Abstract
Stroke survivors today are discharged home from the hospital more quickly than in the past because of shifting economic realities. Survivors continue to experience significant impairments after discharge and families may be poorly prepared for the full extent of caregiving responsibilities. This article describes 39 comprehensive educational guidelines that have been tested with 72 stroke survivors and families during 1,150 home visits throughout the first 6 months after discharge from inpatient rehabilitation. Two case studies illustrate use of the guidelines with stroke survivors and their families.
Stroke is the third leading cause of death and the major cause of long-term disability among older adults in the United States. Approximately 5.7 million stroke survivors live in the United States (American Heart Association [AHA], 2007). The length of inpatient rehabilitation is decreasing, with a change of focus toward community-based rehabilitation (Lincoln, Walker, Dixon, & Knights, 2004), leaving a relatively short time for many stroke survivors and families to absorb all of the information they will need when they go home. Because many stroke survivors have comorbidities such as heart disease and diabetes, their educational needs may be extensive. They require information on risk-factor reduction to prevent future strokes, and also encouragement to live a healthy lifestyle through a wholesome diet, exercise, and stress management.
This article describes a stroke educational program that was offered to 72 stroke survivors and their families as part of an interdisciplinary research study called CAReS (Committed to Assisting with Recovery after Stroke [NR005316]). CAReS was a 5-year randomized clinical intervention study funded by the National Institute for Nursing Research (NINR). As they were discharged home from inpatient rehabilitation, 159 stroke survivors and their spouses were randomized into usual care or home visit groups. Physical and psychosocial data were collected on stroke survivors and spousal caregivers in both groups at discharge and 3, 6, 9, and 12 months after discharge to test for differences between the two groups. All couples received information by mail for 12 months. The group randomized into the home visit group also received home visits for 6 months from nurses and therapists, who used 39 flexible, evidence-based guidelines developed by this article's authors for use with stroke survivors following discharge from inpatient rehabilitation. The guidelines were tested for ease of use and acceptance by stroke survivors and their families during more than 1,150 visits from an interdisciplinary team comprising advanced practice nurses (APNs) and occupational and physical therapists. Case studies illustrate the use of these guidelines based on stroke survivor and family needs. Names of the family members in the case studies have been changed to protect identity.
Literature
Stroke is a catastrophic event for survivors and their families. Because significant numbers of stroke survivors experience limitations after they go home, continuing and targeted education is crucial to minimize stroke's impact. The National Heart, Lung, and Blood Institute's (NHLBI) Framingham Heart Study reported that among stroke survivors 6 months after discharge, 50% had one-sided paralysis, 35% were depressed, 30% were unable to walk without assistance, 25% were dependent in activities of daily living (ADL), and 19% were aphasic (Kelly-Hayes et al., 2003). In a 2006 survey of 523 long-term stroke survivors, the National Stroke Association reported that 87% had ongoing motor problems, 54% had trouble walking, 52% had trouble with hand movements, and 58% experienced spasticity. Forty percent said they had limited success in meeting rehabilitation goals related to mobility and speech (Jones, 2006).
After discharge, stroke survivors have to confront the pervasive effects a stroke may have on their lives. Family members have to learn rehabilitation techniques and adjust to changes in their relationships with the stroke survivor (Coombs, 2007). Although a return to the home environment has distinct advantages for stroke survivors, it also involves less contact with nursing and rehabilitation professionals, resulting in reduced daily professional support for survivors and caregivers. Increased demands on families have been shown to result in decreased mental health for some family caregivers (Andersen et al., 2000; Teel, Duncan & Lai, 2001; White, Poissant, Coté-LeBlanc, & Wood-Dauphinee, 2006). Clark and Smith (1998) reported survivors who were better informed about their stroke and prognosis had less depression and made better functional recoveries than poorly informed patients.
