Abstract
Introduction
Maternal medical care (prenatal and postpartum) involves a set of clinical interventions addressing risk factors associated with important maternal and infant outcomes. Programs to increase the rate of delivery of these interventions in clinical practice have not been widely implemented.
Setting
A practice based research network (PBRN) focused on developing continuous quality improvement (CQI) processes for maternal care among 10 Family Medicine Residency Training sites in the Northeast region of the US (the IMPLICIT Network) from January 2003-September 2007.
Outcomes
Documented delivery of five standard maternal care interventions was assessed before and after initiating a program to increase their frequency. P chart analyses was carried out comparing the period preceding and following implementation of the CQI interventions.
Results
Data were available for 3,936 pregnancies over the course of the study period. Results varied across the clinical interventions. Significant improvement in care processes was seen for three screening activities: prenatal depression symptomatology (by 15 weeks gestation), screening for smoking at 30 weeks gestation, and postpartum contraception planning. Screening for smoking by 15 weeks gestation and testing for asymptomatic bacteriuria were already carried out >90% of the time in the baseline period and did not increase significantly after initiating the CQI program. Screening for postpartum depression symptomatology was recorded in 50-60% of women prior to the CQI program and did not increase significantly.
Conclusions
A practice based research network of family medicine residency practices focused on CQI outcomes was successful in increasing the delivery of some maternal care interventions.
Introduction
Maternal medical care (prenatal and postpartum) in the United States involves a series of well defined interventions that aim to reduce the risk of poor maternal-infant outcomes [1]. While the efficacy of prenatal care as a whole to reduce the risk of some outcomes is unclear, the components of maternal care are justified because of potential benefits to the woman and her child [2, 3]. Despite recommendations and supporting evidence for a range of maternal interventions little research has been carried out to assess the consistency with which these interventions are carried out in clinical care.
Continuous quality improvement (CQI) programs have the potential to increase consistent delivery of standard clinical practices [4]. CQI is a method of continuously examining processes and making them more effective which has been successful in increasing the use of preventive services in areas outside of prenatal care [5-8]. CQI, through audit and feedback techniques, has also been shown to be effective in managing cardiac, diabetes and other health outcomes [9-11].
The goal of this paper is to describe a collaboration of family medicine residency programs (the IMPLICIT network) to improve the rate of delivery of maternal care interventions covering a range of domains; smoking cessation, asymptomatic bacteriuria, depressive symptomatology, and postpartum contraception planning. Using baseline service delivery data and prospective data collected after the implementation of a multi-site CQI program we assess the effect of this program to increase the rates of delivery of these interventions.
Methods
Setting
Ten family medicine residency clinical sites of the IMPLICIT practice based research network were included in the current report (Table 1) [12]. These programs were selected because they participated continuously in data collection over the study period (January 2003 - December 2007). We adopted the name IMPLICIT (Interventions to Minimize Preterm and Low birth weight Infants through Continuous Improvement Techniques) to describe our focus on reducing risk for poor maternal and infant outcomes. A total of 117 faculty physicians and 342 family medicine residents staffed these participating sites. Ongoing collaboration, CQI development, as well as clinical updates are done through monthly conference calls and semi-annual meetings. Site and evidence leaders as well as nursing staff and residents attend these meetings. The Family Medicine Education Consortium hosts a web site (www.fmec.net) for communication and housing documents.
Table 1.
IMPLICIT Network Sites and study participants
| Location | Participants n = 3,936 |
City | State |
|---|---|---|---|
| Beth Israel Family Medicine Residency | 184 | New York | NY |
| Chestnut Hill Family Medicine Residency | 275 | Philadelphia | PA |
| Forbes Family Medicine Residency | 290 | Monroeville | PA |
| Good Sam Hosp. Family Medicine Residency | 371 | Lebanon | PA |
| Lancaster General Hospital Family Medicine Residency | 609 | Lancaster | PA |
| UPMC-McKeesport Family Medicine Residency | 487 | McKeesport | PA |
| UPMC-Shadyside Family Medicine Residency | 491 | Pittsburgh | PA |
| UPMC-St. Margaret Family Medicine Residency | 407 | Pittsburgh | PA |
| Wellspan | 326 | York | PA |
| Williamsport Family Medicine Residency | 496 | Williamsport | PA |
Development of Practice Guidelines
Specific maternal care interventions were selected based on an evidence review process involving independent IMPLICIT working groups. Evidence-based reviews of potential interventions were developed for which there was epidemiologic or clinical evidence for association with risk of preterm birth or low birth weight (PTB/LBW). Reviews were circulated and discussed via teleconference and collaboratively refined. “Evidence leaders” were charged with writing the final guideline for group presentation. Selection of a preventive practice was decided by consensus of participant site leaders at semi-annual meetings. The network initially chose focus areas which include the five for which data is presented: smoking, asymptomatic bacteriuria, bacterial vaginosis (for women with history of preterm birth), inter-pregnancy interval, and depression (Tables 1 and 2). These areas were chosen based on the level of evidence for association with PTB/LBW, the feasibility of implementation, and the availability of recommended treatments.
