Abstract
Objective
Chronic subdural hematoma (CSDH) is one of the most common types of traumatic intracranial hemorrhage, usually occurring in the older patients, with a good surgical prognosis. Burr hole craniostomy is the most frequently used neurosurgical treatment of CSDH. However, there have been only few studies to assess the role of the number of burr holes in respect to recurrence rates. The aim of this study is to compare the postoperative recurrence rates between one and two burr craniostomy with closed-system drainage for CSDH.
Methods
From January 2002 to December 2006, 180 consecutive patients who were treated with burr hole craniostomy with closed-system drainage for the symptomatic CSDH were enrolled. Pre- and post-operative computed tomography (CT) scans and/or magnetic resonance imaging (MRI) were used for radiological evaluation. The number of burr hole was decided by neurosurgeon's preference and was usually made on the maximum width of hematoma. The patients were followed with clinical symptoms or signs and CT scans. All the drainage catheters were maintained below the head level and removed after CT scans showing satisfactory evacuation. All patients were followed-up for at least 1 month after discharge.
Results
Out of 180 patients, 51 patients were treated with one burr hole, whereas 129 were treated with two burr holes. The overall postoperative recurrence rate was 5.6% (n = 10/180) in our study. One of 51 patients (2.0%) operated on with one burr hole recurred, whereas 9 of 129 patients (7.0%) evacuated by two burr holes recurred. Although the number of burr hole in this study is not statistically associated with postoperative recurrence rate (p > 0.05), CSDH treated with two burr holes showed somewhat higher recurrence rates.
Conclusion
In agreement with previous studies, burr hole craniostomy with closed drainage achieved a good surgical prognosis as a treatment of CSDH in this study. Results of our study indicate that burr hole craniostomy with one burr hole would be sufficient to evacuate CSDH with lower recurrence rate.
Keywords: Burr hole, Chronic subdural hematoma, Recurrence
INTRODUCTION
Chronic subdural hematoma (CSDH) is one of the most common types of traumatic intracranial hematoma, and often occurs in the elderly4,5,20). Surgical treatment has been widely accepted as the most effective way to manage CSDH. Although general agreement for indication of surgical treatment is obtained, the optimal method has not been obtained yet8,10,12,15). Craniotomy, burr hole craniostomy and other various surgical techniques have been used for years. Considering the simplicity of procedure, operative risks and efficacy, evacuation through burr hole becomes the procedure of choice in many hospitals, but the reported recurrence rate ranges from 9.2 to 26.5% after surgical evacuation1,5,6,8,14,17,25). And, there are many studies about numerous factors potentially associated with recurrences after the surgical procedures which are still highly controversial8,12,20).
Generally, CSDH in adults are evacuated and flushed via a single or two burr-hole craniostomy frequently followed by closed-system drainage20). However, definite indication for number of burr holes is not established and it mostly depends on neurosurgeon's preference.
In this study, we compared the postoperative recurrence rates between one and two burr hole craniostomy with closed-system drainage, considering the some of the known potential risk factors of CSDH recurrence.
MATERIALS AND METHODS
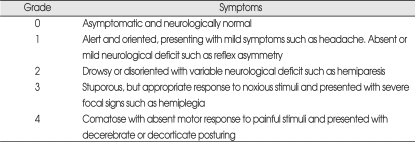
From January 2002 to December 2006, 180 consecutive patients (129 men and 51 women) with CSDH underwent burr hole craniostomy with closed-system drainage at our hospital were retrospectively enrolled in this study. Two patients at the age of 2 months and 1 year were excluded from the study. Three additional patients treated with craniotomy were excluded. Patients were neurologically classified according to Markwalder Grading Scale (Table 1) and Glasgow Coma Scale (GCS).
Table 1.
