ABSTRACT
OBJECTIVE
To determine the views of family medicine (FM) program directors, third-year program coordinators, and residents on the factors affecting demand and allocation of postgraduate year 3 (PGY3) positions and the effects of these programs on the professional activities of program graduates.
DESIGN
Cross-sectional surveys and key informant interviews.
SETTING
Ontario (FM residents) and across Canada (program directors) in 2006.
PARTICIPANTS
All FM residents in Ontario and all core program directors and PGY3 program coordinators nationally were eligible to participate in the surveys. Eighteen key informant interviews were conducted, all in Ontario. Interviewees included all FM program directors, selected PGY3 program coordinators, residents, and other community stakeholders.
METHODS
Resident surveys were Web-based; invitations to participate were delivered by FM programs via e-mail lists. The program director and coordinator surveys were postal surveys. Interviews were audiotaped and transcribed, and the authors coded the interviews for themes.
MAIN FINDINGS
Response rates for the surveys were 34% to 39% for residents and 78% for program directors and coordinators. Respondents agreed that programs should include flexible training options of varied duration. Demand for training is determined more by resident need than community or health system factors, and is either increasing or stable. Overall, respondents believed that approximately one-third of core program graduates should have the opportunity for PGY3 training. They thought re-entry from practice should be permitted, but mandatory return-of-service agreements were not desired. Program allocation and resident selection is a complex process with resident merit playing an important role. Respondents expected PGY3 graduates to practise differently than PGY2 graduates and to provide improved quality of care in their fields. They also thought that PGY3 graduates might play larger roles in leadership and teaching than core program graduates.
CONCLUSION
It is likely that PGY3 programs will continue to grow and form an increasingly important part of the FM training system in Canada. Flexible programs that can adapt to changing educational, health system, and community needs are essential. Training programs and national and provincial colleges of FM will also need to ensure that these physicians are provided with opportunities to maintain their links with the rest of the FM community.
RÉSUMÉ
OBJECTIF
Cerner les points de vue des directeurs de programme de médecine familiale (MF), des coordonnateurs de programme de 3e année et des résidents sur les facteurs qui influent sur la demande et l’attribution de postes de 3e année de formation postdoctorale (R3), de même que les effets de ces programmes sur les activités professionnelles des diplômés du programme.
CONCEPTION
Sondages transversaux et entrevues avec des intervenants clés.
CONTEXTE
Ontario (résidents en MF) et l’ensemble du Canada (directeurs de programme) en 2006.
PARTICIPANTS
Tous les résidents en MF en Ontario et, sur le plan national, tous les directeurs de programme et coordonnateurs de programme de 3e année étaient admissibles à participer aux sondages. On a aussi effectué des entrevues avec 18 intervenants clés, toutes en Ontario. Parmi les personnes interviewées, on compte tous les directeurs de programme de MF, certains coordonnateurs de programme de 3e année, des résidents et d’autres acteurs dans la communauté.
MÉTHODES
Les sondages auprès des résidents étaient accessibles dans le Web; des invitations à y participer ont été envoyées par les programmes de MF au moyen de listes de courriels. Les sondages auprès des directeurs et des coordonnateurs de programme ont été distribués par la poste. Les entrevues ont été enregistrées sur bande sonore et transcrites, puis les auteurs ont codé les entrevues en fonction de grands thèmes.
PRINCIPALES CONSTATATIONS ET RÉSULTATS
Le taux de réponse aux sondages variait entre 34 % et 39 % chez les résidents et se situait à 78 % chez les directeurs et coordonnateurs de programme. Les répondants convenaient que les programmes devraient inclure des options de formation flexibles de durées différentes. La demande de formation est davantage déterminée par les besoins des résidents que par des facteurs reliés à la communauté et au système de santé, et elle est soit stable ou à la hausse. Dans l’ensemble, les répondants croyaient qu’environ le tiers des diplômés du programme de base devraient avoir la possibilité de faire une 3e année de formation. Ils croyaient que le retour de pratique devrait être autorisé, mais que les ententes de réciprocité de service obligatoires n’étaient pas souhaitables. Les attributions de postes au programme et la sélection des résidents sont un processus complexe dans lequel le mérite du résident joue un rôle important. Les répondants prévoyaient que les R3 diplômés pratiqueraient différemment des R2 diplômés et offriraient des soins de meilleure qualité dans leur domaine. Ils croyaient aussi que les R3 diplômés exerceraient des rôles plus prédominants en leadership et en enseignement que les diplômés du programme de base.