Resources that could help with the transition from hospital to home often are fragmented or lacking. Stroke survivors and their caregivers have difficulty obtaining information about their condition (Andersen et al., 2000), managing special cognitive and behavioral problems without assistance (Grant, Glandon, Elliott, Giger, & Weaver, 2004), and obtaining access to community and rehabilitation services (Ski & O'Connell, 2007). In a National Stroke Association survey, 38% of long-term stroke survivors reported a lack of information about community and rehabilitation resources (Jones, 2006).
Managing comorbidities such as hypertension, heart disease, diabetes, high blood cholesterol, and smoking is essential to prevent recurrent strokes. Some studies have suggested these comorbidities are not equally distributed within the population. A study by the World Health Organization (Mackay & Mensah, 2004) found that stroke survivors with lower socioeconomic status (SES) had more previous strokes and more stroke-related comorbidities. Risk reduction education may need to be targeted to those with lower SES, who often are younger, have less education, and represent a larger percentage of minorities.
A catastrophic event such as a stroke may provide the impetus for important life changes. Research on patients with stroke, hypertension, diabetes, and hypercholesterolemia, however, has shown that adherence to self-care management generally is poor. Most patients do not comply with dietary and exercise guidelines, directives to stop smoking, and self-monitoring unless special attention is given to adherence (Kernan & Inzucchi, 2004; Miller, Hill, Kottke, & Ockene, 1997; NHLBI, 2002; Qureshi, Suri, Kirmani, & Divani, 2004; Siskind et al., 2000). The AHA reports that multicomponent strategies including patient education, contracts, self-monitoring, social support, telephone follow-up, and tailoring the educational content to individual and family needs works most effectively toward gaining compliance (Miller et al.).
Recruiting Participants
The CAReS research study was approved by the institutional review boards (IRBs) of the University of Texas Health Science Center at Houston and the Baylor College of Medicine and the individual IRBs of the five healthcare systems from which participants were recruited in the Texas Medical Center (TMC). Stroke survivors in rehabilitation settings were invited to participate if they had experienced a stroke within the last 12 months, were at least 50 years of age and spoke English, lived within 50 miles of TMC, and were to be discharged home with a spouse (or significant other). Stroke survivors were excluded if they were under hospice care or had physical or psychiatric disabilities that prohibited them from participating in the educational aspects of the study (e.g., global aphasia or dementia) or if they did not have a spouse or significant other who was willing to participate in the study. Health Insurance Portability and Accountability Act (HIPAA) waivers and written informed consents were obtained from stroke survivors and their spousal caregivers before program participation. The 159 couples who agreed to participate were randomly assigned to a group that received the at-home educational program described in this article or information delivery by mail. Of the 79 couples randomized to the home-intervention group, 72 completed the 6-month intervention using the educational guidelines described here. Further information on recruitment and retention of the sample can be found in a separate journal article (Schulz, Wasserman, & Ostwald, 2006).
Educational Guidelines
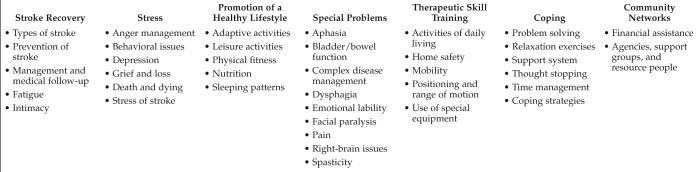
The educational guidelines developed for use in the CAReS project were based on a literature review, clinical experience, and the Agency for Health Care Policy and Research (now the Agency for Healthcare Research and Quality, or AHRQ) Post-Stroke Rehabilitation Clinical Practice Guideline (Gresham et al., 1995). Nurses and physical and occupational therapists examined the literature to develop the multidisciplinary guidelines. The guidelines related to stress and coping also were reviewed by a psychologist, and guidelines related to aphasia and dysphagia were reviewed by a speech therapist. The guidelines were divided into the seven categories illustrated in Figure 1. They were designed to provide education, support, skill training, counseling, and links to social and community resources. The 6-month guideline implementation time frame was chosen to take advantage of the natural window of physiological recovery.
