Abstract
NEP effectiveness at a population level depends on several factors, including the number of IDUs retained, or consistently accessing services. Patterns of retention in the Baltimore Needle Exchange Program (BNEP) from 1994 to 2006 were calculated using enrollment surveys and client records. We used Andersen’s Behavioral Model of Health Services Use to frame our examination of factors associated with retention. Client retention was measured in two ways: whether a client returned to the exchange within twelve months of enrollment and how many times a client returned within these twelve months. BNEP clients (N=12,388) were predominantly male (69%), African-American (73%), and ≥ age 30 (86%). Nearly two-thirds (64%) of clients returned within twelve months of their first BNEP visit. The median number of return visits per client within twelve months was one (IQR 0–5). Young age (<30), being married, having an injection drug use history of less than twenty years, and living farther from the BNEP site were characteristics independently associated with both measures of low retention in multivariate analysis. Among younger injectors, geographical proximity was a particularly important predictor of retention. Further insight into the influence of these factors may help in developing programmatic changes that will be effective in increasing retention.
Keywords: needle exchange, syringe exchange, injection drug user, retention, behavioral model of health services use, african-american, youth, neighborhood
1. INTRODUCTION
Throughout the world, needle exchange programs (NEPs) can be cost-effective interventions associated with reductions in HIV, Hepatitis B, and Hepatitis C virus transmission (Lurie et al., 1998; Wodak and Cooney, 2006). In addition to acquiring sterile syringes for prevention of disease transmission, injection drug users (IDUs) who attend NEPs may receive other medical and social services such as wound care, onsite HIV testing, and drug treatment referrals. (Strathdee and Vlahov, 2001) NEP attendance has been associated with entry into and success with drug treatment (Brooner et al., 1998; Heimer, 1998; Strathdee et al., 1999) as well as a reduction in syringe sharing and other injection risk practices. (Huo and Ouellet, 2007; Ouellet et al., 2004)
NEP effectiveness at a population level depends on several factors, including the number of IDUs ever reached and the number of IDUs who access services consistently over time. (Burrows, 2006) Consistent client participation, or retention, is necessary for the reduction of risk behaviors, and early criticisms of NEPs implied that low client retention limited the effectiveness of the available programs. (Khoshnood et al., 1995) Retention data may provide information on the quality of relationships established between NEP staff and clients. (Hay and McKeganey, 2001) Understanding correlates of retention patterns may also inform service provision models as well as targeted client enrollment, ultimately reaching IDUs at highest risk for disease transmission.(Cottler et al., 1996; Strike et al., 2002)
The existing literature on retention in NEPs is limited; studies in Scotland and New Haven, Connecticut have looked at retention among NEP clients over time (Hay and McKeganey, 2001; Khoshnood et al., 1995) and two studies have examined retention of IDUs participating in an observational cohort study. (Cottler et al., 1996; Messiah et al., 2003) Several sociodemographic characteristics and behaviors were found to be associated with retention, though no clear predictors of retention emerged. Two studies found that white NEP clients and white IDU cohort study participants were more likely to return to the NEP or complete study follow-up.(Cottler et al., 1996; Khoshnood et al., 1995) Female clients were more likely to return to the Scottish NEP, (Hay and McKeganey, 2001) but retention rates were not significantly different by gender in any of the other studies. Only one study showed that IDUs older than 35 were most likely to return to the NEP, (Khoshnood et al., 1995) whereas the other studies did not find age to be a significant predictor of continued follow-up. Low educational attainment (not having a high school diploma or the equivalent) was associated with completing follow-up in just one study. (Messiah et al., 2003) Cohort participants who were employed were more likely to complete follow-up in one cohort,(Cottler et al., 1996) and shorter history of drug use (< 10 years) was found to be associated with client retention only in the New Haven NEP. (Khoshnood et al., 1995) Studies examined retention six months to four years after the initial program implementation, so longer-term patterns of association were not determined. Further investigation of the long-term impacts of sociodemographic and behavioral factors on access and retention is therefore warranted.
Predictors of client retention may be better understood through the lens of Andersen’s Behavioral Model of Health Services Use, a framework that has been used to examine health care access and utilization of services among a variety of special populations. (Andersen, 1995) This model categorizes factors associated with an individual’s health service utilization as predisposing, need, and enabling factors. Predisposing factors are demographic or other individual characteristics (e.g. beliefs) that affect a person’s inclination to seek services. Need characteristics such as diagnosis or symptoms of an illness influence the individual’s objective or perceived need for health care. Enabling factors are personal or community resources, like insurance, social support, or transportation, that enable or impede use of health services. Though this model was originally intended to explore factors important in access to care, we believe that the framework should also apply to an individual’s retention in a health service program. Our study therefore aims to identify the types of factors most closely associated with client retention in an NEP in order to suggest focused programmatic changes and increase retention rates. To investigate the robustness of our findings, we will examine the patterns of these associations over the course of a decade.
