Abstract
The human brain has the potential for self-renewal through adult neurogenesis, which is the birth of new neurons. Neural plasticity implies that the nervous system can change and grow. This understanding has created new possibilities for cognitive enhancement and rehabilitation. However, as individuals age, they have decreased confidence, or memory self-efficacy, which is directly related to their everyday memory performance. In this article, a developmental account of studies about memory self-efficacy and nonpharmacologic cognitive intervention models is presented and a cognitive intervention model, called the cognitive behavioral model of everyday memory, is proposed.
Keywords: cognitive plasticity, cognitive training, everyday memory performance, memory self-efficacy, psychosocial intervention
The findings from the longitudinal Health and Retirement Study showed that more than one third of men and women older than 85 have moderate to severe memory impairment.1 Memory lapses are a widespread concern among the elderly, particularly if a family member had a cognitive impairment or dementia.2-4 In addition to the measurable decrements in everyday memory performance experienced by older adults as they accumulate years of living, they also might have distress as well as lose confidence in their memory performance, known as memory self-efficacy.5,6 Everyday memory, the day-to-day operations of memory in real-world ordinary situations, is one type of memory related to memory self-efficacy concerns.7-9
Complaints of memory impairment are often nonspecific predictors of incipient cognitive decline and portend a diagnosis of mild cognitive impairment (MCI). Adults at risk for memory loss and MCI may have performance deficits in not only cognitive function but also the instrumental activities of daily living. An MCI diagnosis includes the 5 criteria of: cognitive complaints that are not normal for the age of the individual; no dementia; cognitive decline; memory impairment; and essential normal functional activities.10-12
As findings from longitudinal research have accumulated, there has been a paradigm shift away from viewing cognitive aging as an inevitable decremental process and a renewed interest in the use of interventions to prevent or remediate cognitive decline. The “disuse hypothesis”13,14 and the “use it or lose it” learning theory of mental discipline15 are popular models guiding cognitive intervention research, although they were first tested in animal models. Mental stimulation, or exercises for the brain, is hypothesized to assist with the maintenance of cognitive function. This hypothesis can be viewed as a self-help strategy that individuals value and believe will pay off in a reduced incidence of cognitive impairment; however, at this time, the hypothesis is not completely supported empirically.16 Concurrent with the interest in improving cognitive function in adults, there is widespread enthusiasm for psychosocial models that have the ability to predict and explain successful aging and that emphasize a balance between gains and losses through the processes of selection, optimization, and compensation.17-19
This enthusiasm for research on all aspects of cognitive functioning was initiated by the National Institutes of Health and was formalized as the Decade of the Brain.20 Findings from diverse areas of science, both basic and applied, have illuminated mechanisms illustrating that the human brain has the potential for self-renewal through adult neurogenesis, which is the birth of new neurons.21,22 Neural plasticity implies that the nervous system can change and grow and that future growth is differentially channeled. This regeneration is called plasticity, an alteration in structure or function brought about by development, experience, or injury.23-26 When the term is applied to learning and memory, Gaze and Taylor24 argued that the functional alteration resulting from the input experience must be organized rather than chaotic to qualify for plasticity. Chaotic changes in function would not represent plasticity. For optimal cognitive function into late life, the prevention or delay of the disablement process for as long as possible is the goal of cognitive therapies.27,28 Although plasticity, by its very definition, implies retention of pattern and order, the resultant changes from an injury would not imply plasticity.
This understanding of neurogenesis and neuroplasticity has created new possibilities for cognitive enhancement and cognitive rehabilitation.29 The prevention of disability by focusing on prevention of cognitive impairment and dementia, as well as delaying the onset of symptoms, is a worthwhile goal for the future.27 Clearly, treatments or other technologies to promote cognitive function and prevent memory impairment may reduce the burden and cost of care for the millions of people approaching older age both in the United States and globally.
This article has 3 goals: (1) present a developmental account of selected studies focused on the relationship between memory self-efficacy and memory performance; (2) synthesize the literature on nonpharmacologic cognitive intervention models; and (3) propose the cognitive behavioral model of everyday memory (CBMEM) for advancing the science of cognitive intervention research with older adults.
