Abstract
Intradural lumbar disc herniation (ILDH) is rare. In this report, authors present 2 cases of ILDHs associated with severe adhesion between the dural sac and posterior longitudinal ligament. In a 40-year-old man, ILDH occurred in association with epidural adhesion due to ossification of the posterior longitudinal ligament (OPLL). In other 31-year-old man, ILDH occurred in presence of epidural adhesion due to previous spine surgery.
Keywords: Intradural lumbar disc herniation, Ossification of posterior longitudinal ligament, Epidural adhesion
INTRODUCTION
Intradural lumbar disc herniation (ILDH) is rare and the incidence is reported as 0.04-0.33% of lumbar disc herniations4,5). Although the pathogenesis of intradural disc herniation is not certain, adhesion between the dura mater and posterior longitudinal ligament (PLL) has been accepted as a predisposing factor2-4). Authors experienced 2 ILDHs associated with severe adhesion between the dura mater and PLL. One patient had ILDH associated with severe ossification of posterior longitudinal ligament (OPLL) and the other patient had ILDH associated with epidural adhesion due to previous spine surgery. The aim of our report was to introduce our surgical experiences of ILDHs associated with severe epidural adhesion and discuss the pathogenesis and diagnosis of ILDH with a literature review.
CASE REPORT
Case 1
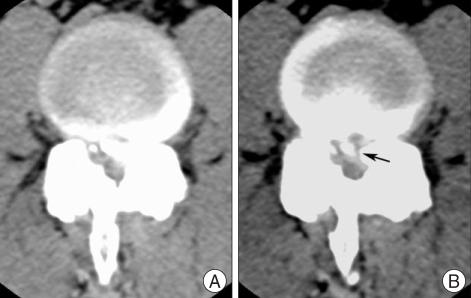
A 40-year-old man was admitted with paraplegia and urinary incontinence that had gradually progressed over 7 days. The neurological examination revealed cauda equina syndrome showing motor weakness in both legs (Grade I), hypesthesia below the L3 dermatome, loss of knee and ankle jerk, and bladder and bowel dysfunction. The computed tomography (CT) scan revealed severe spinal canal stenosis with OPLL and bony spur involving both facets at L2-3 level (Fig. 1). Magnetic resonance imaging (MRI) revealed the mixed form of OPLL and posterocentral disc extrusion with a beak-like appearance and spinal canal stenosis with OPLL at L2-3 level. Gadolinium-enhanced MRI shows no enhancement on extruded disc fragments or surrounding tissue. Intradural disc herniation was not recognized through MRI or CT scan.
Fig. 1.
Preoperative computed tomography shows severe ossification of the posterior longitudinal ligament with bony degenerative changes involving bilateral facets at L2-3 level (Case 1). A defect is seen in the ossification of the posterior longitudinal ligament and the disc is suspected to be herniated through it (black arrow).
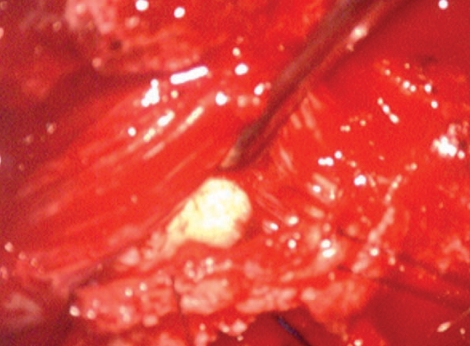
Subtotal laminectomy was performed at L2-3 level and severe adhesion between the dura mater, OPLL, and degenerative bony spur were noted. Under microscopy, the OPLL and bony spur were drilled out and discectomy was performed. After decompression and discectomy, the dural sac was tense and the intradural mass was palpated. An intradural disc fragment beneath the rootlets was removed through midline durotomy (Fig. 2). A ventral dural defect was identified and repaired using dura-allograft. Additionally, pedicle screw instrumentation and posterolateral bony fusion were performed because of wide facetectomy and discectomy. Postoperatively, motor power of both legs gradually improved (Grade III). Three years after the operation, the patient can walk using a cane.
Fig. 2.
The intraoperative finding of Case 1 after opening the dural sac. The cauda equine nerve rootlets are displaced laterally by a large intradural disc fragment.
