Abstract
Few studies have analyzed for-profit and nonprofit differences in the home health care sector. Using data from the National Home and Hospice Care Survey, we found that patients in nonprofit agencies were more likely to be discharged within 30 days under Medicare cost-based payment compared to patients in for-profit agencies. However, this difference in length of enrollment did not translate into meaningful differences in discharge outcomes between nonprofit and for-profit patients, suggesting that – under a cost-based payment system – nonprofits may behave more efficiently relative to for-profits. These results highlight the importance of organizational and payment factors in the delivery of home health care services.
Keywords: home health care, ownership, for-profit, nonprofit, discharge
An important feature of most health care markets in the United States is the dual presence of for-profit and nonprofit-owned providers. Unlike their for-profit counterparts, nonprofits cannot distribute accounting profits to individual equity holders, but they do enjoy several government-conferred advantages, including exemption from corporate income and property taxes. Given that nonprofits lack a defined shareholder, there may be less incentive for these firms to maximize profits and greater incentive to maximize other objectives such as the quality of care and provision of public goods (e.g., charity care) (Hansmann 1980; Newhouse 1970).
Researchers have generated a large empirical literature examining whether for-profit and nonprofit health care providers perform differently along a number of dimensions. For example, a recent review of the nursing home literature identified 38 studies on nonprofit and for-profit quality differences published over the period 1990 through 2002 (Hillmer et al. 2005). In contrast, few studies have analyzed for-profit and nonprofit differences in the home health care sector (Rosenau, and Linder 2001). This lack of recent research is somewhat surprising in the context of the tremendous growth of the home health care sector and the prominent role of for-profit agencies. Between 1980 and 2004, aggregate expenditures on home health care increased from $2.4 billion (0.9% of national health expenditures) to $43.2 billion (2.3%) (Smith et al. 2006). Around half of all home health agencies (52%) operate on a for-profit basis (Medicare Payment Advisory Commission 2004).
According to the 1994 through 2000 waves of the National Home and Hospice Care Survey (NHHCS), Medicare is the primary payer of home health care for nearly two-thirds of patients who receive services (Grabowski et al. 2006). Historically, agencies were paid by Medicare on the basis of their costs, up to pre-established per-visit limits. Under this system, agencies could enhance their revenues by providing a greater number of beneficiaries with additional visits. Given the presence of a defined shareholder, for-profit agencies have a greater incentive to maximize profits by enrolling patients for longer periods under a cost-based payment system. Thus, under a cost-based payment system, we hypothesize that patients in for-profit agencies had longer length of use.
Depending on the marginal productivity of additional home health services, there may be implications of the length of enrollment for patient discharge status. Assessing whether additional home health services are productive is difficult because there are no agreed-upon standards of what constitutes necessary or appropriate home health care, patients have chronic and overlapping care needs, and even the most basic unit of service—the visit—is not specifically defined (U.S. General Accounting Office 2000). Nevertheless, discharge status is a potential outcome measure for post-acute services such as home health care (e.g., Grabowski et al. 2006; Intrator, and Berg 1998; McCall et al. 2002; Wodchis, Fries, and Hirth 2004). For example, acute care hospitalizations are being used as a performance indicator in the ongoing Medicare Home Health Pay-for-Performance Demonstration. If a shorter length of use eliminates productive home health care services, then we would expect higher mortality, more discharges to institutions and more discharges without the goals of care having been met. Alternatively, if additional services are not productive, then we would not expect a change in discharge status.
The literature on for-profit/non-profit differences in home health care to date has largely focused on the association between agency ownership and length of home health care enrollment under a cost-based payment system. Using Cox proportional hazards models, one recent study concluded that ownership status was not associated with length of enrollment (Han, McAuley, and Remsburg 2007). Two other recent studies incorporated home health ownership as a covariate in work focusing on other topics (Han et al. 2004; Murkofsky et al. 2003). These studies found that for-profit status was associated with longer enrollment in home health care. However, none of these studies examined discharge status. It may be the case that a longer length of enrollment among patients at for-profit agencies generated better discharge outcomes.
