Abstract
Background
Women with anterior cruciate ligament reconstruction have different neuromuscular strategies than noninjured women during functional tasks after ligament reconstruction and rehabilitation.
Hypothesis
Landing from a jump creates high loads on the knee creating dynamic instability in women with anterior cruciate ligament reconstruction, whereas noninjured women have stable knee landing mechanics.
Study Design
Controlled laboratory study.
Methods
Fifteen noninjured women and 13 women with anterior cruciate ligament reconstruction performed 5 trials of a single-legged 40-cm drop jump and 2 trials of a 20-cm up-down hop task. Multivariate analyses of variance were used to compare hip and knee joint kinematics, knee joint moments, ground-reaction forces, and electromyographic findings between the dominant leg in noninjured women and reconstructed leg in women with anterior cruciate ligament reconstruction.
Results
No statistically significant differences between groups were found for peak hip and knee joint angles for the drop jump task. Statistically significant differences in neuromuscular activity (P = .001) and anterior-posterior knee shear forces (P < .001) were seen in women with anterior cruciate ligament reconstruction compared with noninjured women in the drop jump task. However, no statistically significant differences (P > .05) between groups were found for either peak hip and knee joint angles, peak joint kinetics, or electromyographic findings during the up-down hop task.
Conclusion
Women with anterior cruciate ligament reconstruction have neuromuscular strategies that allow them to land from a jump similar to healthy women, but they exhibit joint moments that could predispose them to future injury if they participate in sports that require jumping and landing.
Keywords: anterior cruciate ligament (ACL), landing, knee, biomechanics
Disruption of the ACL leads to a sequelae of factors that could predispose patients to further disability related to degeneration of the knee joint.12 Impairments in postural control, muscle strength, functional performance, movement activation patterns, and motor control have been reported in patients with ACL injuries and ACL reconstruction.1,14 Furthermore, proprioceptive and neuromuscular deficits have been observed in the uninjured extremity in patients with unilateral ACL injury.1,14 These deficits continue after surgical reconstruction and rehabilitation.1,14
Deficits in quadriceps muscle strength have been shown to be the result of decreased neuromuscular activation of the quadriceps muscle rather than muscle fiber atrophy.1,14 Researchers have shown that neuromuscular compensatory strategies help patients with ACL deficiency and ACL reconstruction to increase functional knee stability.16,22,43 Others have suggested that ACL reconstruction improves the function of most patients on a short-term basis and decreases long-term instability that could damage additional internal knee structures.13 However, some investigators suggest ACL reconstruction does not restore rotational knee stability during sporting activities.33 Almost 80% of athletes undergoing ACL reconstruction surgery are unable to successfully return to preinjury-level sport participation and therefore quit their sports.7,24,42 Conversely, several investigators have reported functional recovery in patients with ACL reconstruction similar to noninjured individuals in functional tasks such as drop jumps, step-ups, step-downs, and agility drills.10,22,23 Although many investigations have described knee kinematics, kinetics, and neuromuscular strategies in patients with ACL deficiency, few have assessed the same variables in patients with ACL reconstruction.
The purpose of this investigation is to evaluate muscle activation strategies, hip and knee joint angles, and knee joint moments during 2 functional athletic tasks in healthy, noninjured women and women with ACL reconstruction. Based on previous literature7,24,33,42 regarding the deficits in patients after ACL reconstruction compared with noninjured individuals, it is hypothesized that women with ACL reconstruction will exhibit smaller hip and knee flexion joint angles and larger hip and knee mediolateral and rotational joint angles. In addition, greater vertical ground-reaction forces, anterior-posterior shear forces, and peak knee extension and knee valgus moments are expected in women with ACL reconstruction. Furthermore, lower quadriceps/hamstring cocontraction ratios and normalized EMG activity of lower extremity muscles in women with ACL reconstruction are also expected.