MEMORY SELF-EFFICACY AND MEMORY PERFORMANCE
The argument for using Bandura’s self-efficacy theory for research on cognitive aging is that older adults desire to maintain agency and remain in control of their destiny.30 However, owing to personal and social factors, an older adult may lack a sense of mastery for memory abilities, either because they have observed changes in their own memory or because their culture teaches that memory declines are inevitable.5,9,31,32 As a result, older adults do not try as hard as younger adults to remember. Thus, they remember less and experience reduced feelings of self-efficacy. Memory self-efficacy is the belief in one’s own capacity to use memory effectively in various situations, and memory performance is known to vary as a function of individuals’ beliefs about their cognitive abilities.32,33
Knowledge about memory is distinct from memory self-efficacy; thus, an older individual may have extensive and accurate knowledge about how his or her memory functions but may also believe that their ability to remember in a given context is poor. If the individual perceives that memory decreases with age, then he or she is quick to interpret faulty performance as an indicator of declining memory capacity. Individuals who have low self-efficacy may give up trying to remember because of doubts about achieving a desired level of performance. Conversely, individuals who view memory ability as a skill that can be developed and practiced may achieve higher memory capacity. In one study, older adults had higher self-efficacy for everyday problems and generated more viable solutions than young adults.34 Other studies have also shown that memory performance varied as a function of the individual’s beliefs about memory performance.3 In Black and White community elders, memory self-efficacy was related significantly and positively to everyday memory, accounting for 13% of the variance in performance.35
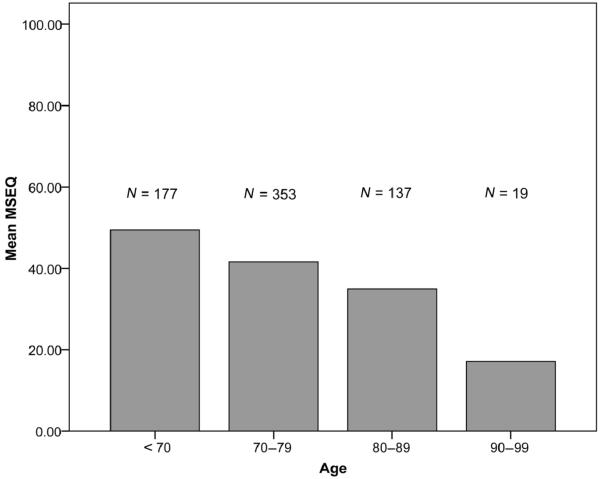
When memory self-efficacy was measured with the 50-item Memory Self-Efficacy Questionnaire, the mean score for a tristate sample of community-residing older adults (N = 686) was 41.56 (SD = 20.16; range, 0.80-98.86) and they had a decrease in memory self-efficacy with age.5,35-41 There was an inverse relationship between chronological age measured in years and memory self-efficacy (P = -0.30, P < 0.001). The mean age was 74.07 years (SD = 7.92; range, 60-99). As illustrated in Figure 1, the mean memory self-efficacy scores decreased in each decade.
Figure 1.
Memory self-efficacy scores by age group measured with the 50-item Memory Self-Efficacy Questionnaire (MSEQ) (N = 686).
In the past 20 years, self-efficacy beliefs have been addressed in studies to improve memory performance. This paradigm shift was a gradual next step following the accumulation of evidence from correlational studies that linked memory performance and memory self-efficacy. A second line of influence in this shift was the influence of self-regulation through goal setting in health-promotion studies aimed at changing or influencing health behaviors.42,43 In a study designed to change memory self-efficacy beliefs, self-efficacy predicted subsequent memory performance when it was measured in terms of subjects’ judgments of their highest memory capability and when they judged their memory efficacy for the most taxing recall task.44 In other studies, memory self-efficacy and memory performance were significantly improved at 4 weeks to 3 months.45-47 Furthermore, perceived self-efficacy predicted memory performance. Therefore, interventions designed to improve self-efficacy (memory beliefs and confidence) may be as important as teaching mnemonic strategies. The results of studies with older adults showed that self-efficacy beliefs predicted memory performance.36,48
MEMORY TRAINING INTERVENTIONS TO ENHANCE MEMORY PERFORMANCE
Mental stimulation may be an approach to remaining cognitively healthy and preventing or delaying the signs of cognitive impairment.48-50 Evidence from many studies indicate that a large proportion of older, nondemented individuals have sufficient numbers of plaques and tangles to meet neuropathologic criteria for Alzheimer’s disease but do not manifest clinical symptoms of the disease during their life spans, which may be explained by a substantial reserve capacity in their fluid intelligence.51,52 This phenomenon has been identified as cognitive reserve. Cognitive reserve may explain why individuals experience differential rates of change in cognitive function and that reserve capacity may provide a buffer to cognitive decline.53,54
After reviewing all published memory training studies, Floyd and Scogin55 and Verhaeghen et al56 concluded from the evidence that an intervention that emphasized teaching participants 1 or 2 mnemonic strategies was better than no intervention, but that future intervention studies must include ways to increase participants’ awareness and knowledge (metamemory) and decrease their negative beliefs (memory self-efficacy) and negative memory-related affect (anxiety). A small group format was recommended over individual or self-directed training. Participants’ benefit from vicarious experience in developing solutions and strategies as well as from learning through their own enactive mastery experiences.5 Investigators have recommended that memory improvement training be multifactorial. For example, combining training in visual imagery skills can also facilitate learning mnemonic strategies, and visual imagery and relaxation skills are often maintained more effectively than teaching 1 or 2 mnemonic strategies.57-59
Evidence of long-term benefits from participation in memory training has been documented in numerous studies. Participants reported that following the training, they used memory strategies between 10% and 51% of the time in their everyday lives.60-63 Six previous studies have reported conflicting findings on the long-term (6+ months) effects of memory training. Sheikh et al64 found that elderly trained with a combination of relaxation and mnemonic techniques maintained their cognitive gains at 6 months. Anschutz et al60 indicated that although 9 of 10 original subjects used the method of loci for remembering a new word list, they did not use this mnemonic strategy to enhance their recall in everyday situations. Scogin and Bienanias,62 who followed 63% of the original participants in a self-taught memory training program, found that the group had a decrease in memory performance and mnemonic usage over time but no change in memory complaints. Hayslip et al61 found that 31% of the participants in fluid ability training reported less use of memory strategies after 3 years. Oswald et al65 found that after 2 years, 309 elderly persons who participated in a combined memory improvement and psychomotor training program maintained their memory performance and functional skills. Willis and colleagues66,67 found that with 5 booster sessions in the second year and 2 in the seventh year, 25 elderly participants maintained their fluid ability training over a 7-year period.
