Abstract
Objective
The purpose of this study was to determine the normal morphometric landmarks of the uniting and dividing points of the brachial plexus (BP) in the periclavicular region to provide useful guidance in surgery of BP injuries.
Methods
A total of 20 brachial plexuses were obtained from 10 adult, formalin-fixed cadavers. Distances were measured on the basis of the Chassaignac tubercle (CT), and the most lateral margin of the BP (LMBP) crossing the superior and inferior edge of the clavicle.
Results
LMBP was located within 25 mm medially from the midpoint in all subjects. In the supraclavicular region, the upper trunk uniting at 21 ± 7 mm from the CT, separating into divisions at 42 ± 5 mm from the CT, and dividing at 19 ± 4 mm from the LMBP crossing the superior edge of the clavicle. In the infraclavicular region, the distance from the inferior edge of the clavicle to the musculocutaneous nerve (MCN) origin was 49 ± 1 mm, to the median nerve origin 57 ± 7 mm, and the ulnar nerve origin 48 ± 6 mm. From the lateral margin of the pectoralis minor to the MCN origin the distance averaged 3.3 ± 10 mm. Mean diameter of the MCN was 4.3 ± 1.1 mm (range, 2.5-6.0) in males (n = 6), and 3.1 ± 1.5 mm (range, 1.6-4.0) in females (n = 4).
Conclusion
We hope these data will aid in understanding the anatomy of the BP and in planning surgical treatment in BP injuries.
Keywords: Brachial plexus, Musculocutaneous nerve, Clavicle, Pectoralis muscles
INTRODUCTION
The avulsed or damaged brachial plexus (BP) resulting from traffic or industrial accidents is increasingly common. Various surgical options have been applied to restore shoulder abduction and elbow flexion in cases of complete or incomplete loss of motor and sensory function (i.e., a flailing arm)3,9,10).
In the case of incomplete injuries, neurotization can be applied to the damaged nerve at the appropriate time. However, in the case of a complete injury, the spinal accessory nerve, the intercostal nerve, or the pectoral nerves are used for neurotization to the musculocutaneous nerve (MCN)4,5,12,15,17). In reality, however, it is difficult for the surgeon to find the sites of the uniting and dividing points of the nerve roots, especially when they are stretched or moved by various damage patterns19).
There is considerable diversity of opinion regarding anatomical landmarks for the BP. Some suggest that dissection should be performed up to the branching point of the nerve root14). However, it is typically difficult to establish where the branch is. Some reports indicate that the supraclavicular triangle or the pectoralis minor muscle should be regarded as the anatomical landmark, but this is not helpful to surgeons who lack practical experience in the operation. Thus, it is necessary to establish anatomical landmarks so that surgeons can readily predict where branches of nerves are in the BP, enabling them to approach the target region rapidly and accurately.
The purpose of this study was to provide the anatomical landmarks to provide insight into the structure of the BP in the periclavicular region. The superior and inferior edges of the clavicle and the inferolateral margin of the pectoralis minor muscle were chosen as landmarks. The distance was measured between the dividing point and the uniting point of each nerve trunk, especially the distance from the inferior edge of clavicle to the exit point of the MCN and to the uniting point with the median nerve. Additionally, authors have examined whether there are sex differences in the diameter of the MCN, which is usually used for nerve transfer in neurotization.
MATERIALS AND METHODS
Ten adult cadavers (6 males, 4 females) were examined. The mean height of the male cadavers was 160 cm and that of the female cadavers was 158 cm. The scalenus anterior muscle, the sternocleidomastoid muscle, and the pectoralis major muscle were removed, preserving the clavicle. The BP above and below the clavicle was exposed from the anterior tubercle of the cervical transverse process to the upper arm. One muscular and three osseous points were selected as anatomical landmarks : the anterior tubercle of the 6th cervical transverse process (the so-called Chassaignac tubercle, CT); the superior edge of the clavicle at the point where the most lateral margin of the BP passes under the clavicle; the inferior edge of the clavicle at the same point; and the point where the most lateral margin of the BP (LMBP) meets the inferolateral margin of the muscle when it passes under the pectoralis minor muscle (Fig. 1).