Clinical grades according to the markwalder grade Scale
CSDH was defined as the presence of a typical neomembrane, liquefied blood within the hematoma cavity, and at least 3 weeks had passed from the event of head trauma. Diagnosis was confirmed by computed tomography (CT) scans and/or magnetic resonance (MR) images in all patients. Operations were performed under either general or local anesthesia. All patients underwent surgical procedures of one or two burr holes over the area of maximal hematoma width and closed-system drainage with the commercial silicone catheter and bag. The selection of the number of burr hole was made by the attending neurosurgeon's preference. Subdural hematoma was spontaneously evacuated after burr hole trephination and the drainage catheter was inserted. A little or no warm saline irrigation through silicone catheter was performed in the cases of one burr hole craniostomy. On the other hand, much irrigation was performed via each burr holes in two burr hole craniostomy until the irrigation return became clear. All patients had closed-system drainage and immediate postoperative CT scans. The patients were mostly old with other medical problems and the most frequent postoperative medical complication was pneumonia17). Therefore, they kept in a position with the head of the bed elevated to 30 to 40 degrees to minimize respiratory distress. All drainage bags were maintained below the head level and removed according to the change of the drainage volume and radiological findings, but mostly removed within 5 days to avoid the complications associated with drainage catheter. Brain CT scans were performed preoperatively, postoperatively and at final follow-up in all cases.
Clinical and/or radiological criteria were used for evaluation of CSDH recurrence. Also, both the clinical and/or radiological criteria were used for determining reoperation. The clinical criteria for recurrence included a change in mental status, worsening of the preexisting neurological deficit and new onset or aggravation of headache. And, the radiological criteria were the CT scans during the follow-up period postsurgically revealed an increased subdural collection and/or the brain parenchyma was compressed compared to the findings of the immediate postoperative CT scans. That is, patients underwent reoperation if neurological symptoms recurred, and/or if the patients developed new neurological symptoms, with the increase in hematoma thickness and volume on follow-up CT scans as defined above. Those who showed no or minimal neurological deficit postoperatively or who had a small amount of residual hematoma were discharged and were followed-up as outpatients.
Statistical analysis was assessed by the Student t-test and chi-square test using SPSS software (version 12.0; SPSS Inc.). Throughout the analysis, a p value of less than 0.05 was considered significant.
RESULTS
Demographic characteristics
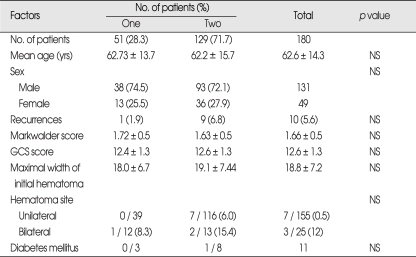
There were a total of 180 patients, 131 men (72.8%, median age 61.7 ± 13.4 years) and 49 women (27.2%, median age 64.9 ± 16.4 years) in the study, ranging in age from 17 from 96 years (median age, 62.6 ± 14.3 years). The demographic characteristics and clinical findings are shown in Table 2.
Table 2.
Comparison of demographic and related factors : one vs. two burr holes
The mean GCS at admission was 12.6 ± 1.3. Fifty-one (28.3%, median age 62.73 ± 13.7 years) and 129 patients (71.7%, median age 62.2 ± 15.7 years) were managed with one and two burr hole craniostomy, respectively.
Among 180 operated patients, 10 patients were reoperated because of recurrence. All patients who recurred had burr hole craniostomy with closed-system drainage. The patients were followed-up for at least 1 month after discharge. The decision to reoperate was determined according to the clinical and/or radiological evidence of recurrence. The mean duration between initial and the repeated operation was 18.8 days which ranged from 4 to 38 days. Seven patients with unilateral CSDH underwent reoperation on previous operation site and 3 patients with bilateral CSDH managed with bilateral burr hole craniostomy had repeated unilateral burr hole craniostomy because of recurrence.