CONCLUSION
Il est probable que les programmes de 3e année de formation continuent à s’accroître et à former une composante de plus en plus importante du système de formation en MF au Canada. Il est essentiel d’avoir des programmes flexibles qui peuvent s’adapter aux systèmes d’éducation et de santé et aux besoins de la collectivité. Les programmes de formation, et les collèges national et provinciaux de MF devront aussi assurer que ces médecins aient la possibilité de maintenir leurs liens avec le reste de la communauté de la MF.
Postgraduate year (PGY) 3 residency programs for graduates in family medicine (FM) are designed to provide additional training in particular areas of practice. Although we did not locate a defining document describing the policy development, design, and implementation of the FM PGY3 program, it seems to owe its roots to a crisis in emergency medicine (EM) staffing in the early 1980s. In 1982, the College of Family Physicians of Canada (CFPC) recognized a third-year training program in EM. Programs in care of the elderly and palliative care soon followed.1 In 1991, 4 of the chairs of FM departments in Ontario noted “a number of weaknesses in the health care system have been identified where family physicians with specific training would be the most efficient and effective way to better serve the community’s needs.”2 Since then, the number of positions in Ontario funded by the Ministry of Health and Long-Term Care (MOHLTC) has grown steadily, reaching 70 in 2005. Decisions about program size and content in Ontario have been influenced by 2 major reports on physician supply, both of which supported the contributions of FM PGY3 programs to meeting community health care needs and supported expansion of these programs.3,4 Nationally, there was also expansion in the development of these programs, from 66 positions (10% of PGY2 positions) in 1989 to about 130 (18% of PGY2 positions) in 1999.5,6 Since then, core FM programs have expanded more rapidly than PGY3 programs so that in 2004 there were 196 positions representing only 12.7% of PGY2 positions.7 Programs now exist in a range of areas, including EM, anesthesia, palliative care, obstetrics, maternal and child health, rural medicine, women’s health, surgery, psychiatry, care of the elderly or geriatrics, sports medicine, addictions, international health, environmental health, HIV and AIDS, aboriginal health, breast diseases, academic FM, and research.8 In the fall of 2001, the CFPC gave final approval to a framework for accreditation of programs for enhanced skills for family practice, “which will provide FM departments with an academic base for planning and overseeing a range of learning opportunities for FM graduates and for practicing physicians who wish to upgrade their skills or acquire new ones to meet the needs of the populations they serve.”9
METHODS
We employed mixed methods for this research. Ethics approval was granted by the Health Science Research Ethics Board at Queen’s University in Kingston, Ont. The study was guided by a steering committee that included representatives from FM programs, the MOHLTC, the Postgraduate Committee of the Council of Ontario Faculties of Medicine, and the Professional Association of Internes and Residents of Ontario. A literature review and feedback from the first program director key informant interview were used to construct the interview guides and a series of related surveys. Draft versions were provided to the steering committee for feedback before implementation. An e-mail request to complete an electronic Web-based survey (www.surveymonkey.com) was distributed by FM programs via e-mail lists of residents. The request was distributed again 2 weeks later. A postal survey of all core program directors and PGY3 program coordinators in Canada was also conducted. Questionnaire recipients received an e-mail reminder approximately 3 weeks after the original mailing. Survey results were entered into Microsoft Access then transferred to SPSS, version 16, and Stata, version 10, for statistical analysis. Descriptive statistics with 95% confidence intervals were calculated for survey responses. We used t tests (for ordinal variables) and χ2 and Fisher exact tests (for categorical variables) to calculate statistical significance between groups.
Semistructured interviews were conducted with various key informants. These included all FM core program directors, a sample of PGY3 program directors and coordinators, first-, second-, and third-year residents from a number of different programs, and key stakeholders, including a representative from the CFPC and a community development officer working on physician recruitment. Recruitment for the interviews was limited to Ontario. All interviews used a standard interview guide, which was not substantially different between groups. Interviews were audiotaped then transcribed. Two transcripts (1 program director and 1 resident) were reviewed by all investigators (M.G., R.V.B., K.M.) and 1 research associate (J.S.), and themes were identified independently. The team then met to review their findings and reach consensus on a preliminary coding structure. The remaining transcripts were reviewed by the research associate (J.S.) and 1 investigator (M.G.) for coding and identification of any additional themes. A final meeting of the full investigative team was convened to determine the final coding structure.