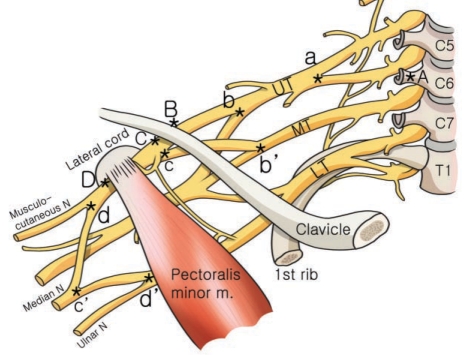
Fig. 1.
Schematic drawing showing the anatomical landmarks of the brachial plexus. A : chassaignac tubercle, B : superior edge of clavicle, C : inferior edge of clavicle, D : inferolateral margin of pectoralis minor muscle, a : uniting point with the upper trunk (UPUT), b : dividing point of the upper trunk into the division (DPUT), b' : dividing point of the middle trunk into the division (DPMT), c : uniting point with the lateral cord (UPLC), c' : uniting point with the median nerve (UPMN), d : the exit point of the musculocutaneous nerve, d' : uniting point with the ulnar nerve (UPUN). UT : upper trunk, MT : middle trunk, LT : lower trunk.
The following distances were measured using a caliper, in the supraclavicular region : the distance from CT to the uniting point with the upper trunk (UPUT)(Fig. 2), to the dividing point of the upper trunk (DPUT) into the division, and to the dividing point of the middle trunk (DPMT) into the division. Next, the distance from the superior edge of the clavicle to the UPUT (Fig. 3) and the distance from the superior edge of clavicle to the DPUT.
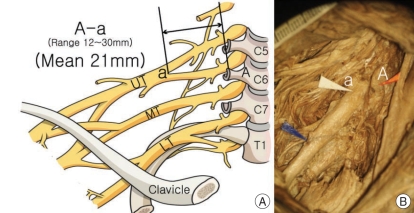
Fig. 2.
Schematic drawing (A) and cadaveric specimen (B) showing the distance from the Chassaignac tubercle to the uniting point of the upper trunk (A-a, mean, 21 mm).
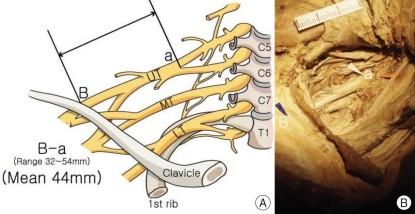
Fig. 3.
Schematic drawing (A) and cadaveric specimen (B) showing the distance from the superior edge of clavicle to uniting point of upper trunk (B-a, mean, 44 mm).
In the infraclavicular region, the followings were measured : the distance from the inferior edge of the clavicle to the uniting point with the lateral cord (UPLC), to the exit point of the MCN (Fig. 4), to the uniting point of median nerve (UPMN), and to the uniting point with the ulnar nerve (UPUN); and from the inferolateral margin of the pectoralis minor muscle to the exit point of the MCN (Fig. 5). The diameters of the MCN and those of the lateral branches of the median nerves were measured at the point where the lateral cord branched. The diameters of the two nerves were analyzed by sex.
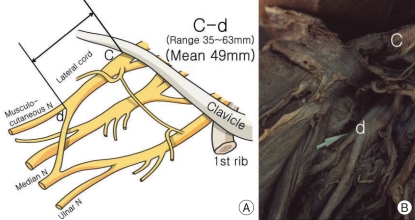
Fig. 4.
Schematic drawing (A) and cadaveric specimen (B) showing the distance from inferior edge of the clavicle to the exit point of the musculocutaneous nerve (C-d, mean, 49mm).
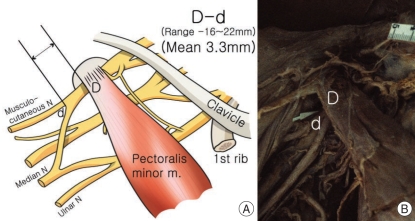
Fig. 5.
Schematic drawing (A) and cadaveric specimen (B) showing the distance from the inferior margin of the pectoralis minor muscle to the exit point of the musculocutaneous nerve (D-d, mean, 3.3 mm).
RESULTS
Gross findings
There was no significant difference in the arm length. In the BP, prefixed forms were difficult to clearly distinguish from postfixed ones. In particular, it was very difficult to establish the course of the T1 root. It was also not easy to find the small branches, such as the suprascapular nerve.
