Abstract
Objective We examined the role of parental monitoring (general and diabetes specific) on metabolic control through better adherence and lower externalizing behaviors for adolescents with type 1 diabetes. Methods Adolescents aged 10–14 (n = 252) completed assessments of general and diabetes-specific mothers’ and fathers’ monitoring, adherence, and the Youth Self Report (YSR). Glycosylated hemoglobin (HbA1c) indexed diabetes control. Results Path analyses revealed that perceived mothers’ general monitoring was indirectly associated with lower HbA1c through lower externalizing behaviors and higher adherence. Perceived fathers’ general monitoring was associated with HbA1c differently at the extremes: low fathers’ monitoring was associated with higher HbA1c through higher externalizing behaviors; high fathers’ monitoring was associated with HbA1c through higher adherence. Diabetes-specific monitoring was not associated with externalizing behaviors. Conclusion Perceived mothers’ and fathers’ general parental monitoring facilitates metabolic control through a similar process, with parental differences largely seen at the extremes.
Keywords: adolescents, diabetes, externalizing behaviors, fathers, monitoring, mothers.
Type 1 diabetes is a difficult disease for the family to manage, especially during adolescence (Anderson, Brackett, Ho, & Laffel, 2000), as adolescents experience changes in cognitive, emotional, autonomy, and physical development (Smetana, Campione-Barr, & Metzger, 2006). Diabetes is a source of stress for adolescents and parents (Beveridge, Berg, Wiebe, & Palmer, 2006; Mellin, Neumark-Stainzer, & Patterson, 2004) who must solve problems dealing with maintaining glycosolated hemoglobin (HbA1c) levels, a healthy diet, regular exercise, and managing diabetes while the adolescent is increasingly away from home. Despite the fact that the adolescent is able to perform more diabetes tasks independently and that parental involvement declines across adolescence (Palmer et al., 2004; Wysocki, Linshied, Taylor, Yeates, Hough, & Naglieri, 1996), active parental involvement remains beneficial to adherence and better metabolic control (Anderson et al., 2000; Wiebe et al., 2005). One way that parents may stay beneficially involved is through active monitoring of their adolescent's diabetes management (Berg et al., 2008; Ellis, Podolski, Frey, Naar-King, Wang, & Moltz, 2007; Ellis, Templin, Naar-King, & Frey, 2008).
Parental monitoring has recently been explored as a key way that parents may be involved to facilitate both adherence and metabolic control (Berg et al., 2008; Ellis et al., 2007). Parental monitoring involves regular contact with adolescents regarding their daily activities and knowledge about and supervision of those activities, and can be either specific to diabetes (e.g., when they took their insulin, did they check their blood glucose) or more general (e.g., who their friends are, where they are). One potential pathway whereby diabetes-specific parental monitoring may be associated with better HbA1c is that such monitoring enhances adherence (Ellis et al., 2007).
Parental monitoring may also be associated with better metabolic control by reducing the frequency of externalizing behaviors, which themselves relate to poorer diabetes outcomes (Bronte-Tinkew, Moore, & Carrano, 2006; DeKlyen, Speltz, & Greenberg, 1998; Ellis et al., 2008). Externalizing behaviors are marked by a broad array of behaviors including poor school performance, aggression (Arbona & Power, 2003; Williams & Kelly, 2005), delinquency, drug and alcohol abuse, and risky sexual behavior (DeKlyen et al., 1998). An extensive developmental literature indicates that externalizing behaviors are a risk for adolescent development, associated with extreme risk taking, dangerous behaviors, and poorer management of an adolescent's health (Arbona & Power, 2003; DeKlyen et al., 1998; Williams & Kelly, 2005). Some studies have indicated that externalizing behaviors are also associated with worse diabetes control (Bryden, Peveler, Stein, Neil, Mayou, & Dunger, 2001; Duke, Geffken, Lewin, Williams, Storch, & Silverstein, 2008; Holmes et al., 2006). Adolescents’ externalizing behaviors (e.g., aggression, rule-breaking behaviors) may hamper optimal adherence resulting in poorer metabolic control (Duke et al., 2008; Rueter & Conger, 1998). Thus, in the present study we explored models that examined whether the beneficial effects of parental monitoring on metabolic control were through increasing adherence and lowering the display of externalizing behaviors.
During adolescence, parents whose adolescents have diabetes must monitor not only the diabetes regimen, but also general domains of adolescent functioning (e.g., curfews, friends, school). There is some indication that these two realms of parental monitoring (diabetes specific and general monitoring) may operate differently for positive youth outcomes. For example, Ellis et al. (2007) found that only diabetes-specific monitoring predicted adherence and metabolic control, whereas general parental monitoring did not. In the case of the link between general externalizing behaviors and diabetes-specific outcomes (i.e., adherence and metabolic control), however, it is likely that both general and diabetes-specific monitoring may be important. An extensive literature supports the link between general monitoring and externalizing behaviors (Webb, Bray, Getz, & Adams, 2002), while diabetes-specific monitoring is associated with better adherence and metabolic control (Berg et al., 2008; Ellis et al., 2007). We examined general and diabetes-specific monitoring in models examining the link between externalizing behaviors and diabetes outcomes.