One vs. two burr holes
As mentioned above, 10 patients experienced postoperative recurrences : 5 men (50%) and 5 women (50%) in this study and ranging in age from 51 to 77 years (median age, 67.8 years). The overall postoperative recurrence rate was 5.6% (3.8 % in men and 9.4% in women). Although female had a higher recurrence rate than male, it was statistically non-significant (p > 0.05). The recurrence rates of one and two burr hole craniostomy were 1.89% (n = 1) and 6.82% (n = 9), respectively. Patients treated with two burr hole craniostomy had a higher rate of recurrence than those of one burr hole craniostomy. However, the number of burr holes as a risk factor of CSDH recurrence was not statistically significantly associated with postoperative recurrence rate (p > 0.05)
Three of 25 (12%) with bilateral CSDH and 7 of 155 (0.5%) with unilateral CSDH patients were recurred (p = 0.13). Thirty-nine patients with unilateral CSDH was managed without recurrence by one burr hole craniostomy. Among the 116 patients with two burr holes, 7 patients were reoperated. One of 12 patients treated with one burr hole in bilateral CSDH underwent reoperation, while 2 of 13 patients with two burr holes recurred.
Related factors for recurrence
We performed multivariate analysis between recurrence and following variables : sex (p = 0.96), age (p = 0.99), GCS score, the site of hematoma (unilateral or bilateral) (p = 0.13), maximal width of hematoma (p = 0.46), number of burr holes (p = 0.18) and diabetes mellitus (p = 0.59). The expected potential risk factors included in this study were not statistically significant (p > 0.05).
DISCUSSION
CSDHs generally occur in older patients by a relatively light trauma and usually at least 3 weeks passed from the event of trauma unnoticed. The annual incidence of CSDH has been steadily increasing. Weber24) reported an annual incidence of CSDH in Switzerland was approximately 1 per 50,000-100,000 in 1969. In 2001, Cousseau et al.3) found an annual incidence of 3.1 per 100,000 people in Argentina. And Lind et al.12) in New Zealand reported 4.6 per 100,000, recently. This can be explained by the fact that the older population have been increased according to the development of medical technology6,18).
Various types of managements including conservative and surgical treatment have been used as a management of CSDH. Currently, conservative management is selected usually for moribund patients with significant comorbidity or asymptomatic patients with a small hematoma among many neurosurgeons. Mostly, literatures have supported a surgical treatment19,25). Burr hole craniostomy is a simple, widely used technique with overall morbidity of 0 to 9%4,5,12,14).
The surgical procedure of authors' hospital is as follows: one or two burr holes are usually drilled and hematoma is spontaneously evacuated. The hematoma is repeatedly irrigated with warm saline by means of nelathon catheter inserted in several directions until the irrigation return became clear. At the end of the procedure, the drainage catheter is inserted and left in the hematoma cavity.
Craniotomy, more invasive technique with greater morbidity than burr hole craniostomy, has no significant difference in the incidence of postoperative recurrence5,6,16,18). Nevertheless, craniotomy as a management of CSDH has indications as followings : solid hematoma and multiple recurrences19).
Recently, burr hole craniostomy as a most widely used surgical treatment of CSDH has been supported in the literatures. The rationale for this has been based on evidences that treatment with burr holes has at least equivalent outcome as compared to craniotomy, but has much lower mortality and morbidity and a shorter postoperative hospital stay11,12,19).
The reported rate of reoperation was 7.9 to 33% in the patients with burr hole craniostomy, not significantly higher than with the craniotomy5,7,16,18,20,22,23). The main reasons for reoperation were residual thick hematoma membranes followed by reaccumulation of subdural fluid due to residual hematoma or to rebleeding4).
One vs. two burr holes
One or two burr-hole craniostomy with closed-system drainage have been generally used as a primary treatment of CSDH in most institutes, recently16). One burr hole craniostomy takes shorter operation time and less invasive than that of two burr-hole craniostomy. But, it is often less efficient to evacuate the hematoma, especially in cases of separated type of CSDH and/or thick hematoma. Yamamoto et al.25) demonstrated that the irrigation with one burr hole is usually sufficient to wash out the hematoma in multiple cavities. They concluded that in most cases of CSDH, multiplicity did not mean multiple closed cavities and that all hematoma cavities were continuous with relatively wide routes of wide connection. Nagakuchi et al.14) demonstrated that the catheter tip located in the frontal showed better surgical outcome in one burr craniostomy with closed-system drainage and irrigation. The recurrence rates were 5% in frontal region, 38% in parietal region, 36% in occipital region and 33% at the temporal base. In this study, all of patients with the tip of catheter in frontal region were not recurred. Among patients with one burr hole, only one of 5 patients with the tip of catheter in parietal region underwent recurrence.