Fig 1.
Major Educational Categories with Specific Content-Based Guidelines
The guidelines were flexible so they could be delivered in any order, based on the needs of the stroke survivor and family. The authors found that in the immediate posthospital phase, stroke survivors and caregivers especially needed information about the effects of the stroke on the survivor, assistance with special nursing and therapy techniques, suggestions for adapting the home for safety and independence, support for day-to-day issues, and ways to access community resources. As seen in Figure 1, this content was covered by the guidelines in the areas of Stroke Recovery, Therapeutic Skill Training, Special Problems, and Community Networks. While all participants received information on topics such as type of stroke, stroke prevention, and home safety, only those with specific needs received information on the topics listed on Figure 1 under Special Problems (i.e., aphasia, pain, and spasticity).
By the end of 3 months, rehabilitation progress usually began to slow and available insurance-reimbursable services were decreasing. The survivor and family often expressed feelings of isolation and frustration because the recovery had not been more complete. Guidelines related to managing stress, coping with chronic illness(es), and developing and maintaining a healthy lifestyle were particularly important to reduce excess disability and caregiver burnout. The topics covered under Stress of Stroke, Coping Strategies, and Promotion of a Healthy Lifestyle are included in Figure 1.
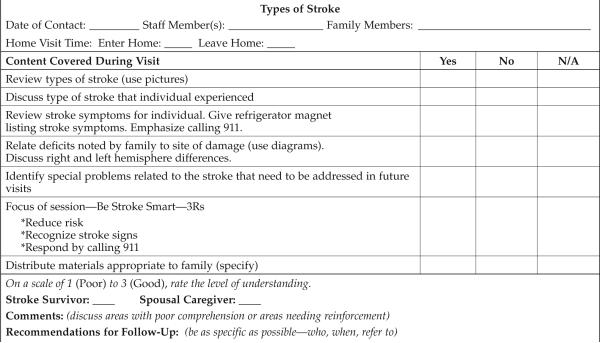
The guidelines were developed to help structure home visits and to record the things that transpired during the visit, the caregiver and survivor's understanding of the content, and recommendations for follow-up. A Microsoft Access database was developed for recording and tracking. An abbreviated example of the guideline, Types of Stroke, is shown in Figure 2.
Fig 2.
Guideline for Education on Types of Stroke
Profile of Stroke Survivors
The average stroke survivor was 66.4 years old (SD = 9.14); survivors were 50-88 years of age. Minority groups were represented in 29 (40%) families. This was the first stroke for 52 (72%) of the stroke survivors; 40 patients (56.3%) had right hemispheric strokes. Twenty-five patients (34.7%) had been identified in the hospital as having depression, and 44 patients (61%) were sent home with antidepressant medications. After discharge, survivors were prescribed an average of 12 (SD = 5.01, range = 2-24) different medications. Sociodemographic and comorbidity characteristics of stroke survivors who received the educational program are shown in Table 1.
Table 1.
