Abstract
Increasing obesity among Americans is a serious issue in the U.S., especially in the pediatric and young adult population. We use a longitudinal design to examine the relationship between childhood poverty/welfare receipt and obesity onset and continuity from adolescence into young adulthood using three waves of the National Longitudinal Study of Adolescent Health. We include multiple measures of disadvantage that co-occur with poverty and model potential mediating mechanisms within a life course framework. We find a significant effect of poverty/welfare receipt in childhood on obesity outcomes for females, but not for males. However, other measures of socioeconomic disadvantage such as neighborhood poverty, and low parental education are related to obesity in both males and females. Poverty may impact female obesity through the mediating effects of physical activity, inadequate sleep, skipping breakfast and certain forms of parental monitoring, while race is an important confounder of poverty's influence. This paper highlights the important influence of poverty and other aspects of social disadvantage on obesity outcomes during this critical transition to adulthood. Implications of this research include physical activity and parenting interventions for low-income youth. In addition, governmental efforts should be made to increase physical activity opportunities in poor neighborhoods.
Keywords: adolescence, family, obesity, poverty
Introduction
One of the most serious public health concerns in the United States today has been the almost three-fold increase in overweight and obesity among children and adolescents over the last three decades (Ogden et al. 2002). The highest rates of obesity occur among the most disadvantaged population groups, those with the least education and the highest poverty rates (Drewnowski & Specter 2004). A large and growing body of research has investigated the relationship between socioeconomic status (SES) and obesity, though most of this research has focused on adults (e.g., Zhang & Wang 2003; Paeratakul et al. 2002). Studies that examine SES and obesity among children and adolescents mainly use cross-sectional data (e.g., Miech et al. 2006; Wang and Zhang 2006; Haas et al. 2003; Wang 2001) or are based on nonrepresentative samples (e.g. Nelson, Chiasson & Ford 2004). Research using longitudinal designs typically does not study children and adolescents; however, a few studies do exist (e.g. Gibson 2004; Strauss & Knight 1999). Other limitations of the research on SES and obesity include differences in measurement of SES and a lack of attention to factors that may mediate the relationship between SES and obesity (Goodman et al. 2003; Wang 2001).
This paper investigates the links between poverty experiences in childhood and adolescence and obesity transitions from adolescence into young adulthood using nationally representative data from the National Longitudinal Study of Adolescent Health (Add Health). We extend the research on poverty and obesity in four important ways. We place poverty in context by including measures of social disadvantage that co-occur with family poverty, such as neighborhood poverty and low parental education. Most research focuses on a particular measure of disadvantage when examining the relationship between poverty and obesity; however, poverty does not occur in isolation. Families that are poor usually struggle to pay bills, live in poor neighborhoods and have less access to educational opportunities (Duncan & Cole 1984). Our utilization of multiple measures of socioeconomic disadvantage that co-occur with poverty better capture the complexities of poverty experiences.
We use a longitudinal design to examine the relationship between poverty experiences and obesity transitions beginning in childhood through the transition to young adulthood using three waves of Add Health data. The longitudinal design enables us to model the temporal ordering of poverty experiences on subsequent obesity, making ours one of the few studies to trace the linkages between poverty and obesity over the adolescent and young adult portion of the life course, with important implications for future adult well-being and health.
We make several contributions in measurement strategies. We make use of the longitudinal data on body mass index to examine the dynamics of obesity status from adolescence into young adulthood and explore pathways of body mass change during a period of increased risk for obesity development (Gordon-Larsen et al. 2004a). With data from two points in time, we create measures that represent continuity and change in obesity status from adolescence into young adulthood, using comparable youth and adult definitions of obesity.
We model the theoretical mechanisms through which poverty may operate to influence obesity transitions utilizing a life course framework. Our exploration of mediating mechanisms contributes to understanding how poverty influences obesity in adolescence and its tracking into young adulthood by examining the role of the family environment and lifestyle in adolescence. Finally, we examine the relationship between poverty and obesity separately for males and females. Previous research indicates the poverty-obesity relationship varies by sex, and we contribute further to this research by exploring how family and lifestyle mechanisms associated with poverty operate differently on obesity for males and females.
Relationship between Poverty and Childhood/Adolescent Obesity
The prevalence of obesity varies across socioeconomic status (SES) in the U.S. (McLaren 2007). In general, there is an inverse relationship between SES and obesity, especially among non-Hispanic white females (McLaren 2007; Stunkard 1993). Research results on the role of SES have been mixed because few studies use national data sets of children and adolescents, and the general lack of a consensus definition of obesity (e.g., Goodman et al. 2003; Cole et al. 2000).
Studies that use national data in a cross-sectional design find an inverse relationship between SES and obesity among adolescents (Wang 2001) when SES measures include income and parental education, however this relationship varies by age, race and sex (Wang & Zhang 2006). Haas and colleagues (2003) found poverty to be associated with a lower prevalence of overweight among adolescents and a higher prevalence of overweight among young children. Miech and colleagues (2006) found that family poverty was related to increasing overweight among older (15-17 years) but not younger (12-14 years) adolescents. Longitudinal studies also find household income during childhood to be negatively related to obesity in adolescence (Strauss & Knight 1999); but other research examining the effects of long-term food stamp participation finds no effect on obesity among adolescents (Gibson 2004).
There have been more consistent findings of sex differences in the relationship between SES and obesity. Studies indicate a stronger inverse association between SES and obesity among females compared to males (McLaren 2007; Zhang and Wang 2003; Wang 2001).
A small but growing body of literature investigates the relationship between food insecurity and obesity, using poverty status and other SES measures as control variables (Alaimo, Olson & Frongillo 2001). Food insecurity is described as an economic and social problem of food insufficiency due to monetary or other constraints (CNSTAT 2006). Many researchers (e.g., Gibson 2004; Frongillo 2003;), link food insecurity status with poverty.
Relevant to the current research, Alaimo and colleagues (2001) analyzed cross-sectional data from NHANES III to examine the relationship between family income, food insufficiency and being overweight in US children and adolescents. They found a positive relationship between low income, food insufficiency and increased risks of overweight, but only among non-Hispanic white children ages 8-16.
Theoretical Framework
The life course perspective serves as an overarching framework to understand the influence of poverty on obesity transitions from adolescence into young adulthood (Elder 1998). This perspective has developed into a dominant theoretical paradigm for studying the transition to adulthood (Shanahan 2000) as well as health trajectories and the development of chronic diseases (Lynch & Smith 2005).
Four central themes define the life course paradigm and help to guide our research. The first theme maintains that human lives are linked through a network of shared relationships and lives are interdependent across generations. For example, choices that parents make about their lifestyles affect their children's lives. Parents' eating behaviors and parenting practices influence the development of their children's eating behaviors (Birch & Fischer 1998).
The second theme focuses on the timing and sequencing of life events that can be conceptualized as a trajectory. The ordering of events determine subsequent states and risks. For example, obesity in childhood increases the risk of obesity in adulthood (Reilly et al. 2003;). In addition, trajectories have the potential to build momentum from reinforcing circumstances. The environment of childhood poverty is characterized by multiple psychosocial and physical risk factors. Each of these risk factors, both singularly and cumulatively, affects the physical and psychological morbidity of low-income children (Evans 2004), and reinforce each other to augment the momentum of a particular trajectory. For example, an obese adolescent living in a poor family may face additional barriers to engaging in physical activity and healthful eating if the person lives in a poor neighborhood with higher crime rates and less access to healthy foods (e.g., Gordon-Larsen et al. 2006; Morland et al. 2002). Therefore, family poverty and neighborhood poverty both serve to reinforce the continuity of obesity from adolescence and into young adulthood.
The third theme emphasizes human agency in choice making. Although individuals are influenced by their social world, they actively make decisions within the constraints of their social, historical and economic context, family backgrounds and stage in the life course. Human agency is relevant in nutritional choices and diets among the poor, within the constraints of food choices in poor communities. The fourth theme relates to the importance of studying individuals in their historical context. Because of the narrow age range in our sample, we assume that the respondents experience similar cultural and normative influences of their shared historical context, a context in which obesity has been rising.