MEMORY INTERVENTION MODELS
A number of intervention models have been developed and tested over the previous 20 years (Table 1). Each model contributed to state-of-the-art cognitive intervention research. The first model, Concentration and Mnemonic Training, emphasized relaxation training and taught 1 or 2 mnemonic strategies.68-71 The second model, the Adult Development and Enrichment Project (ADEPT), emphasized fluid ability training.67,72-77 The third model, Cognitive Restructuring, emphasized control. Individuals had a choice in which they could believe that their memory capacity was either shrinking or controllable, and this might predict how they adapt to their memory ability with advancing age.46,47 The fourth model, the Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) trials, the largest randomized clinical trial to test cognitive training, was implemented at 6 US sites. Three thousand older adults were recruited and randomized to 3 different cognitive interventions and followed for 5 years.78,79 The ACTIVE trials demonstrated that the participants improved their targeted cognitive abilities by an amount approximately equal to the cognitive decline that would naturally occur in older adults without dementia and maintained these gains for 5 years.
Table 1.
Comparison of cognitive intervention models
| Concentration and Mnemonic Training | Cognitive Restructuring | Adult Development and Enrichment Project (ADEPT) | Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) | Cognitive Behavioral Model of Everyday Memory |
|---|---|---|---|---|
| The magnitude of age-related cognitive decline may be reversed with the use of strategic behaviors. | Memory capacity and function is a multifaceted entity “shrinking” vs “controllable.” | Fluid and crystallized intelligence show differential, normal patterns of development in adulthood; fluid declines and crystallized increases or remains stable. | Late-life intellectual stimulation from cognitive and perceptual interventions offers protective effects to skills and behaviors that are necessary for independent living. | Memory and executive function may be adversely influenced by the relationship of modifiable risk factors, such as affect, health, self-efficacy beliefs, and metamemory, with everyday functional performance. |
Three to five 1.5- to 2.5-h sessions:
|
Two 1.5-h sessions:
|
Five 1-h sessions over 2 wk:
|
Ten 60-75 min sessions over 5 to 6 wk that targeted 1 of 3 interventions:
|
Eight 1.5-h sessions, twice a week:
|
| Group instruction, homework, performance feedback, practice, self-regulation, workbooks, and diaries | Group instruction, application self-instruction, videotape, and modeling | Individual practice booklets, feedback, group discussion, and modeling | Small group and individual instruction with exercises to practice, individual and group feedbacks on performance, and a practice test | Book given at first meeting, which was used for content; group instruction, exercises, practice and discussion; homework; performance feedback, transfer to everyday situations |
| Tested in community elderly (often college graduates) and managers (N = 589). No minorities. Emphasizes visual imagery, attention, concentration, progressive muscle relaxation, and mnemonic strategies. Depression and cognitive impairment excluded | Tested in 1 highly educated group of community elderly (N = 105). Three-month follow-up. Emphasizes memory performance and perceptions of control. Minorities not included. Depression not determined and cognitive impairment excluded. | Tested in 2 diverse groups of elderly (N = 398); rural, low education, urban, and high functioning. Emphasizes primary mental abilities. Longitudinal design over 7 y to determine the effects of booster sessions. Minorities not included. | Tested in 6 field sites throughout the United States as cooperative P01. Samples (N = 2,832) were primarily Black and White urbanites. Protocol included the same testing across sites. Three cognitive interventions plus no contact controls were evaluated. Participants were followed up to 5 y beyond the initial enrollment. | Tested in 5 diverse groups (N = 440) of older adults: community, assisted living, nursing home, and retirement village. Emphasis on stress inoculation, metamemory, everyday memory, memory self-efficacy, and strategy use. Minorities, affective and cognitive disorders included. |
Each of these intervention models made important contributions in their respective times to move the science of cognitive stimulation forward. However, important aspects of memory training, now known to influence memory performance, in particular memory self-efficacy (beliefs and confidence), and metamemory (knowledge and perceptions), were excluded from these studies. Furthermore, modification of negative attitudes toward cognitive aging is essential for the success of the intervention.
