Abstract
The potential modulation of TRPV1 nociceptive activity by the CB1 receptor was investigated here using CB1 wild-type (WT) and knock-out (KO) mice as well as selective CB1 inverse agonists. No significant differences were detected in baseline thermal thresholds of ICR, CB1WT or CB1KO mice. Intraplantar capsaicin produced dose- and time-related paw flinch responses in ICR and CB1WT mice and induced plasma extravasation yet minimal responses were seen in CB1KO animals with no apparent differences in TRPV1 channel expression. Capsaicin-evoked CGRP release from spinal cord tissue and capsaicin-evoked action potentials on isolated skin-nerve preparation were significantly decreased in CB1KO mice. Pretreatment with intraplantar galanin and bradykinin, compounds known to sensitize TRPV1 receptors, restored capsaicin-induced flinching in CB1KO mice. The possibility that constitutive activity at the CB1 receptor is required to maintain the TRPV1 receptor in a “sensitized” state was tested using CB1 inverse agonists. The CB1 inverse agonists elicited concentration-related inhibition of capsaicin-induced calcium influx in F-11 cells and produced dose-related inhibition of capsaicin-induced flinching in ICR mice. These data suggest that constitutive activity at the CB1 receptor maintains the TRPV1 channel in a sensitized state responsive to noxious chemical stimuli. Treatment with CB1 inverse agonists may promote desensitization of the channel resulting in antinociceptive actions against chemical stimulus modalities. These studies propose possible therapeutic exploitation of a novel mechanism providing pain relief by CB1 inverse agonists.
Keywords: TRPV1, CB1, capsaicin, pain, phospholipase C, knock-out mouse
Introduction
The transient receptor potential vanilloid 1 (TRPV1) channel has been established as a molecular sensor of noxious heat and chemicals including capsaicin (Caterina et al., 1997). The TRPV1 receptor cannot only be directly activated by protons (Tominaga et al., 1998), lipoxygenase products (Hwang et al., 2000) and endocannabinoids (Zygmunt et al., 1999) but can also be modulated by lipids (Chuang et al., 2001), heat >43°C, low pH (Caterina et al., 1997; Tominaga et al., 1998) and endovanilloids (Premkumar and Ahern, 2000). Additionally, activity at numerous G-protein coupled receptors (GPCRs) including the galanin-R1 (Jimenez-Andrade et al., 2004), somatostatin-S2 (Carlton et al., 2004), bradykinin-B2 (Cesare and McNaughton, 1996), and cannabinoid-CB1 (Hermann et al., 2003; Patwardhan et al., 2006) has also been demonstrated to modulate TRPV1 function. Chimeric and site-directed mutation studies of the TRPV1 have identified unique amino acid sites that are phosphorylated (Bhave et al., 2002, 2003; Jung et al., 2004) resulting in increased responsiveness of the channel to stimuli including capsaicin. Likewise, the dephosphorylation of TRPV1 channels can lead to pharmacological desensitization of the channel (Koplas et al., 1997; Mohapatra and Nau, 2005). Although TRPV1 is modulated by multiple pathways, this channel is an important integrator of nociceptive stimuli (Caterina et al., 2000) resulting from activation of various receptors on afferent fibers leading to intense efforts in developing TRPV1 antagonists as pain relieving drugs.
Endogenous and exogenous cannabinoids have been shown to inhibit pain behaviors (Pertwee, 1997; Richardson et al., 1998a,b) as well as capsaicin-induced release of calcitonin gene-related peptide (CGRP) via CB1 receptors (Richardson et al., 1998a,b; Ahluwalia et al., 2003). However, more recent studies reported that endogenous cannabinoids such as anandamide (AEA) activate TRPV1 which may result in afferent excitation (Zygmunt et al., 1999; Hermann et al., 2003; Price et al., 2005; Evans et al., 2007). Recent reports demonstrate the expression of CB1 and TRPV1 proteins on the same cells (Ahluwalia et al., 2000, 2002; Binzen et al., 2006; Mitrirattanakul et al., 2006) providing an anatomical basis for modulation of TRPV1 function by compounds interacting at the CB1 receptor. Although cannabinoid modulation of the TRPV1 channel has been demonstrated with WIN 55,212–2 which is thought to inhibit capsaicin activity via the activation of calcineurin (Jeske et al., 2006; Patwardhan et al., 2006), the precise pathway(s) by which CB1 receptors modulate TRPV1 function remain to be established. Studies using CB1 receptor inverse agonists including SR141716A and AM251 have suggested constitutive activity at the CB1 receptor in animals (Gifford and Ashby, 1996; Zhou and Shearman, 2004) and humans (Després et al., 2005; Huestis et al., 2007), and CB1 activation was also shown to sensitize TRPV1 receptors in an heterologous expression system (Hermann et al., 2003). Recently it has been shown that repeated administration of SR141716A is effective in alleviating thermal and mechanical hyperalgesia in a rat model of nerve injury (Costa et al., 2005). Here, we further investigate modulation of TRPV1 responsiveness through compounds acting at CB1 receptors, or through intracellular pathways associated with the TRPV1 receptor as well as the possibility that CB1 inverse agonists may negatively modulate TRPV1 responses to produce antinociception relevant to clinical pain states.
Materials and Methods
Animals
Male ICR mice (25–35 g) were purchased from Harlan. Male CB1 receptor wild-type (WT) and knock-out (KO) mice were obtained as a generous gift from Dr. Debra Cockayne, Roche Biosciences and bred in house. All animals were housed on a regular 12 h light/dark cycle (lights on at 07:00 A.M.) in a climate-controlled room with food and water ad libitum. All studies were performed while animals were on their light cycle between the times of 7:00 A.M. and 7:00 P.M. Mice were housed three to a cage and each animal was used only once per experiment. All procedures were approved by the University of Arizona Animal Care and Use Committee and were in accordance with the guidelines of the International Association for the Study of Pain.
Materials
Morphine sulfate and SR141716A were provided by the National Institute on Drug Abuse (Bethesda, MD). AM251 was purchased from Tocris. U73122 was obtained from Biomol International and m-3M3FBS was purchased from EMD Biosciences. Capsaicin, capsazepine, galanin, formalin, mustard oil, ethanol, DMSO, Tween 80 and PEG 400 were obtained from Sigma. Bradykinin was purchased from Bachem. Evans blue dye was purchased from Eastman Kodak Co. All solutions were prepared on the day of each experiment.
Capsaicin-induced paw flinching in ICR mice
Mice were placed separately in Plexiglas boxes for a 20–30 min habituation period. Post habituation, capsaicin (1, 5, or 10 μg) in ethanol (100%) was injected into the plantar side of the mouse left hind paw, using a 30 gauge needle attached to a 25 μl Hamilton syringe in a volume of 5 μl; this volume was used for all intraplantar injections unless otherwise specified. In all studies, flinches of the capsaicin-injected hind paw were recorded in 1 min bins for 5 min. In all studies of modulation of capsaicin-induced flinching, the dose of intraplantar capsaicin was 10 μg. A flinch was defined as a rapid jerk of the injected paw. Control experiments were performed in all studies using the capsaicin vehicle (100% ethanol); the vehicle did not produce any significant nociceptive behaviors when injected into the hind paw at this volume.
Modulation of capsaicin-induced flinching in ICR mice
To investigate the effects of an opioid agonist on capsaicin-induced flinching, morphine (0.3, 1 and 3 mg/kg) was dissolved in saline and administered intraperitoneally (i.p.) using a 27 gauge needle, 15 min before intraplantar capsaicin. Separate animals were used for the different doses of morphine. Control experiments included animals that received saline by the i.p. route and capsaicin by the intraplantar route 15 min post saline. Intraperitoneal injections were performed by holding the animals in a supine position and inserting the extremity of a 27 gauge disposable needle attached to a 1cc disposable syringe into the peritoneal cavity in the lower left quadrant of the abdomen. SR141716A (0.03, 0.3, 1.0 and 3 mg/kg) or AM251 (0.03, 0.1, 0.3 mg/kg) were dissolved in PEG 400 and always administered i.p. 15 min before intraplantar capsaicin. Control animals received the PEG 400 vehicle by the i.p. route 15 min before capsaicin. U73122 (10 and 30 mg/kg), a PLC inhibitor (Hou et al., 2004), was administered i.p. in ICR mice 1 h before intraplantar injection of capsaicin. In separate groups of animals, m-3M3FBS, a PLC activator (Bae et al., 2003), was administered by the i.p. route at 5 mg/kg 30 min before treatment with i.p. SR141716A (0.3 mg/kg) and 45 min before challenge with intraplantar capsaicin. Both U73122 and m-3M3FBS were dissolved in 1:1:8 DMSO/Tween 80/saline.
Capsaicin-induced flinching in CB1WT and CB1KO mice
CB1WT or KO mice respectively received 1, 5 and 10 μg or 1, 5, 10, 30 and 100 μg of capsaicin in the plantar side of the left hind paw. Separate animals received vehicle (100% ethanol) concurrently. The number of flinches was recorded in 1 min bins for 5 min.
Modulation of capsaicin-induced flinching in CB1WT and KO mice
To test whether galanin would restore reduced capsaicin-induced flinching in CB1KO mice, galanin (0.1 ng/20 μl) was administered as in the dose and volume described by Jimenez-Andrade et al. (2004) using ICR, CB1WT and KO mice. Intraplantar capsaicin was administered in the same paw immediately after galanin injection. As a control, galanin administration was followed by intraplantar vehicle (100% ethanol) and flinching behaviors recorded in all strains of mice. Bradykinin was administered by the intraplantar route at 3 μg in a volume of 5 μl in ICR, CB1WT and KO mice. At this dose bradykinin itself induced a small number of flinches, which were recorded but no longer present within 5 min. Intraplantar capsaicin was then injected into the same hind paw, 10 min after the initial bradykinin injection. As a control, intraplantar bradykinin was followed by a challenge with intraplantar vehicle (100% ethanol) as described for capsaicin.
Cell culture of F-11 cells
F-11 cells (a gift from Dr. Fishman) (Platika et al., 1985) (mouse neuroblastoma × rat dorsal root ganglion neuron hybrid cell line) were cultured and maintained in 75 cm2 flasks at 37°C and 5%CO2 in Ham's F-12 supplemented with 15% fetal bovine serum, 5% newborn calf serum, 1% penicillin/streptomycin and 1% HAT. For calcium imaging experiments, 5 × 104 cells were plated in the area of cloning ring attached on the Delta-T dishes (Bioptechs). Cell differentiation was initiated 24 h after plating by replacing culture medium with the following medium: Ham's F-12 supplemented with 1% FBS, 50 ng/ml NGF, 2 μm retinoic acid, 0.5 mm cAMP, 10 μm IBMX, 125 μg/ml insulin, 10 μg/ml transferrin, and 50 IU/ml penicillin/streptomycin. Cultures were maintained for 72 h in this medium before experiments.