FINDINGS
Response rates for the surveys were 34.0% for PGY1 and PGY2 residents, 38.6% for current PGY3 residents, and 78.2% for program directors (Table 1). The investigative team completed interviews with 18 key informants for the review. Six interviews were completed with FM program directors, and 2 interviews were conducted with PGY3 program coordinators. Additionally, 8 FM residents (2 PGY1, 3 PGY2, and 3 PGY3) participated in interviews. Of the PGY3 residents interviewed, 2 were enrolled in EM and 1 in palliative care. The remaining 2 interviews were with a community development officer working on physician recruitment and a key informant from the CFPC. Saturation of themes was achieved with few new ideas emerging after the first 6 interviews.
Table 1.
Survey response rates
| RESPONDENTS | SAMPLE SIZE | NO. OF RESPONSES | RESPONSE RATE |
|---|---|---|---|
| Web-based survey respondents | |||
| • PGY1 and PGY2 | Approximately 400 | 136 | 34.0%* |
| • PGY3 | Approximately 70 | 27 | 38.6%* |
| Mail survey respondents | |||
| • Program directors and PGY3 program coordinators | 80 distributed | 61 | 78.2% |
| 78 valid sample (2 returned to sender) | |||
PGY–postgraduate year.
Note that owing to the time limitations and privacy issues regarding resident e-mail, all communication regarding participation in the Web-based survey was handled by residency training programs, not the research team. The estimated response rates here are based on Canadian Post-M.D. Education Registry census data adjusted for late entry of international medicine graduates and unfilled PGY3 positions. We were not able to do direct follow-up to determine exact numbers of e-mails sent, number of valid e-mail addresses, or number of e-mails received and read, so it is not possible to verify how many residents actually received the request to participate.
Table 2 presents the survey results on desirable characteristics of PGY3 programs. All interviewed groups were supportive of there being a mix of programs with a fixed curriculum and duration targeted at specific areas of practice (eg, EM, anesthesia) as well as programs that were flexible and could be tailored to meet specific needs (resident or community identified). Interviewees generally expressed support for tailored or self-directed training:
Table 2.
Types of PGY3 positions respondents thought should be offered
| QUESTION | PGY1 AND PGY2, % ANSWERING YES (95% CI) N = 136 | PGY3, % ANSWERING YES (95% CI) N = 27 | PROGRAM DIRECTORS AND COORDINATORS, % ANSWERING YES (95% CI) N = 61 | TOTAL , % ANSWERING YES (95% CI) N = 224 |
|---|---|---|---|---|
| Should the length of training be flexible?* | 85.3 (78.2–90.8) | 77.8 (57.7–91.3) | 63.3 (50.6–75.8) | 78.6 (72.6–83.8) |
| Should tailored or self-directed programs be offered?* | 93.6 (90.6–98.4) | 85.2 (66.3–95.8) | 81.7 (70.0–90.6) | 90.6 (86.0–94.1) |
| Should training be linked to return-of-service agreements? | 17.8 (11.6–25.1) | 3.7 (0.1–19.0) | 14.8 (7.0–26.2) | 15.2 (10.7–20.6) |
| Should re-entry candidates have specific allocated positions? | 39.5 (31.4–48.4) | 37 (19.4–57.6) | 52.5 (39.3–65.4) | 42.9 (36.3–49.6) |
| Should re-entry candidates be considered with current residents in the same applicant pool? | 36.4 (28.7–45.5) | 33.3 (16.5–54.0) | 45.9 (33.1–59.2) | 38.8 (32.4–45.6) |
PGY–postgraduate year.
Program directors were significantly less likely than PGY1 and PGY2 residents to support flexible length of training (P = .001) or tailored or self-directed programs (P = .01).
I think that there are a whole range of other [PGY3] experiences that could be much more individually structured because the physician wants to add a particular component to their practice or a service that they can provide to a community … so that they can be more responsive to, you know, the needs of places they may be planning to work. (Program director)
Informants generally agreed that mandatory return-of-service agreements should not be required.
I don’t think that it’s necessarily a fair thing to do. We don’t have an allocation for any other type of general residency program, so I’m not sure what the drive would be to do that in particular with the PGY3 year. I don’t see why it should be differentiated within a family medicine program … so my general feeling would be, that would be something that I wouldn’t want to see. (Program director)
Interviewees tended to view community-sponsored funding more favourably than return-of-service agreements. Interviewees perceived these types of voluntary arrangements as less coercive than programs that were linked with return-of-service agreements as a matter of policy, and thought they should be permitted.