COGNITIVE BEHAVIORAL MODEL OF EVERYDAY MEMORY
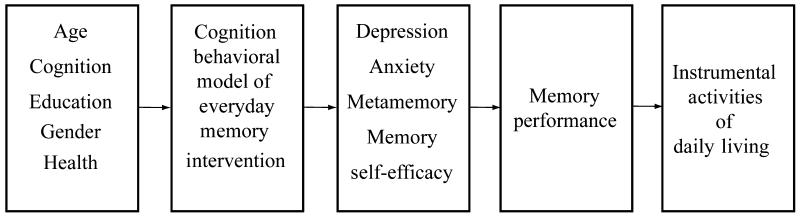
The CBMEM extends the knowledge gained from intervention models designed to enhance older adults’ memory performance (Figure 2).5 This model was derived from Bandura’s80 self-efficacy theory; it addresses the risk factors that are known to influence memory performance, and has many unique features not found in the previous models.5,37 The CBMEM lays out a number of interrelated theoretical components. The first components are identified as antecedent factors, which reside with the individual. They include age, cognition, education, gender, and health. The CBMEM intervention is the second component of the model. The intervention is a psychosocial intervention that emphasizes cognitive and behavioral aspects and combines a unique package of cognitive skill development in exposure, repeated practice, relevant modeling, self-modeling, cognitive skill modeling, exhortation, suggestion, and desensitization. The intervention integrates both didactic content and practical application. The third component is labeled mediators of memory performance. The factors known to affect memory performance include anxiety, depression, metamemory, and memory self-efficacy. The next components are the outcomes. The proximal outcome of the intervention is everyday memory performance. Finally, the distal outcome is function, specifically the instrumental activities of daily living. Theoretically, the intent is to transfer the learning from the classroom to everyday experience.
Figure 2.
The cognitive behavioral model of everyday memory.
Memory improvement may be differentiated as 6 distinct phases in self-efficacy theory, in which participants learn activities and content that are least challenging in the early phases and progress to the most challenging during the final week as the CBMEM moves to completion.5
Modeling techniques: Participants take part in nonthreatening memory exercises that are fun, enjoyable, and constitute a level playing field for every individual.
Observing their memory: Members of the group learn to assess the strengths and weaknesses of their own memory abilities realistically through vicarious experiences with their colleagues and friends as they observe each other participate and perform. Participants use memory without having been tested on new material.
Awareness: Participants develop an awareness of attention and concentration and begin to use more complex models of self-reflection.
Mastery coping: Participants attend the class, which builds their confidence and enjoyment through effective learning experiences and overrides any anxiety about potential embarrassment or having to perform beyond their level of confidence and comfort.
Controlled handling: Participants’ use of the memory textbook allows controlled access to information because although an individual may occasionally miss a class, the content is available by reading the book.
Suspension: Participants relax their anxieties and defenses and develop the ability to observe themselves and their neighbors as they experience memory problems and their solutions, practice relaxation, and use deep breathing in memory-demanding situations, thereby facilitating their out-of-the-classroom confidence in their ability.
The memory intervention covers 4 broad topical areas in the didactic content at the programmatic level (Table 2). The intervention utilizes self-efficacy theory to emphasize stress inoculation, health promotion, memory self-efficacy, and memory strategy training (Figure 2). Memory training programs for older adults have usually emphasized 2 of the 4 components in the CBMEM: mnemonic strategies and stress inoculation. A mnemonic strategy can be defined as any mental strategy or technique that aids the learning of material by using other, initially extraneous, material as an aid to such learning. Mnemonic training may also include visual imagery skills. Imagery procedures have been investigated under the following terms: mental practice, mental imagery practice, mental rehearsal, psyching up, behavior rehearsal, mental preparation, visual imagery, imagery procedures, and covert practice. Usually, a visual image is associated with a mnemonic device. For example, individuals can be taught to increase the elaboration of processing of visual-image associations used in a mnemonic device.
Table 2.
Self-efficacy theory operationalized to the CBMEM curriculum
| Bandura’s Self-efficacy theory | self-efficacy operationalized to the CBMEM | Metacognitive strategies | Goals | Everyday skills taught |
|---|---|---|---|---|
| Enactive mastery experience | Exposure Repeated practice | Verbal elaboration Controlled handling | Activity Complete Monitor Organize |
Alphabet Categorize Create a word Chunking First-letter cue Review Search Story |
| Vicarious experience | Relevant and self-modeling Cognitive self-modeling |
Awareness Exercise Exposure |
Attention Distraction Retention Production Social support |
Association Effort Elaborate Rehearsal Retrieval Retracing |
| Verbal persuasion | Exhortation Suggestion | Think aloud Motivation | Accomplish Confidence Expectancy Imagine Repeat Stimulation |
Calendar Experience List Note Person Place |
| Physiologic and affective states | Desensitization | Imagery Stress inoculation Visualization |
Actively observe Auditory remind Concentration Muscle relax Reduce anxiety |
Control Enjoy Inhale Imagine Laugh |
The CBMEM is the first package to address many unique aspects not included in other intervention models. When delivered in the right dose, the program increases individuals’ belief in their ability to use their memory, which improves their self-efficacy in memory-demanding situations.
