Abstract
Background
Orthopaedic procedures have been reported to have the highest incidence of pain compared to other types of operations. There are limited studies in the literature that investigate postoperative pain.
Materials and Methods
A prospective study of 98 patients undergoing orthopedic foot and ankle operations was undertaken to evaluate their pain experience. A Short-Form McGill Pain Questionnaire (SF-MPQ) was administered preoperatively and postoperatively.
Results
The results showed that patients who experienced pain before the operation anticipated feeling higher pain intensity immediately postoperatively. Patients, on average, experienced higher pain intensity 3 days after the operation than anticipated. The postoperative pain intensity at 3 days was the most severe, while postoperative pain intensity at 6 weeks was the least severe. Age, gender and preoperative diagnosis (acute versus chronic) did not have a significant effect on the severity of pain that patients experienced. Six weeks following the operation, the majority of patients felt no pain. In addition, the severity of preoperative pain was highly predictive of their anticipated postoperative pain and 6-week postoperative pain, and both preoperative pain and anticipated pain predict higher immediate postoperative pain.
Conclusion
The intensity of patients' preoperative pain was predictive of the anticipated postoperative pain. Patients' preoperative pain and anticipated postoperative pain were independently predictive of the 3-day postoperative pain. The higher pain intensity a patient experienced preoperatively suggested that their postoperative pain severity would be greater. Therefore, surgeons should be aware of these findings when treating postoperative pain after orthopaedic foot and ankle operations.
Keywords: Postoperative Pain, Pain Expectations, Foot and Ankle Surgery, SF-MPQ, Short-Form McGill Pain Questionnaire, Longitudinal Pain Study
Introduction
Pain assessment and management is now a health care priority in the United States, but there is a paucity of reports in the literature that specifically assess pain with orthopaedic operations.1,3,5–7,9,12,13,16–18 Patients recovering from major orthopaedic and trauma surgery are at high risk of inadequate pain relief.19
A prospective study by Chung et al.5 evaluated ambulatory surgical patients and found that orthopaedic patients had the highest incidence of pain compared to other types of operations.
The purpose of this study was to characterize the preoperative and postoperative pain experienced by patients undergoing orthopaedic foot and ankle operations. We hypothesized that pain expectations would determine postoperative pain severity. This knowledge may allow us to educate our patients about their likely pain experience after surgery. Their expectations may help determine postoperative pain severity. Therefore influencing patients' pain expectation may be a target for reducing postoperative pain severity. Also, and perhaps more important, surgeons may use this information to treat acute pain more aggressively since poorly controlled pain may incite several pathophysiologic responses that increase postoperative morbidity.19
Materials and Methods
Following IRB approval, 104 consecutive preoperative orthopaedic foot and ankle surgery patients were asked to participate in this pain survey. All patients were treated by a single orthopaedic foot and ankle specialist at one hospital. Patients who declined participation, did not comprehend the English language, or had a history of chronic opioid or substance abuse were excluded from the study. Only one patient declined to participate because he stated that he did not want to be part of a research study. Six patients did not complete the study because they lost their Pain Survey Form or did not return for followup. We evaluated the results of 98 patients (one operation per patient). There were 48 women and 50 men. The average age was 46.5 (range, 17 to 85). The procedures included all foot and ankle operations in a busy academic practice. There were 47 patients with chronic conditions (such as deformities, arthritis), 32 with acute problems (fractures, recent injuries), 16 with hardware removal, and two with sports injuries. Also, the operations were classified as outpatient or inpatient procedures. Generally, an outpatient operation was a short procedure (about one hour operation time), associated with less complications, and possibly less pain severity. Therefore, with an outpatient procedure, the postoperative pain could be managed by the patient with oral analgesics. Fifty-three operations were outpatient that did not require overnight hospitalization, and 45 patients were inpatients.
The Short-Form McGill Pain Questionnaire (SF-MPQ)14 was utilized. The SF-MPQ has demonstrated differences due to treatment, and it includes the Present Pain Intensity (PPI) of the standard McGill Pain Questionnaire (MPQ) and the Visual Analog Scale (VAS). The Present Pain Intensity (PPI) uses a categorical scale with integer values between 0 and 5; and the VAS has continuous values between 0 and 10.5 cm.