The most LMBP was within 25 mm of the midpoint of the clavicle. In relationship to the subclavian and axillary arteries, the BP encircled the medial, lateral, and posterior surfaces of the axillary artery. However, it was difficult to find the anterior and posterior divisions of the branch of the nerve trunk.
Measurements of the BP in the supraclavicular region
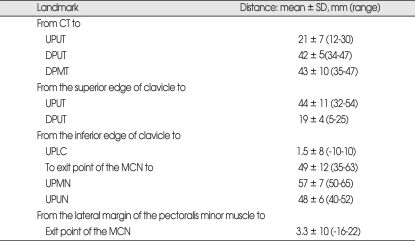
The average distance from the CT to the UPUT was 21 ± 7 mm. The average distance from the CT to the DPUT was 42 ± 5 mm; the latter is about double the former. Also, the average distance from the CT to the DPMT was similar to the distance from the CT to the DPUT (43 ± 10 mm). The average distance from the superior edge of the clavicle to the UPUT was 44 ± 11 mm and to the DPUT was 19 ± 4 mm (Table 1).
Table 1.
Distances measured from the bony and muscular landmarks to the uniting and dividing points of brachial plexus
CT : Chassaignac tubercle, DPMT : dividing point of the middle trunk into the division, DPUT : dividing point of the upper trunk into the division, MCN : musculocutaneous nerve, UPLC : uniting point with the lateral cord, UPMN : uniting point with the median nerve, UPUN : uniting point with the ulnar nerve, UPUT : uniting point with the upper trunk
Measurement of the BP in the infraclavicular region
The distance from the inferior edge of the clavicle to the UPLC was 1.5 ± 8 mm on average. The UPLC was 10 mm proximal or distal to the inferior edge of the clavicle. Specifically, most of the lateral cords were formed around the inferior edge of the clavicle. The distance from the inferior edge of the clavicle to the exit point of the MCN was 49 ± 12 mm, on average. The average distance from the inferior edge of the clavicle to the UPMN was 57 ± 7 mm. On average, the distance from the inferior edge of the clavicle to the UPUN was 48 ± 6 mm. The exit point of the MCN was, on average, 3.3 ± 10 mm from the lateral margin of the pectoralis minor muscle. In most cases, the MCNs exited at the lateral margin of the pectoralis minor muscle. In most cases, MCNs exited at a point 22 mm distal to the lateral margin of the pectoralis minor muscle, rather than 16 mm proximal to the lateral margin of the muscle (Table 1).
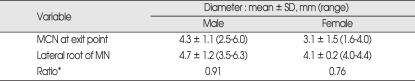
Diameter of the MCN
The diameter of the MCN, which comes out from the lateral cord and enters into the septum of the coracobrachialis muscle, was measured. The MCNs of males were significantly thicker than those of females. The diameter of the MCN, exiting from the lateral cord, was measured, as was the diameter of the lateral branch of the median nerve. In the males, the diameter of the MCN was approximately equivalent to that of the lateral root of the median nerve (91%). However, in the females, the ratio of diameter of the MCN/diameter of the lateral root of median nerve was 76%. Thus, male MCNs were thicker than female MCNs (Table 2).
Table 2.
Diameters of the MCN and lateral root of median nerve by gender
*diameter of the MCN/diameter of the lateral root of MN. MCN : musculocutaneous nerve, MN : median nerve
DISCUSSION
BP injuries can result from trauma, such as stretches or contusions with or without avulsion; gunshot wounds; and lacerations. Non-traumatic injury can occur from tumors and thoracic outlet syndrome of various etiologies. Brachial palsy may also result from obstetric birth injuries11). With regard to damage to the BP, microsurgeries have been performed on the basis of electrophysiological examinations or by operating microscopy. Nevertheless, such surgeries can result in serious motor or sensory disturbances. Youngsters, in particular, who have most of their lives in front of them, may suffer from permanent disability1,2). However, recently, these operations have had increasingly successful outcomes, in part due to accurate planning and appropriate timing of surgery2,8).
