Abstract
The implementation of cigarette smoking abstinence reinforcement programs may be hindered by the time intensive burden placed on patients and treatment providers. The use of remote monitoring and reinforcement of smoking abstinence may enhance the accessibility and acceptability of this intervention, particularly in rural areas where transportation can be unreliable and treatment providers distant. This study determined the effectiveness of an Internet-based abstinence reinforcement intervention in initiating and maintaining smoking abstinence in rural smokers. Sixty-eight smokers were enrolled to evaluate the efficacy of an Internet-based smoking cessation program. During the 6-week intervention period, all participants were asked to record 2 videos of breath carbon monoxide (CO) samples daily. Participants also typed the value of their CO readings into web-based software that provided feedback and reinforcement based on their smoking status. Participants (n=35) in the Abstinence Contingent (AC) group received monetary incentives contingent on recent smoking abstinence (i.e., CO of 4 parts per million or below). Participants (n=33) in the Yoked Control (YC) group received monetary incentives independent of smoking status. Participants in the AC group were significantly more likely than the YC group to post negative CO samples on the study website (OR = 4.56; 95% CI = 2.18–9.52). Participants assigned to AC were also significantly more likely to achieve some level of continuous abstinence over the 6-week intervention compared to those assigned to YC. These results demonstrate the feasibility and short-term efficacy of delivering reinforcement for smoking abstinence over the Internet to rural populations.
Keywords: Abstinence Reinforcement, Smoking Cessation, Rural, Randomized Controlled Trial, Tobacco, Cigarettes
1
Tobacco use and smoking-related disease is a top public health problem in the United States. In 2007, an estimated 60.1 million adults (24.2% of the population) in the United States were current (i.e., using within the past month) cigarette smokers (Substance Abuse and Mental Health Administration [SAMHSA], 2008). Cigarette smoking is more prevalent in rural areas than in non-rural areas and actually increased in prevalence in completely rural areas from 23.3% in 2005 to 30.1% in 2006 (SAMHSA, 2007).
Rural residents are considered a “special population” due to their lack of economic, health and educational resources (U.S. Congress, Office of Technology Assessment, 1990). Fifty one percent of the world’s population lives in a rural area, with 21% of United States residents living in rural locations (United Nations, 2006; U.S. Bureau of the Census, 2000). Compared with their urban counterparts, rural resident frequently encounter conditions that challenge their health and well-being (Eberhardt and Pamuk, 2004). Systemic factors such as lack of public transportation, lower levels of services and a shortage of health care providers contribute to sub-optimal health among rural Americans (Friedell et al., 2001). Appalachia, where this project was conducted, is a largely rural, mountainous region in the Eastern United States. This region is well known for its natural resources (e.g., coal, forests) and community strengths including a tradition of supportive social ties, community engagement and resilience in the face of scarcity and challenge (see also Williams, 2001). As with other rural areas, Appalachian residents lack access to health care providers in general and in particular to those who provide psychiatric or substance abuse services (Stensland et al., 2002). Given the global percentage of rural residents and the documented health disparities, addressing issues specific to rural communities could have a substantial impact on public health.
Compounding and contributing to these challenges, Appalachian regions of the United States experience high rates of smoking and smoking related disease (Behavioral Risk Factor Surveillance System [BRFSS], 2008). In 2007, rates of smoking in rural Appalachian regions were as high as 34.4%; by comparison, the overall prevalence was 28.2% and 19.8% for Kentucky and the U.S., respectively (BRFSS, 2008). Kentucky had the highest prevalence of current adult smokers in 2007 in the United States (BRFSS, 2008). Smoking rates in Appalachian Kentucky exceed state levels and are nearly double the national rate. As a likely consequence of the high rates of smoking and limited access to health care, Appalachia experiences some of the highest incidence of smoking-related mortality and disease. For example, Appalachia has higher cancer incidence rates than the United States average and the prevalence of cardiovascular disease exceeds that observed in most Western nations (Rugg et al, 2008; Wingo et al., 2008). Smoking cessation interventions to treat current smokers and smoking prevention efforts to prohibit smoking initiation are clearly needed and could reduce smoking-related illness and mortality both locally and globally. While the present study focuses on Appalachia, the results described here can inform interventions in rural communities throughout the United States and internationally (e.g., SAMHSA, 2007; Yang et al., 2008).
A variety of treatment options are available for smoking cessation, including medication, supportive counseling and behavioral interventions (Stitzer, 1999). While these interventions have proven effective, it has been suggested that the field is in need of more innovative and intensive approaches for smoking cessation in order to increase current quit rates, particularly in locations where treatment options are limited as is the case for rural areas.
Recent advances have been made with the use of intensive abstinence reinforcement therapies, also known as contingency management, in initiating and promoting smoking cessation in high risk individuals, including pregnant smokers, adolescent smokers, college students and smokers with substance abuse disorders (Correia et al., 2006; Donnatelle et al., 2000; Higgins et al., 2004; Lamb et al., 2004; Roll et al., 2005; Wiseman et al., 2005). Using this approach, smokers receive reinforcement (usually vouchers or money) contingent upon documented smoking abstinence. These interventions are considered highly intensive because they require regular and frequent monitoring of smoking status, such as daily carbon monoxide (CO) monitoring via breath sample collection or cotinine monitoring via urinalysis or saliva testing.