Characteristics of Stroke Survivors Receiving the Educational Program (n = 72)
| Characteristic | n (%) |
|---|---|
| Gender | |
| Male | 49 (68.1) |
| Female | 23 (31.9) |
| Highest Education Level | |
| Less than high school | 12 (16.7) |
| High school graduate | 19 (26.4) |
| Partial college | 16 (22.2) |
| College graduate | 14 (19.4) |
| Graduate/professional school | 11 (15.3) |
| Race/Ethnicity | |
| African American | 13 (18.1) |
| Asian | 2 (2.8) |
| Hispanic | 14 (19.4) |
| Non-Hispanic white | 43 (59.7) |
| Previous Occupation | |
| Housewife | 6 (8.3) |
| Unskilled worker | 1 (1.4) |
| Semiskilled worker | 10 (13.9) |
| Skilled worker | 13 (18.1) |
| Sales/clerical | 6 (8.3) |
| Technician | 11 (15.3) |
| Manager/owner | 10 (13.9) |
| Administrator/professional | 5 (6.9) |
| Executive/professional | 10 (13.9) |
| Comorbidities | |
| Hypertension | 63 (87.5) |
| High cholesterol/lipids | 32 (44.4) |
| Diabetes | 26 (36.1) |
| Valvular heart disease | 21 (29.2) |
| Cardiac arrhythmias | 16 (22.2) |
| Smoking | 20 (27.8) |
| Sleep apnea | 9 (12.5) |
| Alcohol abuse | 9 (12.5) |
| Coronary artery disease | 7 (9.7) |
Guideline Evaluation
Education, support, skill training, and counseling were provided during home visits. Follow-up contacts and referrals usually were handled via telephone. Between 2001 and 2006, 72 stroke survivors and family caregivers received the home-based educational program using the guidelines outlined in Figure 1. The team spent 2,644 hours during 1,150 visits with stroke survivors and families throughout this program's duration. Over 6 months, the average family received 16 visits (range = 8-34), for a total of 36.7 hours (range = 17-80 hours) of education. The mean length of each visit was just over 70 minutes, and nurses and therapists used an average of 25 guidelines over the 6 months based on the survivors' and families' needs. The average family received education using 20 guidelines provided by the APNs, three guidelines given by the occupational therapist, and two guidelines given by the physical therapist.
At the conclusion of each visit, the team member assessed her perceptions of how well the stroke survivor and caregiver understood the content provided during the session (see Fig 2). The nurses and therapists reported that 63% of stroke survivors and 85% of caregivers indicated they understood the content well, while only 6% of stroke survivors and less than 1% of caregivers had significant difficulty understanding the content. Guideline content was repeated as often as necessary, especially if the survivor or family did not understand it or if the situation changed (i.e., new hospital admission). Families were provided with evaluation forms and were asked to anonymously return the forms in self-addressed stamped envelopes to report their satisfaction with the educational program. Most family participants (83.75%) returned at least one evaluation form. The average number of evaluations returned by each family was 4.7 (range = 1-7). In total, families returned 314 evaluation forms and reported overwhelming satisfaction (3.80, range = 2.8-4) on a scale of 1 (not satisfied) to 4 (very satisfied).
Case Studies
The following two case studies illustrate the use of the guidelines to meet individual stroke survivor and family needs.
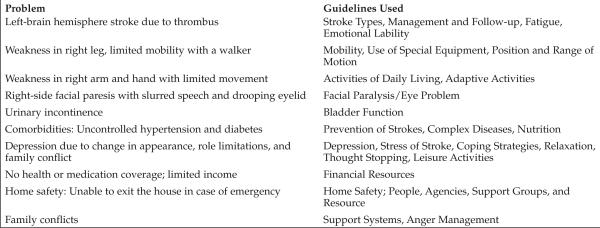
Case Study 1: A.R. and Family
A.R. was a 59-year-old Mexican-American woman who lived with her husband, two daughters, a son-in-law, and three grandchildren in a small converted mobile home. Before her stroke, she had been a school-bus driver; more recently, she had cared for her grandchildren, cooked for her extended family, and managed the home. Her husband was a retired unskilled worker and their family income from his Social Security was $1,100/month; they had no health or medication insurance.
A.R. experienced a thrombus affecting the left hemisphere of her brain while driving her car. She was able to drive home, but unable to get out of the car due to paralysis on the right side of her body; her speech was dysarthric. She was admitted to a local hospital and discharged after 23 days. She received no inpatient rehabilitation and only received in-home physical therapy for 3 weeks, which was discontinued due to lack of ability to pay.