Studies have found high rates of bloodborne infections among young, recent onset IDUs. Early studies among Baltimore IDUs found an HCV prevalence of 65% within one year and 80% within the two years of initiating injection drug use, with a similar trajectory for HBV prevalence (Garfein et al., 1996). In other studies, fewer than half of young urban IDUs used NEPs or pharmacies as their main source of syringes or access NEPs at all. (Bailey et al., 2003; Sherman et al., 2004) Younger IDUs (< 30 years old) have been shown to have substantially higher rates of risk-taking behavior compared to older IDUs (Cassin et al., 1998; Fennema et al., 1997; Kral et al., 2000) but experience with the NEP attenuates some of these risks. (Novelli et al., 2005) Comparing predictors of retention between older and younger IDUs may therefore provide further insight needed to increase NEP client retention in this high-risk subpopulation.
2. METHODS
2.1 Needle Exchange Program Operation
The Baltimore City Needle Exchange Program (BNEP) has been regularly providing syringes for exchange since November 1994, and expanded to 17 sites throughout the city by 2006. The BNEP provides needle exchange and ancillary services at street corner sites six days a week, with morning, afternoon, and evening sites available. BNEP clients complete a short questionnaire at enrollment, with questions about demographic factors and drug use practices. Upon enrollment, clients are assigned a unique identifier; identity is confirmed at subsequent visits by matching the client’s last four digits of social security number, mother’s maiden name, and date of birth. At each visit, BNEP staff record the unique identifier, the date of the visit, the site attended, and the number of syringes returned and distributed. The centralized electronic database has been used at all BNEP sites since 1994, allowing the program to track unique clients’ access patterns even if they attend multiple BNEP sites.
2.2 Study Measures
Demographic variables of interest included age at baseline visit, sex, race, employment, marital status, and housing status. Continuous variables were categorized where appropriate. Drug characteristics included previous experience with drug treatment, injection history, and injection frequency. Years of injection history was calculated by asking clients at what age they first injected drugs and subtracting from their current age. Clients were asked about the number of times they injected drugs per day, per week, or per month, and daily injection rates were calculated based on these reported estimates. Proximity to the BNEP site is a dichotomous variable indicating whether clients’ zip code at enrollment matched the zip code of the BNEP site where a client enrolled. Individuals reporting that they lived in a shelter/welfare boarding house, on the street, or in a transitional housing program were considered homeless. (U.S. House of Representatives, 2005)
Clients were considered to have the outcome of multi-visit usage if they returned to their enrollment site or any other BNEP site within twelve months of the first visit. To ensure that all clients had an opportunity to be classified as having multi-visit usage, we restricted this analysis to those clients enrolled in or before December 2005, as December 2006 was the last month for which data were available for this analysis. Clients who had no additional visits within twelve months after enrollment were considered single-visit clients. The number of return visits by a single client within twelve months after enrollment was ascertained; single-visit clients by definition had zero return visits within twelve months of enrollment.
2.3 Statistical Analyses
Frequency distributions of multi-visit usage and other study measures were generated for the entire study period and per calendar year. The chi-squared test was used to examine differences in multi-visit usage among different groups of clients. Negative binomial regression (used to model overdispered count data) was used to examine differences in number of return visits among different groups of clients. A one-year offset was used in this analysis to account for the twelve months during which clients could return. Chi-square tests for trend and Wilcoxon rank-sum tests were conducted to examine trends in retention over time overall and within demographic subgroups.
Multivariate logistic regression models were used to obtain adjusted odds of having multi-visit usage. Multivariate negative binomial regression was used to obtain the adjusted incidence rate of return visits. Year of enrollment was included in the multivariate models as a categorical variable in order to adjust for variables external to the individual that could impact client retention over time. In order to focus on client-level characteristics that impact retention, associations between the year of enrollment and outcomes are not reported. Goodness of fit was assessed based on likelihood ratio test statistics and the Akaike Information Criterion. To account for clustering of individuals by site where needed, regression models were built by using generalized estimating equations (GEE). Sites that enrolled fewer than 50 clients (n=4) were excluded from the multivariate regression analyses to prevent unstable estimates. Two variables (drug treatment and drug use frequency) were available in the electronic database consistently only after 1998; in order to utilize these data, models were at first restricted to clients enrolling in 1998 or later. When these characteristics were not included in the multivariate models, observations from all years were used. Models were first developed in the full sample and then in samples stratified by age (age < 30 and age ≥ 30). SAS v9.1 was used for data management and analyses.