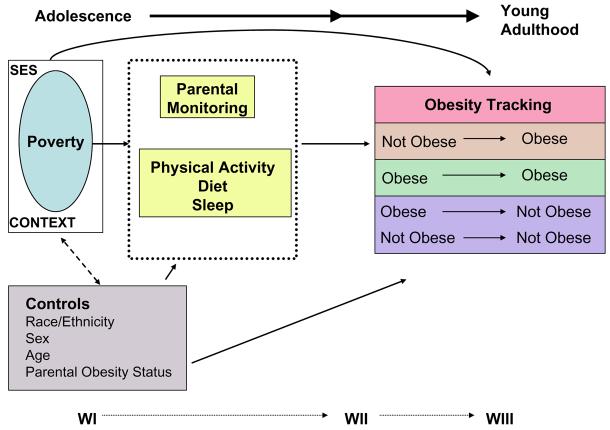
The life course framework informs our conceptual model shown in Figure 1. We use data from all three waves of Add Health, where poverty and related socioeconomic indicators (i.e., low parental education, trouble paying bills, neighborhood poverty, non-two biological parent family structure) are measured in childhood and adolescence, the intervening mechanisms discussed below (parental monitoring, physical exercise, diet [skipping breakfast] and inadequate sleep hours) are measured in adolescence (Waves I and II), and obesity pathways are constructed from data in adolescence (Wave II) and young adulthood (Wave III). All controls are measured at Wave I, our first data point in adolescence. Below we elaborate on the theoretical mechanisms shown in Figure 1 that are involved in the relationship between family poverty experiences and obesity pathways during the transition to adulthood, and state our expectations for their effects. Overall, we expect a positive relationship between poverty and obesity in adolescence and young adulthood, though we expect the poverty effect will be mediated by the intervening mechanisms.
Figure 1.
Conceptual Model
Poverty and the Family Environment
Poverty is an experience defined by differences in family and neighborhood context and cultural norms (Wilson 1987). Poverty scholars have studied how poverty influences the family environment to impact children's well-being and can explain how the effect of income largely operates through the indirect effects of parenting practices, the physical home environment, and health (Duncan & Brooks-Gunn 1997).
Parental Monitoring
When children live at home, parents establish and monitor their lifestyles, including what they eat and when they eat, and their levels of physical activity. Further, consumption of meals with family members increases the quality of adolescents' diets (Videon & Manning 2003). Parental monitoring lowers the number of non-nutritious foods chosen by children and total caloric content of meals (Fisher & Birch 1999). Parental monitoring also influences the regularity of meals, including breakfast, which increases the risk of obesity when regularly skipped, especially among adolescents (e.g., Berkey et al. 2003; Boutelle et al. 2002). Thus, we expect parental monitoring of adolescents' meals will reduce the risks of obesity and potentially mediate the effects of poverty.
Poor parents are less able to monitor their children's diet, diet patterns and physical activity due to stress and time constraints if they work. Mothers who work full-time are less able to monitor their children due to a decrease in maternal presence and availability during the day (Jacobson & Crockett 2000). Monitoring is more affected by the mother's work status because the majority of fathers work full-time, and mother primarily supervise children's activities during the day (Seltzer 1994). Because income (i.e., poverty) is the substantive focus in our model, we expect mother's work status to represent a time constraint on parental monitoring during the day, potentially impacting obesity through unsupervised meals and increased inactivity.
Physical Activity and Diet
At the most basic level, weight gain is the result of energy intake and energy expenditure. Physical activity (energy expenditure) and inactivity are important biological determinants of obesity (Epstein et al. 1997). Inactivity, in particular, TV viewing, has been associated with obesity in cross-sectional studies of children, adolescents and adults (Gortmaker et al. 1996). Physical activity habits, and, specifically, inactivity, track significantly from adolescence into young adulthood (Gordon-Larsen, Nelson & Popkin 2004b). Because poor children have fewer opportunities for outdoor exercise or organized sports participation, we expect physical activity will mediate the effects of poverty on the obesity pathways in our model.
While Add Health does not have a 24-hour recall measure, it does have indicators of diet patterning, an important predictor of poor dietary intake in adolescents (Siega-Riz, Popkin & Carson 1997). We use skipping breakfast, discussed above, as a proxy for poor diet.
Inadequate Amounts of Sleep
The family environment and parental monitoring, through the enforcement of curfews and bedtimes, influence another critical health behavior related to obesity outcomes in hours of sleep. A growing number of epidemiological studies observe an association between short sleep duration and obesity (Gangwisch et al. 2005). Low levels of sleep have also been physiologically linked to heavier weight, operating through hormonal mechanisms (Spiegel et al. 2004). Therefore the enforcement of a curfew and adequate sleep during adolescence is expected to reduce the likelihood of experiencing obesity during the transition to adulthood.
Co-occurring Elements of Social Disadvantage
Poverty does not occur in isolation but is characterized by the experience of multiple risk factors. Non-intact family structures are associated with both poverty and obesity, though probably operating through some of the intervening mechanisms discussed above, including parental monitoring and work status (McLanahan 1995). For example, inadequate monitoring is more common among isolated single mothers who are socially disadvantaged (Jones et al. 2003). Parental education, related to poverty and family structure, may also affect parental monitoring, with more educated parents engaging in more effective monitoring of their children (Lareau 2003). Further, the education of parents directly affects food and diet quality (Cade & Booth 1990). Higher educational levels increase the awareness of health issues and the likelihood of healthy food choices for children.
Poor families also tend to live in poor neighborhoods. Although families choose where they live and may select into a particular neighborhood context (Duncan and Raudenbush 1999; Manski 1993), lifestyle and behavioral choices are constrained by the neighborhood context in which families live. Food choices and diet quality depend on the social environment in which food is bought and consumed (Drewnowski & Specter 2004). High diet quality foods can sometimes be more expensive and less accessible for those residing in economically deprived neighborhoods (Morland, Diez Roux & Wing 2006). Because food availability influences consumption, less wealthy minority neighborhoods are at a distinct disadvantage regarding food choice. In addition, low-SES neighborhoods have reduced access to recreational facilities and higher crime rates (Hannon 2005), which limit physical activity (Gordon-Larsen et al. 2006).
Finally, we include important controls for parental obesity status and race/ethnicity in our models because they are related to both adolescent obesity and poverty (Paeratakul et al. 2002; Whitaker et al. 1997).
Data
The National Longitudinal Study of Adolescent Health (Add Health) is an ongoing nationally representative, school-based study of adolescents in grades 7 to 12 that began in 1994. Add Health was designed to explore the causes of health-related behaviors, with an emphasis on the influence of social context. In 1994 Add Health administered an In-School Questionnaire to every student attending school from a nationally representative sample of schools. A sample of 80 high schools and 52 middle schools from the U.S. was selected using a stratified cluster design. A subsample of individuals in these schools participated in the In-Home Interview in 1995 (WI), given an average of eight months after the In-School Survey1, and again in 1996 (WII). In WIII (2001-02) WI respondents were re-interviewed.
A parent was also interviewed in WI. Ultimately, 20,745 in-home interviews were completed in WI with 85% of parents (primarily the mother) also interviewed. At WII, 14,738 in-home interviews were completed (the seniors in WI were not followed-up). In WIII 15,197 eligible original Wave I respondents completed the survey. In WI, the age of participants ranged from 12 to 19 years, in Wave II from 13 to 20 years and WIII from 18 to 26 years. Harris et al. (2003) provides a more detailed description on the Add Health Study.
This study uses data from the WI In -Home and Parent Questionnaires as well as the follow-up WII and WIII surveys. This analysis is therefore limited to adolescents who participated in all three waves of the study and have complete measured height and weight data (height and weight were not measured at WI). Exclusions include seriously disabled respondents and pregnant females, and the few cases with missing data on covariates, resulting in a final analtyic sample of 4,944 females and 4,786 males.
Measures
Table 1 presents the description and sample statistics of the measures we use in the analysis. To retain the largest number of cases in the analysis, we include dummy variables for missing data on various measures.
Table 1.