Patients were given a SF-MPQ at each of three different time points: (1) 1 to 7 days before the operation (Preoperative Pain) when they did not take pain medication and were asked about their Anticipated Postoperative Pain, (2) 3 days postoperatively, and (3) 6 weeks after the operation. The surveys were filled out by the patient with a co-author in person or by telephone. Outpatients were treated postoperatively with oral hydrocodone/acetaminophen or oxycodone/acetaminophen. Inpatients were treated with Patient-Controlled Analgesia (PCA) with morphine or hydromorphone. Upon discharge from the hospital, they were given prescriptions for the same medications as outpatients. Dosing information was not collected upon patients' discharge from the hospital. The most frequently prescribed pain medications were hydrocodone/acetaminophen and oxydocone/acetaminophen.
Histograms of pain intensities at each time point were created in order to visualize the distributions of pain experienced. Means, standard deviations, and confidence intervals were computed for the pain reported at each time point.
Two-sample t-statistics were computed on 3-Day Postoperative Pain VAS, in order to assess the effect on pain of the following: (1) whether a subject remained as an inpatient following surgery, (2) gender, (3) age, (4) type of diagnosis (acute vs. chronic). In order to determine whether Preoperative Pain and Anticipated Postoperative Pain can be used to predict 3-Day Postoperative Pain, a multivariate linear model was fit using 3-Day Postoperative Pain as the outcome and both Preoperative Pain and Anticipated Postoperative Pain as predictor variables. In addition, two-sample t-statistics were computed between pairs of time points, in order to determine whether there was a significant change in pain reported across time points.
Results
Pain severity was high early following foot and ankle surgery at the 3-Day Postoperative Pain assessment (Figure 2). Figures 1 and 2 shows the distribution of pain anticipated and experienced by patients. Of note, the distribution of pain immediately postoperatively (3-Day Postoperative Pain) appears to be bi-modal with a minority experiencing low pain (VAS less than 4) and a larger group with poorly controlled pain (VAS greater than 5).
Fig. 2.
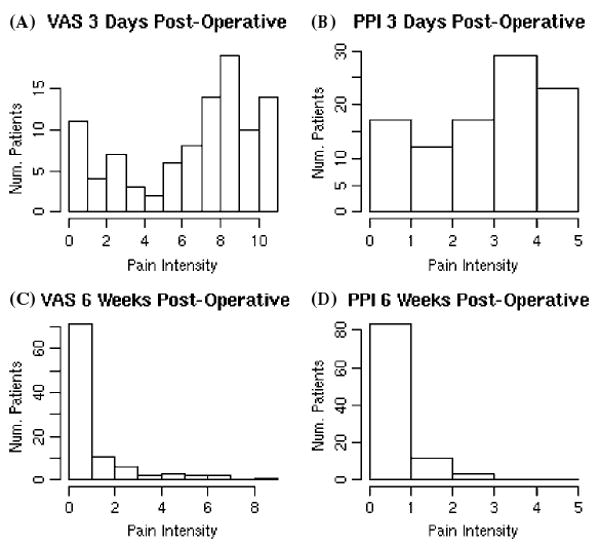
The results of the Visual Analog Scale (VAS) and Present Pain Intensity (PPI) for 3-Day Postoperative Pain and 6-Week Postoperative Pain: VAS for 3-Day Postoperative Pain (A), PPI for 3-Day Postoperative Pain (B), VAS for 6-Week Postoperative Pain, and D) PPI for 6-Week Postoperative Pain (C). Patients were distributed bi-modally with respect to pain early following foot and ankle surgery with the majority experiencing inadequate pain control (VAS 3-Day Postoperative Pain greater than or equal to 5) However, most patients suffered very little pain 6 weeks after the operation, even less than they suffered before the operation.
Fig. 1.