Much of the focus on parental involvement in diabetes management has been on the mother-child relationship because mothers are the primary caregiver (Quittner & DiGirolama, 1998; Seiffge-Krenke, 2002). However, fathers’ monitoring (Berg et al., 2008) and involvement (Wysocki & Gavin, 2006) are associated with adherence and metabolic control. Low father general monitoring may be especially important in the development of externalizing behaviors (Bronte-Tinkew et al., 2006; Williams & Kelly, 2005). For example, DeKlyen et al. (1998) found that the amount of time that fathers spent with their children, especially their sons, was related to lower risk of the development of externalizing behaviors. We found that fathers’ diabetes-specific monitoring was related to metabolic control over and above mothers’ monitoring (Berg et al., 2008). Diabetes-specific monitoring was particularly related to metabolic control when fathers displayed low levels of monitoring, suggestive of a quadratic, as opposed to a simple linear association. Thus, we examined fathers’ and mothers’ monitoring in understanding adherence, externalizing behaviors, and metabolic control.
The purpose of the study was to compare various statistical models that examine whether parental monitoring (general or diabetes-specific) is associated with better metabolic control through better adherence and lower externalizing behaviors. We predicted that both diabetes-specific and general parental monitoring would be associated with better HbA1c both directly as well as indirectly through better adherence and lower externalizing behaviors.
Method
Participants
The study was approved by the appropriate institutional review board. Parents gave written informed consent and adolescents gave written assent. Participants included 252 adolescents (M = 12.49 years, SD = 1.53, 53.6% females) diagnosed with type 1 diabetes mellitus, their mothers (M = 39.64 years, SD = 6.34) and 188 fathers (M = 42.08 years, SD = 6.32) recruited from a university/private partnership clinic (76%) and a community-based private practice (24%), that followed similar treatment regimens and clinic procedures. Eligibility criteria included that adolescents were between 10 and 14 years of age, had diabetes more than 1 year (M = 4.13 years, SD = 3), and were able to read and write either English or Spanish. For each adolescent, one mother and one father were eligible to participate. Adolescents were required to be living with their participating mother because a major goal of the larger project is to model changes in mother–child relationships over time. Step-mothers or adopted mothers (3.2%) were eligible if they had lived with the adolescent for at least 1 year. To ensure that fathers’ involvement in diabetes management was represented, fathers of participating children were actively recruited, with most agreeing to participate (74.6%). If both a biological father and a step-father or adopted father were eligible for participation, we recruited the father that adolescents reported was most involved in their diabetes management. Most (74.6%) participating fathers were biological, with the remainder being step-fathers or adoptive fathers.
Approximately half (50.8%) of adolescents were on an insulin pump, with the remainder prescribed multiple daily injections (MDI). Mothers of adolescents on MDI reported physicians recommended an average of 4.14 insulin injections (SD = 1.81, range 0–10) and 5.53 blood glucose checks per day (SD = 1.70, range 1–11).
Of the qualifying individuals approached, 66% agreed to participate in the study, the first wave of a 3-year longitudinal study (the most common reasons for refusal included distance of commute 18%, too busy 21%, not interested 30%, uncomfortable with being studied 14%, and too much of a time commitment 5%). Comparisons of eligible adolescents who participated versus those who did not indicated that participants versus non-participants were older [12.5 vs. 11.6, t (367) = 6.2, p<.01, η2 = .10] but did not differ on gender, pump status, HbA1c or time since diagnosis (p-values >.20). Families were largely Caucasian (94%) and middle class with most (73%) reporting household incomes averaging $50,000 or more annually, 51% of mothers and 58% of fathers reporting education levels of associate's (2-year college) degrees or beyond, and an average Hollingshead Index value of 42.04, indicating the sample was on average medium business, minor professional, technical status.
Measures
Metabolic Control
As part of the routine clinic visit, children's glycosylated hemoglobin (HbA1c) levels were obtained (lower levels reflect better metabolic control). At all sites, HbA1c was obtained using the Bayer DCA2000 by clinic staff. Participant authorization provided access to children's medical records to obtain HbA1c and other illness information (e.g., duration of diabetes, pump vs. nonpump treatment, etc.).
Adherence
Adolescents independently completed a 16-item Self Care Inventory (adapted from La Greca, Auslander, Greco, Spetter, Fisher, & Santiago, 1995) to assess adherence to the diabetes regimen over the preceding month (1 = never to 5 = always did this as recommended without fail). The tool was adapted so that items were added that reflected current standards of diabetes care with the assistance of a certified diabetes educator (e.g., calculating insulin doses based on carbohydrate content of meals or snacks). Total scores on this scale have good internal consistency (α = .85 in our sample) and correlate well with more time-intensive interview methods for measuring adherence (La Greca et al., 1995). The mean adherence values are comparable to others using La Greca et al.'s (1995) measure.
Parental Monitoring of Management
Adolescents completed a scale of general parental monitoring (Barber, 1996), which shows excellent reliability and external validity (Brown, Mounts, Lamborn, & Steinberg, 1993), predicting an array of positive behaviors (higher academic achievement, less drug use, more self-reliance). This scale consisted of five items to capture adolescents’ views of their parents’ awareness of their daily activities. Adolescents reported how much mothers and fathers “really” know about different aspects of the child's life (e.g., where they go after school, how they spend their money, who their friends are) using a 1 (doesn’t know) to 5 (knows everything) scale. The scale showed excellent reliability for adolescent report of mother (α = .80) and father monitoring (α = .85).