Variable Descriptions, Means and Standard Errors by Sex
| Female | Male | ||||
|---|---|---|---|---|---|
| Variable | Description | Mean | SE | Mean | SE |
| DEPENDENT VARIABLE | |||||
| Change in Obesity Status | |||||
| Become Obese | Not obese at WII but obese at WIII | 0.14 | 0.007 | 0.12 | 0.007 |
| Stay Obese | Obese at WII & obese at WIII | 0.09 | 0.007 | 0.09 | 0.007 |
| Reduce Obese or Stay Non-Obese (Reference Category) | Obese at WII but not obese at WIII or Not obese at WII & not obese at WIII |
0.77 | 0.011 | 0.79 | 0.009 |
| INDEPENDENT VARIABLES | |||||
| Socioeconomic Disadvantage Measures | |||||
| Welfare/Poverty Status | Welfare receipt prior to the age of 18 and/or Family Income less than $16,000/year |
0.29 | 0.016 | 0.30 | 0.018 |
| Parent Education Less than High School | Highest educated parent completed high school or less | 0.64 | 0.020 | 0.63 | 0.020 |
| Family Structure | |||||
| 2 Biological Parents (Reference Category) | 2 Biological/Adoptive Parents | 0.59 | 0.014 | 0.58 | 0.015 |
| Step family | Step family | 0.17 | 0.007 | 0.16 | 0.006 |
| Single mother | Single mother | 0.20 | 0.010 | 0.19 | 0.012 |
| Single father | Single father | 0.02 | 0.003 | 0.03 | 0.003 |
| Other family structure | Other family structure | 0.03 | 0.004 | 0.03 | 0.004 |
| Trouble Paying Bills | Parent reports not having money to pay the bills at Wave I | 0.15 | 0.009 | 0.15 | 0.010 |
| Missing Trouble Paying Bills | Missing parental report | 0.12 | 0.009 | 0.11 | 0.008 |
| Neighborhood Poverty | Proportion of family households in census track below 1989 poverty level |
0.12 | 0.008 | 0.12 | 0.007 |
| Mediating Measures | |||||
| Parental Monitoring | |||||
| TV | Parent monitors how much TV respondent viewed at Waves I and II |
0.06 | 0.006 | 0.07 | 0.006 |
| Dinner | Parent(s) eat(s) dinner with respondent 5 or more times a week at Waves I and II |
0.47 | 0.015 | 0.48 | 0.016 |
| Low Parent-Child Interaction | Respondent reports engaging in less than two activities with parent(s) in the past 4 weeks at WI |
0.28 | 0.011 | 0.34 | 0.011 |
| No Curfew | Respondent reports having no curfew at WI. | 0.25 | 0.009 | 0.35 | 0.013 |
| Full-time Working Mother | Mother works full time | 0.55 | 0.012 | 0.54 | 0.013 |
| Missing Full-time Working Mother | Missing | 0.03 | 0.003 | 0.03 | 0.003 |
| Physical Activity | Continuous measure of average number of bouts of physical activity, Waves I and II (Range 0-18) |
6.05 | 0.110 | 7.73 | 0.111 |
| Skips Breakfast | Respondent reported usually skips breakfast at WI and reported skips breakfast 0-2 days in a week |
0.13 | 0.007 | 0.09 | 0.007 |
| Inadequate Sleep | Respondent reported usually sleeping less than 7 hours at WI and WII |
0.28 | 0.013 | 0.22 | 0.011 |
| Controls | |||||
| Age | Continuous measure of age at WI. | 14.91 | 0.113 | 15.12 | 0.116 |
| Race/Ethnicity | |||||
| Non-Hispanic White (Reference Category) | Respondent reported black | 0.69 | 0.029 | 0.68 | 0.030 |
| Non-Hispanic Black | Respondent reported white | 0.15 | 0.021 | 0.15 | 0.020 |
| Hispanic | Respondent reported Hispanic | 0.11 | 0.016 | 0.12 | 0.018 |
| Asian | Respondent reported Asian | 0.03 | 0.008 | 0.04 | 0.009 |
| Other | Respondent reported other race/ethnicity | 0.01 | 0.002 | 0.01 | 0.003 |
| Parent Obese | Report of mother or father being obese | 0.21 | 0.008 | 0.22 | 0.009 |
| Missing Parent Obese | Missing report | 0.09 | 0.008 | 0.09 | 0.008 |
| N | 4,944 | 4,786 | |||
Data are weighted.
Socioeconomic Disadvantage Measures
Poverty and/or welfare receipt in childhood and adolescence
Welfare/Poverty status is a dichotomous indicator of any welfare receipt before the age of eighteen or family income less than poverty level. This measure is constructed from data on the family's receipt of public assistance or welfare from WI and WII during adolescence in combination with a retrospective report at WIII on the receipt of welfare and public assistance prior to the age of eighteen. Using data from the WI Parent Questionnaire on reported annual income from 1994, family income is categorized as below poverty level if income was less than $16,000 (roughly the poverty level for a family of four in 1994). We chose a welfare- and income-based measure of poverty over an only income-based measure due to the large proportion of missing data on income (≈ 20%). The experience of poverty or welfare receipt in childhood captures a severe form of deprivation and is our main measure of poverty. Twenty-nine percent of the total sample received welfare prior to the age of eighteen and/or was living below poverty at WI.
Trouble paying bills
Using data from the WI Parent Questionnaire, a dichotomous variable indicates whether the respondent's parent had trouble paying bills. This measure has been used to measure respondent perceptions of inadequate income in previous research (e.g., Conger et al. 1992). About 15% of adolescents at WI lived in households where parents had trouble paying their bills.
Family structure
Rich detail is available on adolescents' living arrangements in adolescence. We classify adolescents into five family structure categories: 1) two biological or adoptive parents (reference category); 2) step family, including both biological mother, step father and biological father, step mother; 3) single mother; 4) single father; and 5) surrogate parents (no biological parent in the household) including foster parents, step parents, grandparents, aunts, uncles, siblings, or other adults who act as parent figures.
Parent education level
Using data from the WI Parent Questionnaire, parents' education is measured as the higher of either the mother's or father's education and is represented as a dummy variable indicating that the highest educated parent received a high school diploma or GED or less.
Neighborhood poverty
Neighborhood poverty comes from WI census tract measures. It is a continuous measure of the proportion of families with income in 1989 below poverty level. On average, respondents lived in communities were 12% of families lived below poverty level.
Mediating Measures
Parental monitoring
We include five measures of parental monitoring. The first measures whether a parent regularly ate dinner with the adolescent during the week at WI and WII. Based on the question, “On how many of the past 7 days was at least one of your parents in the room with you while you ate your evening meal?”, we code responses of 5 or more days per week as a ‘1’ for eating dinner together regularly. Responses of less than 5 days per week are coded ‘0’, not eating dinner together regularly. We then form a longitudinal measure over the WI and WII reports where a ‘1’ indicated that at both waves (i.e., during adolescence), parents and adolescents shared the weekly dinner meal, and ‘0’ otherwise. Given research on the connection between shared family mealtimes and diet quality (Neumark-Sztainer et al. 2003; Videon & Manning 2003), parents who consistently eat dinner with their adolescent during most of the days of the week and at both time points in adolescence display the highest level of monitoring of the food and nutritional choices of the adolescent.
The second measure involves monitoring inactivity levels, and in particular, adolescents' TV viewing. Parental monitoring of TV viewing is also measured at WI and WII by adolescent responses to the question, “Do your parents let you make your own decisions about how much television you watch?” If the parent makes the decision about the amount of TV viewing at both Waves I and II, we code parental monitoring of TV viewing as ‘1’for high monitoring, and ‘0’ otherwise, capturing strong and consistent monitoring across both time points in adolescence. Table 1 indicates that while more than two-thirds of parents regularly share the evening meal with children during adolescence, only a small proportion consistently monitor the amount of TV viewing in adolescence (6%).
Our third measure of monitoring is maternal work status. Work status is measured by whether the mother worked full time using both WI respondent and parent reports. Mothers who worked more than 35 hours per work are coded as working full time. Consistent with census data, 54% of the adolescents at WI had a mother who worked full-time.
The last two measures capture a lack of parental monitoring: low parent-child interaction and no curfew. At WI respondents were asked to report the activities they engaged in with each parent in the past four weeks. Adolescents reported up to nine activities ranging from going shopping to working on a school project, and are coded as having a lack of parent-child interaction if the average number of activities in which they engaged with their parent(s) was less than two in the past four weeks. No curfew comes from WI adolescent responses to the question, “Do your parents let you make your own decisions about the time you must be home on weekend nights?” Respondent are coded as having no curfew if they answered the question affirmatively. A higher percentage of males (35%) than females (25%) had no curfew.
Physical activity
Physical activity is measured by a standard physical activity behavior recall in Add Health that is similar to other self-report questionnaires that have been used and validated in other large scale epidemiological studies (e.g., Andersen et al. 1998). In WI and WII, a series of questions asked about participation in moderate to vigorous physical activity, including skating and cycling, exercise and active sports (5-8 metabolic equivalents or METs), in units of times per week2. One MET represents the energy expenditure associated with quiet sitting. Respondents indicated the number of times in which they engaged in moderate to vigorous physical activity for each set of activities according to the following four categories: 0; 1-2; 3-4; and 5+ times per week. We sum the number of times that the respondent engaged in moderate to vigorous physical activity across the three categories of activities at each wave and then average the number of times across WI and WII to create a measure of the average number of bouts of physical activity during adolescence. This measure ranges from 0 to 18 bouts, with a mean of 6 bouts among female adolescents and almost 8 bouts among male adolescents.
Skips breakfast
Using responses from the WI and WII In-Home Questionnaires, a dummy variable is created to indicate whether the respondent skipped breakfast. This variable indicates whether the respondent reported usually eating nothing for breakfast at WI and eating breakfast zero to two times in the seven days prior to their interview at WII.
