Abstract
Purpose
The purpose of this study was to determine the differences in depressive symptoms among a sample of heart failure outpatients by examining sociodemographic and clinical variables: sex, race, marital status, living arrangement/status, heart failure severity, and age. The most frequently reported depressive symptoms were also examined.
Design
A descriptive, cross-sectional design was used.
Setting
Patients were enrolled in a larger research study from 5 clinics in the Midwest (1 adult primary care medicine clinic, 1 heart clinic, and 3 heart failure clinics).
Sample
The sample included 150 patients with mean age of 61.3 years; 88 (59%) were men, and 62 (41%) were women; 47 (31%) were African American, 101 (67%) were white, and 2 (2%) were Asian patients. Forty-seven percent of the patient sample were New York Heart Association class III. Approximately half (51%) of the patient sample were married.
Methods
The Patient Health Questionnaire 8 was used to measure depressive symptoms. Heart failure severity was assessed using the New York Heart Association classification.
Findings
Patients with class III and IV had significantly more depressive symptoms than patients with class I and II (P < .0001). Age was negatively correlated with depressive symptoms scores (P < .0002). There were no significant differences in depressive symptoms among the variables of sex, race, marital status, or living arrangement. The most frequently reported depressive symptom was “feeling tired/no energy.”
Conclusions
The findings from this study may contribute to the development of a broader knowledge base regarding depressive symptoms and its correlates in heart failure and may be used as a foundation for further research.
Keywords: depressive symptoms, heart failure, sociodemographic
Heart failure (HF) is one of the major public health problems facing America today.1 Over the past decade, HF has been the fastest growing form of cardiovascular disease.2 The trajectory of HF is typically one of progressive, functional decline.3 In 2004 the prevalence of HF in America was estimated at 5.2 million, with approximately 550,000 new cases of HF reported annually.1 The incidence of HF approaches 10 per 1000 population after the age of 65 years. The 1-year mortality rate for HF is high, with 1 in 5 patients dying.1 Heart failure is distinguished by the hallmark clinical symptoms of shortness of breath, fluid retention, edema, fatigue, and poor exercise tolerance.4 Individuals with HF endure severe symptom burden, marked functional limitation, and impaired quality of life.5
Depression is a common, comorbid condition among patients with HF.6–11 In the first meta-analytic review of depression and HF, Rutledge and colleagues2 examined 36 publications meeting preset criteria and found that the overall point estimate prevalence rate was 22% in 27 studies among HF patients, a rate that is 2 to 3 times that of the general population. After controlling for the variables of sex, race, and age, Abramson and colleagues12 determined that depression was independently associated with more than a 2-fold higher risk of developing HF compared with nondepressed persons (hazard ratio 2.59; 95% confidence interval 1.57–4.27; P < .001). Among patients with HF, hospitalized patients report the highest rate of depressive symptoms (78%);10 whereas, the reported rates of depressive symptoms among stable outpatients may range from 13% to 48%.13
Depressive symptoms among patients with chronic HF have been significantly associated with poor outcomes including increased clinical events and mortality rates.2,10,13–16 Sherwood and colleagues studied 204 stable outpatients with HF who were receiving standard medical treatment and reported that symptoms of depression were associated with increased risk of death or hospitalization during a median 3-year follow-up.17 During follow-up, 26% died and 62% were hospitalized at least once, including 48% who were hospitalized because of cardiovascular disease. Clinically significant symptoms of depression were observed in 46% of the study sample.17 Depression among patients hospitalized with HF is an independent risk factor for morbidity and mortality regardless of HF etiology.14,18 The reasons remain unknown for the high prevalence of depressive symptoms in HF and the strong association between depressive symptoms and adverse outcomes.5,19
Jiang and colleagues14 prospectively studied 374 patients hospitalized with HF to investigate the prevalence of depression and its effect on all-cause mortality and readmissions during the first year after screening for depression. Using the Beck Depression Inventory (BDI) to assess depression severity, patients with depression had the highest mortality rates at 3 months and one year- 13% and 26%, respectively. The patients with HF who had depression were more than twice as likely as nondepressed patients to die or be rehospitalized within 3 months to 1 year after hospitalization. Among the patients studied, those with advanced age and higher New York Heart Association (NYHA) class experienced higher mortality and readmission rates during the 12 months of the study.14
In their study assessing the relationship between depressive symptoms and long-term mortality, Jiang and colleagues19 reported the following subgroup analysis from 1,006 hospitalized patients with HF: 302 patients (30%) scored 10 or higher on the BDI and were classified as depressed. These patients were significantly younger, less likely to be married, and were NYHA class II or greater. During the follow-up period, 428 patients died, representing 53% of the depressed patients.19
