Abstract
The purpose of this review is to illustrate the utility and value of employing human self-administration procedures in medication development, including abuse liability assessments of novel medications and evaluation of potential pharmacotherapies for substance use disorders. Traditionally, human abuse liability testing has relied primarily on subjective reports describing drug action by use of questionnaires; similarly, drug interactions between putative treatment agents and the drugs of abuse have relied on these measures. Subjective reports are highly valued because they provide qualitative and quantitative information about the characteristics of central and peripheral pharmacodynamic effects as well as safety and tolerability. However, self-administration procedures directly examine the behavior of interest – that is, drug taking. The present paper 1) reviews the most commonly used human self-administration procedures, 2) discusses the concordance of subjective reports and self-administration within the context of medications development for substance use disorders, focusing primarily on illustrative examples from development efforts with opioid and cocaine dependence, and 3) explores the utility of applying self-administration procedures to assess the abuse liability of novel compounds, including “abuse deterrent” formulations (ADFs). The review will focus on opioid and cocaine dependence because a rich database from both clinical laboratory and clinical trial research exists for these two drug classes. The data reviewed suggest that drug-induced changes in self-administration and subjective effects are not always concordant. Therefore, assessment of self-administration in combination with subjective effects provides a more comprehensive picture that may have improved predictive validity for translating to the clinical setting.
1.0 Introduction
Recent epidemiological data reveal that opioid and cocaine dependence is an important area of public health concern (SAMHSA, 2007a; World Health Report, 2005). For example, the number of current heroin users in the U.S. more than doubled from 136,000 individuals in 2005 to 338,000 individuals in 2006. Please note that these values were obtained only from those individuals residing in households and therefore are likely to be lower than the true incidence of current heroin users. Of equal or greater concern is the increasing number of users of prescription pain relievers for non-medical reasons (Comer and Ashworth, In press; Zacny et al., 2003). An estimated 5.2 million people were currently using prescription pain relievers for non-medical purposes in 2006, which was an increase from 4.7 million users in 2005, and 2.6 million users in 1999. Incidence rates for new initiation of illicit drug use also appear to be the highest for prescription pain relievers compared to all illicit drugs, including marijuana, with approximately 2.2 million new initiates among individuals aged 12 and older in 2006 (SAMHSA, 2007a). Correspondingly, data from the Drug Abuse Warning Network (DAWN, 2005) reveal that there were a total of 108 million emergency department visits, approximately 1.4 million of which were associated with drug misuse or abuse. Of these, heroin was involved in approximately 11% of visits and non-medical use of prescription opioids was involved in approximately 33% of visits. With regard to drug-related deaths, in 91% of the geographical areas studied, more drug misuse deaths involved an opioid than any other drug. Although the rates of past month cocaine use remained relatively stable in the U.S. between 2002 and 2006 (NSDUH, 2006), cocaine was involved in close to one in three drug misuse/abuse emergency department visits (31%; DAWN, 2005). Worldwide, approximately 16 million people abuse opiates and 14 million people use cocaine (World Drug Report, 2005). Thus, it is clear that the treatment of opioid and cocaine dependence continues to be an area requiring a great deal of attention.
In addition to prevention efforts, drug dependence can be reduced either by developing new medications with limited abuse liability or by developing new more effective pharmacotherapies. Assessment of the abuse liability of new compounds is an important component in the drug development process. The likelihood of abuse is initially assessed by examination of the chemical structure of the new compound compared to known drugs of abuse, the in vitro receptor pharmacology of the compound, and the results of behavioral studies conducted in laboratory animals. The latter studies often employ drug discrimination and drug self-administration paradigms in order to determine the likelihood of abuse (Ator and Griffiths, 2003). The next major component in the assessment of the abuse liability of a new medication is studies conducted in human research volunteers who are experienced with the effects of the drugs in the same pharmacological class as the test compound and who have used the drugs for non-medical purposes. The choice of this subject population is predicated on the belief that it is this group that will most likely misuse the new medication and that they are known to be sensitive to the euphoric effects of that drug class. The standard procedure in such studies is to measure subjective ratings of drug “liking” and other self-report ratings of positive effects produced by a test compound compared to a drug with known abuse liability. Typically, placebo and several doses of the test compound and of the comparator drug are administered to volunteers residing on an inpatient hospital unit. Studies are typically conducted in a well-controlled environment in order to prevent unsanctioned drug use and control other extraneous variables. In these studies, the adverse effects of the potential medication also are examined, such as subjective ratings of negative effects, impairments in cognitive task performance, or changes in physiological functioning, such as decreases in respiration or increases in blood pressure. Details of the methods used to conduct these studies have been published recently in several excellent reviews (Balster and Bigelow, 2003; Griffiths et al., 2003; McColl and Sellers, 2006; Preston and Walsh, 1998).
These same methods have been applied to the evaluation of putative pharmacotherapies for substance abuse disorders in order to determine whether the potential treatment agent can modify the abuse liability profile of the targeted drug of abuse. In this case, subjective effect measures are typically used to characterize the profile of action of the drug of abuse over a range of doses, both in the presence and absence (ideally, under placebo-controlled conditions) of the putative treatment agent. Although the data obtained from subjective effects batteries in both abuse liability studies and drug-interaction studies for medications development can be quite rich and yield critical qualitative and quantitative information, they can sometimes be difficult to interpret. For example, some drugs produce increases in both positive and negative subjective effects, and the balance of these effects may determine whether the drug will be abused (Foltin and Fischman, 1991). However, the determination of the point at which the positive effects outweigh the negative effects can be difficult to assess. The overall profile of subjective responses for a pharmacologically well-characterized compound can be compared to known drugs of abuse within that same pharmacological class in order to assess its abuse liability (Preston and Jasinski, 1991), but the abuse liability of a pharmacologically novel compound can be more difficult to assess in the absence of knowing the most suitable comparator. In an effort to deter abuse, different formulations of new and existing medications are being developed. Some examples of these new formulations include agonist-antagonist combinations, modifications of the physical properties of tablets to hinder tampering, or the addition of aversive agents, such as capsaicin or niacin. Standard approaches to abuse liability testing of such “abuse-deterrent” formulations (ADFs) may not be applicable in some cases, as described below.
The purpose of the present paper is first to summarize briefly the self-administration procedures that are commonly used in human laboratory research. While measurements of subjective effects are also critical to a comprehensive evaluation of the abuse liability of medications, the utility of these measurements and the specific questionnaires most commonly used have been reviewed recently and so will not be repeated here (Balster and Bigelow, 2003; Comer and Zacny, 2005; Griffiths et al., 2003; McColl and Sellers, 2006; Preston and Walsh, 1998). By contrast, a detailed review of the role of human drug self-administration procedures in abuse liability testing and its predictive validity in terms of clinical trial outcomes has not been made in recent years (although see Haney and Spealman, in press, and Panlilio and Goldberg, 2007 for comparisons of animal and human self-administration studies). We will then discuss the importance of examining drug self-administration in the development of medications for treating substance abuse and assessing the abuse liability of novel compounds for other medical uses, including those formulations specifically designed to reduce abuse and diversion.
2.0 Self-administration Procedures
By traditional definition, a drug “serves as a reinforcer” if the behavior leading to its consumption increases in probability over time (e.g., Foltin and Fischman, 1991; Skinner, 1966). For example, individuals tend to expend more effort accumulating money and locating a specific drug dealer if the drug sold by that dealer is considered to be of good quality than if it is considered to be of poor quality. The measurement of the increased behavior leading to drug consumption is the key feature of most laboratory models of drug reinforcement. The different types of procedures that have been used to measure drug taking by humans, specifically, are summarized briefly below. For more detailed reviews of human models of drug self-administration, please see Bigelow et al., 1976; Foltin and Fischman, 1991; Henningfield et al., 1991; Schuster, 1975.
2.1 Free Access Procedures
The most straightforward self-administration procedure is one in which participants have unlimited or “free access” to a drug (e.g., Griffiths et al., 1986; Liguori et al., 1997; Mooney et al., 2006; Richter et al., 2007; Spiga et al., 1998). These studies typically occur on an inpatient unit where participants can be carefully monitored for adverse reactions to the drug, although some studies have been conducted on an outpatient basis. For example, Griffiths and colleagues (1986) allowed heavy coffee drinkers free access to either decaffeinated or caffeinated coffee on alternating days while they were residing on an inpatient unit. Participants simply asked the research staff for coffee when they desired it. Interestingly, the number of cups ingested was relatively stable across days, suggesting that this procedure was relatively insensitive to differences in the reinforcing effects of caffeinated versus decaffeinated coffee. When a discrete-trial choice procedure was used (see description below), where participants were asked to choose between caffeinated and de-caffeinated coffee, then a clear preference for caffeinated coffee was found, but only when participants had been drinking caffeinated coffee for at least one week prior to testing (i.e., participants were most likely tolerant to and/or physically dependent on caffeine).
2.2 Verbal Choice Procedures
Another simple type of drug self-administration paradigm is one in which participants are given a sample dose of drug and then later asked whether or not they would like to self-administer the same dose, i.e., choice of a pill versus nothing. In separate sessions, participants are given a sample dose of placebo and then later asked whether or not they would like to self-administer the placebo. In this type of study, the operant behavior is a simple verbal response. That is, participants are choosing whether or not to take the dose that is available to them during that session, so when asked if they would like to take the dose again, they respond “yes” or “no.” If participants choose the active dose on more occasions than they choose placebo across sessions, then the active dose is considered to be a reinforcer. However, in this procedure, placebo may be chosen often, making it difficult to demonstrate the reinforcing effects of the active compound (i.e., a ceiling effect; Roehrs et al., 1997).
A more common approach is to use a discrete-trial choice procedure, whereby participants are given a sample of Drug A and then, during a separate session, a sample of Drug B (e.g., de Wit and Chutuape, 1993; Griffiths et al., 1980; Johanson and Uhlenhuth, 1980a, 1980b; Stern et al., 1989). Typically, one of these drugs is placebo and the other is a dose of active drug. Participants are instructed to attend to the effects produced by Drugs A and B and other concurrent stimuli, such as the color of the pill, are used to facilitate the association between the sample drug and the effects produced by that drug. During subsequent choice sessions, participants are instructed to verbally indicate whether they would like to ingest Drug A or Drug B. Typically, participants are given several choice opportunities, with 5 choice opportunities being the most common. The number or percentage of choices of Drug A and Drug B is then calculated. If the active drug is chosen significantly more often than placebo, then the drug is considered to be a reinforcer.
An adaptation of this discrete-trial choice procedure is a money versus drug choice procedure (e.g., Higgins et al., 1994; Mello et al., 1981; Stitzer et al., 1983), in which participants are asked to choose between a dose of drug and a fixed amount of money. A third variant on the money versus drug procedure is one in which the drug dose remains fixed while repeated choices are made between the dose and varying amounts of money; thus yielding an estimate of the value of the dose at the point where choice behavior changes (Donny et al., 2005; Walsh et al., 2001). An advantage of a money versus drug choice procedure is that fewer sample sessions are required (participants do not need to sample the money option because it has face validity as a salient reinforcer). Also, participants have the opportunity to choose a reinforcer other than drug, which is similar to the choice conditions that drug users face in their natural environments. However, there are two potential disadvantages of using money. First, money values need to be determined a priori relative to the value of drug, and the value of the illicit drugs can change over time as a function of the illicit marketplace. Second, due to differing socioeconomic circumstances and histories, fixed values of money may have widely different reinforcing efficacy between participants that can introduce an undesired noise factor (e.g., the participant who chooses money exclusively because of need).