To recover such function and to regrow the axon, neurorrhaphy, cable grafting, or neurotization is typically performed. In such cases, proximal muscles, such as the deltoid, the biceps brachii, the triceps brachii, and the brachioradialis muscles, can recover functionally to some degrees; however, this procedure is generally not effective in recovering motor function in the forearm7,9). Such operations have been applied to the upper trunk, the middle trunk, the lateral cord, the posterior cord, and the axillary nerve in the BP, but they have been recently applied to the MCN, which exits from the lateral cord, to allow elbow flexion17). In cases where the middle trunk is used in such operations, the function of the triceps brachii muscle can be recovered.
It is essential to precisely understand the complicated anatomical structure of the BP to apply these surgical procedures to the damaged BP. To do this, fresh cadavers should ideally be used in measuring distances. However, for various reasons, cadavers treated with formalin were used in this study.
The ventral rami of the C5, C6, C7, C8, and the T1 nerve roots comprise most of the brachial plexuses. Some reports state that the C7 and the C8 nerve roots have the largest ventral rami18), but others have reported that the largest are associated with the C6 and the C7 nerve roots13). Morphometrically, the BP is centered on the C4 nerve root and consists of the C5, C6, C7, and the C8 nerve roots. Some refer to a "prefixed-type" BP as a case where the T1 nerve root is hardly involved, and a "postfixed-type" BP as a case where the C5 nerve root is small, but the C6, C7, C8, T1, and T2 nerve roots are involved. Uysal et al.20) reported that a prefixed plexus was observed in 25.5%, and a postfixed plexus was observed in 2.5% of human fetuses. It is generally agreed that two types are not significant clinically16), although Slingluff et al.18) emphasized that the type should be accurately predicted preoperatively so that an appropriate surgical guideline could be established. They reported that the type could be predicted by understanding the size and shape of the C5 nerve root, through preoperative electromyography and radiologic examination. In this study, however, it was not possible to distinguish the prefixed from the postfixed type.
The nerve root can be deformed by excessively incising connective tissue at the point where nerves are branched, but tissue malformation is found in about 6% and dissymmetry in about 38% of cases21). Malformation is rarely observed around nerve roots, but is common around nerve trunks and each cord. There are also cases where the upper trunk and the middle trunk immediately transit to the lateral cord, cases where the lateral cord and the middle trunk simultaneously form the anterior cord, and even cases where all nerve roots form a only one cord21).
The anterior rami root of the BP exits the intervertebral foramen (IVF) and goes through the scalenus anterior and the middle scalenus muscle via the sulcus nervi spinalis of the transverse process at grade. Next, it forms the upper trunk at the anterolateral surface of the middle scalenus. The C8 nerve root and the T1 nerve root form the lower trunk at the back of the medial margin of the 1st rib, the so-called Sibson's fascia. The three nerve trunks are connected to each other around the 1st rib.
The upper trunk and the middle trunk lie below one-third of the subclavian artery. The lower trunk is found behind the subclavian artery. The point where the nerve trunks are divided into the anterior and the posterior divisions is relevant to the point where the nerve trunk crosses the 1st rib, a point that lies above one-third of the axillary artery and the proximal margin of the clavicle21). Also, without mentioning its relationship to the surrounding tissues, these are described that the uniting points of the each cord lie just above the infrascapular muscle.
The lateral cord lies lateral to one-third of the axillary artery, and the medial cord lies medially along one-third of it. The posterior cord lies behind one-third of it. It has been reported that blood vessels and nerves are laid regularly21). The exit point of the MCN from the lateral cord is around the lateral margin of the pectoralis minor muscle. In 87% of cases, the UPMN, the lateral branch of the medial cord, meets the median branch of the lateral cord and is formed below one-third of the axillary artery. The brachial artery can also be a useful anatomical landmark; the medial cord and the lateral cord join with each other in a Y-shape at the anterior part of the brachial artery and form the median nerve. The entire axillary artery and the brachial artery should be exposed so that the pathway from the nerve trunk to the cord can be observed. In the process, the pectoralis major muscle should be moved from the deltopectoral groove, along the muscle fiber. Simultaneously, the pectoralis minor muscle should be incised. In rare cases, the clavicle should be incised invasively. In cases where the region is damaged due to contusion or hyperextension, the anatomical structure can be excessively distorted making it difficult to establish these positions. As a result, it can be very difficult to approach the deeper parts of the BP. According to the literature14), the branches of the BP are laid around the subclavian artery and the axillary artery, at the anterior part, the posterior part, or behind the brachial artery. Others have reported anatomical landmarks centered on the coracoid process, the pectoralis minor muscle, the scalenus anterior, or even the posterior triangle. However, these anatomical landmarks are vague. In contrast, the anatomical landmarks in this study are objective and can be useful in understanding the anatomical structure.