Ca2+ imaging assay
F-11 cells were washed three times with bath solution and loaded with 5 μm fura-2/AM (Molecular Probes) at 37°C for 40 min. The bath solution (Hanks' balanced salt solution) contained 136 mm NaCl, 5.4 mm KCl, 2 mm CaCl2, 1 mm MgSO4, 5.5 mm glucose, 10 mm HEPES, pH 7.4. Cells were washed twice and incubated at 37°C for another 10 min. The cells were maintained at 37°C throughout the experiment with the Delta TC3 open culture dish system (Bioptechs). Image acquisition was performed using a Nikon TE200 outfitted with a plan fluor 40× oil N.A. 1.3 objective lens, Xenon burner, an ORCA Hi binning 12 bit digital camera, filter wheel with fura-2 filter set controlled by Mutech image master digital workstation and Metafluor imaging software (Universal Imaging). The ratiometric fluorescence images were captured at 6 s intervals. The changes in the fluorescence level of individual cells over time are obtained by digitizing the integrated optical density of fura-2 emission at 510 nm as a ratio of 340 nm/380 nm excitation associated with a designated cell area of the serial images. Individual experiments were performed in triplicate (Lai et al., 2006). SR141716A (10 and 100 nm) or AM251 (10 or 100 nm) were dissolved in PEG 400 and administered 10 min before capsaicin (10 nm).
Western blot analysis
The L4, L5 and L6 dorsal root ganglia (DRG)s and dorsal horns (lumbar enlargement) were removed from mice and homogenized separately in an ice-cold 10 mm sodium phosphate buffer, pH 7.4, containing 100 μm PMSF, bestatin (30 μm) and captopril (10 μm). The membrane fractions of sequentially centrifugal extractions were performed as follows. Briefly, the homogenate was centrifuged at 2000 × g for 10 min at 4°C. The supernatant was removed and centrifuged at 16,500 rpm for 1 h at 4°C. The pellet was solubilized in the 10 mm sodium phosphate buffer containing 2% Triton X-100, 4% SDS and the mixture of protease inhibitors. The resultant membrane protein was refined by passage through 23 gauge and 27.5 gauge needle several times. The protein concentration was determined with a standard Lowry assay as described previously (Bilsky et al., 1996). Protein samples were separated on a SDS-PAGE gradient gel (4–15%; Bio-Rad) and transferred to the nitrocellulose membrane. The blots were blocked with 3% nonfat dry milk, 2% goat serum and 2% mouse serum for 30 min and incubated with rabbit-anti-rat vanilloid receptor subtype 1 (TRPV1) antibodies (Alpha Diagnostic, TX) (3 μg/ml) for 1.5 h at room temperature. The blots were then incubated in goat-anti-rabbit HRP-conjugated secondary antibody 1:5,000 (Jackson ImmunoResearch) for 1 h at room temperature, developed in ECL solution (Amersham Pharmacia) for 1 min, and exposed onto X-films (Hyperfilm; Amersham) for 30 min. The cross-reactivity of the antibody to mouse TRPV1 is proven by the detection of TRPV1 protein in the DRGs from ICR mice. Gαq antibodies (Santa Cruz, CA) 1:500 were applied on the same membrane as an internal loading control although Western blots were not used for quantitative purposes.
Reverse transcription PCR
Total RNA was isolated from F-11 cells and rat DRGs using RNAqueous-total RNA isolation kit (Ambion). First strand cDNA was reverse transcribed using RETROscript kit (Ambion) following manufacturer's instructions. For multiplex PCR amplifications, 3 μl of the first-strand cDNA template were used in 20 μl of reactions containing 1× PCR buffer, 0.25 μm each sense and antisense primer, 125 μm each dNTP, and 1 U of TaqDNA polymerase (Invitrogen). 1× PCR buffer contained 10 mm Tris-HCl, 50 mm KCl, 0.1% Triton X-100, and 1.5 mm MgCl2. PCR was performed in PCR Express Thermal Cycler (Thermo Hybrid) as follows: (1) hold at 94°C for 2 min; (2) 35 cycles at 94°C for 40 s, 55°C for 40 s, and 72°C for 1 min; (3) hold at 4°C. Primer sequences for CB1 were 5′-AAGAGGATCGTCACCAGG-3′ (sense) and 5′-CCAGCCTAATGTCCATGC-3′ (antisense); and that for TRPV1 were 5′-CAACGCAAGGAGTATGTGG-3′ (sense) and 5′-GAGTTACCTGGCTTGCAG-3′. GAPDH (sense primer: 5′-CACGGCAAGTTCAATGGC-3′; antisense primer: 5′-GCCTGCTTCACCACCTTC-3′) was coamplified with CB1 or TRPV1 cDNA as an internal control. The PCR products were run on a 2% agarose gel containing ethidium bromide, visualized by UV illumination, and then photographed. Primers used for PCR amplification were synthesized from Midland.
Skin nerve electrophysiological recordings
Male ICR mice, CB1WT or CB1KO mice were recorded from in random order, and the investigator was blinded as to their genotype. The saphenous nerve and innervated skin were removed from mice and placed in an organ bath and bathed with synthetic interstitial fluid (SIF) buffer as previously described (Stucky et al., 2004). The nerve was placed in a separate chamber filled with mineral oil, desheathed, and teased into fine filaments. Single units were identified by mechanical stimulation with a glass probe. Conduction velocity was determined by applying electrical pulses to the receptive field via a tungsten needle electrode. Only unmyelinated C fibers were recorded for this study and C fibers were identified as units conducting slower than 1.2 m/s. Mechanical threshold was determined by using calibrated von Frey filaments (range, 0.04–147 mN). Data were recorded using Chart (AD Instruments). For chemical stimulation, a stock solution of capsaicin (10 mm) was made in 1-methyl-2-pyrrolidinone (Sigma), a solvent that has no effect on fibers in the skin nerve preparation (Stucky et al., 2004) and stored at −20°C. On the day of recording, the capsaicin stock was diluted in 32°C SIF buffer just before application. The receptive field of the C fiber was isolated with a stainless steel ring (6 mm ID) that was sealed to the skin with a thin layer of vacuum grease. First, a control was performed by applying 1:100 1-methyl-2-pyrrolidinone:SIF buffer (32°C) for 1 min. Next, 100 μm capsaicin was applied for 1 min and the number of evoked action potentials were counted. Capsaicin was applied at 100 μm because this concentration maximally activates C fibers (∼58% of all C fibers) in the skin nerve preparation. The criterion for a positive response to chemical or mechanical stimuli was at least three evoked action potentials. If any action potentials occurred during the application of control solution, these action potentials were subtracted from the total capsaicin-evoked action potentials. To confirm that noncapsaicin responsive fibers were still active, each fiber was stimulated mechanically with a glass rod at the end of recording. Fibers that were unresponsive to the terminal mechanical test were excluded from the data. Only fibers with nonoverlapping receptive fields were used from the same skin preparation.
Plasma extravasation
Extravasation of plasma albumin in mice was assessed by the Evans blue leakage method. Evan's blue dye (100 mg/kg) in saline was injected using a 30 gauge needle attached to a 1 ml syringe in the tail 15 min after capsaicin (10 μg) administration in the left hind paw. Vehicle (100% ethanol) was injected in the contralateral paw (right), so that each mouse served as its own control. Two hours after Evan's blue injection animals were killed under ether and hind paw tissue was removed with an 8 mm hole-puncher. The tissue was incubated in 100% formamide, 50°C water bath for 2 h and samples were centrifuged at 14000 rpm for 20 min. The supernatant was collected and measured by spectrophotometry at 620 nm (Beckman DU-62 Spectrophotometer). The absorbance values were calculated from a calibration curve. The amount of extracted dye was expressed as fmol of dye per gram of wet tissue, as described (Trevisani et al., 2002).
CGRP release assay
Tissue extraction and preparation.
Mice were deeply anesthetized using CO2 and decapitated. The spinal cord was severed at the pelvic girdle. Hydraulic extrusion was performed by inserting a 16 gauge needle into the sacral vertebral canal and expelled with ice-cold saline. The spinal cord was immediately placed on ice in a glass Petri dish, and the dorsal half of the lumbar cord was dissected, weighed and chopped into 0.2 mm cubes with a McIwain tissue chopper (Mickle Laboratory Engineering).
CGRP assays.
Chopped lumbar spinal cord tissue was placed in a 1 cc superfusion chamber and continuously superfused with oxygenated modified Krebs' buffer (135 mm NaCl, 3.5 mm KCl, 20 mm NaHCO3, 1 mm NaHPO4, 2.5 mm CaCl2, 3.3 mm dextrose, 0.1 mm ascorbic acid, 10 mm thiorphan and 0.1% bovine serum albumin) maintained at 37°C, pH 7.4, at a rate of 0.5 ml/min with a Brandel Superfusion Pump. The tissues were equilibrated for 30 min. Superfusate samples were collected into test tubes using a fraction collector (Gilson) every 3 min and measured for CGRP release. A total of 5 fractions (15 min) were collected to establish baseline levels of CGRP release before capsaicin (1 μm) was applied for 2 fractions (6 min). Superfusate was then collected for an additional 8 fractions (24 min). The superfusate obtained from the release assay was preincubated with 100 μl of a C terminus directed anti-CGRP antibody (Peninsula Laboratory) for 24 h at 4°C. The samples were each mixed with 50 μl of goat anti-rabbit antiserum coupled to ferric beads and 100 μl of [125I-Tyr0]CGRP28–37 (at ∼25,000 cpm per assay tube) and incubated for an additional 24 h. The [125I]CGRP bound to the CGRP antibody was separated from the free tracer through immunomagnetic separation (PerSeptive Diagnostics). The immunoprecipitates were determined by gamma counting. Standard curves were generated and CGRP content was determined through logit-log analysis. This assay has a minimal detection limit of 1–3 fmol/tube. The CGRP antiserum used in these experiments binds near the C-terminal end of CGRP and does not cross- react with cholecystokinin, neuropeptide Y, or other peptides with similar C-terminal residues. The CGRP concentrations were plotted against time in 3 min intervals. Evoked release was calculated as the total amount of CGRP released (i.e., CGRP-IR) during the capsaicin infusion above the basal release of CGRP.
Statistical analysis
All data were expressed as mean ± SEM. For behavioral experiments, differences among several means relative to a single baseline group were determined with one-way ANOVA, followed by Fisher's least significant difference test. Fisher's least significant difference test is based on using ANOVA to determine a given value at which, if the difference between two means is equal to or greater than that value, the difference is significant. Differences among several treatment groups were evaluated with ANOVA followed by Student–Neuman–Keuls post hoc test. Differences between two individual means were analyzed with Student's t test. A p < 0.05 was considered significant and is indicated by an asterisk.
Results
Thermal and mechanical testing in CB1WT and KO mice
No significant differences in response latencies to three different temperatures were observed in CB1WT and CB1KO mice. Tail withdrawal latencies from water at 48°C for WT was 25.8 ± 3.1 s and KO 23.6 ± 2.6 s, from water set at 52°C for WT was 8.9 ± 1.2 s and KO 9.3 ± 1.5 s and from water set at 55°C for WT was 4.2 ± 0.2 s and KO 4.3 ± 0.5 s. Non-noxious mechanical thresholds using von Frey filaments also showed no significant differences between WT mice 1.8 ± 0.3 g and KO mice 2.0 ± 0.4 g (n = 6–8 in all experiments).