A.R.'s problem list and the educational guidelines that were used in her household are detailed in Figure 3. She was able to use a walker to ambulate within the house without assistance, but to accommodate her weakness and instability, she used a donated wheelchair when going out of the house. With the team's assistance, she initiated exercises on her right hand and learned to balance herself at the sink and use her right hand to anchor dishes in warm water while she washed them with her left hand. Returning to this familiar role increased her self-esteem and helped reclaim her role within the family. She used a hand mirror to do facial exercises and family members were taught to instill liquid tears into her right eye to prevent dryness. Being with her three young grandchildren encouraged her to practice her speech and use her right hand to balance the children on her lap.
Fig 3.
Problems Identified and Guidelines Used with A.R. and Family
A.R. was denied Social Security disability benefits because her work history was insufficient and the family income was too high for county medical assistance. Her medication bottles were empty. Her blood pressure was 170/94 mm Hg, and her blood glucose was 180 mg/dl. The team helped her apply for free medications from pharmaceutical companies. With the correct medications and lifestyle changes, she learned to successfully manage her diabetes and hypertension. She was unable to leave her home because it had steep concrete-block steps without hand railings. After a referral from the program team, the local area agency on aging replaced the unsafe concrete-block steps at the door with a ramp so she could safely exit the house in her walker or wheelchair. Arguments between A.R. and her husband, stress related to lack of finances, and the presence of three families within one small house resulted in frequent family conflicts. These conflicts escalated until her husband moved out of the house for a time. He returned to help care for her when the daughters and their families moved into their own apartments. Although A.R. remained primarily housebound, she enjoyed reading magazines, watching television, helping to care for her grandchildren, and occasionally going to school events with the family.
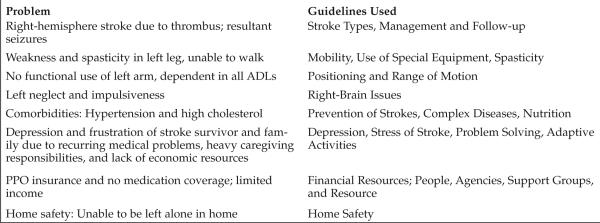
Case Study 2: R.J.
R.J. was a 50-year-old African-American man who lived with his wife and an adult son. He sustained a right-brain thrombotic stroke; this was his second stroke in 2 years. He made a strong recovery after his first stroke and was able to return to work as a car salesperson. He had a preferred provider organization (PPO)-type insurance with no medication coverage. R.J. was hospitalized for 14 days in acute care and 60 days in inpatient rehabilitation before discharge. His PPO was slow to approve his claims for outpatient therapy. As a result, his therapy was episodic, with breaks of 2-3 weeks between each approved set of sessions. R.J.'s wife worked full time as a customer service representative for a local discount store and she expressed frustration at trying to handle the demands of caregiving and a full-time job. An adult son provided care during the day on a temporary basis until his mother could make other arrangements.
R.J.'s problem list and the guidelines used with his family are detailed in Figure 4. He applied for and received Social Security disability benefits and also obtained medical insurance through the county system so he could continue consistent outpatient therapy. He improved his mobility so he could transfer with assistance using a walker, and he also could bear some weight on his left leg. He received botulinum toxin Type A (Botox) injections for his muscle spasticity. The team helped him apply for free medications through programs managed by pharmaceutical companies. He was able to control his hypertension and seizures with medications. His wife was referred to the state provider assistance program, through which she could quit her job and became R.J.'s primary paid caregiver. This allowed her to be compensated for staying home and caring for her husband, relieving much of her stress and frustration over finances and her husband's quality of care.
Fig 4.
Problems Identified and Guidelines Used with R.J. and Family
Discussion
Because inpatient rehabilitation length of stay has become short, stroke survivors are increasingly being discharged home with many educational needs. The education that is provided in the hospital primarily focuses on physical rehabilitation. Once in the home environment, however, stroke survivors and families must adapt to physical and psychological changes in the stroke survivor, changes in family relationships, and environmental and financial challenges.