3. RESULTS
NEP clients (N=12,388) enrolling in the BNEP between November 1994 and December 2005 were predominantly male (69%), African-American (73%), and over the age of 30 (86%) (Table 1). The median age was 39 (IQR 33–45). The median number of years of injection drug use was 17 (IQR 7–25 years) with 83% of clients reporting that they first injected drugs before the age of 30. Clients reported injecting a median of four times per day (IQR 3–5), and 59% reported ever having been in a drug treatment program. About one-third (36%) of clients reported living in the same zip code as the NEP site at which they enrolled, though the proportion living in proximity to the site differed significantly by enrollment site.
Table 1.
Selected characteristics of Baltimore NEP clients at enrollment, November 1994- December 2005 (N=12,388)
| Characteristics | N | % |
|---|---|---|
| Total | 12,388 | |
| Female | 3863 | 31% |
| < Age 30 | 1723 | 14% |
| Homeless | 437 | 4% |
| High school degree/GED | 7483 | 60% |
| Race | ||
| White | 2793 | 23% |
| Black/African-American | 9034 | 73% |
| Other | 543 | 4% |
| Marital Status | ||
| Single | 8232 | 66% |
| Widowed/Separated/Divorced | 2957 | 24% |
| Married | 1109 | 9% |
| Same Zip Code as Enrollment Site | 4321 | 36% |
| Employed | 1729 | 14% |
| Drug treatment (ever)* | 4093 | 59% |
| >20 years of injection drug use | 4808 | 39% |
| ≥ 4 injections per day* | 3375 | 48% |
These variables were collected routinely from 1998. Percentages are calculated out of 6910 unique clients.
Approximately two-thirds (64%) of clients had multi-visit usage within 12 months of the first NEP visit. The median number of return visits was one (IQR: 0–5 visits). Of those clients who returned at least once within one year, the median time to second visit was 20 days (IQR: 7–59 days). In univariate logistic models, several sociodemographic and behavioral characteristics were significantly correlated with having multi-visit usage (Table 2) and number of return visits (Table 3). In multivariate models, older clients (≥30) were more likely to have multi-visit usage. White race, having a high school diploma or the equivalent, being unmarried, having 20 or more years on injection drug use experience, and living within the zip code of the BNEP where the client was first enrolled were characteristics independently associated with multi-visit usage. Older age was also an important correlate of having more return visits in multivariate models. Being unmarried or unemployed, having more than 20 years of injection drug use experience, and living within the BNEP enrollment site zip code were independently associated with having more return visits.
Table 2.
Characteristics of Baltimore NEP clients at enrollment associated with multi-visit usage (N=12,388)
| Single Visit | Multiple visit | |||||
|---|---|---|---|---|---|---|
| Characteristics | N | % | N | % | OR of Multi- Visit (95% CI) | Adjusted Odds Ratio of Multi- Visit (95% CI)** |
| Total | 4458 | 7930 | ||||
| Predisposing | ||||||
| Female | 2489 | 31% | 5441 | 31% | 1.03 (0.95–1.11) | |
| < Age 30 | 774 | 17% | 949 | 12% | 0.65 (0.59–0.72)* | 0.69 (0.61–0.77)* |
| Homeless | 176 | 4% | 261 | 3% | 0.83 (0.68–1.01) | |
| High school degree/GED | 2634 | 59% | 4849 | 62% | 1.10 (1.02–1.18)* | 1.10 (1.02–1.18)* |
| Race | ||||||
| White | 1001 | 23% | 1792 | 23% | Ref | Ref |
| Black/African-American | 3221 | 72% | 5813 | 73% | 1.01 (0.92–1.10) | 0.80 (0.72–0.89)* |
| Other | 232 | 5% | 311 | 4% | 0.75 (0.62–0.90)* | 0.65 (0.53–0.79)* |
| Marital Status | ||||||
| Single | 3066 | 69% | 5166 | 66% | Ref | Ref |
| Widowed/Separated/Divorced | 947 | 21% | 2010 | 26% | 1.26 (1.15–1.38)* | 1.15 (1.04–1.26)* |
| Married | 416 | 9% | 693 | 9% | 0.99 (0.87–1.13) | 0.92 (0.80–1.05)* |
| Enabling | ||||||
| Same Zip Code as Enrollment Site | 1351 | 31% | 3113 | 40% | 1.50 (1.38–1.62)* | 1.49 (1.38–1.62)* |
| Employed | 640 | 14% | 1089 | 14% | 0.96 (0.86–1.06) | |
| Need | ||||||
| Drug treatment (ever) | 1418 | 57% | 2675 | 61% | 1.06 (0.96–1.18) | |
| >20 years of injection drug use | 1565 | 35% | 3243 | 42% | 1.28 (1.19–1.38)* | 1.19 (1.10–1.30)* |
| >4 injections per day | 1144 | 46% | 2231 | 51% | 1.08 (0.97–1.20) | |
Numbers do not sum to total population due to missing data for some variables. Multivariate models contained year of enrollment as a categorical variable to control for the association of external variables with the log odds of multi-visit usage.