Capsaicin-induced paw flinching
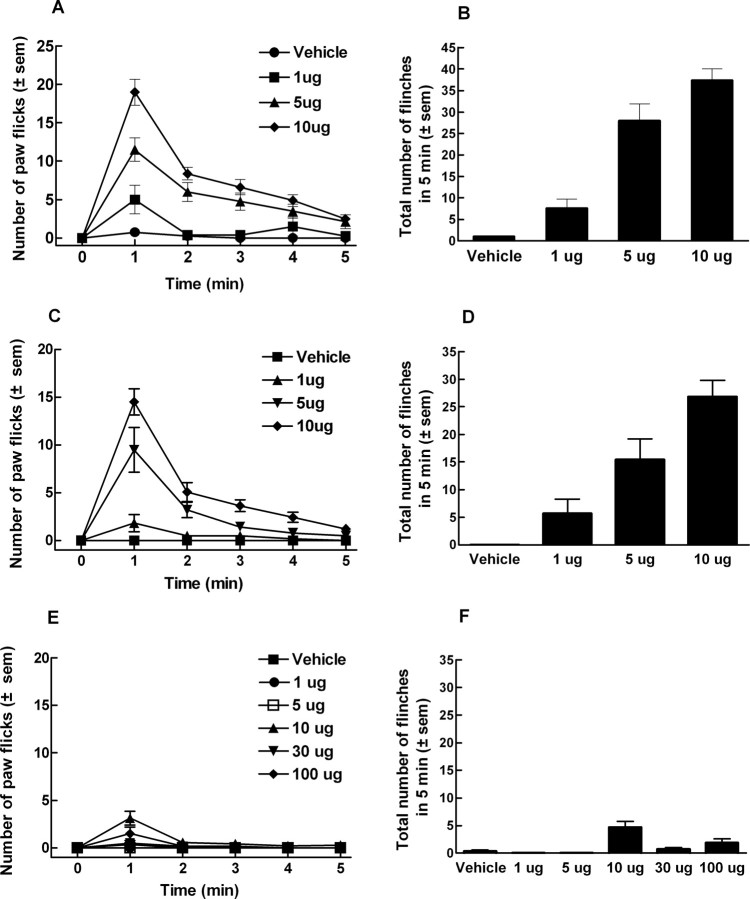
Intraplantar administration of capsaicin produced a time- and dose-related increase in flinching behaviors in ICR mice. The dose producing a 50% response (and 95% C.I.) based on the highest total flinching responses observed throughout all experiments was 2.5 (1.3–3.4) μg (Fig. 1A,B). At the 10 μg dose, the total (cumulative) number of flinches after 1, 5 and 10 min were 19.0 ± 1.7, 37.7 ± 2.8 and 44.5 ± 1.9. The time course for all subsequent capsaicin-induced paw flinch experiments was shortened to 5 min, because the majority of paw flinches occurred during this period.
Figure 1.
ICR, CB1 wild-type (CB1WT) or knock-out (CB1KO) mice received capsaicin or vehicle (100% ethanol) into the plantar surface of the left hind paw. Volume of intraplantar paw administration was 5 μl. A, Number of flinches induced by capsaicin (1, 5, or 10 μg) or vehicle in ICR mice every minute for 5 min. B, Total number of flinches evoked by capsaicin or vehicle in 5 min in ICR mice. Capsaicin induced paw flinches in a dose-dependent manner, resulting in A50 of 2.5 μg. C, Number of flinches induced by capsaicin (1, 5, or 10 μg) or vehicle in CB1WT mice every minute for 5 min. D, Total number of flinches evoked by capsaicin or vehicle in 5 min in CB1WT mice. Capsaicin induced paw flinches in a dose-dependent manner, resulting in A50 of 3.2 μg. E, Number of flinches induced by capsaicin (1, 5, 10, 30, 100 μg) or vehicle in CB1KO mice every minute for 5 min. F, Total number of flinches evoked by the different doses of capsaicin in 5 min was significantly abolished in CB1KO mice (n = 6–12 in all studies).
Systemic morphine significantly and dose-dependently inhibited capsaicin-induced paw flinching in ICR mice. Morphine pretreatment at 1 and 3 mg/kg reduced the total number of flinches to 8.7 ± 1.2 (n = 6) and 2.3 ± 0.3 (n = 6) respectively, when compared with control (vehicle administered) animals receiving capsaicin (24.9 ± 1.5, n = 12) (p < 0.001).
Capsaicin also elicited time and dose-related flinching behaviors in CB1WT mice with responses similar to those observed in ICR mice. The dose producing a 50% response (and 95% C.I.) was 3.2 (2.1–4.4) μg (Fig. 1C,D). After 5 min, the number of flinches induced by capsaicin (10 μg) in CB1WT mice was 26.9 ± 3.0. However, in CB1KO mice, capsaicin elicited significantly fewer flinching responses compared with either CB1WT or ICR control mice. Even when substantially higher doses were administered to CB1KO mice, very few flinches were observed, such that a 50% response could not be calculated (Fig. 1E,F). The total number of flinches after capsaicin at 10 or 100 μg in CB1KO mice were 4.6 ± 1.1 and 1.8 ± 0.8, respectively; these responses were significantly lower than those seen in either ICR or WT mice (p < 0.001, n = 6–12 in all experiments). No responses were seen at the lowest doses of capsaicin (e.g., 1 and 5 μg) suggesting that the lack of response seen at higher doses was not due to desensitization.
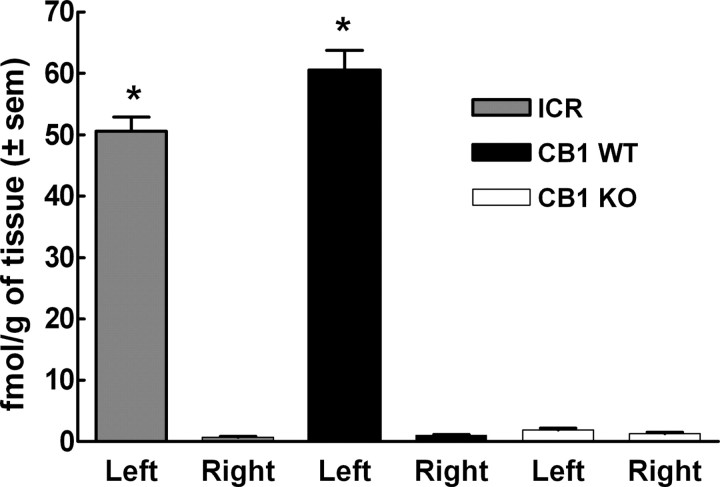
Reduced plasma extravasation is observed in CB1KO mice
Capsaicin resulted in extravasation of Evan's Blue dye after injection into the hind paw of CB1WT (60.6 ± 3.1 fmol/g tissue) or ICR mice (50.6 ± 2.3 fmol/g tissue) (Fig. 2). In contrast, tissues from CB1KO mice showed significantly decreased extravasation in the capsaicin-injected paw (1.9 ± 0.3 fmol/g tissue). In all animals, Evan's blue dye extravasation was minimal in the contralateral (noncapsaicin injected) paw (p < 0.005, n = 5–10 in all studies) (Fig. 2).
Figure 2.
ICR, CB1WT and CB1KO mice received an intraplantar (left paw) injection of capsaicin (10 μg). Intravenous (tail vein) injection of Evan's blue dye (100 mg/kg) was performed 15 min after capsaicin administration. Vehicle for capsaicin (100% ethanol) was injected into the contralateral paw (right paw). Pronounced plasma extravasation expressed as fmol/g tissue was seen in the capsaicin-injected left paw of ICR and CB1WT mice, as opposed to CB1KO, in which no capsaicin evoked plasma extravasation was detected (*p < 0.005, n = 5–10).
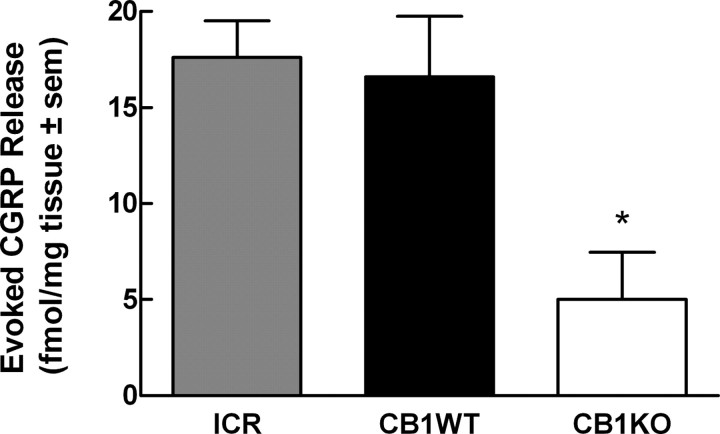
Reduced capsaicin-evoked release of i-CGRP in dorsal spinal cord of CB1KO mice
Baseline levels of CGRP in ICR and CB1WT just before capsaicin administration were 10.3 ± 1.7 and 9.1 ± 1.1 fmol/mg tissue, respectively. Similarly, baseline levels of CGRP in spinal cord tissue from CB1KO mice before capsaicin administration were 6.0 ± 0.2 fmol/mg tissue; these values were not significantly different from those of the ICR or WT tissues. Application of capsaicin (1 μm) for 6 min evoked CGRP release in spinal cord tissue from ICR and CB1WT mice. Capsaicin-evoked CGRP release was significantly reduced in spinal cord tissue from CB1KO mice. Evoked CGRP release was calculated as 17.6 ± 1.9, 16.6 ± 3.1 and 5.0 ± 2.5, fmol/mg in ICR, WT and KO tissues, respectively (p < 0.05, n = 6 in all groups) (Fig. 3).
Figure 3.
Calcitonin gene related peptide (CGRP) was measured from the lumbar spinal cord tissue of ICR, CB1WT, and CB1KO mice. After a 45 min equilibration period in the perfusion chambers, followed by a 12 min collection of perfusate for determination of baseline values, capsaicin (1 μm) was added to the perfusion medium. CGRP content was quantified by radioimmunoassay. Evoked release was defined as the amount of CGRP above the basal values. Capsaicin-evoked CGRP release from spinal cord tissue of ICR and CB1WT mice was significantly higher when compared with spinal cord tissue from CB1KO mice (*p < 0.05, n = 6 in all groups).
Capsaicin-evoked responses are reduced in C-fibers from CB1KO mice
Capsaicin-sensitivity of single cutaneous C-fibers was evaluated in skin-nerve preparations from CB1KO and CB1WT mice. Whereas nearly 60% (16 of 27) of C fibers from CB1WT mice responded to 100 μm capsaicin, only 37% (12 of 32) (1-tailed t test p = 0.07) of C-fibers from CB1KO mice responded to capsaicin with 3 or more action potentials during the capsaicin application. More importantly, the number of capsaicin-evoked action potentials in C-fibers from CB1KO mice (14.6 ± 4.3 spikes/min) was ∼50% less than that in WT mice (25.2 ± 5.6 spikes/min; 1-tailed t test, p = 0.05). There were no differences between the genotypes in C-fiber conduction velocity (WT: 0.57 ± 0.04 m/s; KO: 0.57 ± 0.03 m/s) or von Frey thresholds (WT: median 6.8 mN, lower and upper quartiles 4.0, 11.7 mN; KO: median 9.25 mN, lower and upper quartiles 5.4 mN, 12.8 mN).
