Abstract
An acute myocardial infarction is a rare complication of a subarachnoid haemorrhage. The combination of these two conditions imposes important treatment dilemmas. We describe two patients with this combination of life-threatening conditions. Patient 1 was treated with emergency percutaneous coronary intervention followed by clipping of the anterior communicating artery aneurysm. Six months after discharge the patient's memory and orientation had almost completely recovered. Patient 2 was treated with aspirin until coiling of the aneurysm could be performed. After successful coiling low-molecular-weight heparin was added. One week later the patient died due to a free wall rupture. (Neth Heart J 2009;17:284-7.)
Keywords: subarachnoid haemorrhage, myocardial infarction
The annual incidence of non-traumatic subarachnoid haemorrhage (SAH) varies from 2 to 22 per 100,000.1 The incidence in women is almost twice as high as in men. Primary SAH usually results from rupture of a saccular aneurysm or arteriovenous malformations. Electrocardiographic changes occur during the acute stage in 50 to 100% of SAH cases.2-4 The most common abnormalities are non-specific ST deviations, T-wave inversion and prolonged QT interval. These ECG changes have no clinical or prognostic consequence. Elevated troponin is found in approximately 20% of SAH cases and is associated with an increased risk of hypotension, pulmonary oedema, left ventricular dysfunction and delayed cerebral ischaemia.5-7
Cardiac dysfunction and abnormal left ventricular wall motion after SAH are well-recognised phenomena as well, but the association between SAH and acute myocardial infarction is rare. To our knowledge only two cases describing acute myocardial infarction complicating SAH have been published in international literature.8,9 We report on two female patients admitted with an SAH complicated by an ST-elevation myocardial infarction.
Patient 1
A 48-year-old woman with peripheral vascular disease treated with aspirin presented with decreased consciousness and weakness of the right side of the body. The ambulance electrocardiogram showed an acute inferoposterior myocardial infarction with right ventricular involvement (figure 1). Heparin and clopidogrel were administered. On arrival the neurological impairment had worsened and cranial computed tomography angiography (CTA) showed left frontal subarachnoid haemorrhage originating from a broad-based anterior communicating artery aneurysm, whereupon the heparin was antagonised with protamine (figure 2). Balancing the risk of a conservative strategy against the risk of anticoagulation a percutaneous coronary intervention without stenting was intended. However, massive dissection of the right coronary artery after dilatation made stent implantation inevitable. The peak levels of troponin I and creatine kinase were >100 μg/l (normal value <0.20 μg/l) and 1894 U/l (normal value <200 U/l) respectively. Subsequently, angiography of the cerebral arteries was performed which confirmed the CTA finding of a broad-based aneurysm of the anterior communicating artery. Coiling was not considered possible due to the broad-based neck of the aneurysm and the patient underwent surgical clipping of the aneurysm. During the first few days the patient was dependent on inotropic agents and she remained intubated for another week. Consciousness improved over the next few days. Echocardiography showed a hypokinetic inferior wall of the left ventricle with an impaired residual function of the left ventricle. The patient remained confused and disoriented in time, place and space during the hospitalisation. Six months after discharge the patient's memory and orientation had almost completely recovered.
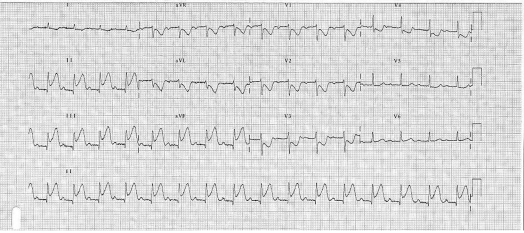
Figure 1.
ECG of patient 1: acute inferoposterior myocardial infarction.
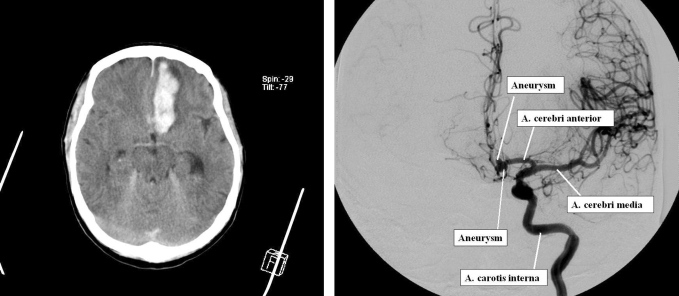
Figure 2.
Left image: CT scan of patient 1 demonstrating subarachnoid and cerebral haemorrhage. Right image: cerebral angiography of patient 1 demonstrating the aneurysm of the anterior communicating artery.
Patient 2
A 62-year-old female without prior medical history who smoked a few cigarettes a day presented with a sudden loss of consciousness which recovered spontaneously over two hours. On admission she was unable to recall what had happened and her only complaints were of a minor headache and chest pain. She said she had had prior episodes of this chest pain in the past few weeks during exercise.
