Abstract
Cytogenetics has an important impact on the prognosis of patients undergoing allogeneic hematopoietic stem cell transplantation (HSCT) for AML or MDS. However, it is unclear whether currently accepted cytogenetic risk groups, which were established for patients treated mostly with standard therapy, are optimally discriminating for patients undergoing HSCT. Also, the impact of cytogenetics in the growing population of patients with therapy-related disease has not been completely elucidated. In this study, we retrospectively analyzed data on 556 patients with AML or MDS transplanted at our institution. We examined, in multivariate analyses, the contribution of cytogenetics to survival, relapse, and non-relapse mortality (NRM) for the 476 patients with de novo disease. We used these results to establish an optimal cytogenetic grouping scheme. We then applied this grouping scheme to the 80 patients with therapy-related disease. Our proposed three-group cytogenetic classification outperformed the established grouping schemes for both de novo and therapy-related disease. When classified by this new scheme, cytogenetics was the strongest prognostic factor for overall survival in our cohort, through its impact on the risk of relapse (and not on NRM). After accounting for cytogenetics, patients with therapy-related AML or MDS had an equivalent outcome to those with de novo disease. This study demonstrates the impact of cytogenetics on the risk of relapse and death for patients with both de novo and therapy-related disease undergoing transplantation; it also emphasizes the necessity of using cytogenetics to stratify patients entering clinical trials, and provides a system for doing so, which can be validated in a multi-institutional database.
INTRODUCTION
Numerous studies have demonstrated the importance of cytogenetic abnormalities for the prognosis of patients with acute myeloid leukemia (AML)1–3 or myelodysplastic syndrome (MDS)4,5 treated with standard therapy. It has also been established that cytogenetics is prognostically significant after allogeneic hematopoietic stem cell transplantation (HSCT)6–10. However, the existing cytogenetic risk grouping schemes may not be optimal for patients undergoing HSCT. Since the efficacy of HSCT relies in part on immune mechanisms, diseases with a given karyotype might behave differently after HSCT than they would after chemotherapy or with supportive care alone. Therefore, cytogenetic risk groups that are based on series of patients treated with conventional chemotherapy may not apply to transplanted patients. Four cooperative groups have proposed cytogenetic grouping schemes for AML, based on independent series of patients11–14. Most of the patients on whom these schemes are based were treated with chemotherapy alone. In the case of MDS, there is only one widely accepted prognostic scheme, the International Prognostic Scoring System (IPSS)5. This scheme was based on a large series of patients treated primarily with supportive care. It is likely that analyzing a series of patients treated uniformly with allogeneic transplantation would result in a new breakdown of cytogenetic risk groups for both diseases. A new grouping scheme would be useful in assessing the impact of cytogenetics on the risk of relapse and the risk of non-relapse mortality (NRM) after HSCT. Moreover, such a scheme would allow stratification of patients with AML or MDS entering clinical trials in transplantation, which is not yet commonly done.
The influence of cytogenetics in patients with therapy-related AML or MDS (tAML/MDS) undergoing HSCT is also unclear15–18. Therapy-related disease is assuming a growing importance, given the number of patients treated with autologous stem cell transplantation (ASCT), a procedure with a documented risk of MDS/AML ranging from 1% to 24%19. Conversely, therapy-related AML represented as many as 13% of unselected consecutive AML cases in one large series20. Patients with tAML/MDS have an inferior outcome in general compared to patients with de novo disease21–23. However, those patients often harbor karyoptypic abnormalities that confer an adverse prognosis in the setting of de novo AML/MDS20,24–27. This could contribute to their inferior survival since, even when AML is therapy-related, cytogenetics are of prognostic significance when patients are treated with chemotherapy21,23,26. Given the poor outcome with chemotherapy for therapy-related disease, allogeneic HSCT is often performed if the patient is a candidate and a suitable donor is available. However, there are no prospective trials to guide this decision. Published retrospective series of patients undergoing HSCT for tAML/MDS vary widely in their estimates of long-term survival, ranging from 0% to 30%15–18,28,29. In order to choose the best treatment for individual patients with tAML/MDS, it would be useful to know the outcome of HSCT for each cytogenetic risk group, and to better understand the contribution of prior therapy to prognosis after transplantation.
We undertook the present study with the following aims: (1) to establish an optimal cytogenetic risk grouping scheme for patients with de novo AML or MDS; (2) to characterize the impact of cytogenetics using this new scheme; (3) to determine whether this scheme can stratify patients with therapy-related disease into prognostically distinct subgroups; and (4) to examine the independent prognostic impact of prior therapy after cytogenetics are taken into account. In order to do this, we retrospectively studied 476 patients with de novo disease and 80 patients with therapy-related disease who underwent allogeneic HSCT at our institution, and analyzed their outcomes using multivariable analysis.
METHODS
Patients and cytogenetics
We reviewed the medical records of 556 consecutive adult patients with AML or MDS who underwent allogeneic stem cell transplantation at the Dana-Farber Cancer Institute between September 1983 and 1997, and at the combined Dana-Farber/Brigham and Women’s Hospital transplant program between 1997 and August 2005. We included patients with AML in whom the clinical circumstances suggested that the leukemia arose from MDS. We do not use the term “secondary AML” for those patients to avoid confusion with therapy-related AML, and instead use the term “myelodysplatic AML” or “mAML”.
We classified patients as having therapy-related disease if they had received alkylating chemotherapy, topoisomerase-II inhibitor therapy, or radiotherapy one year or more prior to their diagnosis of AML/MDS. Eighty patients met this criterion (the remaining 476 were classified as having de novo disease). For patients with AML and a history of leukemogenic therapy, we labeled the disease therapy-related myelodysplastic AML if they had clinical evidence of MDS prior to the diagnosis of AML, and as therapy-related AML (tAML) if not. We calculated the time from prior therapy to diagnosis of tAML/MDS based on the date of the first leukemogenic treatment received.