Although the above procedures are commonly used methods for examining the reinforcing effects of drugs, one potential problem is that they can be time-consuming, involving multiple drug administrations. In response to this limitation, a multiple-choice procedure (MCP) was developed in an attempt to provide a quick and efficient estimate of the reinforcing effects of a drug (Griffiths et al., 1993). As with the other procedures, participants generally are first given doses of the test drug by the experimenter. They subsequently are asked to make a series of choices on a questionnaire between either two doses of drug (Drug A versus Drug B, Drug A versus Drug C, Drug B versus Drug C, etc.) or between drug and money (Drug A versus $0.50, Drug A versus $0.75, Drug A versus $1, etc.) to reflect their hypothetical choice preference. After the questionnaire is completed, one choice is selected randomly (often using a lottery-like procedure) and given to the participant. As in the above procedures, the operant behavior is a simple yes/no answer in response to the question of drug taking. Using this procedure, Griffiths and colleagues (1993) demonstrated a pentobarbital dose-related choice over money. In addition, larger doses of pentobarbital were chosen over smaller doses and over placebo. Similar results have been reported for drugs from other pharmacological classes (e.g., Lile et al., 2004; Tancer and Johanson, 2003, 2007). These results demonstrate that the MCP may be an efficient alternative to the more traditional self-administration procedures described above. However, there are some disadvantages to the MCP. Although drug and money are actually delivered during this procedure, which is similar to the traditional self-administration procedures, the disadvantages are that only a single delivery of drug or money is made, and there is often a substantial delay between the time that the choices are made and the time that the reinforcer is actually delivered. In addition, the procedure is now sometimes used without the lottery portion (Correia and Little, 2006), which essentially removes the component of reinforcer delivery that sets the MCP apart from other questionnaires.
2.3 Non-verbal Operant Procedures
The second major type of self-administration procedure involves the use of non-verbal operant responses that involves more effort than a simple verbal response. Participants are instructed to make responses on a manipulandum (computer mouse, joy stick, bicycle, etc.) in order to receive a drug. This type of study largely grew out of procedures developed in laboratory animals during the early 1960’s (e.g., Deneau et al., 1969; Thompson and Schuster, 1964). Soon thereafter, the study of drug self-administration via operant responding was initiated in human research volunteers (Mendelson and Mello, 1966). One of the simplest operant schedules is the fixed-ratio (FR) schedule, in which participants make a fixed number of responses in order to obtain drug (e.g., Griffiths et al., 1976). For example, after every 200 responses on a manipulandum, participants receive a fixed amount of drug (FR200). A “timeout” period, during which drug is unavailable, usually follows each drug delivery in order to minimize the occurrence of adverse effects, and the maximum number of drug deliveries that can be self administered is often imposed for safety reasons. The rate of responding for drug, pattern of responding, number of drug deliveries, and amount of drug received are the primary dependent variables. When the data are graphed as a function of dose and rate of responding or number of infusions obtained, an inverted U-shaped dose-response curve is sometimes found (e.g., Henningfield and Goldberg, 1983). The ascending portion of the dose-effect curve is thought to reflect increases in the reinforcing effects of the drug, while the descending portion of the dose-effect curve reflects a combination of reinforcing effects and other factors, such as behavioral incapacitation (inability to respond) or drug satiation. Due to concerns about drug toxicity, human studies are generally limited to examining the ascending portion of the dose-response curve.
A second type of operant schedule that is used to examine the reinforcing effects of drugs in humans is the progressive-ratio (PR) schedule (Hodos, 1961; Hodos and Kalman, 1963; for detailed reviews of PR schedules, see Arnold and Roberts, 1997; Rowlett, 2000; Stafford et al., 1998). In this procedure, the number of responses required to receive each drug delivery progressively increases, so that it becomes more and more difficult (i.e., more work is required) to receive the same amount of drug. Oftentimes, the ratio value is increased logarithmically or arithmetically after each drug delivery and the behavioral endpoint is the ratio value at which responding stops. The maximum ratio value completed, which has been termed the “break point value,” is generally the primary dependent variable in studies using PR schedules. A fixed amount of time to complete each ratio value is allotted, and, as with FR procedures, a limit is usually set on the maximum amount of drug that participants are allowed to self-administer. The main advantage of the PR schedule over the FR schedule is that it can be used to examine the relative reinforcing effectiveness or value of a range of different drugs and doses without relying directly on response rates, which are sometimes difficult to interpret. Drugs that maintain larger break point values are also drugs that are considered to have greater abuse liability (Katz, 1990; Stafford et al., 1998).
3.0 Drug Self-administration and Medications Development for Drug Dependence
The potential utility of self-administration procedures in human laboratory research has been examined in the context of the development and evaluation of pharmacotherapies for the treatment of various substance dependence disorders (e.g., O’Brien and Gardner, 2005; Rukstalis et al., 2005; Stoops et al., 2007). These studies are germane to abuse liability testing because they have been commonly employed to detect the ability of the putative pharmacotherapy (typically as a pretreatment) to reduce the abuse liability of the targeted drug of abuse. Moreover, these studies have often collected data using subjective effects batteries (the standard approach to abuse liability evaluation; see above) concurrently with measures of self-administration behavior, providing an opportunity to examine directly the relative sensitivity and predictive validity of each, along with their concordance. Thus, review of these studies can provide guidance from both experimental and conceptual viewpoints regarding the potential strengths and weaknesses of self-administration procedures and their utility for abuse liability evaluations. The studies described below focus on evaluation of pharmacotherapies for opioid dependence, a condition for which effective treatments have been characterized in the laboratory, and cocaine dependence, a condition for which there are presently no approved pharmacological treatments.
3.1 Medications Development for Opioid Dependence
There are presently three agents marketed in many countries for the treatment of opioid dependence—naltrexone, methadone and buprenorphine. The first two have been employed for this purpose for approximately four decades, while the latter was initially approved for use in France in 1996, and then subsequently introduced into other countries (including the United States in 2002). For each of these medications, there are published studies from the human laboratory on self-administration and subjective-effect measures available for examination. In each case, the medication has been clinically proven and accepted as efficacious, and thus, because a valid laboratory method should detect the significant behavioral/pharmacological interactions between the treatment agent and the drug of abuse over the range of doses demonstrated to be clinically effective, the opioid pharmacotherapies provide an opportunity to examine the sensitivity, specificity and potential validity of these approaches.
3.1.1 Naltrexone: Laboratory Evaluation of an Opioid Antagonist Treatment
The clinical effectiveness of naltrexone is derived from its ability to competitively antagonize mu opioid receptors and, thereby, block the effects of illicitly administered opioids. The receptor pharmacology of this drug interaction is relatively straightforward, and thus, maintenance of sufficient receptor blockade (by maintaining adequate plasma levels) can provide protection against opioid abuse. Unfortunately, naltrexone is an unpopular treatment approach: compliance is poor, drop-out is high, and its effective clinical use is quite circumscribed (Kirchmayer et al., 2002; Sullivan et al., 2005). However, as a model medication, it is outstanding because it produces few, if any, direct pharmacological effects of its own.
The first studies to examine the effects of naltrexone on opioid self-administration by humans were conducted by Meyer and colleagues (Altman et al., 1976; Meyer et al., 1976). In these pioneering studies, patients with a history of past treatment failures for heroin dependence were recruited to participate while living on a closed research inpatient unit. An FR schedule was employed that required responses (ranging from FR 300 to FR 2100) on a hand counter for heroin (0.5 mg/unit dose). Patients cycled through a series of study phases that could include initial detoxification to a drug-free status, acquisition of heroin self-administration (using a dose escalation schedule over a period of days up to a maximum of 60 mg/day), methadone detoxification, and heroin self-administration during maintenance on naltrexone. Eight individuals completed the phases of the study required for evaluation of heroin self-administration under “blocked” (i.e., naltrexone maintenance) and “unblocked” (i.e., drug-free) status. Naltrexone maintenance (75 mg/day for most participants) produced a nearly complete elimination of heroin taking in these difficult-to-treat patients.
Mello and colleagues (1981) also examined the effects of naltrexone on heroin self-administration by humans. Individuals who were previously heroin-dependent participated as inpatients while they were maintained on either oral placebo or naltrexone (50 mg/day, p.o.) under double-blind conditions. Intravenous heroin (10 mg, i.v.), which could be obtained by making 300 responses on a response button, was available four times per day during a 10-day period of the study. A similar operant schedule was in place to provide an opportunity to earn an alternate reinforcer, money. Daily intake of heroin was quite stable over the course of the 10-day treatment period for the group maintained on placebo; the average intake was about 35 mg heroin/day with individuals taking between 58 to 100% of the available heroin (40 mg/day). In contrast, after the first day of active naltrexone treatment, heroin self-administration was reduced to nearly zero for all of the participants and, over the 10-day period, this group took only between 3 to 8% of the available doses and stopped working for the drug after taking only one or two injections. This study, like the earlier one by Meyers and colleagues, demonstrated that, in the presence of adequate opioid blockade, the abuse liability of heroin was nearly completely suppressed as evidenced by an absence of self-administration behavior.
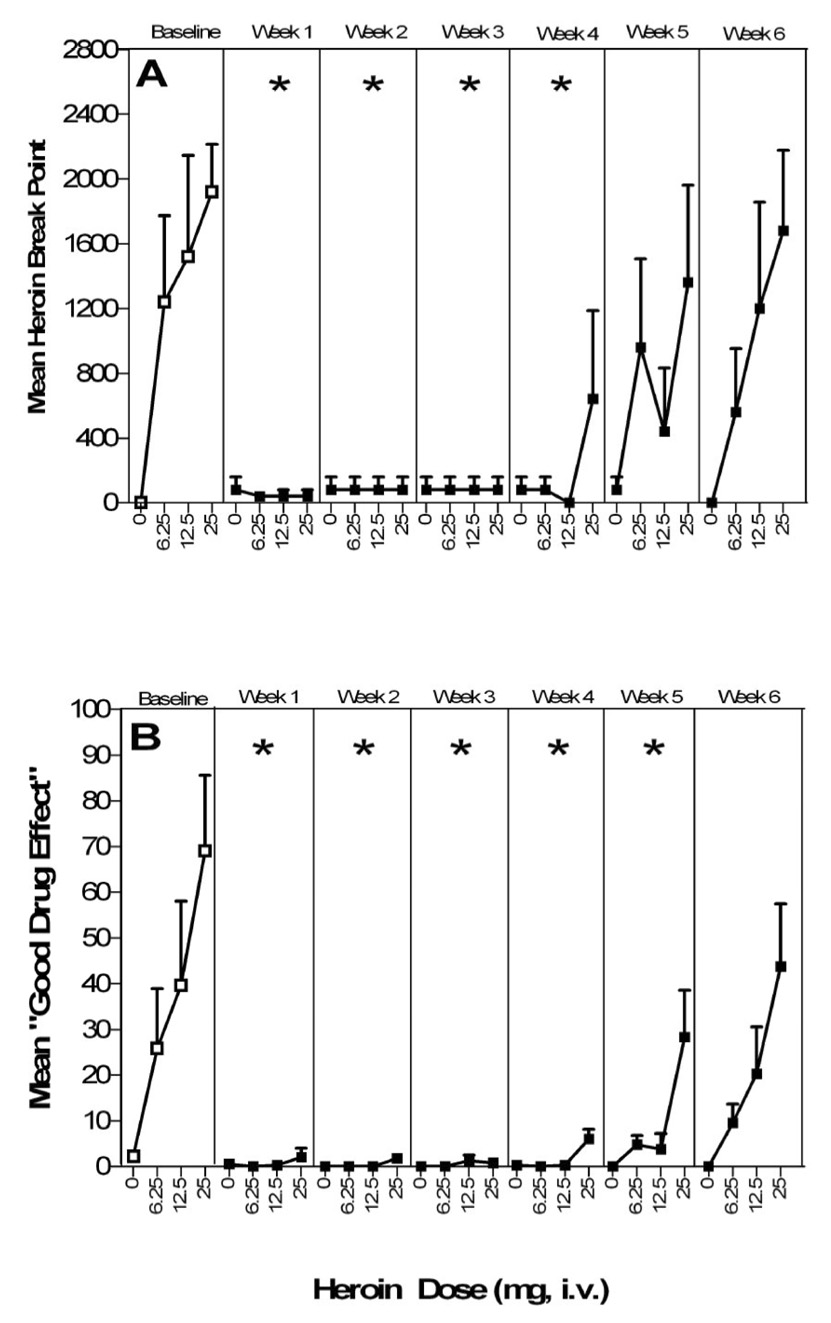
A more recent study examined a novel long-acting depot formulation (Depotrex®) of naltrexone for its ability to alter heroin self-administration (0, 6.25, 12.5 and 25 mg, i.v.) using a PR procedure in five heroin-dependent individuals who underwent detoxification prior to naltrexone dosing (Sullivan et al., 2006). The depot formulation of naltrexone was administered as a single injection previously shown to produce antagonism of heroin-induced effects for at least four weeks (Comer et al., 2002). The findings by Sullivan and colleagues (2006) were concordant with the earlier demonstrations that naltrexone administration produced nearly complete suppression of heroin self-administration, reducing the average break-point value to near zero (Figure 1; top panel). Moreover, subjective effect measures collected during the sample sessions when test doses of heroin were experimenter-administered indicated that participants reported virtually no subjective response on measures predictive of abuse liability (e.g., measures of drug liking and good drug effects) (Figure 1; bottom panel). As elimination of naltrexone occurred from this long-lasting formulation, heroin self-administration recovered to baseline levels, as did increases in subjective ratings of positive or euphoric drug effects indicating a temporal correlation between these two outcomes.