METHODS
Participants
Fourteen physically active young women with ACL reconstruction (age, 25.4 ± 3.1 years; height, 167.5 ± 5.9 cm; body mass, 63.2 ± 6.7 kg) and 15 healthy, noninjured young women (age, 24.6 ± 2.6 years; height, 164.7 ± 6.5 cm; body mass, 58.4 ± 8.9 kg) were recruited by the primary investigators. All participants engaged in recreational fitness activities such as jogging, running, and weight lifting. None of the participants formed part of any intercollegiate, varsity, or competitive sport team. The noninjured women were students recruited from a school of physical therapy. Women with ACL surgery were recruited by word of mouth from local outpatient physical therapy sports medicine clinics in surrounding areas. In this study, it was not feasible to control for surgery- or postsurgical rehabilitation protocol– related variability because of the nature of the recruitment process. Nevertheless, participants reported similarities in their respective rehabilitation protocols such as bracing, cryotherapy, electrotherapy, neuromuscular reeducation, strengthening exercises, and functional training. The mean time after surgery for the women with ACL reconstruction was 7.2 ± 4.2 years (1−16 years after reconstruction). Among the 14 women with ACL reconstruction, 9 had patellar tendon graft reconstructions, 2 had Achilles tendon allograft reconstructions, and 3 had gracilis-semitendinosus tendon graft reconstructions.
The inclusion criterion for all healthy participants was an age range from 18 to 35 years. Exclusion criteria for all healthy participants were (1) low back or lower extremity surgery, (2) other reported injuries or medical problems that would affect legs or trunk, and (3) inability to perform 2 single-legged screening jumps. Inclusion criteria for ACL-reconstructed participants were (1) age range from 18 to 35 years and (2) at least 1 year postsurgery. Exclusion criteria for these participants were (1) leg-to-leg difference of more than 3 mm of anterior tibial displacement as measured by a knee arthrometer, indicating that they had an unstable graft; (2) multiple surgeries on the same knee; or (3) inability to perform 2 screening jumps on the operated leg.
Patients with concomitant meniscal injuries that were surgically addressed were allowed to participate given that concomitant incidence of ACL and meniscal injuries occurs in 91% of cases.12,36 Participants were asked to wear loose-fitting clothing and athletic shoes. Each participant was asked to read and sign a written informed consent approved by the university institutional review board before participation. One of the recruited women among those with ACL reconstruction was not able to perform the screening and practice trials for both tasks; therefore, she was excluded from the study. An additional participant was able to perform the drop jump but not the up-down. This particular participant's performance during the drop jump was similar to the rest of the women with ACL reconstruction and did not represent an outlier during data screening procedures. It can be hypothesized that this young woman was not physically prepared to perform repetitive and high-demand functional tasks such as the up-down hop. Therefore, 13 participants with ACL reconstruction were included in the drop jump analyses and 12 in the up-down analyses.
Procedures
After informed consent procedures, weight, height, and distance between anterior superior iliac spines were measured for all participants. Leg dominance was determined for all healthy participants. Dominant leg was operationally defined as the leg preferred to perform a single-legged hop for distance.6,47 The warm-up protocol consisted of 5 minutes of cycling at 40 to 60 rpm on a cycle ergometer, 10 half squats, 5 continuous vertical jumps (counter-movement jumps), and 2 practice trials of the 2 jump tasks. The tasks used in this investigation were 5 trials of a 40-cm single-legged drop jump (Figure 1) and a 20-cm up-down hop task (Figure 2). These tasks were randomly ordered. Each drop jump consisted of standing initially on both feet on the 40-cm platform and then standing on the jumping leg when the command “ready” was given. After the command “set,” each participant was instructed to drop when she felt ready to do so. Each participant was instructed to perform a maximal-effort vertical jump on landing single-legged on the center of the force plate. Participants were allowed to use their arms freely during task performance for balance purposes. On the basis of pilot data, 5 trials of the drop jump demonstrated good reliability for all kinematic and kinetic variables (intra-class correlation coefficient, > 0.77). Each participant was allowed to rest as much as she wanted to prevent fatigue. No participant was allowed to rest less than 1 minute between trials. The 40-cm height for the drop jump was selected based on findings by Huston et al17 in which differences in landing mechanics between men and women were observed from heights starting at 40 cm. Landing from less than 40 cm presented no differences in knee flexion joint angles between men and women.17 The performance of a vertical jump on landing onto a force plate was selected as a representation of a land-and-go maneuver. Land-and-go maneuvers are commonly observed in sports29 and are related to ACL injuries in sports such as basketball, volleyball, and soccer.15,18,19,30,45
Figure 1.