The 1997 Balanced Budget Act changed Medicare home health eligibility and coverage rules and reformed the payment methodology by instituting a prospective payment system (PPS) for home health care reimbursement (Komisar 2002). Implemented on October 1, 2000, Medicare pays home health agencies a set payment rate for each 60-day episode of care, regardless of the specific services delivered. While the PPS was being developed, the Centers for Medicare & Medicaid Services instituted an interim payment system (IPS). The IPS was phased in beginning October 1997 with the start of each agency's cost reporting period, and it constrained agency reimbursement by reducing the per visit payment limit and introducing an annual per-beneficiary cap on payments. Following implementation of the IPS, there was a sharp decline in Medicare home health expenditures, visits, and overall use (McCall et al. 2003b).
Thus, we also analyze whether there was a differential response to the IPS payment limits between for-profit and nonprofit home health care agencies. We posit more sizable changes in behavior among for-profit agencies following the adoption of the payment caps under the IPS. The rationale for this hypothesis is that—because nonprofits lack a residual claimant—these agencies have less incentive to maximize profits and more incentive to maximize objectives such as the quality of care. As such, theory would hold that nonprofit agencies are less sensitive to a change in payment generosity. Specifically, we would expect patients at for-profit agencies to have a larger decrease in length of use and a greater increase in discharges without the goals of care having been met following the IPS.
Using data from 1994-2000 (prior to Medicare's transition from a cost-based to a PPS for home health care in late 2000, but incorporating the adoption of the IPS Medicare payment limits in 1997), this paper compares the length of home health care use and discharge status for patients receiving care from for-profit and nonprofit agencies.
Data and Methods
Our study used the 1994, 1996, 1998 and 2000 waves of the NHHCS, a nationally representative survey of home and hospice care agencies and their current and discharged patients conducted by the National Center for Health Statistics. This study excludes hospice patients and focuses on discharged home health patients. The data were collected using a two-stage sampling process. In the first stage, agencies were randomly selected (by size) from 24 strata according to agency-type (home health, hospice, or mixed), region (Northeast, Midwest, West or South), and location in a metropolitan statistical area. An interviewer contacted the administrator (or designee) for each sampled agency and collected general information on the agency. In the second stage of the sampling process, up to 6 discharged patients were randomly chosen from each of the selected agencies. Patient-level data were obtained via personal interviews with the agency staff member who was most familiar with the patient's care along with a review of patient records, if necessary. The final sample included 14,088 discharged home health care patients.
In constructing our sample, we included all home health care patients, regardless of primary payer source, rather than restrict the analysis to Medicare patients. We based this decision on recent evidence that Medicare home health care payment incentives have implications for the treatment of non-Medicare patients (Grabowski et al. 2006). From a legal perspective, providers certified to accept Medicaid or Medicare patients are often required by the CMS to provide care of equal quality to all patients, regardless of payer type or generosity. From a behavioral perspective, there is a long-standing notion that professional norms matter in health care (Frank 2004). Behavioral constructs such as trust, fairness and regret may explain why providers value treating all patients according to the same criteria. From an economic perspective, certain aspects of health care are produced jointly for all payer types and may exhibit economies of joint production. For example, an agency's investment in staff training (or lack thereof) would have implications for all patients, regardless of payer source. Nevertheless, our results are generally similar when we exclude non-Medicare patients from the analysis.
Length of use, the first dependent variable of interest, was constructed as the number of days from home health enrollment to discharge. We modeled length of use in this study using dummy variables measuring enrollment for fewer than 30 days and enrollment for 100+ days (Han et al. 2004). We selected these cutoffs because they roughly approximate the median and 85th percentiles. Specifically, our data indicate 47% of the sample was discharged within 30 days and 17% was enrolled for at least 100 days. We focused on short and long stays because Medicare policymakers have been particularly concerned with short- and long-term users. Short-term users constitute the majority of recipients and long-term users constitute the majority of utilization. According to the Medicare Payment Advisory Commission (1998), 51% of recipients received fewer than 30 visits and accounted for 9% of all home health visits in 1996, while 15% of Medicare home health care users in 1996 had 150 visits or more and accounted for 59% of all Medicare home health visits that year. Approximately one-third of the beneficiaries in this latter group received over 300 visits. In secondary analyses, we modeled length of enrollment as a continuous measure using a semi-log approach. Although others have used a Cox proportional hazards model to examine length of home health enrollment (Han et al. 2007), an examination of the scaled Schoenfeld residuals indicated that the hazard function was not proportional by ownership status, thus rejecting the proportionality assumption.