The CBMEM has been tested with multiple groups of older adults (N = 175) in quasi-experimental designs.5,39 Recently (2001-2006), the CBMEM intervention was successfully tested in a 5-year, phase III randomized controlled trial with healthy community elderly (N = 265). On entry into the study, 78 individuals had memory complaints and 105 had no memory complaints. In the complaint group, 32 had normal memory function and 46 had poor memory performance. Among those without memory complaints, 42 had no memory impairment and 63 had poor memory performance. Forty-six individuals (17%) met the criteria of poor everyday memory functioning and memory complaints, whereas another 81 (31%) would be considered at risk on the basis of other MCI criteria.10
CONCLUSION
Memory performance in adulthood is an area of inquiry that is worthy of in-depth investigation because this domain of cognitive function is acknowledged as a highly relevant component of many disease states. Because the human brain has the potential for self-renewal through adult neurogenesis, the ability of the brain to regenerate through plasticity implies that the nervous system can change and grow. In this article, I evaluated selected studies of memory self-efficacy and memory performance and synthesized the nonpharmacologic cognitive intervention models. Finally, I proposed a cognitive intervention model, called the CBMEM, to enhance memory self-efficacy and everyday memory performance. Although memory self-efficacy is related to everyday memory performance, intervention studies have produced mixed findings about whether an individual can change his or her beliefs about an aging memory. Both the subjective and objective aspects of cognitive aging are important areas for further inquiry, particularly in older, minority adults.
Acknowledgments
The unpublished findings were presented at the 2008 Collaboratory entitled “Promoting Health in Underserved Populations: Advancing Healthy Aging,” sponsored by the Center for Health Promotion and Disease Prevention Research in Underserved Populations, funded by the National Institutes of Health, National Institute of Nursing Research (P30 NR005051). The editorial assistance of Fredrick C. Shopfner, MSW, MFA, is acknowledged. The National Institute on Aging supported this research (grant R01 AG15384).
REFERENCES
- 1.Federal Interagency Forum on Aging Related Statistics . Older Americans 2004: Key Indicators of Well-being. US Government Printing Office; Washington, DC: 2004. [Google Scholar]
- 2.McPherson S, LaRue A, Fitz A, Matsuyama S, Jarvik LF. Self-reports of memory problems in relatives of patients with probable Alzheimer’s disease. International Psychogeriatrics. 1995;7(3):367–376. doi: 10.1017/s1041610295002110. [DOI] [PubMed] [Google Scholar]
- 3.Salthouse TA. Memory aging from 18 to 80. Alzheimer Disease and Associated Disorders. 2003;17(3):162–167. doi: 10.1097/00002093-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Smith AD. Memory. In: Birren JE, editor. Encyclopedia of Gerontology: Age, Aging, and the Aged. Academic Press; San Diego: 1996. pp. 107–117. [Google Scholar]
- 5.McDougall GJ. Cognitive interventions among older adults. Annual Review of Nursing Research. 1999;17:219–240. [PMC free article] [PubMed] [Google Scholar]
- 6.McDougall GJ. Memory improvement program for elderly cancer survivors. Geriatric Nursing. 2001;22(4):185–190. doi: 10.1067/mgn.2001.117916. [DOI] [PubMed] [Google Scholar]
- 7.Cohen G. Everyday memory. In: Cohen G, editor. Memory in the Real World. Erlbaum; Hillsdale, NJ: 1989. pp. 1–15. [Google Scholar]
- 8.Gathercole SE, Collins AF. Everyday memory research and its applications. Applied Cognitive Psychology. 1992;6:461–465. [Google Scholar]
- 9.West RL, Crook TH, Barron KL. Everyday memory performance across the life span: effects of age and noncognitive individual differences. Psychology and Aging. 1992;7(1):72–82. doi: 10.1037//0882-7974.7.1.72. [DOI] [PubMed] [Google Scholar]
- 10.McDougall G, Becker H, Arheart KL. Older adults in the SeniorWISE study at-risk for mild cognitive impairment. Archives of Psychiatric Nursing. 2006;20(3):126–134. doi: 10.1016/j.apnu.2005.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McDougall GJ, Vaughan P, Acee T, Becker H. Memory performance, depression, and mild cognitive impairment in Black and White community elders. Ethnicity and Disease. 2007;17(2):381–388. [PMC free article] [PubMed] [Google Scholar]
- 12.Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment—beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. Journal of Internal Medicine. 2004;256(3):240–246. doi: 10.1111/j.1365-2796.2004.01380.x. [DOI] [PubMed] [Google Scholar]
- 13.Salthouse TA, Mitchell DRD. Effects of age and naturally occurring experience on spatial visualization performance. Developmental Psychology. 1990;26:845–854. [Google Scholar]