The 40-cm drop jump. Participants dropped single-legged from the platform onto the force plates. On landing on the force plate, participants performed a maximal vertical jump.
Figure 2.
The up-down hop task. One trial of this task comprised 10 consecutive hops up to and down from the 20-cm step.
The up-down hop task was performed as standardized by Itoh et al21 (Figure 2). Each participant stood facing a 20-cm step. They performed 10 consecutive jumps up to and down from the 20-cm step when they felt ready to do so. The 10 consecutive up and down hops composed 1 trial. Each participant performed 2 trials of this task. On the basis of pilot data, 1 trial of the up-down hop task demonstrated reliable results for all kinematic and kinetic variables (intraclass correlation coefficient > 0.77). Resting time for the up-down was similar to that of the drop jump.
Instrumentation
Participants had 12 retro-reflective markers attached over both anterior superior iliac spines, second sacral vertebra, greater trochanters, lateral femoral epicondyles, middistance between greater trochanters and lateral femoral epicondyles, medial femoral epicondyles, lateral malleoli, middistance between lateral femoral epicondyles and lateral malleoli, medial malleoli, calcaneal tuberosities, and second metatarsophalangeal joints. The motion analysis system consisted of 4 digital cameras (60-Hz sampling rate) that were time synchronized to the force plates (AMTI, Watertown, Mass; 1-kHz sampling rate). Video data were captured with VISOL Multi-DV Capture software (VISOL Inc, Seoul, Korea). Force plate data were recorded with KwonGRF 2.1 software (VISOL Inc).
Before data collection, the volume of the recording space was calibrated according to the manufacturer's recommendation with a 12-point, 81.5-cm3 cube using an 11-parameter direct linear transformation method. A static trial was captured with the participant standing still with arms across the chest to align the joint coordinates to the laboratory recording instruments. After the static trial, the medial epicondyle and medial malleolus markers were removed to prevent interference between medial markers and lower extremities during jumps.
Surface EMG was recorded with 8 bipolar, self-adhesive, Ag/AgCl preamplified surface electrodes (M-00-S, Ambu, Ølstykke, Denmark; overall gain, 2000 mV; total electrode contact area, 4.1 × 3.4 cm; 1.32-cm2 sensor area). Electrodes were placed on the skin over the gluteus maximus, quadriceps, and lateral and medial hamstrings, according to recommendations of Cram et al,8 after skin cleansing with a gauze soaked in alcohol. The reference electrode was placed over the anterior tibial crest. All electrodes were secured with hypoallergenic adhesive tape to reduce movement artifact. Electromyographic data were collected with a computerized telemetry system (Noraxon Inc, Scottsdale, Ariz). Raw muscle activity recordings were transmitted via FM signal from a transmitter each participant wore on a belt. The signal was filtered at a bandwidth of 10 to 500 Hz with 130-Db common-mode rejection within the transmitter. The receiver converted the signal from analog to digital through an external USB A/D converter, and signals were displayed on a computer monitor.