Table 2.
Characteristics of women in study.
| All Sites (n=3936) | |
|---|---|
| Mean Maternal Age (years) | 24.10 |
| Mean Gestational Age (weeks) | 38.7 |
| Medicaid Insurance | 77% |
| Race/Ethnicity | |
| White | 49% |
| Black | 34% |
| Latina | 15% |
| Pre Term Birth Rate | 11% |
| C-section Rate | 21% |
Evidence-based reviews are available to network members on the web site and include a summary of the evidence, references, and recommendations for or against inclusion in the project. Guidelines for the CQI program implementation and specific data collection instruments for the retrospective (pre-intervention) and prospective (post intervention) periods were also provided. New areas of focus and updated protocols are reviewed over time by evidence leaders and working groups comprised of representatives from all participating programs.
Study Design
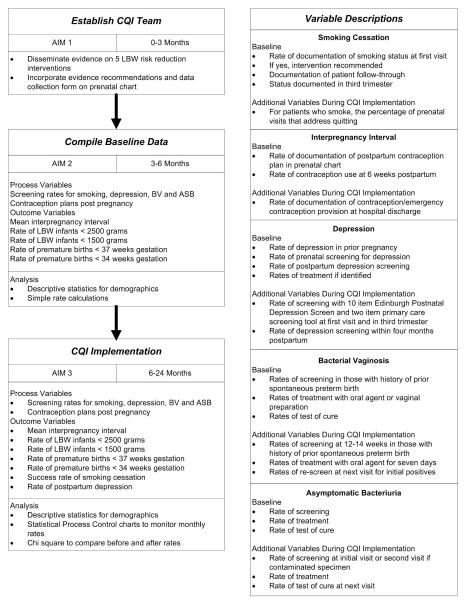
All residency sites were involved in continual attempts to increase and maintain preventive practices that improved rates of care delivery. No randomization or control group was employed. The CQI model required that an aim be identified (increased rate of intervention delivery documentation), which was the criteria for judging whether improvements were made (preventive practice rates improved over time compared to baseline rates), and whether the intended changes took place (incorporation of prevention guidelines) [13]. The conceptual model and study overview are represented in Figure 1. IMPLICIT implementation teams at each site were composed of faculty, resident, nursing, and ancillary staff. Each site implemented practice improvement activities appropriate to that site through dissemination of evidence-based recommendations and continuous feedback on rates of documentation of the interventions among pregnant patients. Audit/feedback was achieved through chart reviews for feedback at 15 and 30 weeks gestation and postpartum. Site-specific feedback/reminder forms were left in the chart to be addressed, if necessary, at the next visit. Success or lack thereof was presented at regular site-specific CQI meetings, and problems or successes were discussed during monthly teleconferences and semi-annual day-long conferences with network clinicians.
Figure 1.
Study Overview and Conceptual Model for Continuous Quality Improvement Program of Maternal Care Delivery
Data Collection
All participating sites received approval from their respective Institutional Review Boards. A unique site and patient code was assigned to each record. Data were collected for live births occurring during the period of January 1, 2003 through September 31, 2004. Data were obtained from chart review, either paper or electronic, using a standardized data abstraction tool and then entered, after being de-identified, into an internet-based centralized database. Faculty and residents carried out data abstraction at most sites. Volunteer pre-med or med students were included at other sites under the supervision of IMPLICIT lead faculty. Sites utilized random sampling of charts at regular intervals to ensure data quality.