significant at p < .05
GEE was used to account for possible clustering effects by site; the exchangeable correlation (rho) for this model was .02.
Table 3.
Characteristics at enrollment associated with number of return visits (N=12,388)
| Characteristics | IRR of Return Visits (95% CI) | Adjusted IRR of Return Visits(95% CI)** |
|---|---|---|
| Predisposing | ||
| Female | 0.93 (0.87–1.00)* | |
| < Age 30 | 0.51 (0.46–0.55)* | 0.19 (0.15–0.24)* |
| Homeless | 0.99 (0.84–1.17) | |
| High school degree/GED | 0.99 (0.93–1.06) | |
| Race | ||
| White | Ref | |
| Black/African-American | ||
| Other | ||
| Marital Status | ||
| Single | Ref | Ref |
| Widowed/Separated/Divorced | 1.13 (1.05–1.21)* | Ref |
| Married | 0.87 (0.78–0.97)* | 0.47 (0.33–0.68)* |
| Enabling | ||
| Same Zip Code as Enrollment Site | 1.45 (1.36–1.55)* | 4.16 (2.64–6.56)* |
| Employed | 0.74 (0.68–0.81)* | 0.46 (0.26–0.81)* |
| Need | ||
| Drug treatment (ever) | 0.96 (0.89–1.04) | |
| >20 years of injection drug use | 1.42 (1.34–1.51)* | 3.38 (2.48–4.61)* |
| >4 injections per day | 1.01 (0.94–1.09) | |
significant at p < .05
GEE was used to account for possible clustering effects by site; the exchangeable correlation (rho) for this model was .03. The overdispersion parameter for this model was 2.68. The offset was one year for all participants.
In order to further explore the predictors of retention among younger clients, we stratified both multivariate models by age group, comparing younger and older IDUs. Adjusted odds ratios and incidence rate ratios for older IDUs were similar to those for the entire population, and are therefore not shown. Among younger IDUs, white clients and those who lived within the BNEP site zip code where they were first enrolled had higher odds of multi-visit usage than non-white clients and those living outside of the BNEP site zip code, respectively (ORwhite 1.28, 95% CI: 1.01–1.62; ORsame zip 1.51, 95% CI: 1.23–1.87). While race was not associated with the number of return visits among younger IDUs, living within the BNEP site zip code remained a significant predictor of an increased number of return visits (IRRsame zip 4.42, 95% CI: 2.60–7.51).
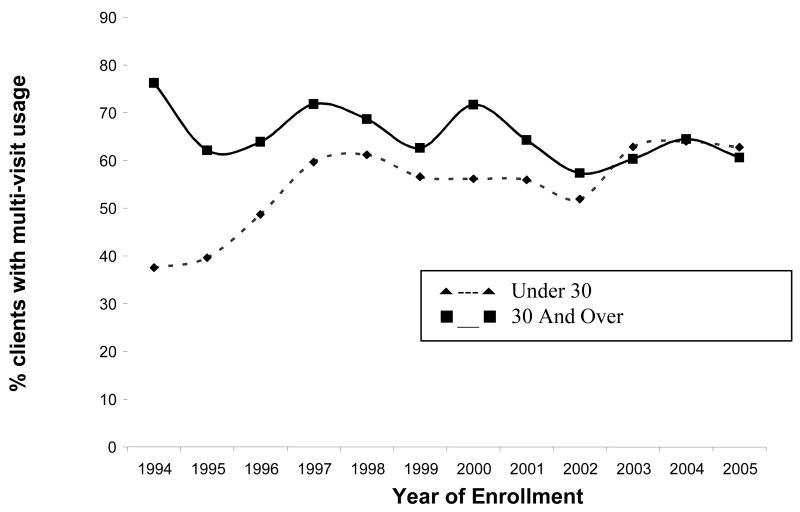
Changing patterns of retention over time were evident when comparing younger IDUs to older IDUs in frequency of multi-visit usage (Figure 1). In the first several years of the BNEP, older IDUs had roughly twice the odds of multi-visit usage compared to younger IDUs. However, since 2001, older IDUs have not been significantly more likely to have multi-visit usage (p>0.5 from 2002 to 2005). Wilcoxon rank-sum tests indicated that older IDUs had significantly greater median number of return visits than younger IDUs each year between 1994 and 2001, and that this difference disappeared in 2002 (p>.08 from 2002 to 2005).