Tumor cytogenetics at diagnosis (for patients in remission) or at the time of transplantation (for patients with active disease) were extracted from the records. Only standard karyotype banding techniques were used for most of the patients, and central review was not required. Risk groups were assigned according to the various published grouping schemes, with the following modifications: first, patients with t(15;17) were classified as favorable under all schemes, even though those patients are not classified under the CALGB or the EORTC/GIMEMA schemes; second, we included patients with del(16q22) in the favorable category if they had M4 AML subtype, as those patients can harbor an undetected CBFβ-MYH11 fusion30,31; finally, “complex cytogenetics” was uniformly defined for all grouping schemes as 3 or more abnormalities. In the case of MDS, we followed the IPSS cytogenetic classification5.
IRB approval was obtained from the Office for the Protection of Research Subjects (OPRS) at Dana-Farber/Harvard Cancer Center to perform this study.
Transplantation
Conditioning regimens were either myeloablative (mostly cyclophosphamide plus total body irradiation) (n=424), or reduced intensity (mostly busulfan plus fludarabine), (n=132). Patients received bone marrow (n=298), peripheral blood stem cells (n=247), or umbilical cord blood (n=11) grafts. Donors were matched related (n=293), matched unrelated (n=199), or mismatched (n=64). Graft-versus-host disease (GVHD) prophylaxis regimens included pharmacologic prophylaxis regimens based on a calcineurin inhibitor (n=235), those based on the combination of calcineurin inhibitor and sirolimus (n=138), and ex vivo T cell depletion (n=183).
Statistics
Two-sided Fisher’s exact test was used to compare baseline cytogenetic characteristics. Overall survival and disease-free survival were calculated using the Kaplan-Meier method. Overall survival was defined as the time from stem cell infusion to death from any cause. Patients who were alive or lost to follow-up were censored at the time last seen alive. Disease-free survival was defined as the time from stem cell infusion to relapse or death from any cause. Patients who were alive without relapse were censored at the time last seen alive and relapse-free. The log-rank test was used for comparisons of Kaplan-Meier curves. Cumulative incidence curves for non-relapse death and relapse with or without death were constructed reflecting time to relapse and time to non-relapse death as competing risks. The difference between cumulative incidence curves in the presence of a competing risk was tested using the Gray method32. Potential prognostic factors for survival, disease-free survival, relapse, and non-relapse death were examined in the proportional hazards model as well as in the competing risks regression model33. Interaction terms including interaction with time were examined in the proportional hazards regression model. Proportional hazards assumption for each variable of interest was tested.
RESULTS
Patient characteristics and cytogenetics
The baseline characteristics of the 476 patients with de novo disease and the 80 patients with therapy-related disease included in this study are shown in Table 1. The median age for the entire cohort was 45 years. Median follow-up for survivors was 34 months (range, 6–246).
Table 1.
Baseline characteristics of the patients
| Variable | De novo disease Number, no. (%*) | Therapy-related disease Number, no. (%*) |
|---|---|---|
| Number of patients: | 476 (100) | 80 (100) |
| Age in years (median, range) | 45 (17–71) | 47 (21–66) |
| Disease: | ||
| AML | 308 (65) | 21 (26) |
| MDS | 74(16) | 42 (53) |
| RA, RARS, RCMD | 39 (8) | 20 (25) |
| RAEB | 35 (7) | 22 (28) |
| AML from MDS | 94 (20) | 17 (21) |
| AML/mAML stage†: | ||
| 1st CR | 154 (38) | 13 (34) |
| 2nd or higher CR | 102 (25) | 6 (16) |
| Active disease | 146 (36) | 19 (50) |
| Graft | ||
| Bone marrow | 260 (55) | 38(48) |
| Peripheral blood | 207 (43) | 40 (50) |
| Umbilical cord blood | 9 (2) | 2 (3) |
| Match | ||
| MRD | 262 (55) | 31 (39) |
| MUD | 159 (33) | 40 (50) |
| Mismatched | 55 (12) | 9 (11) |
| Mismatched related | 13 (3) | 2 (3) |
| Mismatched unrelated | 42 (9) | 7 (9) |
| Conditioning | ||
| Myeloablative | 381 (80) | 43 (54) |
| Reduced intensity | 95 (20) | 37 (46) |
| GVHD prophylaxis | ||
| CnI +/− Mtx or steroids | 203 (43) | 32 (40) |
| CnI + Siro +/− Mtx | 114 (24) | 24 (30) |
| TCD | 159 (33) | 24 (30) |
| Gender recipient/donor | ||
| Male/Female | 107 (22) | 17 (21) |
| Female/Male | 110 (23) | 25 (31) |
| Female/Female | 114 (24) | 19 (24) |
| Male/Male | 140 (29) | 18 (23) |
| Recipient CMV seropositive | 208 (44) | 28 (35) |
| Donor CMV seropositive | 160 (34) | 29 (36) |
| Year of transplantation | ||
| 1983–1989 | 22 (5) | 3 (4) |
| 1990–1999 | 155 (33) | 24 (30) |
| 2000–2005 | 299 (63) | 53 (66) |
RA indicates refractory anemia; RARS, refractory anemia with ringed sideroblasts; RCMD, refractory cytopenia with multilineage dysplasia; RAEB, refractory anemia with excess blasts; CR, complete remission; MRD, matched related donor; MUD, matched unrelated donor; GVHD, graft-versus-host disease; CnI, calcineurin inhibitor (cyclosporine or tacrolimus); Mtx, methotrexate; Siro, sirolimus; TCD, T-cell depletion; and CMV, cytomegalovirus
Percentages may not add to 100 because of rounding
Percentage for this category refers to the percent of AML/mAML patients, not to the percent of total patients
Among the patients with therapy-related disease, most had a primary diagnosis of lymphoma (35% had non-Hodgkin’s lymphoma, 19% had Hodgkin’s lymphoma). Almost all of the patients (95%) had received prior alkylator therapy; 73% had received a topoisomerase II inhibitor, while 65% had received prior radiation. Fifty-three percent of the patients had previously undergone autologous stem cell transplantation. The median time from first leukemogenic therapy to diagnosis of AML/MDS was 7 years (range, 1–25 years).