Bonnel et al.6) measured the lengths of the branches of the BP and reported that adult BPs varied. They also reported that, on average, the uniting point of the nerve trunks was 43 mm from the IVF of the C5 nerve root. This point was 50 mm distant from that of the C6 nerve root. The point was also 58 mm from the IVF of the C7 nerve root to the DPMT. However, the dividing point of the C7 nerve root was not accurately determined. The length of the lateral cord was 60 mm, and that of the medial cord was 50 mm on average. However, the uniting point with the posterior cord could be observed in only 20% of cases.
Slingluff et al.18) measured the number, length, and thickness of nerve trunks and analyzed the distribution of motor nerve fibers and sensory nerve fibers at each nerve trunk and peripheral nerve. They reported that most of motor nerve fibers lay at the anterior part of the nerve root, 20-30 mm distant from the IVF. As motor nerve fibers account for 82% of the posterior cord, it is effective to recover its function through neurorrhaphy. Moreover, motor nerve fibers account for 77%, 41%, and 36% of the radial nerve, the ulnar nerve, and the median nerve respectively.
The diameters of MCNs, which exit the lateral cord and enter into the septum of the coracobrachialis muscle, were measured. It was found that the MCNs in males were significantly thicker than in females. The reason may be that the male brachial biceps and brachioradialis muscles are bigger than those in females. To ascertain whether differences in diameter affect operative manipulation and postoperative recovery, the number of fascicles should be compared with that of axons systematically.
CONCLUSION
When the BP passes the clavicle, the LMBP was at least 25 mm distant from the midpoint of clavicle. The UPUT was 21 ± 7 mm from the CT, and was 44 ± 11 mm distant from the superior edge of the clavicle. The DPUT was 42 ± 5 mm from the CT, and 19 ± 4 mm from the superior edge of clavicle. The lateral cord is formed at the inferior edge of the clavicle. The exit point of the MCN was 49 ± 13 mm distal from the inferior edge of the clavicle. The distance from the UPMN and UPUN to the inferior edge of clavicle was similar. The MCN exited from the lateral cord at the inferolateral margin of the pectoralis minor muscle. The MCNs in males were thicker than those in females.
References
- 1.Ahmed-Labib M, Golan JD, Jacques L. Functional outcome of brachial plexus reconstruction after trauma. Neurosurgery. 2007;61:1016–1022. doi: 10.1227/01.neu.0000303197.87672.31. discussion 1022-1023. [DOI] [PubMed] [Google Scholar]
- 2.Belzberg AJ, Dorsi MJ, Storm PB, Moriarity JL. Surgical repair of brachial plexus injury : a multinational survey of experienced peripheral nerve surgeons. J Neurosurg. 2004;101:365–376. doi: 10.3171/jns.2004.101.3.0365. [DOI] [PubMed] [Google Scholar]
- 3.Bertelli JA, Ghizoni MF. Brachial plexus avulsion injury repairs with nerve transfers and nerve grafts directly implanted into the spinal cord yield partial recovery of shoulder and elbow movements. Neurosurgery. 2003;52:1385–1389. doi: 10.1227/01.neu.0000065134.21334.d7. discussion 1389-1390. [DOI] [PubMed] [Google Scholar]
- 4.Bertelli JA, Ghizoni MF. Improved technique for harvesting the accessory nerve for transfer in brachial plexus injuries. Neurosurgery. 2006;58:ONS-366–ONS-370. doi: 10.1227/01.NEU.0000205286.70890.27. discussion ONS-370. [DOI] [PubMed] [Google Scholar]