Figure 1.
Effects of a long-acting naltrexone formulation on the effects of heroin. For both panels, open symbols represent data collected during the baseline period and closed symbols represent data collected after administration of depot naltrexone. Error bars represent ± 1 standard error of the mean (S.E.M.). Asterisks indicate week difference from baseline at P < 0.01. Top panel (A). Self-administration of heroin as a function of dose (0 to 25 mg) and study week. Data points represent mean breakpoint for heroin. Maximum score = 2800. There was a significant main effect of Study Week (P < 0.0005) and a significant Week by Heroin Dose interaction (P < 0.005). Bottom panel (B). Mean peak VAS ratings of “Good drug effect” after administration of heroin (0 to 25 mg) as a function of dose and study week. Data points represent mean peak ratings. Maximum rating = 100 mm. [Figure reproduced from Sullivan, et al., 2006].
3.1.2 Methadone: Laboratory Evaluation of an Opioid Agonist Treatment
The first demonstration of the efficacy of methadone to suppress opioid self-administration in the human laboratory was published more than three decades ago. Jones and Prada (1975) examined a cohort of six federal prisoners who were incarcerated for narcotic-related offenses. The participants were maintained first on placebo and then, after a 2.5 month period, they began maintenance on oral methadone (from 5 mg escalating up to 100 mg per day over a 6-week period). During each phase, participants were given the opportunity to work for hydromorphone (4 mg, i.v.) three times weekly. The behavioral requirement for earning a drug reinforcer was riding a stationary bicycle for a specified distance (5 or 10 miles). If only a portion of the required distance was covered, participants received a hydromorphone infusion, but the dose was proportional to the amount of the work completed. Maintenance on placebo led to nearly 100% of the available hydromorphone being earned by these six individuals, and none worked for saline infusions. Five of the six participants continued working for hydromorphone at 50 mg methadone/day. During the first weeks of treatment with 100 mg/day methadone, self-administration was reduced even further and was nearly completely suppressed after three weeks of maintenance on this dose. Similarly, subjective effect reports of “liking” in response to hydromorphone were reduced as a function of methadone maintenance dose. This dose response function for methadone obtained under controlled laboratory conditions corresponds closely with clinical trials reporting that methadone at doses near 50 mg/day are less effective at reducing illicit opioid use compared to doses in the 100 mg range (e.g., see Faggiano et al., 2003 and also Strain et al., 1999 for review). Moreover, the observation that a longer period of methadone stabilization (in this case, three weeks rather than one) is consistent with clinical reports that the full therapeutic benefit of methadone maintenance is commonly observed only after an extended period of maintenance (i.e., 3 to 4 weeks).
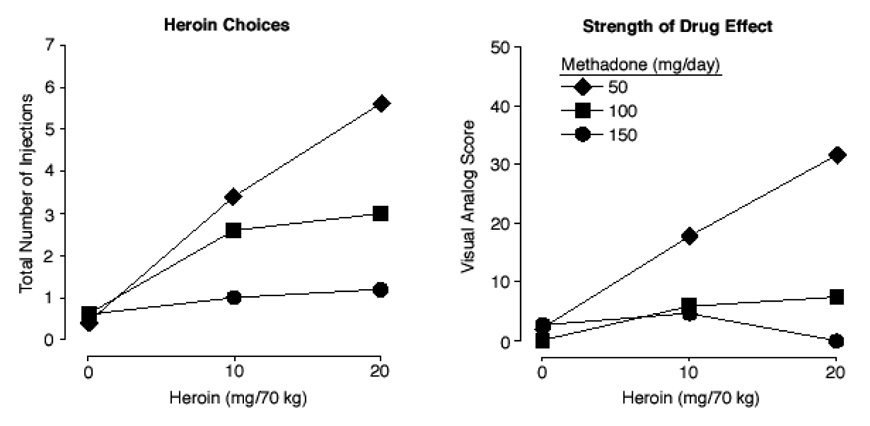
A more recent study employed a choice self-administration procedure to examine methadone over a broader range of doses for its ability to suppress heroin self-administration (Donny et al., 2005). Heroin-dependent volunteers were stabilized on 50, 100 and 150 mg per day of oral methadone in ascending order during three separate outpatient periods. A 4-week inpatient-testing period followed stabilization at each methadone maintenance dose. Participants were given the opportunity to sample three doses of heroin (0, 10, or 20 mg, i.v. given in random order at one dose per week) and were subsequently allowed seven opportunities to choose between another injection of the assigned heroin dose and varying amounts of money (ranging from $2 – $38). Choice for heroin injections was reduced in an orderly fashion as a function of methadone maintenance dose (Figure 2; left panel), but near complete suppression was not achieved until participants were maintenained on the highest methadone dose (150 mg).
Figure 2.
Effects of different maintenance doses of methadone on the effects of heroin. Left panel. Mean total number of injections during the self-administration sessions. There were significant main effects of Methadone Dose and Heroin Dose, as well as an interaction between Methadone and Heroin Dose (P < 0.05). Right panel. Mean change from baseline visual analog rating of “How strong is the drug effect?” There was a significant main effect of Methadone Dose (P < 0.05) and a Methadone Dose by Heroin Dose interaction (P < 0.05). [Figure reproduced from Donny, et al., 2005].
Subjective measures related to the abuse liability of heroin were collected during each of the sample sessions. Heroin-induced subjective effects, including “drug liking” and strength of drug effect (Figure 2; right panel), were also reduced in a dose-dependent manner by methadone. In contrast to the heroin self-administration data, the subjective effects of heroin were largely suppressed by the intermediate dose of methadone (100 mg) and scores were comparable to those observed during maintenance on 150 mg methadone. These findings suggest that the subjective responses to heroin may be more readily attenuated by methadone compared to self-administration behavior, which, in this case, required a larger dose, and that concomitant collection of both outcome measures may yield differential estimates of efficacy.
3.1.3 Buprenorphine: Laboratory Evaluation of a Partial Agonist Treatment
Buprenorphine is a partial mu opioid agonist with demonstrated efficacy in reducing illicit opioid abuse (e.g., Johnson et al., 1992; Ling and Wesson, 2003). Its unique therapeutic advantages include a low risk for clinically significant respiratory depression, long duration of action allowing less-than-daily dosing, and mild withdrawal symptoms upon cessation of use (e.g., Amass et al., 1998; Jasinski et al., 1978; Strain, 2006; Walsh et al., 1995), all of which are attributable, in part, to its partial agonist profile with less-than-maximal intrinsic activity and its high lipophilicity (see Walsh and Eissenberg, 2003 for review). Buprenorphine is marketed in a single drug formulation and also in combination with naloxone, which is intended to deter illicit diversion to the parenteral route. If a patient uses the buprenorphine/naloxone combination product sublingually, as prescribed, naloxone should have little pharmacological effects because of its poor bioavailability by the sublingual route. However, if the opioid-dependent patient uses the medication parenterally (e.g., intravenously, subcutaneously), naloxone would elicit opioid withdrawal symptoms.
The ability of buprenorphine to alter heroin self-administration by humans was originally examined using an operant procedure employing a second order schedule of reinforcement (Mello et al., 1980, 1982). Heroin-experienced individuals, residing as inpatients, were given the opportunity to work (in this case, button pressing) for either heroin (7 or 13.5 mg, i.v.) or money after random assignment to maintenance on either buprenorphine (8 mg/day, s.c.) or placebo. It was demonstrated that less than 30% of the available heroin was self-administered in buprenorphine-maintained individuals compared to more than 90% in those maintained on placebo.
One additional study examined buprenorphine in a solution formulation (prior to the development of the marketed tablets) for its ability to alter opioid self-administration (Greenwald et al., 1999). This outpatient study maintained volunteers on buprenorphine over a range of sublingual doses (2, 4 and 8 mg, s.l. per day) and evaluated self-administration of hydromorphone. The subset of patients who were successful in abstaining from heroin use during the study exhibited little opioid self-administration in the laboratory. In contrast, those patients for whom buprenorphine was not clinically effective in suppressing their illicit opioid use demonstrated significant levels of hydromorphone self-administration in the laboratory. The subjective effects of hydromorphone also differed between the two groups of patients. These findings illustrate a concordance between findings in the laboratory and clinical outcomes with respect to individual differences in therapeutic response.
The marketed preparations of buprenorphine alone (Comer et al., 2001; Greenwald et al., 2002) and buprenorphine formulated in combination with naloxone (Comer et al., 2005) have been examined for their efficacy in reducing opioid self-administration using a PR procedure. Comer and colleagues (2001) demonstrated that buprenorphine maintenance was effective at reducing intravenous heroin self-administration, with larger doses (16 mg/day) demonstrating greater efficacy than smaller doses. In this case, the reduction in heroin self-administration closely paralleled the reduction in positive subjective effects of “liking” and “good drug effects,” but self-administration behavior was not completely suppressed even at the highest dose. Using a different PR procedure, Greenwald and colleagues (2002) reported similar findings indicating that larger doses of buprenorphine were more effective in suppressing hydromorphone self-administration than smaller doses (16 vs. 2 mg/day), and this dose difference was preserved when an alternate-day dosing schedule (with doubled doses of 32 and 4 mg/day) was employed. Finally, the self-administration of intranasal heroin was examined as a function of treatment with the buprenorphine/naloxone combination product using a progressive ratio procedure (Comer et al., 2005). Similar results were obtained whereby larger doses of buprenorphine were more effective than smaller doses at suppressing heroin self-administration with the lowest buprenorphine/naloxone dose (2.0/5 mg) being comparable to placebo. In this case, the subjective ratings in response to heroin were more uniformly reduced by all active doses of buprenorphine in comparison to placebo, suggesting that the subjective effects may be reduced by doses that do not significantly reduce self-administration.