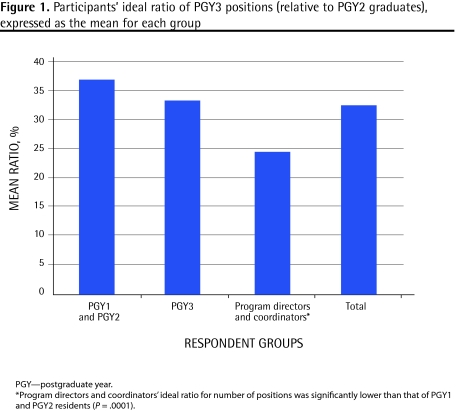
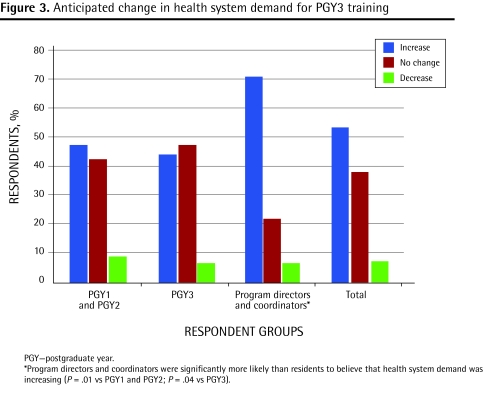
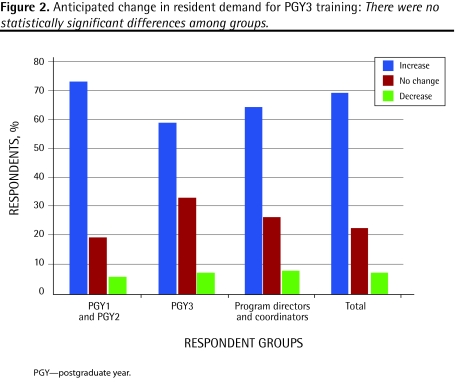
Table 3 and Figures 1 to 3 present survey results on questions about the number of positions that should be offered and anticipated changes in demand in the future. Informants were asked to indicate what they thought was an ideal ratio of PGY3 positions relative to the number of residents graduating from the PGY2 program. Some thought that everybody should have an opportunity to complete PGY3 training if so desired, while others believed minimal positions were required. In general, however, informants thought that approximately 1 PGY3 training position should be available for every 3 PGY2 graduates. Generally, informants believed the demand for PGY3 training positions would increase in the future. Many interviewees cited population demographics as a definitive factor in helping to determine demand for positions. For example, care of the elderly was commonly cited as a program for which demand would increase, given the aging population.
Table 3.
Factors influencing current demand for PGY3 training: Responses are based on a 5-point scale, in which 1 was very important and 5 was not at all important, and are expressed as the mean score of respondents in each group.
| RESPONDENT GROUP | RESIDENT ACADEMIC NEEDS | POPULATION OR COMMUNITY NEEDS | HEALTH SYSTEM NEEDS | EARNING POTENTIAL |
|---|---|---|---|---|
| Postgraduate directors and program coordinators | 2.42* | 2.70 | 2.85 | 3.08 |
| PGY1 and PGY2 | 2.24* | 2.69 | 2.74 | 2.62 |
| PGY3 | 1.81* | 2.93 | 2.96 | 2.56 |
PGY–postgraduate year. *Lowest average values. Scores for resident academic needs were significantly different (paired t tests) from earning potential (program directors and coordinators P = .007; PGY1 and PGY2 P = .004; PGY3 P = .003), health system needs (program directors and coordinators P = .04; PGY1 and PGY2 P < .001; PGY3 P < .001), and population needs (PGY1, PGY2, and PGY3 only P < .001).
Figure 1.
Participants’ ideal ratio of PGY3 positions (relative to PGY2 graduates), expressed as the mean for each group
Figure 3.
Anticipated change in health system demand for PGY3 training
Table 3 further summarizes survey responses to questions about underlying drivers of demand for these programs. Key informants indicated that the demand for PGY3 programs was driven, in large part, by resident demand, with community and health system needs being somewhat less important. A number of resident factors that drive demand were identified. These included the notion that PGY3 training provided an opportunity to acquire additional and specialized skills in a particular area. One resident interviewee stated that residents see PGY3 training programs as a way of “predefining a nice niche for themselves …. I think that’s the major reason people are drawn to them.” Third-year training also enables graduates of the 2-year core program to complete additional training as a means of satisfying academic needs and building greater confidence and competence before entering practice. One resident stated, “residents … feel like they can get that extra year if they need it.” A program director, in referring to competence, stated that some residents are motivated to continue training “after 2 years [because they are] just not feeling that they’re competent at that point for whatever reason …. [I]t’s kind of this need to keep learning.” Informants also indicated that PGY3 training was driven by the anticipation of greater remuneration, employability, lifestyle flexibility, and geographic mobility.