Figure 1.
Proportion of enrolled clients with multi-visit usage over time: younger clients (dashed line), older clients (solid line)
4. DISCUSSION
Roughly one-third of clients enrolled between 1994 and 2005 did not return to the BNEP within twelve months of their first visit, consistent with the retention estimates in other NEPs (Hay and McKeganey, 2001; Khoshnood et al., 1995). Access to NEPs increased as the number and geographic diversity of BNEP sites grew, but retention did not show a clear increase over time. The relative stability of the overall retention rate and consistency with the twelve-month retention rates in the literature may indicate an average client retention among NEPs, robust to changes in program characteristics or population composition. Clients enrolled between 1994 and 2005 had a median of one return visit within twelve months. This is lower than the median number of return visits identified in the other NEP retention studies, though each study approached the calculation of this number differently.
Our study identified several characteristics associated with NEP client retention and found that the relative strength of these factors varied over the course of more than a decade, building upon the findings of earlier research that have examined retention over shorter periods of time (Deck and Carlson, 2005; Khoshnood et al., 1995; Messiah et al., 2003; Riley et al., 2002). Young age (<30), non-white race, not having a high school degree or the equivalent, being married, being unemployed, having an injection drug use history of less than twenty years, and living farther from the BNEP site were all characteristics independently associated with low retention in multivariate analyses. Several characteristics were identified in models examining both measures of retention, and likely reflect stronger underlying associations.
To better understand these associations, we framed our hypotheses using Andersen’s behavior model of health services use. While this model was primarily designed to explain access and initial use of general health services, Andersen notes that health services utilization can refer to initial contact as well as frequency of use, allowing for the adaptation of the model to help understand continued use of specialized health services like NEPs. Andersen also notes that how utilization is measured can have a considerable impact on the types of characteristics identified as determinants.
For both of our utilization outcomes, multi-visit usage and number of return visits, we have used a period of twelve months as the total observation time for each client. The one year period also has practical programmatic significance, with BNEP program objectives, budgets, and staffing often determined on an annual basis. Similar methods of analysis were used to examine retention in other NEPs (Hay and McKeganey, 2001; Khoshnood et al., 1995). Using a period of six months in the analysis would have yielded qualitatively similar results; of those clients who returned at least once within twelve months, 92% returned within the first six months. To capture an additional dimension of retention, we also examined the frequency of a client’s return within twelve months of enrollment.
Andersen’s model predicts that such predisposing factors as age, race, marital status, education, and occupation would be associated with willingness to use the NEP. People in different demographic subgroups have different norms and beliefs about seeking services as well as different service-related needs. We might expect that clients who are demographically similar to the majority of IDUs in Baltimore (e.g. older, African American, male, unmarried, less educated) would have higher rates of return. IDUs who report being unemployed or report living closer to the enrollment site may have more time and more access to the NEP, and we would expect these enabling factors to be associated with increased retention. Clients who report higher injection frequency, a longer history of injection, and no experience with drug treatment would be expected to exhibit more need, and consequently higher rates of return to the NEP.
Not all of the observed associations between predisposing, enabling, and need factors and retention were in the direction we had predicted. Though we expected that clients who looked like the majority at the BNEP to have higher rates of return, African American clients were actually less likely to return than white clients. Neither race nor gender was associated with the number of return visits to the BNEP. Therefore, the impact of predisposing factors may not be related to majority status, rather to the group-specific norms and beliefs about NEP use. Previous studies have shown that peer norms and behavior are highly predictive of injection risk behavior. (Golub et al., 2007; Hawkins et al., 1999; Thiede et al., 2007). Peer influences may play a particularly important role; decreases in the number and proportion of African-American clients accessing the BNEP over time may have lead to less retention of African-American clients.