We modeled the reason for discharge, our second dependent variable of interest, using four mutually exclusive categories: goals of care met, transfer to an inpatient care setting, death and other. The goals met category consists of recovery, stabilization, family and friends resuming care, and services no longer needed. Inpatient care settings include both hospitals and nursing homes. The other category consists of those sample persons that were no longer eligible for services, were transferred to some other outpatient care setting or moved out of the area.
The key independent measure of interest was the ownership status of the agency, and we compared for-profits versus all other agencies. For-profits are agencies operated under private commercial ownership, including individual or private ownership, partnerships, or corporations. The other category includes voluntary or nonprofit (including church-related and nonprofit corporations), Federal, State, or local government, and all other types of ownership (hereafter referred to as “nonprofits”). Unfortunately, the 1996, 1998 and 2000 NHHCS waves did not allow us to distinguish discharges from nonprofit and government agencies, but the 1994 wave indicated that government agencies accounted for only 6.4% of total discharges.
The implementation of the IPS, represented by a dummy variable, is the policy variable of interest. Because the IPS was implemented on October 1, 1997, data from the 1998 and 2000 waves were assigned to the IPS period. A potential issue with this assignment for the 1998 NHHCS wave is that patients may have been admitted before the IPS (approximately 18% of Medicare patients in the 1998 wave were admitted before October 1, 1997) (Han, and Remsburg 2003). Unfortunately, we are not able to correct for this issue using the public use NHHCS files, but if anything, this would bias our results toward finding no effect of the IPS.
A number of covariates were included in our multivariate models (see Table 1 for descriptive statistics). At the person-level, demographic variables included gender, age, race, ethnicity, and marital status. We also included the patient's referral source (physician, hospital, self/family, nursing home, or other), living arrangement (lives alone, institution, or other), primary payer source (Medicare, Medicaid, private insurance, or other), and presence of a primary caregiver. We included dummy variables for the patient's Charlson score calculated from a list of up to 6 diagnoses at admission (Charlson et al. 1987), vision difficulty, and hearing difficulty. The Charlson score ranged from zero to 11 within our sample, with a higher value indicating worse health. At the agency level, we controlled for whether the agency was group-owned and hospital-based. Finally, we included dummy variables for whether the agency was located in a metropolitan statistical area and region of the country. For race, marital status and the agency-level variables, we also included dummy variables for missing observations to maximize our sample size. Because individuals discharged earlier may also have a lower probability of negative outcomes such as death or institutionalization, we also included length of use dummy variables (30-59 days, 60-99 days, >99 days) in the discharge status regressions.
Table 1.