To a lesser extent than resident need, interviewees believed that demand for PGY3 training was driven by community need; however, many thought that community need should be a more prominent factor in driving demand.
[I]t’s probably what they think they can take as family physicians to the community and their assessment of what communities need. (Resident)
Often in smaller communities there’s not the population base to support full Royal College–type specialists; people need to have a varied practice … they can use part of their work to bring out the needed skills for the community. (Program director)
Position allocation is seen as a complex process, which integrates perceived community needs, resident demand, and program needs. Table 4 summarizes the survey responses to questions about current and “ideal” practices for allocating available positions to different programs. One program director interviewee stated, “community need and resident needs, certainly are part of the criteria, funding is clearly a criteri[on], capacity of the various programs to train people is a criteri[on].” Allocation by program type varies minimally between institutions and general commonalities are evident. General targets for the number of positions available for a particular program in a given year are often determined before receiving applications. Some institutions have a set number of positions available in a particular program in a given year, which is viewed as undesirable and inefficient. Many schools have a degree of flexibility to use unfilled positions in one program for candidates interested in other areas. As the EM match is coordinated nationally by the Canadian Resident Matching Service, a decision about the number of EM positions available must be made in accordance with the timelines imposed by this process. Most interviewees suggest that positions should be allocated based on a number of factors. One program director stated, “you really can’t 100% allocate based on students’ needs; I realize that because we’re ultimately servicing the community. [Therefore] I think the major factor is going to have to be … what the needs of the community are.”
Table 4.
Ideal allocation criteria versus current allocation criteria: Responses are based on a 5-point scale, in which 1 was very important and 5 was not at all important, and are expressed as the mean score of respondents in each group.
| CRITERIA | PROGRAM DIRECTORS AND COORDINATORS | PGY1 AND PGY2 | PGY3 | CURRENT CRITERIA* |
|---|---|---|---|---|
| Training program | 2.65 | 2.54 | 2.30 | 2.62 |
| Resident selection | 2.47 | 2.27 | 2.19 | 2.40 |
| Combination of program and resident selection | 2.46 | 2.16† | 2.00 | 2.73 |
| Population or community needs | 2.26† | 2.38 | 2.41 | 3.02 |
| Funding | 3.13 | 2.97 | 2.77 | 2.64 |
| Resident merit | 2.42 | 2.36 | 1.67† | 2.25† |
PGY–postgraduate year.
Current criteria were rated by program directors and coordinators.
Lowest average scores. For program directors and coordinators, funding source was significantly less important (paired t tests P < .01) than resident merit, population or community needs, combined program-resident selection, and resident selection alone. For PGY1 and PGY2 residents, combined program-resident selection was significantly different from program alone (P < .001), funding source (P < .001), and population or community needs (P = .03); resident selection was significantly different from program (P = .005); and funding source was significantly lower (P < .001) than resident selection, merit, and population or community needs. For PGY3 residents, merit was significantly more important (P < .05) than all other options, except for a combination of program and resident selection, and funding was significantly less important (P < .05) than all other factors except for population and community needs. For current criteria, resident merit was significantly different from population or community needs (P < .001), combination of training program and resident selection (P = .01), and training program alone (P = .04); resident selection was significantly different from population or community needs (P = .01).
Candidates are generally accepted to programs based on merit, but a degree of consideration might be given to community and program needs. Table 5 presents program directors’ responses to questions on factors used to select residents for PGY3 positions. Residency programs strive to determine if the objectives of both the resident and the particular position are compatible. Although programs do not restrict the application process to their own PGY2 graduates, informants expressed that PGY2 graduates of a given residency program were at an advantage to receive PGY3 positions at the same institution. One program director stated, “I think [PGY3 positions] should be open to anyone …. Somebody that is from their own medical school might be given a few more points.”
Table 5.
Relative importance of different criteria for the selection of residents for third-year programs: Responses are based on a 5-point scale, in which 1 was very important and 5 was not at all important, and are expressed as the mean score.
| CRITERIA | PROGRAM DIRECTORS’ AND COORDINATORS’ RATING |
|---|---|
| Resident’s demonstrated abilities | 2.03* |
| Resident’s plan for practice | 2.29 |
| Combination of ability and plan for practice | 2.20 |
| Population, community, and institutional needs | 2.72 |
| Funding | 2.59 |
| Resident’s commitment to use PGY3 training | 2.36 |
Lowest average score. Resident ability was significantly more important (paired t tests) than population, community, and institutional needs (P = .001) and funding source (P = .007). Population, community, and institutional needs were significantly less important than resident practice plans (P = .01), combined resident ability and practice plans (P = .008), and commitment to use training (P = .03).