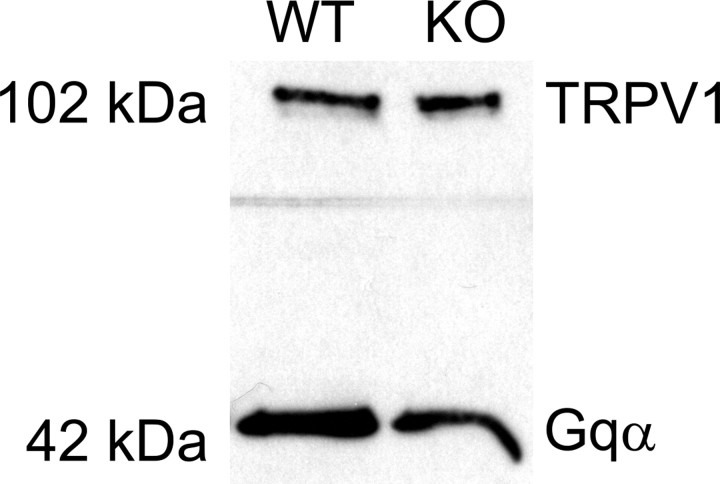
TRPV1 receptors are expressed in DRG of CB1WT and CB1KO mice
The presence of TRPV1 protein in tissues from CB1WT and KO mice was evaluated via Western blot analysis. TRPV1 protein was present in DRG of both CB1WT and CB1KO mice with a molecular weight of ∼95 kDa (Fig. 4). Gqα was used as an internal loading control for membrane proteins. Although Western blots were not performed for quantitative purposes, Gqα bands with a molecular weight of 42 kDa, were identified in both genotypes. Figure 4 is representative of three separate Western blots using DRGs from CB1WT and CB1KO mice.
Figure 4.
Western blot for TRPV1 protein (95 kDa; the figure shows 102 kDa) was performed using lumbar spinal cord tissue or dorsal root ganglia (DRG) from either CB1WT or CB1KO mice. Gqα bands with the molecular weight of 42 kDa were identified and used as an internal loading control for membrane proteins. Image represents a total of three separate Western blots using DRGs from CB1WT and CB1KO mice.
Pretreatment with galanin or bradykinin restores capsaicin-induced flinching in CB1KO mice
Intraplantar galanin (0.1 ng), a peptide known to sensitize TRPV1 channels, followed by intraplantar vehicle did not result in significant flinching responses in ICR, WT or KO mice. Intraplantar galanin followed by capsaicin challenge in ICR and WT mice resulted in an increase in the total number of flinches. In ICR and CB1WT mice, capsaicin elicited 31.6 ± 1.6 and 21.8 ± 2.2 flinches, whereas in CB1KO mice, capsaicin only evoked 3.9 ± 1.4 flinches. Pretreatment with galanin resulted in 40.8 ± 3.2 and 28.9 ± 1.6 flinches in ICR and CB1WT mice, respectively, values which were significantly higher than in the vehicle pretreated group (p < 0.05). More strikingly, in CB1KO mice, galanin pretreatment markedly enhanced capsaicin-evoked flinching from 3.9 ± 1.4 to 33.7 ± 3.1 (p < 0.001). The capsaicin response of galanin pretreated CB1KO mice was not different from that observed in galanin-pretreated ICR or WT mice (Fig. 5A).
Figure 5.
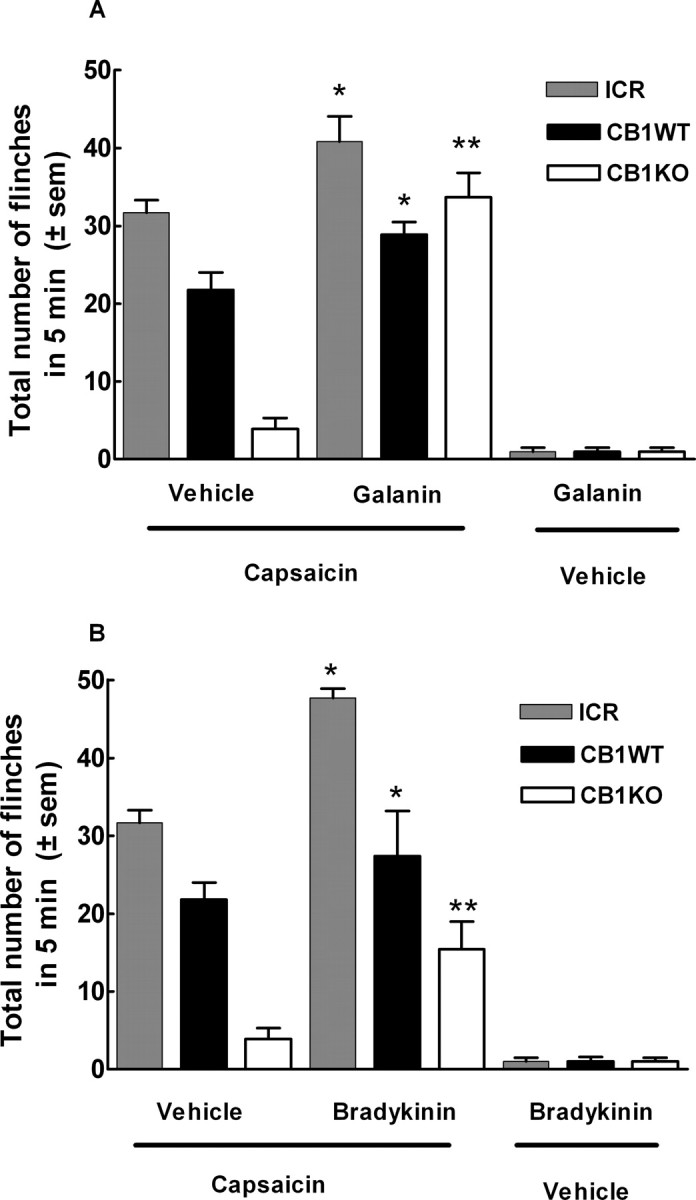
Compounds known to sensitize the TRPV1 channel restore flinching in CB1KO mice. A, ICR, CB1WT and CB1KO mice were administered galanin (0.1 ng) in the ventral side of the left hind paw followed by capsaicin (10 μg) administered in the same paw. In ICR and CB1WT mice, the total number of capsaicin-induced flinches in 5 min was increased in the presence of galanin, when compared with vehicle pretreated animals. Surprisingly, in CB1KO mice, galanin completely restored the capsaicin-evoked response, (*p < 0.05; **p < 0.001, n = 6–10). B, ICR, CB1WT and CB1KO mice were administered bradykinin (3 μg) in the ventral side of the left hind paw 10 min before intraplantar capsaicin (10 μg) administration in the same paw. In ICR and CB1WT mice, the total number of capsaicin-induced flinches in 5 min was increased in the presence of bradykinin, when compared with vehicle pretreated animals. CB1KO mice pretreated with bradykinin resulted in a significant increase in the capsaicin-evoked flinching behavior (*p < 0.05; **p < 0.05, n = 8–10).
Intraplantar bradykinin (3 μg) alone induced a total of 1.0 ± 0.5 and 1.0 ± 0.6 flinches in KO and WT mice, respectively, in the first 5 min; intraplantar saline did not elicit flinching behaviors (data not shown). After 10 min, no remaining bradykinin-induced flinching behaviors were observed. At this time point, animals were challenged with intraplantar capsaicin or vehicle and flinching behaviors were recorded. Bradykinin pretreatment in ICR mice enhanced capsaicin-evoked flinching from 31.6 ± 1.6 to 47.7 ± 1.2. Likewise, bradykinin pretreatment enhanced capsaicin-evoked flinches in WT mice from 21.8 ± 2.2–27.4 ± 5.8. Pretreatment with intraplantar vehicle or bradykinin in KO mice significantly increased the flinching response from 3.9 ± 1.4 to 15.4 ± 3.6 flinches (p < 0.05) (Fig. 5B). The enhancement of capsaicin-evoked flinching by bradykinin pretreatment in KO mice remained significantly lower than the response seen in WT or ICR mice.
CB1 inverse agonists inhibit capsaicin-evoked Ca2+ influx in F-11 cells
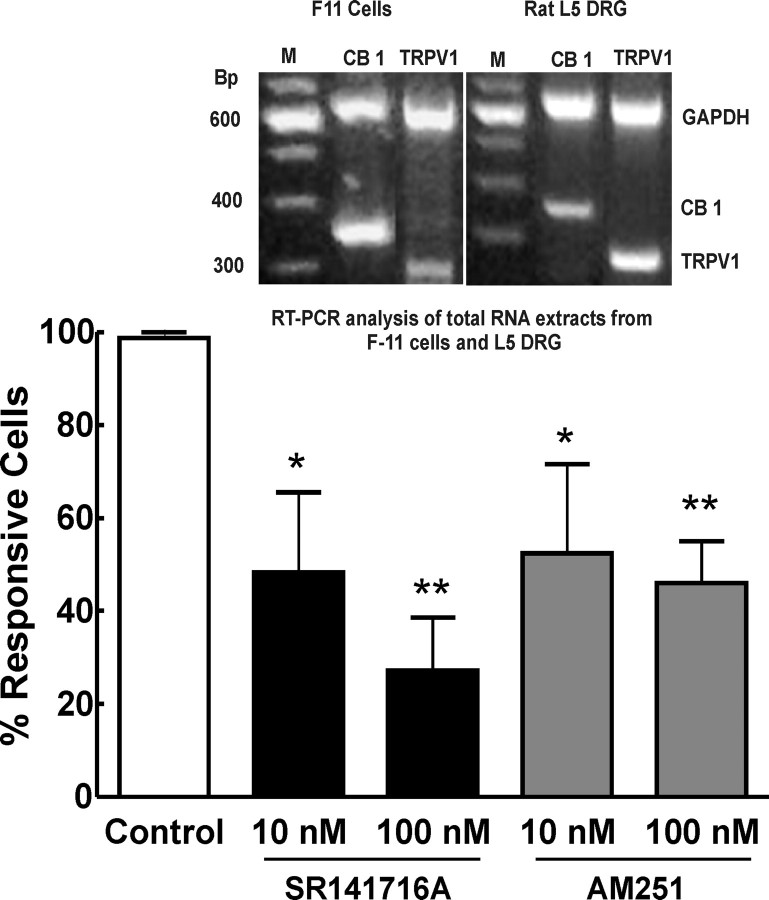
F11 cells were used to characterize the effects of CB1 inverse agonists on TRPV1 channels. The presence of CB1 and TRPV1 receptors were demonstrated by multiplex reverse transcription (RT)-PCR analysis of total RNA extracts from F-11 cells and L5 DRG of male Sprague Dawley rats. The 2% agarose gel electrophoresis displays PCR products demonstrating both CB1 (352 bp product) and TRPV1 (281 bp product) expression in F-11 cells, as well as in rat DRG. GAPDH (638 bp product) as an internal control represented equal total RNA materials for amplification. A 100 bp DNA ladder was used (Fig. 6, inset).
