Abstract
Background
More than 50% of incarcerated individuals have a history of substance use, and over 200,000 individuals with heroin addiction pass through American correctional facilities annually. Opiate replacement therapy (ORT) with methadone or buprenorphine is an effective treatment for opiate dependence and can reduce drug-related disease and recidivism for inmates. Provision of ORT is nevertheless a frequently neglected intervention in the correctional setting.
Objective and Methods
We surveyed the 50 state; Washington, District of Columbia (DC); and Federal Department of Corrections' medical directors or their equivalents about their facilities' ORT prescribing policies and referral programs for inmates leaving prison.
Results
We received responses from 51 of 52 prison systems nationwide. Twenty-eight prison systems (55%) offer methadone to inmates in some situations. Methadone use varies widely across states: over 50% of correctional facilities that offer methadone do so exclusively for pregnant women or for chronic pain management. Seven states' prison systems (14%) offer buprenorphine to some inmates. The most common reason cited for not offering ORT was that facilities “prefer drug-free detoxification over providing methadone or buprenorphine.” Twenty-three states' prison systems (45%) provide referrals for some inmates to methadone maintenance programs after release, which increased from 8% in 2003; 15 states' prison systems (29%) provide some referrals to community buprenorphine providers.
Conclusion
Despite demonstrated social, medical, and economic benefits of providing ORT to inmates during incarceration and linkage to ORT upon release, many prison systems nationwide still do not offer pharmacological treatment for opiate addiction or referrals for ORT upon release.
Keywords: methadone, corrections, buprenorphine, prison, opiate replacement therapy
1. Introduction
The United States has the world's highest incarceration rate, with approximately 10 million individuals incarcerated each year (Sabol and Couture, 2008; Walmsley, 2008). In 2007, over 2.2 million individuals were imprisoned at any given time, and an estimated seven to eight million others cycled through the country's prisons (facilities designated for long-term confinement upon conviction of crimes) and jails (facilities that house individuals detained for short periods of time, usually six months or less, often while they await trial) (Sabol and Couture, 2008). The number of incarcerated individuals has grown steadily since 1980, and in 2007, the number of incarcerated individuals rose 1.8% over 2006 (Sabol and Couture, 2008; Walmsley, 2008). Growth in incarceration rates can be largely attributed to the “war on drugs,” which has resulted in harsher penalties for drug offenses and has led to a three-fold increase in drug-related arrests; over half of all sentences in federal prisons are for federal drug-related offenses (Drucker, 1999)(Greifinger 2007). Studies have found that between 50% and 84% of prison inmates have a history of substance use (Drucker, 1999; Greifinger, 2007; Mumola and Karberg, 2006), most in the year prior to incarceration (Mumola and Karberg, 2006). An estimated 20% of state inmates have a history of injection drug use (Mumola and Karberg, 2006), and approximately 24-36% of all heroin addicts, or over 200,000 individuals, pass through the US criminal justice system each year (Rich et al., 2005a). Moreover, prisoners often engage in substance use during incarceration (Clarke et al., 2001; Kang et al., 2005; Krebs and Simmons, 2002; Seal et al., 2008).
Inmates face disproportionately higher burdens of disease with mental illness, substance use and infectious diseases, including HIV/AIDS, hepatitis, other sexually transmitted infections, tuberculosis and others (Greifinger, 2007; Hammett, 2006). Many inmates are uninsured, lack adequate access to health services, and come from medically underserved communities (Freudenberg, 2001). Because correctional systems have high turnover rates and reincarceration rates, inmate health also profoundly affects the health of the communities to which they return (Greifinger, 2007; Nurco et al., 1991). Providing inmates with comprehensive health services, including treatment for chemical dependency with pharmacological therapy and counseling services, therefore offers a unique public health opportunity (Bick, 2007; Rich et al., 2005b).
Inmates' transitions back to their communities are often associated with increased health risks, particularly increased sexual and drug-related risks (Visher and Mallik-Cane, 2007). Approximately 55% of individuals with a history of substance use will relapse to substance use within one month of release from incarceration (Nurco et al., 1991). Relapse to substance use is also associated with increased criminal activity (Hanlon et al., 1990; Nurco et al., 1991), risk of HIV and HCV infection (Inciardi and Needle, 1998), drug overdose (Binswanger et al., 2007; Bird and Hutchinson, 2003), death from drug related overdose (Krinsky et al., 2009) and reincarceration (Gore et al., 1995; Lipton, 1992). Offering inmates pharmacological treatment and counseling for opiate dependence prior to release decreases the likelihood of drug relapse (Gordon et al., 2008; Kinlock et al., 2008a; Martin, 1999), overdose (Gordon et al., 2008; Martin, 1999), recidivism, and HIV risk behaviors (Springer and Altice, 2007) and increases the likelihood of remaining in long-term drug treatment upon release (Gordon et al., 2008; Kinlock et al., 2002; Kinlock et al., 2008a; Martin, 1999). Incarceration also offers an opportunity to intervene and break the cycle of addiction, health risks, criminal behavior, and re-incarceration.