Gottlieb and colleagues13 conducted one of the first studies that assessed the influence of sex, race, NYHA classification, and age on the frequency of depression in 155 outpatients with HF. One hundred twenty-two patients (79%) were men, and 33 patients (21%) were women. Using the BDI measurement, nearly half (n = 75, 48%) of the patients scored as being depressed. Women with HF were more likely (64%) to score depressed than men (44%) (P = .048). There were slightly more African American patients (n = 89, 57%) than white patients (n = 65, 42%). No significant difference in the frequency of depression was found between the African American patients (n = 40, 53%) and the white patients (n = 35, 47%) (P = .275). There was no difference in depression prevalence among those who lived alone and those who did not live alone. More than half of the patients (68%) were NYHA class III. Patients ranged in age from 33 to 85 years (mean [SD], 64 [12] years). Patients scoring as depressed tended to be younger than nondepressed patients (t = 1.69, P = .086).13
In their study on gender differences in the link between depression and cardiovascular disease, Naqvi and colleagues20 reported that the prevalence of depression is 2 times higher in women than in men. The authors cited the biologic factor of fluctuating hormonal levels and psychosocial factors as contributing to these gender differences. The results from a study of 471 patients with end-stage HF conducted by Adams and colleagues21 showed a significant association between female gender and better survival (P < 0.001). The authors reported that biological differences were an important basis for the survival difference.
In their study of depression and the risk of HF among the elderly, Williams and colleagues11 examined the effect of depression with the Center for Epidemiological Studies Depression Scale in a community sample of 2,812 persons aged 65 years or older. The authors reported that depression was an independent risk factor for HF among elderly women and not elderly men.
Havranek and colleagues15 identified 4 independent predictors associated with the development of depressive symptoms among 245 outpatients with HF, as measured by the Medical Outcomes Study-Depression tool: (1) living alone, (2) alcohol abuse, (3) perceived financial burden from medical care, and (4) worse baseline HF-specific health status as measured by the Kansas City Cardiomyopathy Questionnaire. Patients who developed depressive symptoms at 1-year follow-up were more likely to live alone (40% vs 23%, P = .015), have a history of alcohol abuse (23% vs 11%, P = .013), and perceive medical care as an economic burden (60% vs 34%, P = .003). Mean (SD) Kansas City Cardiomyopathy Questionnaire summary scores of 60 (23) versus 71 (20) were worse in patients who developed significant depressive symptoms at 1 year (P < 0.001). For patients with 1, 2, and 3 risk factors, the incidence of significant depressive symptoms at 1 year was 16%, 36%, and 69%, respectively. There were no significant differences between the patients who developed depressive symptoms and the patients who did not with regard to age, race, or marital status.15
Gottlieb and colleagues13 reported that the frequency of depression differed significantly according to NYHA class. Patients classified as NYHA class III and IV were more likely to be depressed than class II patients, but class III and IV patients did not differ from each other in frequency of depression.13 In their meta-analysis, Rutledge and colleagues2 analyzed the prevalence rates for depression by NYHA class and found an aggregated estimate of 28% (P < 0.001). Higher prevalence rates were associated with worse NYHA class. The rate of depression in patients with class III was nearly double that of patients with class II.2
Freedland and colleagues22 conducted one of the first published studies to examine the prevalence of depression in patients with HF that was not limited to elderly patients. They reported the prevalence of depression in a sample of 682 hospitalized patients with HF. Fifty-five percent of the patients scored above the cutoff for depression (10 or higher) on the BDI. The prevalence of depression differed significantly between strata defined by the functional severity of HF, age, sex, employment status, dependence in activities of daily living, and history of major depression. The authors concluded that the prevalence of depression was considerably higher in certain subgroups of patients with HF, with the 2 strongest independent correlates being higher functional impairment (as measured by the NYHA class) and younger age (younger than 60 years vs 60 years or older).22
More information is needed regarding the differences in depressive symptoms across the sociodemographic subgroups in patients with HF.2 Awareness of these characteristics may help researchers design studies with greater precision in answering specific research questions. With the added knowledge produced from this research, clinicians may be better equipped to provide individualized and specialized treatment with regard to the unique clinical complexion of the sociodemographic subgroups. Therefore, the purpose of this study was to determine the differences in depressive symptoms among subgroups of a sample of HF patients. These subgroups included women and men, African American and white patients, married and unmarried patients, patients living alone and with a support person, patients with varying HF severity, and younger and older patients.