Inadequate sleep
Using responses from the WI and WII In-Home Questionnaires, a dummy variable is created to indicate whether the respondent reported usually sleeping less than 7 hours a week at both waves. A higher percentage of females (28%) experienced short sleep duration than males (22%).
Controls
Race/Ethnicity
Race and ethnicity were self-reported at WI. We use a five-category classification: non-Hispanic white (reference category), non-Hispanic black, Non-Hispanic Asian, Hispanic, and other (largely Native American).
Parent obesity status
Using self-reports from the Parent In-Home Questionnaire, a respondent is coded as having an obese parent if either their biological mother and/or biological father reported themselves as obese in response to a question regarding current health problems. About one in five of the parents reported themselves to be obese.
Age
A continuous variable of self-reported age at WI (in years).
Dependent Variable
Body Mass Index (BMI) is calculated from measured height and weight (kg/m2) as an indicator of obesity. BMI is more highly correlated with body fat than any other indicator of height and weight (CDC & DHHS 2006). Adults with a BMI of 25 to 29.9 are categorized as overweight. Adults with a BMI of 30 or more are considered obese (NHLBI 1998).
Obesity is defined differently for children and adults. Age- and sex-specific BMI percentiles are used as growth references during childhood and adolescence because BMI changes at different rates by age and sex during normal developmental growth. The International Obesity Task Force (IOTF) developed BMI curves, which link childhood and adolescent BMI centiles to adult cut off points of BMI of 25 and 30 kg/m2, and thus, allow greater consistency in the youth versus adult definitions. The BMI curves provide good comparative reference data during the transition period between adolescence and young adulthood (Cole et al. 2000). Because we investigate the incidence of obesity in this transition period, we use the IOTF measures to determine obesity status in this analysis.
Using the IOTF cutoffs, we define obesity at WII and WIII using BMI calculated from measured height and weight. We identify individuals as obese if their BMI falls at or above the age- and sex-specific, IOTF 30 kg/m2 cutpoint in adolescence at WI. For the young adults at WIII, we consistently use the adult BMI cut point of 30 kg/m2. We then form a 2X2 table of obesity status at WII by obesity status at WIII to identify incidence, reversal and continuity in obesity and non-obesity status from adolescence into young adulthood. Our dependent variable contains four groupings that capture change and continuity in obesity status from Wave II to WIII: Become Obese (respondent not obese at WII but obese at WIII); Stay Obese (obese at both WII and WIII); Reduce Obesity (obese at WII but not obese at WIII); and Stay Non-Obese (not obese at both WII and WIII). Because the proportion of individuals in the transition group of reduce obesity was too small to analyze and had a similar relationship with poverty, we combined this group with the stay non-obese group. Over three-fourths of the sample travels this low-risk grouping of remaining non-obese or reducing obesity from adolescence into young adulthood (Table 1). A slightly greater percentage of females become obese (14%) than males (12%) as they enter young adulthood and a similar percentage (9%) remain obese over time. These two groups capture the onset of obesity at two different life stages: those consistently obese are already obese in adolescence, and thus likely experience onset of obesity in early childhood or as they enter early adolescence; whereas those who became obese at WIII experienced onset as they become young adults.
Methods and Analysis Plan
We begin with descriptive analysis of the relationship between our poverty measures and obesity outcomes. We then employ multinomial logistic regression to estimate the relationships displayed in our conceptual model. Multinomial regression is appropriate when the dependent variable is an unordered nominal variable with n categories. The procedure estimates the log of the ratio of the probability of being in the nth category relative to a base category (stay non-obese/reduce obesity), where the effects of independent variables are measured by the relative risk or odds (Long 1997). The fundamental model takes the form:
Multivariate analysis begins with a baseline model of the relationship between poverty/welfare status and obesity transitions and continuity. Model 2 enters the additional measures of socioeconomic disadvantage. Model 3 enters the intervening mechanisms displayed in Figure 1. Model 4 enters the remaining covariates as control variables. Age is controlled for in all models.
Descriptive Analysis
Table 2 shows the relationship between poverty/welfare experience and cross-sectional and longitudinal measures of obesity status at WII and WIII for females and males. Poverty/welfare status during childhood and adolescence are highly related to subsequent obesity status in adolescence and young adulthood for girls, but not at all for boys. Among girls who ever experienced welfare receipt or poverty, 14% are obese during late adolescence at WII, compared to 9% who never experienced welfare receipt or poverty in childhood. The difference is even greater at WIII during early adulthood; 30% of girls with any poverty or welfare experience in childhood are obese compared to 20% with no poverty or welfare experience.
Table 2.
Percent Distribution of Obesity Status by Childhood Welfare/Poverty Experience by Sex
| Female (N=4,944) |
Male (N=4,786) |
|||
|---|---|---|---|---|
| No Welfare/Poverty |
Yes Welfare/Poverty |
No Welfare/Poverty |
Yes Welfare/Poverty |
|
| Cross-sectional Measures of Obesity | ||||
| Obese WII | 0.09*** | 0.14*** | 0.11 | 0.13 |
| Obese WIII | 0.20*** | 0.30*** | 0.20 | 0.23 |
| Longitudinal Measures of Obesity | ||||
| Become Obese | 0.12*** | 0.17*** | 0.12 | 0.12 |
| Stay Obese | 0.08*** | 0.13*** | 0.09 | 0.11 |
| Stay Non- or Reduce Obese | 0.80*** | 0.70*** | 0.80 | 0.77 |
Data are weighted.
Distributions exclude missing
significant at .05 level
significant at .01 level
significant at .001 level
Table 2 also shows the relationship between our poverty measure and longitudinal obesity transitions and continuity constructed from obesity status at WII and WIII. Again we only find significant associations for females. Poverty and welfare receipt during childhood are positively associated with becoming obese and staying obese from adolescence into young adulthood, and negatively associated with the low risk categories of remaining non-obese or reducing obesity. The largest differentials are found in the low-risk group of ending up non-obese in young adulthood where poverty/welfare experiences in childhood put adolescents at a strong disadvantage for traveling this low-risk obesity pathway.
Table 3 shows the bivariate relationship between poverty/welfare status and our mediating mechanisms. The results demonstrate that our mediating mechanisms are highly associated with welfare/poverty status, suggesting that disadvantage may operate through these factors. A higher proportion of poor adolescents have lower levels of parental monitoring measured by TV monitoring (for females only), sharing dinner meals and parent-child interaction. Adolescents from poor families engage in lower levels of physical activity and are less likely to get adequate amounts of sleep. In addition, a higher proportion of females who are on welfare in childhood regularly skip breakfast compared to females who are not on welfare in childhood. There are no differences in curfew by welfare/poverty status.
Table 3.
Means of Mediating Mechanisms by Childhood Welfare/Poverty Experience
| Female (N=4,944) |
Male (N=4,786) |
|||
|---|---|---|---|---|
| No Welfare/Poverty |
Yes Welfare/Poverty |
No Welfare/Poverty |
Yes Welfare/Poverty |
|
| TV Monitoring | 0.07* | 0.04* | 0.07 | 0.07 |
| Dinner Monitoring | 0.49*** | 0.40*** | 0.52*** | 0.40*** |
| Low Parent-Child Interaction | 0.26*** | 0.33*** | 0.30*** | 0.42*** |
| No Curfew | 0.25 | 0.25 | 0.35 | 0.35 |
| Full-time Working Mother | 0.59*** | 0.46*** | 0.57*** | 0.45*** |
| Physical Activity | 6.25*** | 5.53*** | 7.86** | 7.45** |
| Skips Breakfast | 0.11*** | 0.18*** | 0.08 | 0.10 |
| Inadequate Sleep | 0.27* | 0.31* | 0.21* | 0.24* |
Data are weighted.
Distributions exclude missing
significant at .05 level
significant at .01 level
significant at .001 level
Multivariate Analysis
We present results from our multivariate analysis in the next set of tables. We employ multinomial logistic regression to estimate the effects of poverty/welfare status, intervening mechanisms, and control variables shown in our conceptual model in Figure 1. Age is controlled in all models (coefficients not shown). We conduct analysis for females and males separately. Table 4 presents results for family welfare/poverty effects for females.
Table 4.