Adolescents also completed a diabetes specific scale of parental monitoring developed by the authors (Berg et al., 2008). This measure was based on the general parental monitoring scale. This scale consisted of six items to capture adolescents’ views of their parents’ awareness of their diabetes care behaviors. Adolescents reported how much mothers and fathers “really” know about different aspects of the diabetes care (e.g., blood sugar readings; how much insulin has been taken) using a 1 (doesn’t know) to 5 (knows everything) scale. The scale showed excellent reliability for adolescent report of mother (α = .90) and father monitoring (α = .91).
Externalizing Behaviors
Adolescents completed the Youth-Self Report (YSR, Achenbach 1991) from which questions regarding rule-breaking and aggressive behaviors were answered (15 rule-breaking questions and 17 aggressive behavior questions). The rule-breaking scale consisted of the sum of items that dealt with the violation of rules or laws (e.g., I lie or cheat, I steal at home). The aggressive behaviors scale consisted of the sum of the items that dealt with violence or aggression towards others (e.g. I physically attack people). A composite score was computed from the sum of the rule-breaking scale and the aggressive scale, with higher scores indicating greater displays of externalizing behaviors. Excellent reliability was found for the rule-breaking (α = .76) and the aggressive behavior scales (α = .86).1
Procedure
Participants were recruited from the diabetes clinics and received the measures used here in a packet of questionnaires that were to be completed individually and returned at a laboratory appointment or were completed at the laboratory appointment. For questionnaires completed at home, mothers, adolescents, and fathers2 were given separate packets and instructed to complete the questionnaires separately. A cover sheet reiterated the importance of completing the questionnaires separately and asked that questions be directed to the investigators rather than family members.
Statistical Analyses
Path analysis through structural equation modeling (Mplus version 3, Muthén & Muthén, 1988–2005) was used to evaluate the fit of several alternative models. Mardia's coefficient for multivariate kurtosis was within acceptable limits (z = 7.306), suggesting the assumption of normality under maximum likelihood was reasonable given our sample size (Muthén & Kaplan, 1985). All models were tested for gender effects with a multiple-group model; gender did not moderate any paths and was thus not included further. We first tested a fully saturated model that examined whether higher father (or mother) general (or diabetes-specific) monitoring were associated directly with better HbA1c, as well as indirectly through better adherence and lower externalizing behaviors in adolescents, and also whether externalizing behaviors were associated with poorer HbA1c through lowered adherence. We then statistically compared the fit of this full model to several simpler nested models that were obtained by deleting strategically specific paths. Specifically, we examined whether the entire effect of monitoring on HbA1c was through adherence and externalizing behaviors by removing the direct path between externalizing behaviors and adherence. We also tested a model removing the direct path between monitoring and adherence, creating a chain of associations where monitoring was associated with lower externalizing behaviors leading to better adherence and better HbA1c. Models were tested separately for adolescents’ reports of their father's and mother's general and diabetes-specific monitoring.3
Results
Preliminary Analyses
All variables were screened for univariate outliers and six cases were found. After removing these cases and then rerunning the analyses there was no difference between analyses with outliers removed versus in the analyses, thus we kept the six cases in our analyses.4 See Table I for means and standard deviations of all study variables. Adolescents reported high levels of adherence at the same time that their mean HbA1c values were significantly above the ADA's recommendations of 7. The mean of our sample on externalizing behaviors (7.90) was below the mean for nonreferred normative samples (M = 9.8, SD = 6.8 for boys and M = 9.9, SD = 7.3 for girls, for 11–18-year olds). We report and analyze raw scores, rather than T-scores, which are preferable when the sample involves adolescents in the normal, rather than clinical range (Drotar, Stein, & Perrin, 1995).
Table I.
Means, Standard Deviations, and Correlations Among Primary Study Variables
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | M (SD) | |
|---|---|---|---|---|---|---|---|---|
| 1. HbA1c | −.31** | −.083 | −.27** | −.078 | −.27** | .29** | −.06 | 8.37 (1.58) |
| 2. Adolescent report of adherence | .46** | .27** | .38** | .38** | −.24** | .06 | 3.94 (.576) | |
| 3. Adolescent report of mother's general monitoring | .44** | .57** | .29** | −.22** | .01 | 4.26 (.625) | ||
| 4. Adolescent report of father's general monitoring | .20** | .67** | −.20** | −.21** | 3.52 (.957) | |||
| 5. Adolescent report of mother's diabetes monitoring | .33** | −.07 | .01 | 4.10 (.787) | ||||
| 6. Adolescent report of father's diabetes monitoring | −.12 | −.19** | 3.04 (1.07) | |||||
| 7. Adolescent report of externalizing behaviors | −.05 | 7.90 (6.97) | ||||||
| 8. Gender |
**p < .01.
As displayed in Table I, correlations among variables indicated that the hypothesized relationships between monitoring and externalizing behaviors existed only for general monitoring, that both general and diabetes-specific monitoring were associated with better adherence, and that general and diabetes-specific monitoring were associated with lower HbA1c only for adolescents’ reports of fathers.