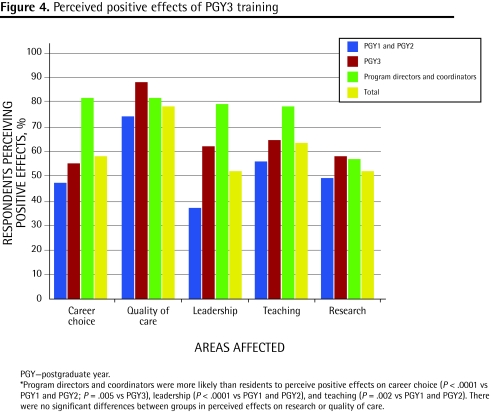
Figure 4 summarizes views on the effects of PGY3 programs on recruitment of medical students to careers in FM; quality of care delivered; and contributions to leadership, teaching, and research in FM. Informants agreed that PGY3 training opportunities in FM had an effect on recruiting medical students. One resident thought “it probably does play a role for recruitment because I think a lot of people are coming in knowing that they can potentially do an extra year of something that focuses them in their interest.” Access to PGY3 training might also be an important consideration to applicants of FM programs during the Canadian Resident Matching Service match. One program director stated, “[O]ne of the probably top 5 questions that we get from applicants is, how many PGY3 programs do you have in your program … [and] what’s the distribution?”
Figure 4.
Perceived positive effects of PGY3 training
Informants agreed that PGY3 training has a definite effect on practice patterns. Many of the informants expressed concern that PGY3 training, most notably in EM, might detract from the practice of FM, which results in less time being devoted to FM. Emergency medicine training is largely thought to result in practice solely dedicated to work in an emergency department. Some informants, however, suggested that such training might create physicians who practise more comprehensive care. One program director stated, “I don’t think [PGY3 training] changes the role of the family doctor; to me it maintains the role of the family doctor in being able to provide some secondary care skills.”
Informants generally agreed that PGY3 training resulted in improved quality of care. One program director stated, “Somebody with 6 months or [an] additional year of training … brings a huge skill set to the community, and I believe it really, substantially raises the bar in terms of standards of care.” There was agreement that quality of care can improve across all aspects of practice owing to an increased knowledge base, enhanced skills, and greater confidence. Most informants believed that improved quality of care was more specific to the area in which the physician completed PGY3 training. Many respondents thought that quality of care levels converged between core program and PGY3 graduates with the passage of time.
In terms of other professional roles, informants thought that PGY3 training could lead to increased roles in leadership, teaching, and research.
[T]o have one person in a rural area … covering small towns … who has a high level of skill in the management of palliative care gives the family doctors through that whole region somebody to call … and say, look, I got this patient with following symptoms … what should I do next? (Program director)
DISCUSSION
The role and effect of PGY3 enhanced skills programs has been a subject of great debate within the FM community. The need for family physicians with specialized skills in particular areas is well recognized.10–15 There are, however, concerns about diversion of effort or individuals away from comprehensive FM and into more specialized practice, particularly in the area of EM.1,16 Saucier’s editorial on the subject in 2004 elicited a strong response from others in the profession.1,17–20 Despite the debate, there has been only a limited amount of original research to help inform the discussion. The findings reported here clearly indicate that the demand for these programs is expected to remain strong and grow in the future. The educational needs and special interests of residents were seen as more important drivers of resident demand than employment opportunities, income or earning potential, or community or health system needs. Overall, survey respondents thought that there should be about 1 PGY3 position for every 3 PGY2 graduates. Program directors and coordinators had the lowest suggested ratio (1:4), which was significantly lower than that suggested by PGY1 and PGY2 residents (2:5). The interviews with program directors in Ontario were more in keeping with a 1:3 ratio, so the national nature of the survey and variation in opinion across regions could account for the lower ratio suggested by this group of respondents. This is, however, also a much lower number than reported in a national survey of core program directors done in 1996, which suggested a ratio of 40%.6 Changes in attitudes over time or inclusion of PGY3 program coordinators as well as core program directors could also account for this finding.
Both survey and interview participants expressed strong support for flexible programs of varying duration. There is almost no support for return-of-service provisions, which participants viewed as unfair and coercive. Interestingly, there were mixed views on how to handle re-entry candidates, with a fairly even split in opinion as to whether they should compete directly with direct-entry candidates or have their own pool of positions.