Estimated Multinomial Regression Coefficients for Obesity Change and Continuity for Females (N=4,944)
| (Reference Category is “Stay Non-Obese or Reduce Obese”) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
| Become Obese |
Stay Obese |
Become Obese |
Stay Obese |
Become Obese |
Stay Obese |
Become Obese |
Stay Obese |
|
| Socioeconomic Disadvantage Measures | ||||||||
| Welfare/Poverty Status | 0.450 *** | 0.532 ** | 0.229 | 0.160 | 0.211 | 0.083 | 0.223 | 0.096 |
| (0.120) | (0.151) | (0.125) | (0.155) | (0.124) | (0.152) | (0.124) | (0.159) | |
| Parent Education Less than High School | 0.456 ** | 0.481 ** | 0.436 ** | 0.421 ** | 0.434 ** | 0.426 ** | ||
| (0.136) | (0.152) | (0.137) | (0.152) | (0.140) | (0.160) | |||
| Family Structure | ||||||||
| Step family | 0.071 | −0.475 * | 0.052 | −0.440 * | 0.043 | −0.400 * | ||
| (0.141) | (0.180) | (0.145) | (0.182) | (0.144) | (0.197) | |||
| Single mother | 0.155 | −0.021 | 0.113 | −0.021 | 0.061 | −0.096 | ||
| (0.159) | (0.178) | (0.165) | (0.183) | (0.171) | (0.194) | |||
| Single father | 0.225 | −0.201 | 0.784 | −0.040 | 0.793 | −0.063 | ||
| (0.339) | (0.464) | (0.529) | (0.532) | (0.539) | (0.513) | |||
| Other family structure | 0.229 | −0.279 | 0.233 | −0.342 | 0.238 | −0.217 | ||
| (0.305) | (0.371) | (0.316) | (0.379) | (0.330) | (0.375) | |||
| Trouble Paying Bills | 0.012 | 0.261 | 0.011 | 0.265 | −0.029 | 0.192 | ||
| (0.153) | (0.181) | (0.153) | (0.176) | (0.153) | (0.177) | |||
| Neighborhood Poverty | 0.071 | 0.235 *** | 0.062 | 0.245 *** | 0.025 | 0.194 ** | ||
| (0.047) | (0.048) | (0.049) | (0.052) | (0.058) | (0.069) | |||
| Mediating Measures | ||||||||
| Parental Monitoring | ||||||||
| TV | −0.062 | −0.541 | −0.069 | −0.543 | ||||
| (0.239) | (0.391) | (0.243) | (0.413) | |||||
| Dinner | −0.104 | 0.288 * | −0.080 | 0.310 * | ||||
| (0.128) | (0.152) | (0.126) | (0.157) | |||||
| Low Parent-Child Interaction | 0.202 | −0.043 | 0.215 | −0.016 | ||||
| (0.135) | (0.150) | (0.135) | (0.161) | |||||
| No Curfew | −0.118 | 0.356 * | −0.105 | 0.372 * | ||||
| (0.132) | (0.140) | (0.135) | (0.147) | |||||
| Full-time Working Mother | 0.094 | −0.206 | 0.078 | −0.22 | ||||
| (0.129) | (0.142) | (0.128) | (0.144) | |||||
| Physical Activity | −0.010 | −0.060 * | −0.007 | −0.051 * | ||||
| (0.020) | (0.025) | (0.020) | (0.025) | |||||
| Skips Breakfast | 0.181 | 0.521 ** | 0.203 | 0.595 ** | ||||
| (0.152) | (0.191) | (0.153) | (0.198) | |||||
| Inadequate Sleep | 0.287 * | 0.085 | 0.273 * | 0.021 | ||||
| (0.128) | (0.157) | (0.129) | (0.165) | |||||
| Controls | ||||||||
| Race/Ethnicity | ||||||||
| Non-Hispanic Black | 0.314 | 0.596 ** | ||||||
| (0.192) | (0.209) | |||||||
| Hispanic | 0.232 | 0.384 * | ||||||
| (0.185) | (0.190) | |||||||
| Asian | −0.915 * | −1.950 ** | ||||||
| (0.363) | (0.627) | |||||||
| Other | 0.711 | 0.148 | ||||||
| (0.450) | (0.467) | |||||||
| Parent Obese | 0.657 *** | 1.615 *** | ||||||
| (0.130) | (0.150) | |||||||
| Constant | −2.832 *** | −4.288 *** | −3.140 *** | −4.812 *** | −2.678 *** | −3.856 *** | −2.818 *** | −4.467 *** |
| (0.584) | (0.599) | (0.558) | (0.616) | (0.640) | (0.810) | (0.636) | (0.826) | |
| Pseudo Log Likelihood | −5545254.2 | −5545254.2 | −5463286.4 | −5463286.4 | −5394916.3 | −5394916.3 | −5169884.6 | −5169884.6 |
significant at .05 level
significant at .01 level
significant at .001 level
Note:
Standard Errors are in parentheses
Omitted Categories are: race/ethnicity: white; family structure: two biological parents
Equation includes missing data indicators; these are not shown above.
All models control for age.
Model 1 presents the regression coefficients of welfare/poverty status on obesity pathways. This model replicates the descriptive results in Table 2, indicating that welfare/poverty status significantly increases the odds of becoming and staying obese compared to remaining non-obese/reducing obese by young adulthood. Welfare/poverty status in adolescence is especially strong in keeping females on a path of obesity into young adulthood compared to non-obesity; the relative risk ratio of the coefficient .532 is 1.70, indicating that the odds of staying obese relative to staying non-obese/reducing obese from adolescence into young adulthood is 70% higher if the adolescent lives in poverty or received welfare in adolescence compared to having a family who did not.
Model 2 enters our additional measures of social disadvantage. The results indicate that compositional factors related to poverty confound the effects of welfare/poverty on female obesity transitions and continuity as the coefficients become insignificant in Model 2. Important and well-known differences by neighborhood poverty and parental education are found. Among females, higher neighborhood poverty is associated with higher likelihood of persistent obesity. Low parental education increases the odds that females both become and remain obese in the transition to young adulthood. There is a marginally significant (p=0.054) negative relationship between coming from a stepparent home (compared to a two biological parent home) and staying obese.
Model 3 enters potential mediating mechanisms in the relationship between poverty and obesity, and indicate some mediating influence. Inadequate sleep is significantly related to becoming obese, while having no curfew, skipping breakfast, regularly eating dinner with parents and physical activity are significant for the remain obese versus remain non-obese/reduce obese contrast. Sleeping less than 7 hours on average in adolescence is associated with a higher likelihood of becoming obese from adolescence into young adulthood. Having no curfew and skipping breakfast in adolescence are associated with a higher likelihood of staying obese from adolescence into young adulthood. Surprisingly, eating dinner regularly with parents increases the likelihood of staying obese. Although sharing family meals could be considered a protective mechanism of parental monitoring, it is also a context in which parents may serve as role models for less healthy eating habits. The more physical exercise females get in adolescence, the lower their likelihood of being continuously obese from adolescence to young adulthood. Because poverty is associated with less physical exercise and a higher likelihood of skipping breakfast in adolescence, these intervening variables reduce the size of the poverty coefficient by about 50% for the female category of staying obese. Inadequate sleep, also associated with poverty in adolescence, reduces the size of the poverty coefficient by about 20% for the female incidence of obesity in adulthood. Interestingly, other than lack of curfew and sharing dinner meals, no other direct measures of parental monitoring are significantly related to obesity outcomes. Inadequate sleep and skipping breakfast are subject to some level of parental monitoring because parents are able to control these behaviors through setting bed times and being present for breakfast meals.3
Model 4 enters other covariates associated with both poverty and obesity. Important and well-known differences by race are found. Black and Hispanic females are more likely than white females to remain obese from adolescence into young adulthood. Asian females are less likely to become obese or to stay obese from adolescence into young adulthood. Finally, a strong intergenerational effect is found for parental obesity increasing the odds that females remain obese from adolescence into young adulthood, suggesting both unmeasured family environment influences as well as genetic influence in the continuity of obesity both over generations and across time. It is also important to note that the effects of the intervening mechanisms significant in Model 3 remain significant with the addition of controls in Model 4.4
Table 5 shows results for the same models for males. Consistent with the results in Table 2, there are no significant effects of poverty/welfare status on male obesity transitions and continuity in Model 1. However, Model 2 indicates that low parental education and neighborhood poverty increase the likelihood of staying obese from adolescence and into young adulthood for males. In addition, males from a family with no biological parent present (with the exception of a two parent adoptive family) compared to a two-biological parent family are more likely to become obese than to remain non-obese. In Model 3 we find a similar protective effect of physical exercise that reduces the odds of remaining obese from adolescence into young adulthood compared to remaining non-obese. Skipping breakfast increases the likelihood of both becoming and staying obese for males. Inadequate sleep increases the likelihood of staying obese for males. Similar to females, we find that sharing dinner regularly with parents increases the likelihood of males remaining obese. Given the null effects of poverty/welfare status at the individual level on obesity for males, we cannot determine mediating effects. It should be noted that parental education effects were mediated by these intervening factors for both males and females. In Model 4 we see equally strong intergenerational effects of parental obesity for males in predicting the odds of obesity pathways, especially the persistence of obesity pathway from adolescence into young adulthood. Surprisingly, there are no statistically significant effects of race/ethnicity.