- 14.Salthouse TA, Berish DE, Miles JD. The role of cognitive stimulation on the relations between age and cognitive functioning. Psychology and Aging. 2002;17(4):548–557. doi: 10.1037//0882-7974.17.4.548. [DOI] [PubMed] [Google Scholar]
- 15.Bigee ML. How does learning transfer to new situations? In: Bigee ML, Shermis SS, editors. Learning Theories for Teachers. 6th ed. Longman; New York: 1999. pp. 211–235. [Google Scholar]
- 16.Salthouse TA. Mental exercise and mental aging: evaluating the validity of the “use it or lose it” hypothesis. Perspectives on Psychological Science. 2006;1(1):68–87. doi: 10.1111/j.1745-6916.2006.00005.x. [DOI] [PubMed] [Google Scholar]
- 17.Baltes PB. On the incomplete architecture of human ontogeny. Selection, optimization, and compensation as foundation of developmental theory. American Journal of Psychology. 1997;52(4):366–380. doi: 10.1037//0003-066x.52.4.366. [DOI] [PubMed] [Google Scholar]
- 18.Freund AM, Baltes PB. Selection, optimization, and compensation as strategies of life management: correlations with subjective indicators of successful aging. Psychology and Aging. 1998;13(4):531–543. doi: 10.1037//0882-7974.13.4.531. [DOI] [PubMed] [Google Scholar]
- 19.Woodruff-Pak DS. Aging and intelligence: changing perspectives in the twentieth century. Journal of Aging Studies. 1989;3(2):91–118. [Google Scholar]
- 20.Subcommittee on Brain and Behavioral Sciences . Maximizing Human Potential: Decade of the Brain 1990-2000. US Department of Health and Human Services; Washington, DC: 1991. [Google Scholar]
- 21.Eriksson PS, Perfilieva E, Björk-Eriksson T, et al. Neurogenesis in the adult human hippocampus. Nature Medicine. 1998;4(11):1313–1317. doi: 10.1038/3305. [DOI] [PubMed] [Google Scholar]
- 22.Fuchs E, Gould E. In vivo neurogenesis in the adult brain: regulation and functional implications. European Journal of Neuroscience. 2000;12(7):2211–2214. doi: 10.1046/j.1460-9568.2000.00130.x. [DOI] [PubMed] [Google Scholar]
- 23.Baltes PB, Singer T. Plasticity and the ageing mind: an exemplar of the bio-cultural orchestration of brain and behavior. European Review. 2001;1:59–76. [Google Scholar]
- 24.Gaze RM, Taylor JSH. Plasticity in the nervous system. In: Gregory RL, editor. The Oxford Companion to the Mind. Oxford University Press; Oxford: 1987. pp. 623–628. [Google Scholar]
- 25.Greenwood PM. Functional plasticity in cognitive aging: review and hypothesis. Neuropsychology. 2007;21(6):657–673. doi: 10.1037/0894-4105.21.6.657. [DOI] [PubMed] [Google Scholar]
- 26.Wingfield A, Grossman M. Language and the aging brain: patterns of neural compensation revealed by functional brain imaging. Journal of Neurophysiology. 2006;96(6):2830–2839. doi: 10.1152/jn.00628.2006. [DOI] [PubMed] [Google Scholar]
- 27.Freedman VA, Hodgson N, Lynn J, et al. Promoting declines in the prevalence of late-life disability: comparisons of three potentially high-impact interventions. Milbank Quarterly. 2006;84(3):493–520. doi: 10.1111/j.1468-0009.2006.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lawrence RH, Jette AM. Disentangling the disablement process. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1996;51(4):S173–S182. doi: 10.1093/geronb/51b.4.s173. [DOI] [PubMed] [Google Scholar]
- 29.Kozorovitskiy Y, Gould E. Adult neurogenesis: a mechanism for brain repair? Journal of Clinical and Experimental Neuropsychology. 2003;25(5):721–732. doi: 10.1076/jcen.25.5.721.14580. [DOI] [PubMed] [Google Scholar]
- 30.Bandura A. Social cognitive theory: an agentic perspective. Annual Review of Psychology. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 31.Bandura A. Regulation of cognitive processes through perceived self-efficacy. Developmental Psychology. 1989;25(5):729–735. [Google Scholar]
- 32.Berry JM, West RL. Cognitive self-efficacy in relation to personal mastery and goal setting across the life span. International Journal of Behavioral Development. 1993;16(2):351–379. [Google Scholar]
- 33.Berry JM. Cognitive efficacy across the life span: introduction of the special series. Developmental Psychology. 1989;25(5):683–686. [Google Scholar]
- 34.Artistico D, Cervone D, Pezzuti L. Perceived self-efficacy and everyday problem solving among young and older adults. Psychology and Aging. 2003;18(1):68–79. doi: 10.1037/0882-7974.18.1.68. [DOI] [PubMed] [Google Scholar]
- 35.McDougall GJ. Memory self-efficacy and memory performance in Black and White community elders. Nursing Research. 2004;53(5):323–331. doi: 10.1097/00006199-200409000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McDougall GJ. Predictors of metamemory in older adults. Nursing Research. 1994;43(4):212–218. [PMC free article] [PubMed] [Google Scholar]
