Abstract
Previous study has shown that administration of melatonin into the anterior cingulate cortex contralateral to peripheral nerve injury prevented exacerbation of mechanical allodynia with a concurrent improvement of depression-like behavior in Wistar-Kyoto (WKY) rats, a genetic variation of Wistar rats. In the present study, we examined the effect of the individual versus combined treatment of melatonin and/or dextromethorphan (DM), a clinically available N-methyl-D-aspartate (NMDA) receptor antagonist, on pain behaviors in WKY rats with chronic constriction sciatic nerve injury (CCI). Pain behaviors (thermal hyperalgesia and mechanical allodynia) were established at one week after CCI. WKY rats were then treated intraperitoneally with various doses of melatonin, DM or their combination once daily for the following week. At the end of this one-week treatment, behavioral tests were repeated in these same rats. While DM alone was effective in reducing thermal hyperalgesia at three tested doses (15, 30 or 60 mg/kg), it reduced mechanical allodynia only at high doses (30 or 60 mg/kg). By comparison, administration of melatonin alone was effective in reducing thermal hyperalgesia only at the highest dose (120 mg/kg, but not 30 or 60 mg/kg) tested in this experiment. Melatonin alone failed to reverse allodynia at all three tested doses (30, 60 and 120 mg/kg). However, the combined intraperitoneal administration of melatonin (30 mg/kg) and DM (15 mg/kg) effectively reversed both thermal hyperalgesia and mechanical allodynia although each individual dose alone did not reduce pain behaviors. These results suggest that a combination of melatonin with a clinically available NMDA receptor antagonist might be more effective than either drug alone for the treatment of neuropathic pain.
Keywords: Melatonin, Dextromethorphan, Neuropathic pain, depression
1. Introduction
Injury to the peripheral and/or central nervous system can result in neuropathic pain (Thomas 1984; Woolf and Mannion, 1999). Despite extensive research over years (Arner and Meyerson, 1988; Dubner and Hargreaves, 1989; Kupers et al., 1991; Jadad et al., 1992; Mao et al., 1995a,b; Ossipov et al., 1995; Wegert et al., 1997), neuropathic pain remains very difficult to treat (Watson et al., 1982; Max et al., 1991,1992; Max 1994; Sindrup and Jensen, 1999; Mao and Chen, 2000a,b).
Melatonin (5-methoxy-N-acetyltryptamine), a pineal neurohormone and a derivative of serotonin, regulates important biological functions including circadian rhythms, sleep, and mood (Sugden, 1983; Morgan et al., 1994; Vanecek, 1998; Raghavendra et al., 2000; Von Gall et al., 2002; Zahn et al., 2003; Pandi-Perumal et al., 2006). Melatonin receptors have been localized in the spinal cord and many brain regions (Vitte et al., 1990; Stankov et al., 1991; Morgan et al., 1994; Zahn et al., 2003). Functionally, melatonin produces an antinociceptive effect in rats and mice (Yu et al., 2000a,b; Tu et al., 2004; Onal et al., 2004). Melatonin also reduces lipopolysaccharide-induced hyperalgesia (Raghavendra et al., 2000) and interacts with opioid antinociception (Golombek et al., 1991; Raghavendra and Kulkarni, 2000; Pang et al., 2001; Li et al., 2005; Shavali et al., 2005).
Dextromethorphan (DM) is a low-affinity noncompetitive NMDA (N-methyl-D-aspartate) receptor antagonist and also a commonly used antitussive drug. Low dose of DM (1.25, 2.5, and 5 mg/kg), which did not change baseline nociception, showed a significant antinociceptive effect during both phases of a formalin test (Fazli-Tabaei et al., 2008). However, due to its low efficacy, DM is usually combined with other analgesic agents such as morphine and ketamine for an improved analgesic effect (Galer et al., 2005; Frymoyer et al., 2007; Cohen et al., 2006; Elesen et al., 2007).
A subset of Wistar-Kyoto (WKY) rats, a genetic variation of the Wistar strain (Okamoto and Aoli, 1963; Porsolt et al., 1977, 1978a,b), as well as Flinders sensitive line (FSL) rats (Overstreet et al., 2005), has been used as preclinical models of depression. WKY rats are hypersensitive to stress secondary to disrupted hypothalamic–pituitary–adrenal and hypothalamic–pituitary–thyroid axes. Moreover, WKY rats exhibit an overall decreased activity, few exploratory behaviors, hypolocomotion, and a high level of behavioral immobility in the forced swimming test (Pare, 1993, 1994, 1996; Armario et al., 1995). Pharmacologically, desipramine (a tricyclic antidepressant) acutely reverses depression-like behavior such as a prolonged duration of immobility in the forced swimming test in WKY rats (Porsolt et al., 1978a,b; Lopez-Rubalcava, Lucki, 2000; De La Garza and Mahoney, 2004). In our previous study, we showed that WKY rats demonstrated an exacerbation of mechanical allodynia following chronic constriction sciatic nerve injury (CCI), which was prevented by melatonin administered into the contralateral anterior cingulate cortex with a concurrent improvement of depression-like behavior (Zeng et al., 2008).
In the present study, we compared the effect of individual versus combined treatment of melatonin and/or DM, a clinically available NMDA receptor antagonist, on CCI-induced pain behaviors in WKY rats.
2. Results
Effect of dextromethorphan alone
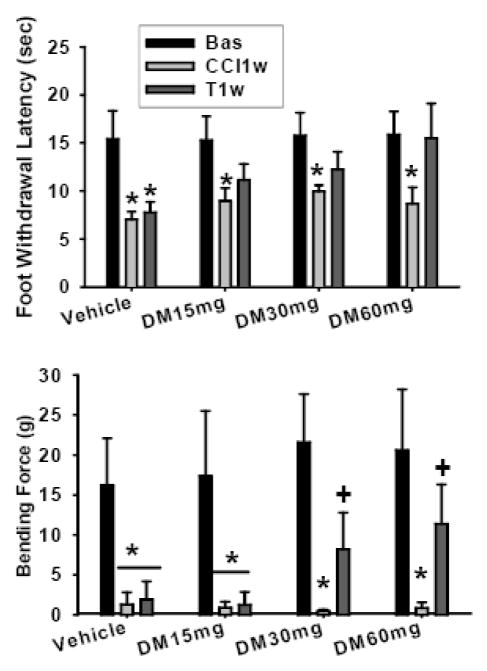
The WKY rats showed thermal hyperalgesia and mechanical allodynia when tested at one week after CCI but not sham operation. Beginning the second week after CCI (i.e., day 8 after CCI), once daily administration of various doses of DM or vehicle was given intraperitoneally for one week. When tested at the end of this one-week treatment (i.e., on day 15 after CCI), thermal hyperalgesia was significantly reduced in each group of WKY rats treated with 15, 30 or 60 mg/kg DM as compared with the baseline in the same group (P< 0.05, Fig. 1a). The vehicle treatment did not change thermal hyperalgesia (P> 0.05, Fig. 1a). Moreover, mechanical allodynia was also improved by two higher doses of DM (30 or 60 mg/kg; P< 0.05, Fig. 1b). Neither a low DM dose (15 mg/kg) nor vehicle alone changed mechanical allodynia (P> 0.05, Fig. 1b). The ED50 dose for the effect of DM was 26.3 mg/kg (Fig. 2). The results indicate that DM was effective in reducing both hyperalgesia and allodynia in WKY rats, particularly at higher doses tested in the experiment.
Fig. 1. Effect of dextromethorphan alone on pain behavior in WKY rats.