Methadone maintenance therapy (MMT) is an opiate replacement therapy (ORT) that has been used in the United States for nearly 50 years to treat chronic heroin addiction (Dole et al., 1969; McLellan et al., 1993). Methadone prevents withdrawal symptoms and drug cravings, blocks the euphoric effects of other opiates, and reduces the risk of relapse to illicit use of opiates, infectious disease transmission, and overdose death (Gerra et al., 2003; Kreek, 1992, 2000). MMT use among prisoners, particularly around the time of release, is associated with reduced drug injection, HIV and HCV transmission (Marsch, 1998; Springer and Altice, 2007), drug-related criminal activities (Gordon et al., 2008; Kinlock et al., 2008b), recidivism, and increased participation in drug treatment programs (Gordon et al., 2008; Kinlock et al., 2002; Kinlock et al., 2008b)
Buprenorphine is an ORT that acts as a partial opioid agonist (Fiellin and O'Connor, 2002). Buprenorphine was approved by the FDA in 2002 for the management of opioid addiction by community and correctional physicians (Comer and Collins, 2002). Buprenorphine is often combined with naloxone and administered sublingually as Suboxone© to reduce the likelihood of diversion (Comer and Collins, 2002). Since its 1996 approval in France, buprenorphine has been prescribed widely for ORT and is associated with improved stability in housing and employment; reduced self-reported heroin use; and decreased risk of HIV, HBV, and HCV infection; and mortality decline attributable to overdose (Auriacombe et al., 2004; Auriacombe et al., 2001; Carrieri et al., 2006; Fhima et al., 2001). Compared with methadone, buprenorphine has fewer regulations governing its use, lower likelihood of fatal overdose, and is associated with less social stigma. Because buprenorphine must be prescribed by a physician, it also provides opportunities for more routine medical care. Although the cost of Suboxone© has been a barrier to its widespread use, its orphan drug status expires in October 2009, which will allow generic manufacturing of the medication and anticipated concomitant decreased cost.
Given the health and social risks associated with opiate use, both the Center for Disease Control and Prevention (CDC) and the World Health Organization (WHO) recommend that correctional systems offer health programs to prevent substance use relapse upon community transition (CDC, 2002; WHO, 2007). In addition, WHO includes both methadone and suboxone in the essential medicines list (EML) (Møller et al., 2007). The EML is a list of pharmaceutical products that WHO recommends that all health systems or governments should make available to their populations. WHO guidelines also hold that drugs made available in the community should also be made available in prison (Møller et al., 2007). The Commission of the European Communities reports that numerous European Union member states have adopted these recommendations: 17 provide methadone maintenance and 10 provide buprenorphine treatment in prisons, although coverage varies widely (CEC, 2007). However, most prison systems in the rest of the world do not offer MMT and buprenorphine in the correctional setting (WHO, 2005) (WHO, 2008).
Our 2003 survey examining the attitudes and practices of medical directors of state and federal prisons regarding methadone treatment found that just under 50% of US prison systems used methadone; when used, methadone is limited primarily to the treatment of pregnant inmates or for acute detoxification (Rich et al., 2005b). Only 8% of prison systems referred inmates with a history of opiate dependence to community-based methadone programs upon release; approximately 30% reported that they believed that methadone benefits opiate-dependent prisoners. To assess changes in attitudes and practices during the last five years, and to learn more about buprenorphine prescribing and referral practices since its approval, we surveyed the medical directors, their equivalents, or appointed designees of state prisons and the District of Columbia and federal prison systems about their opinions and prescribing practices for methadone and buprenorphine. Our survey also included questions about prison policies related to referring prisoners to community-based ORT programs upon release.
2. Methods
We emailed or faxed a 17-question survey to the medical directors, equivalent health authorities, or their designees of the 50 state Departments of Corrections. The 50 state Departments of Corrections collectively house approximately 1.4 million prisoners. We also surveyed the Federal Bureau of Prisons and the District of Columbia prison, which collectively house approximately 200,000 prisoners (Sabol and Couture, 2008). We subsequently contacted several respondents by email and telephone to remind them to complete the survey. Survey questions addressed opiate screening practices, methadone and buprenorphine provision within the prison setting; attitudes about the utility of buprenorphine and methadone; and prison ORT referral practices for inmates leaving prison. Some questions allowed respondents to provide open-ended responses to complement close-ended survey questions. The survey concluded with a free response question encouraging respondents to provide any additional comments related to prescribing and referral practices. Respondents did not receive any compensation or incentives for responding to the survey. The survey is available online at the Center for Prisoner Health and Human Rights: http://www.prisonerhealth.org/.
Respondents who indicated their facilities provided methadone or buprenorphine were asked to provide information about the circumstances in which each is prescribed, how the medications are provided, and how many patients were using the medication. If the respondent indicated that methadone and/or buprenorphine were not used, they were asked why the medications were not offered to inmates. All respondents were asked to rate the utility of both medications, and whether they referred opiate-dependent inmates to community-based ORT providers upon release.
Respondents submitted the completed survey either by fax or through an online survey service. In nine cases, surveys were administered over the telephone when respondents did not answer emails and fax requests. Data were entered into Microsoft Excel. Summary statistics and cross-tabulations were created in Microsoft Excel.