Path Model Examining Monitoring, Externalizing Behaviors, Adherence, and HbA1c General Monitoring
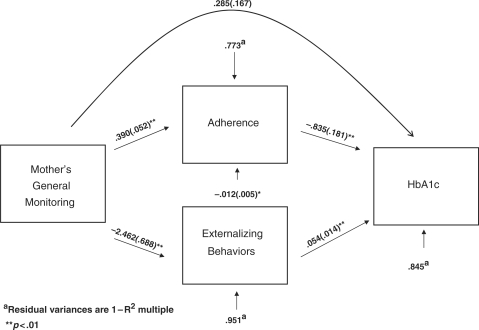
We tested models for mothers’ and fathers’ general and diabetes-specific monitoring separately, reporting first the results for mothers’ general monitoring. We began with the fully saturated model depicted in Figure 1, where maternal general monitoring had both direct associations with HbA1c, and indirect associations through adherence and externalizing behaviors, and where externalizing behaviors related to HbA1c through poorer adherence. The numbers depicted are the unstandardized coefficients with the standard errors in parentheses. The results confirm that each pathway was significant in the model, except the direct path from mothers’ general monitoring to HbA1c (total R2 = 0.155 for HbA1c). The total indirect effect of mother's monitoring on HbA1c was significant (b = −.484, SE = 0.099, z = −4.814). We then compared this fully saturated model to a series of simpler nested models to assess whether there was a reduction in fit (these models were nested with the fully saturated model, but not necessarily with each other). First, we tested a model that fixed to zero the direct path between externalizing behaviors and adherence. This model provided a significantly worse fit [χ2(1) = 6.43, p<.05] compared to the fully saturated model. Second, starting from the saturated model, we fixed the direct pathway from mothers’ monitoring to adherence to zero, only leaving the chain of mothers’ monitoring to externalizing behaviors to lower adherence and poorer HbA1c. This model was a significantly worse fit [χ2(1) = 50.17, p<.01] compared to the fully saturated model. Thus, the best fitting model for adolescents’ perceptions of maternal monitoring indicated that general monitoring was associated with lower HbA1c only indirectly through better adherence and lower externalizing behaviors, with externalizing behaviors associated both directly with poorer HbA1c and indirectly through poorer adherence.
Figure 1.
Path model examining general maternal monitoring, adherence, externalizing behaviors, and HbA1c.
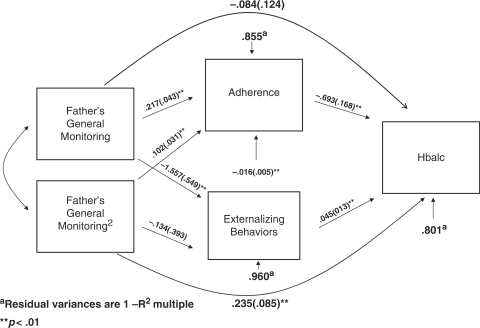
The same model was applied to adolescents’ reports of fathers’ general monitoring (see Figure 2). Because our previous work (Berg et al., 2008) indicated that fathers’ monitoring had its effects largely at low levels of father monitoring, we added the quadratic effect for both the direct effect and the indirect effect of fathers’ general monitoring on HbA1c. As with mothers’ monitoring, the initial model was fully saturated. Note that the nested test for the exclusion of the quadratic terms in predicting the outcomes indicated poorer fit for both general monitoring [χ2(3) = 18.81, p<.01] and diabetes-specific monitoring [χ2(3) = 18.81, p<.01]. This model indicated that when fathers’ monitoring was average, there was no direct effect of monitoring on HbA1c. However, monitoring had an indirect association with HbA1c through higher adherence and lower externalizing behaviors (total R2 = 0.199 for HbA1c). Because the quadratic was significant in predicting HbA1c both directly and indirectly, we examined the model when fathers’ monitoring was 1 SD below the mean and 1 SD above the mean, consistent with viewing a polynomial as the simplest form of interaction (where a variable interacts with itself; Aiken & West, 1991). When fathers’ monitoring was low, monitoring was directly associated with higher HbA1c and the total indirect effect was not significant (b = −.088, SE = 0.052, z = − 1.69). When fathers’ monitoring was high, there was no direct association with HbA1c, but the total indirect effect was significant (b = −.387, SE = 0.115, z = − 3.354). We then compared this fully saturated model to the same models examined for mothers. First, the model that fixed the direct path between externalizing behaviors and adherence to zero was a significantly poorer fit [χ2(1) = 9.80, p<.01] compared to the fully saturated model. Second, starting from the saturated model, we fixed to zero the direct pathway from fathers’ monitoring to adherence, creating a hypothesized chain of fathers’ monitoring leading to externalizing leading to lower adherence and lower HbA1c. This model was a significantly worse fit [χ2(1) = 24.35, p<.01] compared to the fully saturated model.
Figure 2.
Path model examining general paternal monitoring, adherence, externalizing behaviors, and HbA1c.
Diabetes-Specific Monitoring
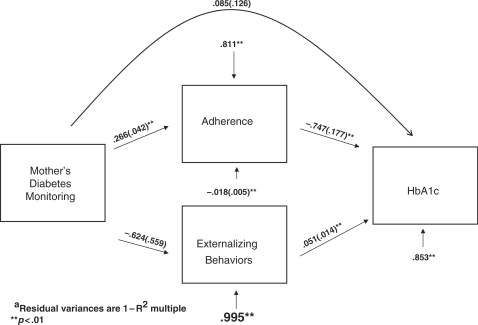
Similar models were tested for mothers’ and fathers’ diabetes-specific monitoring. As can be seen in Figure 3, the fully saturated model for mothers’ diabetes monitoring was similar to the model for general monitoring, with one important exception. The path between mothers’ diabetes-specific monitoring and externalizing behaviors was not significant (total R2 = 0.147 for HbA1c). Nevertheless, the total indirect effect of mother's monitoring on HbA1c was significant (b = −.239, SE = 0.067, z = −3.551). Both simpler nested models were a significantly worse fit to the data, including the model fixing the path from externalizing behaviors to adherence to zero [χ2(1) = 13.58, p<.01] and the model fixing the mother monitoring to adherence path to zero [χ2(1) = 37.43, p<.01].