Two burr-hole craniostomy is useful to evacuate hematoma through repeated irrigations. Kuroki et al.10) have compared 'closed-system drainage with irrigation' (n = 45) with 'strict closed-system drainage' (n = 56) in CSDH managements, and found five recurrences in the former and one in the latter group. The result suggested that postoperative residual intracapsular air is a factor of recurrence which was statistically significant (p < 0.05). But, there is lack of general agreement as to what is the exact role of postoperative subdural air in the recurrence of CSDH.
In our study, patients operated on with one burr hole had lower postoperative recurrence rate than those of two burr holes (1.89 vs. 6.82%), although it was not statistically significant (p > 0.05). There is hypothesis for higher postoperative recurrence rate after two burr craniostomy as in our study. While we performed repeated saline irrigations via two burr holes, one burr hole patients were less irrigated. Thus, the patients with one burr hole might have decreased tendency to accumulate postoperative subdural air. Amirjamshidi et al.2) reported that the persistence of the postoperative subdural cavity is a risk factor for reaccumulation of the hematoma and the presence of postoperative residual air prevents reduction of the cavity. Oishi et al.15) demonstrated irrigation should be avoided to prevent complications caused by a sudden decrease in intracranial pressure and intraoperative invasion. Taussky et al.22) reported that patients operated on with one burr hole had a statistically significant higher rate of recurrence, wound infection and longer hospital stay. The theoretical explanation for higher recurrence rate of one burr craniostomy is following : the residual hematoma fluid contains large concentrations of vasoactive cytokines, inflammatory mediator and fibrinolytic factors. The complete evacuation of hematoma seems to be directly linked to the success of surgical procedure. Thus, two burr hole is more efficient to flush out subdural fluid collection19,21).
Related factors for recurrence
Many risk factors for recurrences of CSDH have been reported previously, including age, history of trauma, bleeding tendency, brain atrophy, alcohol abuse, bilateral CSDHs, higher hematoma density, postoperative air accumulation and some technical aspects of surgery. However, the results reported have sometimes been inconsistent1,2,13,19,24).
Some authors have regarded older age is one of the risk factors of CSDH recurrence, while other do not agree7). The results in this study are consistent with the non-agreement group.
Markwalder grade score and GCS score on admission have been considered as a risk factor of recurrence in previous studies. Amirjamshidi et al.2) evaluated the role of GCS scores in the recurrence of CSDH. The results showed that GCS scores had a strong association with CSDH recurrence. Also, a study demonstrated significant correlations between GCS/GOS and CT scan findings in CSDH. Lee et al.11) reported that the duration of postoperative brain re-expansion was not only related with immediate brain re-expansion or pulsation during operation, but also preoperative GCS score.
The width of a hematoma is usually determined at the level of its maximum thickness and has been reported to be correlated with patient age. This result is attributed to the brain atrophy associated with aging, which provides the hematoma with space in which to grow. Yamamoto et al.25) and Kang et al.7) demonstrated that larger hematomas had a greater tendency to recur because postoperative subdural space was larger than that found after removal of a small hematoma. Kang et al.7) evaluated 302 patients with CSDH. Among the recurrent group, the one with a width greater than 2 cm was significantly higher than that of below 2 cm (p < 0.05). However, in agreement with a previous reports2,19), hematoma thickness on the preoperative imaging studies were found not to affect postoperative recurrence rate significantly in this study.
Three of 25 (12%) with bilateral CSDH and 7 of 155 (0.5%) with unilateral CSDH patients were recurred in present study. As mentioned earlier, bilateral CSDH showed higher recurrence rate which was not statistically significant (p > 0.05). It is still unclear that a hematoma location is associated with CSDH recurrence. Kurokawa et al.9) concluded that the bilateral CSDH should be treated as early as possible with bilateral decompression of hematoma pressure, even if the patients showed no or minor neurological deficits.