Once daily administration of various doses of DM reduced thermal hyperalgesia in each group of WKY rats treated with 15, 30 or 60 mg/kg DM as compared with the baseline (P< 0.05, Fig. 1a). The vehicle treatment did not change thermal hyperalgesia (P> 0.05, Fig. 1a). Mechanical allodynia was improved by two higher doses of DM (30 or 60 mg/kg; P< 0.05, Fig. 1b). Neither a low DM dose (15 mg/kg) nor vehicle alone changed mechanical allodynia (P> 0.05, Fig. 1b). DM15, 30, and 60mg: DM at 15, 30 and 60mg/kg, respectively; Bas, Baseline; CCI1w, 1 week after CCI; T1W, 1 week after CCI followed by 1-week treatment with vehicle or DM. *, P<0.05 as compared with baseline in the same group; +, P<0.05 as compared with CCI1w in the same group.
Fig. 2. The effect of dextromethorphan on pain behavior.
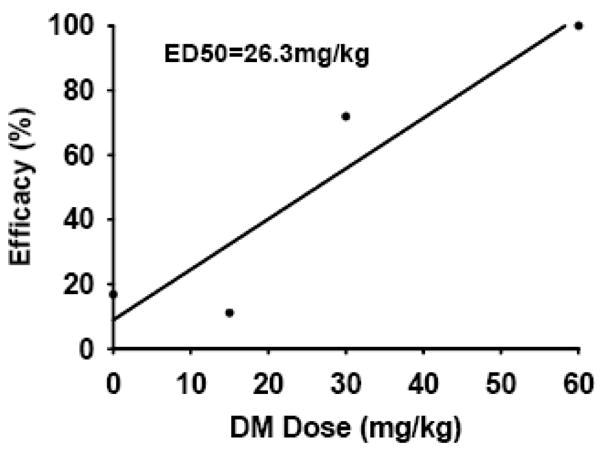
The plot shows that the ED50 dose for DM was 26.3 mg/kg.
Effect of melatonin alone
Using the same treatment regimen as for DM, once daily administration of various doses of melatonin or vehicle was given intraperitoneally for one week, beginning in the second week after CCI (i.e., day 8 after CCI). When tested at the end of this one-week treatment (i.e., on day 15 after CCI), thermal hyperalgesia was significantly reduced only in WKY rats treated with the highest melatonin dose (120 mg/kg; P< 0.05; Fig. 3a) but not 30 or 60 mg/kg melatonin or vehicle, as compared with the baseline of each corresponding group (P> 0.05, Fig. 3a). Moreover, this one-week treatment with melatonin at all three doses (30, 60, 120 mg/kg) failed to relief mechanical allodynia (P> 0.05, Fig. 3b). These results indicate that melatonin alone was largely ineffective in reducing either hyperalgesia or allodynia in WKY rats at the doses tested in this experiment. The ED50 dose for melatonin was not calculated due to the lack of a dose-response relationship.
Fig. 3. Effect of melatonin alone on pain behavior in WKY rats.
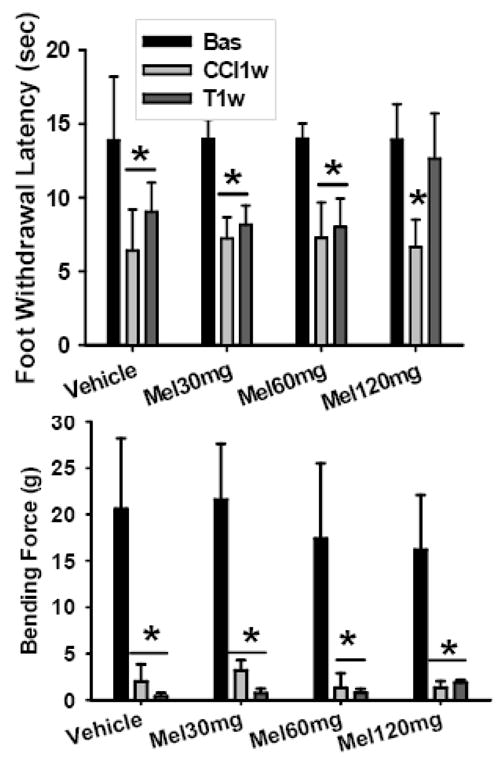
Once daily administration of various doses of melatonin had a limited or no effect on thermal hyperalgesia in each group of WKY rats treated with 30, 60 or 120 mg/kg melatonin as compared with the baseline in the same group. Only the highest dose (120 mg/kg) had an effect (P< 0.05, Fig. 3a). The vehicle treatment did not change thermal hyperalgesia (P> 0.05, Fig. 3a). Mechanical allodynia was not improved by all three doses of melatonin (P> 0.05, Fig. 3b). Mel30, 60 and 120mg: melatonin 30, 60 and 120mg/kg, respectively; Bas, Baseline; CCI1w, 1 week after CCI; T1W, 1 week after CCI followed by 1-week treatment with vehicle or DM. *, P<0.05 as compared with baseline in the same group.
Effect of the combined dextromethorphan and melatonin treatment
To examine whether a combination of DM and melatonin would be more effective than either drug alone in reducing neuropathic pain behaviors, we selected the lowest dose of both drugs (15 mg/kg for DM and 30 mg/kg for melatonin) tested in the above experiments. A single drug or the combination was given intraperitoneally once daily for a week, beginning in the second week after CCI (i.e., day 8 after CCI). While melatonin alone was ineffective, and DM alone was only marginally effective, in reducing thermal hyperalgesia, their combination significantly reduced thermal hyperalgesia as compared with each corresponding baseline (P< 0.05, Fig. 4a), when examined at the end of this one-week treatment (i.e., on day 15 after CCI). Similarly, neither melatonin nor DM alone was effective in reducing mechanical allodynia, but their combination significantly improved mechanical allodynia when examined at the end of this one-week treatment as compared with each corresponding baseline (P< 0.05, Fig. 4b). There were no motor deficits or sedation as judged by the gait and overall appearance of these rats. These results indicate that the combined treatment with melatonin and DM produced the antihyperalgesic and antiallodynic effect in WKY rats in contrast to either of these two drugs administered alone.
Fig. 4. Effect of the combined dextromethorphan and melatonin treatment on pain behavior in WKY rats.
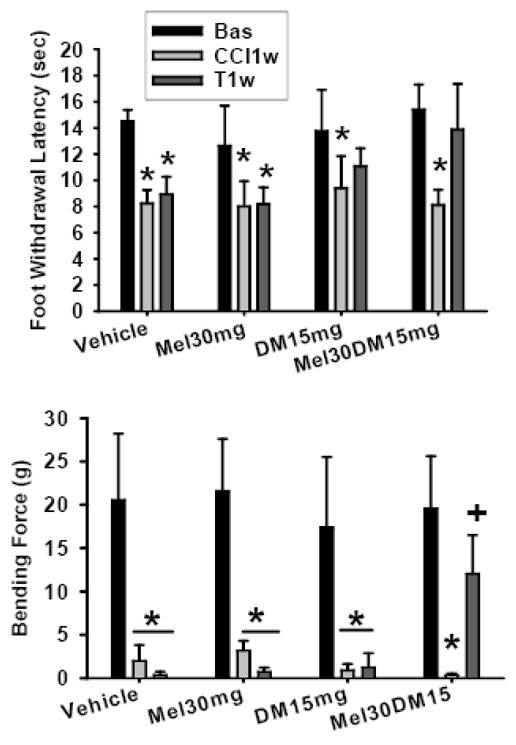
A combination of 15 mg/kg DM and 30 mg/kg melatonin given intraperitoneally once daily for a week was more effective than either drug alone in reducing neuropathic pain behaviors. The combination significantly reduced thermal hyperalgesia (P< 0.05, Fig. 4a) and mechanical allodynia (P< 0.05, Fig. 4b), as compared with their corresponding baseline. Mel30, DM15, Mel30DM15: 30 mg/kg melatonin, 15 mg/kg DM, and 30 mg/kg melatonin combined with 15 mg/kg DM, respectively; Bas, Baseline; CCI1w, 1 week after CCI; T1w, 1 week after CCI followed by 1-week treatment with vehicle, melatonin (Mel) or dextromethorphan (DM) alone, or their combination. *, P<0.05, as compared with baseline in the same group; +, P<0.05 as compared with CCI1w in the same group.