Figure 6.
Capsaicin (10 nm)-induced transient [Ca2+] influx in F-11 cells was performed in the presence and absence of the CB1 inverse agonists SR141716A or AM251. Capsaicin-induced calcium influx in the F11 cells was significantly blocked in a concentration-dependent manner by either SR141716A (n = 29 at 10 nm and n = 89 at 100 nm) or AM251 (n = 35 at 10 nm and n = 86 at 100 nm) (*p < 0.05, **p < 0.001). RT-PCR was performed using Sprague Dawley rat L5 DRG or the mouse neuroblastoma rat DRG hybrid F11 cell line (inset). A 2% agarose gel electrophoresis of multiplex PCR products demonstrating both CB1 (352 bp product) and TRPV1 (281 bp product) expression in F-11 cells as well as in rat DRG. GAPDH (638 bp product) as an internal control represented equal total RNA materials for amplification. Inset, A 100 bp DNA ladder.
The acute application of 10 nm capsaicin resulted in a an increase in [Ca2+]i in 56% of the total recorded cells (322 of 577). When cells were challenged a second time with the same capsaicin test, 81% of capsaicin responsive cells were desensitized (n = 172 of 212). In contrast, allowing cells to recover for 5 min after the first capsaicin application resulted in desensitization of only 3% of capsaicin-responsive cells (n = 1 of 33) (Fig. 6, control group). Therefore, experiments were performed using this protocol to assure capsaicin sensitive cells yet exclude the factor of capsaicin/TRPV1 desensitization. As a control to assure activity via the TRPV1 channel, effects of capsaicin on transient [Ca2+] influx were suppressed after incubation of the cells with capsazepine. Preincubation, 10 min, with capsazepine at 100 nm or 1 μm decreased the number of capsaicin-responsive cells by 82% (n = 42) or 93% (n = 42), respectively. SR141716A or AM251 (10 or 100 nm) significantly inhibited capsaicin-evoked transient [Ca2+] influx in F11 cells (Fig. 6). In the presence of 10 and 100 nm SR141716A, number of capsaicin responsive cells was decreased by 45% and 79%, respectively. Similar results were seen with AM251 at 10 and 100 nm; the number of capsaicin responsive cells was decreased by 37 and 61%, respectively (Fig. 6).
CB1 inverse agonists suppress capsaicin-induced flinching in ICR mice
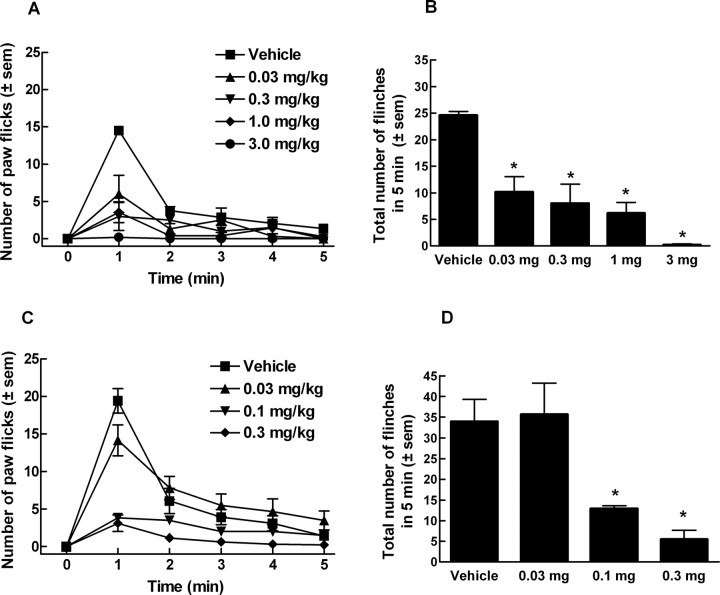
Intraperitoneal pretreatment with SR141617A (0.03–3 mg/kg) significantly suppressed intraplantar capsaicin-induced flinching in ICR mice. Intraplantar capsaicin elicited 24.6 ± 0.8 flinches in vehicle pretreated animals and 10.2 ± 2.9, 8.0 ± 3.6, 6.1 ± 2.0, and 0.2 ± 0.2 flinches after pretreatment with doses of 0.03, 0.3, 1.0 and 3 mg/kg SR171416A, respectively (Fig. 7A,B). In the same manner, preadministration of AM251 significantly decreased total capsaicin-induced flinching at the doses of 0.1 and 0.3 mg/kg resulting in 12.8 ± 0.8 and 5.5 ± 2.2 flinches, respectively (Fig. 7C,D).
Figure 7.
ICR mice received CB1 inverse agonist, SR141716A, or vehicle (PEG 400) intraperitoneally 15 min before intraplantar capsaicin. A, Number of flinches induced by capsaicin (10 μg) every minute for 5 min in the presence of SR141716A (0.03, 0.3, 1.0, and 3 mg/kg). B, Total number of flinches in the presence of SR141716A. C, Number of flinches induced by capsaicin (10 μg) every minute for 5 min in the presence of AM251 (0.03, 0.1, 0.3 mg/kg). D, Total number of capsaicin-induced flinches in the presence of AM251. (*p < 0.05, n = 6 in all groups).
Suppression of capsaicin-induced flinching by U73122, a PLC inhibitor
Pretreatment with U73122 (Hou et al., 2004) significantly attenuated capsaicin-induced flinching in ICR mice. Vehicle treated mice showed 51.6 ± 4.5 flinches. U73122 given at 10 and 30 mg/kg, resulted in 39.0 ± 4.8 and 26.3 ± 3.4 flinches, respectively indicating a 29 and 49% decrease in capsaicin-induced flinching (p < 0.001) (Fig. 8A).
Figure 8.
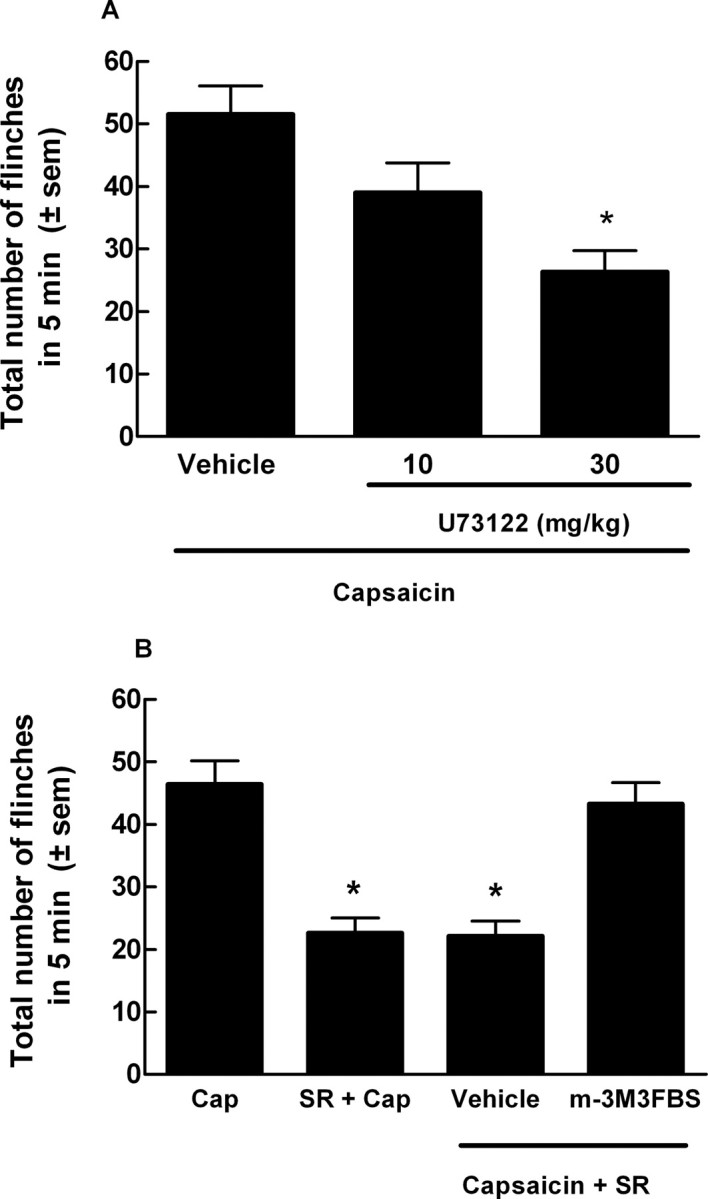
Compounds that modulate PLC, the enzyme responsible for PIP2 breakdown, affect capsaicin-induced flinching. A, ICR mice were pretreated with U73122 (10 or 30 mg/kg, i.p.), a PLC inhibitor, intraperitoneally 1 h before intraplantar injection of capsaicin (10 μg). U73122 produced a 29% (10 mg/kg) and 49% (30 mg/kg) blockade of total number of capsaicin-evoked flinches, when compared with vehicle pretreated mice (*p < 0.001, n = 10). B, m-3M3FBS (5 mg/kg, i.p.), a PLC activator, was given 30 min before intraperitoneal administration of SR141716A (SR, 0.3 mg/kg). SR141716A was given 15 min before capsaicin (Cap) injection. The total number of capsaicin-induced flinches in 5 min was significantly inhibited by pretreatment with SR141716A (*p < 0.05), yet restored by pretreatment with m-3M3FBS but not by vehicle (n = 10–14). m-3M3FBS alone did not enhance capsaicin-induced flinching and had no effect on vehicle (data not shown).
Blockade of SR141716A-induced antinociception by m-3M3FBS, a PLC activator
When administered alone, m-3M3FBS (5 mg/kg) (Bae et al., 2003) did not alter responses to intraplantar vehicle (4.3 ± 0.4 flinches) or alter capsaicin-induced flinching (42.0 ± 5.1 flinches). However, pretreatment with m-3M3FBS (5 mg/kg) 30 min before i.p. SR141716A (0.3 mg/kg) and 45 min before intraplantar capsaicin injection blocked the antinociceptive effects of the CB1 inverse agonist in ICR mice. The total number of capsaicin-induced flinches (46.4 ± 3.7) was significantly inhibited by pretreatment with SR141716A (22.6 ± 2.4), but restored by the PLC activator m-3M3FBS (43.3 ± 3.4 flinches) (Fig. 8B). Pretreatment with vehicle did not restore capsaicin-induced flinching (22.1 ± 2.4) in animals treated with SR141716A.
Discussion
Findings presented here support the idea that tonic activity of the CB1 receptor maintains the TRPV1 channel in a “sensitized” state through a PLC-dependent process. Our studies have shown that inhibition of CB1 function either through genetic deletion of the receptor or by activity of inverse agonists results in diminished reactions to capsaicin. In CB1KO mice, diminished capsaicin-induced responses included flinching behaviors, neurogenic inflammation, generation of action potentials, and evoked release of CGRP in spinal cord tissue.