Research Questions
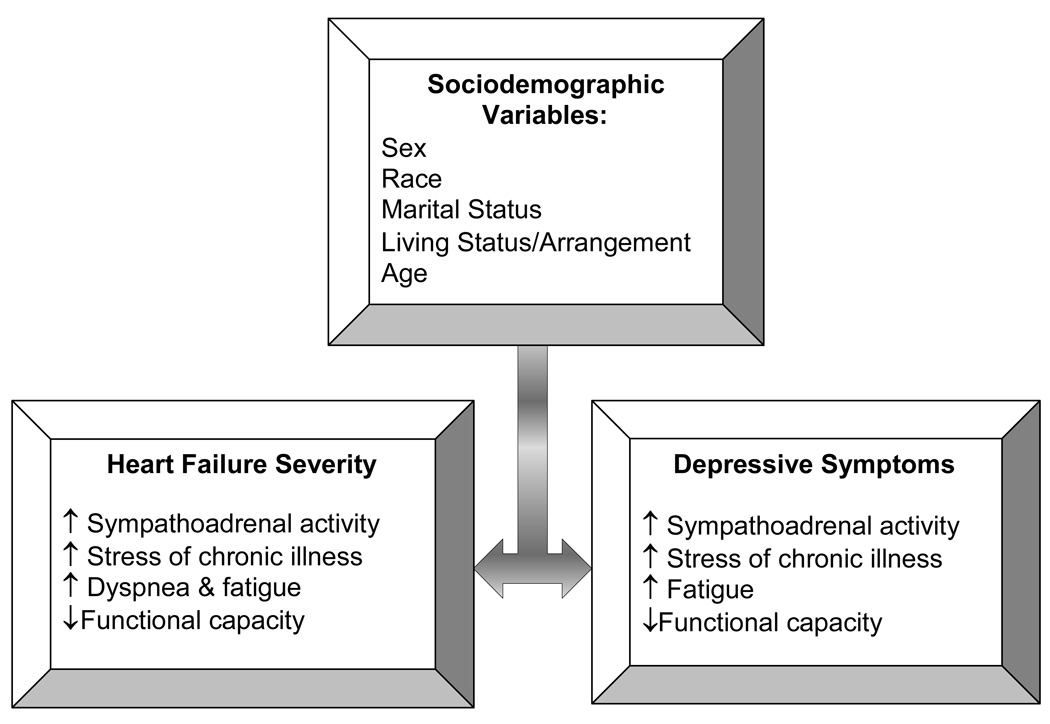
The following research questions were proposed in this study: (1) Are there differences in depressive symptoms between women and men with HF? (2) Are there differences in depressive symptoms between African American patients and white patients with HF? (3) Are there differences in depressive symptoms between married and unmarried patients with HF? (4) Are there differences in depressive symptoms based on living arrangements/status of patients with HF (HF patients living alone or living with support person)? (5) Are there differences in depressive symptoms among the 4 classes (I-IV) of NYHA HF severity? (6) Is age correlated with depressive symptoms? (7) What are the most frequently reported depressive symptoms? (8) What are the most frequently reported depressive symptoms reported by the patients with HF who scored high on the Patient Health Questionnaire 8 (PHQ-8) self-administered depression scale? The relationships between HF and the selected sociodemographic variables for this study are depicted in Figure 1.
Figure 1.
Schematic representation of heart failure, depressive symptoms, and sociodemographic variables. Worsening depressive symptoms may potentially have a negative impact on heart failure severity, with a reciprocal negative impact on depressive symptoms.
Methods
Procedure
This study used a descriptive, cross-sectional design. The study was approved by the institutional review boards of the university and study sites. Patients were enrolled from 5 clinics in the Midwest. All participants provided written informed consent before face-to-face interviews.
Sample
Eligible patients were adults 21 years or older. Patients must have (1) been able to understand English, (2) been able to hear normal conversation, (3) access to a working telephone, and (4) a current medical diagnosis of chronic HF with left ventricular systolic dysfunction validated by echocardiography or nuclear imaging.23 An analysis was conducted with data obtained from the first 150 HF patients who participated in the parent research study entitled “Cognitive Deficits in Chronic Heart Failure.”