Demographic data elements included age, race, and insurance status; the birth outcomes of gestational age, birth weight, and vaginal or cesarean birth were also recorded. The PTB rate was calculated as the percentage of babies born at <37 weeks gestation divided by the total number of deliveries, after excluding all multiple gestation deliveries (1.9%) from the data set. The main outcome variables were documentation of provider behavior around the five maternal care focus areas (Figure 1). These outcome variables were as follows: 1) promotion of prenatal smoking cessation (≤15 and ≤ 30 weeks gestation), 2) screening for prenatal (≤15 weeks gestation) and postpartum (≤16 weeks postpartum) depressive symptomatology, 3) contraception planning by 30 weeks gestation, 4) screening for bacterial vaginosis in women with a history of previous spontaneous preterm birth, and 5) screening for asymptomatic bacteriuria.
Statistical Analysis
Baseline data was analyzed as descriptive statistics for demographic variables. The computer program STATA Intercooled, version 8.2 was used for these computations. Statistical process control (SPC) chart analysis was used to assess the statistical significance of changes in the delivery of preventive behaviors before and after the implementation of the CQI program. Two quarters in the period of CQI implementation were excluded from analysis because of heterogeneity of implementation of this program. Data from the 8 quarters preceding and 8 quarters following the CQI implementation period were used for the SPC analysis. SPC chart analysis is a strategy and a set of methods for the ongoing improvement of systems, processes, and outcomes with recent applications in healthcare [14]. SPC chart analysis assesses whether a process has changed over time beyond the normal random variation. Rather than determining a p value, as in standard statistical tests, the analysis employs sigma levels which are similar to a standard deviation measurement. Generally, a process is considered changed when it’s deviated by three sigma levels, or having a 99% probability of being different from the baseline. Discrete outcomes, i.e., provider behavior rates, were analyzed with proportions charts, or p-charts, and adjusted for demographic variables with confidence intervals representing three sigma level variation from pre-CQI rates. SPC chart analysis was performed with Minitab®, version 15.
Results
Sample Characteristics
A total of 3,936 women were included in the current analysis. The description of the study sample is included in Table 1. Overall the sample was comprised primarily of young, low income women with demographic characteristics consistent with that setting. The mean age of the participants was approximately 24 years, with mean gestational age of approximately 39 weeks, nearly 80% with Medicaid insurance, and approximately 50% were white. The PTB rate is consistent with the risk factor mix of this study sample and cesarean section rate was within the range seen nationally.
SPC Analysis
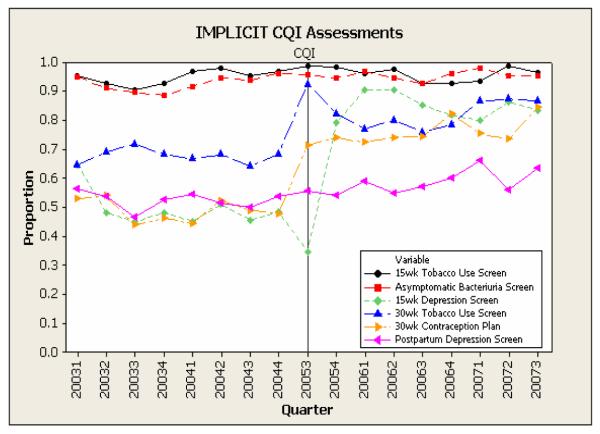
Rates of documented delivery of the targeted maternal care interventions is represented for the full study period in Figure 2. Because of the low prevalence of history of preterm birth, screening for bacterial vaginosis did not provide a stable estimate and so was not included. As can be seen from this P chart representation, there were three primary patterns of delivery of the targeted maternal care services over the study period: 1) high rates of baseline adherence to care recommendations which remains high after initiation of the CQI program (smoking screening ≤15 weeks gestation, and screening for asymptomatic bacteriuria); 2) low rates of baseline adherence with an increase after initiation of the CQI program (prenatal depressive symptomatology screening ≤15 weeks gestation, tobacco use screening at 30 weeks, and contraception plan by 30 weeks of pregnancy); and 3) low rates of baseline adherence which is present also after initiation of the CQI program (postpartum depressive symptomatology screening).
Figure 2.