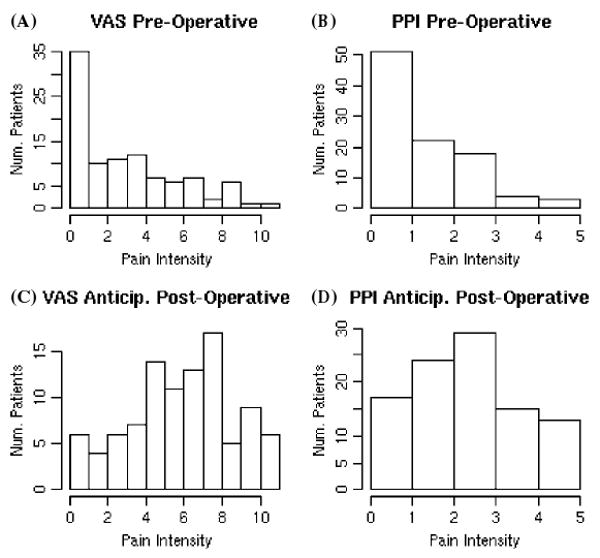
The graphs summarize the results of the Visual Analog Scale (VAS) and Present Pain Intensity (PPI) for Preoperative Pain and Anticipated Postoperative Pain: VAS for Preoperative Pain (A), PPI for Preoperative Pain (B), VAS for Anticipated Postoperative Pain (C), and PPI for Anticipated Postoperative Pain (D). Despite minimal preoperative pain, patients expect moderate to severe postoperative pain.
To evaluate this further, we stratified patients according to whether they remained as inpatients following surgery. Figure 3, shows the 3-Day Postoperative Pain VAS of inpatients and outpatients. These results indicate that while inpatients tend to uniformly have more pain, outpatients fall into one of two groups with either adequate pain control or poor pain control.
Fig. 3.
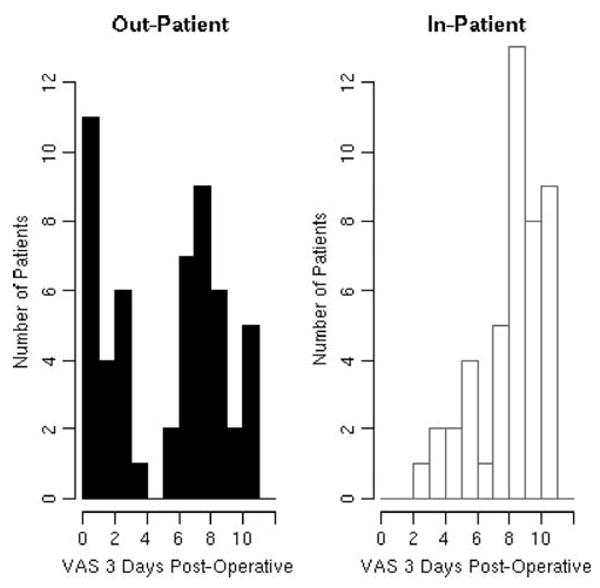
Histogram of outpatient VAS pain at 3-Day Postoperative Pain (black) is shown with the histogram of inpatient VAS pain at 3-Day Postoperative Pain (white). The figures are histograms, not bar graphs, because the VAS measurements were continuous. The bins in the histogram correspond to pain levels between 0 and 1, between 1 and 2, between 2 and 3, etc. These results indicate that while inpatients tend to uniformly have more pain, outpatients fall into one of two groups with either low pain control or high scores.
Two-sample t-statistics were performed in order to determine the effects of gender, age, and type of diagnosis (acute versus chronic) on pain experienced. However, the results were not statistically significant (the p-values exceeded 0.05).
Multivariate linear regression identified that anticipated pain (Anticipated Postoperative Pain VAS, p < 0.001) and preoperative pain (Preoperative Pain VAS, p < 0.021) both independently, significantly predicted immediate (3-Day Postoperative Pain VAS) postoperative pain (adjusted R-squared is 0.19, p < 0.0001).
Six weeks after the operation, the majority of people felt no pain. The most severe pain was felt three days after the operation, and the least severe pain was felt six weeks after the operation.
There was a correlation between the responses that patients gave using the PPI and VAS measures. At the time points Preoperative Pain, 3-Day Postoperative Pain, and 6-Week Postoperative Pain, the correlation coefficients between PPI and VAS were 0.83, 0.85, and 0.90, respectively. However, the correlation coefficient between PPI and VAS for anticipated pain was only 0.60.
Table 1 summarizes the statistics based on VAS pain measure. The 95% confidence intervals for the mean pain experienced (as measured by VAS) before the operation, 3 days after the operation, and 6 weeks after the operation had no overlap. Upon correcting for multiple comparisons, preoperatively anticipated pain and actual early postoperative pain did not differ significantly. All other between time point comparisons were significant at the p < 0.05 level.
Table 1.