Measures
Depressive symptoms were measured using the PHQ-8.24 The items on the PHQ-8 were developed based on the criteria for depression listed in the Diagnostic and Statistical Manual Fourth Edition.25 The questionnaire contains 8 items on which the individual ranked how often he or she was bothered by the problem (0 = “not at all,” 1 = “several days,” 2 = “more than half the days,” and 3 = “nearly every day”). A total score was calculated by summing the 8 items. Scores equal to or greater than 10 indicate a likelihood of depression and the need for clinical assessment.24
Heart failure severity was measured by the NYHA classification.26 This scale is commonly used to quantify the degree of functional limitation imposed by HF.27 Patients are assigned to 1 of 4 classes, depending on the degree of effort needed to elicit symptoms. Patients may have symptoms of HF at rest (class IV), during less than routine activities (class III), during ordinary activity (class II), or only during activities that would limit normal individuals (class I).27 Sociodemographic variables (sex, race, marital status, living arrangements, and age) were obtained by self report during the face-to-face interviews.
Statistical Analyses
A secondary analysis was performed on the data from the first 150 patients enrolled in the parent study. Descriptive statistics were computed for all variables. Internal consistency reliability of the PHQ-8 was estimated with the Cronbach α at 0.83. Differences in the depressive symptoms mean scores between women and men with HF were assessed with the Student t test, as were the differences between African American patients and white patients with HF, between married and unmarried patients with HF, and between patients living alone and those living with a support person. The differences in depressive symptoms scores among the 4 classes (I-IV) of NYHA classification were assessed by analysis of variance. Significance levels were set at P < .05.
Pearson correlations were computed to analyze the relationship between age and depressive symptoms. Differences in sex, NYHA class, and marital status between HF patients with high depressive symptoms scores (10 or higher) and HF patients with low depressive symptoms scores were analyzed with Student t test and analysis of variance. Frequency analyses were performed on the most frequently reported depressive symptoms by HF patients who completed the PHQ-8 depression scale and by HF patients who scored high on the PHQ-8 depression scale.
Results
A description of the sociodemographic and clinical variables for this sample is provided in Table 1. The sample included 150 patients: 88 (59%) men and 62 (41%) women; 47 (31%) African American patients, 101 (67%) white patients, and 2 (2%) Asian patients. Fifty-one percent of the patients were married (n = 77) and 49% of the patients were not married (n = 73); 108 patients (72%) were living with family or friends, and 42 patients (28%) were living alone. Fifteen percent of the patients were NYHA class I (n = 23), 27% of the patients were NYHA class II (n = 40), 47% of the patients were NYHA class III (n = 71), and 11% of the patients were NYHA class IV (n = 16). The mean age of the sample was 61.3 years (Table 1).
Table 1.
Sociodemographic variables (n = 150)
| Variables | N | PHQ-8 Mean Score | t-Test | P |
|---|---|---|---|---|
| Age | ||||
| Mean (SD) | 61.3 (15.0) | |||
| Range | 20 – 93 | |||
| Sex | ||||
| Men (SD) | 88 | 6.1 (5.4) | ||
| Women (SD) | 62 | 7.8 (5.6) | 1.82 | 0.07 |
| Race* | ||||
| African American (SD) | 47 | 7.5 (5.9) | ||
| White (SD) | 101 | 6.5 (5.4) | 1.06 | 0.290 |
| Marital Status | ||||
| Married (SD) | 77 | 6.2 (4.9) | ||
| Not Married (SD) | 73 | 7.4 (6.1) | 1.41 | 0.160 |
| Living Arrangement | ||||
| Living Alone (SD) | 42 | 7.6 (6.1) | ||
| Not Living Alone (SD) | 108 | 6.5 (5.3) | 1.11 | 0.270 |
Data from Asian patients (n = 2) excluded from race analysis due to low numbers
The PHQ-8 mean (SD) depressive symptoms score for this sample was 6.77 (5.52). Forty-two patients (28%) had scores equal to or greater than 10, suggesting the need for clinical evaluation. There were no statistically significant differences in depressive symptoms between women and men (t = 1.82, P = .07), African American and white patients (t = 1.06, P = .29), married and unmarried patients (t = 1.41, P = .16), or patients living alone and living with family or friends (t = 1.11, P = .27) (Table 1).
Patients with worse NYHA class reported significantly more depressive symptoms (F = 16.3, P < .0001). The patients with NYHA class III and IV had more depressive symptoms compared with patients with NYHA class I and II (Tukey-Kramer = I < III and IV; II < III and IV) (Table 2). A significant inverse correlation was found between depressive symptoms and age. Younger patients reported more depressive symptoms than the older patients (r = −0.30, P = .0002).
