Abstract
A 61-year-old male with a history of metastatic colorectal cancer was referred to our hospital for primary coronary intervention because of acute ST-elevation myocardial infarction. Coronary angiography, however, revealed no significant stenoses. When asked, the patient revealed that capecitabine (Xeloda®) was started by his oncologist one day before admission. It is known that this oral 5-FU analogue drug, used in metastatic colorectal cancer, can cause coronary artery spasms. The main treatment of capecitabine-induced vasospasm is discontinuation of the drug. Indeed, after cessation of the drug the patient remained free of symptoms and the ECG abnormalities normalised. (Neth Heart J 2009;17:288-91.)
Keywords: coronary artery spasm, capecitabine, 5-fluorouracil, myocardial infarction, colon cancer
A 61-year-old male was admitted to a referring hospital because of acute chest pain. Three years ago he had suffered an acute coronary syndrome. Coronary angiography (CAG) showed focal coronary sclerosis in the right coronary artery, but no obstructive lesions and the patient was treated conservatively with aspirin, metoprolol, isosorbide-5-mononitrate and rosuvastatin. Furthermore, he had colon cancer with metastases in the liver and the lungs.
After dinner the patient experienced 30 minutes of retrosternal chest pain without radiation. Because the chest pain was not relieved by sublingual nitroglycerin he contacted his general practitioner who sent him to hospital for observation. At the referring hospital he had no symptoms. The electrocardiogram (ECG) at admittance showed sinus rhythm with early repolarisation (figure 1). Four hours after admission, while waiting for the second troponin, there was recurrence of heavy retrosternal chest discomfort with radiation to the left arm. A new ECG was taken immediately and revealed sinus rhythm with ST-segment elevation in the inferolateral leads and peaked T-waves (figure 2). An ST-elevation myocardial infarction was diagnosed and he was sent to our hospital for primary coronary intervention. Immediate treatment with 600 mg clopidogrel, 5000 units heparin and 160 mg aspirin was initiated and he was sent directly to our catheterisation laboratory. At presentation to the catheterisation laboratory he was free of symptoms. CAG revealed diffuse coronary sclerosis, but no significant stenosis in the coronary arteries with TIMI 3 flow in all vessels. In comparison with his CAG performed three years ago, no changes were seen. He was admitted to the coronary care unit. His blood pressure was 134/70 mmHg and the pulse 77 beats/min. There was no fever. No abnormalities were discovered on physical examination. The cardiac enzymes and the inflammation parameters were not elevated. His renal function was normal. Transthoracic echocardiography showed normal left and right ventricular function and no pericardial effusion. Two hours later, the severe chest discomfort returned with ST-segment elevation similar to the ECG at the referring hospital and nitroglycerin IV was started. Because of the intermittent character of his complaints with concomitant ST-segment changes, coronary artery vasospasms were now suspected as the cause of the symptoms. When asked, the patient revealed that capecitabine (Xeloda®) 1500 mg twice a day had been started just one day earlier. Capecitabine can indeed cause coronary artery spasms. A calcium channel blocker (nifedipine) was started and the capecitabine was stopped after consultation with the oncologist. The patient became free of symptoms and the ECG showed normalised ST segments. He was transported back to the referring hospital in good condition.
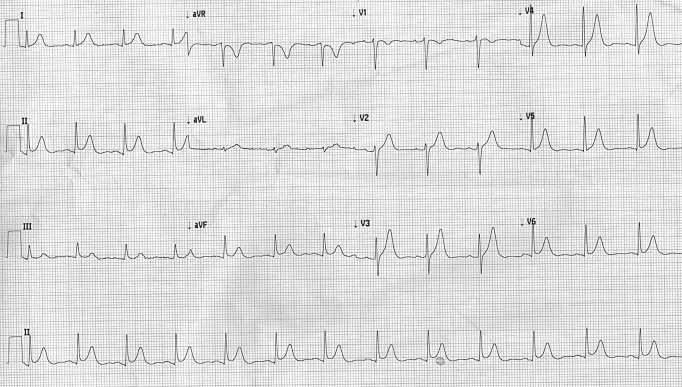
Figure 1.