In summary, each of the three medications proven effective for the treatment of opioid dependence has also been demonstrated to suppress opioid self-administration in the laboratory setting in concordance with their ability to suppress illicit opioid self-administration. These studies employed an array of self-administration procedures including operant schedules with substantial response requirements, choice procedures with and without alternate reinforcers, progressive ratio procedures, and different opioid drugs of abuse and routes of administration, thus demonstrating the robust sensitivity of the self-administration paradigm to detect medication effects at doses in the clinically therapeutic range. The findings generally reveal dose-related efficacy (where multiple doses are examined) and a concomitant decrease in ratings of positive subjective effects in response to challenge with the drug of abuse. These reductions are not always perfectly correlated with reductions in self-administration and, in some cases, the subjective responses are significantly attenuated by doses that are less effective at suppressing self-administration. This suggests that subjective effects may be more readily modifiable than drug-taking behavior.
3.2 Medications Development for Cocaine Dependence
Extensive research efforts to develop an effective pharmacotherapy for the treatment of cocaine dependence has been underway for nearly two decades in the United States. While, unfortunately, no medications have been approved for this indication and none has proven broadly effective from this extensive program, a large scientific body of data and knowledge has emerged from this work. Cocaine has a more complex neuropharmacological profile of action in comparison to the mu opioid agonists. Cocaine produces activity through numerous neurochemical systems that may be altered differentially in response to acute versus chronic exposure, and its primary neurochemical actions related to its abuse liability (i.e., inhibition of neurotransmitter reuptake at monoaminergic sites) are not mediated through single receptor interactions. Thus, from a pharmacological standpoint, it has been a tremendous challenge to identify the correct biological target(s) for development of an efficacious treatment, and, accordingly, agents from diverse pharmacological classes have been evaluated.
For the purposes of the present paper, an exhaustive review of all of the potential pharmacotherapies that have undergone some clinical evaluation is unnecessary and is available elsewhere (e.g., Vocci and Elkashef, 2005). Rather, this section will focus only on those agents that have been evaluated in the human laboratory for both their ability to alter 1) the subjective profile of cocaine, and 2) self-administration of cocaine (Table 1) under similar dosing conditions. In many (but not all) cases, there is also at least one published clinical trial using good randomized and controlled conditions available to provide some comparative evidence on the potential clinical efficacy in a treatment population.
Table 1.
Outcomes from drug interaction testing of putative pharmacotherapies against cocaine on subjective effect measures and self-administration.
| Test Agent | Change in Subjective Responses1 | Change in Self-administration | References |
|---|---|---|---|
| Flupenthixol | - | - | Evans et al., 2001 |
| Butorphanol | - | - | Walsh et al., 2001 |
| Phenytoin | - | - | Sofuoglu et al., 1999 |
| Desipramine | ↓/↑ | - | Fischman et al., 1990 |
| Enadoline | ↓▯ | - | Walsh et al., 2001 |
| Gabapentin | ↓▯ | - | Hart et al., 2004 |
| Pergolide | ↓▯ | - | Haney et al., 1998 |
| ABT-431 | ↓▯ | - | Haney et al., 1999 |
| Memantine | ↑▯ | - | Collins et al., 2006 |
| Baclofen | −/↓ | ↓▯ | Haney et al., 2006 |
| Buprenorphine | ↑ | ↓▯ | Foltin & Fischman, 1994 |
| Ecopipam | ↑/− | ↑/− | Haney et al., 2001, Nann-Vernotica et al., 2001 |
| Modafinil | ↓▯ | ↓▯ | Hart et al., 2008 |
Arrows denote the direction of change whereby subjective response to cocaine on abuse liability measures was either increased (↑), decreased (↓) or no change was observed (−).
Table 1 includes agents representing a diverse range of pharmacological classes, including antidepressants, anticonvulsants, antispasmodics, and a wide range of neuropharmacological targets, including dopamine, GABA, glutamate, and mu and kappa opioid systems. Agents are arranged within the table according to the outcomes for and concordance between the test procedures. That is, the first three agents shown [flupenthixol (a dopamine D1/D2 receptor antagonist and alpha adrenergic receptor antagonist), butorphanol (a partial opioid agonist at mu and kappa receptors), and phenytoin (an anticonvulsant with an unknown mechanism of action)] are those for which clinical studies demonstrated that pretreatment or maintenance on the test agent failed to alter the subjective response to cocaine challenge and failed to alter cocaine self-administration, thus demonstrating good concordance between the procedures with these medications.
The next six agents listed [desipramine (a tricyclic antidepressant), enadoline (a kappa opioid receptor agonist), gabapentin (a nonselective GABA agonist), pergolide (a dopamine D1/D2 receptor agonist), ABT-431 (a selective dopamine D1 receptor agonist) and memantine (a low affinity N-methyl-D-aspartate receptor antagonist)] are those for which some significant alterations in the subjective response to cocaine (the direction of change is indicated by the arrows) were observed in the absence of significant changes in self-administration behavior. The dissociation between these two outcomes is not completely surprising. First, the controlled nature of the laboratory setting and the careful construction of subjective effect measures are designed to provide a sensitive assay of direct pharmacodynamic effects and drug interactions. Thus, modest modifications in the subjective effects profile of the drug of abuse, in this case cocaine, may lead to significant changes at doses which are below the threshold for those which may produce changes in self-administration and/or clinically meaningful effects. This suggestion is supported by examples from the opioid treatment field where the clinically effective dose of the treatment agent is known. For example, while the daily therapeutic dose of naltrexone is 50 mg, laboratory data reveal that significant reductions or blockade of opioid agonist effects will occur at substantively smaller doses (i.e., subtherapeutic) than those needed for effective clinical treatment (e.g., Walsh et al., 1996). This is also consistent with findings from some preclinical studies, which report that a pretreatment agent may significantly alter the discriminative stimulus effects of a drug (frequently likened to subjective effects in human laboratory research) at doses that do not alter self-administration behavior (e.g., Barrett et al., 2005; Filip et al., 2007). Thus, subjective effect measures may provide a more sensitive assay of specific pharmacological interaction than self-administration behavior. However, because it is unknown what magnitude of interaction is required to alter drug-taking behavior (the target in medications development for substance abuse), it is also possible that this sensitivity may lead to a higher rate of false positive findings (i.e., those medications which produce a positive signal in the laboratory setting but fail in the clinic). Additionally, it is unknown, in the case of cocaine, how the direction of interaction may impact drug-taking behavior. For example, it is possible that a partial reduction in the euphoric effects of cocaine (rather than complete blockade which has yet to be achieved by any agent) will lead to an increase, rather than a decrease, in drug taking reflecting some compensation for the attenuated drug effect. There is some support for this from laboratory findings (e.g., Walsh et al., 2001) and from some clinical trials, which have reported increased rates of cocaine use in active versus placebo treatment groups (e.g., Kampman et al., 2003).
The final group of compounds is that for which significant alterations in the subjective response to cocaine and significant changes in cocaine self-administration behavior were concurrently observed. In the case of baclofen, a GABAB receptor agonist, a reduction in self-administration occurred only at the lowest dose of smoked cocaine tested (12 mg) and not at the larger doses (25 and 50 mg), which are associated with greater abuse liability (Haney et al., 2006). Baclofen also decreased subjective ratings of craving for cocaine and the amount participants were willing to pay for cocaine, although other subjective ratings typically associated with abuse liability such as drug liking and good drug effects were unaffected by baclofen. Thus, while the findings were concordant between the two outcomes, the signal was relatively weak in that a reduction in self-administration was only found with the lowest dose of smoked cocaine and only a subset of positive subjective responses was altered. Using an acute pretreatment procedure and lower doses of baclofen than those used by Haney and colleagues (2006), Lile et al. (2007) reported that baclofen did not significantly alter the subjective effects of intranasal cocaine and it did not alter responding on the multiple choice procedure. In the case of buprenorphine (Foltin and Fischman, 1994), the nature of the interaction between this partial mu agonist and cocaine on the subjective effect measures was one of potentiation – that is, the combination of the opioid agonist and cocaine produced a constellation of drug responses that reflected the activity of both drugs and increased the magnitude of the response for measures of their shared effects (e.g., ratings of “high”). Under the high dose conditions, buprenorphine reduced cocaine self-administration; however, participants were reported to be significantly intoxicated from the drug combination. Thus, the observed reduction in self-administration may reflect a compensatory change in drug taking in response to the increased euphoric and impairing effects of the drug combination. This suggestion is complementary to the compensatory changes described above for the case of reduced subjective effects. In the case of ecopipam, a dopamine D1/D5 antagonist also known as SCH 39166, mixed results were obtained across studies. Nann-Vernotica and colleagues (2001) reported that ecopipam, up to maintenance doses of 100 mg, failed to alter the subjective effects of cocaine. In contrast, Haney and colleagues (2001) reported that 100 mg ecopipam increased the reinforcing effects of a small dose of smoked cocaine (12 mg) and it increased subjective ratings of “good drug effect,” “high,” “stimulated,” and dose quality produced by a large dose of cocaine (50 mg). Combined with the data collected in studies using laboratory animals (e.g., Kleven and Woolverton, 1990), a possible explanation is that dopamine receptor supersensitivity occurred following chronic administration of a D1/D5 antagonist, which mediated the increases in the subjective and reinforcing effects of cocaine.
The final agent in the list is modafinil – one for which the findings are concordant across the two paradigms and may be the best example of the desired profile of findings for a promising agent. Although the receptor pharmacology of modafinil is not fully understood, it appears to occupy both dopamine and norepinephrine transporters at therapeutic doses (Madras et al., 2006). In this study, modafinil pretreatment significantly reduced the subjective response to cocaine in the absence of producing unpleasant side effects and significantly reduced cocaine self-administration in a dose-dependent fashion (Hart et al., 2008). These findings are in agreement with a small-scale clinical trial that examined the efficacy of modafinil compared to placebo in individuals seeking treatment for cocaine dependence and reported significant reductions in cocaine use in the group treated with modafinil (Dackis et al., 2005).
3.3 Summary of Medications Development for Opioid and Cocaine Dependence
In summary, studies from the opioid literature examining medications of proven efficacy (i.e., naltrexone, methadone and buprenorphine) reveal that the subjective mood effects related to abuse liability are reliably blunted and, at sufficient doses, completely blocked by treatment with these therapeutic agents. Under conditions of adequate blockade of the euphoric effects of the abused substance, comparable decreases in drug self-administration are observed. Across the range of medications reviewed for the treatment of opioid dependence, this is true regardless of the specific method employed for measuring self-administration. For example, fairly simple choice procedures (drug versus no drug), choice procedures involving fixed versus changing alternative reinforcers, behavioral arrangements requiring simple requirements, such as button pressing or bicycle riding, and progressive ratio procedures alone or in combination with alternative reinforcers yield concordant outcomes. Findings from research on medications development for cocaine dependence, for which drugs of unknown potential clinical efficacy have been evaluated, suggest that studies of subjective effect measures and self-administration behavior may yield concordant outcomes under some conditions. However, a number of studies also demonstrate that significant alterations in subjective responses to cocaine may occur in the absence of changes in self-administration behavior (it is important to note that no studies have reported the opposite dissociation – that is, changes in self-administration in the absence of subjective effects measures). Findings from both the opioid and cocaine medications development arenas indicate that subjective effects may be more readily modified at smaller doses of the putative therapeutic agent compared to those required to alter self-administration behavior.