3. Results
We received a total of 51 of 52 responses; only one Midwestern state, which houses only approximately 1,400 prisoners (or less than 0.1% of all prisoners nationwide) (Sabol and Couture, 2008), declined to complete the survey. Table 1 and Figure 1 highlight regional and aggregate findings regarding methadone and buprenorphine prescribing and referral practices in state prisons nationwide. Although methadone is offered more frequently than buprenorphine, only 55% of prison systems (including state and federal systems) offer methadone under any circumstances. Methadone use varies widely across states: some states report treating more than 500 patients with methadone, but over 50% who offer methadone do so exclusively for pregnant women, acute opiate withdrawal, or for chronic pain management. By summing the reported number of prisoners receiving methadone in all states and federal jurisdictions responding to our survey, we estimate that between 1,614 and 1,817 prisoners receive methadone in state and federal correction systems nationwide. (We note, however, that two states responded “do not know” in response to the question about approximately how many prisoners receive MMT in their systems). Similarly, 45% of facilities provided some community linkage to methadone treatment post-release.
Table 1.
Availability of methadone and buprenorphine in state prisons and referrals for released inmates by region* (N = 51)
| Northeast N (%) |
South N (%) |
Midwest N (%) |
West N (%) |
Federal N |
Total N (%) |
|
|---|---|---|---|---|---|---|
| Any methadone is offered in state prison system | ||||||
| Yes | 6 (67) | 6 (35) | 7 (64) | 8 (62) | 1 | 28 (55) |
| No | 3 (33) | 11 (65) | 4 (36) | 5 (38) | 0 | 23 (45) |
| Any buprenorphine is offered in state prison system | ||||||
| Yes | 3 (33) | 2 (12) | 1 (9) | 1 (8) | 0 | 7 (14) |
| No | 6 (67) | 15 (88) | 10 (91) | 12 (92) | 1 | 44 (86) |
| Any referrals to community based methadone clinics offered upon release | ||||||
| Yes | 7 (78) | 7 (41) | 5 (45) | 4 (31) | 0 | 23 (45) |
| No | 2 (22) | 10 (59) | 6 (55) | 9 (69) | 1 | 28 (55) |
| Any referrals to community based buprenorphine providers offered upon release | ||||||
| Yes | 6 (67) | 4 (24) | 2 (18) | 3 (23) | 0 | 15 (29) |
| No | 3 (33) | 13 (76) | 9 (82) | 10 (77) | 1 | 36 (71) |
Geographic regions, as defined by the Centers for Disease Control and Prevention (CDC), are as follows:
Northeast: Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont
South: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, N. Carolina, Oklahoma, S. Carolina, Tennessee, Texas, Virginia, and W. Virginia
Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, Ohio, S. Dakota, Wisconsin, and N. Dakota (no response)
West: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming
Figure 1.
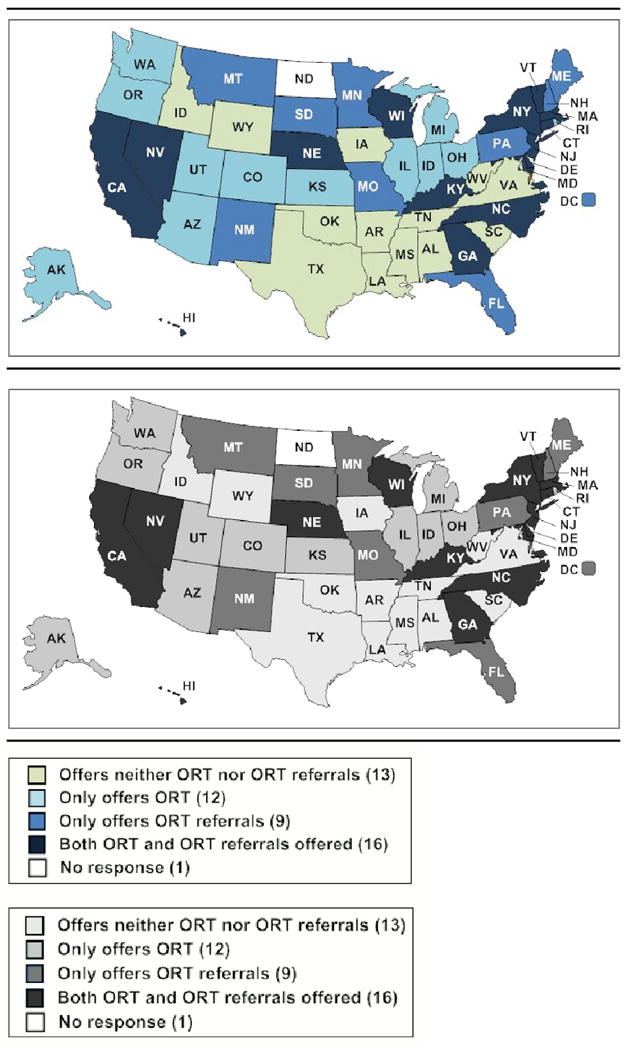
Current status of state prison systems offering opiate replacement therapy (ORT) and referrals to community-based ORT providers
Seven prison systems (14%) offer buprenorphine in some circumstances and 15 (29%) offer referrals for some inmates to community buprenorphine providers upon release. By summing the reported number of prisoners receiving buprenorphine in all states and federal jurisdictions responding to our survey, we estimate that between 57 and 150 prisoners receive buprenorphine in state and federal correction systems nationwide.