Data Reduction
Joint angles, ground-reaction forces, and knee joint moment data were synchronized and analyzed with Kwon3D 3.1 (VISOL Inc). Joint angles were derived from the 3-dimensional trajectory of retro-reflective markers filtered through a second-order low-pass Butterworth filter (6 Hz). Hip and knee joint angles were defined in sagittal, frontal, and transverse planes as the first, second, and third rotations, respectively. Joint moments were derived by an inverse dynamics method instrumented in the software. For this investigation, the peak knee extension joint moment was operationally defined as peak ground-reaction forces passing posterior to the knee joint center for which the quadriceps muscle needed to counteract the specific magnitude created by the ground-reaction forces. Peak knee valgus moments were operationally defined as peak ground-reaction forces traveling lateral to the knee joint center in which a lift-off or gap of the medial joint line was created.
The kinematic and kinetic data of interest for the drop jump were the peak values during the ground-contact phase: from initial contact as identified by the force plate to pushoff from the force plate into the vertical jump. For the up-down, the first 2 and last 2 jumps out of the total 10 were excluded from the analysis to account for acceleration and deceleration variability. Therefore, peak kinematic and kinetic values of the middle 6 jumps were averaged for analyses.
The EMG data were time synchronized to the force plates. The EMG raw data were amplified (×1000) and full-wave rectified using Myoresearch software (Noraxon Inc). The EMG data were normalized by using a dynamic normalization procedure in which the mean signal for each muscle group in the window of interest was divided by the maximum signal generated on the specific trial analyzed. This method has been widely used to analyze EMG activity during dynamic tasks2,9,26,27,34,35 and has been shown to reduce participant variability when compared with maximal isometric voluntary contractions.2,41 In addition, this procedure controls for the variability between trials caused by fatigue during dynamic tasks with multiple trials.9 Because the hamstring muscle group was separated into medial and lateral compartments, the normalized results were summed and averaged to represent the hamstring group in its entirety.2,26 Hamstring values were averaged to be fitted into a cocontraction ratio.2,26 The first step for calculating the cocontraction ratio involved obtaining the normalized values for both the quadriceps and hamstring muscle groups during the targeted window of time.2,26 The hamstring value was used as the divisor if its value was greater than that of the quadriceps; however, the quadriceps value was used if its value was greater than that of the hamstrings.2,26 Therefore, the cocontraction ratio value was always less than or equal to 1.2,26 This ratio represented joint stiffness and the relative activation of the flexor and extensor muscle groups crossing the knee joint.2,26 A cocontraction ratio closer to 1 indicated excellent cocontraction, whereas values closer to 0 represented poor cocontraction between the quadriceps and hamstring muscle groups.2,26
Data Analysis
All kinematic, kinetic, and EMG data were screened for normality assumptions and outliers using the Shapiro-Wilk test and histograms. Paired t tests with Bonferroni correction were conducted to compare the involved and uninvolved legs of the participants with ACL reconstructions on all variables. Three separate multivariate analyses of variance, with follow-up univariate analyses of variance, were used for comparisons of each group of kinematics, kinetics, and EMG data between groups. The multivariate alpha level was set at .05. Follow-up univariate analyses of variance alpha level was adjusted after correction for type I error. Effect size (ES) and power (β) were calculated for all analyses.
RESULTS
Descriptive data for all dependent variables for both groups in both tasks are presented in Tables 1 and 2 and Figures 3 and 4.
TABLE 1.
Peak Hip and Knee Joint Angles for Healthy Noninjured Women and Women With ACL Reconstruction (ACLr) for the Drop Jump and Up-Down Tasksa
| Drop Jump |
Up-Down |
|||
|---|---|---|---|---|
| Variable, deg | Healthy (n = 15) | ACLr (n = 13) | Healthy (n = 15) | ACLr (n = 12) |
| Hip flexion | 49.51 ± 6.91 | 45.93 ± 7.10 | 40.45 ± 9.92 | 36.69 ± 7.08 |
| Hip adduction | 4.37 ± 5.04 | 4.13 ± 4.46 | 5.58 ± 5.24 | 4.68 ± 3.19 |
| Hip internal rotation | 1.89 ± 2.19 | 5 ± 5 | 4.47 ± 6.60 | 6.57 ± 5.17 |
| Knee flexion | 57.85 ± 5.68 | 57.73 ± 8.88 | 49.27 ± 5.43 | 48.71 ± 9.74 |
| Knee valgus | 9.89 ± 5.34 | 7.15 ± 5.81 | 5.80 ± 3.84 | 6.09 ± 5.02 |
| Knee external rotation | 5.64 ± 5.18 | 10.52 ± 10.71 | 10.60 ± 11.97 | 6.51 ± 6.92 |
Data are means ± SD.