- 5.Blaauw G, Slooff AC. Transfer of pectoral nerves to the musculocutaneous nerve in obstetric upper brachial plexus palsy. Neurosurgery. 2003;53:338–341. doi: 10.1227/01.neu.0000073420.66113.66. discussion 341-342. [DOI] [PubMed] [Google Scholar]
- 6.Bonnel F, Rabischong P. Anatomy and systematization of the brachial plexus in the adult. Anat Clin. 1981;2:289–298. [Google Scholar]
- 7.Guha A, Graham B, Kline DG, Hudson AR. Brachial plexus injuries. In: Wilkins RH, Rengachary SS, editors. Neurosurgery. 2nd ed. New York: McGraw-Hill; 1996. pp. 3121–3122. [Google Scholar]
- 8.Haninec P, Sámal F, Tomás R, Houstava L, Dubóvwy P. Direct repair (nerve grafting), neurotization, and end-to-side neurorrhaphy in the treatment of brachial plexus injury. J Neurosurg. 2007;106:391–399. doi: 10.3171/jns.2007.106.3.391. [DOI] [PubMed] [Google Scholar]
- 9.Harris M, Tindall SC. Surgical anatomy and exposures of the peripheral nervous system. In: Tindall GT, Cooper PR, editors. The practice of neurosurgery. Vol 3. Philadelpbia: Lippincott Williams & Wilkins; 1996. pp. 2831–2836. [Google Scholar]
- 10.Kawai H, Kawabata H, Masada K, Ono K, Yamamoto K, Tsuyuguchi Y, et al. Nerve repairs for traumatic brachial plexus palsy with root avulsion. Clin Orthop Relat Res. 1988;237:75–86. [PubMed] [Google Scholar]
- 11.Kim DH, Murovic JA, Kline DG. Brachial plexus injury : mechanisms, surgical treatment and outcomes. J Korean Neurosurg Soc. 2004;36:177–185. [Google Scholar]
- 12.Kline DG, Judice DJ. Operative management of selected brachial plexus lesions. J Neurosurg. 1983;58:631–649. doi: 10.3171/jns.1983.58.5.0631. [DOI] [PubMed] [Google Scholar]
- 13.Lee HY, Chung IH, Sir WS, Kang HS, Lee HS, Ko JS, et al. Variations of the ventral rami of the brachial plexus. J Korean Med Sci. 1992;7:19–24. doi: 10.3346/jkms.1992.7.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGillicuddy JE. Neurosurgery Clinics of North America. 1991. Surgical anatomy and management of brachial plexus injury; pp. 2860–2863. [PubMed] [Google Scholar]
- 15.Narakas AO, Hentz VR. Neurotization in brachial plexus injuries. Indication and results. Clin Orthop Relat Res. 1988:43–56. [PubMed] [Google Scholar]
- 16.Parent A. Carpenter's human neuroanatomy. ed 9. Philadelphia: Lippincott, Williams & Wilkins; 1966. pp. 275–283. [Google Scholar]
- 17.Samii M, Carvalho GA, Nikkhah G, Penkert G. Surgical reconstruction of the musculocutaneous nerve in traumatic brachial plexus injuries. J Neurosurg. 1997;87:881–886. doi: 10.3171/jns.1997.87.6.0881. [DOI] [PubMed] [Google Scholar]
- 18.Slingluff CL, Terzis JK, Edgerton MT. The quantitative microanatomy of the brachial plexus in man. In: Terzis JK, editor. Microreconstruction of nerve injury. WB Saunders; 1987. pp. 285–324. [Google Scholar]
- 19.Tender GC, Kline DG. Anterior supraclavicular approach to the brachial plexus. Neurosurgery. 2006;58:ONS-364–ONS-365. doi: 10.1227/01.NEU.0000209027.52848.A3. discussion ONS-364-ONS-365. [DOI] [PubMed] [Google Scholar]
- 20.Uysal II, Seker M, Karabulut AK, Büyükmumcu M, Ziylan T. Brachial plexus variations in human fetuses. Neurosurgery. 2003;53:676–684. doi: 10.1227/01.neu.0000079485.24016.70. discussion 684. [DOI] [PubMed] [Google Scholar]
- 21.Wolock B, Millesi H. Brachial plexus-applied anatomy and operative exposure. In: Gelberman RH, editor. Operative nerve repair and reconstruction. Lippincott; 1991. pp. 1255–1272. [Google Scholar]