To assess regional differences in provision of ORT in prison systems and linkage to ORT post release, we stratified the data by geographic region, as defined by the Centers for Disease Control and Prevention (CDC). The proportion of facilities offering methadone to incarcerated inmates was similar across the Northeastern, Midwestern and Western regions of the US, while relatively few facilities offered methadone to inmates in the South (35%). The Northeast was the only region of the US reporting common provision of buprenorphine treatment for inmates; nearly a third of Northeastern prison systems offered this treatment option. Similarly, a much greater proportion of prison systems in the Northeast referred inmates to community-based ORT treatment upon release (78% and 67% for methadone and buprenorphine, respectively). Notably, five respondents (10%) reported that heroin use is infrequent in their state, citing low opiate addiction prevalence as the primary reason they did not offer ORT. The federal prison system offers methadone but not buprenorphine and does not provide ORT referrals upon release.
Table 2 describes reasons why ORT is not available in prison systems as well as reasons why ORT referrals are not available post-release. When asked how beneficial methadone is for treating inmates with opiate addiction, 18% of respondents responded “very beneficial;” 39% responded “somewhat beneficial,” 16% responded “not beneficial,” and 27% responded that they did not know how beneficial methadone is for treating inmates with opiate addiction. The federal prison system respondent responded that methadone is “somewhat beneficial” (data not shown). When asked how beneficial buprenorphine is for treating inmates with opiate addiction, 12% of respondents responded “very beneficial;” 29% responded “somewhat beneficial,” 10% responded “not beneficial,” and 49% responded that they did not know how beneficial buprenorphine is for treating inmates with opiate addiction. The federal prison system respondent responded that buprenorphine was somewhat beneficial.
Table 2.
Reasons why methadone or buprenorphine and ORT referrals not provided in US state and federal prisons (N=51)
| N (%)* | |
|---|---|
| Reason for not offering methadone in prison | |
| Methadone is not beneficial to inmates | 2 (9) |
| Facility offers buprenorphine instead | 0 (0) |
| Facility favors drug-free detox over methadone | 13 (57) |
| Cost is prohibitive | 0 (0) |
| Security concerns | 5 (22) |
| Administrative opposition | 5 (22) |
| Lack of health care providers | 1 (4) |
| Opiate addiction is an uncommon problem | 2 (9) |
| Administrative burdens of implementing methadone | 3 (13) |
| Don't know/unsure | 2 (9) |
| Other | 1 (4) |
| Reason for not offering buprenorphine in prison | |
| Buprenorphine is not beneficial to inmates | 0 (0) |
| Facility offers methadone instead | 9 (20) |
| Facility favors drug-free detox over buprenorphine | 17 (39) |
| Cost is prohibitive | 8 (18) |
| Security concerns | 9 (20) |
| Administrative opposition | 2 (5) |
| Lack of health care providers | 4 (9) |
| Opiate addiction is an uncommon problem | 3 (7) |
| Decisions are made on a case by case basis | 3 (7) |
| Don't know/unsure | 2 (5) |
| Other | 2 (5) |
| Reason referrals to community-based methadone clinics are not offered | |
| Administrative opposition | 1 (4) |
| Facility prefers drug free detox over methadone | 14 (50) |
| Limited partnerships with community providers | 7 (25) |
| Cost is prohibitive for inmates upon release | 3 (11) |
| Facility focuses on inmate health during incarceration | 7 (25) |
| Human resource limitations | 1 (4) |
| Director feels that opiate dependence is uncommon in state | 2 (7) |
| Don't know / unsure | 3 (11) |
| Reason referrals to community-based buprenorphine providers are not offered | |
| Administrative opposition | 3 (8) |
| Facility prefers drug free detox over methadone | 13 (36) |
| Limited partnerships with community providers | 12 (33) |
| Cost is prohibitive for inmates upon release | 3 (8) |
| Facility focuses on inmate health during incarceration | 8 (22) |
| Human resource limitations | 1 (3) |
| Director feels that opiate dependence is uncommon in state | 4 (11) |
| Don't know / unsure | 5 (14) |
| Missing | 2 (6) |
Percentages do not sum to 100% because response categories are not mutually exclusive
We asked respondents who did not offer ORT during incarceration or upon release why their facilities did not offer ORT and ORT referrals. The most common reason why facilities did not offer ORT to inmates was that they favored drug-free detoxification over ORT (57% and 39% for methadone and buprenorphine, respectively). Interestingly, 22% of prison facilities cited security concerns about providing methadone to inmates; 20% of facilities cited security concerns about providing buprenorphine. An additional barrier to both provision of ORT to inmates and linkage to ORT post-release was lack of partnerships with community ORT providers (Table 2). Many providers also indicated that their focus on inmate health during incarceration rather than upon release as another reason for not linking inmates to ORT post-release (25% of respondents indicated this for methadone referrals and 22% for buprenorphine referrals). The federal responses were very similar: neither methadone nor buprenorphine referrals were offered because “prisoners are detoxified prior to release.”