Although CB1KO mice demonstrated decreased responses to a chemical activator of the TRPV1 channel, their responses to three different noxious temperatures were not different from those in ICR and CB1WT. These findings are consistent with previous reports (Zimmer et al., 1999; Bölcskei et al., 2005) and may reflect the contributions of other heat-sensitive channels (Güler et al., 2002). Unlike heat, capsaicin is selective for the TRPV1 channel (Caterina and Julius, 2001). One explanation for such loss of capsaicin activity in the CB1KO mice is that genetic deletion of the CB1 receptor alters the expression of the TRPV1 channel. However, our findings indicate that the expression of TRPV1 was similar in tissues from WT and KO mice.
Since the discovery that the CB1 agonist anandamide (AEA) could also activate TRPV1 (Zygmunt et al., 1999; Smart et al., 2000), a barrage of investigations has focused on the relationship between these receptors, particularly in C-fibers, in which activation of TRPV1 and CB1 receptor lead to nociceptive and antinociceptive effects respectively (for reviews, see Morisset et al., 2001; Ross, 2003; Immke and Gavva, 2006). Although CB1 activation typically exerts inhibitory effects over neurons expressing TRPV1, Hermann and colleagues (2003) were the first to report that CB1 activation could sensitize TRPV1 through PI-3-K or PLC pathways in the absence of activated cAMP cascade in HEK-293 cells. Evans et al. (2007) also observed CB1 receptor-mediated TRPV1 sensitization in DRG neurons cultured in high NGF concentration. In addition to sensory neurons, CB1-TRPV1 crosstalk has been demonstrated in central dopaminergic neurons in which extended opening of the TRPV1 channels resulted in cell death via either TRPV1 or indirectly via CB1 receptors (Kim et al., 2005, 2008). Consistent with the requirement for their close anatomical localization to enable a functional crosstalk, many studies reported a high level of coexpression of CB1 and TRPV1 in DRG (Ahluwalia et al., 2000; Mitrirattanakul et al., 2006) and CNS (Cristino et al., 2006) neurons.
The CB1 receptor has been well established as having constitutive activity both in in vitro and in vivo (Gifford and Ashby, 1996; Zhou and Shearman, 2004). Costa and colleagues (2005) demonstrated that SR141716A (Rimonabant) relieved hypersensitivities in a rat model of sciatic nerve constriction. In clinical studies, Rimonabant has resulted in weight loss, reduction in low-density lipoproteins, and decrease in craving of cigarette smoking suggesting a significant tonic activation of CB1 receptors (Després et al., 2005; Huestis et al., 2007). Such tonic activity maintains an endogenous intracellular level of second messengers that can be altered by inverse agonism. Therefore, to confirm our findings in CB1KO mice, we used two different CB1 inverse agonists to attenuate the constitutive activity of the CB1 receptor and measured capsaicin's ability to provoke an effect via the TRPV1 channel.
Using F-11 cells containing functional CB1 and TRPV1 receptors we demonstrated that application of CB1 inverse agonists blocked capsaicin-induced calcium influx in a concentration-dependent manner. Although it has been reported that SR141716A may act directly at the TRPV1 channel in concentrations >1 μm (De Petrocellis et al., 2001; Gibson et al., 2008), our in vitro studies used SR141716A at concentrations 10- to 100-fold lower, suggesting that this ligand is acting selectively at CB1 receptors. A similar blockade of capsaicin-induced calcium influx was observed with AM251, a different selective CB1 inverse agonist, which has not been shown to bind to TRPV1 channels. Together, our in vitro data combined with the blockade of capsaicin-induced flinching produced by SR141716A and AM251 in ICR mice confirm our findings in CB1KO, and support the idea that suppression of CB1 receptor constitutive activity leads to decreased TRPV1 sensitivity to capsaicin.
Although several studies reported CB1 receptor precoupling to G-proteins in heterologous systems (Bouaboula et al., 1997; Pan et al., 1998) and cultured neurons (Meschler et al., 2000; Leterrier et al., 2006), in our studies we cannot exclude the role of endogenous agonists in the tonic activation of CB1 receptors. In agreement with an endocannabinoid-dependent CB1 sensitization of TRPV1 channel, HU-210 sensitized TRPV1 to capsaicin in HEK-293 cells coexpressing CB1 and TRPV1 (Hermann et al., 2003). Furthermore, in this study the authors observed an enhanced AEA-induced TRPV1-mediated Ca+2 influx, supporting a possible CB1 receptor-mediated sensitization of TRPV1. In contrast to our findings, SR141716 (0.5 μm) showed no effect on capsaicin-induced response (Hermann et al., 2003) suggesting a lack of CB1 receptor constitutive activity. However, it is likely that in F-11 cells and in vivo the level of endocannabinoids (Pertwee, 2005) and/or the coupling machinery is different from what is present in transfected human embryonic kidney cells. What we do not know is the precise optimal level of endocannabinoids and the ratio of CB1 agonist to CB1 receptor as well as to G-protein(s) necessary to induce tonic activation.
The possibility of altering the response to capsaicin stimulation in CB1KO mice through the actions of GPCRs that are known to modulate the responsiveness of the TRPV1 channel was explored with galanin and bradykinin, which act through Gαq-coupling to activate PLC, leading to PKC-mediated phosphorylation of TRPV1 and thus increased responses to capsaicin (Cesare and McNaughton, 1996; Chuang et al., 2001; Jimenez-Andrade et al., 2004). Galanin or bradykinin, when preadministered at low doses to CB1KO mice, restored capsaicin responses in CB1KO mice to levels similar to those observed with capsaicin alone in WT mice. These findings suggest that the TRPV1 channel is present in a desensitized state in CB1KO mice, and when known sensitizing compounds are preadministered, re-sensitization of the TRPV1 channel to capsaicin takes place.
Although the CB1 receptor has traditionally been classified as a Gαi/o-protein coupled receptor (Bayewitch et al., 1995) studies have also demonstrated CB1 receptor coupling to Gαq and PLC (Ho et al., 1999, 2002; Lauckner et al., 2005; De Petrocellis et al., 2007) and β-gamma portions of G-proteins that activate PLC isoforms (Liu and Simon, 1996; Huang et al., 1998), indicating that activation of CB1 receptors can result in a decrease in PIP2 and an increase in PKC and Ca+2-induced kinases, intracellular activities that sensitize TRPV1 channels to capsaicin (Vellani et al., 2001; Rathee et al., 2002; Bhave et al., 2003; Jung et al., 2004).
To further explore a potential PLC-mediated mechanism, we have demonstrated that the preadministration of the PLC inhibitor U73122 significantly reduces behavioral responses to capsaicin in ICR mice similar to levels seen in CB1KO mice or in animals pretreated with SR141716A. More interestingly, the significant reduction of capsaicin-induced flinching by the CB1 inverse agonist SR141716A was attenuated by the preadministration of the PLC activator m-3M3FBS. Furthermore, increases in cAMP/PKA, which occur in the presence of the inverse agonist SR141716A, result in the inhibition of PLC activity (Wen et al., 1992; Liu and Simon, 1996). Together with the effects of bradykinin and galanin in CB1KO mice, these findings point to PLC as a link in this CB1-TRPV1 crosstalk, a hypothesis supported by several studies (Premkumar and Ahern, 2000; Hermann et al., 2003; van der Stelt et al., 2005; Vellani et al., 2008).
Recent reports further implicate PLC- and PKC-mediated mechanisms in the biosynthesis of AEA (van der Stelt et al., 2005; Liu et al., 2006; Vellani et al., 2008), resulting in additional pathways for production of endovanilloids. Thus modulation of the aforementioned enzymes may alter TRPV1 function also due to changes in levels of AEA, which activate and sensitize this channel (Premkumar and Ahern, 2000). Finally, we propose that tonic CB1 receptor function activates PLC which 1) releases TRPV1 from PIP2 inhibition, 2) promotes PKC-mediated sensitization of TRPV1 and 3) stimulates synthesis of AEA, which activate and sensitize TRPV1 channels.
The recent development of TRPV1 antagonists for acute and inflammatory pain have resulted in some unwanted side effects including increasing body temperature (Gavva et al., 2007) and some uncertainty in such antagonists for drug development, yet a very recent study by the same group reported TRPV1 antagonists that may or may not result in hyperthermia in humans (Lehto et al., 2008). Although TRPV1 is a promiscuous channel with multiple intracellular messengers and surface receptors modulating its function, such complimentary pathways may lead to novel pharmaceutical targets. The endogenous cannabinoid system may be one such pathway that when attenuated may result in the inhibition of some types of inflammatory pain. Thus far the CB1 receptor has demonstrated a propensity to be constitutively activated or tonically activated by endocannabinoids and is plausible as a receptor that maintains an intracellular environment resulting in a capsaicin-sensitized TRPV1 channel. These studies support an antihyperalgesic role for CB1 inverse agonists in conditions of inflammatory pain in which TRPV1 receptors have been shown to promote hypersensitivity and suggest that strategies to indirectly modulate TRPV1-function warrant increased exploration.
Footnotes
We thank Wenjun-Jack Zhang and Rachel Johnson for their technical assistance. Dr. Henry I. Yamamura, a Regent's Professor in Pharmacology and Neurosciences at the University of Arizona, passed away on September 4th, 2008. He will be dearly missed by his colleagues, friends, and the international neuroscience community.