While individuals enrolled in abstinence reinforcement interventions have shown rates of prolonged drug abstinence during the intervention (e.g., in studies of cocaine dependent individuals, nearly 50% achieve a significant period of sustained abstinence; reviewed in Higgins et al., 2002), the nature of these interventions may also be a limitation. Previously, abstinence reinforcement interventions using vouchers or other reinforcers for smoking cessation have required that participants provide at least one and preferably two breath samples per day, in person, during the entire intervention period (Higgins et al., 2004; Javors et al., 2005; Lamb et al., 2005). While this level of frequency and intensity may be important for the effectiveness of the intervention, it may also be too burdensome for some smokers in need of such interventions, especially for smokers living in rural regions where lack of resources, including access to preventive services and transportation, can be a major obstacle to receiving needed health services (Nemet and Bailey, 2000). Traditional (i.e., face to face) smoking cessation interventions may also be too time consuming for overburdened health care providers, especially in areas where there is a shortage of these providers (Gamm, 2004).
An innovative, novel and effective voucher-based abstinence reinforcement therapy for smoking has recently been developed wherein smokers are regularly monitored and their abstinence reinforced via the Internet (Dallery and Glenn, 2005; Dallery et al., 2007; Glenn and Dallery, 2007; Reynolds et al., 2008). The purpose of this study was to implement and evaluate an Internet-based abstinence reinforcement intervention for smokers in rural Appalachian communities in Kentucky. To this end, sixty-eight smokers living in Appalachian Kentucky were enrolled and randomly assigned into one of two groups: an abstinence contingent group (AC) that received monetary reinforcement for breath CO samples indicating smoking abstinence and a yoked control group (YC) that received monetary reinforcement independent of breath CO levels. The groups engaged in a 6-week intervention and follow-up assessments were completed at 2, 4, 6 and 12 weeks following enrollment into the intervention.
2. Method
2.1 Participants
Sixty-eight smokers, ages 18 and older, were randomly assigned to either the AC or YC group (described below). An additional 16 smokers were screened but were not enrolled either because they did not meet criteria or decided they did not want to take part in the intervention. Subjects were recruited by advertisement in local media and by word of mouth. Table 1 displays demographic characteristics for the two groups. To be considered eligible, participants had to report smoking 10 or more cigarettes a day, have a CO reading of 8 parts per million or greater at screening, report residence in one of the 54 Appalachian counties in Kentucky and own a home computer with access to the Internet. Appalachian Kentucky is a largely rural area, with population rates generally ranging from 6–199 people per square mile (www.arc.gov, 2003). Participants were drawn from highly rural areas as well as the relatively more densely populated cities and towns of Appalachian Kentucky surrounding Hazard, KY, which served as the home base for this project. Participants reporting smoking marijuana more than twice per month or having current or past medical or psychiatric illness that would interfere with study participation were excluded. The University of Kentucky Medical Institutional Review Board reviewed and approved the conduct of this protocol and all participants had to provide written, informed consent prior to engaging in any study activities.
Table 1.
Group Demographics.
| Variable | AC Group | YC Group |
|---|---|---|
| Number/Group | 35 | 33 |
| Mean Age (Range) | 38 (21–58) | 40 (18–61) |
| Sex | 26 Female, 9 Male | 25 Female, 8 Male |
| Self-Identified Race | 33 White, 2 Black | 31 White, 2 Biracial |
| % Currently Married | 54 | 64 |
| % Reporting Employment Outside the Home | 71 | 42 |
| % Graduated High School or Having GED | 94 | 88 |
| % Reporting Household Income > $21,000/year | 60 | 48 |
| Mean Number of Cigarettes Smoked Per Day at Intake (Range) | 30 (12–60) | 30 (13–60) |
| Mean CO at Intake | 26.4 (10–59) | 23.9 (8–60) |
| Mean Years Smoking at Intake (Range) | 21 (5–43) | 22 (4–41) |
| Mean Fagerstrom at Intake (Range) | 5 (3–8) | 5 (2–8) |
Abbreviations: AC:Abstinence Contingent;YC: Yoked Control;GED: General Equivalency Degree
Participants that appeared to meet inclusion criteria based on a phone interview were scheduled to complete an intake assessment. Participants completed the intake assessment and if they met all inclusion criteria and no exclusion criteria, they were offered enrollment in the study and were randomly assigned to either the AC or YC group. They then participated in a 6-week intervention and evaluation period. Assessments of CO and saliva cotinine were conducted at the end of weeks 2, 4 (for all participants except the first two assigned to the AC group) and 6 of the 6-week intervention period and at 12 weeks from the start of the 6-week intervention period.
2.2 Experimental Design
The study utilized a randomized, controlled, parallel group design.
2.3 Random assignment
A modified dynamic balanced randomization (Signorini et al., 1993) was used to assign participants sequentially to the two treatment conditions, with the exception that the first 5 participants enrolled were assigned to the AC group to ensure that a sufficient number of participants was available to match in the YC group. Since amount of baseline drug use has been inversely associated with responsiveness to voucher-based abstinence reinforcement (Silverman et al., 1996; 1998), we stratified on the number of cigarettes smoked per day (>20 cigarettes per day, yes/no). Participants were also stratified based on sex (male/female) and age (≥50 years old, yes/no). All participants who were randomly assigned and recorded at least one video on the study website were included in the “intent to treat” sample analyses.
2.4 General procedure
The Internet-based monitoring system involved user-friendly Internet technology to verify breath CO measurements. This system consisted of a study website housed on a secure server at the University of Kentucky, the participant’s personal computer and a CO monitor and web camera provided to participants. The study website allowed participants to record CO breath samples, receive immediate feedback about reinforcement for abstinence and track progress both in terms of study earnings and meeting the target behavior, abstinence from smoking. Following random assignment into a group, research staff arranged a date and time with research participants to set up the Internet-based monitoring system and provide extensive training in study procedures, generally in the participant’s home. During this visit, study staff provided participants with their study user name and password. Participants then logged on to the study website with this information and recorded their training videos (see below). All research participants were informed that the 6-week intervention period began the day immediately following protocol training, which also served as their quit day.