These guidelines represent an evidence-based interdisciplinary approach to comprehensive education for stroke survivors and their families. The content was individualized to survivors' and families' situations and their level of understanding. Information provided in the hospital setting was reviewed and reinforced with pictures, diagrams, and printed materials. Materials that have been developed by expert organizations such as the American Stroke Association (www.strokeassociation.org) and the National Stroke Association (www.stroke.org) were used liberally. These materials, which are available online or for a nominal fee, are written at various reading levels and tailored to different racial or ethnic groups; many also are available in Spanish.
A unique aspect of this educational program was the interdisciplinary team approach. The majority of visits were made by APNs, but families saw physical therapists for mobility and equipment issues and to address problems such as spasticity. Occupational therapists provided expertise on issues related to home safety, adaptive and leisure activities, and community reintegration. The team met weekly to discuss families and their needs, to identify the appropriate staff member to make the next visit, and to discuss referrals to community resources. All staff members were prepared to follow up on the guidelines because they had been involved in their initial development and families benefited from the high level of staff communication. The APNs benefited from weekly consultations with physical and occupational therapists on topics related to mobility, equipment, positioning, spasticity, home safety, and activities, while nurses provided expertise to therapists regarding specific medical and nursing problems, disease prevention, health promotion, and stress management.
Summary
Numerous studies show caregivers sustain negative psychological effects during the first year after a stroke survivor is discharged home (Blake, Lincoln, & Clarke, 2003; Burton, 2000; Clark & Smith, 1998; Coombs, 2007; Grant et al., 2004; Ski & O'Connell, 2007). Recent research finds stroke survivors often do not reach their rehabilitation goals and lack of information is a major barrier to continued recovery (Jones, 2006). Consequently, posthospitalization educational programs provided to stroke survivors and their families must be interactive, interdisciplinary, and focused on identified needs. In this program, not only was the content comprehensive, but multiple strategies were used, as suggested by Miller and colleagues (1997). These strategies include one-on-one education reinforced with pictures, diagrams, and written materials and tailored to survivors' and families' needs and level of understanding. Team members demonstrated and encouraged survivors and caregivers to accurately demonstrate self-monitoring techniques such as how to take a pulse and properly use home blood-pressure-monitoring equipment and glucometers and canes, walkers, and wheelchairs. The team followed up on suggestions via telephone and provided additional information by mail. Social support and referrals to groups and agencies that could provide ongoing information and social or financial support also were part of the educational program.
Stroke is a multifaceted disease with physical, psychological, and behavioral problems differing among survivors. Even those with similar types of impairment may experience differences in degree of severity, trajectory of recovery, and social and financial resources. As illustrated in the two case studies, APNs and therapists were able to use the guidelines to educate, support, counsel, train, and link the families to community agencies and financial resources. In doing so, they helped these two families better understand their diseases, control their comorbidities, and decrease their risk of recurrent strokes to progress toward recovery and to garner the many resources necessary to improve their health, safety, and quality of life.
Acknowledgments
This work was supported by the National Institutes of Health, National Institute for Nursing Research RO1 NR005316 (Sharon K. Ostwald, PI) and the Isla Carroll Turner Friendship Trust. We wish to thank Debra Griffith, BSN RN, Myrna Khan, PhD, and Jamel Ostwald, PhD, for their assistance with this project.
References
- American Heart Association Heart Disease and Stroke Statistics—2007 Update. 2007 Retrieved July 26, 2007, from www. americanheart.org/downloadable/heart/1166712318459HS_ StatsInsideText.pdf.