To examine whether these treatment regimens would alter the forced swimming test, indicative of depression-like behavior, rats from these groups were subject to the forced swimming test following the pain behavior test. There were no differences in the time spent in the forced swimming test among these groups with or without treatment (P> 0.05, Fig. 5), suggesting that the effect of melatonin, DM, or their combination, at current dose, on thermal hyperalgesia and mechanical allodynia was not due to a concurrent improvement of depression-like behavior in WKY rats.
Fig. 5. Forced swimming test in WKY rats before and after a drug treatment.
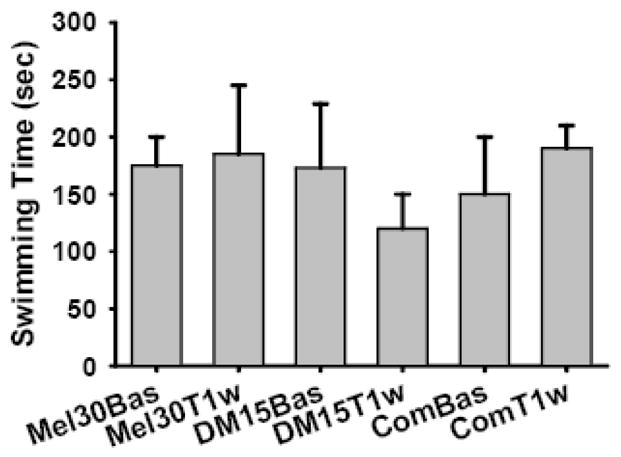
There were no differences in the time spent in the forced swimming test among these groups (P> 0.05, Fig. 5). Mel30Bas and Mel30T1w: baseline and after 1-week treatment with melatonin 30mg/kg, respectively; DM15Bas and DM15T1w: baseline and after 1-week treatment with DM 15mg/kg, respectively; ComBas and ComT1w: baseline and after 1-week treatment with melatonin 30mg/kg and DM 15mg/kg, resepectively. One way ANOVA, P=0.42.
3. Discussion
Using a rat model of peripheral nerve injury, we demonstrated that a combination of a low dose of DM and of melatonin produced a significant reduction of both thermal hyperalgesia and mechanical allodynia in WKY rats, although treatment with either drug alone resulted in marginal, if any, reduction of neuropathic pain behaviors in WKY rats. A technical caveat concerning the present data is that we were unable to conduct an isobolographic analysis of the dose-response relationship between a single versus combined treatment regimen due to the lack of an overall melatonin effect when administered alone in this experiment. Therefore, we could not ascertain whether the combined effect of DM and melatonin on hyperalgesia and allodynia represents a synergistic or additive effect from these two drugs. Nonetheless, our results clearly indicate that the combination of both drugs is more effective than either drug alone in this rat model of neuropathic pain behaviors.
Previous studies have suggested that melatonin may be critically involved in the regulation of both mood and pain (Sugden, 1983). It has been shown that melatonin receptor type 1 (MT1)-knockout mice displayed depression-like behavior with altered sensory responses and attention deficits (Weil et al., 2006). Moreover, melatonin produces antinociception and enhances morphine analgesia mediated through spinal MT receptors (Tu et al., 2004; Li et al., 2005). Clinically, melatonin has been reported to improve cluster headache, irritable bowel syndrome, and fibromyalgia (Waldenlind et al., 1987; Leone et al., 1995, 1996; Citera et al., 2000; Song et al., 2005), although the mechanism of its action remains unclear. Evidence also exists that implicates melatonin in mood regulation (Brzezinski, 1997). For example, clinical depression has been shown to be associated with nocturnal and diurnal changes in the plasma melatonin concentration (Halbreich et al., 1981; Wetterberg, 1985; Beck-Friis et al., 1985; Frazer et al., 1986). Moreover, preclinical studies also indicate that knockout of MT1 receptors increased (Weil et al., 2006), whereas a melatonin analog decreased, the immobility time in the forced swimming test (Overstreet et al., 1998).
DM is a common antitussive drug and also a low-affinity NMDA antagonist (Siu and Drachtman, 2007). DM has been shown to modulate pain behaviors in rats by blocking the activation of NMDA receptors, a known cellular mechanism of pathological pain. For example, intraperitoneal administration of DM (60 mg/kg) produced antinociception during the second phase of a formalin test (Fazli-Tabaei et al., 2008). Moreover, DM has been shown to reduce pain behaviors in various studies (Olesen et al., 2007; Siu and Drachtman, 2007; Frymoyer et al., 2007; Cohen et al., 2006, 2004; Duedahl et al., 2006; Grisel et al., 2005; Galer et. al, 2005; Staud et al., 2005; Lynch et al., 2004; Carlsson et al., 2004; Redwine and Trujillo, 2003; Ben et al., 2003; Sawynok and Reid, 2003, 2002; Chang et al., 1999). However, due to its low efficacy, DM is usually combined with other analgesic agents such as morphine and general anesthetics as ketamine (Frymoyer et al., 2007; Cohen et al., 2006; Galer et al., 2005; Elesen et al., 2007).
Our data were in agreement with previous findings on the DM’s effect on pain behaviors, because a single dose of DM (particularly at 30 or 60 mg/kg) alone effectively reduced both thermal hyperalgesia and mechanical allodynia. By contrast, melatonin alone given systemically appears to produce a minimal effect, if any, on neuropathic pain behaviors. Combination of both drugs, even at a subtherapeutic dose, substantially improved their effect on neuropathic pain behaviors without demonstrable side effects on motor function or sedation. These results suggest that the combination of melatonin with a clinically available NMDA receptor antagonist may be more effective than either drug alone in the treatment of neuropathic pain.
A clinical relationship between pain and depression has long been recognized. Several epidemiological studies have shown that pain and depression frequently co-exist in the clinical setting (Arnow et al., 2006; Bair et al., 2003; Magni et al., 1985; Von Knorring et al., 1983). Depression may result in a decreased pain threshold and increased analgesic requirement (Jackson and Onge, 2003). It is estimated that the occurrence of depression in patients with chronic pain is higher, ranging from 30% to 54%, than that (about 17%) in the general population (Sullivan et al., 1992; Banks and Kerns, 1996; Ferrer-Garcia et al., 2006). Moreover, the risk of developing chronic pain increases in subjects with depressive disorder (Leino and Magni, 1993; Magni et al., 1993, 1994). While antidepressants affect mood in chronic pain patients, they do not always improve outcome measures of clinical pain (Littlejohn and Guymer, 2006; Carter, 2002). Indeed, several studies have suggested that the effect of antidepressants on chronic pain may not be related to their anti-depression property (Atkinson et al., 1998; Collins et al., 2000; Max et al., 1987, 1992; Mico et al., 2006; Sharav et al., 1987). To date, the relationship between pain and depression remains unclear.
In this experiment, we showed that the combination of DM and melatonin improve pain behaviors without a change in depression-like behaviors as demonstrated by the forced swimming test, at least with the dose tested in this experiment. Of interest to note is that the results from our previous study (Zeng et al., 2008) suggest that the reduction of mechanical allodynia in WKY rats resulting from the administration of melatonin into the anterior cingulate cortex occurred concurrently with the improvement of depression-like behavior, because the same treatment also prolonged the forced swimming time. It remains to be investigated whether the route of melatonin administration (e.g., systemic versus direct injection into the anterior cingulate cortex) and different dose combinations may reduce neuropathic pain behaviors via different mechanisms.