Table 5.
Estimated Multinomial Regression Coefficients for Obesity Change and Continuity for Males (N=4,786)
| (Reference Category is “Stay Non-Obese or Reduce Obese”) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
| Become Obese |
Stay Obese |
Become Obese |
Stay Obese |
Become Obese |
Stay Obese |
Become Obese |
Stay Obese |
|
| Socioeconomic Disadvantage Measures | ||||||||
| Welfare/Poverty Status | 0.070 | 0.261 | −0.079 | 0.040 | −0.062 | 0.051 | −0.098 | −0.001 |
| (0.133) | (0.159) | (0.146) | (0.181) | (0.147) | (0.172) | (0.149) | (0.179) | |
| Parent Education Less than High School | 0.073 | 0.467 ** | 0.083 | 0.422 ** | 0.070 | 0.390 ** | ||
| (0.121) | (0.147) | (0.122) | (0.141) | (0.120) | (0.141) | |||
| Family Structure | ||||||||
| Step family | 0.219 | −0.281 | 0.209 | −0.281 * | 0.259 | −0.209 | ||
| (0.165) | (0.219) | (0.173) | (0.214) | (0.176) | (0.211) | |||
| Single mother | 0.052 | −0.143 | 0.027 | −0.152 | 0.023 | −0.166 | ||
| (0.180) | (0.191) | (0.188) | (0.191) | (0.187) | (0.198) | |||
| Single father | 0.166 | −0.570 | 0.192 | −0.159 | 0.276 | −0.017 | ||
| (0.313) | (0.499) | (0.449) | (0.703) | (0.462) | (0.783) | |||
| Other family structure | 0.860 ** | 0.190 | 0.846 ** | 0.135 | 0.914 ** | 0.240 | ||
| (0.273) | (0.384) | (0.280) | (0.383) | (0.287) | (0.384) | |||
| Trouble Paying Bills | −0.013 | 0.076 | 0.007 | 0.110 | −0.031 | 0.059 | ||
| (0.183) | (0.240) | (0.184) | (0.237) | (0.182) | (0.245) | |||
| Neighborhood Poverty | 0.096 | 0.171 * | 0.108 | 0.190 ** | 0.100 | 0.185 * | ||
| (0.062) | (0.068) | (0.061) | (0.066) | (0.072) | (0.072) | |||
| Mediating Measures | ||||||||
| Parental Monitoring | ||||||||
| TV | −0.208 | −0.510 | −0.215 | −0.481 | ||||
| (0.226) | (0.368) | (0.225) | (0.370) | |||||
| Dinner | 0.130 | 0.353 * | 0.112 | 0.305 * | ||||
| (0.119) | (0.151) | (0.122) | (0.153) | |||||
| Low Parent-Child Interaction | −0.130 | −0.160 | −0.123 | −0.153 | ||||
| (0.146) | (0.160) | (0.147) | (0.162) | |||||
| No Curfew | −0.022 | 0.053 | −0.040 | 0.017 * | ||||
| (0.109) | (0.128) | (0.111) | (0.138) | |||||
| Full-time Working Mother | 0.058 | 0.047 | 0.044 | 0.031 | ||||
| (0.115) | (0.135) | (0.118) | (0.137) | |||||
| Physical Activity | −0.005 | −0.075 *** | −0.003 | −0.071 ** | ||||
| (0.019) | (0.021) | (0.019) | (0.021) | |||||
| Skips Breakfast | 0.667 *** | 0.941 *** | 0.627 ** | 0.872 *** | ||||
| (0.181) | (0.206) | (0.184) | (0.195) | |||||
| Inadequate Sleep | 0.107 | 0.450 * | 0.053 | 0.370 | ||||
| (0.124) | (0.177) | (0.126) | (0.181) * | |||||
| Controls | ||||||||
| Race/Ethnicity | ||||||||
| Non-Hispanic Black | 0.050 | −0.001 | ||||||
| (0.202) | (0.270) | |||||||
| Hispanic | −0.013 | −0.003 | ||||||
| (0.174) | (0.207) | |||||||
| Asian | 0.170 | −0.221 | ||||||
| (0.265) | (0.433) | |||||||
| Other | 0.566 | 0.236 | ||||||
| (0.521) | (0.600) | |||||||
| Parent Obese | 0.759 *** | 1.236 *** | ||||||
| (0.133) | (0.125) | |||||||
| Constant | −3.687 *** | −2.243 *** | −3.773 *** | −2.607 *** | −3.637 *** | −1.192 | −3.799 *** | −1.431 |
| (0.543) | (0.797) | (0.555) | (0.786) | (0.634) | (1.036) | (0.638) | (1.048) | |
| Pseudo Log Likelihood | −5781917.9 | −5781917.9 | −5723613.8 | −5723613.8 | −5616010.8 | −5616010.8 | −5468052.8 | −5468052.8 |
significant at .05 level
significant at .01 level
significant at .001 level
Note:
Standard Errors are in parentheses
Omitted Categories are: race/ethnicity: white; family structure: two biological parents
Equation includes missing data indicators; these are not shown above.
Discussion and Conclusion
Using nationally representative data, we examine the relationship between poverty/welfare experienced in childhood and adolescence and obesity transitions and continuity from adolescence into young adulthood. Our research is one of the few studies to examine socioeconomic obesity determinants among adolescents; for most research on obesity focuses on adults, or research that does examine children uses non-representative data that cannot be generalized to the broader population of young people in America. Further, we use a multi-dimensional set of indicators of SES in recognition of the interrelated types of association these factors may have with obesity. We also contribute to the scant research on obesity among children by using a longitudinal design that allows us to trace changes and continuity in obesity beginning in adolescence and continuing through the transition to young adulthood. Our longitudinal design enables us to sort out the temporal ordering of the effects by measuring poverty experiences in childhood and adolescence, the intervening mechanisms through which poverty may operate during adolescence, and obesity outcomes as measures of change and continuity from adolescence to young adulthood. Finally, we use dynamic measures of both poverty and obesity, and account for the additional indicators of socioeconomic deprivation that co-occur with poverty.
There are several limitations to the current work. The Add Health survey does not include a 24-hour dietary recall or direct measures of physical activity, thus precluding study of biological pathways through which poverty may operate. However, we are not attempting to model energy balance in this study, but rather examine longitudinal changes in obesity status over time. We are also limited in that the earlier waves of Add Health begin at adolescence, and there is a fair amount of pre-existing overweight. As such, we are unable to determine exactly when poverty might have begun to influence persistent obesity status. However, our longitudinal design captures incident obesity and allows us to look at time-varying impacts of poverty a heretofore understudied relationship. Our sample excludes individuals with missing data, which can be a concern, but our analysis of “missingness” indicates little bias to our results.5
Perhaps our most noteworthy finding is that poverty influenced obesity transitions and continuity for females only; there are no effects of poverty on obesity among males. However, poverty at the neighborhood level and low parental education strongly influences obesity continuity for both males and females. Their close correlation with poverty and welfare receipt swamp the direct effects of welfare/poverty for females. In addition, neighborhood poverty influences obesity risks beyond the influence of individual level poverty, highlighting the important role of neighborhood environment in affecting the health outcomes of youth.
The male-female difference in the relationship between poverty and obesity is an important finding. Although documented in previous research, it remains unclear why these differences exist between males and females. A few explanations have been offered in regards to the adult population that can be extended to the adolescent population. Low-income men might engage in higher levels of physical activity because they engage in more manual occupational labor (Chang and Lauderdale 2005). Similarly, low-income boys might engage in more physical activity playing outside than low-income girls who might tend to stay inside due to household responsibilities and safety. In addition, the link between income and weight-related ideals, which is frequently used to explain the inverse association observed among white females (Jeffery and French 1996), may not exist for males or vary across groups.
Although we see fairly divergent social processes influencing the development of obesity among females compared to males in regards to the influence of welfare/poverty, the effects of other elements of disadvantage (e.g., parental education, family structure), parental monitoring (e.g., dinner meals, curfew) and other risk behaviors (e.g., physical activity, diet, sleep) related to parental monitoring are strikingly similar. This highlights the importance of the family context in obesity transitions and continuity for both males and females across the life course.
The dynamics of obesity during the transition to adulthood reveal that the majority of adolescents, over three-quarters, are not obese in adolescence and remain non-obese by young adulthood. A small proportion who are obese in adolescence reduce their weight to be non-obese by young adulthood. The remaining two obesity pathways forebode health risks in adulthood: about 13% become obese during the transition to adulthood and another 9% are obese in adolescence and remain obese in young adulthood.