Ninety-one percent of all patients had available cytogenetic data, which are presented in Table 2. We used the MRC and IPSS grouping schemes as our starting points for AML and MDS, respectively. When classified according to these schemes, 27% of patients with de novo disease had favorable cytogenetics, versus 11% of patients with therapy-related disease (p=0.003); 47% of patients with de novo disease had intermediate cytogenetics, compared to 21% of patients with therapy-related disease (p<0.0001); and 17% of patients with de novo disease had adverse cytogenetics, compared to 60% of patients with therapy-related disease (p<0.0001).
Table 2.
Cytogenetics
| Variable | De novo disease Number, no. (%*) | Therapy-related disease Number, no. (%*) | p value |
|---|---|---|---|
| AML cytogenetics† | |||
| Number of patients | 308 (100) | 21 (100) | |
| Favorable | 45 (15) | 2 (10) | 0.8 |
| t(8;21) | 5 (5) | 0 (0) | |
| inv(16) or t(16;16) | 18 (6) | 0 (0) | |
| t(15;17) | 12 (4) | 2 (10) | |
| Intermediate | 186 (60) | 11 (52) | 0.5 |
| Normal | 119 (39) | 5 (24) | |
| +8 | 17 (6) | 0 (0) | |
| del(9q) | 4 (1) | 0 (0) | |
| Abnormality of 11q23 | 2 (4) | 2 (10) | |
| t(9;22) | 4 (1) | 0 (0) | |
| t(6;9) | 4 (1) | 0 (0) | |
| Other | 26 (8) | 4 (19) | |
| Adverse | 42 (14) | 7 (33) | 0.024 |
| −5, del(5q), or −7 | 16 (5) | 3 (14) | |
| Abnormal 3q | 1 (0) | 0 (0) | |
| Complex | 25 (8) | 4 (19) | |
| Not obtained/not available | 35 (11) | 1 (5) | 0.1 |
| MDS and mAML cytogenetics‡ | |||
| Number of patients | 168 (100) | 59 (100) | |
| Favorable MDS | 82 (49) | 7 (12) | <0.0001 |
| 5q- | 2 (1) | 0 (0) | |
| 20q- | 1 (1) | 0 (0) | |
| Y- | 0 (0) | 0 (0) | |
| Normal | 79 (47) | 7 (12) | |
| Intermediate MDS | 37 (22) | 6 (10) | 0.12 |
| All others | 37 (22) | 6 (10) | |
| Adverse MDS | 38 (23) | 41 (69) | <0.0001 |
| Abnormal 7 | 11 (7) | 16 (27) | |
| Complex | 27 (16) | 25 (42) | |
| Not obtained/not available | 11 (7) | 5 (8) | 0.6 |
Percentages may not add to 100 because of rounding
Classified according to MRC grouping scheme
Classified according to the IPSS grouping scheme
There was a significant association between cytogenetic risk group and both age and remission status in our series. Twenty-seven percent of the patients age 40 and over had adverse cytogenetics, compared to 18% of the patients under age 40 (p=0.043); 6% of the patients 40 and over had favorable cytogenetics compared to 13% of patients under age 40 (p=0.007). Among patients with acute leukemia, 25% of patients with early stage disease had adverse cytogenetics, compared to 11% of patients beyond CR1 (p=0.0002); 2% of patients with early stage disease had favorable cytogenetics, compared to 15% of patients beyond CR1 (p<0.0001).
Prognostic factors for overall survival (OS) in de novo AML and MDS
We first considered the group of 476 patients with de novo disease. We assigned patients to cytogenetic risk groups using the MRC scheme for AML and the IPSS scheme for MDS or AML arising from MDS (mAML). Using proportional hazards modeling including all of the variables from Table 1, we found the following to be significant prognostic factors for OS in this population: age, cytogenetic risk group, disease type, disease stage at transplant, GVHD prophylaxis regimen and HLA match (data not shown). In this model, the hazard ratio (HR) for patients with favorable cytogenetics (compared to those with intermediate cytogenetics) was 0.5 (p<0.0001); the HR for adverse cytogenetics compared to intermediate was 1.7 (p=0.003). Of note, the HR for patients whose cytogenetics was not obtainable or not available was 1.1 (p=0.6) in comparison to the entire group with available cytogenetics. Thus, the group of patients with available cytogenetics does not appear to be a biased subsample of the entire study population. The results confirm the importance of cytogenetics in transplantation outcome; they remained essentially unchanged whether we used the MRC11, CALGB12, SWOG/ECOG13, or EORTC/GIMEMA14 schemes for classification of AML cytogenetics.
New cytogenetic risk groups for de novo patients
We repeated the multivariate analysis considering only the 308 patients with de novo AML, separating cytogenetics into individual abnormalities. We only considered abnormalities found in more than 3 patients. Abnormalities found in fewer than 3 patients, and classified as intermediate under the MRC grouping scheme, were lumped into an “all others” category. We added to the model the prognostic factors identified above. The results, shown in Table 3 (top), suggest the existence of three distinct risk groups for AML. The same analysis, performed for the 168 patients with de novo MDS or mAML, suggest the existence of 2 distinct groups (Table 3, bottom). An analysis limited to the patients with MDS yielded the same grouping scheme as one combining patients with MDS and mAML. When we examined which of the existing grouping schemes (including existing AML and MDS schemes, and our new groups for AML and MDS) could best stratify the 94 patients with mAML in multivariate analysis, our new MDS grouping scheme was the most discriminating (p=0.002).
Table 3.