Summary statistics based on VAS pain measure
| Assessment | Mean and Standard Deviation | 95% C.I. for Mean |
|---|---|---|
| PP | 3 ± 3 | (2.36, 3.50) |
| APP | 6 ± 3 | (5.36, 6.46) |
| 3DPP | 7 ± 3 | (5.86, 7.21) |
| 6WPP | 0.9 ± 2 | (0.59, 1.27) |
VA S = Visual Analog Scale, PP = Preoperative Pain, APP = Anticipated Postoperative Pain, 3DPP = 3-Day Postoperative Pain, 6WPP = 6-Week Postoperative Pain.
Table 2 summarizes the statistics of the PPI pain measure. The 95% confidence intervals for the mean pain suffered (as measured by PPI) before the operation, 3 days after the operation, and 6 weeks after the operation had no overlap. On the other hand, there is overlap between the 95% confidence intervals for the mean pain experienced 3 days after the operation and for the anticipated mean pain experienced.
Table 2.
Summary statistics based on PPI pain measure
| Time | Mean and Standard Deviation | 95% C.I. for Mean |
|---|---|---|
| PP | 1 ± 1 | (1.19, 1.75) |
| APP | 3 ± 1 | (2.44, 3.02) |
| 3DPP | 3 ± 2 | (2.89, 3.52) |
| 6WPP | 0.5 ± 1 | (0.34, 0.68) |
PPI = Present Pain Intensity, PP = Preoperative Pain, APP = Anticipated Postoperative Pain, 3DPP = 3-Day Postoperative Pain, 6WPP = 6-Week Postoperative Pain.
Discussion
We found that anticipated pain significantly predicted early postoperative pain. Also, the majority of patients following foot and ankle operations reported high pain in the early postoperative period. They experienced VAS pain scores greater than 5 in the early postoperative period (3-Day Postoperative Pain VAS) (Figure 2). Even among outpatients, the majority reported high pain. The important statistics relating to the VAS and PPI pain intensity measures can be seen in Tables 1 and 2. As seen from the confidence intervals, the amounts of pain experienced at time points Preoperative Pain, 3-Day Postoperative Pain and 6-Week Postoperative Pain are quite different. The most severe pain was at 3-Day Postoperative Pain and the least at 6-Week Postoperative Pain. The difference between Anticipated Postoperative Pain and 3-Day Postoperative Pain was not as large as the other differences.
Our finding that patients with high levels of pre-surgical pain severity experienced greater postoperative pain reproduced findings suggested by other authors.1,2 Chung et al.5 evaluated postoperative pain in 10,008 patients prospectively. Orthopaedic patients had the highest incidence of pain. Body mass index, duration of anesthesia and certain types of operations were predictors of severe pain. Interestingly, the type of anesthesia was not used as a predictive factor because it was dependent on the type of operation. Another report by McGrath et al.,13 evaluated 5,703 patients postoperatively and found that orthopaedic surgery procedures were among the most painful in ambulatory surgery. In fact, two of the seven most painful procedures were ankle and knee operations.
Importantly, we found that preoperative pain severity and the degree of pain patients anticipated significantly predicted increased pain severity following foot and ankle operations. Anticipated pain independently predicted actual early postoperative pain following foot and ankle operations. This finding may simply reflect that patients are good at predicting the likely consequences of operations. Alternatively, the very expectation of greater pain may contribute to its subsequent occurrence. If true, a surgeon could conceivably reduce a patient's postoperative pain by reducing their expectations of pain during their preoperative visit. In support of this hypothesis, preliminary data suggests that the expectation of pain changes the brain's processing of incoming noxious stimuli in the nucleus cuneiformis.11 Additionally, expectations of increased pain may increase the actual experience of pain by augmenting the activity of brain projections to the spinal cord that specifically enhance the strength of ascending pain signals.2,15 Our findings extend this work by suggesting that the expectation of pain in the perioperative setting may contribute to its subsequent occurrence.