Clinical comorbidity associated with pain, such as depression, is an important issue and confounding factor in clinical pain management. Although antidepressants have been used in clinical pain management, their mechanisms of action remain unclear. For example, a tricyclic antidepressant improved pain in patients with low back pain but without clinical depression (Collins et al., 2000), whereas in other cases antidepressants including selective serotonin or norepinephrine reuptake inhibitors failed to improve chronic pain (Mico et al., 2006). While the present study does not provide direct evidence for a relationship between the improvement of depressive behavior and pain behavior, the role of melatonin in the regulation of mood and clinical pain and the known NMDA receptor mechanism in neuropathic pain suggest that the combined DM and melatonin treatment may warrant further investigation in human subjects in order to explore new treatment options for those patients with both neuropathic pain and depression.
4. Experimental Procedure
Surgical procedure for the CCI model
Adult male WKY rats weighing 200–250 g (Charles River Lab, Wilmington, MA) were used and maintained by the accredited animal facility at the Massachusetts General Hospital. The experimental protocol was approved by our Institutional Animal Care and Use Committee. The animal room was artificially lighted from 7 AM to 7 PM and the room temperature was maintained at 22 °C. Food pellets and water were available ad libitum and the bedding was changed daily. Rats were housed individually in each cage and the experiments started at least three days after their arrival.
The surgical procedure was performed under pentobarbital anesthesia (50 mg/kg, intraperitoneally). CCI rats were produced by loosely ligating the common sciatic nerve on one side according to the method of Bennett and Xie (1988). Briefly, the right sciatic nerve was exposed in the mid-thigh and separated from the adjacent tissue. Four loose ligatures using 4-0 chromic gut sutures were made around the dissected nerve with a 1.0–1.5mm interval between each pair of ligatures. The skin wound was closed using stainless steel pins. In sham rats, the same surgical procedure was followed except for nerve ligation.
Intraperitoneal drug administration
DM and melatonin (Sigma, St. Louis, MO, US) were diluted in 10% DMSO. Melatonin was always diluted before usage. The MDSO (10%) was also used for vehicle control.
Behavioral tests and statistical analysis
Animals were habituated to the test environment once daily (a 60-min session) for two consecutive days before the baseline testing. For testing mechanical allodynia, each rat was placed on a metal mesh floor, covered with a plastic box (12×5×8 inch), and allowed to settle down for 15 min before the test. Von Frey filaments were used to determine the lowest mechanical threshold required for a brisk paw withdrawal according to the method (using an ascending and descending order of filaments) described by Tal and Bennett (1994) and in our previous report (Mao et al., 1997). A filament was applied perpendicularly to the rat’s plantar area and a 5-second interval was used between two applications. A positive response was defined as at least one clear withdrawal response out of five applications. The cutoff force was 26 g. Both the baseline and post-CCI testing were conducted between 9:00 A.M. and 12 P.M. Testing for thermal hyperalgesia was performed according to a previously published method (Hargreaves et al., 1988). Temperature was set to have the baseline latency at 10–12 sec and a cutoff of 20 sec.
Forced swimming test
The forced swim test was performed based on the original method described by Porsolt et al. (1977, 1978a,b) to examine depression-like behavior in WKY rats. One day prior to the test, a rat was placed for conditioning in a clear plastic tank (45×35×60 cm) containing water 30 cm deep (24±0.5 °C) for 5 min (pretest session). Twenty-four hours later, the rat was tested under the same conditions for 5 min (test session). Following each session, the rat was removed from the water tank, dried with a tissue towel, placed in a warm air flow for 15 min, and then returned to the home cage. Each test session was recorded with a stopwatch. A rat was judged to be non-swimming when its hind legs were no longer moving forcefully and the rat was hunched forward (a floating position). The total duration of immobility (non-swimming) within a 5-min session was recorded as immobility scores (in seconds) and compared among groups (Detke et al., 1995; Lopez-Rubalcava and Lucki, 2000). All sessions were observed by the same experimenter blinded to the group assignment to minimize between-experimenter and between-session variations. All swimming test sessions took place between 2 PM and 5 PM.
Statistical Analysis
Behavioral data were analyzed by using repeated measure one-way ANOVA to detect overall differences among treatment groups, followed by post-hoc Newman–Keuls tests. Differences were considered to be statistically significant at the level of P<0.05. ED50 for DM was generated from a linear regression model. ED50 dose for melatonin was not calculated because of the ineffectiveness of a single melatonin dose alone in pain behaviors. In addition, the isobolographic analysis was not performed to examine the synergism of the combined drug treatment due to the lack of a dose-related effect from the melatonin treatment alone. Accordingly, the statistical analysis in this study was not meant to determine whether there was a synergistic or additive effect from the combined treatment of melatonin and DM on pain behaviors in WKY rats.
Acknowledgments
This study is supported by NIH RO1 grants DE18214, DE18538, and NS45681.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Armario A, Gavalda A, Marti J. Comparison of the behavioural and endocrine response to forced swimming stress in five inbred strains of rats. Psychoneuroendocrinology. 1995;20:879–890. doi: 10.1016/0306-4530(95)00018-6. [DOI] [PubMed] [Google Scholar]
- Arner S, Meyerson BA. Lack of analgesic effect of opioids on neuropathic and idiopathic forms of pain. Pain. 1988;33:11–23. doi: 10.1016/0304-3959(88)90198-4. [DOI] [PubMed] [Google Scholar]
- Arnow BA, Hunkeler EM, Blasey CM, Lee J, Constantino MJ, Fireman B, Kraemer HC, Dea R, Robinson R, Hayward C. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68:262–268. doi: 10.1097/01.psy.0000204851.15499.fc. [DOI] [PubMed] [Google Scholar]
- Atkinson JH, Slater MA, Williams RA, Zisook S, Patterson TL, Grant I, Wahlgren DR, Abramson I, Garfin SR. A placebo-controlled randomized clinical trial of nortriptyline for chronic low back pain. Pain. 1998;76:287–296. doi: 10.1016/S0304-3959(98)00064-5. [DOI] [PubMed] [Google Scholar]
- Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity; a literature review. Arch Intern Med. 2003;163:2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- Banks S, Kerns R. Explaining high rates of depression in chronic pain. A diathesis-stress framework. Psychol Bull. 1996;119:95–110. [Google Scholar]
- Beck-Friis J, Kjellman BF, Aperia B, Unden F, von Rosen D, Ljunggren JG, Wetterberg L. Serum melatonin in relation to clinical variables in patients with major depressive disorder and a hypothesis of a low melatonin syndrome. Acta Psychiatr Scand. 1985;71:319–330. doi: 10.1111/j.1600-0447.1985.tb02531.x. [DOI] [PubMed] [Google Scholar]
- Ben Abraham R, Marouani N, Weinbroum AA. Dextromethorphan mitigates phantom pain in cancer amputees. Ann Surg Oncol. 2003;10:268–274. doi: 10.1245/aso.2003.08.007. [DOI] [PubMed] [Google Scholar]
- Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain. 1988;33:87–107. doi: 10.1016/0304-3959(88)90209-6. [DOI] [PubMed] [Google Scholar]
- Blackburn-Munro G, Blackburn-Munro R. Pain in the brain: are hormones to blame? Trends Endocrinol Metab. 2003;14:20–27. doi: 10.1016/s1043-2760(02)00004-8. [DOI] [PubMed] [Google Scholar]
- Blackburn-Munro G, Blackburn-Munro RE. Chronic pain, chronic stress and depression: coincidence or consequence. J Neuroendocrinol. 2001;13:1009–1023. doi: 10.1046/j.0007-1331.2001.00727.x. [DOI] [PubMed] [Google Scholar]
- Brzezinski A. Melatonin in humans. New Eng J Med. 1997;336:186–195. doi: 10.1056/NEJM199701163360306. [DOI] [PubMed] [Google Scholar]
- Carlsson KC, Hoem NO, Moberg ER, Mathisen LC. Analgesic effect of dextromethorphan in neuropathic pain. Acta Anaesthesiol Scand. 2004;48:328–236. doi: 10.1111/j.0001-5172.2004.0325.x. [DOI] [PubMed] [Google Scholar]
- Carter GT. Antidepressants in pain management. Curr Opin Investig Drugs. 2002;3:454–458. [PubMed] [Google Scholar]
- Chang FL, Wu CT, Yeh CC, Lin TC, Ho ST, Wong CS. Postoperative intramuscular dextromethorphan injection provides postoperative pain relief and decreases opioid requirement after hemorrhoidectomy. Acta Anaesthesiol Sin. 1999;37:179–183. [PubMed] [Google Scholar]
- Citera G, Arias MA, Maldonado-Cocco JA, Lazaro MA, Rosemffet MG, Brusco LI, Scheines EJ, Cardinalli DP. The effect of melatonin in patients with fibromyalgia: a pilot study. Clin Rheumatol. 2000;19:9–13. doi: 10.1007/s100670050003. [DOI] [PubMed] [Google Scholar]
- Cohen SP, Chang AS, Larkin T, Mao J. The intravenous ketamine test: a predictive response tool for oral dextromethorphan treatment in neuropathic pain. Anesth Analg. 2004;99:1753–1759. doi: 10.1213/01.ANE.0000136953.11583.7B. table of contents. [DOI] [PubMed] [Google Scholar]
- Cohen SP, Verdolin MH, Chang AS, Kurihara C, Morlando BJ, Mao J. The intravenous ketamine test predicts subsequent response to an oral dextromethorphan treatment regimen in fibromyalgia patients. J Pain. 2006;7:391–398. doi: 10.1016/j.jpain.2005.12.010. [DOI] [PubMed] [Google Scholar]
- Collins SL, Moore RA, McQuay HJ, Wiffen P. Antidepressants and anticonvulsants for diabetic neuropathy and postherpetic neuralgia: a quantitative systematic review. J Pain Symptom Manage. 2000;20:449–458. doi: 10.1016/s0885-3924(00)00218-9. [DOI] [PubMed] [Google Scholar]
- De La Garza R, Mahoney JJ. A distinct neurochemical profile in WKY rats at baseline and in response to acute stress: implications for animal models of anxiety and depression. Brain Res. 2004;1021:209–218. doi: 10.1016/j.brainres.2004.06.052. [DOI] [PubMed] [Google Scholar]
- Detke MJ, Rickels M, Lucki I. Active behaviors in the rat forced swimming test differentially produced by serotonergic and noradrenergic antidepressants. Psychopharmacology (Berl) 1995;21:66–72. doi: 10.1007/BF02245592. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Raphael KG, Marbach JJ, Gallagher RM. Why is depression comorbid with chronic myofascial face pain? A family study test of alternative hypotheses. Pain. 1999;83:183–192. doi: 10.1016/s0304-3959(99)00100-1. [DOI] [PubMed] [Google Scholar]
- Dubner R, Hargreaves KM. The neurobiology of pain and its modulation. Clin J Pain. 1989;(Suppl 2):S1. doi: 10.1097/00002508-198906002-00002. [DOI] [PubMed] [Google Scholar]
- Duedahl TH, Rømsing J, Møiniche S, Dahl JB. A qualitative systematic review of peri-operative dextromethorphan in post-operative pain. Acta Anaesthesiol Scand. 2006;50:1–13. doi: 10.1111/j.1399-6576.2006.00900.x. [DOI] [PubMed] [Google Scholar]
- Duman RS, Heninger GR, Nestler EJ. A molecular and cellular theory of depression. Arch Gen Psychiatry. 1997;54:597–606. doi: 10.1001/archpsyc.1997.01830190015002. [DOI] [PubMed] [Google Scholar]
- Duric V, McCarson KE. Hippocampal neurokinin-1 receptor and brain-derived neurotrophic factor gene expression is decreased in rat models of pain and stress. Neuroscience. 2005;133:999–1006. doi: 10.1016/j.neuroscience.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Fazli-Tabaei S, Maghsoudi A, Bazaz N, Modirzadeh A, Zarrindast MR. Effect of dextromethorphan on antinociception and tolerance induced by swim-stress in the formalin test. Arch Iran Med. 2008;11:286–292. [PubMed] [Google Scholar]
- Ferrer-Garcia MD, Wernicke JF, Detke MJ, Iyengar S. The depression–pain complex: overlap between the two problems and implications for neuropathic pain. In: Campbell JN, Basbaum AI, Dray A, Dubner R, Dworkin RH, Sang CN, editors. Emerging Strategies for the Treatment of Neuropathic Pain. IASP Press; Seattle: 2006. pp. 307–325. [Google Scholar]
- Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain. 1997;13:116–137. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]
- Frankland PW, Teixeira CM. A pain in the ACC. Mol Pain. 2005;1:14–16. doi: 10.1186/1744-8069-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazer A, Brown R, Kocsis J, Caroff S, Amsterdam J, Winokur A, Sweeney J, Stokes P. Patterns of melatonin rhythms in depression. J Neural Transm Suppl. 1986;21:269–290. [PubMed] [Google Scholar]
- Frymoyer AR, Rowbotham MC, Petersen KL. Placebo-controlled comparison of a morphine/dextromethorphan combination with morphine on experimental pain and hyperalgesia in healthy volunteers. J Pain. 2007;8:19–25. doi: 10.1016/j.jpain.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Galer BS, Lee D, Ma T, Nagle B, Schlagheck TG. MorphiDex (morphine sulfate/dextromethorphan hydrobromide combination) in the treatment of chronic pain: three multicenter, randomized, double-blind, controlled clinical trials fail to demonstrate enhanced opioid analgesia or reduction in tolerance. Pain. 2005;115:284–295. doi: 10.1016/j.pain.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Gao JY, Ren WH, Zhang YQ, Zhao ZQ. Contributions of the anterior cingulate cortex and amygdala to pain- and fear-conditioned place avoidance in rats. Pain. 2004;110:343–353. doi: 10.1016/j.pain.2004.04.030. [DOI] [PubMed] [Google Scholar]