Risk group determination for de novo patients
| AML cytogenetic abnormality | HR | p | Risk group |
|---|---|---|---|
| t(8;21) alone | 0.2 | 0.035 | Favorable |
| inv(16)/t(16;16)/del(16q22) with M4 | 0.2 | 0.002 | |
| t(15;17) | 0.3 | 0.025 | |
| del(9q) | 0.7 | 0.6 | Standard |
| All others | 0.9 | 0.9 | |
| Normal (reference group) | 1.0 | ||
| t(8;21) + del(9q) or complex | 1.1 | 0.9 | |
| Trisomy 8 | 1.1 | 0.9 | |
| Abnormal 5 or 7 | 1.1 | 0.8 | |
| Abnormal 11q23 | 1.4 | 0.4 | |
| Complex | 2.6 | 0.0005 | Adverse |
| t(9;22) | 3.6 | 0.024 | |
| t(6;9) | 11.6 | <0.0001 | |
| MDS/mAML cytogenetic abnormality | |||
| Abnormal 3q | 0.7 | 0.7 | Standard |
| Normal (reference group) | 1.0 | ||
| Abnormal 5 | 1.2 | 0.9 | |
| Trisomy 8 | 1.2 | 0.7 | |
| All others | 1.4 | 0.1 | |
| Abnormal 7 | 2.2 | 0.050 | Adverse |
| Complex | 3.4 | <0.0001 | |
HR indicates hazard ratio.
Based on the above results, there are seven potentially distinct disease/cytogenetic categories for transplanted patients: 3 for AML, 2 for MDS, and 2 for mAML. In order to further simplify our system, we considered each of the seven groups in turn, and used it as the reference group in a multivariate analysis, with the 6 other groups as comparisons. The models (not shown) suggest the existence of three distinct overall risk groups, summarized in Table 4. Within each group, there was no statistically significant difference in survival between any of the group members. Between any members of distinct groups, there was a statistically significant difference in survival (p<0.05).
Table 4.
Summary of new grouping scheme
| Group | AML | MDS or AML arising from MDS |
|---|---|---|
| Favorable | t(8;21) alone inv(16)/t(16;16)/del(16q22) with M4 t(15;17) |
|
| Standard-risk | Normal del(9q) t(8;21) + del(9q) or complex Trisomy 8 Abnormal 5 or 7 Abnormal 11q23 All others |
Normal Abnormal 3q Abnormal 5 Trisomy 8 All others |
| Adverse | Complex t(9;22) t(6;9) |
Abnormal 7 Complex |
Patients with AML and abnormal 3q, as well as patients with MDS and 5q-, 20q-, or Y- are not classified in this analysis, as too few patients with those abnormalities were present in our cohort to assign to a risk group
Impact of cytogenetics in de novo disease using new classification
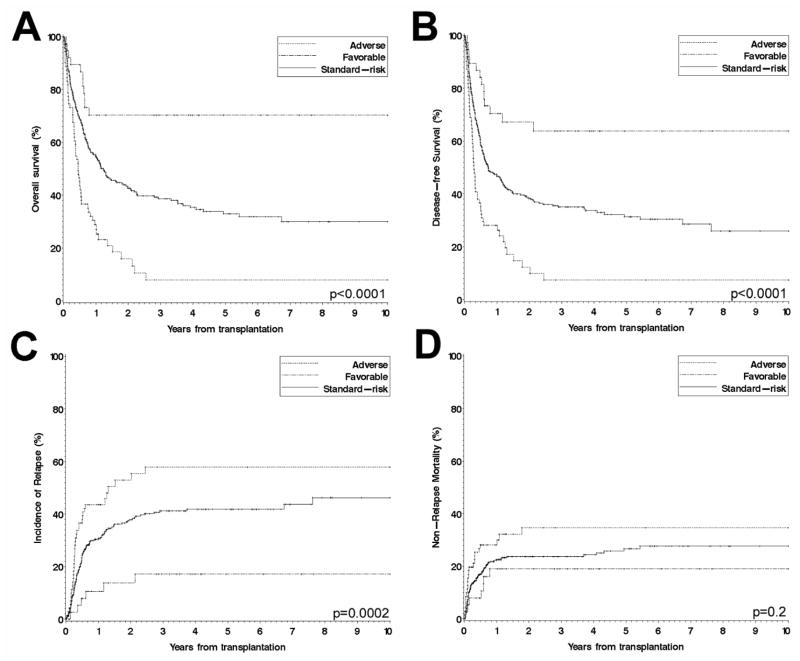
Figure 1 shows the outcomes of all patients with de novo disease (AML, MDS, and mAML) when categorized by this scheme. Overall survival is shown in Figure 1A; 5-year OS for the favorable, standard-risk, and adverse groups were 70% (95% confidence interval (CI), 56–85), 33% (CI, 27–39) and 8% (CI, 0–16), respectively. Disease-free survival (DFS) is shown in Figure 1B; 5-year DFS for the favorable, standard-risk, and adverse groups were 64% (CI, 48–80), 32% (CI, 26–37) and 7% (CI, 0–15), respectively. Cumulative incidence of relapse (CIR) is shown in Figure 1C. In competing risk regression analyses33 for CIR using our new risk groups and the other variables from Table 1, cytogenetics significantly affected the risk of relapse, with HR=2.0 (p=0.002) for adverse risk, and HR=0.3 (p=0.006) for favorable risk, compared to standard risk (Table 5). In contrast, cytogenetics did not significantly affect non-relapse mortality (Figure 1D), with HR=1.6 (p=0.07) for adverse, and HR=0.6 (p=0.2) for favorable (compared to standard risk) in competing risks regression analysis (Table 5).
Figure 1. Survival, relapse, and non-relapse mortality for all de novo patients, stratified by cytogenetics according to new grouping scheme.
(A) Overall survival; (B) Disease-free survival; (C) Cumulative incidence of relapse; (D) Non-relapse mortality.
Table 5.