TABLE 2.
Peak Kinetic Variables for Healthy Women and Women With ACL Reconstruction (ACLr) for the Drop Jump and Up-Down Taska
| Drop Jump |
Up-Down |
|||
|---|---|---|---|---|
| Variable | Healthy (n = 15) | ACLr (n = 13) | Healthy (n = 15) | ACLr (n = 12) |
| Knee extension moments, N·m/Kg | 3.0 ± 0.55b | 3.5 ± 0.69b | 2.8 ± 0.52 | 3.0 ± 0.60 |
| Knee valgus moments, N·m/Kg | 0.07 ± 0.05b | 0.20 ± 0.22b | 0.33 ± 0.13 | 0.35 ± 0.19 |
| Peak vertical GRF/BW | 4.62 ± 0.55 | 4.36 ± 0.76 | 3.33 ± 0.29 | 3.80 ± 0.59 |
| Peak AP shear forces/BW | 0.90 ± 0.16b,c | 0.29 ± 0.18b,c | 0.64 ± 0.12 | 0.73 ± 0.10 |
Data are means ± SD. GRF/BW, ground-reaction forces normalized to body weight; N·m/Kg, joint moments in Newton-meters per kilogram of body mass.
P < .05, during follow-up analysis of variance after Bonferroni correction.
P < .017, during follow-up analysis of variance after Bonferroni correction.
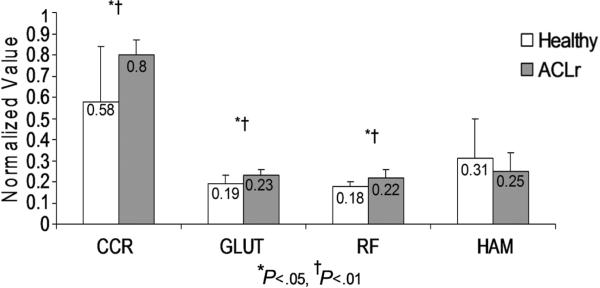
Figure 3.
Cocontraction ratio (CCR) and normalized EMG for noninjured, healthy women and women with ACL reconstruction during the drop jump. ACLr, ACL reconstructed; GLUT, gluteus maximus/medius; HAM, hamstrings; RF, rectus femoris. *P < .05 and †P < .01 during follow-up analysis of variance.
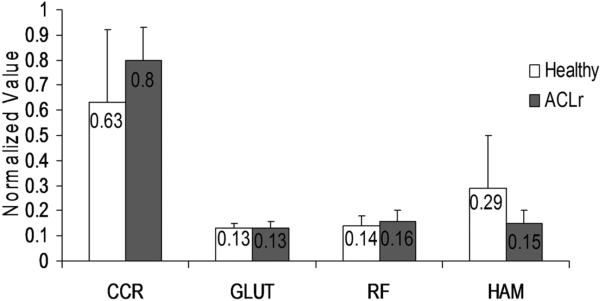
Figure 4.
Cocontraction ratio (CCR) and normalized EMG for noninjured, healthy women and women with ACL reconstruction during the up-down hop task. ACLr, ACL reconstructed; GLUT, gluteus maximus/medius; HAM, hamstrings; RF, rectus femoris.
Drop Jump
Between-legs Comparison
Paired-sample t tests with Bonferroni correction between the involved and noninvolved legs in participants with ACL reconstruction exhibited no differences for all kinematic, kinetic, and EMG dependent variables.