Figure 3.
Path model examining diabetes-specific maternal monitoring, adherence, externalizing behaviors, and HbA1c.
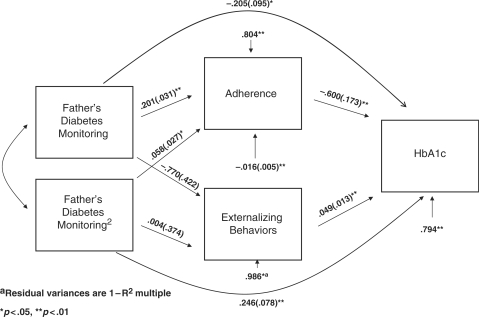
Similarly, for fathers’ diabetes-specific monitoring (see Figure 4), the fully saturated model indicated similar effects as for general monitoring, with the exception being that fathers’ diabetes-specific monitoring was not associated with externalizing behaviors (total R2 = .206 for HbA1c). When fathers’ monitoring was low, monitoring was directly associated with higher HbA1c and the total indirect effect was not significantly (b = −.092, SE = 0.064, z = − 1.44). When fathers’ monitoring was high, there was no direct association with HbA1c, but the total indirect effect was significant (b = −.240, SE = 0.090, z = −2.655). Both simpler nested models were a significantly worse fit to the data, including the model fixing the path from externalizing behaviors to adherence to zero [χ2(1) = 11.53, p<.01] and the model fixing father monitoring to adherence path to zero [χ2(2) = 39.50, p<.01].
Figure 4.
Path model examining diabetes-specific paternal monitoring, adherence, externalizing behaviors, and HbA1c.
Summary
In sum, higher general parental monitoring was associated with lower HbA1c, both directly (only for fathers) and indirectly as a result of higher adherence and lower externalizing behaviors. Furthermore, externalizing behaviors were associated with higher HbA1c directly and indirectly through lower adherence. Diabetes-specific monitoring was associated both directly (only for fathers) and indirectly with HbA1c as a result of higher adherence only. Diabetes-specific monitoring was not associated with externalizing behaviors for either mother or father. Finally, quadratic associations for fathers’ monitoring indicated that fathers’ monitoring was associated with HbA1c through different processes when fathers’ monitoring was low versus high.
Discussion
Adolescents’ perceptions of both general and diabetes-specific monitoring are important when managing an illness such as type 1 diabetes (Berg et al., 2008; Ellis et al., 2007). This study examined the role of both diabetes-specific and general parental monitoring on HbA1c through lower externalizing behaviors and higher adherence. The primary difference between general parental monitoring and diabetes-specific monitoring was that only general monitoring was associated with externalizing behaviors. Adolescents’ appraisals of mothers’ and fathers’ general and diabetes-specific monitoring differed in their direct and indirect effects. Adolescents’ appraisals of mothers’ general monitoring was only indirectly associated with lower HbA1c through lower externalizing behaviors and higher adherence. Adolescents’ appraisals of fathers’ general monitoring were associated both directly and indirectly with HbA1c and differently at the extremes: when fathers’ monitoring was low, it was associated with poorer HbA1c through higher externalizing behaviors and when fathers’ monitoring was high it was associated with HbA1c through higher adherence.
The findings add to the small literature linking parental monitoring with good diabetes outcomes (Berg et al., 2008; Ellis et al., 2007) by indicating that these effects may be associated with better adherence (consistent with Ellis’ research) and lower externalizing behaviors (for general monitoring only). The model tested is consistent with findings in the field: externalizing behaviors were associated with higher HbA1c levels (Bryden et al., 2001; Duke et al., 2008; Holmes et al., 2006) and externalizing behaviors were associated with higher HbA1c through lower adherence (Duke et al., 2008). Thus, general parental monitoring was associated with better HbA1c both by increasing adherence and lowering the display of externalizing behaviors. These results are consistent with a large developmental literature that links general parenting practices (e.g., coercive behavior, intrusiveness, and abuse) to both the emergence and maintenance of externalizing behaviors (Arbona & Power, 2003; Simons, Paternite, & Shore; 2001) and risk for poor developmental outcomes (e.g., substance abuse, academic failure, externalizing behaviors; see Crouter & Head, 2002; Dishion & McMahon, 1998).
Reports of both general and diabetes-specific parental monitoring were important to the management of an adolescent's diabetes, but only general monitoring was associated with externalizing behaviors. Research has shown that diabetes-specific monitoring is important for better diabetes outcomes (Berg et al., 2008; Ellis et al., 2007). However, Ellis et al. (2007) found that general parental monitoring was not associated with adherence. One possible explanation for the discrepancies in findings is that Ellis’ measure includes both parental monitoring (i.e., being present when the adolescent manages his or her diabetes) and parental knowledge (i.e., knowing when the adolescent is out of test strips or insulin). In the current study parental monitoring may have captured more of the knowledge component. In addition, the fact that only general monitoring was associated with externalizing behaviors may reflect that externalizing behaviors contain a broad array of behaviors (e.g., rule breaking, drinking, smoking) that may be more affected by the parent's general monitoring of the adolescent's activities and friends, rather than monitoring diabetes-specific behaviors (e.g., insulin injections, food intake). It is likely that diabetes-specific monitoring may relate to externalizing behaviors that are more diabetes specific (e.g., faking the diabetes log, diluting the insulin, binge eating, skipping insulin). In addition, links between diabetes-specific monitoring and externalizing behaviors may derive from other components of monitoring (e.g., adolescent disclosure) that our measure was not able to capture (Ellis et al., 2008).