The studies described above demonstrate that a good concordance exists between medications that are effective in reducing the reinforcing effects of opioids and in reducing opioid use in clinical settings. Therefore, good external validity exists for the laboratory models of opioid self-administration. However, there are currently no effective treatments for cocaine dependence, so it is not possible to make definitive statements about the external validity of cocaine self-administration procedures other than to note that virtually all of the medications that have been ineffective in the laboratory are also ineffective in the clinic.
4.0 Direct Assessments of the Reinforcing Effects of Test Compounds
In addition to medications development for treating substance dependence, another use of the self-administration procedure has been to evaluate the abuse liability of the treatment agents themselves. When the receptor pharmacology of the compound is known, as is the case for many opioids, the use of the self-administration paradigm is relatively straightforward as long as attention is paid to certain experimental details. Because buprenorphine, a partial mu opioid agonist, is one of the best characterized medications in terms of abuse liability testing, it will be described in some detail here. The reinforcing effects of intravenously delivered buprenorphine were examined in a series of studies in recently-detoxified human research volunteers using a drug versus money PR choice procedure (Comer et al., 2002, 2005; Comer and Collins, 2002). In all of these studies, i.v. buprenorphine was self-administered above placebo levels. When buprenorphine was compared to the full mu opioid agonist methadone, the reinforcing and subjective effects of the two medications were remarkably similar (Comer et al., 2005).
When i.v. buprenorphine was compared to i.v. buprenorphine/naloxone in recently-detoxified individuals, the breakpoint values for the two medications did not differ (Comer and Collins, 2002). In this study, however, the magnitude of the positive subjective responses produced by the buprenorphine/naloxone combination was less than that of buprenorphine alone. Interestingly, the buprenorphine/naloxone combination was self-administered even at doses that produced no statistically significant increases in subjective responses. [Similar results (i.e., drug self-administration in the absence of changes in subjective responses) have been reported for morphine (Lamb et al., 1991) and for cocaine (Martinez et al., 2004).] When participants were asked why they self-administered buprenorphine/naloxone when they felt no measurable subjective effects, they reported that they slept better that night or that they had less muscle pain. In these studies with buprenorphine, all of the participants were detoxified from heroin only 1–2 weeks prior to initiation of the experimental sessions and so they were still experiencing some mild withdrawal symptoms. Based upon these self-reports, it appears that participants were self-administering buprenorphine both for its positive subjective effects, i.e., positive reinforcement, and/or to alleviate subtle withdrawal symptoms, i.e., negative reinforcement. In contrast to the results obtained in recently detoxified, heroin-dependent individuals (Comer and Collins, 2002), a separate study conducted in individuals maintained on divided doses of morphine showed that i.v. buprenorphine was not self-administered at any of the doses that were tested, even those that produced increases in positive subjective responses (Comer et al., in press). In these physically-dependent individuals, buprenorphine produced positive subjective responses, but it also precipitated mild opioid withdrawal.
Clearly, because subjective responses and drug self-administration may be dissociable, concurrent collection of both measures will yield a richer and more informative data set and potentially improve the concordance between the laboratory and clinical outcomes. Furthermore, it is important to note that the state of physical dependence, when dealing with a drug class known to produce physical dependence, should be carefully controlled. And finally, a comparator drug of known abuse liability (i.e., a positive control) should be included in the assessment in order to make conclusions about the abuse liability of the test medication relative to a drug with known abuse liability. For medications that are known to produce their pharmacological effects through opioid receptors, the studies can be relatively straightforward. Abuse liability studies of other medications, for example those with actions at multiple receptor systems, “first-in-class” compounds, or different formulations of existing medications can be more challenging. Using the latter category as an example, the section below describes some of these challenges and also offers some possible solutions.
5.0 Assessing Abuse-Deterrent Formulations
In response to the increased awareness of prescription medication tampering (Cone, 2006), industry and academic scientists have begun to develop an array of novel abuse-deterrent formulations designed to make the manipulation of modified-release formulations more difficult for abusers and, thus, less attractive (Table 2). Most of these technologies either 1) add one or more aversive agents, 2) add an antagonist, 3) make pills difficult to crush, 4) make extraction difficult, 5) use pro-drugs, or 6) employ a combination of two or more of these approaches. Only a selective review of abuse liability testing of abuse-deterrent formulations will be made here, in part, because these studies have not yet been performed for some of the strategies listed.
Table 2.
Abuse deterrent formulations that have been or are under development.
| Compound | ADF Approach | Source |
|---|---|---|
| oxycodone | antagonist (naloxone) | Heins, 2002 |
| oxycodone | sequestered antagonist* (naltrexone) | Gorski, 2002 |
| Kadian NT (morphine) | sequestered antagonist (naltrexone) | Johnson et al., 2007 |
| Oxycodone-NT | sequestered antagonist (naltrexone) | www.alpharma.com |
| OxyNal (ELI-216) | sequestered antagonist (naltrexone) | www.elitepharma.com |
| Opioid, not disclosed | hard, non-crushable tablet | Abstracts / Drug and Alcohol Dependence 83S (2006) S84 |
| Remoxy (oxycodone) | ORODUR; hard-gel capsule | www.paintrials.com |
| PTI-202 (opioid, not disclosed) | ORODUR hard-gel capsule | www.paintrials.com |
| TQ-1017 (Tramadol OAD) | "SECUREL™", resists crushing | www.theraquest.com |
| OxyADF (oxycodone) | subtherapeutic amount of niaicin to cause flushing | www.acurapharm.com |
| Vynase (lisdexamfetamine) | Pro-drug | www.shire.com |
| NRP290 (hydrocodone) | Pro-drug | www.shire.com |
ADF = Abuse Deterrent Formulation
sequestered antagonist = the antagonist is sequestered within the core of the pill and theoretically is only released if product tampering occurs by crushing or dissolving
One general strategy for reducing abuse potential has been to develop formulations that deliver the drug in a slow and controlled manner. For example, OxyContin® (controlled-release oxycodone), given twice daily (BID), delivers the same daily dose of immediate-release oxycodone administered four times daily (QID), but reaches a lower maximum concentration (Cmax) and has a delayed time to maximum concentration (Tmax). While these features were developed for patient convenience (need for less frequent dosing over the course of the day), it is generally accepted that these pharmacokinetic properties (e.g., a slower onset of central pharmacodynamic effects) result in a lower abuse potential (de Wit et al., 1993; Abreu et al., 2001; Roset et al., 2001). Interestingly, however, the abuse liability of OxyContin® as prescribed, has not been characterized experimentally. Although abuse of the intact tablet occurs, drug abusers often tamper with these types of formulations to circumvent their controlled-release properties, thereby converting them into high-dose, immediate-release preparations providing for the self-administration of the entire dose and the opportunity to use an alternate route of administration (Zacny et al., 2003).
The approach of adding an antagonist to an agonist as an abuse deterrent has been used for several medications (e.g., pentazocine, tilidine, methadone, buprenorphine) and has been studied using the standard approach of measuring subjective responses, as well as self-administration procedures. For example, Suboxone® (sublingual tablets containing buprenorphine combined with naloxone) was primarily developed because of concerns about parenteral abuse of Subutex® (sublingual tablets containing buprenorphine). Given the low sublingual bioavailability, but high parenteral bioavailability of naloxone, this approach is primarily intended to deter intravenous and potentially intranasal abuse of buprenorphine. Weinhold and colleagues (1992) compared the effects of intramuscular administration of buprenorphine alone and buprenorphine in combination with naloxone in non-opioid-dependent individuals who abuse heroin. The buprenorphine and naloxone in combination reduced subjective and physiological effects, relative to buprenorphine alone, suggesting that the combination would have lower abuse liability. A subsequent study conducted in recently-detoxified, non-opioid-dependent heroin abusers also showed that the subjective effects of parenteral (in this case, intravenous) buprenorphine and buprenorphine in combination with naloxone differed significantly (Comer et al., 2002). However, the reinforcing effects, as assessed by self-administration, of buprenorphine alone compared to the combination did not differ in this study because both were able to alleviate some lingering, mild opioid withdrawal symptoms. Overall, these studies suggest that buprenorphine in combination with naloxone may have reduced abuse potential compared to buprenorphine alone in non-dependent heroin abusers in the absence of withdrawal symptomatology.
In individuals who are physically dependent on short-acting opioids, parenteral abuse of the buprenorphine/naloxone combination is likely to be low because it induces opioid withdrawal symptoms. For example, Stoller and colleagues (2001) reported that intramuscular administration of the buprenorphine/naloxone combination precipitated opioid withdrawal symptoms in individuals maintained on orally delivered hydromorphone. Interestingly, several positive subjective ratings (“High,” “Good Effects,” “Liking”) increased at intermediate doses of buprenorphine/naloxone, but these effects were not significantly different from placebo. Intramuscular administration of buprenorphine alone did produce significant increases in positive subjective responses under these experimental conditions. Mendelson and colleagues (1999) further reported that intravenous administration of buprenorphine to morphine-maintained individuals produced opioid agonist-like subjective effects and did not precipitate opioid withdrawal, while the buprenorphine/naloxone combination precipitated opioid withdrawal symptoms. Direct comparisons of the reinforcing effects of buprenorphine alone compared to the buprenorphine/naloxone combination in individuals who are physically dependent on short-acting opioids have not yet been conducted. Given the recent data showing that i.v. buprenorphine alone had no reinforcing effects in morphine-maintained individuals (Comer et al., in press) and the intriguing data with buprenorphine/naloxone in the study by Stoller and colleagues (2001), such a study would be quite informative.
Abuse deterrent formulations that rely on the physical characteristics of the formulation, rather than its pharmacological profile of action, present an interesting challenge for both human and animal abuse liability testing. ADFs that alter the mechanical stability of tablets are designed to prevent abuse via tampering with the intact tablets. As with the vast majority of ADFs under development, these “tamper-resistant” products represent reformulations of currently marketed compounds (e.g., oxycodone, morphine), the abuse liability profiles of which are usually well established. Most of these reformulations are designed to provide a controlled and slow release of medication. Simple measurements of subjective responses after administration of the intact tablets can be made, but may not provide a valid assessment of the effectiveness of the tamper-resistant mechanism. Measurements of subjective responses after administration of crushed tablets that are provided by the investigators also may be insufficient because the abuse liability of the medication contained within the crushed tablets typically is already known. In this interesting situation, the crucial variable that needs to be assessed is the success of the tamper-resistant mechanism. That is, participants need to be given the opportunity to tamper with the ADF tablet and assessments need to be made of how difficult it is to extract the medication. Drug self-administration procedures would be particularly useful complements to subjective effects testing in examining the abuse liabilities of novel formulations that use mechanical barriers to deter abuse.
In addition to pharmacokinetic studies and safety evaluations related to the excipients contained in the new formulation, selecting the appropriate model to investigate the formulation’s potential effect on abuse liability will largely be guided by the results of bench-top testing (e.g., testing the ability of the tablet to withstand heating, freezing, crushing, extractability in common solvents, etc.), the abuse liability of the active compound, and knowledge of the patterns of abuse and/or tampering of the currently marketed formulation (Grudzinskas et al., 2006; Katz et al., 2007; Wright et al., 2006). In addition, it may be advisable, when feasible, to conduct a study for each type of potential abuser relevant to the test compound. For instance, some abusers chew controlled-release tablets, while others snort the crushed powder or inject an extracted solution from the tablet. Three separate abuse liability studies with different subject populations (chewers, snorters, injectors) would be needed in this case to obtain a comprehensive picture of the abuse liability and bioavailability of the compound when administered by each route. The development of several different types of abuse deterrent formulations highlights the challenges presented to investigators, pharmaceutical companies, and federal regulatory agencies in assessing abuse liability, and, for some formulations, underscores the need for measurements of both drug-taking behavior and subjective responses.