Summary Statistics (N=14,088)
| Total Sample |
For-Profit | Nonprofit | |
|---|---|---|---|
| For-Profit Agency | 31% | ||
| Mean length of use (in days) | 93.87 | 99.68 | 91.22 |
| Length of use less than 30 days | 47% | 42%** | 50% |
| Length of use greater than 99 days | 17% | 22%** | 15% |
| Discharged: Death | 4% | 5% | 4% |
| Discharged: Institution | 17% | 18% | 17% |
| Discharged: Goals met | 68% | 64%* | 69% |
| Discharged: Other | 11% | 13% | 10% |
| Person-level control variables | |||
| Medicare | 66% | 63% | 68% |
| Medicaid | 10% | 9% | 11% |
| Private Insurance | 17% | 21%* | 16% |
| Other payer | 6% | 8% | 5% |
| Female | 62% | 62% | 63% |
| Married | 38% | 36% | 39% |
| Marital status missing | 12% | 16%** | 10% |
| African American | 10% | 12% | 9% |
| White | 69% | 65%* | 71% |
| Other race | 4% | 4% | 4% |
| Race missing | 17% | 20% | 16% |
| Hispanic | 5% | 6% | 4% |
| Lives in Metropolitan Statistical Area | 86% | 88% | 84% |
| Region: West | 16% | 20% | 14% |
| Region: South | 27% | 41%** | 21% |
| Region: Midwest | 21% | 17% | 23% |
| Region: Northeast | 36% | 22%** | 42% |
| Age less than 65 | 30% | 32% | 29% |
| Age 65-74 | 22% | 21% | 23% |
| Age 75-84 | 31% | 28%* | 32% |
| Age 85+ | 17% | 19% | 16% |
| Lives alone | 27% | 27% | 26% |
| Lives in an institution | 7% | 9%** | 6% |
| Referral source: self/family | 3% | 4% | 3% |
| Referral source: hospital | 47% | 35%** | 53% |
| Referral source: nursing home | 2% | 2% | 3% |
| Referral source: Doctor | 35% | 43%** | 31% |
| Referral source: other | 12% | 16%** | 10% |
| Has primary caregiver | 79% | 76%* | 81% |
| Vision difficulty | 17% | 19% | 17% |
| Hearing difficulty | 16% | 16% | 16% |
| Charlson score = 0 | 46% | 50%** | 45% |
| Charlson score = 1 | 28% | 26% | 28% |
| Charlson score = 2 | 18% | 17% | 18% |
| Charlson score = 3 | 5% | 4% | 5% |
| Charlson score = 4+ | 4% | 3%* | 4% |
| Agency-level control variables | |||
| Group-owned agency | 45% | 60%** | 38% |
| Group-owned missing | 4% | 1%** | 5% |
| Hospital-based agency | 41% | 18%** | 51% |
| Hospital-based missing | 3% | 1%** | 4% |
| Time | |||
| 1994 wave | 18% | 16% | 19% |
| 1996 wave | 26% | 27% | 26% |
| 1998 wave | 29% | 36%* | 25% |
| 2000 wave | 27% | 22%* | 29% |
Notes: Asterisks identify a statistically significant difference between for-profit and nonprofit agencies.
p<.01
p< 0.05
We present both unadjusted and adjusted comparisons of length of enrollment and discharge status between for-profit and nonprofit agencies. Given the binary nature of the outcomes, the multivariate models were estimated as probits, but the coefficients are presented as marginal probability effects. Thus, the coefficient estimates can be interpreted as the percentage point change in the dependent variable associated with for-profit status. Given the complex survey design, the “svy” (i.e., survey) commands in Stata software (version 8.02) were used to incorporate the NHHCS weights to account for the unequal selection probability of patients and also correct the standard errors for clustering within agencies. Because strata were not included on the NHHCS public use file, we constructed this measure using the agency type, region and metropolitan statistical area variables (Carlson, Gallo, and Bradley 2004). In the discharge outcome models, Stata does not allow complex survey weights in the estimation of multinomial probit models. As such, the 4-category multinomial response model was estimated by three binary response models, which separately contrasted death, an inpatient admission or ‘other’ discharge to the reference category (discharge with the goals of care met). This approach produces results with somewhat less efficient estimates (i.e., larger standard errors) than those obtained by estimation of the full multinomial response model (Begg, and Gray 1984).
In order to test the response to the IPS between ownership types, we include an interaction term (IPS*for-profit) in the regression models. However, the interaction term in a probit model is not directly interpretable (Ai, and Norton 2003), and existing software to correct for this issue does not take account of complex survey weights (Norton, Wang, and Ai 2004). Thus, the model including this interaction term was estimated using a linear probability model. Once again, the coefficient estimates can be interpreted as the percentage point change in the dependent variable. In a set of robustness checks excluding the complex survey weights, these results were similar in magnitude and precision to the probit marginal probability estimates.