During training, participants were required to send three consecutive video clips recorded using a web cam that captured each of the following components: 1) the CO monitor showing that it was calibrated to zero, 2) the participant holding his/her breath while the monitor counted down, 3) the participant blowing into the CO monitor and 4) the final CO reading. These components were observed seamlessly in real-time within a single video clip. The average of the three training CO samples collected during this procedure served as each participant’s baseline CO level prior to the start of the 6-week intervention period.
During the 6-week intervention period, all participants were asked to send 2 video clips per 24-hour period from 5:00 a.m. to 4:00 a.m. the next day, separated by at least 8 hours, because of the half-life of breath CO (Crowley et al., 1991; Middleton and Morice, 2000). This video clip was recorded when subjects logged onto the secure website, programmed using Java, and enabled the video recording software embedded in the website (Motiv8, Red5 Systems, http://www.red5systems.com, New York, NY). When participants submitted each video clip, they also entered their CO level reading from that video using a standard keypad. Research staff then viewed the video clips to verify CO level entry. Feedback, and reinforcement if applicable, were given immediately on the participant’s web page of the study website.
2.5 Study web site
Participants logged on to a secured website in order to provide CO samples and receive reinforcement. Daily results, a cumulative graph of CO results and the amount of money earned for CO samples demonstrating recent abstinence and overall participation was displayed on each participant’s home page. Participants were able to request payments of accumulated earnings whenever they wished. Participants were paid with a check at the time of their request, which usually occurred at scheduled study assessments or after study completion. Although there was usually a delay between earning money for smoking abstinence (i.e., up to 12 weeks if a participant decided to wait to receive all accumulated earnings), all participants understood that they could request and receive payment at any time and none complained about the delay between earning and provision of reinforcers.
2.6 CO Measurement
The piCO Smokerlyzer is a hand-held, lightweight, battery powered breath CO monitor (Bedfont Inc. Medford, NJ). The measurement procedure required participants to hold their breath for approximately 15 seconds as the monitor counted down and then exhale into the mouthpiece. The monitor measures breath CO in parts per million based on the conversion of CO to a catalytically active electrode. A LED readout provided feedback regarding breath CO levels, which were then entered by the participant directly into the secured website.
2.7 Abstinence Contingent Reinforcement Group
Participants in the AC group were instructed that they would be required to provide breath samples that indicated recent smoking abstinence (i.e., CO ≤ 4, except in the Target reduction period described below) in order to receive monetary reinforcement. Missed samples were always counted as positive.
2.7.1 Target reduction period
During week 1 of the intervention period, a participant was considered to have met the target for reductions in smoking if his or her breath CO concentration decreased by ≥ 15% from the last sample provided, until it was 4 parts per million or below. In order for participants to earn their first voucher demonstrating smoking reduction and receive reinforcement, participants were required to provide a CO sample that was ≥ 15% of the average of the 3 CO samples taken during the initial set-up. Thus, participants could receive reinforcement with a CO value greater than 4 parts per million during this period, as long as it was reduced by at least 15% from the previous sample and the participant had not already provided a CO that was 4 parts per million or below. A target reduction period has been implemented in previous research using the Internet to reinforce smoking cessation as a means of shaping the target behavior (Dallery et al., 2007).
2.7.2 Abstinence induction period
During weeks 2–5, participants were considered abstinent from smoking and received reinforcement if they provided a breath sample that had a CO level of ≤ 4 parts per million.
2.7.3 Escalating pay schedule with reset contingency
During weeks 1–5, when participants provided a CO sample that met the target reduction or recent smoking abstinence requirement, they earned a monetary voucher on an escalating pay schedule for sustained abstinence. Under this schedule, the first breath sample that met the criterion of recent abstinence earned a voucher with an initial value of $1.00. Vouchers then increased in value by $0.25 for each consecutive breath sample that met the abstinence criterion. Participants also earned a $5.00 bonus for every 6 consecutive breath samples that met the abstinence criterion. Participants could earn a maximum of approximately $800 during study participation.
If a breath sample did not meet the abstinence criterion, then the participant did not receive reinforcement and the value of the next voucher was reset to $1.00. However, if, after a reset, the participant provided three consecutive samples that met the criterion for recent abstinence, then the voucher returned to the value at which the reset occurred.
2.7.4 Thinning period
During week 6 of the intervention condition, participants earned a $5 voucher for every 2 consecutive negative samples (CO ≤ 4 parts per million). If a sample tested positive (CO > 4), the participant did not earn a voucher for that sample. A reset in the voucher value was not implemented during this phase. A thinning period has been implemented in previous, similar research as a means of gradually reducing reinforcement of the target behavior (Dallery et al., 2007).
2.8 Yoked Control Group
The conditions, length and schedule of the intervention were identical to that described above except reinforcement was NOT contingent upon providing CO samples demonstrating recent abstinence. Each participant in the YC group was “yoked,” or matched, to a participant in the contingent reinforcement group and was reinforced on a schedule identical to that of their “yoked” partner when they posted videos at time points corresponding to those of that partner. Individuals in the YC group were instructed to set a quit date and that they would receive a congratulatory message for meeting target CO levels as described above. They were also instructed that monetary reinforcement would be randomly presented when they uploaded a video.
Yoking of participants was based on the stratification variables mentioned above. That is, individuals were generally matched on 2 of the 3 following variables: number of cigarettes smoked per day, sex and age. For example, two females who smoked more than 20 cigarettes per day could be “yoked” together. Participants in the YC group received reinforcement of comparable value and frequency as participants in the AC group but independent of their CO results. For example, if a subject in the AC condition received reinforcement for the first scheduled sample in the intervention ($1.00), the subject in the YC group “yoked” to that individual would also receive $1.00 if he or she posted a video for the first scheduled sample, regardless of the CO level.