Evidence based plans should include regional anesthesia in some form. A recent randomized controlled trial found that patients receiving local anesthetic through an indwelling popliteal sciatic catheter following foot and ankle operations had markedly less pain, opioid use, sleep disturbance and improved overall satisfaction.10 Placement of these catheters will likely become more widespread as the advent of ultrasound guided regional anesthesia brings these techniques within the technical grasp of a larger number of anesthesiologists.8 In addition to reducing postoperative pain, inclusion of these techniques might also be expected to improve early postoperative rehabilitation based on published experience in knee operations.4
Another noteworthy finding is the number of patients who reported no pain preoperatively (Figure 1A). More than one-third (35%) of patients had a VAS of zero. Some patients were stable in splints for Achilles tendon ruptures or fractures and reported no pain. Also, there were patients with chronic disorders including deformities who did not experience pain preoperatively.
There are limitations to this study. First, we did not measure the use of pain medication. This aspect would significantly increase the complexity and variables of pain evaluation. Patients were asked about their pain when they did not take pain medication. Furthermore, we did not include the previous history of pain experiences, such as injuries and other operations. Another limitation of this study is that all types of foot and ankle procedures were included. All patients were from the academic practice of a single orthopaedic foot and ankle surgeon, hence many types of disorders were treated. However, one might argue that inpatient procedures would naturally cause more pain which was the primary reason the patients were being admitted to the hospital following surgery. Because the intensity of pain experience was seen in some patients as severe with even minor procedures, the specific procedure type was not used as a factor in the evaluation. For the same reason, the type of anesthesia was not a factor in the pain intensity experience. As previously discussed, Chung et al.5 found that the type of anesthesia was not used as a predictive factor. Another limitation was excluding patients who did not comprehend English. These patients could have been included. When the study was designed, some of the postoperative surveys would be filled out by patients at home while being instructed by a physician by telephone. We were concerned that an interpreter may not be available. Despite these study limitations, we think this is a helpful step in assessment and management of pain of orthopaedic patients. We plan to further investigate pain associated with orthopaedic foot and ankle surgery by evaluating associated factors of pain, including specific type of operations, anesthesia, past pain history, and monitor or record the type, route, frequency and dose of pain medication.
Conclusion
This is the first study evaluating preoperative and postoperative pain experienced by patients undergoing orthopaedic foot and ankle operations. Our results show that the majority of patients experience significant pain despite commonly used oral opioid regimens or even intravenous Patient-Controlled Analgesia (PCA) administered opioids following foot and ankle operations. Also, this work may help surgeons modify their treatment of acute pain postoperatively to prevent increased postoperative morbidity associated with poorly controlled pain after orthopaedic foot and ankle operations.
Footnotes
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Aida S, Fujijara H, Taga K, Fukuda S, Shimoji K. Involvement of presurgical pain in preemptive analgesia for orthopedic surgery: a randomized double blind study. Pain. 2000;84:169–173. doi: 10.1016/s0304-3959(99)00196-7. http://dx.doi.org/10.1016/S0304-3959(99)00196-7. [DOI] [PubMed]
- 2.Brown CA, Seymour B, Boyle Y, El-Deredy W, Jones AK. Modulation of pain ratings by expectation and uncertainty: Behavioral characteristics and anticipatory neural correlates. Pain. 2007 Jul 3; doi: 10.1016/j.pain.2007.05.022. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 3.Camu F, Beecher T, Recker DP, Verburg KM. Valdecoxib, a COX-2-specific inhibitor, is an efficacious, opioid-sparing analgesic in patients undergoing hip arthroplasty. Am J Ther. 2002;9:43–51. doi: 10.1097/00045391-200201000-00009. http://dx.doi.org/10.1097/00045391-200201000-00009. [DOI] [PubMed]