Competing risks regression analysis of relapse and non-relapse mortality for all patients with de novo disease, using new cytogenetic risk groups
| Variable | HR for relapse | p | HR for NRM | p |
|---|---|---|---|---|
| Cytogenetics | ||||
| Standard-risk (reference) | 1.0 | 1.0 | ||
| Favorable | 0.3 | 0.006 | 0.6 | 0.2 |
| Adverse | 2.0 | 0.002 | 1.6 | 0.070 |
| Age | NS | 1.03 | 0.008 | |
| Disease/Stage | ||||
| AML in CR1 (reference) | 1.0 | 1.0 | ||
| CR≥1 | 1.8 | 0.009 | 1.7 | 0.058 |
| Active disease | 2.6 | <0.0001 | 1.0 | 0.9 |
| RA/RARS/RCMD | 0.4 | 0.041 | 1.6 | 0.3 |
| RAEB | 0.7 | 0.4 | 1.3 | 0.5 |
| mAML in CR1 | 0.9 | 0.7 | 1.6 | 0.078 |
| Match | ||||
| MRD (reference) | 1.0 | 1.0 | ||
| MUD | 0.8 | 0.2 | 2.6 | <0.0001 |
| Mismatched | 0.7 | 0.4 | 3.4 | 0.0002 |
| Conditioning | ||||
| Cy/TBI (reference) | 1.0 | 1.0 | ||
| Bu/Cy | 1.3 | 0.6 | 0.7 | 0.7 |
| Reduced intensity | 2.7 | .0005 | 0.1 | <0.0001 |
| GVHD prophylaxis | ||||
| CnI +/− Mtx* (reference) | 1.0 | 1.0 | ||
| CnI + Rapa +/− Mtx | 1.2 | 0.4 | 0.3 | 0.003 |
| TCD | 1.2 | 0.5 | 0.9 | 0.8 |
Graft source (bone marrow versus peripheral blood versus cord blood), CMV serostatus of donor and recipient (positive versus negative or unknown), female-to-male transplant, and year of transplant (in 10-year blocks) were not significant in this analysis.
HR indicates hazard ratio; NRM, non-relapse mortality; NS, non-significant; Cy, cyclophosphamide; TBI, total body irradiation; Bu, busulfan; other abbreviations are explained in Table 1
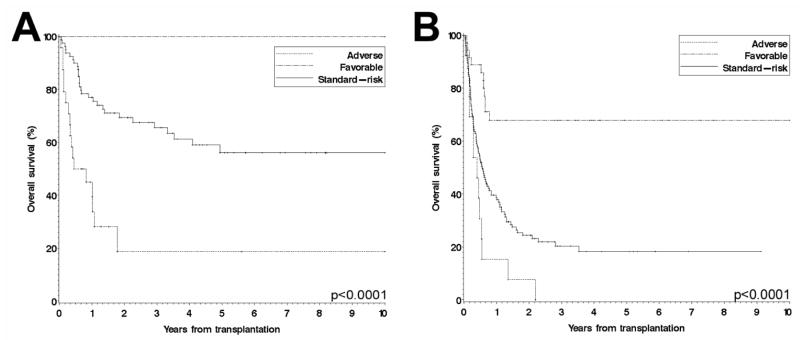
This grouping scheme retained statistically significant prognostic importance if the analysis was confined to any one of the following disease groups: AML in CR1 or beyond CR1 (Figure 2), MDS, or mAML. It also applied equally well to patients receiving a T-cell depleted grafts and to those receiving a T-cell replete one (not shown).
Figure 2. Overall survival of patients with AML, stratified by cytogenetics according to new grouping scheme.
(A) Patients with AML in CR1; (B) Patients with AML beyond CR1.
Prognosis in therapy-related disease
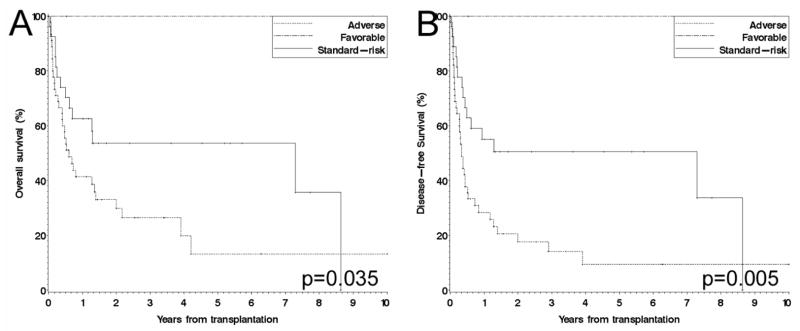
We built proportional hazards model for the 80 patients with therapy-related disease (AML, MDS, or mAML), using cytogenetics grouped according to our new system, as well as all of the covariates from Table 1. We emphasize that those 80 patients were not included in the derivation of the grouping scheme. In this model, the HR for adverse cytogenetics (compared to standard risk) was 2.6 (p=0.046). Because there were only 2 patients with therapy-related disease and favorable cytogenetics (with 5-year survival of 100%), we could not draw meaningful statistical conclusions for this group. Although adverse cytogenetics appeared to be associated with inferior survival using any of the previously established grouping schemes, our new classification was the only one that allowed statistically significant stratification. Figure 3 shows the outcomes of all patients with therapy-related disease when categorized by this scheme. Overall survival is shown in Figure 3A; 5-year OS for the favorable, standard-risk, and adverse groups were 100% (CI, not obtainable), 54% (CI, 34–73) and 13% (CI, 0–28), respectively. Disease-free survival (DFS) is shown in Figure 3B; 5-year DFS for the favorable, standard-risk, and adverse groups were 100% (CI, not obtainable), 51% (CI, 31–70) and 9% (CI, 0–20), respectively.
Figure 3. Survival of all patients with therapy-related disease, stratified by cytogenetics according to new grouping scheme.
(A) Overall survival; (B) Disease-free survival. Note that the favorable group included only 2 patients.
Given that our classification system was as applicable to therapy-related disease as it was to de novo disease, we performed multivariate analyses for OS on the entire cohort of 556 patients, including both patients with de novo disease and those with therapy-related disease, using cytogenetics (grouped by our new system) and a term for prior therapy (as well as all covariates from Table 1). The results are displayed in Table 6. Adverse cytogenetics was associated with a HR of 2.4 compared to standard-risk (and of 9.4 when compared to favorable), and favorable cytogenetics with a HR of 0.3 compared to standard-risk (all with p<0.0001). Notably, prior therapy was not a significant prognostic factor for OS (HR=0.9, p=0.5), or for DFS; this was the also case if tAML and tMDS/mAML were considered individually. This held true when using any of the existing cytogenetic risk grouping schemes. Using competing risk regression analysis accounting for cytogenetic risk group, we found no significant difference between de novo disease and therapy-related disease for either incidence of relapse (for therapy-related disease compared to de novo, HR=0.8, p=0.5) or non-relapse mortality (HR=1.3, p=0.3). In further multivariate analyses (not shown), neither the type of prior therapy received (alkylator versus topoisomerase II inhibitor versus radiotherapy), nor a prior history of autologous stem cell transplantation, nor the time between first leukemogenic therapy and diagnosis of tAML/MDS, significantly affected overall survival.