6.0 Conclusions
As reviewed above, drug self-administration paradigms have been used for decades to examine the abuse liability of psychoactive drugs in infrahuman and, to a lesser extent, human studies. There is generally good concordance between those drugs that are self-administered in laboratory settings and those that are abused in the natural environment. Similarly, medications effective at reducing drug self-administration in the laboratory generally reduce drug use in clinical settings. The opioid system in particular is an outstanding example of the sensitivity and validity of the model. Under most conditions, good concordance is found between the reinforcing and subjective effects of drugs. However, this relationship is not always straightforward. On the one hand, a large number of variables are known to affect drug taking behavior, including the presence of competing reinforcers, the cost of the drug, the state of physical dependence, and the behavioral demands placed upon individuals after drug self-administration occurs. Unless carefully controlled in the experimental design, these variables can make interpretations of the reinforcing effects of drugs difficult. On the other hand, assessing the abuse liability of drugs based solely upon subjective effects questionnaires also can be difficult, especially when a mixed profile of both positive and negative subjective effects are produced or when drug interactions are under study in which both agents produce direct effects on mood, as can occur in the case of medications development studies. Obtaining data in both domains is especially important under certain circumstances, such as when examining the abuse liability of medications that are designed specifically to reduce illicit use and diversion. For practical reasons, assessment of some abuse deterrent formulations may not lend themselves to sole reliance on subjective effect outcomes. The challenge in assessing these newer formulations will be to design studies that will provide the most valid and reliable data. In summary, concurrent assessment of direct subjective effects along with drug taking behavior should yield a more comprehensive picture than either approach when used alone, and, as illustrated above, can often clarify the underlying reasons for the observed changes in behavior and, thus, inform clinical utility and practice.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abreu ME, Bigelow GE, Fleisher L, Walsh SL. Effect of intravenous injection speed on responses to cocaine and hydromorphone in humans. Psychopharmacol. 2001;154:76–84. doi: 10.1007/s002130000624. [DOI] [PubMed] [Google Scholar]
- Altman JL, Meyer RE, Mirin SM, McNamee, McDougle HB. Opiate antagonists and the modification of heroin self-administration behavior in man: An experimental study. Int. J. Addict. 1976;11:485–499. doi: 10.3109/10826087609056165. [DOI] [PubMed] [Google Scholar]
- Amass L, Bickel WK, Crean JP, Blake J, Higgins ST. Alternate-day buprenorphine dosing is preferred to daily dosing by opioid-dependent humans. Psychopharmacol. 1998;136:217–225. doi: 10.1007/s002130050559. [DOI] [PubMed] [Google Scholar]
- Amass L, Kamien JB, Rieber C, Branstetter SA. Abuse liability of i.v. buprenorphine-naloxone, buprenorphine, and hydromorphone in buprenorphine-naloxone maintained volunteers. Drug Alcohol Depend. 2000;60 Suppl 1:S6–S7. [Google Scholar]
- Arnold JM, Roberts DCS. A critique of fixed and progressive ratio schedules used to examine the neural substrates of drug reinforcement. Pharmacol. Biochem. Behav. 1997;57(3):441–447. doi: 10.1016/s0091-3057(96)00445-5. [DOI] [PubMed] [Google Scholar]
- Ator NA, Griffiths RR. Principles of drug abuse liability assessment in laboratory animals. Drug Alcohol Depend. 2003;70:S55–S72. doi: 10.1016/s0376-8716(03)00099-1. [DOI] [PubMed] [Google Scholar]
- Balster RL, Bigelow GE. Guidelines and methodological reviews concerning drug abuse liability assessment. Drug Alcohol Depend. 2003;70:S13–S40. doi: 10.1016/s0376-8716(03)00097-8. [DOI] [PubMed] [Google Scholar]
- Barrett AC, Negus SS, Mello NK, Caine SB. Effect of GABA agonists and GABA-A receptor modulators on cocaine- and food-maintained responding and cocaine discrimination in rats. J. Pharmacol. Exp. Ther. 2005;315:858–871. doi: 10.1124/jpet.105.086033. [DOI] [PubMed] [Google Scholar]
- Bigelow G, Griffiths R, Liebson I. Experimental human drug self-administration: Methodology and application to the study of sedative abuse. Pharmcol. Reviews. 1976;27(4):523–531. [PubMed] [Google Scholar]
- Collins ED, Vosburg SK, Ward AS, Haney M, Foltin RW. Memantine increases cardiovascular but not behavioral effects of cocaine in methadone-maintained humans. Pharmacol. Biochem. Behav. 2006;83(1):47–55. doi: 10.1016/j.pbb.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Comer SD, Ashworth JB. The growth of prescription opioid abuse. In: Passik S, editor. Pain and Chemical Dependency. In press. [Google Scholar]
- Comer SD, Collins ED. Self-administration of intravenous buprenorphine and the buprenorphine/naloxone combination by recently detoxified heroin abusers. J. Pharmacol. Exp. Ther. 2002;303:694–703. doi: 10.1124/jpet.102.038141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer SD, Collins ED, Fischman MW. Buprenorphine sublingual tablets: effects on IV heroin self-administration by humans. Psychopharmacol. 2001;154:28–37. doi: 10.1007/s002130000623. [DOI] [PubMed] [Google Scholar]
- Comer SD, Collins ED, Fischman MW. Intravenous buprenorphine self-administration by detoxified heroin abusers. J. Pharmacol. Exp. Ther. 2002;301:266–276. doi: 10.1124/jpet.301.1.266. [DOI] [PubMed] [Google Scholar]
- Comer SD, Collins ED, Kleber HD, Nuwayser ES, Kerrigan JH, Fischman MW. Depot naltrexone: Long-lasting antagonism of the effects of heroin in humans. Psychopharmacol. 2002;159:351–360. doi: 10.1007/s002130100909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer SD, Sullivan MA, Walker EA. Comparison of intravenous buprenorphine and methadone self-administration by recently detoxified heroindependent individuals. J. Pharmacol. Exp. Ther. 2005;315:1320–1330. doi: 10.1124/jpet.105.090423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer SD, Sullivan MA, Whittington RA, Vosburg SK, Kowalczyk WJ. Abuse liability of prescription opioids compared to heroin in morphine-maintained heroin abusers. Neuropsychopharmacol. 2007 doi: 10.1038/sj.npp.1301479. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer SD, Walker EA, Collins ED. Buprenorphine/naloxone reduces the reinforcing and subjective effects of heroin in heroin-dependent volunteers. Psychopharmacol. 2005;181:664–675. doi: 10.1007/s00213-005-0023-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer SD, Zacny JP. Subjective effects of opioids. In: Earleywine M, editor. Mind-altering drugs: The science of subjective experience. New York: Oxford University Press; 2005. pp. 217–239. [Google Scholar]
- Cone EJ. Ephemeral profiles of prescription drug and formulation tampering: Evolving pseudoscience on the Internet. Drug Alcohol Depend. 2006;83 Suppl 1:S31–S39. doi: 10.1016/j.drugalcdep.2005.11.027. [DOI] [PubMed] [Google Scholar]
- Dackis CA, Kampman KM, Lynch KG, Pettinati HM, O’Brien CP. A double-blind, placebo-controlled trial of modafinil for cocaine dependence. Neuropsychopharmacol. 2005;30:205–211. doi: 10.1038/sj.npp.1300600. [DOI] [PubMed] [Google Scholar]
- Deneau GE, Yanagita T, Seevers M. Self-administration of psychoactive substances by the monkey – A measure of psychological dependence. Psychopharmacol. (Berl) 1969;16:30–48. doi: 10.1007/BF00405254. [DOI] [PubMed] [Google Scholar]
- de Wit H, Chutuape MA. Increased ethanol choice in social drinkers following ethanol preload. Behav. Pharmacol. 1993;4(1):29–36. [PubMed] [Google Scholar]
- de Wit H, Dudish S, Ambre J. Subjective and behavioral effects of diazepam depend on its rate of onset. Psychopharmacol. (Berl) 1993;112(2–3):324–330. doi: 10.1007/BF02244928. [DOI] [PubMed] [Google Scholar]
- Donny EC, Brasser SM, Bigelow GE, Stitzer ML, Walsh SL. Methadone doses of 100 mg or greater are more effective than lower doses at suppressing heroin self-administration in opioid-dependent volunteers. Addict. 2005;100:1496–1509. doi: 10.1111/j.1360-0443.2005.01232.x. [DOI] [PubMed] [Google Scholar]
- Evans SM, Walsh SL, Levin FR, Foltin RW, Fischman MW, Bigelow GE. The effects of flupenthixol on the subjective and cardiovascular effects of intravenous cocaine in humans. Drug Alcohol Depend. 2001;64:271–283. doi: 10.1016/s0376-8716(01)00129-6. [DOI] [PubMed] [Google Scholar]
- Faggiano F, Vigna-Taglianti F, Versino E, Lemma P. Methadone maintenance at different dosages for opioid dependence. Cochrane Database System Rev. 2003;(3) doi: 10.1002/14651858.CD002208. CD002208. [DOI] [PubMed] [Google Scholar]
- Filip M, Frankowska M, Przegalinski E. Effects of GABAB receptor antagonist, agonists and allosteric positive modulator on the cocaine-induced self-administration and drug discrimination. Eur. J. Pharmacol. 2007;574:148–157. doi: 10.1016/j.ejphar.2007.07.048. [DOI] [PubMed] [Google Scholar]
- Fischman MW, Foltin RW, Nestadt G, Pearlson GD. Effects of desipramine maintenance on cocaine self-administration by humans. J. Pharmacol. Exp. Ther. 1990;253(2):760–770. [PubMed] [Google Scholar]
- Foltin RW, Fischman MW. Assessment of abuse liability of stimulant drugs in humans: A methodological survey. Drug Alcohol Depend. 1991;28:3–48. doi: 10.1016/0376-8716(91)90052-z. [DOI] [PubMed] [Google Scholar]
- Foltin RW, Fischman MW. Effects of buprenorphine on the self-administration of cocaine by humans. Behav. Pharmacol. 1994;5:78–89. doi: 10.1097/00008877-199402000-00009. [DOI] [PubMed] [Google Scholar]
- Gorski TT. [Accessed July 9, 2007];Oxycontin—Manufacturer plans for a safer pain medication. 2002 http://www.tgorski.com/drug_updates/OxyContin - Manufactures Plan For A Safer Pain Medication 010808.htm.