Hip and Knee Joint Angles
The multivariate analyses of variance results revealed no statistically significant differences between groups for peak hip and knee joint angles (F6,21 = 1.67, P > .05, P = .179; ES = .32, β= 0.50) (see Table 1).
Joint Kinetics
Significant differences between groups were found for the kinetic variables (F5,22 = 41.1, P < .001; ES = 0.90, β = 1.0). Follow-up analyses of variance on each kinetic variable showed significantly lower peak anterior-posterior shear forces (F1,26 = 69.33, P < .001; ES = 0.73, β = 1.0). Women with ACL reconstruction exhibited greater peak knee extension moments (F1,26 = 4.8, P = .04; ES = 0.2, β = 0.56) and greater peak knee valgus joint moments (F1,26 = 5.3, P = .03; ES = 0.17, β = 0.60), but these results were not statistically significant in the follow-up analysis of variance after Bonferroni corrections.
Electromyography
Multivariate analysis for EMG variables showed statistically significant differences between groups (F4,23 = 6.47, P = .001; ES = 0.53, β = 0.97). Follow-up analyses of variance on each EMG variable showed significantly greater cocontraction ratios (F1,26 = 8.83, P = .006; ES = 0.25, β = 0.82), greater gluteus maximus full-wave rectified normalized EMG (F1,26 = 10.64, P = .003; ES = 0.29, β = 0.88), and greater rectus femoris full-wave rectified normalized EMG (F1,26 = 14.73, P = .001; ES = 0.36, β = 0.96) in the group with ACL reconstruction (Figure 3).
Up-Down
Between-legs Comparison
Paired-sample t tests with Bonferroni correction between the involved and noninvolved legs in the group with ACL reconstruction exhibited no differences for all kinematic and EMG dependent variables. However, paired t test analysis showed a statistically significant difference (P = .004) in peak knee extension moments between legs in the group with ACL reconstruction (noninvolved, 210.1 ± 35.8 N·m; involved, 178.7 ± 42.9 N·m).
Hip and Knee Joint Angles
Multivariate analyses showed no statistically significant differences between groups for all kinematic variables (F6,20 = 1.84, P = .14; ES = 0.36, β= 0.55) (see Table 1).
Joint Kinetics
Multivariate analyses showed no statistically significant differences between groups for all kinetic variables (F5,20 = 1.71, P = .18; ES = 0.29, β = 0.48) (Table 2).
Electromyography
Multivariate analyses showed no statistically significant differences between groups for all EMG dependent variables (F4,22 = 1.66, P = .196; ES = 0.23, β = 0.42) (Figure 4).
DISCUSSION
The main purpose of this study was to compare kinematic, kinetic, and neuromuscular performance between women with ACL reconstruction and healthy, noninjured young women during 2 jump tasks. The study of landing mechanics is important in understanding the large eccentric loads encountered in sports.10 Therefore, performance analysis of landing tasks provided information about landing strategies implemented by young women with ACL injuries after surgical reconstruction.10 The drop jump task is an ideal task to study landing strategies because of its ability to maximally create eccentric loading on the lower extremity.46 The up-down is another task that has been recommended to be used to detect knee joint instability because of its high sensitivity value (.58).20,21,31
The kinematic results of this investigation supported the overall null hypothesis by demonstrating that women with ACL reconstruction exhibited peak hip and knee joint angles similar to those of healthy, noninjured young women in both tasks. However, statistically significant differences were found for the kinetic and EMG measures during the drop jump, in support of the alternate hypothesis.