- Golombek DA, Escolar E, Burin LJ, De Brito Sanchez MG, Cardinali DP. Time-dependent melatonin analgesia in mice: inhibition by opiate or benzodiazepine antagonism. Eur J Pharmacol. 1991;194:25–30. doi: 10.1016/0014-2999(91)90119-b. [DOI] [PubMed] [Google Scholar]
- Grisel JE, Allen S, Nemmani KV, Fee JR, Carliss R. The influence of dextromethorphan on morphine analgesia in Swiss Webster mice is sex-specific. Pharmacol Biochem Behav. 2005;81:131–138. doi: 10.1016/j.pbb.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Halbreich U, Weinberg U, Stewart J, Klein DF, Weitzman ED, Quitkin FM. An inverse correlation between serum levels of desmethylimipramine and melatonin-like immunoreactivity in DMI-responsive depressives. Psychiatry Res. 1981;4:109–113. doi: 10.1016/0165-1781(81)90014-7. [DOI] [PubMed] [Google Scholar]
- Hargreaves K, Dubner R, Brown F, Flores C, Joris J. A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia. Pain. 1988;32:77–88. doi: 10.1016/0304-3959(88)90026-7. [DOI] [PubMed] [Google Scholar]
- Jackson KC, 2nd, St Onge EL. Antidepressant pharmacotherapy: considerations for the pain clinician. Pain Pract. 2003;3:135–143. doi: 10.1046/j.1533-2500.2003.03020.x. [DOI] [PubMed] [Google Scholar]
- Jadad AR, Carroll D, Glynn CJ, Moore RA, McQuay HJ. Morphine responsiveness of chronic pain: double-blind randomized crossover study with patient-controlled analgesia. Lancet. 1992;339:1367–1371. doi: 10.1016/0140-6736(92)91194-d. [DOI] [PubMed] [Google Scholar]
- Jasmin L, Rabkin SD, Granato A, Boudah A, Ohara PT. Analgesia and hyperalgesia from GABA-mediated modulation of the cerebral cortex. Nature. 2003;424:316–320. doi: 10.1038/nature01808. [DOI] [PubMed] [Google Scholar]
- Johansen JP, Fields HL, Manning BH. The affective component of pain in rodents: direct evidence for a contribution of the anterior cingulated cortex. Proc Natl Acad Sci USA. 2001;98:8077–8082. doi: 10.1073/pnas.141218998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korszun A. Facial pain, depression and stress —connections and directions. J Oral Pathol Med. 2002;31:615–619. doi: 10.1034/j.1600-0714.2002.00091.x. [DOI] [PubMed] [Google Scholar]
- Kupers RC, Konings H, Adriaensen H, Gybels JM. Morphine differentially affects the sensory and affective pain rating in neurogenic pain and idiopathic forms of pain. Pain. 1991;47:5–12. doi: 10.1016/0304-3959(91)90004-H. [DOI] [PubMed] [Google Scholar]
- LaGraize Stacey C, Labuda Christopher J, Rutledge Margaret A, Jackson Raymond L, Fuchs Perry N. Differential effect of anterior cingulate cortex lesion on mechanical hypersensitivity and escape/avoidance behavior in an animal model of neuropathic pain. Exp Neurol. 2004;188:139–148. doi: 10.1016/j.expneurol.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Leino P, Magni G. Depression and distress symptoms as predictors of low back pain, neck–shoulder pain, and other musculoskeletal morbidity: a 10 year follow-up of metal industry employees. Pain. 1993;53:89–94. doi: 10.1016/0304-3959(93)90060-3. [DOI] [PubMed] [Google Scholar]
- Leone M, D’Amico D, Moschiano F, Fraschini F, Bussone G. Melatonin versus placebo in the prophylaxis of cluster headache: a double-blind pilot study with parallel groups. Cephalalgia. 1996;16:494–496. doi: 10.1046/j.1468-2982.1996.1607494.x. [DOI] [PubMed] [Google Scholar]
- Leone M, Lucini V, D’Amico D, Moschiano F, Maltempo C, Fraschini F, Bussone G. Twenty-four-hour melatonin and cortisol plasma levels in relation to timing of cluster headache. Cephalalgia. 1995;15:224–229. doi: 10.1046/j.1468-2982.1995.015003224.x. [DOI] [PubMed] [Google Scholar]
- Li SR, Wang T, Wang R, Dai X, Chen Q, Li RD. Melatonin enhances antinociceptive effects of delta-, but not mu-opioid agonist in mice. Brain Res. 2005;1043:132–138. doi: 10.1016/j.brainres.2005.02.067. [DOI] [PubMed] [Google Scholar]
- Littlejohn GO, Guymer EK. Fibromyalgia syndrome: which antidepressant drug should we choose? Curr Pharm Des. 2006;12:3–9. [PubMed] [Google Scholar]
- Lopez-Rubalcava C, Lucki I. Strain differences in the behavioral effects of antidepressant drugs in the rat forced swimming test. Neuropsychopharmacology. 2000;22:191–199. doi: 10.1016/S0893-133X(99)00100-1. [DOI] [PubMed] [Google Scholar]
- Lynch JJ, 3rd, Wade CL, Zhong CM, Mikusa JP, Honore P. Attenuation of mechanical allodynia by clinically utilized drugs in a rat chemotherapy-induced neuropathic pain model. Pain. 2004;110:56–63. doi: 10.1016/j.pain.2004.03.010. [DOI] [PubMed] [Google Scholar]
- Magni G, Marchetti M, Moreschi C, Merskey H, Luchini SR. Chronic musculoskeletal pain and depression symptoms in the National Health and Nutrition Examination. I. Epidemiologic follow-up study. Pain. 1993;53:163–168. doi: 10.1016/0304-3959(93)90076-2. [DOI] [PubMed] [Google Scholar]
- Magni G, Moreschi C, Rigatti-Luchini S, Merskey H. Prospective study on the relationship between depression symptoms and chronic musculoskeletal pain. Pain. 1994;56:289–297. doi: 10.1016/0304-3959(94)90167-8. [DOI] [PubMed] [Google Scholar]
- Magni G, Schifano F, De Leo D. Pain as a symptom in elderly depressed patients. Eur Arch Psychiatry Neurol Sci. 1985;235:143–145. doi: 10.1007/BF00380984. [DOI] [PubMed] [Google Scholar]
- Mao J, Chen LL. Gabapentin in pain management. Anesth Analg. 2000a;91:680–687. doi: 10.1097/00000539-200009000-00034. [DOI] [PubMed] [Google Scholar]
- Mao J, Chen LL. Systemic lidocaine for neuropathic pain relief. Pain. 2000b;87:7–17. doi: 10.1016/S0304-3959(00)00229-3. [DOI] [PubMed] [Google Scholar]
- Mao J, Price DD, Mayer DJ. Mechanisms of hyperalgesia and opiate tolerance: a current view of their possible interactions. Pain. 1995a;62:259–274. doi: 10.1016/0304-3959(95)00073-2. [DOI] [PubMed] [Google Scholar]
- Mao J, Price DD, Mayer DJ. Experimental mononeuropathy reduces the antinociceptive effects of morphine: implications for common intracellular mechanisms involved in morphine tolerance and neuropathic pain. Pain. 1995b;61:353–364. doi: 10.1016/0304-3959(95)00022-K. [DOI] [PubMed] [Google Scholar]
- Mao J, Price DD, Zhu J, Lu J, Mayer DJ. The inhibition of nitric oxide-activated poly (ADP-ribose) synthetase attenuates transsynaptic alteration of spinal cord dorsal horn neurons and neuropathic pain in the rat. Pain. 1997;72:355–366. doi: 10.1016/s0304-3959(97)00063-8. [DOI] [PubMed] [Google Scholar]
- Max B, Kishore-Kumar R, Schafer SC, Merster B, Gracely RH, Smoller B, et al. Efficacy of desipramine in painful diabetic neuropathy: a placebo-controlled trial. Pain. 1991;45:3–9. doi: 10.1016/0304-3959(91)90157-S. [DOI] [PubMed] [Google Scholar]