Table 2.
Differences in PHQ-8 Total Scores Among NYHA Classes
| NYHA Class | N | Mean (SD) | F | P | Tukey-Kramer |
|---|---|---|---|---|---|
| I | 23 | 2.7 (1) | 16.3 | < .0001 | I < III and IV |
| II | 40 | 4.2 (0.8) | II < III and IV | ||
| III | 71 | 8.7 (0.6) | |||
| IV | 16 | 10.6 (1.2) |
On a scale of 0 (not at all) to 3 (nearly every day), the most frequently reported depressive symptom was “feeling tired/no energy,” with 47 (31%) patients reporting a score of 3 (nearly every day) (mean = 1.5). The next most frequently reported depressive symptom was “trouble falling or staying asleep,” with 29 (19%) patients reporting a score of 3 (mean = 1.1). The most frequently reported depressive symptom reported by the patients who scored high on the PHQ-8 (10 or higher) (n = 42) was “feeling tired/no energy,” with 29 (69%) patients reporting a score of 3 (mean = 2.6). The next most frequently reported depressive symptom was “trouble falling or staying asleep,” with 20 (43%) patients reporting a score of 3 (mean = 2.0).
Discussion
The purpose of this study was to examine the sociodemographic factors associated with depressive symptoms among patients with HF. The most significant findings from the present study demonstrate the following: (1) patients with higher HF severity as assessed by worse NYHA class had more depressive symptoms; (2) younger age was significantly associated with more depressive symptoms; and (3) the most frequently reported depressive symptom was “feeling tired/no energy,” with the next most frequently reported depressive symptom being “trouble falling or staying asleep.” The women had higher depressive symptoms scores on average than men, although they were not significantly different.
The findings from this study were consistent with previous research, indicating that the patients with higher HF severity experience more depressive symptoms.2,13,14,22 One potential etiology of the elevated prevalence of depressive symptoms in patients with HF may be due to a shared pathophysiology.28,29 Lesperance and Frasure-Smith30 hypothesized that the 2 conditions may co-occur because of a common pathophysiological mechanism. A link between depressive symptoms and the course of HF may be expected because depressed individuals have elevated sympathoadrenal activation.10
According to Rutledge and colleagues2 and Abramson and colleagues,12 depression has been linked to excessive activation of the sympathetic nervous system. This increased activation is also significantly involved in the pathogenesis of HF.23 Depression-induced sympathetic activation could represent a shared pathway for the development and progression of coexisting HF. This association would give credence to further investigation of the biological role of depression in cardiac disease. In their review of underlying pathophysiological mechanisms and genetic contribution to depression and cardiac disease, McCaffery and colleagues31 present evidence in support of a genetic vulnerability that is common to both depressive symptoms and cardiac disease.
The findings from this study were also consistent with previous research demonstrating that depressive symptoms are negatively correlated with age.13,19,20,22 One possible explanation as to why younger patients with HF report more depressive symptoms may be due to the number of stressors in their lives. Younger persons may be managing family and work issues. In addition, research has shown that coping strategies change with age, becoming more effective and realistic as people mature.32
In a study evaluating coping styles and depressive symptoms among 75 adults with HF (aged 27–82 years; mean age, 55 years), the problem-focused coping strategies had a direct, negative relationship with depressive symptoms (r = −0.27, P = .02), and emotion-focused coping strategies (escape-avoidance) had a direct, positive relationship with depressive symptoms (r = 0.45; P < .001).33 Regression analysis revealed that single individuals with more functional impairment who used less problem-focused coping reported more depressive symptoms. These findings suggest that the ways individuals cope with the stressors of HF may contribute to depressive symptoms.
Although there were no statistically significant differences in depressive symptoms scores found between women and men in our sample, the difference was approaching significance. In previous research, women with HF were found to score significantly higher with depressive symptoms when compared with men.11,13,20,21 It is important to note that varying prevalence rates of depressive symptoms have been reported, in part, because of the instrument used to measure depressive symptoms. From the reviewed literature, the most common instrument used has been the BDI, which has demonstrated higher rates of depressive symptoms. The BDI provides a measure of the severity of symptoms based solely on a self-report inventory and is not based on actual criteria for the diagnosis of depression. The PHQ-8 may measure depressive symptoms more accurately since the items were developed based on the criteria for depression listed in the Diagnostic and Statistical Manual Fourth Edition. Therefore, a lower rate of depressive symptoms may have been reported in the current study when compared to previous studies. The use of the PHQ-8 is considered one of the strengths of the current study; however, more research is needed in this area.