Suzuki and Takaku21) reported that osmotherapy performed using 20% mannitol was effective in preventing repeated bleeding of a CSDH. In the same fashion, the blood of patients with DM has a high osmotic pressure and increased platelet aggregation and this suggests that DM may contribute to decrease the rebleeding tendency of a CSDH and the recurrence of CSDH25).
The present study was a non-randomized, retrospective study, and thus is potentially subject to sources of bias and variation. Further investigations with larger sample size, quantitative controlled prospective study are required to assess the role of number of burr hole as a independent risk factor of CSDH recurrence.
CONCLUSION
In agreement with previous reports, the surgical outcome after burr hole craniostomy with closed-system drainage as a treatment of CSDH was fairly good. The patients who treated with two burr hole craniostomy had higher incidence rates of recurrence than those with one burr hole craniostomy, but statistically not significant. We conclude that CSDH can be efficiently evacuated by one burr hole craniostomy which is less invasive procedure and takes shorter operation time, even with lower recurrence rate.
References
- 1.Abouzari M, Rashidi A, Rezaii J, Esfandiari K, Asadollahi M, Aleali H, et al. The role of postoperative patient posture in the recurrence of traumatic chronic subdural hematoma after burr-hole surgery. Neurosurgery. 2007;61:794–797. doi: 10.1227/01.NEU.0000298908.94129.67. discussion 797. [DOI] [PubMed] [Google Scholar]
- 2.Amirjamshidi A, Abouzari M, Eftekhar B, Rashidi A, Rezaii J, Esfandiari K, et al. Outcomes and recurrence rates in chronic subdural hematoma. Br J Neurosurg. 2007;21:272–275. doi: 10.1080/02688690701272232. [DOI] [PubMed] [Google Scholar]
- 3.Cousseau DH, Echevarria MG, Gaspari M, Gonorazky SE. [Chronic and subacute subdural hematoma. An epidemiological study in a captive population] Rev Neurol. 2001;32:821–824. [PubMed] [Google Scholar]
- 4.Ernestus RI, Beldzinski P, Lanfermann H, Klug N. Chronic subdural hematoma : surgical treatment and outcome in 104 patients. Surg Neurol. 1997;48:220–225. doi: 10.1016/s0090-3019(97)80031-6. [DOI] [PubMed] [Google Scholar]
- 5.Jeong CA, Kim TW, Park KH, Chi MP, Kim JO, Kim JC. Retrospective analysis of reoperated patients after chronic subdural hematoma surgery. J Korean Neurosurg Soc. 2005;38:116–120. [Google Scholar]
- 6.Jeong JE, Kim GK, Park JT, Lim YJ, Kim TS, Rhee BA, et al. A clinical analysis of chronic subdural hematoma according to age factor. J Korean Neurosurg Soc. 2000;29:748–753. [Google Scholar]
- 7.Kang MS, Koh HS, Kwon HJ, Choi SW, Kim SH, Youm JY. Factors influencing recurrent chronic subdural hematoma after surgery. J Korean Neurosurg Soc. 2007;41:11–15. [Google Scholar]
- 8.Krupp WF, Jans PJ. Treatment of chronic subdural hematoma with burr-hole craniostomy and closed drainage. Br J Neurosurg. 1995;9:619–627. doi: 10.1080/02688699550040909. [DOI] [PubMed] [Google Scholar]
- 9.Kurokawa Y, Ishizaki E, Inaba K. Bilateral chronic subdural hematoma cases showing rapid and progressive aggravation. Surg Neurol. 2005;64:444–449. doi: 10.1016/j.surneu.2004.12.030. discussion 449. [DOI] [PubMed] [Google Scholar]
- 10.Kuroki T, Katsume M, Harada N, Yamazaki T, Aoki K, Takasu N. Strict closed-system drainage for treating chronic subdural hematoma. Acta Neurochir (Wien) 2001;143:1041–1044. doi: 10.1007/s007010170010. [DOI] [PubMed] [Google Scholar]