- Greenwald MK, Johanson CE, Schuster CR. Opioid reinforcement in heroin-dependent volunteers during outpatient buprenorphine maintenance. Drug Alcohol Depend. 1999;56:191–203. doi: 10.1016/s0376-8716(99)00032-0. [DOI] [PubMed] [Google Scholar]
- Greenwald MK, Schuh KJ, Hopper JA, Schuster CR, Johanson CE. Effects of buprenorphine sublingual tablet maintenance on opioid drug-seeking behavior by humans. Psychopharmacol. 2002;160:344–352. doi: 10.1007/s00213-001-0975-0. [DOI] [PubMed] [Google Scholar]
- Griffiths RR, Bigelow GE, Ator NA. Principles of initial experimental drug abuse liability assessment in humans. Drug Alcohol Depend. 2003;70:S41–S54. doi: 10.1016/s0376-8716(03)00098-x. [DOI] [PubMed] [Google Scholar]
- Griffiths RR, Bigelow GE, Liebson IA. Facilitation of human tobacco self-administration by ethanol: A behavioral analysis. J. Exp. Anal. Behav. 1976;25:279–292. doi: 10.1901/jeab.1976.25-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths RR, Bigelow GE, Liebson IA, Kaliszak JE. Drug preference in humans: Double-blind choice comparison of pentobarbital, diazepam, and placebo. J. Pharmacol. Exp. Ther. 1980;215(3):649–661. [PubMed] [Google Scholar]
- Griffiths RR, Bigelow GE, Liebson IA. Human coffee drinking: Reinforcing and physical dependence producing effects of caffeine. J. Pharmacol. Exp. Ther. 1986;239:416–425. [PubMed] [Google Scholar]
- Griffiths RR, Troisi JR, Silverman K, Mumford GK. Multiple-choice procedure: An efficient approach for investigating drug reinforcement in humans. Behav. Pharmacol. 1993;4:3–13. [PubMed] [Google Scholar]
- Grudzinskas C, Balster RL, Gorodetzky CW, Griffiths RR, Henningfield JE, Johanson CE, Mansbach RS, McCormick CG, Schnoll SH, Strain EC, Wright C. Impact of formulation on the abuse liability, safety and regulation of medications: The expert panel. Drug Alcohol Depend. 2006;83S:S77–S82. doi: 10.1016/j.drugalcdep.2006.02.008. [DOI] [PubMed] [Google Scholar]
- Haney M, Collins ED, Ward AS, Foltin RW, Fischman MW. Effect of a selective dopamine D1 agonist (ABT-431) on smoked cocaine self-administration in humans. Psychopharmacol. 1999;143:102–110. doi: 10.1007/s002130050925. [DOI] [PubMed] [Google Scholar]
- Haney M, Foltin RW, Fischman MW. Effects of pergolide on intravenous cocaine self-administration in men and women. Psychopharmacol. 1998;137:15–24. doi: 10.1007/s002130050588. [DOI] [PubMed] [Google Scholar]
- Haney M, Hart CL, Foltin RW. Effects of baclofen on cocaine self-administration: Opioid- and nonopioid-dependent volunteers. Neuropsychopharmacol. 2006;31(8):1814–1821. doi: 10.1038/sj.npp.1300999. [DOI] [PubMed] [Google Scholar]
- Haney M, Spealman R. Controversies in translational research: Drug self-administration. Psychopharmacol. 2008 doi: 10.1007/s00213-008-1079-x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haney M, Ward AS, Foltin RW, Fischman MW. Effects of ecopipam, a selective D1 antagonist, on smoke cocaine self-administration by humans. Psychopharmacol. 2001;155:330–337. doi: 10.1007/s002130100725. [DOI] [PubMed] [Google Scholar]
- Hart CL, Haney M, Vosburg SK, Rubin E, Foltin RW. Smoked cocaine self-administration is decreased by modafinil. Neuropsychopharmacol. 2008;33:761–768. doi: 10.1038/sj.npp.1301472. [DOI] [PubMed] [Google Scholar]
- Hart CL, Ward AS, Collins ED, Haney M, Foltin RW. Gabapentin maintenance decreases smoked cocaine-related subjective effects, but not self-administration by humans. Drug Alcohol Depend. 2004;73:279–287. doi: 10.1016/j.drugalcdep.2003.10.015. [DOI] [PubMed] [Google Scholar]
- Heins J. [Accessed July 9, 2007];Purdue Pharma provides update on development of new abuse-resistant pain medications—FDA cites patient needs as first priority, New Drug Application delayed. 2002 http://www.purduepharma.com/pressroom/news/oxycontinnews/20020618.htm.
- Henningfield JE, Cohen C, Heishman SJ. Drug self-administration methods in abuse liability evaluation. Brit. J. Addict. 1991;86:1571–1577. doi: 10.1111/j.1360-0443.1991.tb01750.x. [DOI] [PubMed] [Google Scholar]
- Henningfield JE, Goldberg SR. Control of behavior by intravenous nicotine injections in human subjects. Pharmacol. Biochem. Behav. 1983;19:1021–1026. doi: 10.1016/0091-3057(83)90409-4. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Bickel WT, Hughes JR. Influence of an alternative reinforcer on human cocaine self-administration. Life Sci. 1994;55(3):179–187. doi: 10.1016/0024-3205(94)00878-7. [DOI] [PubMed] [Google Scholar]
- Hodos W. Progressive-ratio as a measure of reward strength. Science. 1961;134:943–944. doi: 10.1126/science.134.3483.943. [DOI] [PubMed] [Google Scholar]
- Hodos W, Kalman G. Effects of increment size and reinforcer volume on progressive-ratio performance. J. Exp. Anal. Behav. 1963;6:387–392. doi: 10.1901/jeab.1963.6-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe JH, Jaffe FK. Historical perspectives on the use of subjective effects measures in assessing abuse potential of drugs. In: Fischman MW, Mello NK, editors. Testing for abuse liability of drugs in humans. NIDA Research Monograph Series No. 92. Rockville, MD: Department of Health and Human Services, National Institute on Drug Abuse; 1989. pp. 163–174. [Google Scholar]
- Jasinski DR, Pevnick JS, Griffith JD. Human pharmacology and abuse potential of the analgesic buprenorphine. Arch. Gen. Psychiatry. 1978;35:01–516. doi: 10.1001/archpsyc.1978.01770280111012. [DOI] [PubMed] [Google Scholar]
- Johanson CE, Uhlenhuth EH. Drug preference and mood in humans: diazepam. Psychopharmacol. 1980a;71(3):269–273. doi: 10.1007/BF00433061. [DOI] [PubMed] [Google Scholar]
- Johanson CE, Uhlenhuth EH. Drug preference and mood in humans: d-amphetamine. Psychopharmacol. 1980b;71(3):275–279. doi: 10.1007/BF00433062. [DOI] [PubMed] [Google Scholar]
- Johnson RE, Jaffe JH, Fudala PJ. A controlled trial of buprenorphine treatment for opioid dependence. JAMA. 1992;267:2750–2755. [PubMed] [Google Scholar]
- Johnson F, Sun S, Stauffer J, Wagner G. (757)Morphine release profile in a formulation containing polymer-coated extended-release morphine sulfate plus sequestered naltrexone. J. Pain. 2007;8(4) suppl. 1:S40. [Google Scholar]
- Jones BE, Prada JA. Drug-seeking behavior during methadone maintenance. Psychopharmacol. 1975;41:7–10. doi: 10.1007/BF00421297. [DOI] [PubMed] [Google Scholar]
- Kampman KM, Pettinati H, Lynch KG, Sparkman T, O’Brien CP. A pilot trial of olanzapine for the treatment of cocaine dependence. Drug Alcohol Depend. 2003;70:265–273. doi: 10.1016/s0376-8716(03)00009-7. [DOI] [PubMed] [Google Scholar]
- Katz JL. Models of relative reinforcing efficacy of drugs and their predictive utility. Behav. Pharmacol. 1990;1(4):283–301. doi: 10.1097/00008877-199000140-00003. [DOI] [PubMed] [Google Scholar]
- Katz NP, Adams EH, Chilcoat H, Colucci RD, Comer SD, Goliber P, Grudzinskas C, Jasinski D, Lande SD, Passik SD, Schnoll SH, Sellers E, Travers D, Weiss R. Challenges in the development of prescription opioid abuse-deterrent formulations. Clin. J. Pain. 2007;23(8):648–660. doi: 10.1097/AJP.0b013e318125c5e8. [DOI] [PubMed] [Google Scholar]
- Kirchmayer U, Davoli M, Verster A, Amato L, Feri M, Perucci CA. A systematic review on the efficacy of naltrexone maintenance treatment in opioid ependence. Addiction. 2002;97:1241–1249. doi: 10.1046/j.1360-0443.2002.00217.x. [DOI] [PubMed] [Google Scholar]
- Kleven MS, Woolverton WL. Effects of continuous infusions of SCH 23390 on cocaine- or food-maintained behavior in rhesus monkeys. Behav. Pharmacol. 1990;1:365–373. doi: 10.1097/00008877-199000140-00010. [DOI] [PubMed] [Google Scholar]
- Lamb RJ, Preston KL, Schindler CW, Meisch RA, Davis F, Katz JL, Henningfield JE, Goldberg SR. The reinforcing and subjective effects of morphine in post-addicts: a dose-response study. J. Pharmacol. Exp. Ther. 1991;259:1165–1173. [PubMed] [Google Scholar]
- Liguori A, Hughes JR, Oliveto AH. Caffeine self-administration in humans: 1. Efficacy of cola vehicle. Exp. Clin. Psychopharmacol. 1997;5(3):286–294. doi: 10.1037//1064-1297.5.3.286. [DOI] [PubMed] [Google Scholar]
- Lile JA, Stoops WW, Allen TS, Glaser PEA, Hays LR, Rush CR. Baclofen does not alter the reinforcing, subject-rated or cardiovascular effects of intranasal cocaine in humans. Psychopharmacol. 2007;171:441–449. doi: 10.1007/s00213-003-1598-4. [DOI] [PubMed] [Google Scholar]
- Lile JA, Stoops WW, Glaser PEA, Hays LR, Rush CR. Acute administration of the GABA reuptake inhibitor tiagabine does not alter the effects of oral cocaine in humans. Drug Alcohol Depend. 2004;76(1):81–91. doi: 10.1016/j.drugalcdep.2004.04.010. [DOI] [PubMed] [Google Scholar]
- Ling W, Wesson DR. Clinical efficacy of buprenorphine: Comparison to methadone and placebo. Drug Alcohol Depend. 2003;70(2 Suppl):S49–S57. doi: 10.1016/s0376-8716(03)00059-0. [DOI] [PubMed] [Google Scholar]
- Little C, Correia CJ. Use of a multiple-choice procedure with college student drinkers. Psychol. Addict. Behav. 2006;20(4):445–452. doi: 10.1037/0893-164X.20.4.445. [DOI] [PubMed] [Google Scholar]
- Madras BK, Xie Z, Lin Z, Jassen A, Panas H, Lynch L, Johnson R, Livni E, Spencer TJ, Bonab AA, Miller GM, Fischman AJ. Modafinil occupies dopamine and norepinephrine transporters in vivo and modulates the transporters and trace amine activity in vitro. J. Pharmacol. Exp. Ther. 2006;319:561–569. doi: 10.1124/jpet.106.106583. [DOI] [PubMed] [Google Scholar]
- Martinez D, Broft A, Foltin RW, Slifstein M, Hwang D-R, Huang Y, Perez A, Frankel WG, Cooper T, Kleber HD, Fischman MW, Laruelle M. Cocaine dependence and D2 receptor availability in the functional subdivisions of the striatum: Relationship with cocaine-seeking behavior. Neuropsychopharmacol. 2004;29(6):1190–1202. doi: 10.1038/sj.npp.1300420. [DOI] [PubMed] [Google Scholar]
- McColl S, Sellers EM. Research design strategies to evaluate the impact of formulations on abuse liability. Drug Alcohol Depend. 2006;83S:S52–S62. doi: 10.1016/j.drugalcdep.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Mello NK, Mendelson JH. Buprenorphine suppresses heroin use by heroin addicts. Science. 1980;207:657–659. doi: 10.1126/science.7352279. [DOI] [PubMed] [Google Scholar]