In addition to the structured survey questions, we provided an opportunity for respondents to comment about ORT in the correctional setting. Many comments reflected respondents' opposition to pharmacological management of opiate dependence. For example, one respondent remarked that:
We don't have ORT programs and inmates are detoxed when they leave. I can't think of a better time to get your life straight than when you have nothing to do but sit and think. We do not support long-term maintenance programs for addicted individuals.
Similarly, with regard to linkage to ORT upon release, one respondent stated that:
Inmates are off drugs while in prison, so there's no reason for them to be referred; they wouldn't fit the criteria for referral. They don't need detox because they've been rehabilitated while in prison. It is assumed that they are no longer [drug] users.
Another respondent commented that “facilitating addiction seems inconsistent with the mission of incarceration.” A fourth respondent indicated that ORT is not appropriate for inmates by stating that: “ORT certainly has a use, but is not appropriate or desirable in many patients, especially prisoners.”
Several respondents in favor of expanding access to ORT cited institutional barriers beyond their control that limit its implementation. One respondent indicated that even if medical directors favor provision of ORT, they must often overcome significant administrative barriers or undertake dramatic shifts in prison policy, and remarked:
We're making a huge effort to improve discharge planning and to connect people with primary care providers. It's a huge paradigm and cultural shift.
Another respondent who favored expansion of ORT provision in his prison system responded:
DOC staff and leadership don't know how to provide ORT and don't have an appreciation of its importance, particularly in an underfunded program like ours where everything is broken…There is also a huge political challenge to overcome, a lot of work needs to be done to sensitize people about the importance of this issue.
4. Discussion
This is the first national survey to document important attitudes and practices among state and federal correctional medical directors regarding both methadone and buprenorphine prescribing policies. In spite of CDC and WHO guidelines recommending provision of ORT during incarceration and upon release, as well as several studies that demonstrate the efficacy and health and social benefits of such policies (Dolan et al., 2005; Fallon, 2001; Heimer et al., 2006; Kakko et al., 2003; Marsch, 1998; McKenzie et al., 2005; Springer and Altice, 2007), just over half of US prison systems provide any methadone. Moreover, the total number of people receiving methadone represents only a minute fraction of the estimated 9% (15,689) of federal and 13% (163,005) of state inmates who reported regularly using heroin in 2004 (Mumola and Karberg, 2006). Our results also support a 2006 Department of Justice report that found that less than 0.5% of state and federal prisoners received drug maintenance therapy (Mumola and Karberg, 2006). Our estimates are also similar to results from our 2003 survey that finds that only 47% of US prison systems provided methadone to prisoners, most of which limited MMT provision to pregnant women (Rich et al., 2005a). However, while the 2003 survey finds that only 8% of prison systems provided MMT referrals upon release, we find that 46% of prison systems provide referrals in some circumstances. This suggests there have been considerable increases in the number of prisons providing referrals to MMT upon release since 2003. Furthermore, since buprenorphine has been approved, some prison systems (14%) provide it, and 29% of prison systems refer some released inmates to community buprenorphine providers. Our results suggest that in spite of a growing body of literature supporting the feasibility and demonstrated health and social benefits associated with ORT use, fewer than 2,000 prisoners in state and federal prisons receive ORT, and access to ORT in the correctional setting has improved only slightly since 2003.
Our open-ended responses highlight several important discoveries about ORT and referral provision in the correctional setting. First, there is still a great deal of stigma attached to ORT provision, and a general preference for abstinence-based drug treatment policies rather than pharmacological and therapeutic treatment of opiate addiction. Many respondents have misperceptions about the nature of addiction and incorrectly associate forced detoxification with curing opiate dependence. This attitude ignores important evidence about common relapse to addiction after forced detoxification. We also find that administrative barriers and personal opinions of prison medical directors often influence their facilities' ORT prescribing and referral policies in positive or negative ways. For example, one respondent commented that a former medical director was personally opposed to the use of pharmacological intervention for drug use and thus maintained abstinence-based drug treatment policies. When this medical director was replaced, the new director immediately began working to implement ORT within the state prison system. Another respondent underscored the value of buprenorphine for prisoners, commenting that his facility was launching a new buprenorphine treatment and referral program for inmates. However, we find common misperceptions about the magnitude of the opiate addiction among prisoners. For example, a medical director in one Northeastern state with very high rates of prisoners with a history of heroin use commented that opiate addiction was not a significant problem among prisoners.
Initiation of ORT for inmates while in prison has been shown to decrease high risk behavior during incarceration and upon release, including transmission of HIV and hepatitis C due to sharing needles and other drug paraphernalia (Heimer et al., 2006). When correctional-based ORT programs are successfully linked with community ORT providers, they have been shown to reduce relapse to opiate use, mortality, criminality, and recidivism (Dolan et al., 2005). Prisoners who successfully remain on ORT in the community are also more likely to sustain employment and to improve social function (Kakko et al., 2003). In spite of improvements in the number of prisons offering ORT referrals since 2003, our findings suggest that most prisons are still missing opportunities to break the cycle of incarceration and addiction by failing to link inmates with a history of opiate dependence to ORT programs upon release.