The means by which positions are allocated to programs and residents are selected into these programs is currently a complex process that combines selection and allocation, such that the quality of the applicants can exert an influence over the number of positions allocated to a particular area of training. Although program directors thought that population and community health needs should be the most important criteria for determining how positions are allocated, at present resident merit tops the list. Residents’ plans for future practice are also an important consideration. None of the programs in Ontario is using data on health system needs to determine allocation of positions, in large part owing to the lack of a consistent reliable source of information on what those needs are.
By far, most respondents were convinced that PGY3 training has a substantial effect on future patterns of practice and that such training results in improved quality of care. Concern remains about diversion of activity from FM to specialized areas of care, in particular to EM. Most also believed that such programs exerted a positive influence in attracting medical students to careers in FM and producing future teachers for our profession; approximately half of respondents believed PGY3 training affects leadership and research.
Limitations
Study limitations include the restriction of interviews to Ontario and the response rate of the resident Web-based surveys. The lower participation rate for residents increases the possibility of a selection bias. If one is present, it would most likely result in an increase in the reported level of interest in PGY3 programs, as those residents who were not interested would be less likely to respond to the request to participate. This same effect might make the respondents more likely to have positive views of PGY3 programs in general.
Conclusion
These results suggest that PGY3 programs are likely to form an increasingly important part of the FM training system in the future. Demand is high and rising, and it seems likely that the number and types of positions offered will continue to grow. Flexible programs that are able to respond to the changing educational needs of core program graduates and to changes in demand for particular services are considered particularly desirable. It will be important to ensure that the numbers and content of these programs meet health system needs in addition to the educational needs and interests of trainees. Training programs and national and provincial colleges of FM will also need to ensure that these physicians are provided with opportunities to maintain their ties with the rest of the FM community.
Figure 2.
Anticipated change in resident demand for PGY3 training: There were no statistically significant differences among groups.
Acknowledgment
This study was funded by the Council of Ontario Universities and the Ontario Ministry of Health and Long-Term Care. The views presented here are those of the authors and not of the Ministry of Health and Long-Term Care or the Council of Ontario Universities. We would like to thank the members of our steering committee for their valuable input: Anna Cain, Marg Harrington, Dr Leslie Flynn, Dr Maureen Topps, Dr David Tannenbaum, Dr Roy Wyman, and Dr Erika Catford.
EDITOR’S KEY POINTS
The role and effect of third-year enhanced skills programs has been a subject of great debate within the family medicine community. The need for family physicians with specialized skills in particular areas is well recognized, but there are concerns about diversion of effort or individuals away from comprehensive family medicine and toward more specialized practice.
There has been only a limited amount of original research to help inform the discussion. This article and a companion paper comparing the practice patterns of 2- and 3-year program graduates aim to provide additional information about current trends and future needs.
POINTS DE REPÈRE DU RÉDACTEUR
Le rôle et l’influence des programmes de 3e année de formation en compétences avancées font l’objet de grands débats au sein de la communauté de la médecine familiale. On reconnaît bien la nécessité d’avoir des médecins de famille ayant des habiletés spécialisées dans certains domaines, mais on s’inquiète d’une éventuelle diversion des efforts ou d’un éloignement de la pratique familiale complète au profit d’une pratique plus spécialisée.
Il n’existe pas beaucoup de recherche originale sur le sujet pour aider à éclairer le débat. Cet article et un document d’accompagnement comparant les habitudes de pratique des R2 et des R3 diplômés visent à fournir des renseignements additionnels au sujet des tendances actuelles et des besoins futurs.
Footnotes
*Full text is available in English at www.cfp.ca.
A companion paper on the practice patterns of 2- and 3-year program graduates can be found on page 906.
Competing interests
Dr Green, Dr Birtwhitle, and Mr MacDonald all received consulting fees from the Ontario Ministry of Health and Long-Term Care and the Council of Ontario Universities to conduct this research.
Contributors
Dr Green, Dr Birtwhistle, and Mr MacDonald all contributed to the study design. Dr Green and Mr Schmelzle performed the key informant interviews and conducted the analysis of survey results. Dr Green, Dr Birtwhistle, Mr Schmelzle, and Mr MacDonald participated in the analysis of transcripts for the qualitative portion of the study. All authors contributed to the drafting and revising of the manuscripts.
This article has been peer reviewed.