Other predisposing factors were associated with retention in the expected directions. We found that younger IDUs were less likely to return to the BNEP even after adjustment for a range of factors, results that are consistent with other studies that have identified younger IDUs as less likely to return to an NEP, (Khoshnood et al., 1995) less likely to seek drug treatment after a referral, (Riley et al., 2002) and less likely to be retained in drug treatment once enrolled (Deck and Carlson, 2005). Similar factors may therefore influence retention among younger IDUs in all three harm-reduction strategies. Low retention among younger BNEP clients could also reflect younger IDUs’ infrequent use of general health services as compared to older IDUs. Older IDUs (≥40 years old) participating in the ALIVE study, a cohort study of IDUs in Baltimore, were significantly more likely to use health care services than younger IDUs, even though reported access to health care services did not differ by age group (Knowlton et al., 2001). Younger IDUs in ALIVE were also more likely to stop injecting drugs and enter drug treatment than older IDUs (Galai et al., 2003). Younger IDUs may also be less likely to return for a second BNEP visit because they may have a higher probability of being incarcerated. Younger IDUs in Baltimore’s ALIVE study were more likely to have been incarcerated than older participants (S. Mehta, personal comm.), with 26% of young IDUs in another Baltimore study reporting incarceration in the previous 6 months (Sherman et al., 2004).
Also as expected, clients reporting that they were married at enrollment had lower retention rates than unmarried clients. Married clients may be more likely to reduce their substance use (Duncan et al., 2006; Merline et al., 2008). Married clients may also have more stability and access to health care than unmarried clients, allowing them to seek treatment rather than NEP services (Schütz et al., 1994; Zanis et al., 1994).
Proximity to an NEP enrollment site, an enabling factor, was associated with retention, differing slightly from previous findings. Proximity to the site was not found to be predictive of retention in an urban NEP (Khoshnood et al., 1995) or of retention in a methadone maintenance program, (Deck and Carlson, 2005) though the geographical units used in these studies (e.g. city, county) were much larger than the zip code-level analysis conducted here. In qualitative reports, NEP clients have previously identified residing too far from the treatment facility as a barrier to accessing drug treatment after a referral (Riley et al., 2002), indicating that IDUs themselves consider proximity to be an important enabling factor in accessing and continuing involvement with harm-reduction services. While employment was not independently associated with multi-visit usage, clients who reported that they were employed tended to have fewer return visits than unemployed clients. Employed clients may be restricted in their ability to attend the BNEP sites because of the hours and days of site operation; night and weekend hours are not offered at all BNEP locations.
One indicator of need for services, injection drug use history, was associated with retention. As expected, clients with fewer years of injection history were less likely to return to the BNEP and had fewer return visits. IDUs with a more established injection history are less likely to quit injection than recent onset IDUs (Galai et al., 2003; Huo et al., 2006). Though need factors like injection frequency and drug treatment history should figure strongly in initial access to services, there may not be enough variability in need for services among IDUs already accessing the NEP to predict tcontinued use. Andersen’s model also notes the importance of the structural and political contexts in health service utilization, which are factors likely to influence day to day NEP operations and therefore both initial and continued use of the NEP.
Our study is subject to some limitations. Using administrative data to determine when clients accessed the BNEP does not allow us to identify clients who do not return because they enter drug treatment, those who are no longer using injection drugs, those who overdose, or those who are incarcerated for a drug-related offense. All variables except for return to the BNEP are self-reported and may be subject to misclassification due to issues with recall or social desirability, though studies have shown that most behavioral and demographic variables self-reported by IDUs tend to be valid and reliable (Gibson and Young, 1994).
Barriers to continued use of NEP services likely exist for all IDUs in Baltimore, but these barriers may disproportionately affect newer, younger, and non-white IDUs, as well as those who live further from BNEP sites. These barriers to accessing harm reduction activities are particularly detrimental for those IDU subgroups known to be at high risk of viral infections, such as new and young IDUs.