- 37.McDougall GJ. Increasing memory strategy use and self-efficacy in Hispanic elders. Clinical Gerontologist. 1998;19(2):57–76. doi: 10.1300/j018v19n02_05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McDougall GJ. Rehabilitation of memory and memory self-efficacy in cognitively impaired nursing home residents. Clinical Gerontologist. 2001;23(34):127–139. doi: 10.1300/J018v23n03_11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McDougall GJ. Memory improvement in octogenarians. Applied Nursing Research. 2002;15(1):2–10. doi: 10.1053/apnr.2002.29518. [DOI] [PubMed] [Google Scholar]
- 40.Austin-Wells V, McDougall GJ, Becker H. Recruiting and retaining an ethnically diverse sample of older adults in a longitudinal intervention study. Educational Gerontology. 2006;32:159–170. doi: 10.1080/03601270500388190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McDougall GJ, Montgomery KS, Eddy N, et al. Aging memory self-efficacy: elders share their thoughts and experience. Geriatric Nursing. 2003;24(3):162–168. doi: 10.1067/mgn.2003.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bandura A, Locke EA. Negative self-efficacy and goal effects revisited. Journal of Applied Psychology. 2003;88(1):87–99. doi: 10.1037/0021-9010.88.1.87. [DOI] [PubMed] [Google Scholar]
- 43.Bandura A. The primacy of self-regulation in health promotion. Applied Psychology An International Review. 2005;54(2):245–254. [Google Scholar]
- 44.Rebok GW, Balcerak LJ. Memory self-efficacy and performance differences in young and old adults: the effect of mnemonic training. Developmental Psychology. 1989;25(5):714–721. [Google Scholar]
- 45.Best DL, Hamlett KW, Davis SW. Memory complaint and memory performance in the elderly: the effects of memory skills training and expectancy change. Applied Cognitive Psychology. 1992;6:405–416. [Google Scholar]
- 46.Lachman ME, Steinberg ES, Trotter SD. Effects of control beliefs and attributions on memory self-assessments and performance. Psychology and Aging. 1987;2(3):266–271. doi: 10.1037//0882-7974.2.3.266. [DOI] [PubMed] [Google Scholar]
- 47.Lachman ME, Weaver SL, Bandura M, Elliott E, Lewkowic CJ. Improving memory and control beliefs through cognitive restructuring and self-generated strategies. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1992;47(5):P293–P299. doi: 10.1093/geronj/47.5.p293. [DOI] [PubMed] [Google Scholar]
- 48.Dellefield KS, McDougall GJ. Increasing metamemory in community elderly. Nursing Research. 1996;45(5):284–290. doi: 10.1097/00006199-199609000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sliwinski M, Lipton RB, Buschke H, Stewart W. The effects of preclinical dementia on estimates of normal cognitive functioning in aging. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1996;51B(4):P217–P225. doi: 10.1093/geronb/51b.4.p217. [DOI] [PubMed] [Google Scholar]
- 50.Swabb DF. Brain aging and Alzheimer’s disease, “wear and tear” versus “use it or lose it.”. Neurobiology of Aging. 1991;12:317–324. doi: 10.1016/0197-4580(91)90008-8. [DOI] [PubMed] [Google Scholar]
- 51.Greiner PA, Snowdon DA, Schmitt FA. The loss of independence in activities of daily living: the role of low normal cognitive function in elderly nuns. American Journal of Public Health. 1996;86(1):62–66. doi: 10.2105/ajph.86.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mortimer JA. Brain reserve and the clinical expression of Alzheimer’s disease. Geriatrics. 1997;52(suppl 2):S50–S53. [PubMed] [Google Scholar]
- 53.Scarmeas N, Stern Y. Cognitive reserve and lifestyle. Journal of Clinical and Experimental Neuropsychology. 2003;25(5):625–633. doi: 10.1076/jcen.25.5.625.14576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stine-Morrow EA, Parisi JM, Morrow DG, Greene J, Park DC. An engagement model of cognitive optimization through adulthood. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2007;62B(special no 1):62–69. doi: 10.1093/geronb/62.special_issue_1.62. [DOI] [PubMed] [Google Scholar]
- 55.Floyd M, Scogin F. Effects of memory training on the subjective memory functioning and mental health of older adults: a meta-analysis. Psychology and Aging. 1997;12(1):150–161. doi: 10.1037//0882-7974.12.1.150. [DOI] [PubMed] [Google Scholar]
- 56.Verhaeghen P, Marcoen A, Goossens L. Improving memory performance in the aged through mnemonic training: a meta-analytic study. Psychology and Aging. 1992;7(2):242–251. doi: 10.1037//0882-7974.7.2.242. [DOI] [PubMed] [Google Scholar]
- 57.Stigsdotter Neely A, Backman L. Maintenance of gains following multifactorial and unifactorial memory training in late adulthood. Educational Gerontology. 1993;19:105–117. [Google Scholar]
- 58.Stigsdotter Neely A, Backman L. Effects of multifactorial memory training in old age: generalizability across tasks and individuals. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1995;50B(3):P134–P140. doi: 10.1093/geronb/50b.3.p134. [DOI] [PubMed] [Google Scholar]