2.9 Outcome Measures
The primary outcome for this study was CO level recorded on the website during the active intervention. Secondary outcomes to confirm the data gathered from the website obtained during scheduled assessments included: on site CO levels and semi-quantitative saliva cotinine levels (NicAlert, Nymox Pharmaceutical Corporation, Hasbrouck Heights, NJ). Study staff conducted scheduled assessments in our project offices, participants’ homes or intermediate locations (e.g., libraries or community centers). Other measures (e.g., Beck Depression Inventory, Questionnaire of Smoking Urges, Minnesota Nicotine Withdrawal Scale) were completed during these assessments but those outcomes will not be reported here. The primary outcomes were coded as positive (i.e., missing samples or CO levels < 15% below the last sample in week 1 or > 4 parts per million for the remainder of the trial; cotinine saliva results > 0 [greater than 10 ng/ml]) or negative (i.e., CO levels ≥ 15% reduction from last sample in week 1 or ≤ 4 for the remainder of the trial; cotinine saliva results = 0 [10 ng/ml or less]).
The primary outcomes described above were used to develop two measures of feasibility and five measures of smoking abstinence as a function of group. The first measure of feasibility was study retention (i.e., proportion of participants that withdrew before completing the 6-week intervention and number of days in the study). Number of days in the study was defined as the time of the last posted video of each participant. The second measure of feasibility was percentage of data collected using the website (i.e., number of videos recorded/number of videos expected).
The first measure of smoking abstinence was the proportion of CO negative (≤ 4 parts per million) breath samples collected during the twice-daily assessments throughout the 6-week intervention period (treated as a dichotomous variable, Y/N for each sample). The second smoking abstinence measure was longest duration of sustained abstinence based on the twice-daily breath samples during the 6-week intervention period (treated as a dichotomous variable, Y/N for each sample). The remaining measures of abstinence were derived from assessments at the end of weeks 2, 4 and 6 of the intervention evaluation period and 12 weeks from the start of the 6-week intervention evaluation period. These data were gathered from the scheduled assessments and were used to calculate proportions of negative samples as defined above.
2.10 Statistical Analysis
Cox survival analysis and t-tests were used to examine drop out rates as a function of group assignment. Dichotomous abstinence outcomes assessed repeatedly over the intervention periods were analyzed with an exchangeable correlation structure using General Estimating Equations (GEE) (Zeger et al., 1988). GEE is particularly suited for analyses of longitudinal data and allows for correlations among observations within an individual participant, for the presence of missing data, for participants measured at different time points and for covariates that change over time. Results are reported as odds ratios (OR), indicating the likelihood that the AC group had different outcomes from the YC group and 95% CIs surrounding the OR. If the CIs included 1.00 for a given outcome, groups were not considered significantly different from each other. Data gathered during the intervention period and assessments were analyzed with an autoregressive covariance structure using SAS Proc Mixed (Singer, 1998). Continuous abstinence data were analyzed using Chi Square analyses with Fisher’s Exact Test used to compare groups if a significant effect was observed. All outcomes were considered statistically significant for p < 0.05, except for GEE analyses as described above. All analyses were conducted using SAS 9.1 for Windows.
3. Results
3.1 Study Retention and Data Collection Rates
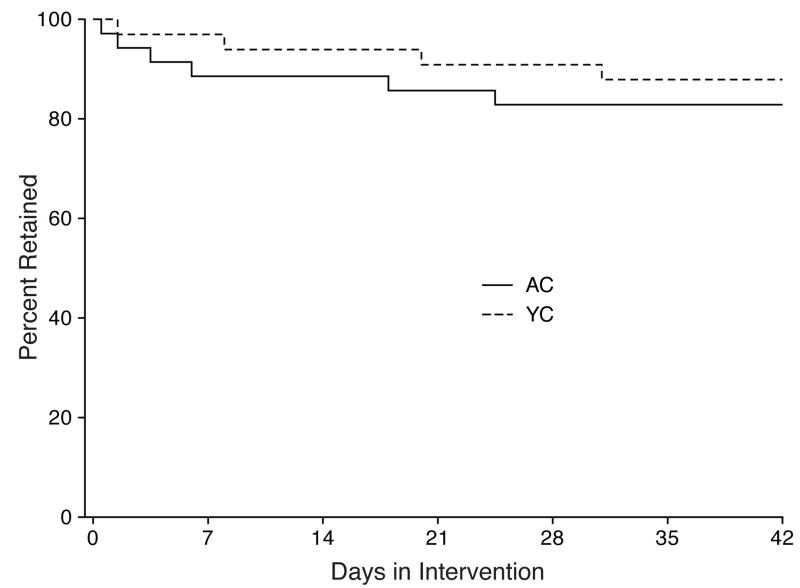
Cox survival analysis failed to detect a difference in terms of study retention across groups (Hazard Ratio = 1.49, p=0.54). A total of 10 participants withdrew during participation, 6 from the AC group and 4 from the YC group. Figure 1 shows the retention curves for both groups. Participants in the AC group completed an average of 36.3±2.3 days and those in the YC group completed an average of 38.7±1.7 days in the intervention.
Figure 1.
The percentage of subjects retained in the study as a function of group assignment. The solid line represents data from the AC (Abstinence Contingent) group and the dashed line represents data from the YC (Yoked Control) group. The X axis shows the number of Day in the intervention.
GEE did not reveal a significant effect of group on odds of posting videos to the website (i.e., capturing the sample) (OR = 1.07; 95% CI = 0.54–2.14). Excluding missing data from participants after they withdrew from the study, the AC group posted 68% of the total number of videos expected, whereas the YC group posted 67% of the total number of videos expected. All outcome data from all scheduled biweekly and 12-week follow up assessments were collected from all participants that did not withdraw from the study.