- Max B, Lynch SA, Muir J, Shoaf SE, Smoller B, Dubner R. Effects of desipramine, amitriptyline, and fluoxetine on pain in diabetic neuropathy. N Engl J Med. 1992;326:1250–1256. doi: 10.1056/NEJM199205073261904. [DOI] [PubMed] [Google Scholar]
- Max MB. Treatment of post-herpetic neuralgia: antidepressants. Ann Neurol. 1994;35:S50–S53. doi: 10.1002/ana.410350715. [DOI] [PubMed] [Google Scholar]
- Max MB, Culnane M, Schafer SC. Amitriptyline relieves diabetic neuropathy pain in patients with normal or depressed mood. Neurology. 1987;37:589–596. doi: 10.1212/wnl.37.4.589. [DOI] [PubMed] [Google Scholar]
- Max MB, Lynch S, Muir J. Effects of desipramine, amitriptyline and fluoxetine on pain in diabetic neuropathy. New Eng J Med. 1992;326:1250–1256. doi: 10.1056/NEJM199205073261904. [DOI] [PubMed] [Google Scholar]
- Mico JA, Ardid D, Berrocoso E, Eschalier A. Antidepressants and pain. Trends Pharmacol Sci. 2006;27:348–354. doi: 10.1016/j.tips.2006.05.004. [DOI] [PubMed] [Google Scholar]
- Morgan PJ, Barrett P, Howell HE, Helliwell R. Melatonin receptor: localization, molecular pharmacology and physiological significance. Neurochem Int. 1994;24:101–146. doi: 10.1016/0197-0186(94)90100-7. [DOI] [PubMed] [Google Scholar]
- Nibuya M, Morinobu S, Duman RS. Regulation of BDNF and trkB mRNA in rat brain by chronic electroconvulsive seizure and antidepressant drug treatments. J Neurosci. 1995;15:7539–7547. doi: 10.1523/JNEUROSCI.15-11-07539.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nibuya M, Takahashi M, Russell DS, Duman RS. Repeated stress increases catalytic TrkB mRNA in rat hippocampus. Neurosci Lett. 1999;267:81–84. doi: 10.1016/s0304-3940(99)00335-3. [DOI] [PubMed] [Google Scholar]
- Okamoto K, Aoli K. Development of a stroma of spontaneously hypertensive rats. Jpn Circ J. 1963;27:282–293. doi: 10.1253/jcj.27.282. [DOI] [PubMed] [Google Scholar]
- Olesen AE, Staahl C, Ali Z, Drewes AM, Arendt-Nielsen L. Effects of paracetamol combined with dextromethorphan in human experimental muscle and skin pain. Basic Clin Pharmacol Toxicol. 2007;101:172–176. doi: 10.1111/j.1742-7843.2007.00095.x. [DOI] [PubMed] [Google Scholar]
- Onal SA, Inalkac S, Kutlu S, Kelestimur H. Intrathecal melatonin increases the mechanical nociceptive threshold in the rat. Agri. 2004;16:35–40. [PubMed] [Google Scholar]
- Ossipov MH, Lopez Y, Nichols ML, Bian D, Porreca F. The loss of antinociceptive efficacy of spinal morphine in rats with nerve ligation injury is prevented by reducing spinal afferent drive. Neurosci Lett. 1995;199:87–90. doi: 10.1016/0304-3940(95)12022-v. [DOI] [PubMed] [Google Scholar]
- Overstreet DH, Friedman E, Mathe AA, Yadid G. The Flinders sensitive line rat: a selectively bred putative animal model of depression. Neurosci Biobehav Rev. 2005;29:739–759. doi: 10.1016/j.neubiorev.2005.03.015. [DOI] [PubMed] [Google Scholar]
- Overstreet DH, Pucilowski O, Retton MC, Delagrange P, Guardiola-Lemaitre B. Effects of melatonin receptor ligands on swim test immobility. Neuroreport. 1998;9:249–253. doi: 10.1097/00001756-199801260-00014. [DOI] [PubMed] [Google Scholar]
- Pandi-Perumal SR, Srinivasan V, Maestroni GJM, Cardinali DP, Poeggeler B, Hardeland R. Melatonin: nature’s most versatile biological signal? FEBS J. 2006;273:2813–2838. doi: 10.1111/j.1742-4658.2006.05322.x. [DOI] [PubMed] [Google Scholar]
- Pang CS, Tsang SF, Yang JC. Effects of melatonin, morphine and diazepam on formalin-induced nociception in mice. Life Sci. 2001;68:943–951. doi: 10.1016/s0024-3205(00)00996-6. [DOI] [PubMed] [Google Scholar]
- Pare WP. Enhanced retrieval of unpleasant memories influenced by shock controllability, shock sequence and rat strain. Biol Psychiatry. 1996;39:808–813. doi: 10.1016/0006-3223(95)00220-0. [DOI] [PubMed] [Google Scholar]
- Pare WP. Open field, learned helplessness, defensive burying, and forced-swim tests in WKY rats. Physiol Behav. 1994;55:433–439. doi: 10.1016/0031-9384(94)90097-3. [DOI] [PubMed] [Google Scholar]
- Pare WP. Passive-avoidance behavior in Wistar-Kyoto (WKY), Wistar and Fischer-344 rats. Physiol Behav. 1993;54:845–852. doi: 10.1016/0031-9384(93)90291-m. [DOI] [PubMed] [Google Scholar]
- Porsolt RD, Anton G, Blavet N, Jalfre M. Behavioral despair in rats: a new model sensitive to antidepressant treatment. Eur J Pharmacol. 1978a;47:379–391. doi: 10.1016/0014-2999(78)90118-8. [DOI] [PubMed] [Google Scholar]
- Porsolt RD, Bertin A, Jalfre M. Behavioral despair?in rats and mice: strain differences and the effects of imipramine. Eur J Pharmacol. 1978b;51:291–294. doi: 10.1016/0014-2999(78)90414-4. [DOI] [PubMed] [Google Scholar]
- Porsolt RD, Le Pichon M, Jalfre M. Depression: a new animal model sensitive to antidepressant treatments. Nature. 1977;266:730–732. doi: 10.1038/266730a0. [DOI] [PubMed] [Google Scholar]
- Rabe-Jablonska J, Miller A. Links between pain and depression. Psychiatr Pol. 2005;39:7–20. [PubMed] [Google Scholar]
- Raghavendra V, Agrewala JN, Kulkarni SK. Melatonin reversal of lipopolysaccharides-induced thermal and behavioral hyperalgesia in mice. Eur J Pharmacol. 2000;395:15–21. doi: 10.1016/s0014-2999(00)00196-5. [DOI] [PubMed] [Google Scholar]
- Raghavendra V, Kulkarni SK. Possible mechanisms of action in melatonin reversal of morphine tolerance and dependence in mice. Eur J Pharmacol. 2000;409:279–289. doi: 10.1016/s0014-2999(00)00849-9. [DOI] [PubMed] [Google Scholar]
- Redwine KE, Trujillo KA. Effects of NMDA receptor antagonists on acute mu-opioid analgesia in the rat. Pharmacol Biochem Behav. 2003;76:361–72. doi: 10.1016/j.pbb.2003.08.009. [DOI] [PubMed] [Google Scholar]
- Sawynok J, Reid A. Modulation of formalin-induced behaviors and edema by local and systemic administration of dextromethorphan, memantine and ketamine. Eur J Pharmacol. 2002;450:153–162. doi: 10.1016/s0014-2999(02)02119-2. [DOI] [PubMed] [Google Scholar]
- Sawynok J, Reid A. Peripheral interactions between dextromethorphan, ketamine and amitriptyline on ormalin-evoked behaviors and paw edema in rats. Pain. 2003;102:179–86. doi: 10.1016/s0304-3959(02)00373-1. [DOI] [PubMed] [Google Scholar]
- Schatzberg Alan F. Depression and physical symptoms: the mind–body connection. J Clin Psychiatry. 2004;65:867–876. doi: 10.4088/jcp.v65n0621. [DOI] [PubMed] [Google Scholar]
- Sharav Y, Singer E, Schmidt E, Dionne RA, Dubner R. The analgesic effect of amitriptyline on chronic facial pain. Pain. 1987;31:199–209. doi: 10.1016/0304-3959(87)90036-4. [DOI] [PubMed] [Google Scholar]