Proportion of study participants per yearly quarter with documentation of specific prenatal interventions
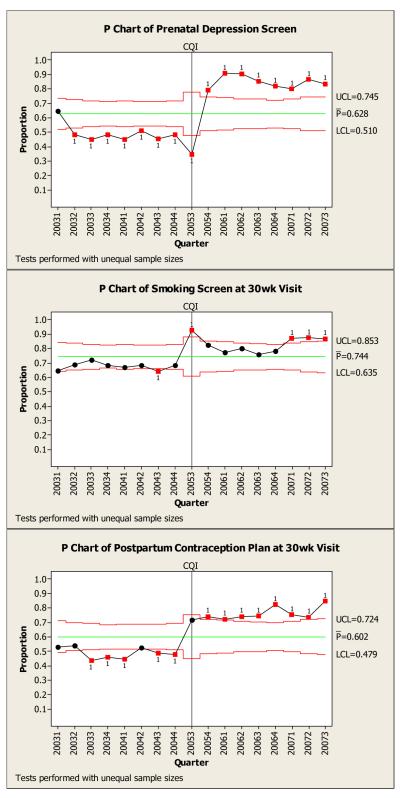
In Figure 3, the P charts with confidence intervals are shown for the three interventions showing increases in rates of intervention delivery following initiation of the CQI program. In each case there is a significant increase in these rates although for the repeat smoking screening (30 weeks gestation) the increase is only seen in the last three quarters of the study period. For prenatal depressive symptomatology screening and contraception planning there was an increase that was sustained throughout the study period.
Figure 3.
P charts of smoking cessation screening, contraception planning, and depression screening.
Discussion
The purpose of this article was to describe a continuous quality improvement project in a family medicine residency practice based research network to improve the rates of delivery of several recommended maternal care interventions. We found that there was evidence for a range of effects of this intervention on provider behaviors. Interventions with high rates of adherence in the baseline phase of the study (90+%) did not increase significantly following the initiation of the intervention probably reflecting a ceiling effect for these interventions. Three interventions were initially low and had significant increases following the initiation of the CQI program. These interventions span three distinct domains of maternal health (emotional distress, smoking cessation, and contraception planning) suggesting that the CQI approach can be effective across thematic areas within maternal care. Interestingly screening for postpartum depressive symptomatology had low initial rates of delivery and which did not increase following the CQI program suggesting that additional attention must be paid to this intervention.
The differences identified in care delivery rates could in part be explained by how well established a certain practice is. For instance, screening for asymptomatic bacteriuria has an “A” level recommendation from the US Preventive Health Service Panel and has long been part of prenatal care. However smoking cessation interventions generally focus only on the initial prenatal period despite the fact that portions of women who smoke in early pregnancy continue through gestation [15]. Given this fact it was hopeful to see that the CQI intervention was able (though not initially) to modify provider behavior and increase screening for smoking late in pregnancy. Depressive symptomatology screening has only recently been widely recommended in the maternal care setting and is complicated by issues of treatment options during pregnancy [16]. Interestingly we found an increase in prenatal but not in postpartum screening suggesting that additional efforts are needed in the later period.
The data presented here expose the limitations of our perinatal care routines and point the way to areas of improvement. This is exactly why the CQI phase of this project has the potential to be successful in increasing rates of maternal care delivery. Through continual feedback on our performance and re-engineering of care processes through stakeholder discussions, we believe there is potential to improve perinatal care.
This study has several limitations; foremost of which is the non-randomized design. We chose to include all network residency programs because of the nature of the CQI process. Also, although many aspects of the project are standardized, it is critical for the site teams to develop site-specific implementation processes and there was an inherent variability in this approach. However we believe that this is a critical component of the network as each site must deal with a unique context with distinct real life challenges that must be addressed. There is no “one size fits all” approach to overcoming obstacles to care delivery. This variability also provides an opportunity for innovation which is shared among members of the network. Data quality measures are also somewhat limited. Each site was asked to implement a random assessment of the accuracy of data submitted to the network and the details of these assessments varied from one site to another. Finally the generalizability of our findings is unknowm. The data are from family medicine residency programs; this may not reflect how prenatal care processes are carried out in private office or community health center sites. Further work is needed to determine if a similar approach can be successful in these settings. Despite these limitations we feel that this work provides important initial support for the use of a CQI approach to increase the rates of delivery of maternal care interventions.
Acknowledgements
Thanks to all of the contributing members of the IMPLICIT network as well as the support of Larry Bauer and the Family Medicine Educational Consortium (FMEC; www.fmec.net) for critical contributions and support which made this work possible.
Financial Support: This work was supported by a grant from the March of Dimes. Dr.Bennett was supported by grants from the NICHD (1K23HD048915-01A2) and the NIMH (1R03MH074750-01).
