findings from a study of Alameda county's new maintenance policy. Journal of Psychoactive Drugs. 1987;19(1):13–19. doi: 10.1080/02791072.1987.10472375. [DOI] [PubMed] [Google Scholar]
- 33.Anglin MD, Speckart GR, Booth MW, et al. Consequences and costs of shutting off methadone. Addictive Behaviors. 1989;14:307–326. doi: 10.1016/0306-4603(89)90062-2. [DOI] [PubMed] [Google Scholar]
- 34.McGlothlin WH, Anglin MD. Shutting off methadone. Costs and benefits. Archives of General Psychiatry. 1991;38:885–892. doi: 10.1001/archpsyc.1981.01780330043004. [DOI] [PubMed] [Google Scholar]
- 35.Campbell KM, Deck DD, Cox A, Broderick C. The Link King user manual Version 5.2. Division of Alcohol and Substance Abuse; Olympia, WA: 2006. http://www.the-link-king.com/user_manual.zip. [Google Scholar]
- 36.Whalen D, Pepitone A, Graver L, Bush JD. Linking Client Records from Substance Abuse, Mental Health and Medicaid State Agencies. U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration; Rockville, MD: 2001. http://csat.samhsa.gov/IDBSE/idb/modules/linking/ material/linking.pdf. [Google Scholar]
- 37.Campbell KM, Deck DD, Krupski A. Record linkage software in the public domain: A comparison of Link Plus, The Link King, and a “basic” deterministic algorithm. Health Informatics Journal. doi: 10.1177/1460458208088855. In press. [DOI] [PubMed] [Google Scholar]
- 38.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 39.D'Agostino RB. Tutorial in Biostatistics: Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Statistics in Medicine. 1998;17(19):2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 40.Shadish WR, Clark MH. An introduction to propensity scores. Metodologia de las Ciencias del Comportamiento Journal. 2002;4(2):291–300. [Google Scholar]
- 41.Orwin RG, Campbell B, Campbell K, Krupski A. Welfare reform and addiction: A priori hypotheses, post hoc explorations, and assisted sensemaking in evaluation the effects of terminating benefits for chronic substance abusers. American Journal of Evaluation. 2004;25(4):409–441. [Google Scholar]
- 42.Deck DD, Vander Ley K. Medicaid eligibility and access to mental health services among adolescents in substance abuse treatment. Psychiatric Services. 2006;57(2):263–265. doi: 10.1176/appi.ps.57.2.263. [DOI] [PubMed] [Google Scholar]
- 43.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 44.McCullough CE, Searle SR. Generalized, linear, and mixed models. John Wiley and Sons; New York: 2001. [Google Scholar]
- 45.Raudenbush SW, Bryk AS. Hierarchical linear models. second edition Sage Publications; Thousand Oaks: 2002. [Google Scholar]
- 46.Roudenbush SW, Bryk AS, Cheong YF, Congdon R. HLM6: Hierarchical Linear and Nonlinear Modeling. SSI Scientific Software International; Lincolnwood, IL: 2004. [Google Scholar]
- 47.Campbell KM, Deck DD, Krupski A. Impact of substance abuse treatment on arrests among opiate users in Washington state. American Journal on Addictions. doi: 10.1080/10550490701641157. In press. [DOI] [PubMed] [Google Scholar]
- 48.Nordlund DJ, Estee S, Mancuso D, Felver B. Methadone treatment for opiate addiction lowers health care costs and reduces arrests and convictions. DSHS Research and Data Analysis Division; Washinton Stae Department of Scoial and Health Services: 2004. http://www1.dshs.wa.gov/pdf/ms/rda/research/4/49.pdf. [Google Scholar]
- 49.New York State Committee of Methadone Program Administrators . Regarding Methadone Treatment: A review. New Your, NY: 2007. [Google Scholar]
- 50.Substance Abuse and Mental Health Services Administration . Alcohol and Services Study: The National Treatment System: Outpatient Methadone Facilities. SAMSHA, Office of Applied Studies; Rockville, MD: 2004. http://www.samhsa.gov/adass.htm. [Google Scholar]
- 51.McClellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance and outcome evaluation. Journal of the American Medical Association. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 52.McClellan AT. Paper presented at the Summer Institute on Longitudinal Research. Center for Advancing Longitudinal Drug Abuse Research; Los Angeles, CA: Aug 14, 2006. What if addiction were treated, evaluated and reimbursed as a chronic illness? http://www.caldar.org/HTML/mclellan.html. [Google Scholar]