References
- Ahluwalia J, Urban L, Capogna M, Bevan S, Nagy I. Cannabinoid 1 receptors are expressed in nociceptive primary sensory neurons. Neuroscience. 2000;100:685–688. doi: 10.1016/s0306-4522(00)00389-4. [DOI] [PubMed] [Google Scholar]
- Ahluwalia J, Urban L, Bevan S, Capogna M, Nagy I. Cannabinoid 1 receptors are expressed by nerve growth factor- and glial cell-derived neurotrophic factor-responsive primary sensory neurones. Neuroscience. 2002;110:747–753. doi: 10.1016/s0306-4522(01)00601-7. [DOI] [PubMed] [Google Scholar]
- Ahluwalia J, Urban L, Bevan S, Nagy I. Anandamide regulates neuropeptide release from capsaicin-sensitive primary sensory neurons by activating both the cannabinoid 1 receptor and the vanilloid receptor 1 in vitro. Eur J Neurosci. 2003;17:2611–2618. doi: 10.1046/j.1460-9568.2003.02703.x. [DOI] [PubMed] [Google Scholar]
- Bae YS, Lee TG, Park JC, Hur JH, Kim Y, Heo K, Kwak JY, Suh PG, Ryu SH. Identification of a compound that directly stimulates phospholipase C activity. Mol Pharmacol. 2003;63:1043–1050. doi: 10.1124/mol.63.5.1043. [DOI] [PubMed] [Google Scholar]
- Bayewitch M, Avidor-Reiss T, Levy R, Barg J, Mechoulam R, Vogel Z. The peripheral cannabinoid receptor: adenylate cyclase inhibition and G protein coupling. FEBS Lett. 1995;375:143–147. doi: 10.1016/0014-5793(95)01207-u. [DOI] [PubMed] [Google Scholar]
- Bhave G, Zhu W, Wang H, Brasier DJ, Oxford GS, Gereau RW., 4th cAMP-dependent protein kinase regulates desensitization of the capsaicin receptor (VR1) by direct phosphorylation. Neuron. 2002;35:721–731. doi: 10.1016/s0896-6273(02)00802-4. [DOI] [PubMed] [Google Scholar]
- Bhave G, Hu HJ, Glauner KS, Zhu W, Wang H, Brasier DJ, Oxford GS, Gereau RW., 4th Protein kinase C phosphorylation sensitizes but does not activate the capsaicin receptor transient receptor potential vanilloid 1 (TRPV1) Proc Natl Acad Sci U S A. 2003;100:12480–12485. doi: 10.1073/pnas.2032100100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilsky EJ, Bernstein RN, Hruby VJ, Rothman RB, Lai J, Porreca F. Characterization of antinociception to opioid receptor selective agonists after antisense oligodeoxynucleotide-mediated “knock-down” of opioid receptor in vivo. J Pharmacol Exp Ther. 1996;277:491–501. [PubMed] [Google Scholar]
- Binzen U, Greffrath W, Hennessy S, Bausen M, Saaler-Reinhardt S, Treede RD. Co-expression of the voltage-gated potassium channel Kv1.4 with transient receptor potential channels (TRPV1 and TRPV2) and the cannabinoid receptor CB1 in rat dorsal root ganglion neurons. Neuroscience. 2006;142:527–539. doi: 10.1016/j.neuroscience.2006.06.020. [DOI] [PubMed] [Google Scholar]
- Bölcskei K, Helyes Z, Szabó A, Sándor K, Elekes K, Németh J, Almási R, Pintér E, Petho G, Szolcsányi J. Investigation of the role of TRPV1 receptors in acute and chronic nociceptive processes using gene-deficient mice. Pain. 2005;117:368–376. doi: 10.1016/j.pain.2005.06.024. [DOI] [PubMed] [Google Scholar]
- Bouaboula M, Perrachon S, Milligan L, Canat X, Rinaldi-Carmona M, Portier M, Barth F, Calandra B, Pecceu F, Lupker J, Maffrand JP, Le Fur G, Casellas P. A selective inverse agonist for central cannabinoid receptor inhibits mitogen-activated protein kinase activation stimulated by insulin or insulin-like growth factor 1. Evidence for a new model of receptor/ligand interactions. J Biol Chem. 1997;272:22330–22339. doi: 10.1074/jbc.272.35.22330. [DOI] [PubMed] [Google Scholar]
- Carlton SM, Zhou S, Du J, Hargett GL, Ji G, Coggeshall RE. Somatostatin modulates the transient receptor potential vanilloid 1 (TRPV1) ion channel. Pain. 2004;110:616–627. doi: 10.1016/j.pain.2004.04.042. [DOI] [PubMed] [Google Scholar]
- Caterina MJ, Julius D. The vanilloid receptor: a molecular gateway to the pain pathway. Annu Rev Neurosci. 2001;24:487–517. doi: 10.1146/annurev.neuro.24.1.487. [DOI] [PubMed] [Google Scholar]
- Caterina MJ, Schumacher MA, Tominaga M, Rosen TA, Levine JD, Julius D. The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature. 1997;389:816–824. doi: 10.1038/39807. [DOI] [PubMed] [Google Scholar]
- Caterina MJ, Leffler A, Malmberg AB, Martin WJ, Trafton J, Petersen-Zeitz KR, Koltzenburg M, Basbaum AI, Julius D. Impaired nociception and pain sensation in mice lacking the capsaicin receptor. Science. 2000;288:306–313. doi: 10.1126/science.288.5464.306. [DOI] [PubMed] [Google Scholar]
- Cesare P, McNaughton P. A novel heat-activated current in nociceptive neurons and its sensitization by bradykinin. Proc Natl Acad Sci U S A. 1996;93:15435–15439. doi: 10.1073/pnas.93.26.15435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang HH, Prescott ED, Kong H, Shields S, Jordt SE, Basbaum AI, Chao MV, Julius D. Bradykinin and nerve growth factor release the capsaicin receptor from PtdIns(4,5)P2-mediated inhibition. Nature. 2001;411:957–962. doi: 10.1038/35082088. [DOI] [PubMed] [Google Scholar]
- Costa B, Trovato AE, Colleoni M, Giagnoni G, Zarini E, Croci T. Effect of the cannabinoid CB1 receptor antagonist, SR141716, on nociceptive response and nerve demyelination in rodents with chronic constriction injury of the sciatic nerve. Pain. 2005;116:52–61. doi: 10.1016/j.pain.2005.03.043. [DOI] [PubMed] [Google Scholar]
- Cristino L, de Petrocellis L, Pryce G, Baker D, Guglielmotti V, Di Marzo V. Immunohistochemical localization of cannabinoid type 1 and vanilloid transient receptor potential vanilloid type 1 receptors in the mouse brain. Neuroscience. 2006;139:1405–1415. doi: 10.1016/j.neuroscience.2006.02.074. [DOI] [PubMed] [Google Scholar]
- De Petrocellis L, Bisogno T, Maccarrone M, Davis JB, Finazzi-Agro A, Di Marzo V. The activity of anandamide at vanilloid VR1 receptors requires facilitated transport across the cell membrane and is limited by intracellular metabolism. J Biol Chem. 2001;276:12856–12863. doi: 10.1074/jbc.M008555200. [DOI] [PubMed] [Google Scholar]
- De Petrocellis L, Starowicz K, Moriello AS, Vivese M, Orlando P, Di Marzo V. Regulation of transient receptor potential channels of melastatin type 8 (TRPM8): effect of cAMP, cannabinoid CB1 receptors and endovanniloids. Exp Cell Res. 2007;303:1911–1920. doi: 10.1016/j.yexcr.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Després JP, Golay A, Sjöström L. Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N Engl J Med. 2005;353:2121–2134. doi: 10.1056/NEJMoa044537. [DOI] [PubMed] [Google Scholar]
- Evans RM, Scott RH, Ross RA. Chronic exposure of sensory neurones to increased levels of nerve growth factor modulates CB1/TRPV1 receptor crosstalk. Br J Pharmacol. 2007;152:404–413. doi: 10.1038/sj.bjp.0707411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavva NR, Bannon AW, Hovland DN, Jr, Lehto SG, Klionsky L, Surapaneni S, Immke DC, Henley C, Arik L, Bak A, Davis J, Ernst N, Hever G, Kuang R, Shi L, Tamir R, Wang J, Wang W, Zajic G, Zhu D, et al. Repeated administration of vanilloid receptor TRPV1 antagonists attenuates hyperthermia elicited by TRPV1 blockade. J Pharmacol Exp Ther. 2007;323:128–137. doi: 10.1124/jpet.107.125674. [DOI] [PubMed] [Google Scholar]
- Gibson HE, Edwards JG, Page RS, Van Hook MJ, Kauer JA. TRPV1 channels mediate long-term depression at synapses on hippocampal interneurons. Neuron. 2008;57:746–759. doi: 10.1016/j.neuron.2007.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gifford AN, Ashby CR., Jr Electrically evoked acetylcholine release from hippocampal slices is inhibited by the cannabinoid receptor agonist, WIN 55212-2, and is potentiated by the cannabinoid antagonist, SR 141716A. J Pharmacol Exp Ther. 1996;277:1431–1436. [PubMed] [Google Scholar]
- Güler AD, Lee H, Iida T, Shimizu I, Tominaga M, Caterina M. Heat-evoked activation of the ion channel, TRPV4. J Neurosci. 2002;22:6408–6414. doi: 10.1523/JNEUROSCI.22-15-06408.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermann H, De Petrocellis L, Bisogno T, Schiano Moriello A, Lutz B, Di Marzo V. Dual effect of cannabinoid CB1 receptor stimulation on a vanilloid VR1 receptor-mediated response. Cell Mol Life Sci. 2003;60:607–616. doi: 10.1007/s000180300052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho BY, Uezono Y, Takada S, Takase I, Izumi F. Coupling of the expressed cannabinoid CB1 and CB2 receptors to phospholipase C and G protein-coupled inwardly rectifying K+ channels. Receptors Channels. 1999;6:363–374. [PubMed] [Google Scholar]
- Ho BY, Current L, Drewett JG. Role of intracellular loops of cannabinoid CB(1) receptor in functional interaction with G(alpha16) FEBS Lett. 2002;522:130–134. doi: 10.1016/s0014-5793(02)02917-4. [DOI] [PubMed] [Google Scholar]
- Hou C, Kirchner T, Singer M, Matheis M, Argentieri D, Cavender D. In vivo activity of a phospholipase C inhibitor, 1-(6-((17beta-3-methoxyestra-1,3,5(10)-trien-17-yl)amino)hexyl)-1H-pyrrole-2,5-dione (U73122), in acute and chronic inflammatory reactions. J Pharmacol Exp Ther. 2004;309:697–704. doi: 10.1124/jpet.103.060574. [DOI] [PubMed] [Google Scholar]
- Huang CL, Feng S, Hilgemann DW. Direct activation of inward rectifier potassium channels by PIP2 and its stabilization by Gbetagamma. Nature. 1998;391:803–806. doi: 10.1038/35882. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Boyd SJ, Heishman SJ, Preston KL, Bonnet D, Le FG, Gorelick DA. Single and multiple doses of rimonabant antagonize acute effects of smoked cannabis in male cannabis users. Psychopharmacology (Berl) 2007;194:505–515. doi: 10.1007/s00213-007-0861-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang SW, Cho H, Kwak J, Lee SY, Kang CJ, Jung J, Cho S, Min KH, Suh YG, Kim D, Oh U. Direct activation of capsaicin receptor by products of lipoxygenases: endogenous capsaicin-like substances. Proc Natl Acad Sci U S A. 2000;97:6155–6160. doi: 10.1073/pnas.97.11.6155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Immke DC, Gavva NR. The TRPV1 receptor and nociception. Semin Cell Dev Biol. 2006;17:582–591. doi: 10.1016/j.semcdb.2006.09.004. [DOI] [PubMed] [Google Scholar]