3.2 Efficacy
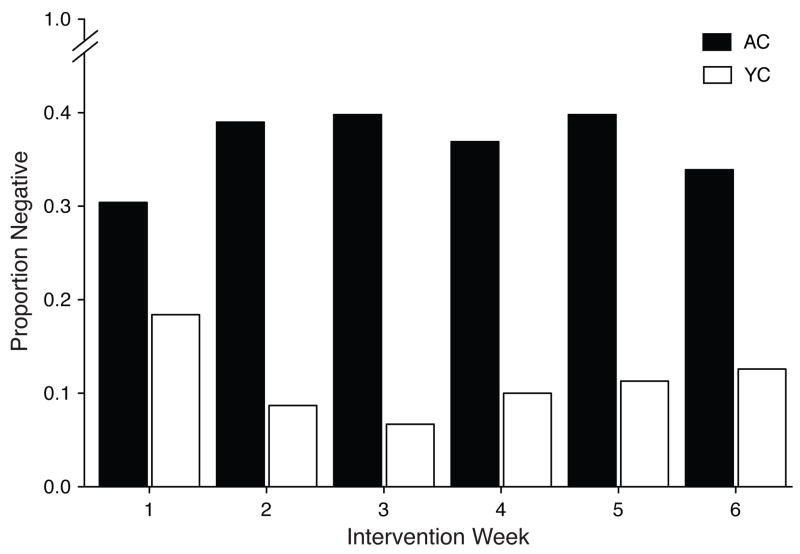
GEE revealed a significant effect of group assignment for proportion of negative samples posted to the website. Participants assigned to AC were more likely to provide a negative sample than those assigned to YC (OR = 4.56; 95% CI = 2.18–9.52). Figure 2 shows the proportion of samples indicating recent abstinence (i.e., negative) as a function of group assignment across the intervention weeks. Percentage of negative samples for weeks 1, 2, 3, 4, 5 and 6 were 30.4, 39.0, 39.8, 36.9, 39.8 and 33.9, respectively, for the AC group. Percentage of negative samples for weeks 1, 2, 3, 4, 5 and 6 were 18.4, 8.7, 6.7, 10.0, 11.3 and 12.6, respectively, for the YC group. Participants in the AC group earned an average of $201.90 ($1.00–784.25) during the trial. Participants in the YC group earned $147.08 ($1.00–636.25) during the trial.
Figure 2.
The proportion of negative samples posted to the study website as a function of group assignment. Closed bars represent data from the AC (Abstinence Contingent) group and open bars represent data from the YC (Yoked Control) group. X axis: Week in the intervention.
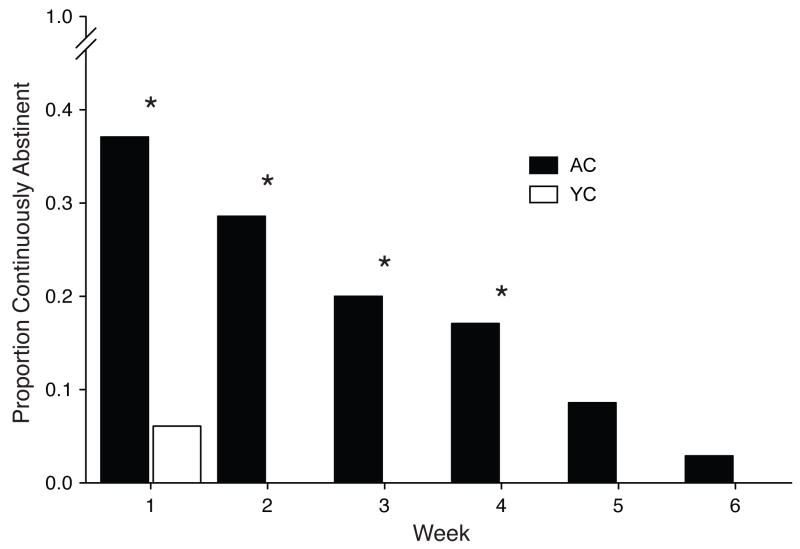
Chi Square revealed a significant effect of group on proportion of participants achieving continuous abstinence. Participants assigned to AC were significantly more likely to achieve 4, 3 and 2 weeks, as well as 1 week, of continuous abstinence over the 6-week intervention compared to those assigned to YC (Chi’s > 6.21, p’s < 0.05). Figure 3 shows the proportion of individuals achieving continuous abstinence as a function of group. Percentage of individuals achieving 1, 2, 3, 4, 5 or 6 weeks of continuous abstinence was 37.1, 28.6, 20.0, 17.1, 8.6 and 2.9, respectively, for the AC group. Percentage of negative samples for Weeks 1, 2, 3, 4, 5 and 6 was 6.1, 0.0, 0.0, 0.0, 0.0, 0.0 and 0.0, respectively, for the YC group.
Figure 3.
The proportion of individuals achieving sustained abstinence based upon videos posted to the study website as a function of group assignment. Closed bars represent data from the AC (Abstinence Contingent) group and open bars represent data from the YC (Yoked Control) group. Bars are missing for 2 through 6 weeks because no YC participants achieved those durations of abstinence. X axis: Weeks of sustained abstinence. Asterisks indicate a significant difference between groups.
An initial GEE analysis of the outcome data gathered from assessments that used Group and Assessment as the factors failed to converge, making ORs incalculable, so data were collapsed across Assessment. This secondary GEE analysis revealed a significant effect of group assignment on odds of providing a negative CO sample. As with data posted to the website, participants assigned to AC were significantly more likely to provide a negative sample than those assigned to YC (OR = 5.30; 95% CI = 1.89–14.82). When collapsed across assessments, 23.4% of CO samples were negative for the AC group compared to 5.5% for the YC group. There was not a significant difference in number of negative cotinine samples as a function of group (OR = 5.47; 95% CI = 0.58–51.49).