Results
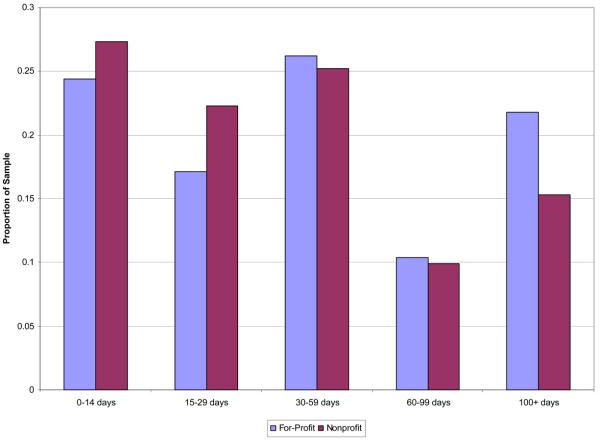
Figure 1 presents the distribution of length of home health care enrollment by ownership status. This figure indicates large differences in utilization by ownership at the low and high ends of the distribution, but relatively similar rates in the middle of the distribution. Specifically, nonprofits in the bottom two groups (<30 days) account for 41.5% of for-profit discharges and 49.6% of nonprofit discharges. The next two groups (or days 31-99) account for 36.6% of for-profit discharges and 35.1% of nonprofit discharges. Finally, the last group (days 100+) account for 21.8% of for-profit discharges and 15.3% of nonprofit discharges. These results suggest a nonlinear relationship between ownership status and length of enrollment.
Figure 1.
Home Health Care Length of Enrollment, by Ownership
Table 1 summarizes the unadjusted differences between patients receiving care from for-profit and nonprofit agencies. Although patients in for-profit agencies had more days in home health care relative to nonprofit patients, this difference was not statistically meaningful. However, patients in for-profit agencies were significantly less likely than patients in non-profit agencies to have a length of enrollment less than 30 days and significantly more likely to have an enrollment of greater than 99 days. Discharge status by ownership was not significantly different for the death or inpatient categories. However, patients in nonprofits were significantly more likely to be discharged with the goals of care met (69% versus 64%) and less likely to be in the ‘other’ discharge category (10% versus 13%). Other measures that differed significantly by ownership type included payer source, marital status, race, ethnicity, region of the country, residence in a metropolitan statistical area, age, residence in an institution, referral source, the presence of a primary caregiver, Charlson score, whether the agency was group-owned, whether the agency was hospital-based and the year of survey. Of note, although enrollees of for-profit agencies were slightly older than those of other agencies, they were also healthier.
The probit estimates support the hypothesis that patients in for-profit agencies had longer periods of home health care enrollment under a cost-based payment system (see Table 2). Patients in for-profit agencies were 6.5 percentage points (p<.01) less likely to have a period of home health care enrollment less than 30 days. In regards to discharge status, there was no significant difference by ownership status in discharge to an inpatient setting, death or the “other” discharge category compared with the goals met category. Additionally, although not reported in the table, the adoption of the Medicare IPS was significantly associated with earlier discharge, but not independently associated with discharge outcome.
Table 2.
Association between ownership status and home health care discharge: All patients
| Dependent variable | Absolute percentage point change for patients in for-profit agencies vs. nonprofit agencies |
Absolute percentage point change after the IPS for patients in for- profit agencies vs. nonprofit agencies |
N |
|---|---|---|---|
| Length of use < 30 days (vs. ≥30 days) | −6.5** (0.006) |
−8.1* (0.037) |
14,088 |
| Length of use > 99 days (vs. ≤99 days) | 3.4 (0.064) |
−4.3 (0.234) |
14,088 |
| Discharged: death (vs. goals met) | −0.2 (0.677) |
−1.5 (0.581) |
9,487 |
| Discharged: institution (vs. goals met) | 3.4 (0.057) |
−5.0 (0.098) |
11,137 |
| Discharged: other (vs. goals met) | 2.3 (0.142) |
−3.6 (0.254) |
10,496 |
Notes: Estimates in Column 1 are the main effects from a multivariate probit model and estimates from column 2 are the interaction terms (for-profit * Interim Payment System) from a linear probability model. The regressions adjust for all the variables in Table 1. Marginal probability effects are presented and can be interpreted as the percentage point change in the dependent variable. P-values are presented in parentheses. The discharge status models include dummy variables controlling for length of use.