- Andersen HE, Schultz-Larsen K, Kreiner S, Forchhammer BH, Driksen K, Brown A. Can readmission after stroke be prevented? Results of a randomized clinical study: A postdischarge follow-up service for stroke survivors. Stroke. 2000;31:1038–1045. doi: 10.1161/01.str.31.5.1038. [DOI] [PubMed] [Google Scholar]
- Blake H, Lincoln NB, Clarke DD. Caregiver strain in spouses of stroke patients. Clinical Rehabilitation. 2003;17(3):312–317. doi: 10.1191/0269215503cr613oa. [DOI] [PubMed] [Google Scholar]
- Burton CR. Re-thinking stroke rehabilitation: The Corbin and Strauss chronic illness trajectory framework. Journal of Advanced Nursing. 2000;32(3):595–602. doi: 10.1046/j.1365-2648.2000.01517.x. [DOI] [PubMed] [Google Scholar]
- Clark MS, Smith DS. Factors contributing to patient satisfaction with rehab following stroke. International Journal of Rehabilitation Research. 1998;21:143–154. doi: 10.1097/00004356-199806000-00003. [DOI] [PubMed] [Google Scholar]
- Coombs UE. Spousal caregiving for stroke survivors. Journal of Neuroscience Nursing. 2007;39(2):112–119. doi: 10.1097/01376517-200704000-00008. [DOI] [PubMed] [Google Scholar]
- Grant JS, Glandon GL, Elliott TR, Giger JN, Weaver M. Caregiving problems and feelings experienced by family caregivers of stroke survivors the first month after discharge. International Journal of Rehabilitation Research. 2004;27(2):105–111. doi: 10.1097/01.mrr.0000127639.47494.e3. [Information and treatment recommendations from Medical Agency on Depression, in Swedish]. Retrieved April 7, 2008, from www.lakemedelsverket.se/upload/H%C3%A4lso-%20och% 20sjukv%C3%A5rd/behandlingsrek/depressionvuxna.pdf. [DOI] [PubMed]
- Mohr DC, Cox D. Multiple sclerosis: Empirical literature for the clinical health psychologist. Journal of Clinical Psychology. 2001;57(4):479–499. doi: 10.1002/jclp.1042. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Dick LP, Russo D, Pinn J, Boudewyn AC, Likosky W, et al. The psychosocial impact of multiple sclerosis: Exploring the patient's perspective. Health Psychology. 1999;18(4):376–382. doi: 10.1037//0278-6133.18.4.376. [DOI] [PubMed] [Google Scholar]
- Nortvedt MW, Riise T. The use of quality of life measures in multiple sclerosis research. Multiple Sclerosis. 2003;9:63–72. doi: 10.1191/1352458503ms871oa. [DOI] [PubMed] [Google Scholar]
- Olek M, Dawsson D. Multiple sclerosis and other inflammatory demyelinating diseases of the central nervous system. In: Marsden C, editor. Neurology in clinical practice. Butterworth-Heinemann; Boston: 2000. pp. 1431–1463. [Google Scholar]
- Olshansky S. Chronic sorrow: A response to having a mentally defective child. Social Casework. 1962;43:190–193. [Google Scholar]
- Pakenham KI. The positive impact of multiple sclerosis (MS) on carers: Associations between carer benefit finding and positive and negative adjustment domains. Disability and Rehabilitation. 2005;27(17):985–997. doi: 10.1080/09638280500052583. [DOI] [PubMed] [Google Scholar]
- Poser CM, Paty DW, Scheinberg L, McDonald WI, Davis FA, Ebers GC, et al. New diagnostic criteria for multiple sclerosis: Guidelines for research protocols. Annals of Neurology. 1983;13(3):227–231. doi: 10.1002/ana.410130302. [DOI] [PubMed] [Google Scholar]
- Schreier AM, Droes NS. Theory of chronic sorrow. In: Tomey AM, Alligood MR, editors. Nursing theorists and their work. 6th ed. Mosby; St. Louis: 2006. pp. 679–695. [Google Scholar]
- Siegert RJ, Abernethy DA. Depression Depression in in mulmultiple sclerosis: A review. Journal of Neurology, Neurosurgery, and Psychiatry. 2005;76(4):469–475. doi: 10.1136/jnnp.2004.054635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerfield MR, McCrae RR. Stress and coping research. American Psychologist. 2000;55(6):620–625. [PubMed] [Google Scholar]
- Wollin JA, Yates PM, Kristjanson LJ. Supportive Supportive and and palliative care needs identified by multiple sclerosis patients and their families. International Journal of Palliative Nursing. 2006;12(1):20–26. doi: 10.12968/ijpn.2006.12.1.20392. [DOI] [PubMed] [Google Scholar]
- Gresham GE, Duncan PW, Stason WB, Adams HP, Jr., Adelman AM, Alexander DN, et al. Post-Stroke Rehabilitation. Clinical Practice Guideline, No. 16. U.S. Department of Health and Human Services. Public Health Service, Agency for Health Care Policy and Research; Rockville, MD: 1995. AHCPR Publication No. 95-0662. [PubMed] [Google Scholar]
- Jones VN. The forgotten survivor [Electronic version] Stroke Smart. 2006 Retrieved July 19, 2007, from www.stroke.org/site/PageServer?pagename= SS_MAG_so2006_feature_forgot.