4. Discussion
The results of this study demonstrate the feasibility of using the Internet to promote smoking cessation in rural Kentuckians. To the best of our knowledge, this is the first study to use a randomized, controlled design to also demonstrate that participation in the active portion of an abstinence reinforcement intervention over the Internet promotes smoking cessation. Participants were retained for over 85% of study days on average and over two thirds of expected videos were recorded. Given recent findings that rural residents generally do not access the Internet for health care purposes, this sample collection rate is encouraging but could be improved (Miller and West, 2009). Groups did not differ with respect to retention and sample collection. These results also suggest that abstinence reinforcement delivered over the Internet is efficacious in initiating and maintaining smoking abstinence during the active intervention, but that these effects are not prolonged after the intervention ends. Twice daily CO samples recorded on the study website showed that over one third of samples demonstrated recent abstinence in the AC group, which was over 3-fold higher than the rate observed for the YC group. Furthermore, participants assigned to the AC group were more likely to achieve continuous abstinence than those assigned to the YC group.
The rates of abstinence observed with the twice-daily web videos were higher than what was observed at the bi-weekly assessments for the AC group (36.6% versus 23.4%, collapsed across time). The reason for the discrepancy between daily results and data from assessments is not known, but may suggest that daily monitoring over the Internet is either more likely to capture smoking abstinence or to record false negatives than less frequent assessments. It is also important to note that the behavior reinforced in the AC group, posting breath samples of 4 parts per million or below to the website, is where the largest effect was observed. Reinforcement of low CO levels posted to the website possibly contributed to the reduced CO levels gathered at assessments. Future studies may need to reinforce abstinence evidenced by multiple objective indicators (i.e., negative CO levels gathered using the web and negative CO levels and cotinine samples at assessments) to more effectively promote smoking cessation and abstinence.
Regardless of the divergence between abstinence outcomes, this study contributes to and extends an existing literature suggesting that Internet technology can be an effective tool for promoting smoking cessation (Dallery and Glenn, 2005; Dallery et al., 2007; Glenn and Dallery, 2007; Reynolds et al., 2008). Web based smoking-abstinence reinforcement interventions similar to the one used here have resulted in both cigarette smoking cessation and prolonged abstinence from smoking (Dallery and Glenn, 2005; Dallery et al., 2007; Glenn and Dallery, 2007; Reynolds et al., 2008). Up to 60% of samples collected in those studies were negative for smoking, a rate higher than that observed here. The reason for the discrepancy between rates of abstinence observed across studies is not known, but could be due to variations in negative CO thresholds, populations (i.e., largely rural versus not specifically rural) or study designs (i.e., between- versus within-subject). The rates of abstinence observed here are also lower than those observed in traditional abstinence reinforcement interventions, although this difference may also be due to the stricter CO threshold used in the present study (Stitzer et al., 1986). For example, previous studies have deemed CO levels of 7 or 8 parts per million or lower to indicate smoking abstinence (Dallery et al., 2007; Stitzer et al., 1986). Thus, future research will need to determine how to maximize the efficacy of this intervention in rural communities to increase rates of abstinence. The use of a longer intervention period or greater value of alternative reinforcers may be necessary to enhance the efficacy of this intervention in this population.
The results observed in this randomized controlled evaluation provide early empirical support that the Internet can be used to initiate and maintain abstinence from smoking in Appalachian residents. As described above, this population is in great need of effective smoking interventions (BRFSS, 2008; U.S. Congress, Office of Technology Assessment, 1990). These high rates of smoking observed in this special population contribute to high incidence of smoking related mortality and disease.
The intervention evaluated in this trial could be ideal for delivery to rural residents because it minimizes the need for twice daily visits to a clinic, as is practiced in traditional abstinence reinforcement interventions, and only requires a participant to have a computer with Internet access. As noted above, over half of the global population resides in a rural area (United Nations, 2006). Thus, while this intervention was implemented in an Appalachian community, these data suggest that similar interventions could be implemented in other rural areas where smoking prevalence is high. This adaptation partially addresses transportation difficulties and burden on overtaxed healthcare workers often described in rural areas (Gamm, 2004; Nemet and Bailey, 2000).
In rural communities, smoking cessation interventions of any type are difficult to access, but our results suggest the use of the Internet to treat rural cigarette smokers may be an effective way to address this barrier. One obstacle to the implementation of this intervention may be the perception that rural community members do not have access to computers or the Internet. Indeed, there is a gap between rural and non-rural communities when it comes to Internet access, but that gap has become smaller in recent years (Horrigan and Murray, 2006). Moreover, inroads in this area have been made resulting in Kentucky, a largely rural state, leading the nation in broadband expansion, along with other telecommunication advances (ConnectKentucky.org, 2008). This growth in Internet access is not limited to the Kentucky or the United States. Global internet access has increased by over 300% from 2000 to 2008 (www.internetworldstats.com, 2009).
There are several limitations that need to be acknowledged in the present study. First, this study was relatively racially homogenous and enrolled more women than men. Given the demographics of Appalachia, a largely White study population could be expected, but the reason for a higher enrollment of women is not known. It is possible that participation in the generally home-based intervention was more feasible for women than men. Second, use of NRT was not controlled in this study. Participants were free to use NRT after enrolling into the study and a number of participants chose to do so. Twenty one and twenty three participants in the AC and YC groups, respectively, reported initiating NRT after study enrollment. Thus, any effect NRT may have had on the intervention is indeterminable, but the even distribution of NRT use indicates that it was not responsible for group differences in smoking abstinence. In addition, the cotinine outcomes described above may be ascribed to the fact that we did not control the use of NRT. Third, although not analyzed statistically due to lack of power (see below), abstinence at 12-week follow up assessments was limited to about 5% of those in the AC group and 0% in the YC group. High rates of relapse are observed for cigarette smokers in general, however (Carmody, 1992). More research is necessary to determine how to prolong abstinence following the end of smoking cessation interventions. Fourth, the current randomized controlled trial was powered to detect a treatment difference in the primary outcome, percent of breath samples demonstrating recent abstinence posted to the study website. It is likely that many more subjects would be required to demonstrate efficacy on the secondary outcome measures or point-prevalence measures of smoking abstinence. Fifth, about two thirds of expected videos were posted by participants to the study website. Future research should take steps to enhance data collection rates like staff follow-up or coaching for participants that miss posting a scheduled video or providing several central video recording locations should a participant’s computer fail.