We find that many prison medical directors are not familiar with the potential medical and social benefits of providing ORT in the correctional setting, particularly buprenorphine. Additionally, a focus on inmate health exclusively during incarceration ignores the common social, public health and recidivism challenges associated with inmate relapse to substance use immediately after release. In summary, our results suggest that in spite of this evidence base, formidable political and administrative barriers to widespread ORT provision in and upon release from the US correctional system remain. Given the proven efficacy of ORT interventions in reducing health and social harms, these barriers have serious health and public policy implications.
In addition to educating and encouraging correctional administrators and policy makers to improve provision of and linkage to ORT for prisoners upon release, ORT providers could be encouraged to develop connections and working relationships with correctional systems. This might be facilitated by ORT regulators who could require or encourage such relationships. Also, given the common goals of reduced drug use, criminal behavior and recidivism, Probation and Parole Departments could also encourage ORT prior to or upon release from prison.
In spite of the remarkably high response rate to our survey, our findings are subject to a few limitations. There are approximately 114 federal prisons nationwide. Although medical and drug policies for federal prisons are centralized, there may be local differences about prescribing attitudes related to ORT that our survey did not capture. Additionally, our survey focused exclusively on prisons rather than local jails, so it may not provide a comprehensive picture of nationwide ORT prescribing and referral attitudes and practices for all correctional settings. Moreover, our survey relied on the self-report and estimates of each medical director; we were unable to independently confirm the actual numbers of people prescribed or referred to ORT in each prison participating in the survey. It is therefore difficult to extrapolate the exact numbers of inmates receiving ORT from our findings. Finally, while we document an increase in the number of prison systems reporting referrals to ORT upon release, because our survey did not include a question about how many prisoners are referred to ORT upon release, we are unable to estimate the impact of this increase on the number of prisoners receiving ORT in the community. This could be a potential avenue of new research, as could exploration of prisoner opinions about ORT in prison and upon release. Additionally, given the important role of parole officers in helping inmates transition to the community, new research might explore probation officers' attitudes about and roles in promoting access to ORT.
Our results related to ORT policies may partially reflect regional drug use trends in the United States. Opiate use is twice or three times as common in the Northeastern United States than elsewhere (SAMHSA, 2007). Several medical directors commented that heroin addiction was not a common problem among inmates, citing other local drug epidemics such as cocaine and crystal methamphetamine use. In these cases, lack of ORT programs may be partially attributable to each state's drug epidemics rather than lack of prison commitments to ORT; future research should focus on these regional phenomena.
5. Conclusion
Our survey suggests that prison systems nationwide have made some progress in providing ORT to prisoners: a few prisons now provide buprenorphine to prisoners, and the number of facilities providing referrals to ORT upon release has increased since 2003. Overall, however, pharmacological treatment of opiate dependence is still an important but under- utilized intervention in US prison settings; the number of prisoners with opiate dependence who receive ORT during incarceration remains quite limited. In spite of the demonstrated medical, social and economic benefits of providing opiate dependent inmates with ORT (particularly upon return to the community), federal and state prisons in the US often do not provide ORT to inmates during incarceration or refer them to community ORT programs upon release. This is a missed public health opportunity; greater national leadership is needed to change criminal justice policies that deny addiction treatment services to prisoners. Political and administrative opposition to pharmacological treatment of opiate dependence also suggests that educating prison staff and policymakers about the medical and social benefits of ORT for treatment of opiate dependence, as well as exploring other ways to encourage greater ORT in the correctional setting, should be important public health priorities.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Auriacombe M, Fatseas M, Dubernet J, Daulouede JP, Tignol J. French field experience with buprenorphine. Am J Addict. 2004;12 1:S17–28. doi: 10.1080/10550490490440780. [DOI] [PubMed] [Google Scholar]
- Auriacombe M, Franques P, Tignol J. Deaths attributable to methadone vs buprenorphine in France. JAMA. 2001;285:45. doi: 10.1001/jama.285.1.45. [DOI] [PubMed] [Google Scholar]