Table 6.
Multivariate analysis of overall survival for all patients combined, using new cytogenetic risk groups
| Variable | Hazard ratio | p |
|---|---|---|
| Prior therapy | 0.9 | 0.4 |
| Cytogenetics | ||
| Standard-risk (reference) | 1.0 | |
| Favorable | 0.3 | <0.0001 |
| Adverse | 2.4 | <0.0001 |
| Not available | 1.3 | 0.2 |
| Age | 1.03 | <0.0001 |
| Disease/Stage | ||
| AML in CR1 (reference) | 1.0 | |
| CR≥1 | 2.7 | <0.0001 |
| Active disease | 2.7 | <0.0001 |
| RA/RARS/RCMD | 0.9 | 0.6 |
| RAEB | 1.3 | 0.3 |
| mAML in CR1 | 0.9 | 0.3 |
| Match | ||
| MRD (reference) | 1.0 | |
| MUD | 1.3 | 0.038 |
| Mismatched | 2.1 | 0.0002 |
| GVHD prophylaxis | ||
| CnI +/− Mtx* (reference) | 1.0 | |
| CnI + Rapa +/− Mtx | 0.7 | 0.036 |
| TCD | 1.0 | 0.8 |
Conditioning regimen (myeloablative versus reduced-intensity), graft source (bone marrow versus peripheral blood versus cord blood), CMV serostatus of donor and recipient (positive versus negative or unknown), female-to-male transplant, and year of transplant (in 10-year blocks) were not significant in this analysis.
+/− steroids
Abbreviations are explained in Table 1.
DISCUSSION
Our results confirm the critical prognostic role of cytogenetics for patients with AML or MDS undergoing HSCT6–10, even after controlling for other known prognostic factors. When grouped according to our transplant-specific scheme, cytogenetic risk group carried the greatest prognostic weight of any of the examined risk factors in our cohort. Specifically, cytogenetic risk group was a more important determinant of outcome than disease type, conditioning regimen intensity, use of T cell depletion or choice of pharmacologic regimen for GVHD prophylaxis. Although 9% of the patients in our cohort did not have available cytogenetic information, their outcome was not different from that of the patients with available cytogenetics, implying the absence of a significant selection bias for cytogenetics. Naturally, since this study is a retrospective analysis of patients selected for transplantation, the results do not necessarily apply to patients at the time of diagnosis; in particular, cytogenetics11,12, prior MDS, and prior therapy21,26,34 can both affect the rate of remission for AML, which our data does not capture.
The major difference between our AML grouping scheme and the existing AML schemes is the inclusion of AML patients with abnormalities of chromosome 5 or 7 in the standard-risk group. Because the effect of cytogenetics was primarily on the risk of relapse, and because there was no apparent interaction between conditioning regimen intensity and cytogenetic risk group, this suggests that those karyoptypic abnormalities, although they appear to confer increased resistance to standard chemotherapy, may be sensitive to the immunologic effect of transplantation. It must be noted that this is conclusion based on a small number of patients, and will require validation in a larger study.
Another important finding from our analysis is that prior therapy does not by itself constitute an adverse prognostic factor after transplantation. This conclusion can only be drawn after accounting for cytogenetics, as patients with therapy-related disease more often harbor adverse karyotypic abnormalities than their de novo counterparts (as they did in our cohort). Our results can be considered in the context of treatment decisions for patients with therapy-related disease. Unfortunately, there are no prospective trials comparing consolidation chemotherapy to HSCT for this group of patients specifically. The survivals of transplanted patients with tAML/MDS in our series (5-year OS of 100%, 54% and 13% for favorable, standard and adverse cytogenetic risk, respectively) compare very favorably with the previously reported survivals of tAML/MDS patients treated with standard therapy (5-year OS of 47–54% in the largest series of patients with therapy-related AML with favorable cytogenetics35, and 5y OS of 0–10% and 0–5% in recent studies of tAML/MDS patients with standard and adverse cytogenetics23,25, respectively). This comparison lends some measure of support, albeit through retrospective data, to the use of allogeneic transplantation in this setting.
Validation of our classification scheme on an independent series of transplant patients will be critical in three ways. First, this study is a retrospective study, which spans a large time interval; moreover, the most recently transplanted patients do not have extended follow-up. Therefore, our classification scheme should be viewed as tentative until it can be validated in a larger patient series. Second, such validation will help in classifying patients with AML and abnormal 3q, or with MDS and 5q-, 20q-, or Y-, which we were unable to do because of insufficient representation; finally, a larger cohort may allow finer subgroupings (e.g., separating “abnormalities of 5 or 7” into 5-, 5q-,7-, and 7q-). Further in the future, risk grouping schemes will likely be refined by improvements in cytogenetic techniques; by the use of fluorescence in-situ hybridization and polymerase chain reaction to detect unapparent cytogenetic abnormalities and molecular defects, respectively; and, perhaps more importantly, by testing for molecular abnormalities, such as FLT-3, KIT or NPM1 mutations, or BAALC expression36–39, that are now recognized as having a significant prognostic role in the outcome of patients with AML.
In summary, we have confirmed a powerful prognostic role for cytogenetics in the outcome of patients undergoing allogeneic HSCT, through its influence on the risk of relapse. We propose a new cytogenetic risk grouping scheme specifically applicable to this patient population, which we hope to validate in a multi-institution database. This scheme applies to patients regardless of disease, stage, or prior history of leukemogenic therapy. Prior therapy by itself does not appear to be an adverse risk factor after transplantation, once cytogenetic risk group is taken into account. Our results strongly underscore the necessity of stratifying patients by cytogenetics in clinical trials, which is not currently routinely done. Once validated, our grouping system could provide a basis for such stratification.