This study implemented and evaluated an abstinence reinforcement intervention to rural smokers using the Internet. The 6-week intervention resulted in decreased smoking and sustained abstinence with limited evidence to suggest a prolonged effect after the end of the intervention. The use of Internet technology to promote smoking cessation in rural communities holds promise, but more research is necessary to maximize the efficacy of this intervention and tailor it to rural populations.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Behavioral Risk Factor Surveillance System. [<Accessed on September 3, 2008>];State Prevalence Data Charts. Available at: http://www.cdc.gov/brfss/
- Carmody TP. Preventing relapse in the treatment of nicotine addiction: current issues and future directions. J Psychoactive Drugs. 1992;24(2):31–58. doi: 10.1080/02791072.1992.10471634. [DOI] [PubMed] [Google Scholar]
- ConnectKentucky.org. [<Accessed on 12 March 2009>];Progress Report. 2008 Available at: http://www.connectkentucky.org/_documents/ConnectKentuckyProgressReport2008.pdf.
- Correia CJ, Benson TA. The use of contingency management to reduce cigarette smoking among college students. Exp Clin Psychopharmacol. 2006;14:171–179. doi: 10.1037/1064-1297.14.2.171. [DOI] [PubMed] [Google Scholar]
- Crowley TJ, MacDonald MJ, Zerbe GO, Petty TL. Reinforcing breath carbon monoxide reductions in chronic obstructive pulmonary disease. Drug Alcohol Depend. 1991;29:47–62. doi: 10.1016/0376-8716(91)90021-p. [DOI] [PubMed] [Google Scholar]
- Dallery J, Glenn I. Effects of a voucher reinforcement program for smoking cessation: A feasibility study. J Appl Behav Anal. 2005;38:349–357. doi: 10.1901/jaba.2005.150-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Glenn IM, Raiff BR. An Internet-based abstinence reinforcement treatment for cigarette smoking. Drug Alcohol Depend. 2007;86:230–238. doi: 10.1016/j.drugalcdep.2006.06.013. [DOI] [PubMed] [Google Scholar]
- Donatelle RJ, Prows SL, Champeau D, Hudson D. Randomized controlled trial using social support and financial incentives for high risk pregnant smokers: Significant other support (SOS) program. Tob Control. 2000;9:67–69. doi: 10.1136/tc.9.suppl_3.iii67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberhardt MS, Pamuk ER. The Importance of Place of Residence: Examining Health in Rural and Nonrural Areas. Am J Public Health. 2004;94:1682–1686. doi: 10.2105/ajph.94.10.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedell GH, Rubio A, Maretzki A, Garland B, Brown P, Crane M, Hickman P. Community cancer control in a rural, underserved population: The Appalachian leadership initiative on cancer project. J Health Care Poor Underserv. 2001;12:5–19. doi: 10.1353/hpu.2010.0523. [DOI] [PubMed] [Google Scholar]
- Gamm LD. Mental health and substance abuse services among rural minorities. J Rural Health. 2004;20:206–209. doi: 10.1111/j.1748-0361.2004.tb00030.x. [DOI] [PubMed] [Google Scholar]
- Glenn IM, Dallery J. Effects of internet-based voucher reinforcement and a transdermal nicotine patch on cigarette smoking. J Appl Behav Anal. 2007;40:1–13. doi: 10.1901/jaba.2007.40-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Alessi SM, Dantona RL. Voucher-based incentives: A substance abuse treatment innovation. Addict Behav. 2002;27:887–910. doi: 10.1016/s0306-4603(02)00297-6. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Heil SH, Solomon LJ, Bernstein IM, Lussier JP, Abel RL, Lynch ME, Badger GJ. A pilot study on voucher-based incentives to promote abstinence from cigarette smoking during pregnancy and postpartum. Nicotine Tob Res. 2004;6:1015–20. doi: 10.1080/14622200412331324910. [DOI] [PubMed] [Google Scholar]
- Horrigan J, Murray K. Rural broadband internet use. [<Accessed 24 March 2009>];Pew Internet and American Life Project. 2006 Available at: http://www.pewinternet.org/Reports/2006/Home-Broadband-Adoption-in-Rural-America.aspx.