Adolescents’ appraisals of fathers’ monitoring revealed that high versus low fathers’ monitoring were associated with HbA1c via different pathways. When fathers’ general monitoring was low, the relation between monitoring and HbA1c occurred through more externalizing behaviors. However, when fathers’ general monitoring was high, the relation between monitoring and HbA1c occurred through greater adherence. Appraisal of mothers’ general monitoring was associated with HbA1c via adherence and externalizing behaviors across different levels of monitoring. The fact that fathers’ general monitoring had these differential effects at different levels of monitoring could be due to their lower levels of monitoring (Berg et al., 2008) and overall involvement (Seiffge-Krenke, 2002) than mothers, consistent with mothers having a more active role in the care of a chronically ill child (Quittner & DiGirolama, 1998). Future research will benefit from an examination of how both mothers and fathers work together to manage diabetes during adolescence.
Although our results are consistent with the idea that the beneficial effects of general parental monitoring are through lowered externalizing behaviors and both general and diabetes-specific monitoring are through higher adherence, the cross-sectional nature of our study prevents us from making causal statements. The current model is identical mathematically with a model that specifies that monitoring serves as a mediator between externalizing behaviors and HbA1c, due to the saturated nature of our model. However, analyses of simpler models (not completely saturated) clearly indicated that externalizing and adherence were mediators between monitoring and HbA1c and not the reverse. In addition, Valdovinos and Weyand (2006) found that problem behaviors occur in response to high blood glucose levels. Further longitudinal research may begin to address directions of effects, however, other paradigms (e.g., experimental paradigms) may be needed to tease apart temporal associations that are most likely bidirectional (Pardini, Fite, & Burke, 2008).
The results should be interpreted in the context of some limitations. First, our sample of families included predominantly intact white, English-speaking, middle-class participants. Monitoring may be even more important among samples with greater diversity both in terms of ethnic status, but also family background (e.g., single parent households), where a greater range of monitoring levels may be found (Ellis et al., 2007). Such diverse samples may also contain adolescents with higher levels of externalizing behaviors (Dishion & McMahon, 1998). Given our potentially limited diversity in both parental monitoring and externalizing behaviors, our results are even more compelling. Second, our results were based largely on self-report measures (adherence, externalizing behaviors, and mothers’ and fathers’ monitoring), assessed by the adolescent. Additional analyses conducted using mothers’ and fathers’ reports of monitoring revealed no significant relationships between parent report of monitoring and HbA1c or adherence and thus prevented additional modeling. Adolescents’ versus parents’ reports of monitoring are clearly different in some important ways and the discrepancies between these reports may themselves be important for understanding aspects of diabetes management (Berg et al., 2008). Finally, two aspects of our use of the YSR deserve mention. First, we used raw scores rather than T-scores, as recommended by Drotar et al. (1995) when individuals are in the normal rather than the clinical range. This approach, however, does limit conclusions that can be drawn about age and gender comparisons. Second, we used the YSR with 10-year-olds, despite the fact that norms are only published starting at 11. The fact that our results were the same whether the 10-year-olds were included versus dropped from analyses, lends confidence to our use of the YSR.
These findings suggest that adolescents’ perceptions of parental monitoring are paramount in understanding successful diabetes management. The developmental literature is replete with sound interventions that could be applied to diabetes to boost parental monitoring (Dishion & Andrews, 1995; Dishion & McMahon, 1998; Patterson & Stouthamer-Loeber, 1984; Soenens, Vansteenkiste Luyckx, & Goossens, 2006). Our results suggest that such interventions should not only focus on diabetes-specific parental involvement (Anderson et al., 1999; Wysocki et al., 2006), but also address more general ways that parents monitor adolescents’ activities and friends. The management of diabetes is one task among many (school, friends, autonomy development) that adolescents deal with in their daily lives (Smetana et al., 2006). Interventions directed at bolstering general and diabetes-specific monitoring may facilitate HbA1c through multiple pathways not only during adolescence, but beyond this time period as well (Weissberg-Benchell, J., Wolpert, H., & Anderson, 2007). Such interventions may be especially important during adolescence, when management demands become difficult, and particularly for those displaying externalizing behaviors.
Funding
The project was supported by Grant Number R01DK063044 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
Conflict of interest: None declared.
Acknowledgments
We thank the families who participated, the staff of the Utah Diabetes Center and Michael Swinyard's practice, as well as the additional members of the ADAPT team (Jorie Butler, Jon Butner, Katie Fortenberry, Donna Gelfand, Kelly Ko, Hai Le, Michael Johnson, Jenni McCabe, Peter Osborn, Debra Palmer, Marie Simard, Michelle Skinner, and Nathan Story).
Footnotes
1Because the YSR was validated for adolescents 11–18, we did additional analyses to address whether the data from 10-year-olds was reliable and valid. Reliabilities of the two subscales that comprised the externalizing behavior scale revealed somewhat lower reliabilities for the rule breaking scale for 10-year-olds versus the rest of the sample (α = .64 vs. .77), with similar reliabilities for the aggressive behavior scale (α = .86 vs. .86). We thus conducted all analyses reported in this article in two ways, including all participants and then restricting the analyses to the 11–14-year olds. We report in the article the results from the full sample as no significant differences were revealed in these two sets of analyses.