- Jeske NA, Patwardhan AM, Gamper N, Price TJ, Akopian AN, Hargreaves KM. Cannabinoid WIN 55,212–2 regulates TRPV1 phosphorylation in sensory neurons. J Biol Chem. 2006;281:32879–32890. doi: 10.1074/jbc.M603220200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez-Andrade JM, Zhou S, Du J, Yamani A, Grady JJ, Castañeda-Hernandez G, Carlton SM. Pro-nociceptive role of peripheral galanin in inflammatory pain. Pain. 2004;110:10–21. doi: 10.1016/j.pain.2004.02.032. [DOI] [PubMed] [Google Scholar]
- Jung J, Shin JS, Lee SY, Hwang SW, Koo J, Cho H, Oh U. Phosphorylation of vanilloid receptor 1 by Ca2+/calmodulin-dependent kinase II regulates its vanilloid binding. J Biol Chem. 2004;279:7048–7054. doi: 10.1074/jbc.M311448200. [DOI] [PubMed] [Google Scholar]
- Kim SR, Bok E, Chung YC, Chung ES, Jin BK. Interactions between CB(1) receptors and TRPV1 channels mediated by 12-HPETE are cytotoxic to mesencephalic dopaminergic neurons. Br J Pharmacol. 2008;155:253–264. doi: 10.1038/bjp.2008.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koplas PA, Rosenberg RL, Oxford GS. The role of calcium in the desensitization of capsaicin responses in rat dorsal root ganglion neurons. J Neurosci. 1997;17:3525–3537. doi: 10.1523/JNEUROSCI.17-10-03525.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J, Luo MC, Chen Q, Ma S, Gardell LR, Ossipov MH, Porreca F. Dynorphin A activates bradykinin receptors to maintain neuropathic pain. Nat Neurosci. 2006;9:1534–1540. doi: 10.1038/nn1804. [DOI] [PubMed] [Google Scholar]
- Lauckner JE, Hille B, Mackie K. The cannabinoid agonist WIN55,212–2 increases intracellular calcium via CB1 receptor coupling to Gq/11 G proteins. Proc Natl Acad Sci U S A. 2005;102:19144–19149. doi: 10.1073/pnas.0509588102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehto SG, Tamir R, Deng H, Klionsky L, Kuang R, Le A, Lee D, Louis JC, Magal E, Manning BH, Rubino J, Surapaneni S, Tamayo N, Wang T, Wang J, Wang J, Wang W, Youngblood B, Zhang M, Zhu D, et al. Antihyperalgesic effects of (R,E)-N-(2-hydroxy-2,3-dihydro-1H-inden-4-yl)-3-(2-(piperi-din-1-yl)-4-(trifluoromethyl)phenyl)-acrylamide (AMG8562), a novel transient receptor potential vanilloid type 1 modulator that does not cause hyperthermia in rats. J Pharmacol Exp Ther. 2008;326:218–229. doi: 10.1124/jpet.107.132233. [DOI] [PubMed] [Google Scholar]
- Leterrier C, Lainé J, Darmon M, Boudin H, Rossier J, Lenkei Z. Constitutive activation drives compartment-selective endocytosis and axonal targeting of type 1 cannabinoid receptors. J Neurosci. 2006;26:3141–3153. doi: 10.1523/JNEUROSCI.5437-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Wang L, Harvey-White J, Osei-Hyiaman D, Razdan R, Gong Q, Chan AC, Zhou Z, Huang BX, Kim HY, Kunos G. A biosynthetic pathway for anandamide. Proc Natl Acad Sci U S A. 2006;103:13345–13350. doi: 10.1073/pnas.0601832103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu M, Simon MI. Regulation by cAMP-dependent protein kinease of a G-protein-mediated phospholipase C. Nature. 1996;382:83–87. doi: 10.1038/382083a0. [DOI] [PubMed] [Google Scholar]
- Meschler JP, Kraichely DM, Wilken GH, Howlett AC. Inverse agonist properties of N-(piperidin-1-yl)-5-(4-chlorophenyl)-1-(2, 4-dichlorophenyl)-4-methyl-1H-pyrazole-3-carboxamide HCl (SR141716A) and 1-(2-chlorophenyl)-4-cyano-5-(4-methoxyphenyl)-1H-pyrazole-3-carboxyl ic acid phenylamide (CP-272871) for the CB(1) cannabinoid receptor. Biochem Pharmacol. 2000;60:1315–1323. doi: 10.1016/s0006-2952(00)00447-0. [DOI] [PubMed] [Google Scholar]
- Mitrirattanakul S, Ramakul N, Guerrero AV, Matsuka Y, Ono T, Iwase H, Mackie K, Faull KF, Spigelman I. Site-specific increases in peripheral cannabinoid receptors and their endogenous ligands in a model of neuropathic pain. Pain. 2006;126:102–114. doi: 10.1016/j.pain.2006.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohapatra DP, Nau C. Regulation of Ca2+-dependent desensitization in the vanilloid receptor TRPV1 by calcineurin and cAMP-dependent protein kinase. J Biol Chem. 2005;280:13424–13432. doi: 10.1074/jbc.M410917200. [DOI] [PubMed] [Google Scholar]
- Morisset V, Ahluwalia J, Nagy I, Urban L. Possible mechanisms of cannabinoid-induced antinociception in the spinal cord. Eur J Pharmacol. 2001;429:93–100. doi: 10.1016/s0014-2999(01)01309-7. [DOI] [PubMed] [Google Scholar]
- Pan X, Ikeda SR, Lewis DL. SR 141716A acts as an inverse agonist to increase neuronal voltage-dependent Ca2+ currents by reversal of tonic CB1 cannabinoid receptor activity. Mol Pharmacol. 1998;54:1064–1072. doi: 10.1124/mol.54.6.1064. [DOI] [PubMed] [Google Scholar]
- Patwardhan AM, Jeske NA, Price TJ, Gamper N, Akopian AN, Hargreaves KM. The cannabinoid WIN 55,212–2 inhibits transient receptor potential vanilloid 1 (TRPV1) and evokes peripheral antihyperalgesia via calcineurin. Proc Natl Acad Sci U S A. 2006;103:11393–11398. doi: 10.1073/pnas.0603861103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertwee RG. Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacol Ther. 1997;74:129–180. doi: 10.1016/s0163-7258(97)82001-3. [DOI] [PubMed] [Google Scholar]
- Pertwee RG. Inverse agonism and neutral antagonism at cannabinoid CB1 receptors. Life Sci. 2005;76:1307–1324. doi: 10.1016/j.lfs.2004.10.025. [DOI] [PubMed] [Google Scholar]
- Platika D, Boulos MH, Baizer L, Fishman MC. Neuronal traits of clonal cell lines derived by fusion of dorsal root ganglia neurons with neuroblastoma cells. Proc Natl Acad Sci U S A. 1985;82:3499–3503. doi: 10.1073/pnas.82.10.3499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Premkumar LS, Ahern GP. Induction of vanilloid receptor channel activity by protein kinase C. Nature. 2000;408:985–990. doi: 10.1038/35050121. [DOI] [PubMed] [Google Scholar]
- Price TJ, Louria MD, Candelario-Soto D, Dussor GO, Jeske NA, Patwardhan AM, Diogenes A, Trott AA, Hargreaves KM, Flores CM. Treatment of trigeminal ganglion neurons in vitro with NGF, GDNF or BDNF: effects on neuronal survival, neurochemical properties and TRPV1-mediated neuropeptide secretion. BMC Neurosci. 2005;6:4. doi: 10.1186/1471-2202-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathee PK, Distler C, Obreja O, Neuhuber W, Wang GK, Wang SY, Nau C, Kress M. PKA/AKAP/VR-1 module: a common link of Gs-mediated signaling to thermal hyperalgesia. J Neurosci. 2002;22:4740–4745. doi: 10.1523/JNEUROSCI.22-11-04740.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson JD, Kilo S, Hargreaves KM. Cannabinoids reduce hyperalgesia and inflammation via interaction with peripheral CB1 receptors. Pain. 1998a;75:111–119. doi: 10.1016/S0304-3959(97)00213-3. [DOI] [PubMed] [Google Scholar]
- Richardson JD, Aanonsen L, Hargreaves KM. Antihyperalgesic effects of spinal cannabinoids. Eur J Pharmacol. 1998b;345:145–153. doi: 10.1016/s0014-2999(97)01621-x. [DOI] [PubMed] [Google Scholar]
- Ross RA. Anandamide and vanilloid TRPV1 receptors. Br J Pharmacol. 2003;140:790–801. doi: 10.1038/sj.bjp.0705467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart D, Gunthorpe MJ, Jerman JC, Nasir S, Gray J, Muir AI, Chambers JK, Randall AD, Davis JB. The endogenous lipid anandamide is a full agonist at the human vanilloid receptor (hVR1) Br J Pharmacol. 2000;129:227–230. doi: 10.1038/sj.bjp.0703050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stucky CL, Medler KA, Molliver DC. The P2Y agonist UTP activates cutaneous afferent fibers. Pain. 2004;109:36–44. doi: 10.1016/j.pain.2004.01.007. [DOI] [PubMed] [Google Scholar]
- Tominaga M, Caterina MJ, Malmberg AB, Rosen TA, Gilbert H, Skinner K, Raumann BE, Basbaum AI, Julius D. The cloned capsaicin receptor integrates multiple pain-producing stimuli. Neuron. 1998;21:531–543. doi: 10.1016/s0896-6273(00)80564-4. [DOI] [PubMed] [Google Scholar]
- Trevisani M, Smart D, Gunthorpe MJ, Tognetto M, Barbieri M, Campi B, Amadesi S, Gray J, Jerman JC, Brough SJ, Owen D, Smith GD, Randall AD, Harrison S, Bianchi A, Davis JB, Geppetti P. Ethanol elicits and potentiates nociceptor responses via the vanilloid receptor-1. Nat Neurosci. 2002;5:546–551. doi: 10.1038/nn0602-852. [DOI] [PubMed] [Google Scholar]
- van der Stelt M, Trevisani M, Vellani V, De Petrocellis L, Schiano Moriello A, Campi B, McNaughton P, Geppetti P, Di Marzo V. Anandamide acts as an intracellular messenger amplifying Ca2+ influx via TRPV1 channels. EMBO J. 2005;24:3026–3037. doi: 10.1038/sj.emboj.7600784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vellani V, Mapplebeck S, Moriondo A, Davis JB, McNaughton PA. Protein kinase C activation potentiates gating of the vanilloid receptor VR1 by capsaicin, protons, heat and anandamide. J Physiol. 2001;534:813–825. doi: 10.1111/j.1469-7793.2001.00813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vellani V, Petrosino S, De Petrocellis L, Valenti M, Prandini M, Magherini PC, McNaughton PA, Di Marzo V. Functional lipidomics. Calcium-independent activation of endocannabinoid/endovanilloid lipid signalling in sensory neurons by protein kinases C and A and thrombin. Neuropharmacology. 2008 doi: 10.1016/j.neuropharm.2008.01.010. in press. [DOI] [PubMed] [Google Scholar]
- Wen Y, Anwer K, Singh SP, Sanborn BM. Protein kinase-A inhibits phospholipase-C activity and alters protein phosphorylation in rat myometrial plasma membranes. Endocrinology. 1992;131:1377–1382. doi: 10.1210/endo.131.3.1324160. [DOI] [PubMed] [Google Scholar]
- Zhou D, Shearman LP. Voluntary exercise augments acute effects of CB1-receptor inverse agonist on body weight loss in obese and lean mice. Pharmacol Biochem Behav. 2004;77:117–125. doi: 10.1016/j.pbb.2003.10.015. [DOI] [PubMed] [Google Scholar]
- Zimmer A, Zimmer AM, Hohmann AG, Herkenham M, Bonner TI. Increased mortality, hypoactivity, and hypoalgesia in cannabinoid CB1 receptor knockout mice. Proc Natl Acad Sci U S A. 1999;96:5780–5785. doi: 10.1073/pnas.96.10.5780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zygmunt PM, Petersson J, Andersson DA, Chuang H, Sørgård M, Di Marzo V, Julius D, Högestätt ED. Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide. Nature. 1999;400:452–457. doi: 10.1038/22761. [DOI] [PubMed] [Google Scholar]