Acknowledgments
Support: NIAID U19 AI 29530
NHLBI PO1 HL 070149
Ted and Eileen Pasquarello Research Fund.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bloomfield CD, Goldman A, Hassfeld D, de la Chapelle A. Fourth International Workshop on Chromosomes in Leukemia 1982: Clinical significance of chromosomal abnormalities in acute nonlymphoblastic leukemia. Cancer Genet Cytogenet. 1984;11:332–350. doi: 10.1016/s0165-4608(84)80022-9. [DOI] [PubMed] [Google Scholar]
- 2.Walker H, Smith FJ, Betts DR. Cytogenetics in acute myeloid leukaemia. Blood Rev. 1994;8:30–36. doi: 10.1016/0268-960x(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 3.Grimwade D, Moorman A, Hills R, et al. Impact of karyotype on treatment outcome in acute myeloid leukemia. Ann Hematol. 2004;83 Suppl 1:S45–48. doi: 10.1007/s00277-004-0849-8. [DOI] [PubMed] [Google Scholar]
- 4.Heim S. Cytogenetic findings in primary and secondary MDS. Leuk Res. 1992;16:43–46. doi: 10.1016/0145-2126(92)90098-r. [DOI] [PubMed] [Google Scholar]
- 5.Greenberg P, Cox C, LeBeau MM, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–2088. [PubMed] [Google Scholar]
- 6.Ferrant A, Labopin M, Frassoni F, et al. Karyotype in acute myeloblastic leukemia: prognostic significance for bone marrow transplantation in first remission: a European Group for Blood and Marrow Transplantation study. Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT) Blood. 1997;90:2931–2938. [PubMed] [Google Scholar]
- 7.Gale RP, Horowitz MM, Weiner RS, et al. Impact of cytogenetic abnormalities on outcome of bone marrow transplants in acute myelogenous leukemia in first remission. Bone Marrow Transplant. 1995;16:203–208. [PubMed] [Google Scholar]
- 8.Kim DH, Sohn SK, Kim JG, et al. Parameters for predicting allogeneic PBSCT outcome of acute myeloid leukemia: cytogenetics at presentation versus disease status at transplantation. Ann Hematol. 2005;84:25–32. doi: 10.1007/s00277-004-0942-z. [DOI] [PubMed] [Google Scholar]
- 9.Ogawa H, Ikegame K, Kawakami M, et al. Impact of cytogenetics on outcome of stem cell transplantation for acute myeloid leukemia in first remission: a large-scale retrospective analysis of data from the Japan Society for Hematopoietic Cell Transplantation. Int J Hematol. 2004;79:495–500. doi: 10.1532/ijh97.03166. [DOI] [PubMed] [Google Scholar]
- 10.Nevill TJ, Fung HC, Shepherd JD, et al. Cytogenetic abnormalities in primary myelodysplastic syndrome are highly predictive of outcome after allogeneic bone marrow transplantation. Blood. 1998;92:1910–1917. [PubMed] [Google Scholar]
- 11.Grimwade D, Walker H, Oliver F, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children’s Leukaemia Working Parties. Blood. 1998;92:2322–2333. [PubMed] [Google Scholar]
- 12.Byrd JC, Mrozek K, Dodge RK, et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461) Blood. 2002;100:4325–4336. doi: 10.1182/blood-2002-03-0772. [DOI] [PubMed] [Google Scholar]
- 13.Slovak ML, Kopecky KJ, Cassileth PA, et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood. 2000;96:4075–4083. [PubMed] [Google Scholar]
- 14.Suciu S, Mandelli F, de Witte T, et al. Allogeneic compared with autologous stem cell transplantation in the treatment of patients younger than 46 years with acute myeloid leukemia (AML) in first complete remission (CR1): an intention-to-treat analysis of the EORTC/GIMEMAAML-10 trial. Blood. 2003;102:1232–1240. doi: 10.1182/blood-2002-12-3714. [DOI] [PubMed] [Google Scholar]
- 15.Yakoub-Agha I, de La Salmoniere P, Ribaud P, et al. Allogeneic bone marrow transplantation for therapy-related myelodysplastic syndrome and acute myeloid leukemia: a long-term study of 70 patients-report of the French society of bone marrow transplantation. J Clin Oncol. 2000;18:963–971. doi: 10.1200/JCO.2000.18.5.963. [DOI] [PubMed] [Google Scholar]
- 16.Witherspoon RP, Deeg HJ, Storer B, Anasetti C, Storb R, Appelbaum FR. Hematopoietic stem-cell transplantation for treatment-related leukemia or myelodysplasia. J Clin Oncol. 2001;19:2134–2141. doi: 10.1200/JCO.2001.19.8.2134. [DOI] [PubMed] [Google Scholar]
- 17.Ballen KK, Gilliland DG, Guinan EC, et al. Bone marrow transplantation for therapy-related myelodysplasia: comparison with primary myelodysplasia. Bone Marrow Transplant. 1997;20:737–743. doi: 10.1038/sj.bmt.1700971. [DOI] [PubMed] [Google Scholar]
- 18.Anderson JE, Gooley TA, Schoch G, et al. Stem cell transplantation for secondary acute myeloid leukemia: evaluation of transplantation as initial therapy or following induction chemotherapy. Blood. 1997;89:2578–2585. [PubMed] [Google Scholar]
- 19.Pedersen-Bjergaard J, Philip P, Larsen SO, Jensen G, Byrsting K. Chromosome aberrations and prognostic factors in therapy-related myelodysplasia and acute nonlymphocytic leukemia. Blood. 1990;76:1083–1091. [PubMed] [Google Scholar]