- Shavali S, Ho B, Govitrapong P, Sawlom S, Ajjimaporn A, Klongpanichapak S, Ebadi M. Melatonin exerts its analgesic actions not by binding to opioid receptor subtypes but by increasing the release of beta-endorphin an endogenous opioid. Brain Res Bull. 2005;64:471–479. doi: 10.1016/j.brainresbull.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Sindrup SH, Jensen TS. Efficacy of pharmacological treatment of neuropathic pain: an update and effect related to mechanism of drug action. Pain. 1999;83:389–900. doi: 10.1016/S0304-3959(99)00154-2. [DOI] [PubMed] [Google Scholar]
- Siu A, Drachtman R. Dextromethorphan: a review of N-methyl-d-aspartate receptor antagonist in the management of pain. CNS Drug Rev. 2007;13:96–106. doi: 10.1111/j.1527-3458.2007.00006.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song GH, Leng PH, Gwee KA, Moochhala SM, Ho KY. Melatonin improves abdominal pain in irritable bowel syndrome patients who have sleep disturbances: a randomised, double blind, placebo controlled study. Gut. 2005;54:1402–1407. doi: 10.1136/gut.2004.062034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stankov B, Cozzi B, Lucini V, Capsoni S, Fauteck J, Fumagalli P, Fraschini F. Localization and characterization of melatonin binding sites in the brain of the rabbit (Oryctolagus cuniculus) by autoradiography and in vitro ligand–receptor binding. Neurosci Lett. 1991;133:68–72. doi: 10.1016/0304-3940(91)90059-3. [DOI] [PubMed] [Google Scholar]
- Staud R, Vierck CJ, Robinson ME, Price DD. Effects of the N-methyl-D-aspartate receptor antagonist dextromethorphan on temporal summation of pain are similar in fibromyalgia patients and normal control subjects. J Pain. 2005;6:323–332. doi: 10.1016/j.jpain.2005.01.357. [DOI] [PubMed] [Google Scholar]
- Sugden D. Psychopharmacological effects of melatonin in mouse and rat. J Pharmacol Exp Ther. 1983;227:587–591. [PubMed] [Google Scholar]
- Sullivan MJ, Reesor K, Mikail S, Fisher R. The treatment of depression in chronic low back pain: review and recommendations. Pain. 1992;50:5–13. doi: 10.1016/0304-3959(92)90107-M. [DOI] [PubMed] [Google Scholar]
- Thomas PK. Clinical features and differential diagnosis of peripheral neuropathy. In: Dyck PJ, Thomas PK, Lambert EH, Bunge R, editors. Peripheral neuropathy. Philadelphia: W.B. Saunders Company; 1984. pp. 1169–1190. [Google Scholar]
- Tsigos C, Chrousos GP. Hypothalamic–pituitary–adrenal axis, neuroendocrine factors and stress. J Psychosom Res. 2002;53:865–871. doi: 10.1016/s0022-3999(02)00429-4. [DOI] [PubMed] [Google Scholar]
- Tu Y, Sun RQ, Willis WD. Effects of intrathecal injections of melatonin analogs on capsaicin-induced secondary mechanical allodynia and hyperalgesia in rats. Pain. 2004;109:340–350. doi: 10.1016/j.pain.2004.01.027. [DOI] [PubMed] [Google Scholar]
- Vanecek J. Cellular mechanisms of melatonin action. Physiol Rev. 1998;78:687–721. doi: 10.1152/physrev.1998.78.3.687. [DOI] [PubMed] [Google Scholar]
- Vitte PA, Harthe C, Pevet P, Claustrat B. Brain autoradiographic study in the golden hamster after intracarotid injection of [14C]melatonin. Neurosci Lett. 1990;110:1–5. doi: 10.1016/0304-3940(90)90777-7. [DOI] [PubMed] [Google Scholar]
- Vogt BA. Pain and emotion interactions in subregions of the cingulated gyrus. Nat Rev Neurosci. 2005;6:533–544. doi: 10.1038/nrn1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Gall C, Stehle JH, Weaver DR. Mammalian melatonin receptors: molecular biology and signal transduction. Cell Tissue Res. 2002;309:151–162. doi: 10.1007/s00441-002-0581-4. [DOI] [PubMed] [Google Scholar]
- Von Knorring L, Perris C, Eisemann M, Erisksson U, Perris H. Pain as a symptom in depressive disorders. I. Relationship to diagnostic subgroup and depressive symptomatology. Pain. 1983;15:19–26. [Google Scholar]
- Von Korff M, Simon G. The relationship between pain and depression. Br J Psychiatry Suppl. 1996;30:101–108. [PubMed] [Google Scholar]
- Waldenlind E, Gustafsson SA, Ekbom K, Wetterberg L. Circadian secretion of cortisol and melatonin in cluster headache during active cluster periods and remission. J Neurol Neurosurg Psychiatry. 1987;50:207–213. doi: 10.1136/jnnp.50.2.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walf AA, Frye CA. Antianxiety and antidepressive behavior produced by physiological estradiol regimen may be modulated by hypothalamic–pituitary–adrenal axis activity. Neuropsychopharmacology. 2005;30:1288–1301. doi: 10.1038/sj.npp.1300708. [DOI] [PubMed] [Google Scholar]
- Watson CPN, Evans RJ, Reed K, Merskey H, Goldsmith L, Warsh J. Amitriptyline versus placebo in postherpetic neuralgia. Neurology. 1982;32:671–673. doi: 10.1212/wnl.32.6.671. [DOI] [PubMed] [Google Scholar]
- Wegert S, Ossipov MH, Nichols ML, Bian D, Vanderah TW, Malan TP, Jr, Porreca F. Differential activities of intrathecal MK-801 or morphine to alter responses to thermal and mechanical stimuli in normal and nerve-injured rats. Pain. 1997;71:57–64. doi: 10.1016/s0304-3959(97)03337-x. [DOI] [PubMed] [Google Scholar]
- Weil ZM, Hotchkiss AK, Gatien ML, Pieke-Dahl S, Nelson RJ. Melatonin receptor (MT1) knockout mice display depression-like behaviors and deficits in sensorimotor gating. Brain Res Bull. 2006;68:425–429. doi: 10.1016/j.brainresbull.2005.09.016. [DOI] [PubMed] [Google Scholar]
- Wetterberg L. Melatonin and affective disorders. Ciba Found Symp. 1985;17:253–265. doi: 10.1002/9780470720981.ch15. [DOI] [PubMed] [Google Scholar]
- Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet. 1999;353:1959–1964. doi: 10.1016/S0140-6736(99)01307-0. [DOI] [PubMed] [Google Scholar]
- Yu CX, Zhu CB, Xu SF, Cao XD, Wu GC. Selective MT (2) melatonin receptor antagonist blocks melatonin-induced antinociception in rats. Neurosci Lett. 2000a;24:161–164. doi: 10.1016/s0304-3940(00)00883-1. [DOI] [PubMed] [Google Scholar]
- Yu CX, Zhu CB, Xu SF, Cao XD, Wu GC. The analgesic effects of peripheral and central administration of melatonin in rats. Eur J Pharmacol. 2000b;l:49–53. doi: 10.1016/s0014-2999(00)00421-0. [DOI] [PubMed] [Google Scholar]
- Zahn PK, Lansmann T, Berger E, Speckmann EJ, Musshoff U. Gene expression and functional characterization of melatonin receptors in the spinal cord of the rat: implications for pain modulation. J Pineal Res. 2003;35:24–31. doi: 10.1034/j.1600-079x.2003.00047.x. [DOI] [PubMed] [Google Scholar]
- Zeng Q, Wang S, Lim G, Yang L, Mao J, Sung B, Chang Y, Lim JA, Guo G, Mao J. Exacerbated mechanical allodynia in rats with depression-like behavior. Brain Res. 2008;1200:27–38. doi: 10.1016/j.brainres.2008.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Zhang Y, Zhao ZQ. Anterior cingulated cortex contributes to the descending facilitatory modulation of pain via dorsal reticular nucleus. Eur J Neurosci. 2005;22:1141–1148. doi: 10.1111/j.1460-9568.2005.04302.x. [DOI] [PubMed] [Google Scholar]