Electrocardiogram at admission (25 mm/s, 10 mm/mV).
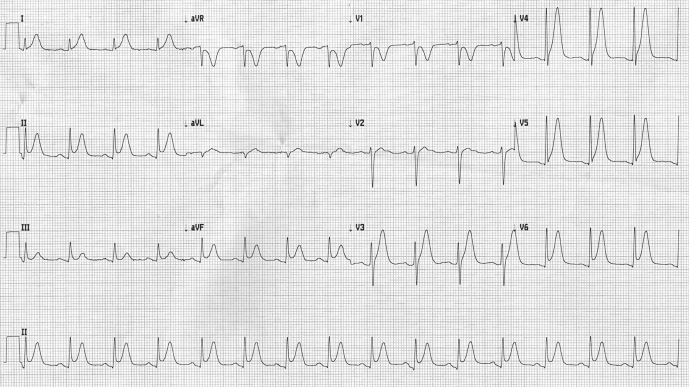
Figure 2.
Electrocardiogram taken during chest pain (25 mm/s, 10 mm/mV).
Discussion
Capecitabine (Xeloda®) is an orally administrated prodrug of 5-fluorouracil (5-FU) and is used as adjuvant chemotherapy. In patients with metastatic colorectal cancer, capecitabine is an established firstline treatment and has now replaced intravenous (IV) 5-FU.1 The toxic effect of IV 5-FU on the coronary endothelium and myocardium is rare but it can be lethal with potential myocardial infarction, ventricular arrhythmias and sudden death.2 In a recent Swedish analysis the incidence of reported 5-FU cardiotoxicity is around 4.3%, but is higher when renal function is impaired.3 In the last ten years several case reports of induced cardiotoxicity by the oral 5-FU analogue capecitabine have been published.2,4-14 In these reports, the exact pathophysiology of cardiac injury is not elucidated. It has been postulated that capecitabine has the same mechanism of side effects as IV 5-FU. Possible mechanisms in animal models suggest a direct toxic effect on the coronary endothelial intima, toxic myocarditis, coronary artery thrombosis and vasospasm. Depending on the dose, cardiac side effects can occur within 24 hours after taking the drug. A list of the potential cardiotoxicity of IV 5-FU and capecitabine is summarised in table 1. Patients with a history of coronary artery disease may have a higher prevalence of capecitabine-induced toxicity, probably because of the expression of thymidine phosphorylase in atherosclerotic plaques. Thymidine phosphorylase is one of the enzymes converting capecitabine to fluorouracil and is present in high concentrations in tumour tissues.15
Table 1.
List of reported potential cardiotoxicity in patients using capecitabine or intravenous 5-fluorouracil (IV 5-FU).
| Capecitabine | IV 5-FU | |
|---|---|---|
| Coronary artery spasm with ST-segment changes | X | X |
| (Exercise-induced) myocardial ischaemia with or without troponin release | X | X |
| Myocardial infarction | X | |
| Myocarditis | X | X |
| Silent ST-segment deviation | X | X |
| Supraventricular tachycardia | X | X |
| Sudden death | X | |
| Ventricular tachycardia | X |
We report a case of coronary artery vasospasm, without myocardial necrosis, in a patient recently treated with capecitabine. The clinical presentation of capecitabine-induced coronary artery spasm can mimic myocardial infarction and/or unstable angina pectoris. Since our patient had a history of coronary artery disease and the ECG showed ST-segment elevation, the patient was sent immediately to the catheterisation laboratory. However, the triad of 1) intermittent chest pain with ST-segment elevation but no reciprocal ST depressions, 2) the immediate ST resolution when chest pain resolves and 3) the normal transthoracic echocardiography is more typical for coronary artery spasms. The presence of (mild) coronary artery disease in our patient could have made him more susceptible to the side effects of capecitabine. Administering capecitabine in these patients has not been an absolute contraindication for oncologists. Furthermore, many patients with colorectal metastatic cancer have no cardiac history and are of middle and high age with several cardiac risk factors, but still receive this drug without screening them for coronary artery disease. This is why the cardiologist should be aware of the possible cardiac side effects when confronted with a patient presenting with chest pain who has recently started treatment with capecitabine. The main treatment of capecitabine-induced coronary vasospasm is withdrawal of the drug. Supportive medications as calcium-channel blockers in combination with longacting nitrates are also recommended in the treatment of coronary artery spasms.