This work has identified predisposing, enabling, and need factors that predict decreased retention among Baltimore NEP clients, and examined the patterns of these associations over time. More research is needed on the mechanisms by which age, race, and proximity to NEP site influence retention. Further qualitative work would be needed to explore the attitudes and beliefs associated with return among demographic subgroups. Further insight may help in developing programmatic changes that will be effective in increasing retention. Encouraging continued NEP access will be an important method to reduce infections, especially among younger IDUs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of health and social behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Bailey SL, Huo D, Garfein RS, Ouellet LJ. The use of needle exchange by young injection drug users. J Acquir Immune Defic Syndr. 2003;34:67–70. doi: 10.1097/00126334-200309010-00010. [DOI] [PubMed] [Google Scholar]
- Brooner R, Kidorf M, King V, Beilenson P, Svikis D, Vlahov D. Drug abuse treatment success among needle exchange participants. Public Health Rep. 1998;113(Suppl 1):129–139. [PMC free article] [PubMed] [Google Scholar]
- Burrows D. Rethinking coverage of needle exchange programs. Subst Use Misuse. 2006;41:1045–1048. doi: 10.1080/10826080600667201. [DOI] [PubMed] [Google Scholar]
- Cassin S, Geoghegan T, Cox G. Young injectors: a comparative analysis of risk behaviour. Irish journal of medical science. 1998;167:234–237. doi: 10.1007/BF02937420. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Compton WM, Ben-Abdallah A, Horne M, Claverie D. Achieving a 96.6 percent follow-up rate in a longitudinal study of drug abusers. Drug Alcohol Depend. 1996;41:209–217. doi: 10.1016/0376-8716(96)01254-9. [DOI] [PubMed] [Google Scholar]
- Deck D, Carlson MJ. Retention in publicly funded methadone maintenance treatment in two Western States. J Behav Health Serv Res. 2005;32:43–60. doi: 10.1007/BF02287327. [DOI] [PubMed] [Google Scholar]
- Duncan GJ, Wilkerson B, England P. Cleaning up their act: the effects of marriage and cohabitation on licit and illicit drug use. Demography. 2006;43:691–710. doi: 10.1353/dem.2006.0032. [DOI] [PubMed] [Google Scholar]
- Fennema JS, Van Ameijden EJ, Van Den Hoek A, Coutinho RA. Young and recent-onset injecting drug users are at higher risk for HIV. Addiction. 1997;92:1457–1465. [PubMed] [Google Scholar]
- Galai N, Safaeian M, Vlahov D, Bolotin A, Celentano DD. Longitudinal patterns of drug injection behavior in the ALIVE Study cohort, 1988–2000: description and determinants. Am J Epidemiol. 2003;158:695–704. doi: 10.1093/aje/kwg209. [DOI] [PubMed] [Google Scholar]
- Garfein RS, Vlahov D, Galai N, Doherty MC, Nelson KE. Viral infections in short-term injection drug users: the prevalence of the hepatitis C, hepatitis B, human immunodeficiency, and human T-lymphotropic viruses. Am J Public Health. 1996;86:655–661. doi: 10.2105/ajph.86.5.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson DR, Young M. Assessing the reliability and validity of self reported risk behavior. In: Battjes RJ, Sloboda Z, Grace WC, editors. The Context of HIV Risk Among Drug Users and Their Sexual Partners. NIDA; Rockville, Maryland: 1994. pp. 218–235. [Google Scholar]
- Golub ET, Strathdee SA, Bailey SL, Hagan H, Latka MH, Hudson SM, Garfein RS. Distributive syringe sharing among young adult injection drug users in five U.S. cities. Drug Alcohol Depend. 2007 doi: 10.1016/j.drugalcdep.2007.02.013. [DOI] [PubMed] [Google Scholar]
- Hawkins WE, Latkin C, Mandel W, Oziemkowska M. Do actions speak louder than words? Perceived peer influences on needle sharing and cleaning in a sample of injection drug users. AIDS Educ Prev. 1999;11:122–131. [PubMed] [Google Scholar]
- Hay G, McKeganey N. The attendance pattern of clients at a Scottish needle exchange. Addiction. 2001;96:259–266. doi: 10.1046/j.1360-0443.2001.9622599.x. [DOI] [PubMed] [Google Scholar]
- Heimer R. Can syringe exchange serve as a conduit to substance abuse treatment? J Subst Abuse Treat. 1998;15:183–191. doi: 10.1016/s0740-5472(97)00220-1. [DOI] [PubMed] [Google Scholar]
- Huo D, Bailey SL, Ouellet LJ. Cessation of injection drug use and change in injection frequency: the Chicago Needle Exchange Evaluation Study. Addiction. 2006;101:1606–1613. doi: 10.1111/j.1360-0443.2006.01577.x. [DOI] [PubMed] [Google Scholar]
- Huo D, Ouellet LJ. Needle exchange and injection-related risk behaviors in Chicago: a longitudinal study. J Acquir Immune Defic Syndr. 2007;45:108–114. doi: 10.1097/QAI.0b013e318050d260. [DOI] [PubMed] [Google Scholar]