The results for the marital status and living arrangement variables did not demonstrate significant differences in this study, which is consistent with some previous research. The findings from this study would not seem to support a strong relationship with the social variables studied. Rather, the nonsignificant findings from this study would more likely support the relationship with the biological pathophysiology of HF and depressive symptoms compared with the patient’s environment or social situation as contributing factors.
The depressive symptom of “feeling tired/no energy” was the most frequently reported symptom overall, with the second most frequently reported symptom of “trouble falling or staying asleep.” Previous research has reported that HF and depression share a constellation of symptoms, particularly fatigue.6,7 This overlap is important to consider when assessing HF patients’ fatigue levels. The HF and depressive symptoms may contribute to the fatigue experienced by patients, making it more severe and requiring the need for more intensive therapeutic interventions.
Limitations
A limitation of this study was the cross-sectional nature of the study, which only allows for data to be collected at one point in time and does not allow for inferences or changes over time. However, significant associations between depressive symptoms and HF severity and the prevalence among younger-aged patients within this time period were demonstrated in this study.
Implications for Advanced Practice Nurses
Currently, advanced practice nurses provide the majority of care to patients with HF in the nurse-managed models of care delivery, as evidenced in today’s outpatient specialty clinics. Given their autonomy and expertise in evidence-based practice and education-focused care, clinical nurse specialists are integral in facilitating the internal and external resources that patients with HF and depression require (ie, coping skills and support systems). By partnering with their patients, clinical nurse specialists are in the vital position of focusing on the clinical, educational, and supportive needs of HF patients and their caregivers.
The American Heart Association’s recent advisory on the screening, referral, and treatment of patients with depression and heart disease recommends, at a minimum, that an assessment of depressive symptoms be performed using versions of the Patient Health Questionnaire.34 Depressive symptoms must be recognized so that further comprehensive evaluation and treatment may be undertaken. Because of the high prevalence and untoward effects of depression in patients with HF, advanced practice nurses are best equipped to implement their specialized knowledge and skills in the identification and treatment of depression. To this end, the impact of advanced practice nurses within the HF population is enormous.
Strategies should focus predominantly on individualized patient assessment, enhanced patient-nurse communication, pharmacologic and nonpharmacologic interventions, self-management strategies, intensive patient/caregiver education regarding chronic illnesses and comorbid conditions, recognition of worsening symptoms, and resource allocation. Comprehensive nursing assessment should delineate specific constellations of HF signs and symptoms as well as the contribution of depression, and this practice should be included in HF education programs and treatment guidelines.35,36
Conclusion
In summary, the findings from the current study demonstrate that higher NYHA class and younger age were associated with more depressive symptoms. The most frequently reported depressive symptoms were “feeling tired/no energy” and “trouble falling or staying asleep.” For future research endeavors, longitudinal, biobehavioral studies are needed to investigate the relationships among biological factors (ie, overstimulation of the adrenergic system), depressive symptoms, and HF. Advanced practice nurses need to assess patients for depressive symptoms, and approaches need to be individually tailored to therapeutically address depressive symptoms in patients with HF. Depression is one of the most prevalent yet treatable mental health conditions presenting in clinic settings. Detecting depression, initiating treatment, and monitoring therapy are crucial actions necessary in improving clinical outcomes and reducing medical costs in patients with HF.24
Acknowledgements
National Institute of Nursing Research RO1 NR008147. Permission to acknowledge the coinvestigators for the study “Cognitive Deficits in Chronic Heart Failure” was obtained: Irmina Gradus-Pizlo, MD; David Kareken, PhD; JinShil Kim, RN, PhD; Susan M. Perkins, PhD; Mary Jane Sauve, RN, PhD; R. Sloan, RN, PhD; and Usha Subramanian, MD.
Biographies
Linda M. Rohyans, R.N., B.S.N.: Indiana University School of Nursing, Indianapolis, IN. Currently a Graduate Student in the Clinical Nurse Specialist-Adult Health Program. Clinical experience: Congestive heart failure; Clinical Research Coordinator. Clinical research interests: heart failure; exercise physiology. Cardiac Stress Testing Nursing Supervisor, Cardiac Stress Testing Laboratory, Krannert Institute of Cardiology, Indianapolis, IN.