Case 2
A 31-year-old man was admitted with radiating pain in the left leg. The patient had a past history of laminotomy and discectomy on left L4-5 and L5-S1 levels, 13 years ago. The patient revisited the hospital, 10 years after surgery, because of recurrent left leg pain. MRI revealed recurred disc herniation at L4-5 level. A T2-weighted axial image revealed a disc fragment that extruded with a tear drop appearance toward the left side (Fig. 3). The symptom resolved with conservative management. Three years after recurrence, the patient revisited the outpatient clinic, complaining of severe radiating pain in his left leg. At this moment, the neurological examination revealed 30 degrees of straight leg raising test and Grade III motor power in dorsiflexion of left big toe. MRI showed that the previous disc fragment extruded further compared to the image of the previous MRI. Gadolinium-enhanced MR image showed peripheral rim enhancement at the sequestrated fragment (Fig. 3).
Fig. 3.
T2 weighted magnetic resonance images 3 years ago show recurred disc herniation with a tear drop appearance and the continuity between the intradural disc and extradural disc at the L4-5 levels (A and B). The preoperative gadolinium-enhanced magnetic resonance images show sequestrated disc fragment with rim enhancement and progression compared with the images from 3 years ago (C and D) (Case 2).
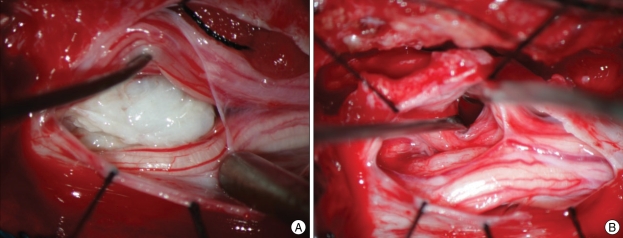
Subtotal laminectomy, medial facetectomy, and foraminotomy were performed at L4-5 level. Severe adhesion and fibrosis due to the previous surgery was found between the dura mater and PLL. At first, adhesiolysis and complete discectomy were performed. Nevertheless, the dural sac was still tense and intradural mass was palpated. Intradural disc fragments were removed through midline durotomy (Fig. 4). A ventral dural defect was identified and repaired using dura-allograft. After complete discectomy, posterior lumbar interbody fusion was performed using an expandable cage. Postoperatively, radiating pain resolved completely and motor power of the left great toe gradually improved (Grade IV).
Fig. 4.
The intraoperative finding of Case 2 after opening the dural sac. The cauda equine nerve rootlets are displaced laterally by a large intradural disc fragment (A) and a dural defect is seen on the ventral dura after removal of the intradural disc fragment (B).
DISCUSSION
Intradural disc herniation is rare condition and comprises 0.27% of all disc herniations5,7). In 92% of cases, intradural disc herniations occur in the lumbar region and the most affected site is the L4-5 (55%), followed by L3-4 (16%), and L5-S1 (10%)3,7). ILDHs at L2-3 or L1-2 levels, such as our case (Case 1), are rarely reported.
Although the pathogenesis of intradural disc herniation is not certain, congenital or acquired adhesion between the dural sac and PLL has been accepted as a predisposing factor2-4). Yildizhan et al.10) suggested prenatal adhesion formation between the PLL and dural sac in cadaver study. However, congenital union as the cause of intradural disc herniation is controversial because it is difficult clinically to prove the existence of a congenital union in patients with ILDH. Instead, acquired adhesion through previous surgery or chronic herniated disc may be accepted as the main cause of intradural disc herniation1,8). Previous surgery is the definite predisposing factor for intradural disc herniation and approximately 15% of patients in reported cases had past history of previous lumbar surgery3,8). Chronic herniated disc is another possible cause of adhesion. Chronic inflammation on herniated disc can cause adhesion and thinning of the dura, which results in intradural rupture. We think that the hypothesis of chronic inflammation due to a preexisting disc herniation is most applicable in patients without past history of surgery because many patients with ILDH had a several-month to year history of lower back pain and typical MRI finding of ILDH is rim enhancement of a disc fragment, which implies chronic inflammation. In case 2, the patient had both predisposing factors of epidural adhesion due to previous surgery and chronic herniated disc. Severe adhesion around the dural sac and PLL due to previous surgery was seen in the operative field, and dissection of the dural sac and nerve root was very difficult. In Case 1, in particular, ILDH occurred in epidural adhesion associated with OPLL. OPLL also can be a predisposing factor for ILDH because OPLL itself can adhere to the dura mater and thin it. However, ILDH associated with OPLL is very rare because OPLL is not common in the lumbar region and the hardness of OPLL can act as a strong barrier that prevents intradural rupture. Although approximately 140 cases of intradural disc herniation have been reported, as much as we are aware, the case of ILDH associated OPLL presented here is the first report. For occurrence of ILDH, we speculate that the disc fragment extruded into the dural sac through a small defect in the OPLL. A small defect in the OPLL was seen on the preoperative CT scan, but we failed to identify the defect intraoperatively.