We conclude that with its increasing use in cancer therapy, the cardiologist should have knowledge of the cardiotoxicity of capecitabine, especially when used in patients with documented coronary artery disease.
References
- 1.Scheithauer W, McKendrick J, Begbie S, Borner M, Burns WI, Burns HA, et al. Oral capecitabine as an alternative to i.v. 5-fluorouracil-based adjuvant therapy for colon cancer: safety results of a randomized, phase III trial. Ann Oncol 2003;14:1735-43. [DOI] [PubMed] [Google Scholar]
- 2.Kosmas C, Kallistratos MS, Kopterides P, Syrios J, Skopelitis H, Mylonakis N, et al. Cardiotoxicity of fluoropyrimidines in different schedules of administration: a prospective study. J Cancer Res Clin Oncol 2008;134;75-82. [DOI] [PubMed] [Google Scholar]
- 3.Jensen SA, Sorensen JB. Risk factors and prevention of cardiotoxicity induced by 5-fluorouracil or capecitabine. Cancer Chemother Pharmacol 2006;58:487-93. [DOI] [PubMed] [Google Scholar]
- 4.Goldsmith YB, Roistacher N, Baum MS. Capecitabine-induced coronary vasospasm. J Clin Oncol 2008;26:3802-4. [DOI] [PubMed] [Google Scholar]
- 5.Papadopoulos CA, Wilson H. Capecitabine-associated coronary vasospasm: a case report. Emerg Med J 2008;25:307-9. [DOI] [PubMed] [Google Scholar]
- 6.Scott PA, Ferchow L, Hobson A, Curzen NP. Coronary spasm induced by capecitabine mimicks ST elevation myocardial infarction. Emerg Med J 2008;25:699-700. [DOI] [PubMed] [Google Scholar]
- 7.Arbea L, Coma-Canella I, Martinez-Monge R, Garcia-Foncillas J. A case of capecitabine-induced coronary microspasm in a patient with rectal cancer. World J Gastroenterol 2007;13:2135-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Halteren HK, Liem AH, Planting AS. Myocardial ischemia as a result of treatment with capecitabine. Ned Tijdschr Geneeskd 2007;151:1469-73. [PubMed] [Google Scholar]
- 9.Wijesinghe N, Thompson PI, McAlister H. Acute coronary syndrome induced by capecitabine therapy. Heart Lung Circ 2006;15:337-9. [DOI] [PubMed] [Google Scholar]
- 10.Sestito A, Sgueglia GA, Pozzo C, Cassano A, Barone C, Crea F, et al. Coronary artery spasm induced by capecitabine. J Cardiovasc Med 2006;7:136-8. [DOI] [PubMed] [Google Scholar]
- 11.Rizvi AA, Schauer P, Owlia D, Kallal JE. Capecitabine-induced coronary vasospasm. Angiology 2004;55:93-7. [DOI] [PubMed] [Google Scholar]
- 12.Frickhofen N, Beck FJ, Jung B, Fuhr HG, Andrasch H, Sigmund H. Capecitabine can induce acute coronary syndrome similar to 5-fluorouracil. Ann Oncol 2002;13:797-801. [DOI] [PubMed] [Google Scholar]
- 13.Gorgulu S, Celik S, Tezel T. A case of coronary spasm induced by 5-fluorouracil. Acta Cardiol 2002;57:381-3. [DOI] [PubMed] [Google Scholar]
- 14.Schnetzler B, Popova N, Collao Lamb C, Sappino AP. Coronary spasm induced by capecitabine. Ann Oncol 2001;12:723-4. [DOI] [PubMed] [Google Scholar]
- 15.Boyle JJ, Wilson B, Harrower S, Weissberg PL, Fan TP. Expression of angiogenic factor thymidine phosphorylase and angiogenesis in human atherosclerosis. J Pathol 2000;192:234-42. [DOI] [PubMed] [Google Scholar]