- Bick J. HIV and Viral Hepatitis in Corrections: A Public Health Opportunity. In: Greifinger R, editor. Public Health Behind Bars. Springer International; New York: 2007. [Google Scholar]
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, Koepsell TD. Release from prison--a high risk of death for former inmates. N Engl J Med. 2007;356:157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird SM, Hutchinson SJ. Male drugs-related deaths in the fortnight after release from prison: Scotland, 1996-99. Addiction. 2003;98:185–190. doi: 10.1046/j.1360-0443.2003.00264.x. [DOI] [PubMed] [Google Scholar]
- Carrieri MP, Amass L, Lucas GM, Vlahov D, Wodak A, Woody GE. Buprenorphine use: the international experience. Clin Infect Dis. 2006;43 4:S197–215. doi: 10.1086/508184. [DOI] [PubMed] [Google Scholar]
- CDC. Substance abuse treatment for injecting drug users: a strategy with many benefits. Centers for Disease Control and Prevention; Atlanta: 2002. [Google Scholar]
- CEC. Report from the Commission to the European Parliament and the Council on the implemenation of the Council Recommendation of 18 June 2003 on the prevention and reduction of health-related harm associated with drug dependence. Commission of the European Communities; 2007. [Google Scholar]
- Clarke JG, Stein MD, Hanna L, Sobota M, Rich JD. Active and Former Injection Drug Users Report of HIV Risk Behaviors During Periods of Incarceration. Subst Abus. 2001;22:209–216. doi: 10.1080/08897070109511463. [DOI] [PubMed] [Google Scholar]
- Comer SD, Collins ED. Self-administration of intravenous buprenorphine and the buprenorphine/naloxone combination by recently detoxified heroin abusers. J Pharmacol Exp Ther. 2002;303:695–703. doi: 10.1124/jpet.102.038141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan KA, Shearer J, White B, Zhou J, Kaldor J, Wodak AD. Four-year follow-up of imprisoned male heroin users and methadone treatment: mortality, re-incarceration and hepatitis C infection. Addiction. 2005;100:820–828. doi: 10.1111/j.1360-0443.2005.01050.x. [DOI] [PubMed] [Google Scholar]
- Dole VP, Robinson JW, Orraca J, Towns E, Searcy P, Caine E. Methadone treatment of randomly selected criminal addicts. N Engl J Med. 1969;280:1372–1375. doi: 10.1056/NEJM196906192802502. [DOI] [PubMed] [Google Scholar]
- Drucker E. Drug prohibition and public health: 25 years of evidence. Public Health Rep. 1999;114:14–29. doi: 10.1093/phr/114.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallon BM. The Key Extended Entry Program (KEEP): from the community side of the bridge. Mt Sinai J Med. 2001;68:21–27. [PubMed] [Google Scholar]
- Fhima A, Henrion R, Lowenstein W, Charpak Y. Two-year follow-up of an opioid-user cohort treated with high-dose buprenorphine (Subutex) Ann Med Interne (Paris) 2001;152 3:IS26–36. [PubMed] [Google Scholar]
- Fiellin DA, O'Connor PG. Clinical practice. Office-based treatment of opioid-dependent patients. N Engl J Med. 2002;347:817–823. doi: 10.1056/NEJMcp013579. [DOI] [PubMed] [Google Scholar]
- Freudenberg N. Jails, prisons, and the health of urban populations: a review of the impact of the correctional system on community health. J Urban Health. 2001;78:214–235. doi: 10.1093/jurban/78.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerra G, Ferri M, Polidori E, Santoro G, Zaimovic A, Sternieri E. Long-term methadone maintenance effectiveness: psychosocial and pharmacological variables. J Subst Abuse Treat. 2003;25:1–8. doi: 10.1016/s0740-5472(03)00031-x. [DOI] [PubMed] [Google Scholar]
- Gordon MS, Kinlock TW, Schwartz RP, O'Grady KE. A randomized clinical trial of methadone maintenance for prisoners: findings at 6 months post-release. Addiction. 2008;103:1333–1342. doi: 10.1111/j.1360-0443.2008.002238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gore SM, Bird AG, Burns SM, Goldberg DJ, Ross AJ, Macgregor J. Drug injection and HIV prevalence in inmates of Glenochil prison. BMJ. 1995;310:293–296. doi: 10.1136/bmj.310.6975.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greifinger R. Thirty Years Since Estelle v. Gamble. In: Greifinger R, editor. Public Health Behind Bars: from Prisons to Communities. Springer International; New York: 2007. [Google Scholar]
- Hammett TM. HIV/AIDS and other infectious diseases among correctional inmates: transmission, burden, and an appropriate response. Am J Public Health. 2006;96:974–978. doi: 10.2105/AJPH.2005.066993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanlon TE, Nurco DN, Kinlock TW, Duszynski KR. Trends in criminal activity and drug use over an addiction career. Am J Drug Alcohol Abuse. 1990;16:223–238. doi: 10.3109/00952999009001585. [DOI] [PubMed] [Google Scholar]
- Heimer R, Catania H, Newman RG, Zambrano J, Brunet A, Ortiz AM. Methadone maintenance in prison: evaluation of a pilot program in Puerto Rico. Drug Alcohol Depend. 2006;83:122–129. doi: 10.1016/j.drugalcdep.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Inciardi JA, Needle RH. Editors' introduction: HIV/AIDS interventions for out-of-treatment drug users. J Psychoactive Drugs. 1998;30:225–229. doi: 10.1080/02791072.1998.10399696. [DOI] [PubMed] [Google Scholar]
- Kakko J, Svanborg KD, Kreek MJ, Heilig M. 1-year retention and social function after buprenorphine-assisted relapse prevention treatment for heroin dependence in Sweden: a randomised, placebo-controlled trial. Lancet. 2003;361:662–668. doi: 10.1016/S0140-6736(03)12600-1. [DOI] [PubMed] [Google Scholar]