- Khoshnood K, Kaplan EH, Heimer R. ‘Dropouts’ or ‘drop-ins’? Client retention and participation in New Haven’s needle exchange program. Public Health Rep. 1995;110:462–466. [PMC free article] [PubMed] [Google Scholar]
- Knowlton AR, Hoover DR, Chung SE, Celentano DD, Vlahov D, Latkin CA. Access to medical care and service utilization among injection drug users with HIV/AIDS. Drug Alcohol Depend. 2001;64:55–62. doi: 10.1016/s0376-8716(00)00228-3. [DOI] [PubMed] [Google Scholar]
- Kral AH, Lorvick J, Edlin BR. Sex- and drug-related risk among populations of younger and older injection drug users in adjacent neighborhoods in San Francisco. J Acquir Immune Defic Syndr. 2000;24:162–167. doi: 10.1097/00126334-200006010-00011. [DOI] [PubMed] [Google Scholar]
- Lurie P, Gorsky R, Jones TS, Shomphe L. An economic analysis of needle exchange and pharmacy-based programs to increase sterile syringe availability for injection drug users. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18(Suppl 1):S126–132. doi: 10.1097/00042560-199802001-00021. [DOI] [PubMed] [Google Scholar]
- Merline AC, Schulenberg JE, O’Malley PM, Bachman JG, Johnston LD. Substance use in marital dyads: premarital assortment and change over time. J Stud Alcohol Drugs. 2008;69:352–361. doi: 10.15288/jsad.2008.69.352. [DOI] [PubMed] [Google Scholar]
- Messiah A, Navaline H, Davis-Vogel A, Tobin-Fiore D, Metzger D. Sociodemographic and behavioral characteristics associated with timeliness and retention in a 6-month follow-up study of high-risk injection drug users. Am J Epidemiol. 2003;157:930–939. doi: 10.1093/aje/kwg065. [DOI] [PubMed] [Google Scholar]
- Novelli LA, Sherman SG, Havens JR, Strathdee SA, Sapun M. Circumstances surrounding the first injection experience and their association with future syringe sharing behaviors in young urban injection drug users. Drug Alcohol Depend. 2005;77:303–309. doi: 10.1016/j.drugalcdep.2004.08.021. [DOI] [PubMed] [Google Scholar]
- Ouellet L, Huo D, Bailey SL. HIV risk practices among needle exchange users and nonusers in Chicago. J Acquir Immune Defic Syndr. 2004;37:1187–1196. doi: 10.1097/01.qai.0000120802.43677.ea. [DOI] [PubMed] [Google Scholar]
- Riley ED, Safaeian M, Strathdee SA, Brooner RK, Beilenson P, Vlahov D. Drug user treatment referrals and entry among participants of a needle exchange program. Subst Use Misuse. 2002;37:1869–1886. doi: 10.1081/ja-120014088. [DOI] [PubMed] [Google Scholar]
- Schütz C, Rapiti E, Vlahov D, Anthony J. Suspected determinants of enrollment into detoxification and methadone maintenance treatment among injecting drug users. Drug and Alcohol Dependence. 1994;36:129–138. doi: 10.1016/0376-8716(94)90095-7. [DOI] [PubMed] [Google Scholar]
- Sherman SG, Rusch M, Golub ET. Correlates of safe syringe acquisition and disposal practices among young IDUs: broadening our notion of risk. Journal of Drug Issues. 2004;34:895–912. [Google Scholar]
- Strathdee S, Vlahov D. The effectiveness of needle exchange programs: A review of the science and policy. AIDScience. 2001;1 [Google Scholar]
- Strathdee SA, Celentano DD, Shah N, Lyles C, Stambolis VA, Macalino G, Nelson K, Vlahov D. Needle-exchange attendance and health care utilization promote entry into detoxification. J Urban Health. 1999;76:448–460. doi: 10.1007/BF02351502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strike CJ, Challacombe L, Myers T, Millson M. Needle exchange programs. Delivery and access issues. Can J Public Health. 2002;93:339–343. doi: 10.1007/BF03404565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiede H, Hagan H, Campbell JV, Strathdee SA, Bailey SL, Hudson SM, Kapadia F, Garfein RS. Prevalence and correlates of indirect sharing practices among young adult injection drug users in five U.S. cities. Drug Alcohol Depend. 2007 doi: 10.1016/j.drugalcdep.2007.03.001. [DOI] [PubMed] [Google Scholar]
- U.S. House of Representatives. General definition of homeless individual. Office of the Law Revision Counsel, U.S.H.o.R; 2005. [Google Scholar]
- Wodak A, Cooney A. Do needle syringe programs reduce HIV infection among injecting drug users: a comprehensive review of the international evidence. Subst Use Misuse. 2006;41:777–813. doi: 10.1080/10826080600669579. [DOI] [PubMed] [Google Scholar]
- Zanis DA, Metzger DS, McLellan AT. Factors associated with employment among methadone patients. J Subst Abuse Treat. 1994;11:443–447. doi: 10.1016/0740-5472(94)90097-3. [DOI] [PubMed] [Google Scholar]