Footnotes
Portions of his work have been presented at the 2009 Society of Teachers of Family Medicine annual meeting, Denver Colorado.
Conflict of Interest: All of the authors declare no conflict of interest in this work.
References
- 1.Ratcliffe S, Baxley E, Byrd J, Sakornbut E, editors. Family Practice Obstetrics. 2ed Hanley & Belfus; 2001. [Google Scholar]
- 2.Alexander GR, Kotelchuck M. Assessing the role and effectiveness of prenatal care: history, challenges, and directions for future research. Public Health Rep. 2001;116:306–16. doi: 10.1016/S0033-3549(04)50052-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu MC, Tache V, Alexander GR, Kotelchuck M, Halfon N. Preventing low birth weight: is prenatal care the answer? Journal of Maternal-Fetal & Neonatal Medicine. 2003;13:362–80. doi: 10.1080/jmf.13.6.362.380. [DOI] [PubMed] [Google Scholar]
- 4.Atkins D, Clancy C. Multiple risk factors interventions: Are we up to the challenge? Am J Prev Med. 2004;27(2S) doi: 10.1016/j.amepre.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 5.Leshan LA, Fitzsimmons M, Marbella A, Gottlieb M. Increasing clinical prevention efforts in a family practice residency program through CQI methods. Jt Comm J Qual Improv. 1997;23(7):391–400. doi: 10.1016/s1070-3241(16)30327-3. [DOI] [PubMed] [Google Scholar]
- 6.Zazove P, Klinkman MS. Developing a CQI program in a family medicine department. Jt Comm J Qual Improv. 1998;24(8):391–406. doi: 10.1016/s1070-3241(16)30390-x. [DOI] [PubMed] [Google Scholar]
- 7.Ornstein SM, Jenkins RG, Lee FW, et al. The computer-based patient record as a CQI tool in a family medicine center. Jt Comm J Qual Improv. 1997;23(7):347–361. doi: 10.1016/s1070-3241(16)30324-8. [DOI] [PubMed] [Google Scholar]
- 8.Anctil B, Winters M. Linking customer judgments with process measures to improve access to ambulatory care. Jt Comm J Qual Improv. 1996;22(5):345–357. doi: 10.1016/s1070-3241(16)30238-3. [DOI] [PubMed] [Google Scholar]
- 9.O’Brien T, Oxman AD, Davis DA, Haynes RB, Freemantle N, Harvey EL. The Cochrane Library. Update Software; Oxford: 2003. Audit and feedback: effects on professional practice and health care outcomes (Cochrane Review) [DOI] [PubMed] [Google Scholar]
- 10.Ornstein S, Jenkins RG, Nietert PF, Feifer C, Roylance LF, Nemetn L, Corley S, et al. A multimethod quality improvement intervention to improve preventive cardiovascular care. Ann Intern Med. 2004;141:523–532. doi: 10.7326/0003-4819-141-7-200410050-00008. [DOI] [PubMed] [Google Scholar]
- 11.Kiefe CI, Allison JJ, Williams OD, Person SD, Weaver MT, Weissman NW. Improving quality improvement using achievable benchmarks for physician feedback: a randomized controlled trial. JAMA. 2001;285:2871–2879. doi: 10.1001/jama.285.22.2871. [DOI] [PubMed] [Google Scholar]
- 12.Bennett IM, Coco A, Coyne JC, Mitchell AJ, Nicholson J, Johnson E, et al. Efficiency of a two-item pre-screen to reduce the burden of depression screening in pregnancy and postpartum: An IMPLICIT network study. 2008. pp. 317–25. [DOI] [PMC free article] [PubMed]
- 13.Langley GJ, Nolan KM, Nolan TW, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. Jossey-Bass Publishers; San Francisco: 1996. [Google Scholar]
- 14.Woodall WH. The use of control charts in health-care and public-health surveillance. J Qual Tech. 2006;38:89–104. [Google Scholar]
- 15.Castrucci BC, Culhane JF, Chung EK, Bennett I, McCollum KF. Smoking in pregnancy: patient and provider risk reduction behavior. Journal of Public Health Management & Practice. 2006;12:68–76. doi: 10.1097/00124784-200601000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, et al. Evidence Report: Technology Assessment. Agency for Healthcare Research and Quality; Rockville: 2005. Perinatal depression: prevalence, screening accuracy, and screening outcomes; pp. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]