- 4.Capdevila X, Barthelet Y, Biboulet P, et al. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999;91:8–15. doi: 10.1097/00000542-199907000-00006. http://dx.doi.org/10.1097/00000542-199907000-00006. [DOI] [PubMed]
- 5.Chung F, Ritchie E, Su J. Postoperative pain in ambulatory surgery. Anesth Analg. 1997;85:808–16. doi: 10.1097/00000539-199710000-00017. http://dx.doi.org/10.1097/00000539-199710000-00017. [DOI] [PubMed]
- 6.Closs SJ, Briggs M. Patients' verbal descriptions of pain and discomfort following orthopaedic surgery. Int J Nursing Studies. 2002;39:563–572. doi: 10.1016/s0020-7489(01)00067-0. http://dx.doi.org/10.1016/S0020-7489(01)00067-0. [DOI] [PubMed]
- 7.Delgado-Martinez AD, Marchal-Escalona JM. Supramalleolar ankle block anesthesia and ankle tourniquet for foot surgery. Foot Ankle Int. 2001;22:836–838. doi: 10.1177/107110070102201011. [DOI] [PubMed] [Google Scholar]
- 8.Gray AT. Ultrasound-guided regional anesthesia: current state of the art. Anesthesiology. 2006;104:368–673. doi: 10.1097/00000542-200602000-00024. http://dx.doi.org/10.1097/00000542-200602000-00024. [DOI] [PubMed]
- 9.Hubbard RC, Naumann TM, Traylor L, Dhadda S. Parecoxib sodium has opioid-sparing effects in patients undergoing total knee arthroplasty under spinal anaesthesia. Br J Anaesth. 2003;90:166–172. doi: 10.1093/bja/aeg038. http://dx.doi.org/10.1093/bja/aeg038. [DOI] [PubMed]
- 10.Ilfeld BM, Morey TE, Wang RD, Enneking FK. Continuous popliteal sciatic nerve block for postoperative pain control at home: a randomized, double-blinded, placebo-controlled study. Anesthesiology. 2002;97:959–965. doi: 10.1097/00000542-200210000-00031. http://dx.doi.org/10.1097/00000542-200210000-00031. [DOI] [PubMed]
- 11.Keltner JR, Furst A, Fan C, et al. Isolating the modulatory effect of expectation on pain transmission: a functional magnetic resonance imaging study. J Neurosci. 2006;26:4437–4443. doi: 10.1523/JNEUROSCI.4463-05.2006. http://dx.doi.org/10.1523/JNEUROSCI.4463-05.2006. [DOI] [PMC free article] [PubMed]
- 12.Malan TP, Marsh G, Hakki SI, et al. Parecoxib sodium, a parenteral cyclooxygenase 2 selective inhibitor, improves morphine analgesia and is opioid-sparing following total hip arthroplasty. Anesthesiology. 2003;98:950–956. doi: 10.1097/00000542-200304000-00023. http://dx.doi.org/10.1097/00000542-200304000-00023. [DOI] [PubMed]
- 13.McGrath B, Elgendy H, Chung F, Kamming D, Curti B, King S. Thirty percent of patients have moderate to severe pain 24 hour after ambulatory surgery: a survey of 5,703 patients. Can J Anes. 2004;51:886–891. doi: 10.1007/BF03018885. [DOI] [PubMed] [Google Scholar]
- 14.Melzack R. The short-form McGill pain questionnaire. Pain. 1987;30:191–197. doi: 10.1016/0304-3959(87)91074-8. http://dx.doi.org/10.1016/0304-3959(87)91074-8. [DOI] [PubMed]
- 15.Ploghaus A, Tracey I, Gati JS, et al. Dissociating pain from its anticipation in the human brain. Science. 1999;284:1979–1981. doi: 10.1126/science.284.5422.1979. http://dx.doi.org/10.1126/science.284.5422.1979. [DOI] [PubMed]
- 16.Rasmussen GL, Steckner K, Hogue C, Torri S, Hubbard RC. Intravenous parecoxib sodium for acute pain after orthopedic knee surgery. Am J Orthop. 31:336–343. 2002. [PubMed] [Google Scholar]
- 17.Reuben SS, Bhopatkar S, Maciolek H, Joshi W, Sklar J. The preemptive analgesic effect of rofecoxib after ambulatory arthroscopic knee surgery. Anesth Analg. 2002;94:55–59. doi: 10.1097/00000539-200201000-00010. http://dx.doi.org/10.1097/00000539-200201000-00010. [DOI] [PubMed]
- 18.Reynolds LW, Hoo RK, Brill RJ, et al. The COX-2 specific inhibitor, valdecoxib, is an effective, opioid-sparing analgesic in patients undergoing total knee arthroplasty. J Pain Symptom Manage. 2003;25:133–141. doi: 10.1016/s0885-3924(02)00637-1. http://dx.doi.org/10.1016/S0885-3924(02)00637-1. [DOI] [PubMed]
- 19.Sinatra RS, Torres J, Bustos AM. Pain management after major orthopaedic surgery: current strategies and new concepts. J Am Acad Orthop Surg. 2002;10:117–129. doi: 10.5435/00124635-200203000-00007. [DOI] [PubMed] [Google Scholar]