Among females, poverty/welfare receipt patterns are strongly related to obesity, increasing the risks of obesity in pathways of becoming obese or staying obese from adolescence into young adulthood. When we examine the potential mediating mechanisms through which poverty may operate on obesity, we find important intervening effects of certain aspects of parental monitoring, physical activity, inadequate sleep and skipping breakfast. We argue that skipping breakfast and inadequate sleep and important health habits that are also subject to parental monitoring because they can be directly controlled by parents via setting bedtimes and being present for breakfast meals, especially among younger adolescents.
Consistent with prior research, we find strong and consistent effects of physical activity as a mediator of poverty. Thus, poverty and welfare receipt are associated with less physical exercise among children, especially among girls, placing children at risk for obesity through this important pathway. The effects of race, ethnicity, and parental obesity were expected and consistent with the obesity literature.
By focusing on intervening mechanisms through which poverty may affect obesity, our research contributes to an understanding of the processes of obesity development during childhood and adolescence. Our findings point to possible interventions that can combat obesity among young people who are poor. Findings about physical activity and skipping breakfast are not new, and these recommendations are widespread in the public informational system about weight management, though programs in neighborhoods and schools might further encourage or require physical exercise among children. Schools could also teach the importance of eating breakfast and provide free healthful breakfast to adolescents, especially low-income adolescents. In addition, behaviors such as physical activity and dietary habits are predominantly formed in adolescence and continue into adulthood (Gillman 2004). Adolescence might be an ideal time to alter the risk of future obesity, cardiovascular disease and diabetes through short-term interventions (Lawlor & Chaturvedi 2006).
The Add Health data replicate clinical as well as other survey research linking low levels of sleep to the onset of obesity. Low levels of sleep in adolescence increases the likelihood of obesity incidence (for females) and continuity (for males) from adolescence into young adulthood. Related to sleep, having no curfew is associated with increasing risks of persistent obesity for females. Short-term interventions could also be put in place to educate parents about the importance of setting curfews and ensuring that their children get adequate amounts of sleep. Lastly, policy changes to increase affordable and accessible healthy food and recreation options in low-income communities are imperative (Nestle & Jacobson 2000).
Acknowledgments
We gratefully acknowledge research support from the Carolina Population Center to Lee through an NICHD pre-doctoral fellowship and from the National Institute of Child Health and Human Development to Harris through grant P01 HD31921 as part of the Add Health program project and grant U01 HD37558 as part of the NICHD Family and Child Well-being Research Network, and to Penny Gordon-Larsen through grant K01 HD044263-01 from the NICHD. This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P01-HD31921 from the National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining data files from Add Health should contact Add Health, Carolina Population Center, 123 W. Franklin Street, Chapel Hill, NC 27516-2524 (www.cpc.unc.edu/addhealth/contract.html).
Footnotes
This paper was presented previously at the 100th Annual Meeting of the American Sociological Association, Philadelphia, PA, August, 2005.
Selected special oversamples (including ethnic, disabled, and sibling over-samples) were also included in the in-home sample.
The questions for moderate to vigorous physical activity are: 1) During the past week, how many times did you go roller-blading, roller-skating, skate-boarding, or bicycling?; 2) During the past week, how many times did you play an active sport, such as baseball, softball, basketball, soccer, swimming, or football?; and 3) During the past week, how many times did you do exercise, such as jogging, walking, karate, jumping rope, gymnastics or dancing?
We also ran models including welfare/poverty status and our intervening mechanisms (excluding additional socioeconomic measures). Welfare/poverty was mediated by similar intervening factors as reported in Model 3, but remained significant.
We also ran models for females controlling for parity given weight gains associated with fertility. The results did not substantively change.
Our analysis is limited to adolescents who participated in all three waves of the study and have complete measured height and weight data. We exclude seriously disabled respondents, pregnant females, and individuals missing sampling weights or had missing data on covariates, which generally came from missing data on the parent questionnaire. We ran basic descriptive statistics (including, race/ethnicity, sex, age, family structure and immigrant generation) of those individuals with missing data and who were excluded for the reasons stated above. Although we do not include immigrant generation in our analysis, our missing sample has a much larger percentage of first generation immigrants (10%) than our non-missing sample (5%). This is due to the fact that a larger proportion of parents of first and second generation immigrant respondents did not complete the parent questionnaire. In addition, a larger proportion of blacks (24%), Hispanics (18%) and Asians (6%) were represented among those with missing data compared to our sample without missing data. This means that the missing sample is overrepresented by racial/ethnic minorities. The overrepresentation among Hispanics and Asians may be due to a higher proportion of first and second generation immigrants in the missing sample. The sample is also slightly overrepresented by non-two biological parent households. Mean age for the missing data sample is about a year older than our sample without missing data. In general, descriptive statistics indicate that individuals with missing data come from slightly more vulnerable disadvantaged minority groups. Thus, the effect sizes in this analysis may be somewhat underestimated, assuming that the addition of disadvantaged sample members would strengthen our results. Nevertheless, we do not suspect that missingness biases the parameter estimates based on Add Health analysis of attrition bias which shows little to no bias (Chantala, Kalsbeek & Andraca 2004).
REFERENCES
- Alaimo K, Olson CM, Frongillo EA., Jr. Low family income and food insufficiency in relation to overweight in US children: Is there a paradox? Archives of Pediatrics and Adolescent Medicine. 2001;155:1161–1167. doi: 10.1001/archpedi.155.10.1161. [DOI] [PubMed] [Google Scholar]
- Andersen RE, Crespo CJ, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children: Results from the third national health and nutrition examination survey. Journal of the American Medical Association. 1998;279:938–942. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- Berkey CS, Rockett HR, Gillman MW, Field AE, Colditz GA. Longitudinal study of skipping breakfast and weight change in adolescents. International Journal of Obesity. 2003;27:1258–1266. doi: 10.1038/sj.ijo.0802402. [DOI] [PubMed] [Google Scholar]
- Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–549. [PubMed] [Google Scholar]
- Boutelle K, Neumark-Sztainer D, Story M, Resnick M. Weight control behaviors among obese, overweight, and nonoverweight adolescents. Journal of Pediatric Psychology. 2002;27:531–540. doi: 10.1093/jpepsy/27.6.531. [DOI] [PubMed] [Google Scholar]
- Cade J, Booth S. What can people eat to meet the dietary goal and how much does it cost? Journal of Human Nutrition and Dietetics. 1990;3:199–207. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) U.S. Department of Health and Human Services (DHHS) BMI—body mass index. Centers for Disease Control. 2006 Retrieved September 21, 2006, from http://www.cdc.gov/nccdphp/dnpa/bmi/index.htm.
- Chang VW, Lauderdale DS. Income disparities in body mass index and obesity in the United States, 1971-2002. Archives of Internal Medicine. 2005;165:2122–2128. doi: 10.1001/archinte.165.18.2122. [DOI] [PubMed] [Google Scholar]
- Chantala K, Kalsbeek WD, Andraca E. Non-response in wave III of the Add Health study. Carolina Population Center. 2004 Retrieved April 15, 2008, from http://www.cpc.unc.edu/projects/addhealth/files/W3nonres.pdf.