References
- 1.Saucier D. Second thoughts on third-year training. Can Fam Physician. 2004;50:687–9. 693–5. Eng. Fr. [PMC free article] [PubMed] [Google Scholar]
- 2.Rosser WW, Forster J, Hennan B, Sorbie J. Paper prepared for the Council of Ontario Faculties of Medicine. Toronto, ON: Council of Ontario Faculties of Medicine; 1991. Towards improving health care delivery for Ontario citizens: third year residency positions in family medicine. [Google Scholar]
- 3.McKendry R. Report of the Fact Finder on Physician Resources in Ontario. Toronto, ON: Ontario Ministry of Health and Long-Term Care; 1999. Physicians for Ontario. Too many? Too few? For 2000 and beyond. [Google Scholar]
- 4.George P, Goodwin S, Walker P, Howcroft M, Lapaine M, Beck G, et al. Report of the Expert Panel on Health Professional Human Resources. Toronto, ON: Ontario Ministry of Health and Long-Term Care; 2001. Shaping Ontario’s physician workforce: building Ontario’s capacity to plan, educate, recruit and retain physicians to meet health needs. [Google Scholar]
- 5.Busing N. Survey of third-year postgraduate training positions in family medicine. Can Fam Physician. 1992;38:1393–6. [PMC free article] [PubMed] [Google Scholar]
- 6.Chaytors RG, Spooner GR, Moores DG, Woodhead-Lyons SC. Postgraduate training positions. Follow-up survey of third-year residents in family medicine. Can Fam Physician. 1999;45:88–91. [PMC free article] [PubMed] [Google Scholar]
- 7.Canadian Post-M.D. Education Registry. Individual specialty. Tables, family medicine. Ottawa, ON: Canadian Post-M.D. Education Registry; 2004. [Accessed 2009 Jan 31]. Available from: www.caper.ca/data_tables_2004/individual_specialties_family_medicine_en.php#Field%20of%20Training:%20Family%20Medicine. [Google Scholar]
- 8.Naismith A, Warneboldt J. The diversity of family medicine fellowship programs. Can J Rural Med. 2005;10(4):268. [PubMed] [Google Scholar]
- 9.Gutkin C, Rainsberry P. Innovative new program: enhanced skills for family practice. Can J Rural Med. 2002;7:77–8. [Google Scholar]
- 10.Lloyd S, Streiner D, Shannon S. Family medicine residency programs. Evaluating the need for different third-year programs. Can Fam Physician. 1994;40:273–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Chiasson PM, Roy P. Role of the general practitioner in the delivery of surgical and anesthesia services in rural western Canada. CMAJ. 1995;153(10):1447–52. [PMC free article] [PubMed] [Google Scholar]
- 12.Ducharme J. Preparing emergency physicians for the future. CMAJ. 2003;168(12):1548–9. [PMC free article] [PubMed] [Google Scholar]
- 13.Brown G, Godwin M, Seguin R, Ashbury EL. Family medicine anesthesia. Sustaining an essential service. Can Fam Physician. 2005;51:538–9. [PMC free article] [PubMed] [Google Scholar]
- 14.College of Family Physicians of Canada, Society of Rural Physicians of Canada, Society of Obstetricians and Gynaecologists of Canada. Joint position paper on training for rural family practitioners in advanced maternity skills and cesarean section. Can Fam Physician. 1999;45:2416–22. 2426–32. Eng. Fr. [PMC free article] [PubMed] [Google Scholar]
- 15.Working Group on Postgraduate Education for Rural Family Practice. Postgraduate education for rural family practice. Vision and recommendations for the new millennium. Can Fam Physician. 1999;45:2698, 2700, 2703–4, 2717–21. Eng. Fr. [PMC free article] [PubMed] [Google Scholar]
- 16.Chan BT. Do family physicians with emergency certification actually practise family medicine? CMAJ. 2002;167(8):869–70. [PMC free article] [PubMed] [Google Scholar]
- 17.Letovsky S. Third year in family medicine: headed for disaster [Letters] Can Fam Physician. 2004;50:1209. [PMC free article] [PubMed] [Google Scholar]
- 18.Webster RW. Third year in family medicine: headed for disaster [Letters] Can Fam Physician. 2004;50:1209–10. [PMC free article] [PubMed] [Google Scholar]
- 19.Wong E. Third year in family medicine: headed for disaster [Letters] Can Fam Physician. 2004;50:1210–1. [PMC free article] [PubMed] [Google Scholar]
- 20.Goertzen J. More thoughts on third-year training [Letters] Can Fam Physician. 2004;50:1355. [PMC free article] [PubMed] [Google Scholar]