Cranial CT showed an SAH from an aneurysm of the anterior communicating artery. The ECG demonstrated an acute inferoposterior myocardial infarction with right ventricular involvement (figure 3). The peak troponin level measured was 32.0 μg/l (normal value <0.20 μg/l). Given the unprotected aneurysm, the initial therapy for the myocardial infarction was limited to aspirin. After successful coiling of the aneurysm the next day, low-molecular-weight heparin and a β-blocker were added.
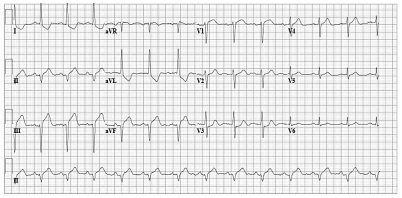
Figure 3.
ECG of patient 2: acute inferoposterior myocardial infarction with right ventricular involvement.
One week after admission the patient died of a sudden circulatory arrest in spite of an attempted reanimation. Autopsy revealed cardiac tamponade due to a free wall rupture, thrombus in the right coronary artery and a one-week-old posterior myocardial infarction (figure 4).
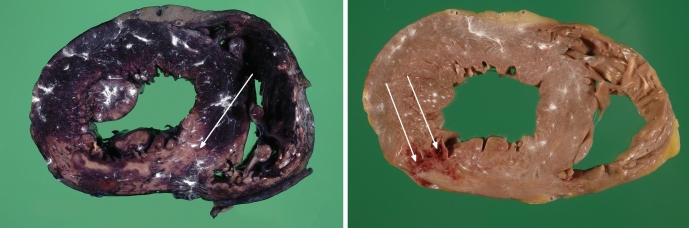
Figure 4.
Autopsy findings of patient 2. Left image: a one-week-old (confirmed microscopically) posterior myocardial infarction of the left ventricle (cross section of the heart after LDH reaction). Right image: a rupture of approximately 1 cm in the posterior wall of the left ventricle (cross section of the heart).
Discussion
Although ECG abnormalities, elevated troponin and abnormal left ventricular wall motion in patients with SAH are well-known phenomena, the association with ST-elevation myocardial infarction is rare. This unfortunate combination implicates a dilemma for physicians of different disciplines. The acute myocardial infarction would prompt the cardiologist to perform emergency percutaneous coronary intervention and administer antithrombotic drugs. The unprotected aneurysm would make the neurologist reluctant to administrate these antithrombotic agents, given the risk of rebleeding. Routine treatment of a subarachnoid haemorrhage consists of coiling or clipping of the aneurysm within 72 hours. Ideally, treatment of an unprotected aneurysm with concomitant myocardial infarction would consist of immediate coiling or clipping of the aneurysm followed by percutaneous coronary intervention. Antithrombotic drugs can only be safely installed after coiling or clipping. However, endovascular coiling is not offered around the clock and not all aneurysms are suitable for coiling. When the aneurysm cannot be coiled immediately, coronary intervention can be considered as initial treatment despite the use of antithrombotic drugs. The extent of the myocardium at risk indicated by cumulative ST elevation on the ECG plays an important role in this decision-making process. If the ST elevation is limited, conservative treatment can be considered. A large STelevation myocardial infarction makes reperfusion therapy essential for myocardial salvage and mortality reduction.
The mechanism leading to an ST-elevation myocardial infarction in the patient presenting with an SAH is unclear. Relatively more is known of more subtle cardiac abnormalities complicating SAH. The cardiac injury that is found in up to 15% of cases of SAH is probably caused by the massive catecholamine release. This hypothesis is supported by research with animal models: experimental SAH in dogs led to cathecholamine release in the myocardium and ECG changes.10
Transient left ventricular dysfunction with an akinetic or dyskinetic apex has also been described in SAH patients without significant coronary heart disease.11,12 This phenomenon has recently become known as Takotsubo cardiomyopathy or transient left ventricular apical ballooning.13 This cardiomyopathy is caused by severe physical (e.g. an SAH) or emotional stress and more than 95% of the patients that experienced this stress-induced cardiomyopathy are female.14 Plasma catecholamine concentrations in these patients are remarkably higher than in patients presenting with myocardial infarction. A possible explanation of this cardiomyopathy is ischaemia caused by coronary spasm. In a recent angiographic study in Takotsubo cardiomyopathy patients, coronary spasm was observed or could be provoked by ergonovine or acetylcholine in about 70%.13 In most cases of stress-induced cardiomyopathy, however, spasm cannot be provoked and ST elevations are absent. Microvascular spasm and direct myocyte damage by catecholamines could be other possible mechanisms in the pathogenesis of Takotsubo cardiomyopathy.15
However, in both the cases we describe here, a thrombotic occlusion of a coronary artery was found and the definition of Takotsubo cardiomyopathy comprises the absence of critical coronary lesions. In the setting of SAH, several factors may contribute to the occurrence of a myocardial infarction: blood pressure rises, cathecholamines are released and a state of hypercoagulability is induced. In patients with preexisting coronary artery disease the most probable cause of an acute myocardial infarction when an SAH occurs is thrombus formation or plaque rupture triggered by a combination of these factors. Takotsubo cardiomyopathy might be a complication of SAH but we do not believe that the thrombotic occlusions in these two patients were caused by this syndrome.