p<.01
p< 0.05
We also examined the response to the Medicare IPS between ownership types by including an interaction of for-profit status and the IPS period. The second column of Table 2 presents the results from the interaction terms. Following the implementation of the IPS, patients at for-profit agencies were 8.1 percentage points (p<.05) less likely to be discharged within 30 days relative to patients at nonprofit agencies. There was no significant difference between ownership types on the likelihood of being enrolled greater than 99 days following the IPS. In terms of discharge status, patients at for-profit agencies were 5 percentage points less likely to be discharged to an institution (vs. discharged because the goals of care were met) following the adoption of the IPS relative to patients at nonprofit agencies, but this result was only marginally significant (p<.1). Thus, contrary to our hypothesis, we obtained some limited evidence of a larger response to a Medicare payment limit by nonprofit agencies.
In our (unreported) secondary analyses, the treatment of length of enrollment as a continuous measure generated results of the expected sign, but the results were not statistically different from zero.
Discussion
This study represents one of the few efforts to examine ownership differences in the home health care sector. Using a nationally representative survey of discharged home health care patients over the 1994 through 2000 period, we found support for the prediction that patients in for-profit home health care agencies experienced differential enrollment under cost-based Medicare payment relative to nonprofit patients. Specifically, for-profit patients were less likely to be discharged within 30 days. However, in spite of this difference, patients receiving care from for-profit agencies were no more likely to be discharged with the goals of care met. Contrary to our second hypothesis however, we found that patients at nonprofit agencies compared with for-profit agencies had an increased likelihood of discharge within 30 days following the Medicare payment limits imposed under the IPS.
A common theme within the empirical literature on ownership in health care is that poor outcomes may result from opportunistic behavior by for-profit providers (Hirth 1999). If nonprofit providers, often affiliated with religious or charitable organizations, are less willing to compromise care for the sake of profit, then ownership status may provide a low cost signal that the promised services will be delivered. Under a cost-based Medicare payment system, however, our study indicated for-profit agencies actually enrolled patients for longer durations relative to their nonprofit counterparts. This finding is consistent with a profit maximization strategy in which additional visits entail increased Medicare payments. Somewhat paradoxically however, for-profit agencies were less responsive than nonprofit agencies to the discharge incentives under the Medicare payment limits of the IPS. Nonprofits may have been more responsive to the IPS in anticipation of an even bigger Medicare payment change under the PPS in 2000. Moreover, although our models control for patient health, for-profits may have selectively admitted healthier patients following the IPS. Indeed, data from the General Accounting Office (GAO) suggest a larger relative decrease in the average number of home health care visits by patients at for-profit agencies following the IPS (U.S. General Accounting Office 2000).
Our results also indicated relatively stable discharge outcomes between for-profit and nonprofit agencies following Medicare payment limits. Although we cannot measure other important outcomes such as morbidity, independence and family stress, our findings are similar to earlier work showing no decline in these other outcomes under the IPS (McCall et al. 2003a, 2004). One interpretation of our results is that the additional services provided by for-profit agencies under cost-based reimbursement may not have constituted beneficial services. Once again, there are not agreed-upon standards of what constitutes medically necessary or appropriate home health care services. In support of this point, the GAO (2000) has reported wide geographic variation in Medicare home health care utilization under cost-based payment. For example, Medicare home health care users in Maryland received an average of 37 visits in 1997 while users in Louisiana received 161 visits. This variation in use, which persists after controlling for patient diagnoses, may suggest that the service use difference between for-profit and nonprofit agencies under cost-based payment represented “flat of the curve” home health care, offering few additional benefits for patients.
Weisbrod (1988) has outlined two goals for public policy towards the nonprofit sector: (1) public policy should help encourage nonprofits to achieve their social goals, and (2) public policy should help achieve a better balance of institutional responsibilities between nonprofits, for-profits and governments. The typical assumption in health care is that nonprofits have a competitive advantage in “trustworthiness” while for-profits have greater incentives for efficiency. For example, Grabowski and Hirth (2003) found that nursing home markets with a greater nonprofit market share have higher overall quality, while Kessler and McClellan (2002) found that areas with a stronger presence of for-profit hospitals have 2.4% lower overall hospital expenditures. However, our results suggest that – under a cost-based payment system – nonprofits behave more efficiently relative to for-profits. With the subsequent shift to the Medicare PPS, the home health care sector might now more closely mirror the hospital and nursing home markets in terms of nonprofit and for-profit roles. However, our results paradoxically indicate a stronger response by nonprofit agencies to the Medicare IPS limits. It will be important to update this analysis following the implementation of the full PPS.