- Javors MA, Hatch JP, Lamb RJ. Cut-off levels for breath carbon monoxide as a marker for cigarette smoking. Addiction. 2005;100:159–167. doi: 10.1111/j.1360-0443.2004.00957.x. [DOI] [PubMed] [Google Scholar]
- Lamb RJ, Kirby KC, Morral AR, Galbicka G, Iguchi MY. Improving contingency management programs for addiction. Addict Behav. 2004;29:507–523. doi: 10.1016/j.addbeh.2003.08.021. [DOI] [PubMed] [Google Scholar]
- Lamb RJ, Morral AR, Galbicka G, Kirby KC, Iguchi M. Shaping reduced smoking in smokers without cessation plans. Exp Clin Psychopharmacol. 2005;13:83–92. doi: 10.1037/1064-1297.13.2.83. [DOI] [PubMed] [Google Scholar]
- Middleton ET, Morice AH. Breath carbon monoxide as an indication of smoking habit. Chest. 2000;117:758–163. doi: 10.1378/chest.117.3.758. [DOI] [PubMed] [Google Scholar]
- Miller EA, West DM. Where’s the revolution? Digital technology and health care in the internet age. J Health Polit Policy Law. 2009;34:261–84. doi: 10.1215/03616878-2008-046. [DOI] [PubMed] [Google Scholar]
- Nemet GF, Bailey AJ. Distance and health care utilization among rural elderly. Soc Sci Med. 2000;50:1197–1208. doi: 10.1016/s0277-9536(99)00365-2. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Dallery J, Shroff P, Patak M, Leraas KA. Web-based contingency management program with adolescent smokers. J Appl Behav Anal. 2008;41(4):597–601. doi: 10.1901/jaba.2008.41-597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll JM, Prendergast ML, Sorensen K, Prakash S, Chudzynski JE. A comparison of voucher exchanges between criminal justice involved and noninvolved participants enrolled in voucher-based contingency management drug abuse treatment programs. Am J Drug Alcohol Abuse. 2005;31:393–401. doi: 10.1081/ada-200056774. [DOI] [PubMed] [Google Scholar]
- Rugg SS, Bailey AL, Browning SR. Preventing cardiovascular disease in Kentucky: epidemiology, trends and strategies for the future. J Ky Med Assoc. 2008;106:149–161. [PubMed] [Google Scholar]
- Signorini DF, Leung O, Simes RJ, Beller E, Gebski VJ, Callaghan T. Dynamic balanced randomization for clinical trials. Stat Med. 1993;12:2343–2350. doi: 10.1002/sim.4780122410. [DOI] [PubMed] [Google Scholar]
- Silverman K, Higgins ST, Brooner RK, Montoya ID, Cone EJ, Schuster CR, Preston KL. Sustained cocaine abstinence in methadone maintenance patients through voucher-based reinforcement therapy. Arch Gen Psychiatry. 1996;53:409–415. doi: 10.1001/archpsyc.1996.01830050045007. [DOI] [PubMed] [Google Scholar]
- Silverman K, Wong CJ, Umbricht-Schneiter A, Montoya ID, Schuster CR, Preston KL. Broad beneficial effects of reinforcement for cocaine abstinence in methadone patients. J Consult Clinical Psychol. 1998;66:811–824. doi: 10.1037//0022-006x.66.5.811. [DOI] [PubMed] [Google Scholar]
- Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models and individual growth models. J Educ Behav Stat. 1998;24:323–355. [Google Scholar]
- Stensland J, Mueller C, Sutton J. An Analysis of the Financial Conditions of Health Care Institutions in the Appalachian Region and their Economic Impacts. [<Accessed on September 10, 2008>];2002 Available at: http://www.arc.gov/index.do?nodeId=1647.
- Stitzer ML, Rand CS, Bigelow GE, Mead AM. Contingent payment procedures for smoking reduction and cessation. J Appl Behav Anal. 1986;9(2):197–202. doi: 10.1901/jaba.1986.19-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stitzer ML. Combined behavioral and pharmacological treatments for smoking cessation. Nicotine Tob Res. 1999;1:S181–S187. doi: 10.1080/14622299050012041. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2006 National Survey on Drug Use and Health: National Findings. Rockville, MD: US Office of Applied Studies; 2007. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: National Findings. Rockville, MD: US Office of Applied Studies; 2008. [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division. Urban and Rural Areas, 2005. New York, NY: United Nations; 2006. [Google Scholar]
- U.S. Census Bureau. [<Accessed on 11 May 2009>];United States -- Urban/Rural and Inside/Outside Metropolitan Area. 2000 Available at: http://factfinder.census.gov/servlet/GCTTable?_bm=y&-geo_id=01000US&-_box_head_nbr=GCT-P1&-ds_name=DEC_2000_SF1_U&-format=US-1.
- U.S. Congress, Office of Technology Assessment. Health Care in Rural America. Washington, DC: Government Printing Office; 1990. [Google Scholar]
- Williams JA. Appalachia: A History. Chapel Hill, NC: University of North Carolina Press; 2001. [Google Scholar]
- Wingo PA, Tucker TC, Jamison PM, Martin H, McLaughlin C, Bayakly R, Bolick-Aldrich S, Colsher P, Indian R, Knight K, Neloms S, Wilson R, Richards TB. Cancer in Appalachia, 2001–2003. Cancer. 2008;112:181–192. doi: 10.1002/cncr.23132. [DOI] [PubMed] [Google Scholar]
- Wiseman EJ, Williams DK, McMillan DE. Effectiveness of payment for reduced carbon monoxide levels and noncontingent payments on smoking behaviors in cocaine-abusing outpatients wearing nicotine or placebo patches. Exp Clin Psychopharmacol. 2005;13:102–110. doi: 10.1037/1064-1297.13.2.102. [DOI] [PubMed] [Google Scholar]
- www.arc.gov, 2003. Population Density Rates in Appalachia, 2000. http://www.arc.gov/index.do?nodeId=2853 <Accessed 12 May 2009>
- www.internetworldstats.com, 2009. Internet Usage Statistics: The Internet Big Picture World Internet Users and Population Stats. http://www.internetworldstats.com/stats.htm <Accessed 11 May 2009>
- Yang T, Li F, Yang X, Wu Z, Feng X, Wang Y, Wang X, Abdullah AS. Smoking patterns and sociodemographic factors associated with tobacco use among Chinese rural male residents: a descriptive analysis. BMC Public Health. 2008;8:248. doi: 10.1186/1471-2458-8-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang K-Y, Albert P. Models for longitudinal data, a generalized estimating equation approach. Biometrics. 1988;44:1049–10. [PubMed] [Google Scholar]