2Analyses examining similar models using parent report of externalizing behaviors and monitoring were not reported, because parent report of monitoring was not associated with adherence or Hba1c (Berg et al., 2008).
3We also conducted analyses comparing diabetes-specific and general monitoring through stacked models to allow for specific comparisons between general and diabetes-specific monitoring. These results yielded identical results for adolescents’ reports of mothers’ data and similar results for fathers’ data, indicating that the primary difference was that only general monitoring was associated with externalizing behaviors. These results are not reported because fathers’ data revealed slight differences in the relationship between monitoring (both linear and quadratic effects) that appeared to be due to alterations in the model that were due largely to the shared variance between these two forms of monitoring.
4All analyses were run controlling for pump status (being on a pump versus not) and duration of diabetes. All results were the same controlling for these variables, which were not included in the analyses reported in the article.
References
- Achenbach TM. Manual for the Child Behavior Checklist. Burlington. VT: University of Vermont; 1991. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications; 1991. [Google Scholar]
- Anderson BJ, Brackett J, Ho J, Laffel LMB. An intervention to promote family teamwork in Diabetes management tasks: Relationships among parental involvement, adherence to blood glucose monitoring, and glycemic control in young adolescents with type 1 diabetes. In: Drotar D, editor. Promoting adherence to medical treatment in chronic childhood illness: Concepts, methods, and interventions. Mahwah, NJ: Lawrence Erlbaum; 2000. pp. 347–365. [Google Scholar]
- Arbona C, Power TG. Parental attachment, self-esteem, and antisocial behaviors among African American, European American, and Mexican American adolescents. Journal of Counseling Psychology. 2003;50:40–51. [Google Scholar]
- Barber BK. Parental psychological control: Revisiting a neglected construct. Child Development. 1996;67:3296–3319. [PubMed] [Google Scholar]
- Berg CA, Butler JM, Osborn P, King G, Palmer D, Butner J, Murray M, Lindsay R, Donaldson D, Foster C, Swinyard M, Wiebe DJ. The role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care. 2008;31:678–683. doi: 10.2337/dc07-1678. [DOI] [PubMed] [Google Scholar]
- Beveridge RM, Berg CA, Wiebe DJ, Palmer DA. Mother and adolescent representations of illness ownership and stressful events surrounding diabetes. Journal of Pediatric Psychology. 2006;31:818–827. doi: 10.1093/jpepsy/jsj094. [DOI] [PubMed] [Google Scholar]
- Bronte-Tinkew J, Moore KA, Carrano J. The father-child relationship, parenting styles, and adolescent risk behaviors in intact families. Journal of Family Issues. 2006;27:850–881. [Google Scholar]
- Brown BB, Mounts N, Lamborn SD, Steinberg L. Parenting practices and peer group afiliation in adolescence. Child Development. 1993;64:467–482. doi: 10.1111/j.1467-8624.1993.tb02922.x. [DOI] [PubMed] [Google Scholar]
- Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood. Diabetes Care. 2001;24:1536–1540. doi: 10.2337/diacare.24.9.1536. [DOI] [PubMed] [Google Scholar]
- Crouter AC, Head MR. Parental monitoring and knowledge of children. In: Bornstein MH, editor. Handbook of parenting: Vol 3: Being and becoming a parent. Mahwah, NJ: Lawrence Erlbaum; 2002. pp. 461–483. [Google Scholar]
- DeKlyen M, Speltz ML, Greenberg MT. Fathering and early onset conduct problems: positive and negative parenting, father-son attachment, and he marital context. Clinical Child and Family Psychology Review. 1998;1:3–21. doi: 10.1023/a:1021844214633. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Andrews DA. Preventing escalation in problem behaviors with high-risk young adolescents: immediate and 1-year outcomes. Journal of Consulting and Clinical Psychology. 1995;63:538–548. doi: 10.1037//0022-006x.63.4.538. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, McMahon RJ. Parental monitoring and the prevention of child and adolescent problem behavior: A conceptual empirical formulation. Clinical Child and Family Psychology. 1998;1:61–75. doi: 10.1023/a:1021800432380. [DOI] [PubMed] [Google Scholar]
- Drotar D, Stein REK, Perrin EC. Methodological issues in using the child behavior checklist and its related instruments in clinical child psychology research. Journal of Clinical Child Psychology. 1995;24:184–192. [Google Scholar]
- Duke DC, Geffken GR, Lewin AB, Williams LB, Storch EA, Silverstein JH. Glycemic control in youth with type 1 diabetes: Family predictors and mediators. Journal of Pediatric Psychology. 2008;33:719–727. doi: 10.1093/jpepsy/jsn012. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Podolski CL, Frey M, Naar-King S, Wang B, Moltz K. The role of parental mMonitoring in adolescent health outcomes: impact on regimen adherence in youth with type 1 diabetes. Journal of Pediatric Psychology. 2007;32:907–917. doi: 10.1093/jpepsy/jsm009. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Templin TN, Naar-King S, Frey MA. Toward conceptual clarity in a critical parenting construct: Parental monitoring in youth with chronic illness. Journal of Pediatric Psychology. 2008;33:799–808. doi: 10.1093/jpepsy/jsn044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes CS, Chen R, Streisand R, Marschall DE, Souter S, Swift EE, et al. Predictors of youth diabetes care behaviors and metabolic control: A structural equation modeling approach. Journal of Pediatric Psychology. 2006;31:770–784. doi: 10.1093/jpepsy/jsj083. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Auslander WF, Greco P, Spetter D, Fisher E, Santiago JV. I get by with a little help from my family and friends: Adolescents’ support for diabetes care. Journal of Pediatric Psychology. 1995;20:449–476. doi: 10.1093/jpepsy/20.4.449. [DOI] [PubMed] [Google Scholar]