MRI finding of ILDH is important for its preoperative identification. Since Wasserstrom et al.9) first made a diagnosis of intradural disc herniation by a gadolinium-enhanced MRI in 1993, rim enhancement of herniated disc has been accepted as a typical MRI finding of intradural disc herniation2). In our second case, rim enhancement of the herniated disc was also seen on the gadolinium-enhanced MRI. However, a gadolinium-enhanced MRI is not routinely performed and acute herniated disc shows no rim enhancement6). Therefore, we think the usefulness of gadolinium-enhanced MRI is limited in the differential diagnosis of intradural disc herniation when intradural lesions are suspected on non-enhanced MRI. Choi et al.2) presented loss of continuity of PLL and a sharp, beak-like appearance on T2-weighted image for the prediction of intradural disc herniation. In spite of these MRI findings of intraudral disc herniation, the preoperative diagnosis of ILDH is difficult due to limited use of gadolinium-enhanced MRI and rarity of ILDH. Therefore, we think that in the diagnosis of intradural disc herniation, suspicion for the possibility of intradural disc herniation and palpation of intradural mass through the dural sac are most important when intraoperative findings are different from MRI findings or the dural sac and root are tense after discectomy.
CONCLUSION
We report 2 rare cases of ILDHs which occurred in condition of severe epidural adhesion due to OPLL and previous lumbar surgery. Although MRI findings can be helpful for the preoperative diagnosis of ILDH, we think suspicion for the possibility of intradural disc herniation and palpation of the dural sac are most important when intraoperative finding is different from preoperative MRI finding.
References
- 1.Borota L, Jonasson P, Agolli A. Spontaneous resorption of intradural lumbar disc fragments. Spine J. 2008;8:397–403. doi: 10.1016/j.spinee.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 2.Choi JY, Lee WS, Sung KH. Intradural lumbar disc herniation--is it predictable preoperatively? A report of two cases. Spine J. 2007;7:111–117. doi: 10.1016/j.spinee.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 3.D'Andrea G, Trillò G, Roperto R, Celli P, Orlando ER, Ferrante L. Intradural lumbar disc herniations : the role of MRI in preoperative diagnosis and review of the literature. Neurosurg Rev. 2004;27:75–80. doi: 10.1007/s10143-003-0296-3. discussion 81-82. [DOI] [PubMed] [Google Scholar]
- 4.Kataoka O, Nishibayashi Y, Sho T. Intradural lumbar disc herniation. Report of three cases with a review of the literature. Spine (Phila Pa 1976) 1989;14:529–533. [PubMed] [Google Scholar]
- 5.Koç RK, Akdemir H, Oktem IS, Menkü A. Intradural lumbar disc herniation: report of two cases. Neurosurg Rev. 2001;24:44–47. doi: 10.1007/pl00011967. [DOI] [PubMed] [Google Scholar]
- 6.Mailleux R, Redant C, Milbouw G. MR diagnosis of transdural disc herniation causing cauda equine syndrome. . JBR-BTR. 2006;89:303–305. [PubMed] [Google Scholar]
- 7.Oztürk A, Avci E, Yazgan P, Torun F, Yücetaş S, Karabağ H. Intradural herniation of intervertebral disc at the level of Lumbar 1-Lumbar 2. Turk Neurosurg. 2007;17:134–137. [PubMed] [Google Scholar]
- 8.Schisano G, Franco A, Nina P. Intraradicular and intradural lumbar disc herniation : experiences with nine cases. Surg Neurol. 1995;44:536–543. doi: 10.1016/0090-3019(95)00248-0. [DOI] [PubMed] [Google Scholar]
- 9.Wasserstrom R, Mamourian AC, Black JF, Lehman RA. Intradural lumbar disk fragment with ring enhancement on MR. AJNR Am J Neuroradiol. 1993;14:401–404. [PMC free article] [PubMed] [Google Scholar]
- 10.Yildizhan A, Paşaoğlu A, Okten T, Ekinci N, Aycan K, Aral O. Intradural disc herniations pathogenesis, clinical picture, diagnosis and treatment. Acta Neurochir (Wien) 1991;110:160–165. doi: 10.1007/BF01400685. [DOI] [PubMed] [Google Scholar]