Our results also have potential implications for tax policy and value-based payment. Our findings suggest that the tax exempt status afforded nonprofits should be maintained if future results continue to indicate more efficient performance by nonprofits. Moreover, our results indicate that nonprofit agencies produce comparable discharge outcomes at a lower cost to Medicare. As Medicare considers the adoption of home health care pay-for-performance and other refinements to the PPS, there is an opportunity to further introduce payment structures that recognize both superior quality and strong financial performance.
As with any observational study of home health care ownership, we acknowledge the potential limitation that we cannot unambiguously rule out potential bias in our estimates due to unobserved differences between patients at nonprofit and for-profit agencies. With the NHHCS, we were able to control for a number of patient level factors, but it still may be the case that there are other unmeasured factors which differ by ownership. Future work should consider an instrumental variables approach to address this issue.
With the continued growth of the home health care sector, it is essential for patients, clinicians, other health care professionals and policymakers to be cognizant of the organizational factors that potentially influence the delivery of services. Under a cost-based payment system, we observed significant differences in the length of home health care enrollment by ownership type, and slight differences in discharge outcomes. As new data become available, it will be important to extend this research following the adoption of the PPS and alternate outcomes.
Acknowledgments
The authors are grateful to Harvard's Program in the Global Demography of Aging, funded by the National Institute of Aging, for providing financial support for this study. The authors also acknowledge and thank Hocine Azeni for assistance with statistical programming.
References
- Ai C, Norton EC. Interaction Terms in Logit and Probit Models. Economics Letters. 2003;80(1):123–29. [Google Scholar]
- Begg CB, Gray R. Calculation of polychotomous logistic regression parameters using individualized regressions. Biometrika. 1984;71(1):11–18. [Google Scholar]
- Carlson MD, Gallo WT, Bradley EH. Ownership status and patterns of care in hospice: results from the National Home and Hospice Care Survey. Med Care. 2004;42(5):432–8. doi: 10.1097/01.mlr.0000124246.86156.54. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Frank RG. NBER Working Papers. National Bureau of Economic Research, Inc; 2004. Behavioral Economics and Health Economics. [Google Scholar]
- Grabowski DC, Hirth RA. Competitive spillovers across non-profit and for-profit nursing homes. Journal of Health Economics. 2003;22(1):1–22. doi: 10.1016/s0167-6296(02)00093-0. [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Stevenson DG, Huskamp HA, Keating NL. The influence of Medicare home health payment incentives: does payer source matter? Inquiry. 2006;43(2):135–49. doi: 10.5034/inquiryjrnl_43.2.135. [DOI] [PubMed] [Google Scholar]
- Han B, McAuley WJ, Remsburg RE. Agency ownership, patient payment source, and length of service in home care, 1992 2000. Gerontologist. 2007;47(4):438–46. doi: 10.1093/geront/47.4.438. [DOI] [PubMed] [Google Scholar]
- Han B, Remsburg RE. The 1997 Balanced Budget Act and home services among medicare patients. Jama. 2003;290(20):2661. doi: 10.1001/jama.290.20.2661-a. [DOI] [PubMed] [Google Scholar]
- Han B, Remsburg RE, Lubitz J, Goulding M. Payment source and length of use among home health agency discharges. Med Care. 2004;42(11):1081–90. doi: 10.1097/00005650-200411000-00007. [DOI] [PubMed] [Google Scholar]
- Hansmann HB. The Role of Nonprofit Enterprise. The Yale Law Journal. 1980;89(5):835–901. [Google Scholar]