- 11.Lee SC, Kang JK, Jung HT, Dho JO. Factors affecting brain re-expansion after simple burr hole drainage in chronic subdural hematoma. J Korean Neurosurg Soc. 1998;27:757–762. [Google Scholar]
- 12.Lind CRP, Lind CJ, Mee EW. Reduction in the number of repeated operations for the treatment of subacute and chronic subdural hematomas by placement of subdural drains. J Neurosurg. 2003;99:44–46. doi: 10.3171/jns.2003.99.1.0044. [DOI] [PubMed] [Google Scholar]
- 13.Markwalder TM, Steinsiepe KF, Rohner M, Reichenbach W, Markwalder H. The course of chronic subdural hematomas after burr-hole craniostomy and closed-system drainage. J Neurosurg. 1981;55:390–396. doi: 10.3171/jns.1981.55.3.0390. [DOI] [PubMed] [Google Scholar]
- 14.Nakaguchi H, Tanishima T, Yoshimasu N. Relationship between drainage catheter location and postoperative recurrence of chronic subdural hematoma after burr-hole irrigation and closed-system drainage. J Neurosurg. 2000;93:791–795. doi: 10.3171/jns.2000.93.5.0791. [DOI] [PubMed] [Google Scholar]
- 15.Oishi M, Toyama M, tamatani S, Kitazawa T, Saito M. Clinical factors of recurrent chronic subdural hematoma. Neurol Med Chir(Tokyo) 2001;41:382–386. doi: 10.2176/nmc.41.382. [DOI] [PubMed] [Google Scholar]
- 16.Robinson RG. Chronic subdural hematoma: surgical management in 133 patients. J Neurosurg. 1984;61:263–268. doi: 10.3171/jns.1984.61.2.0263. [DOI] [PubMed] [Google Scholar]
- 17.Rohde V, Graf G, Hassler W. Complication of burr-hole craniostomy and closed-system drainage for chronic subdural hematomas : a retrospective analysis of 376 patients. Neurosurg Rev. 2002;25:89–94. doi: 10.1007/s101430100182. [DOI] [PubMed] [Google Scholar]
- 18.Sambasivan M. An overview of chronic subdural hematoma : experience with 2300 cases. Surg Neurol. 1997;47:418–422. doi: 10.1016/s0090-3019(97)00188-2. [DOI] [PubMed] [Google Scholar]
- 19.Santarius T, Hutchinson PJ. Chronic subdural haematoma : time to rationalize treatment? Br J Neurosurg. 2004;18:328–332. doi: 10.1080/02688690400004845. [DOI] [PubMed] [Google Scholar]
- 20.Stanisic M, Lund-Johansen M, Mahesparan R. Treatment of chronic subdural hematoma by burr-hole craniostomy in adults : influence of some factors on postoperative recurrence. Acta Neurochir (Wien) 2005;147:1249–1256. doi: 10.1007/s00701-005-0616-1. discussion 1256-1257. [DOI] [PubMed] [Google Scholar]
- 21.Suzuki J, Takaku A. Nonsurgical treatment of chronic subdural hematoma. J Neurosurg. 1970;33:548–553. doi: 10.3171/jns.1970.33.5.0548. [DOI] [PubMed] [Google Scholar]
- 22.Taussky P, Fandino J, Landolt H. Number of burr holes as independent predictor of postoperative recurrence in chronic subdural haematoma. Br J Neurosurg. 2008;22:279–282. doi: 10.1080/02688690701818885. [DOI] [PubMed] [Google Scholar]
- 23.Wakai S, Hashimoto K, Watanabe N, Inoh S, Ochiai C, Nagai M. Efficacy of closed-system drainage in treating chronic subdural hematoma : a prospective comparative study. Neurosurgery. 1990;26:771–773. doi: 10.1097/00006123-199005000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Weber G. [Chronic subdural hematoma] Schweiz Med Wochenschr. 1969;99:1483–1488. [PubMed] [Google Scholar]
- 25.Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S. Independent predictors of recurrence of chronic subdural hematoma : results of multivariate analysis performed using a logistic regression model. J Neurosurg. 2003;98:1217–1221. doi: 10.3171/jns.2003.98.6.1217. [DOI] [PubMed] [Google Scholar]