- 59.West RL. Planning practical memory training for the aged. In: Poon LW, Rubin DC, Wilson BA, editors. Everyday Cognition in Adulthood and Late Life. Cambridge University Press; Cambridge: 1989. pp. 573–597. [Google Scholar]
- 60.Anschutz L, Camp CJ, Markley RP, Kramer JJ. Remembering mnemonics: a three-year follow-up on the effects of mnemonics training in elderly adults. Experimental Aging Research. 1987;13:141–143. doi: 10.1080/03610738708259315. [DOI] [PubMed] [Google Scholar]
- 61.Hayslip B, Maloy RM, Kohl R. Long-term efficacy of fluid ability interventions with older adults. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1995;50B(3):P141–P149. doi: 10.1093/geronb/50b.3.p141. [DOI] [PubMed] [Google Scholar]
- 62.Scogin F, Bienanias J. A three-year follow-up of older adult participants in a memory skill-skills training program. Psychology and Aging. 1988;3:334–337. doi: 10.1037//0882-7974.3.4.334. [DOI] [PubMed] [Google Scholar]
- 63.Stigsdotter Neely A, Backman L. Long-term maintenance of gains from memory training in older adults: two 3½-year follow-up studies. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1993;48B(3):P233–P237. doi: 10.1093/geronj/48.5.p233. [DOI] [PubMed] [Google Scholar]
- 64.Sheikh J, Hill RD, Yesavage JA. Long-term efficacy of cognitive training for age-associated memory impairment: a 6-month follow-up study. Developmental Neuropsychology. 1986;2:413–421. [Google Scholar]
- 65.Oswald WD, Rupprecht R, Gunzelmann T, Tritt K. The SIMA-project: effects of 1 year cognitive and psychomotor training on cognitive abilities of elderly. Behavioural Brain Research. 1996;78:67–72. doi: 10.1016/0166-4328(95)00219-7. [DOI] [PubMed] [Google Scholar]
- 66.Willis SL, Nesselroade CS. Long term effects of fluid ability training in old-old age. Developmental Psychology. 1990;26:905–910. [Google Scholar]
- 67.Willis SL, Blieszner R, Baltes PB. Intellectual training research in aging: modification of performance on the fluid ability of figural relations. Journal of Educational Psychology. 1981;73(1):41–50. [Google Scholar]
- 68.Yesavage JA. Imagery pretraining and memory training in the elderly. Gerontology. 1983;29:271–275. doi: 10.1159/000213126. [DOI] [PubMed] [Google Scholar]
- 69.Yesavage JA. Relaxation and memory training in 39 elderly patients. American Journal of Psychiatry. 1984;141(6):778–781. doi: 10.1176/ajp.141.6.778. [DOI] [PubMed] [Google Scholar]
- 70.Yesavage JA, Rose TL, Spiegel D. Relaxation training and memory improvement in elderly normals: correlation of anxiety ratings and recall improvement. Experimental Aging Research. 1982;8(4):195–197. doi: 10.1080/03610738208260365. [DOI] [PubMed] [Google Scholar]
- 71.Yesavage JA, Jacob R. Effects of relaxation and mnemonics on memory, attention, and anxiety in the elderly. Experimental Aging Research. 1984;10(4):211–214. doi: 10.1080/03610738408258467. [DOI] [PubMed] [Google Scholar]
- 72.Baltes PB, Kliegel R, Dittmann-Kohli F. On the locus of training gains in research on the plasticity of fluid intelligence in old age. Journal of Educational Psychology. 1988;80(3):392–400. [Google Scholar]
- 73.Baltes PB, Sowarka D, Kliegel R. Cognitive training research on fluid intelligence in old age: what can older adults achieve by themselves? Psychology and Aging. 1989;4(2):217–221. doi: 10.1037/0882-7974.4.2.217. [DOI] [PubMed] [Google Scholar]
- 74.Dittmann-Kohli F, Lachman ME, Kliegl R, Baltes P. Effects of cognitive training and testing on intellectual efficacy beliefs in elderly adults. Journal of Gerontology. 1991;46(4):162–164. doi: 10.1093/geronj/46.4.p162. [DOI] [PubMed] [Google Scholar]
- 75.Willis SL, Blieszner R, Baltes PB. Intellectual training research in aging: modification of performance on the fluid ability of figural relations. Journal of Educational Psychology. 1981;73(1):41–50. [Google Scholar]
- 76.Willis SL, Schaie KW. Training the elderly on the ability factors of spatial orientation and inductive reasoning. Psychology and Aging. 1986;1(3):239–247. doi: 10.1037//0882-7974.1.3.239. [DOI] [PubMed] [Google Scholar]
- 77.Willis SL, Jay GM, Diehl M, Marsiske M. Longitudinal change and prediction of everyday task competence in the elderly. Research on Aging. 1992;14:68–91. doi: 10.1177/0164027592141004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ball K, Berch DB, Helmers KF, et al. Advanced cognitive training for independent and vital elderly study group. The Journal of the American Medical Association. 2002;288(18):2271–2281. [Google Scholar]
- 79.Willis SL, Tennstedt SL, Marsiske M, et al. Long-term effects of cognitive training on everyday functional outcomes in older adults. The Journal of the American Medical Association. 2006;296(23):2805–2814. doi: 10.1001/jama.296.23.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bandura A. Self-efficacy: The Exercise of Control. WH Freeman & Co; New York: 1997. [Google Scholar]