Conclusion
In patients with a subarachnoid haemorrhage troponin is elevated in approximately 20% and ECG changes without prognostic significance occur in 50 to 100%. The combination with an ST-elevation myocardial infarction is very rare. When ST-elevation myocardial infarction complicates a subarachnoid haemorrhage, a rapid decision about percutaneous coronary intervention and the use of antithrombotic drugs has to be made. Whenever feasible, immediate coiling of the aneurysm followed by percutaneous coronary intervention should be performed, followed by administration of antithrombotic agents.
References
- 1.Ingall T, Asplund K, Mahonen M, Bonita R. A multinational comparison of subarachnoid hemorrhage epidemiology in the WHO MONICA stroke study. Stroke 2000: 31: 1054. [DOI] [PubMed] [Google Scholar]
- 2.Sommargren CE, Zaroff JG, Banki N, Drew BJ. Electrocardiographic repolarization abnormalities in subarachnoid hemorrhage. J Electrocardiol 2002: 35(suppl):257-62. [DOI] [PubMed] [Google Scholar]
- 3.Zaroff JG, Rordorf GA, Newell JB, Ogilvy CS, Levinson JR. Cardiac outcome in patients with subarachnoid hemorrhage and electrocardiographic abnormalities. Neurosurgery 1999: 44: 34-9. [DOI] [PubMed] [Google Scholar]
- 4.Brouwers PJAM, Wijdicks EFM, Hasan D, Vermeulen M, Wever EFD, Frericks H, et al. Serial electrocardiographic recording in aneurysmal subarachnoid hemorrhage. Stroke 1989: 20: 1162-7. [DOI] [PubMed] [Google Scholar]
- 5.Tung P, Kopelnik A, Banki N, Ong K, Ko N, Lawton MT, et al. Predictors of neurocardiogenic injury after subarachnoid hemorrhage. Stroke 2004: 35: 548-53. [DOI] [PubMed] [Google Scholar]
- 6.Horowitz MB, Willet D, Keffer J. The use of cardiac troponin-I (cTnI) to determine the incidence of myocardial ischemia and injury in patients with aneurysmal and presumed aneurysmal subarachnoid hemorrhage. Acta Neurochir (Wien) 1998: 140: 87-93. [DOI] [PubMed] [Google Scholar]
- 7.Parekh N, Venkatesh B, Cross D, Leditschke A, Atherton J, Miles W, et al. Cardiac troponin I predicts myocardial dysfunction in aneurysmal subarachnoid hemorrhage. J Am Coll Cardiol 2000; 36:1328-35. [DOI] [PubMed] [Google Scholar]
- 8.Bárcena JP, Rota JI, Ramírez JH, Sala MF, JI. Subarachnoid hemorrhage and acute myocardial infarction. Intensive Care Med 2000: 26: 1160-1. [DOI] [PubMed] [Google Scholar]
- 9.Pine DS, Tierney L. Clinical problem-solving. A stressful interaction. N Engl J Med 1996: 335: 1530-4. [DOI] [PubMed] [Google Scholar]
- 10.Elrifai AM, Bailes JE, Shih SR, Dianzumba S, Brillman J. Characterization of the cardiac effects of acute subarachnoid hemorrhage in dogs. Stroke 1996: 27: 737-41. [DOI] [PubMed] [Google Scholar]
- 11.Otomo S, Tashimo M, Shimoda O. Two cases of transient left ventricular apical ballooning syndrome associated with subarachnoid hemorrhage. Anesth Analg 2006: 103: 583-6. [DOI] [PubMed] [Google Scholar]
- 12.Lee VH, Conolly HM, Fulgham JR, Manno EM, Brown RD Jr, Wijdicks EF. Tako-tsubo cardiomyopathy in aneurysmal subarachnoid hemorrhage: an underappreciated ventricular dysfunction. J Neurosurg 2006: 105: 264-70. [DOI] [PubMed] [Google Scholar]
- 13.Kurisu S, Sato H, Kawagoe T, Ishihara M, Shimatani Y, Nishioka K et al. Tako-tsubo-like left ventricular dysfunction with STsegment elevation: a novel cardiac syndrome mimicking acute myocardial infarction. Am Heart J 2002: 143: 448-55. [DOI] [PubMed] [Google Scholar]
- 14.Wittstein IS, Thiemann DR, Lima JAC, Baughman KL, Schulman SP, Gerstenblith G, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005; 352: 539-48. [DOI] [PubMed] [Google Scholar]
- 15.Banki NM, Kopelnik A, Dae MW. Acute neurocardiogenic injury after subarachnoid hemorrhage. Circulation 2005: 112: 3314-9. [DOI] [PubMed] [Google Scholar]