- Kang SY, Deren S, Andia J, Colon HM, Robles R, Oliver-Velez D. HIV transmission behaviors in jail/prison among puerto rican drug injectors in New York and Puerto Rico. AIDS Behav. 2005;9:377–386. doi: 10.1007/s10461-005-9011-4. [DOI] [PubMed] [Google Scholar]
- Kinlock TW, Battjes RJ, Schwartz RP. A novel opioid maintenance program for prisoners: preliminary findings. J Subst Abuse Treat. 2002;22:141–147. doi: 10.1016/s0740-5472(02)00226-x. [DOI] [PubMed] [Google Scholar]
- Kinlock TW, Gordon MS, Schwartz RP, O'Grady K. A Study of Methadone Maintenance for Male Prisoners: 3 Month Post-Release Outcomes. Criminal Justice and Behavior. 2008a;35:34–47. doi: 10.1177/0093854807309111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinlock TW, Gordon MS, Schwartz RP, O'Grady KE. A Study of Methadone Maintenance For Male Prisoners: 3-Month Postrelease Outcomes. Crim Justice Behav. 2008b;35:34–47. doi: 10.1177/0093854807309111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs CP, Simmons M. Intraprison HIV transmission: an assessment of whether it occurs, how it occurs, and who is at risk. AIDS Educ Prev. 2002;14:53–64. doi: 10.1521/aeap.14.7.53.23865. [DOI] [PubMed] [Google Scholar]
- Kreek MJ. Rationale for maintenance pharmacotherapy of opiate dependence. Res Publ Assoc Res Nerv Ment Dis. 1992;70:205–230. [PubMed] [Google Scholar]
- Kreek MJ. Methadone-related opioid agonist pharmacotherapy for heroin addiction. History, recent molecular and neurochemical research and future in mainstream medicine. Ann N Y Acad Sci. 2000;909:186–216. doi: 10.1111/j.1749-6632.2000.tb06683.x. [DOI] [PubMed] [Google Scholar]
- Krinsky CS, Lathrop SL, Brown P, Nolte KB. Drugs, detention, and death: a study of the mortality of recently released prisoners. Am J Forensic Med Pathol. 2009;30:6–9. doi: 10.1097/PAF.0b013e3181873784. [DOI] [PubMed] [Google Scholar]
- Lipton DS. Correctional Drug Abuse Treatment in the United States: An Overview. In: Leukefeld CG, Tims FM, editors. Drug Abuse Treatment in Prisons and Jails. National Institute on Drug Abuse Research Monograph Series; Washington, D.C.: 1992. [Google Scholar]
- Marsch L. The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: a meta-analysis. Addiction. 1998;93:515–532. doi: 10.1046/j.1360-0443.1998.9345157.x. [DOI] [PubMed] [Google Scholar]
- Martin S. Three Year Outcomes of therapeutic community treatment for drug-involved offenders in Delaware: From prison to work release to aftercare. The Prison Journal. 1999;79 [Google Scholar]
- McKenzie M, Macalino G, McClung C, Shield DC, Rich JD. Opiate replacement therapy at time of release from incarceration: Project MOD, a pilot program. J Opioid Manag. 2005;1:147–151. doi: 10.5055/jom.2005.0034. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Arndt IO, Metzger DS, Woody GE, O'Brien CP. The effects of psychosocial services in substance abuse treatment. JAMA. 1993;269:1953–1959. [PubMed] [Google Scholar]
- Møller L, Stöver H, Jürgens R, Gatherer A, Nikogosian H. Health in prisons: A WHO guide to the essentials in prison health. World Health Organization; Geneva: 2007. [Google Scholar]
- Mumola C, Karberg J. Drug Use and Dependence, State and Federal Prisoners. U.S. Department of Justice, Office of Justice Programs; Washington DC: 2006. [Google Scholar]
- Nurco DN, Hanlon TE, Kinlock TW. Recent research on the relationship between illicit drug use and crime. Behavioral Sciences and the Law. 1991;9:221–242. [Google Scholar]
- Rich JD, Boutwell AE, Shield DC, Key RG, McKenzie M, Clarke JG, Friedmann PD. Attitudes and practices regarding the use of methadone in US state and federal prisons. J Urban Health. 2005a;82:411–419. doi: 10.1093/jurban/jti072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich JD, McKenzie M, Shield DC, Wolf FA, Key RG, Poshkus M, Clarke J. Linkage with methadone treatment upon release from incarceration: a promising opportunity. J Addict Dis. 2005b;24:49–59. doi: 10.1300/J069v24n03_04. [DOI] [PubMed] [Google Scholar]
- Sabol W, Couture H. Prison Inmates at Midyear 2007. US Department of Justice; 2008. [Google Scholar]
- SAMHSA. National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration, Office of Applied Studies; Washington DC: 2007. [Google Scholar]
- Seal DW, Margolis AD, Morrow KM, Belcher L, Sosman J, Askew J. Substance use and sexual behavior during incarceration among 18- to 29-year old men: prevalence and correlates. AIDS Behav. 2008;12:27–40. doi: 10.1007/s10461-007-9217-8. [DOI] [PubMed] [Google Scholar]
- Springer S, Altice F. Improving the Care for HIV-Infected Prisoners Public Health Behind Bars. Springer; New York: 2007. pp. 535–555. [Google Scholar]
- Visher C, Mallik-Cane K. Reentry experiences of men with health problems. In: Greifinger R, editor. Public Health Behind Bars. Springer International; New Yorker: 2007. [Google Scholar]
- Walmsley R. World Prison Population List. Kings College of London International Centre for Prison Studies; London: 2008. [Google Scholar]
- WHO. WHO Status Paper on Prisons, Drugs and Harm Reduction. 2005 [PubMed] [Google Scholar]
- WHO. Interventions to Address HIV in Prison: Drug Dependence Treatment. World Health Organization; Geneva: 2007. [Google Scholar]