- Kelly-Hayes M, Beiser A, Kase CS, Scaramucci A, D'Agostino RB, Wolf PA. The influence of gender and age on disability following ischemic stroke: The Framingham Study. Journal of Stroke and Cerebrovascular Diseases. 2003;12(3):119–126. doi: 10.1016/S1052-3057(03)00042-9. [DOI] [PubMed] [Google Scholar]
- Kernan WN, Inzucchi SE. Type 2 diabetes mellitus and insulin resistance: Stroke prevention and management. Current Treatment Options in Neurology. 2004;6(6):443–450. doi: 10.1007/s11940-004-0002-y. [DOI] [PubMed] [Google Scholar]
- Lincoln NB, Walker MF, Dixon A, Knights P. Evaluation of a multiprofessional community stroke team: A randomized control trial. Clinical Rehabilitation. 2004;18:40–47. doi: 10.1191/0269215504cr700oa. [DOI] [PubMed] [Google Scholar]
- Mackay J, Mensah G. The atlas of heart disease and stroke. World Health Organization; Geneva, Switzerland: 2004. [Google Scholar]
- Miller NH, Hill M, Kottke T, Ockene IS. The multilevel compliance challenge: Recommendations for a call to action: A statement for healthcare professionals. Circulation. 1997;95(4):1085–1090. doi: 10.1161/01.cir.95.4.1085. [DOI] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute . Detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) Author; Bethesda, MD: 2002. NIH Publication No. 02-5215. [Google Scholar]
- Qureshi AI, Suri MFK, Kirmani JF, Divani AA. The relative impact of inadequate primary and secondary prevention on cardiovascular mortality in the United States. Stroke. 2004;35(10):2346–2350. doi: 10.1161/01.STR.0000141417.66620.09. [DOI] [PubMed] [Google Scholar]
- Schulz C, Wasserman J, Ostwald SK. Recruitment and retention of stroke survivors: The CAReS experience. Journal of Physical and Occupational Therapy in Geriatrics. 2006;25(1):17–29. [Google Scholar]
- Siskind A, Johnson M, Qureshi A, Solow B, Chesebro D, Oldham N. The impact of automatic prescriptions on reducing low-density lipoprotein cholesterol levels. Effective Clinical Practice. 2000;3(5):240–246. [PubMed] [Google Scholar]
- Ski C, O'Connell B. Stroke: The increasing complexity of carer needs. Journal of Neuroscience Nursing. 2007;39(3):172–179. [PubMed] [Google Scholar]
- Teel CS, Duncan P, Lai SM. Caregiving experiences after stroke. Nursing Research. 2001;50(1):53–56. doi: 10.1097/00006199-200101000-00008. [DOI] [PubMed] [Google Scholar]
- White CL, Poissant L, Coté-LeBlanc G, Wood-Dauphinee S. Long-term caregiving after stroke: The impact on care-givers' quality of life. Journal of Neuroscience Nursing. 2006;38(5):354–360. [PubMed] [Google Scholar]