Susan J. Pressler, RN, DNS, FAAN, FAHA, Professor of Nursing. Dr. Pressler has an ongoing research program focused on patient problems that diminish quality of life in heart failure. She is the principal investigator for a study about cognitive deficits and quality of life in heart failure (NIH NR008147).
Contributor Information
Linda M. Rohyans, MPC-2 Building, Suite 4000, 1801 N. Senate Boulevard, Indianapolis, IN 46202; telephone (317) 962-0519; email lrohyans@iupui.edu; Staff Nurse, Cardiac Stress Testing Laboratory, Krannert Institute of Cardiology, Indiana University School of Nursing, Indianapolis, IN.
Susan J. Pressler, University of Michigan School of Nursing, 400 N. Ingalls, Ann Arbor, MI 48109; telephone (734) 763-5650; fax (734) 936-5525; email spressle@umich.edu; School of Nursing Faculty Member..
References
- 1.American Heart Association. Heart disease and stroke statistics – 2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007:e119–e121. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 2.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure. A meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48(8):1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 3.Klein DM, Turvey CL, Pies CJ. Relationship of coping styles with quality of life and depressive symptoms in older heart failure patients. J Aging Health. 2007;19(1):22–38. doi: 10.1177/0898264306296398. [DOI] [PubMed] [Google Scholar]
- 4.Adams KF, Lindenfeld J, Arnold JM, et al. HFSA 2006 comprehensive heart failure practice guideline. J Card Failure. 2006;12:e1–e122. doi: 10.1016/j.cardfail.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Rumsfeld JS, Havranek E, Masoudi FA, et al. Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol. 2003;42:1811–1817. doi: 10.1016/j.jacc.2003.07.013. [DOI] [PubMed] [Google Scholar]
- 6.Grippo AJ, Johnson AK. Biological mechanisms in the relationship between depression and heart disease. Neurosci Biobehav Rev. 2002;26:941–962. doi: 10.1016/s0149-7634(03)00003-4. [DOI] [PubMed] [Google Scholar]
- 7.Havranek EP, Ware MG, Lowes BD. Prevalence of depression in congestive heart failure. Am J Cardiol. 1999;84:348–350. doi: 10.1016/s0002-9149(99)00293-3. [DOI] [PubMed] [Google Scholar]
- 8.Noel PH, Williams JW, Jr, Unutzer J, et al. Depression and comorbid illness in elderly primary care patients: Impact on multiple domains of health status and well-being. Ann Fam Med. 2004;2:555–562. doi: 10.1370/afm.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pasic J, Levy WC, Sullivan MD. Cytokines in depression and heart failure. Psychosom Med. 2003;65:181–193. doi: 10.1097/01.psy.0000058372.50240.38. [DOI] [PubMed] [Google Scholar]
- 10.Vaccarino V, Kasl SV, Abramson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol. 2001;38:199–205. doi: 10.1016/s0735-1097(01)01334-1. [DOI] [PubMed] [Google Scholar]
- 11.Williams SA, Kasl SV, Heiat A, Abramson JL, Krumholz HM, Vaccarino V. Depression and risk of heart failure among the elderly: A prospective community-based study. Psychosom Med. 2002;64:6–12. doi: 10.1097/00006842-200201000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Abramson J, Berger A, Krumholz HM, Vaccarino V. Depression and risk of heart failure among older persons with isolated systolic hypertension. Arch Intern Med. 2001;161:1725–1730. doi: 10.1001/archinte.161.14.1725. [DOI] [PubMed] [Google Scholar]
- 13.Gottlieb SS, Khatta M, Friedmann E, et al. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol. 2004;43(9):1542–1549. doi: 10.1016/j.jacc.2003.10.064. [DOI] [PubMed] [Google Scholar]
- 14.Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 15.Havranek EP, Spertus JA, Masoudi FA, Jones PG, Rumsfeld JS. Predictors of the onset of depressive symptoms in patients with heart failure. J Am Coll Cardiol. 2004;44:2333–2338. doi: 10.1016/j.jacc.2004.09.034. [DOI] [PubMed] [Google Scholar]
- 16.Murberg TA, Bru E, Svebak S, Tveteras R, Aarsland T. Depressed mood and subjective health symptoms as predictors of mortality in patients with congestive heart failure: a two-year follow-up study. Int J Psychiatry Med. 1999;29(3):311–326. doi: 10.2190/0C1C-A63U-V5XQ-1DAL. [DOI] [PubMed] [Google Scholar]