- LaGreca AM, Swales T, Klemp S, Madigan S, Skyler J. Adolescents with diabetes: Gender differences in psychosocial functioning and glycemic control. Children's Health Care. 1995;24:61–78. [Google Scholar]
- Mellin AE, Neumark-Tainzer D, Patterson JM. Parenting adolescent girls with type 1 diabetes: Parents’ perspectives. Journal of Pediatric Psychology. 2004;29:221–230. doi: 10.1093/jpepsy/jsh023. [DOI] [PubMed] [Google Scholar]
- Muthén B, Kaplan D. A comparison of some methodologies for the factor analysis of non-normal Likert variables. British Journal of Mathematical and Statistical Psychology. 1985;38:171–189. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide: Third edition. Los Angeles, CA: Muthén & Muthén; 1998–2005. [Google Scholar]
- Palmer DL, Berg CA, Wiebe DJ, Beveridge RM, Korbel CD, Upchurch R, Swinyard MT, Lindsay R, Donaldson DL. The role of autonomy and pubertal status in understanding age differences in maternal involvement in diabetes responsibility across adolescence. Journal of Pediatric Psychology. 2004;29:35–46. doi: 10.1093/jpepsy/jsh005. [DOI] [PubMed] [Google Scholar]
- Pardini DA, Fite PJ, Burke JD. Bidirectional associations between parenting practices and conduct problems in boys from childhood to adolescence: The moderating effect of age and African-American Ethnicity. Journal of Abnormal Child Psychology. 2008;36:647–662. doi: 10.1007/s10802-007-9162-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, Stouthamer-Loeber M. The correlation of family management practices and delinquencies. Child Development. 1984;55:1299–1307. [PubMed] [Google Scholar]
- Quittner AL, DeGirolamo AM. Handbook of Pediatric Psychology and Psychiatry. Boston: Allyn & Bacon; 1998. Family adaptation to childhood disability and illness; pp. 70–120. [Google Scholar]
- Rueter MA, Conger RD. Reciprocal influences between parenting and adolescent problem-solving behavior. Developmental Psychology. 1998;34:1470–1482. doi: 10.1037//0012-1649.34.6.1470. [DOI] [PubMed] [Google Scholar]
- Seiffge-Krenke I. “Come on, say something, Dad!”: Communication and coping in fathers of diabetic adolescents. Journal of Pediatric Psychology. 2002;27:439–450. doi: 10.1093/jpepsy/27.5.439. [DOI] [PubMed] [Google Scholar]
- Simons KJ, Paternite CE, Shore C. Quality of parent/adolescent attachment and aggression in young adolescents. Journal of Early Adolescence. 2001;21:182–203. [Google Scholar]
- Smetana JG, Campione-Barr N, Metzger A. Adolescent development in interpersonal and societal contexts. Annual Review of Psychology. 2006;57:255–284. doi: 10.1146/annurev.psych.57.102904.190124. [DOI] [PubMed] [Google Scholar]
- Soenens B, Vansteenkiste M, Luyeckx K, Goossens L. Parenting and adolescent problem behavior: An integrated model with adolescent self disclosure and perceived parental knowledge as intervening variables. Developmental Psychology. 2006;42:305–318. doi: 10.1037/0012-1649.42.2.305. [DOI] [PubMed] [Google Scholar]
- Valdovinos MG, Weyand D. Blood glucose levels and problem behavior. Research in Developmental Disabilities. 2006;27:227–231. doi: 10.1016/j.ridd.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Webb JA, Bray JH, Getz JG, Adams G. Gender, perceived parental monitoring and behavioral adjustment: Influences on adolescent alcohol use. American Journal of Orthopsychiatry. 2002;72:392–400. doi: 10.1037/0002-9432.72.3.392. [DOI] [PubMed] [Google Scholar]
- Weissberg-Benchell J, Wolpert H, Anderson BJ. Transitioning from pediatric to adult care: A new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care. 2007;30:2441–2446. doi: 10.2337/dc07-1249. [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Berg CA, Korbel C, Palmer DA, Beveridge RM, Upchurch R, Lindsay R, Swinyard MT, Donaldson DL. Children's appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology. 2005;30:167–178. doi: 10.1093/jpepsy/jsi004. [DOI] [PubMed] [Google Scholar]
- Williams SK, Kelly FD. Relationships among involvement, attachment, and behavioral problems in adolescence: Examining father's influence. Journal of Early Adolescence. 2005;25:168–196. [Google Scholar]
- Wysocki T, Linschied TR, Taylor A, Yeates KO, Hough BS, Naglieri JA. Deviation from developmentally appropriate self-care autonomy. Diabetes Care. 1996;19:119–125. doi: 10.2337/diacare.19.2.119. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Wysocki T, Gavin L. Parental Involvement in the Management of Pediatric Chronic Diseases: Associations with Adherence, Quality of Life, and Health Status. Journal of Pediatric Psychology. 2006;31:501–511. doi: 10.1093/jpepsy/jsj042. [DOI] [PubMed] [Google Scholar]