- 20.Mauritzson N, Albin M, Rylander L, et al. Pooled analysis of clinical and cytogenetic features in treatment-related and de novo adult acute myeloid leukemia and myelodysplastic syndromes based on a consecutive series of 761 patients analyzed 1976–1993 and on 5098 unselected cases reported in the literature 1974–2001. Leukemia. 2002;16:2366–2378. doi: 10.1038/sj.leu.2402713. [DOI] [PubMed] [Google Scholar]
- 21.Goldstone A, Burnett A, Avivi IRHKW. Secondary acute myeloid leukemia has a worse outcome than de novo AML, even taking into account cytogenetics and age: AML 10, 11, 12 MRC Trials. Blood. 2002;100:88a. [Google Scholar]
- 22.Josting A, Wiedenmann S, Franklin J, et al. Secondary myeloid leukemia and myelodysplastic syndromes in patients treated for Hodgkin’s disease: a report from the German Hodgkin’s Lymphoma Study Group. J Clin Oncol. 2003;21:3440–3446. doi: 10.1200/JCO.2003.07.160. [DOI] [PubMed] [Google Scholar]
- 23.Kern W, Haferlach T, Schnittger S, Hiddemann W, Schoch C. Prognosis in therapy-related acute myeloid leukemia and impact of karyotype. J Clin Oncol. 2004;22:2510–2511. doi: 10.1200/JCO.2004.99.301. [DOI] [PubMed] [Google Scholar]
- 24.Rowley JD, Golomb HM, Vardiman JW. Nonrandom chromosome abnormalities in acute leukemia and dysmyelopoietic syndromes in patients with previously treated malignant disease. Blood. 1981;58:759–767. [PubMed] [Google Scholar]
- 25.Smith SM, Le Beau MM, Huo D, et al. Clinical-cytogenetic associations in 306 patients with therapy-related myelodysplasia and myeloid leukemia: the University of Chicago series. Blood. 2003;102:43–52. doi: 10.1182/blood-2002-11-3343. [DOI] [PubMed] [Google Scholar]
- 26.Kantarjian HM, Keating MJ, Walters RS, et al. Therapy-related leukemia and myelodysplastic syndrome: clinical, cytogenetic, and prognostic features. J Clin Oncol. 1986;4:1748–1757. doi: 10.1200/JCO.1986.4.12.1748. [DOI] [PubMed] [Google Scholar]
- 27.Michels SD, McKenna RW, Arthur DC, Brunning RD. Therapy-related acute myeloid leukemia and myelodysplastic syndrome: a clinical and morphologic study of 65 cases. Blood. 1985;65:1364–1372. [PubMed] [Google Scholar]
- 28.Witherspoon RP, Deeg HJ. Allogeneic bone marrow transplantation for secondary leukemia or myelodysplasia. Haematologica. 1999;84:1085–1087. [PubMed] [Google Scholar]
- 29.Friedberg JW, Neuberg D, Stone RM, et al. Outcome in patients with myelodysplastic syndrome after autologous bone marrow transplantation for non-Hodgkin’s lymphoma. J Clin Oncol. 1999;17:3128–3135. doi: 10.1200/JCO.1999.17.10.3128. [DOI] [PubMed] [Google Scholar]
- 30.Mrozek K, Prior TW, Edwards C, et al. Comparison of cytogenetic and molecular genetic detection of t(8;21) and inv(16) in a prospective series of adults with de novo acute myeloid leukemia: a Cancer and Leukemia Group B Study. J Clin Oncol. 2001;19:2482–2492. doi: 10.1200/JCO.2001.19.9.2482. [DOI] [PubMed] [Google Scholar]
- 31.Tobal K, Johnson PR, Saunders MJ, Harrison CJ, Liu Yin JA. Detection of CBFB/MYH11 transcripts in patients with inversion and other abnormalities of chromosome 16 at presentation and remission. Br J Haematol. 1995;91:104–108. doi: 10.1111/j.1365-2141.1995.tb05253.x. [DOI] [PubMed] [Google Scholar]
- 32.Gray R. A class of K-sample tests for comparing the cumulative incidence of a competing risk. The Annals of Statistics. 1988;16:1140–1154. [Google Scholar]
- 33.Fine J, Gray R. A proportional hazards model for the subdistribution of a competing risk. Journal of the American Statistical Association. 1999;94:496–509. [Google Scholar]
- 34.Hoyle CF, de Bastos M, Wheatley K, et al. AML associated with previous cytotoxic therapy, MDS or myeloproliferative disorders: results from the MRC’s 9th AML trial. Br J Haematol. 1989;72:45–53. doi: 10.1111/j.1365-2141.1989.tb07650.x. [DOI] [PubMed] [Google Scholar]
- 35.Quesnel B, Kantarjian H, Bjergaard JP, et al. Therapy-related acute myeloid leukemia with t(8;21), inv(16), and t(8;16): a report on 25 cases and review of the literature. J Clin Oncol. 1993;11:2370–2379. doi: 10.1200/JCO.1993.11.12.2370. [DOI] [PubMed] [Google Scholar]
- 36.Schnittger S, Kohl TM, Haferlach T, et al. KIT-D816 mutations in AML1-ETO-positive AML are associated with impaired event-free and overall survival. Blood. 2006;107:1791–1799. doi: 10.1182/blood-2005-04-1466. [DOI] [PubMed] [Google Scholar]
- 37.Baldus CD, Thiede C, Soucek S, Bloomfield CD, Thiel E, Ehninger G. BAALC expression and FLT3 internal tandem duplication mutations in acute myeloid leukemia patients with normal cytogenetics: prognostic implications. J Clin Oncol. 2006;24:790–797. doi: 10.1200/JCO.2005.01.6253. [DOI] [PubMed] [Google Scholar]
- 38.Thiede C, Koch S, Creutzig E, et al. Prevalence and prognostic impact of NPM1 mutations in 1485 adult patients with acute myeloid leukemia (AML) Blood. 2006;107:4011–4020. doi: 10.1182/blood-2005-08-3167. [DOI] [PubMed] [Google Scholar]
- 39.Paschka P, Marcucci G, Ruppert AS, et al. Mutations of KIT tyrosine kinase (TK) gene predict relapse in adult patients (pts) with core binding factor acute myeloid leukemia (CBF AML): A Cancer and Leukemia Group B (CALGB) study. Journal of Clinical Oncology. 2006;24:2. [Google Scholar]