- Hillmer MP, Wodchis WP, Gill SS, Anderson GM, Rochon PA. Nursing home profit status and quality of care: is there any evidence of an association? Medical Care Research and Review. 2005;62(2):139–66. doi: 10.1177/1077558704273769. [DOI] [PubMed] [Google Scholar]
- Hirth RA. Consumer information and competition between nonprofit and for-profit nursing homes. J Health Econ. 1999;18(2):219–40. doi: 10.1016/s0167-6296(98)00035-6. [DOI] [PubMed] [Google Scholar]
- Intrator O, Berg K. Benefits of home health care after inpatient rehabilitation for hip fracture: health service use by Medicare beneficiaries, 1987-1992. Archives of Physical Medicine and Rehabilitation. 1998;79(10):1195–9. doi: 10.1016/s0003-9993(98)90261-1. [DOI] [PubMed] [Google Scholar]
- Kessler DP, McClellan MB. The effects of hospital ownership on medical productivity. Rand Journal of Economics. 2002;33(3):488–506. [PubMed] [Google Scholar]
- Komisar HL. Rolling back Medicare home health. Health Care Financ Rev. 2002;24(2):33–55. [PMC free article] [PubMed] [Google Scholar]
- McCall N, Korb J, Petersons A, Moore S. Constraining Medicare home health reimbursement: what are the outcomes? Health Care Financ Rev. 2002;24(2):57–76. [PMC free article] [PubMed] [Google Scholar]
- McCall N, Korb J, Petersons A, Moore S. Reforming Medicare payment: early effects of the 1997 Balanced Budget Act on postacute care. Milbank Quarterly. 2003a;81(2):277–303. doi: 10.1111/1468-0009.t01-1-00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall N, Korb J, Petersons A, Moore S. Decreased home health use: does it decrease satisfaction? Med Care Res Rev. 2004;61(1):64–88. doi: 10.1177/1077558703260183. [DOI] [PubMed] [Google Scholar]
- McCall N, Petersons A, Moore S, Korb J. Utilization of home health services before and after the Balanced Budget Act of 1997: what were the initial effects? Health Serv Res. 2003b;38(1 Pt 1):85–106. doi: 10.1111/1475-6773.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission . Report to the Congress: Context for a Changing Medicare Program. Medicare Payment Advisory Commission; Washington, DC: 1998. [Google Scholar]
- Medicare Payment Advisory Commission . Report to the Congress: Medicare Payment Policy. Medicare Payment Advisory Commission; Washington, DC: 2004. [Google Scholar]
- Murkofsky RL, Phillips RS, McCarthy EP, Davis RB, Hamel MB. Length of stay in home care before and after the 1997 Balanced Budget Act. Jama. 2003;289(21):2841–8. doi: 10.1001/jama.289.21.2841. [DOI] [PubMed] [Google Scholar]
- Newhouse JP. Toward a Theory of Nonprofit Institutions: An Economic Model of a Hospital. American Economic Review. 1970;60(1):64–74. [Google Scholar]
- Norton EC, Wang H, Ai C. Computing interaction effects and standard errors in logit and probit models. The Stata Journal. 2004;4(2):103–16. [Google Scholar]
- Rosenau PV, Linder SH. The comparative performance of for-profit and nonprofit home health care services in the US. Home Health Care Services Quarterly. 2001;20(2):47–59. doi: 10.1300/J027v20n02_03. [DOI] [PubMed] [Google Scholar]
- Smith C, Cowan C, Heffler S, Catlin A. National health spending in 2004: recent slowdown led by prescription drug spending. Health Affairs (Millwood) 2006;25(1):186–96. doi: 10.1377/hlthaff.25.1.186. [DOI] [PubMed] [Google Scholar]
- U.S. General Accounting Office . Medicare Home Health Care: Prospective Payment System Could Reverse Recent Decline in Spending. U.S. General Accounting Office; Washington, D.C.: 2000. [Google Scholar]
- Weisbrod BA. The Nonprofit Economy. Harvard University Press; Cambridge, MA: 1988. [Google Scholar]
- Wodchis WP, Fries BE, Hirth RA. The effect of Medicare's prospective payment system on discharge outcomes of skilled nursing facility residents. Inquiry. 2004;41(4):418–34. doi: 10.5034/inquiryjrnl_41.4.418. [DOI] [PubMed] [Google Scholar]