- Cole TJ, Bellizi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. British Medical Journal. 2000;320:1–6. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on National Statistics (CNSTAT) Food insecurity and hunger in the United States: An assessment of the measure. The National Academies Press; Washington: 2006. [Google Scholar]
- Conger RD, Conger KJ, Elder GH, Jr., Lorenz FO, Simons RL, Whitbeck LB. A family process model of economic hardship and adjustment of early adolescent boys. Child Development. 1992;63:526–541. doi: 10.1111/j.1467-8624.1992.tb01644.x. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. American Journal of Clinical Nutrition. 2004;79:6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- Duncan GJ, Brooks-Gunn J. Consequences of growing up poor. Russell Sage Foundation; New York: 1997. [Google Scholar]
- Duncan GJ, Cole RD. Years of poverty, years of plenty: The changing economic fortunes of American workers and families. Survey Research Center, Institute for Social Research, the University of Michigan; Ann Arbor: 1984. [Google Scholar]
- Duncan GJ, Raudenbush SW. Assessing the effects of context in studies of child and youth development. Educational Psychologist. 1999;34:29–41. [Google Scholar]
- Elder GH., Jr. The life course as developmental theory. Child Development. 1998;69:1–12. [PubMed] [Google Scholar]
- Epstein LH, Saelens BE, Myers MD, Vito D. Effects of decreasing sedentary behaviors on activity choice in obese children. Health Psychology. 1997;16:107–113. doi: 10.1037//0278-6133.16.2.107. [DOI] [PubMed] [Google Scholar]
- Evans GW. The environment of childhood poverty. American Psychologist. 2004;59:77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Restricting access to foods and children's eating. Appetite. 1999;32:405–419. doi: 10.1006/appe.1999.0231. [DOI] [PubMed] [Google Scholar]
- Frongillo E. Understanding obesity and program participation in the context of poverty and food insecurity. Journal of Nutrition. 2003;133:2117–2118. doi: 10.1093/jn/133.7.2117. [DOI] [PubMed] [Google Scholar]
- Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: Analyses of the NHANES I. Sleep. 2005;28:1289–1296. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- Gibson D. Long-term food stamp program participation is differentially related to overweight in young girls and boys. Journal of Nutrition. 2004;134:372–379. doi: 10.1093/jn/134.2.372. [DOI] [PubMed] [Google Scholar]
- Gillman MW. A lifecourse approach to obesity. In: Kuh D, Ben-Shlomo Y, editors. A life course approach to chronic disease epidemiology. 2nd edition Oxford University Press; New York: 2004. pp. 189–217. [Google Scholar]
- Goodman E, Adler NE, Daniels SR, Morrison JA, Slap GB, Dolan LM. Impact of objective and subjective social status on obesity in a biracial cohort of adolescents. Obesity Research. 2003;11:1018–1026. doi: 10.1038/oby.2003.140. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM. Five-year obesity incidence in the transition period between adolescence and adulthood: The national longitudinal study of adolescent health. American Journal of Clinical Nutrition. 2004a;80:569–575. doi: 10.1093/ajcn/80.3.569. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Popkin BM. Longitudinal physical activity and sedentary behavior trends: Adolescence to adulthood. American Journal of Preventive Medicine. 2004b;27:277–283. doi: 10.1016/j.amepre.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- Gortmaker SL, Sobal AM, Peterson K, Colditz CA, Dietz WH. Television viewing as a cause of increasing obesity among children in the United States. Archives of Pediatrics and Adolescent Medicine. 1996;150:536–562. doi: 10.1001/archpedi.1996.02170290022003. [DOI] [PubMed] [Google Scholar]
- Haas JS, Lee LB, Kaplan CP, Sonneborn D, Phillips KA, Liang S. The association of race, socioeconomic status, and health insurance status with prevalence of overweight among children and adolescents. American Journal of Public Health. 2003;93:2105–2110. doi: 10.2105/ajph.93.12.2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannon LE. Extremely poor neighborhoods and homicide. Social Science Quarterly. 2005;86:1418–1434. [Google Scholar]
- Harris KM, Florey F, Tabor JW, Bearman PS, Jones J, Udry JR. The national longitudinal study of adolescent health: research design. 2003 Retrieved September 21, 2004, from http://www.cpc.unc.edu/projects/addhealth/design.html.
- Jacobson KC, Crockett LJ. Parental monitoring and adolescent adjustment: An ecological perspective. Journal of Research on Adolescence. 2000;10:65–97. [Google Scholar]
- Jeffery RW, French SA. Socioeconomic status and weight control practices among 20- to 45-year-old women. American Journal of Public Health. 1996;1996:1005–1010. doi: 10.2105/ajph.86.7.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones DJ, Forehand R, Brody G, Armistead L. Parental monitoring in African American, single mother-headed families: An ecological approach to the identification of predictors. Behavior Modification. 2003;27:435–457. doi: 10.1177/0145445503255432. [DOI] [PubMed] [Google Scholar]
- Lareau A. Unequal childhoods: Race, class and family life. University of California Press; Berkeley: 2003. [Google Scholar]
- Lawlor DA, Chatuverdi N. Treatment and prevention of obesity—Are there critical periods for intervention? International Journal of Epidemiology. 2006;35:3–9. doi: 10.1093/ije/dyi309. [DOI] [PubMed] [Google Scholar]
- Long SJ. Regression models for categorical and limited dependent variables. SAGE Publications Inc.; Thousand Oaks: 1997. [Google Scholar]
- Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annual Review of Public Health. 2005;26:1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- Manski C. Identification of endogenous social effects: The reflection problem. Review of Economic Studies. 1993;60:531–542. [Google Scholar]
- McLanahan SS. DHHS Pub (PHS) 95-1257, Report to congress on out-of-wedlock childbearing. National Center for Health Statistics; Hyattsville: 1995. The consequences of nonmarital childbearing for women.”; pp. 229–239. [Google Scholar]
- Lindsay McLaren. Socioeconomic status and obesity. Epidemiologic Reviews. 2007;29:29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. Trends in the association of poverty with overweight among US adolescents, 1971-2004. Journal of the American Medical Association. 2006;295:2385–2393. doi: 10.1001/jama.295.20.2385. [DOI] [PubMed] [Google Scholar]
- Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. American Journal of Preventive Medicine. 2002;22:23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- Morland K, Diez Roux A, Wing S. Supermarkets, other food stores, and obesity: The atherosclerosis risk in communities study. American Journal of Preventive Medicine. 2006;30:333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- NHLBI NHLBI expert panel on the identification, evaluation, and treatment of overweight and obesity in adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Obesity Research. 1998;6(Suppl):51S–209S. [PubMed] [Google Scholar]
- Nelson JA, Chiasson MA, Ford V. Childhood overweight in New York City WIC population.”. Research and Practice. 2004;94:458–462. doi: 10.2105/ajph.94.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nestle M, Jacobson MJ. Halting the obesity epidemic: A public health policy approach. Public Health Reports. 2000;115:12–24. doi: 10.1093/phr/115.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Story M, Perry C. Correlates of unhealthy weight control behaviors among adolescent girls and boys: Implications for the primary prevention of disordered eating. Health Psychology. 2003;22(1):88–98. doi: 10.1037//0278-6133.22.1.88. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LRC, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004.”. Journal of the American Medical Association. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Paeratakul S, Lovejoy JC, Ryan DH, Bray GA. The relation of gender, race and socioeconomic status to obesity and obesity comorbidities in a sample of US adults. International Journal of Obesity. 2002;26:1205–1210. doi: 10.1038/sj.ijo.0802026. [DOI] [PubMed] [Google Scholar]
- Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, Kelnar CJH. Health consequences of obesity. Archives of Disease in Childhood. 2003;88:748–752. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer JA. Consequences of marital dissolution for children. Annual Review of Sociology. 1994;20:235–266. doi: 10.1146/annurev.so.20.080194.001315. [DOI] [PubMed] [Google Scholar]
- Shanahan MJ. Pathways to adulthood in changing societies: Variability and mechanisms in life course perspective. Annual Review of Sociology. 2000;26:667–692. [Google Scholar]
- Siega-Riz AM, Popkin BM, Carson T. Three squares or mostly snacks what do teens really eat?: A sociodemographic study of meal patterns. The Journal of Adolescent Health. 1997;22:29–36. doi: 10.1016/S1054-139X(97)00125-0. [DOI] [PubMed] [Google Scholar]
- Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine. 2004;141:846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics. 1999;103:e85. doi: 10.1542/peds.103.6.e85. Retrieved October 18, 2005, from http://pediatrics.aappublications.org/cgi/reprint/103/6/e85. [DOI] [PubMed]
- Stunkard AJ. Obesity and socioeconomic status—A complex relation. The New England Journal of Medicine. 1993;329:1036–1037. doi: 10.1056/NEJM199309303291411. [DOI] [PubMed] [Google Scholar]
- Videon TM, Manning CK. Influences on adolescent eating patterns: The importance of family meals. Journal of Adolescent Health. 2003;32:365–373. doi: 10.1016/s1054-139x(02)00711-5. [DOI] [PubMed] [Google Scholar]
- Wang Y. Cross-national comparison of childhood obesity: The epidemic and the relationship between obesity and socioeconomic status. International Journal of Epidemiology. 2001;30:1129–1136. doi: 10.1093/ije/30.5.1129. [DOI] [PubMed] [Google Scholar]
- Wang y., Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. American Journal of Clinical Nutrition. 2006;84:707–716. doi: 10.1093/ajcn/84.4.707. [DOI] [PubMed] [Google Scholar]
- Wilson WJ. The truly disadvantaged. University of Chicago Press; Chicago: 1987. [Google Scholar]
- Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. New England Journal of Medicine. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- Zhang Q, Wang Y. Socioeconomic inequality of obesity in the United States: Do gender, age and ethnicity matter? Social Science and Medicine. 2003;58:1–17. doi: 10.1016/s0277-9536(03)00288-0. [DOI] [PubMed] [Google Scholar]