- 17.Sherwood A, Blumenthal JA, Trivedi R, et al. Relationship of depression to death or hospitalization in patients with heart failure. Arch Intern Med. 2007;167:367–373. doi: 10.1001/archinte.167.4.367. [DOI] [PubMed] [Google Scholar]
- 18.Jiang W, Kuchibhatla M, Cuffe MS, et al. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004;110:3452–3456. doi: 10.1161/01.CIR.0000148138.25157.F9. [DOI] [PubMed] [Google Scholar]
- 19.Jiang W, Kuchibhatla M, Clary GL, et al. Relationship between depressive symptoms and long-term mortality in patients with heart failure. Am Heart J. 2007;154:102–108. doi: 10.1016/j.ahj.2007.03.043. [DOI] [PubMed] [Google Scholar]
- 20.Naqvi TZ, Naqvi SS, Merz CN. Gender differences in the link between depression and cardiovascular disease. Psychosom Med. 2005;67(S1):15–18. doi: 10.1097/01.psy.0000164013.55453.05. [DOI] [PubMed] [Google Scholar]
- 21.Adams KF, Sueta CA, Gheorghiade M, et al. Gender differences in survival in advanced heart failure: Insights from the FIRST study. Circulation. 1999;99:1816–1821. doi: 10.1161/01.cir.99.14.1816. [DOI] [PubMed] [Google Scholar]
- 22.Freedland KE, Rich MW, Skala JA, Carney RM, Davila-Roman VG, Jaffe AS. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom Med. 2003;65:119–128. doi: 10.1097/01.psy.0000038938.67401.85. [DOI] [PubMed] [Google Scholar]
- 23.Zipes DP, Libby P, Bonow RO, Braunwald E. Braunwald’s Heart disease: A textbook of cardiovascular medicine. 7th ed. Philadelphia, PA: W.B. Saunders Company; 2005. pp. 509–538. [Google Scholar]
- 24.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(9):1–7. [Google Scholar]
- 25.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: R.R. Donnelley & Sons Company; 2000. [Google Scholar]
- 26.New York Heart Association Criteria Committee. Disease of the heart and blood vessels: Nomenclature and criteria for diagnosis. 6th ed. Boston, MA: Little, Brown & Co; 1964. [Google Scholar]
- 27.Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 Guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2005;112:e154–e235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 28.Doering LV, Cross R, Vredevoe D, Martinez-Maza O, Cowan MJ. Infection, depression, and immunity in women after coronary artery bypass: A pilot study of cognitive behavioral therapy. Altern Ther Health Med. 2007;13(3):18–21. [PubMed] [Google Scholar]
- 29.Joynt KE, Whellan DJ, O’Connor CM. Why is depression bad for the failing heart? A review of the mechanistic relationship between depression and heart failure. J Card Failure. 2004;10(3):258–271. doi: 10.1016/j.cardfail.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 30.Lesperance F, Frasure-Smith N. The seduction of death. Psychosom Med. 1999;61:18–20. doi: 10.1097/00006842-199901000-00004. [DOI] [PubMed] [Google Scholar]
- 31.McCaffery JM, Frasure-Smith N, Dube M, et al. Common genetic vulnerability to depressive symptoms and coronary artery disease: A review and development of candidate genes related to inflammation and serotonin. Psychosom Med. 2006;68:187–200. doi: 10.1097/01.psy.0000208630.79271.a0. [DOI] [PubMed] [Google Scholar]
- 32.Lazarus RS, Folkman S. Stress, appraisal and coping. New York, NY: Springer Publishing, Inc; 1984. [Google Scholar]
- 33.Vollman MW, LaMontagne LL, Hepworth JT. Coping and depressive symptoms in adults living with heart failure. J Cardiovasc Nurs. 2007;22(2):125–130. doi: 10.1097/00005082-200703000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Lichtman JH, Bigger JT, Blumenthal JA, et al. Depression and coronary heart disease. Recommendations for screening, referral, and treatment. A science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research. Circulation. 2008;118:1–8. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 35.Johansson P, Dahlstrom U, Brostrom A. Consequences and predictors of depression in patients with chronic heart failure: Implications for nursing care and future research. Prog Cardiovasc Nurs. 2006;21:202–211. doi: 10.1111/j.0889-7204.2006.05415.x. [DOI] [PubMed] [Google Scholar]
- 36.McCauley KM, Bixby MB, Naylor MD. Advanced practice nurse strategies to improve outcomes and reduce cost in elders with heart failure. Disease Management. 2006;9:302–310. doi: 10.1089/dis.2006.9.302. [DOI] [PubMed] [Google Scholar]