- Mello NK, Mendelson JH, Kuehnle JC, Sellers MS. Operant analysis of human heroin self-administration and the effects of naltrexone. J. Pharmacol. Exp. Ther. 1981;216:45–54. [PubMed] [Google Scholar]
- Mello NK, Mendelson JH, Kuehnle JC. Buprenorphine effects on human heroin self-administration: An operant analysis. J. Pharmacol. Exp. Ther. 1982;223:30–39. [PubMed] [Google Scholar]
- Mendelson JH, Mello NK. Experimental analysis of drinking behavior of chronic alcoholics. Ann. New York Acad. Sci. 1966;133:828–845. doi: 10.1111/j.1749-6632.1966.tb50930.x. [DOI] [PubMed] [Google Scholar]
- Meyer RE, McNamee HB, Mirin SM, Altman JL. Analysis and modification of opiate reinforcement. Int. J. Addict. 1976;11:467–484. doi: 10.3109/10826087609056164. [DOI] [PubMed] [Google Scholar]
- Mooney M, Green C, Hatsukami D. Nicotine self-administration: Cigarette versus nicotine gum diurnal topography. Hum. Psychopharmacol. Clin. Exp. 2006;21:539–548. doi: 10.1002/hup.808. [DOI] [PubMed] [Google Scholar]
- Nann-Vernotica E, Donny EC, Bigelow GE, Walsh SL. The D1/5 antagonist, ecopipam, fails to attenuate the subjective and physiological effects of cocaine. Psychopharmacol. 2001;155:338–347. doi: 10.1007/s002130100724. [DOI] [PubMed] [Google Scholar]
- O’Brien CP, Gardner EL. Critical assessment of how to study addiction and its treatment: Human and non-human animal models. Pharmacol. Ther. 2005;108:18–58. doi: 10.1016/j.pharmthera.2005.06.018. [DOI] [PubMed] [Google Scholar]
- Panlilio LV, Goldberg SR. Self-administration of drugs in animals and humans as a model and an investigative tool. Addiction. 2007;102:1863–1870. doi: 10.1111/j.1360-0443.2007.02011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Bickel WK. Buprenorphine dose self-selection: Effects of an alternative reinforcer, behavioral economic analysis of demand and examination of subjective drug effects. Exp. Clin. Psychopharmacol. 1999;7:38–48. doi: 10.1037//1064-1297.7.1.38. [DOI] [PubMed] [Google Scholar]
- Preston KL, Jasinski DR. Abuse liability studies of opioid agonist-antagonists in humans. Drug Alcohol Depend. 1991;28:49–82. doi: 10.1016/0376-8716(91)90053-2. [DOI] [PubMed] [Google Scholar]
- Preston KL, Walsh SL. Evaluating abuse liability: Methods and predictive value. In: Karch SB, editor. Drug Abuse Handbook. Boca Raton, Florida: CRC Press; 1998. pp. 276–306. [Google Scholar]
- Richter KP, Hamilton AK, Hall S, Catley D, Cox LS, Grobe J. Patterns of smoking and methadone dose in drug treatment patients. Exp. Clin. Psychopharmacol. 2007;15:144–153. doi: 10.1037/1064-1297.15.2.144. [DOI] [PubMed] [Google Scholar]
- Roehrs T, Pedrosi B, Rosenthal L, Zorick F, Roth T. Hypnotic self-administration: Forced-choice versus single-choice. Psychopharmacol. 1997;133:121–126. doi: 10.1007/s002130050381. [DOI] [PubMed] [Google Scholar]
- Roset PN, Farre N, de la Torre R, Mas M, Menoyo E, Hernandez C, Cami J. Modulation of rate of onset and intensity of drug effects reduces abuse potential in healthy males. Drug Alcohol Depend. 2001;64(3):285–298. doi: 10.1016/s0376-8716(01)00127-2. [DOI] [PubMed] [Google Scholar]
- Rowlett JK. A labor-supply analysis of cocaine self-administration under progressive-ratio schedules: Antecedents, methodologies, and perspectives. Psychopharmacol. 2000;153:1–16. doi: 10.1007/s002130000610. [DOI] [PubMed] [Google Scholar]
- Rukstalis M, Jepson C, Strasser A, Lynch KG, Perkins K, Patterson F, Lerman C. Naltrexone reduces the relative reinforcing value of nicotine in a cigarette smoking choice paradigm. Psychopharmacol. 2005;180(1):41–48. doi: 10.1007/s00213-004-2136-8. [DOI] [PubMed] [Google Scholar]
- Schuster CR. Drugs as reinforcers in monkeys and man. Pharmacol. Reviews. 1976;27(4):511–521. [PubMed] [Google Scholar]
- Skinner BF. What is the experimental analysis of behavior? J. Exp. Anal. Behav. 1966;9:213–218. doi: 10.1901/jeab.1966.9-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofuoglu M, Pentel PR, Bliss RL, Goldman AI, Hatsukami DK. Effects of phenytoin on cocaine self-administration in humans. Drug Alcohol Depend. 1999;53(3):273–275. doi: 10.1016/s0376-8716(98)00140-9. [DOI] [PubMed] [Google Scholar]
- Spiga R, Schmitz J, Day J. Effects of nicotine on methadone self-administration in humans. Drug Alcohol Depend. 1998;50:157–165. doi: 10.1016/s0376-8716(98)00020-9. [DOI] [PubMed] [Google Scholar]
- Stafford D, LeSage MG, Glowa JR. Progressive-ratio schedules of drug delivery in the analysis of drug self-administration: A review. Psychopharmacol. 1998;139:169–184. doi: 10.1007/s002130050702. [DOI] [PubMed] [Google Scholar]
- Stern KN, Chait LD, Johanson CE. Reinforcing and subjective effects of oral tripelennamine in normal human volunteers. Behav. Pharmacol. 1989;1(2):161–167. [PubMed] [Google Scholar]
- Stitzer ML, McCaul ME, Bigelow GE, Liebson IA. Oral methadone self-administration: Effects of dose and alternative reinforcers. Clin. Pharmacol. Ther. 1983;34(1):29–35. doi: 10.1038/clpt.1983.124. [DOI] [PubMed] [Google Scholar]
- Stoller KB, Bigelow GE, Walsh SL, Strain EC. Effects of buprenorphine/naloxone in opioid-dependent humans. Psychopharmacol. 2001;154(3):230–242. doi: 10.1007/s002130000637. [DOI] [PubMed] [Google Scholar]
- Strain EC. Clinical use of buprenorphine. In: Stitzer M, Strain EC, editors. The Treatment of Opioid Dependence. Second Edition. Baltimore: The Johns Hopkins University Press; 2006. pp. 230–252. [Google Scholar]
- Strain EC, Bigelow GE, Liebson IA, Stitzer ML. Moderate- vs. high-dose methadone in the treatment of opioid dependence: A randomized trial. JAMA. 1999;281:1000–1005. doi: 10.1001/jama.281.11.1000. [DOI] [PubMed] [Google Scholar]
- Strain EC, Stoller KB, Walsh SL, Bigelow GE. Effects of buprenorphine versus buprenorphine/naloxone tablets in non-dependent opioid abusers. Psychopharmacol. 2000;148:374–383. doi: 10.1007/s002130050066. [DOI] [PubMed] [Google Scholar]
- Stoops WW, Vansickel AR, Lile JA, Rush CR. Acute d-amphetamine pretreatment does not alter stimulant self-administration in humans. Pharmacol. Biochem. Behav. 2007;87(1):20–29. doi: 10.1016/j.pbb.2007.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Office of Applied Studies. Rockville, MD: SAMHSA; Results from the 2003 National Survey on Drug Use and Health: National Findings (NSDUH Series H-25, DHHS Publication No. SMA 04-3964) 2004a
- Substance Abuse and Mental Health Services Administration (SAMHSA) Office of Applied Studies. Rockville, MD: SAMHSA; Results from the 2006 National Survey on Drug Use and Health: National Findings (NSDUH Series H-32, DHHS Publication No. SMA 07-4293) 2007a
- Substance Abuse and Mental Health Services Administration (SAMHSA) Office of Applied Studies. Rockville, MD: SAMHSA; Treatment Episode Data Set (TEDS): 1995–2005. National Admissions to Substance Abuse Treatment Services. (NSDUH Series S-37, DHHS Publication No. SMA 07-4234) 2007b
- Sullivan MA, Comer SD, Nunes E. Pharmacology and clinical use of naltrexone. In: Stitzer M, Strain EC, editors. The Treatment of Opioid Dependence. Second Edition. Baltimore: The Johns Hopkins University Press; 2005. pp. 295–320. [Google Scholar]
- Sullivan MA, Vosburg SK, Comer SD. Depot naltrexone: Antagonism of the reinforcing, subjective, and physiological effects of heroin. Psychopharmacol. 2006;189:37–46. doi: 10.1007/s00213-006-0509-x. [DOI] [PubMed] [Google Scholar]
- Tancer M, Johanson CE. Reinforcing, subjective and physiological effects of MDMA in humans: A comparison with d-amphetamine and mCPP. Drug Alcohol Depend. 2003;72(1):33–44. doi: 10.1016/s0376-8716(03)00172-8. [DOI] [PubMed] [Google Scholar]
- Tancer M, Johanson CE. The effects of fluoxetine on the subjective and physiological effects of 3,4-methylenedioxymethamphetamine (MDMA) in humans. Psychopharmacol. 2007;189:565–573. doi: 10.1007/s00213-006-0576-z. [DOI] [PubMed] [Google Scholar]
- Thompson T, Schuster CR. Morphine self-administration, food-reinforced and avoidance behaviors in rhesus monkeys. Psychopharmacol. 1964;5:87–94. doi: 10.1007/BF00413045. [DOI] [PubMed] [Google Scholar]
- Vocci FJ, Elkashef A. Pharmacotherapy and other treatments for cocaine abuse and dependence. Curr. Opin. Psychiat. 2005;18:265–270. doi: 10.1097/01.yco.0000165596.98552.02. [DOI] [PubMed] [Google Scholar]
- Walsh SL, Preston KL, Bigelow GE, Stitzer ML. Acute administration of buprenorphine in humans: Partial agonist and blockade effects. J. Pharmacol. Exp. Ther. 1995;274:361–372. [PubMed] [Google Scholar]
- Walsh SL, Sullivan JT, Preston KL, Garner JE, Bigelow GE. Effects of naltrexone on response to intravenous cocaine, hydromorphone, and their combination in humans. J. Pharmacol. Exp. Ther. 1996;279:524–538. [PubMed] [Google Scholar]
- Walsh SL, Eissenberg T. The clinical pharmacology of buprenorphine: Extrapolating from the laboratory to the clinic. Drug Alcohol Depend. 2003;70:S13–S27. doi: 10.1016/s0376-8716(03)00056-5. [DOI] [PubMed] [Google Scholar]
- Walsh SL, Geter-Douglas B, Strain EC, Bigelow GE. Enadoline and butorphanol: Evaluation of κ agonists on cocaine pharmacodynamics and cocaine self-administration in humans. J. Pharmacol. Exp. Ther. 2001;299:147–158. [PubMed] [Google Scholar]
- Weinhold LL, Preston KL, Farre M, Liebson IA, Bigelow GW. Buprenorphine alone and in combination with naloxone in non-dependent humans. Drug Alcohol Depend. 1992;30:263–274. doi: 10.1016/0376-8716(92)90061-g. [DOI] [PubMed] [Google Scholar]
- World Drug Report. United Nations Office on Drugs and Crime; Volume 1: Analysis. 2005:39–79. United Nations Publication Sales No. E.05.XI.10 ISBN 92-1-148200-3.
- Wright C, Kramer ED, Zalman MA, Smith MY, Haddox JD. Risk identification, risk assessment, and risk management of abusable drug formulations. Drug Alcohol Depend. 2006;83S:S68–S76. doi: 10.1016/j.drugalcdep.2005.12.012. [DOI] [PubMed] [Google Scholar]
- Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. College on Problems of Drug Dependence taskforce on prescription opioid non-medical use and abuse: Position statement. Drug Alcohol Depend. 2003;69:215–232. doi: 10.1016/s0376-8716(03)00003-6. [DOI] [PubMed] [Google Scholar]