Drop Jump
The findings of this investigation regarding comparisons between legs in women with ACL reconstruction demonstrated that both limbs exhibited similar landing mechanics and neuromuscular performance during the drop jump. These findings contradict reports from some investigators in which differences between the reconstructed and noninjured legs have been reported for integrated EMG11,28 and tibial internal/external rotation.33 However, other investigators have reported results similar to this investigation for integrated EMG,43 anterior-posterior femoral translation,22 and tibial internal/external rotation.22 This controversy makes it unclear if neuromuscular deficits carry over to the noninjured leg in patients with ACL reconstruction or if full recovery of the injured leg can be expected. On the basis of the results of this investigation, this controversy needs to be analyzed with caution given the range of years after ACL reconstruction of the women who participated in this investigation. The postoperative range of this group was 1 to 16 years, making it difficult to draw conclusions if between-limb deficits existed earlier in the postoperative period or disappeared after a period of time.
This investigation demonstrated that landing mechanics represented by peak hip and knee joint angles in all 3 planes of motion were similar between healthy, noninjured women and women with more than 1 year after ACL reconstruction. These data suggest that landing mechanics might be restored after surgical reconstruction of the ACL in physically active young women and support the findings of Decker et al,10 who reported no differences in peak hip and knee joint flexion angles between women with ACL reconstruction and noninjured recreational athletes during the landing from a 60-cm bilateral drop jump. The present kinematic findings contradict several investigations in which restoration of function in patients with ACL reconstruction was not found during the performance of different functional tasks.5,33
Previous research has demonstrated that individuals labeled as copers exhibit jumping strategies similar to those of noninjured individuals.37-39 Although the labels copers and noncopers have been attributed only to ACL-deficient individuals,37-39 patients with ACL reconstruction could be categorized in a similar fashion given the fact that not all patients with ACL reconstruction can return to their previous levels of function.12,13 Several researchers have demonstrated that patients with ACL reconstruction exhibit similar tibial internal/external rotation,22 similar anterior-posterior femoral translation,22 and identical integrated EMG of the quadriceps and hamstring muscle groups43 compared with noninjured individuals. Therefore, it might be possible that all participants with ACL reconstruction in this investigation belong to the group of copers in which ACL reconstruction returned function to the reconstructed knee joint. These compensatory strategies could be related to restoration of mechanical function of the knee joint,22,43 neuromuscular plasticity,16 reactivation of preinjury neuromuscular patterns,43 or graft reinnervation.43 Nonetheless, this categorization requires further exploration before conclusions can be drawn.
The statistically significant greater normalized EMG for the gluteus maximus and quadriceps and the quadriceps/hamstrings cocontraction ratios in the group with ACL reconstruction contradict the initial hypothesis. A previous study reported greater hamstring normalized averaged EMG in ACL-deficient individuals as a compensatory strategy to increase dynamic stability at the knee in functional activities.4 However, literature reporting greater gluteus maximus or rectus femoris EMG in ACL-reconstructed participants when compared with noninjured individuals is scarce. Several investigators11,43 reported similarities in integrated EMG of thigh muscles between ACL-reconstructed patients and noninjured individuals during functional activities. Neuromuscular strategies that could explain these findings have been assessed by several researchers.23,38,40 Snyder-Mackler et al40 reported that ACL-reconstructed patients did not present quadriceps femoris muscle inhibition measured by a burst-superimposition technique during maximal isometric quadriceps contraction 3 months after surgical reconstruction. Keays et al23 reported statistically significant improvements in performance during several agility tasks after ACL reconstruction, although quadriceps femoris strength deficits existed. Rudolph et al38 reported quadriceps and hamstrings neuromuscular activity results similar to previous investigations during hopping activities between copers and noninjured individuals. These findings indicate that ACL-reconstructed and ACL-deficient patients develop neuromuscular strategies that helped them reach levels of dynamic joint stability needed to perform functional tasks.
Previous studies2,25,26 assessing knee joint stability using the cocontraction ratio found the level of difficulty of a specific task dictated the amount of neuromuscular activation and subsequently the level of dynamic knee joint stability required for task completion. In addition, neuromuscular activation increases as the specific task creates greater joint moments in the frontal and transverse planes.2,25,26 It may be possible that the greater neuromuscular activation observed in the ACL-reconstructed participants represents an indication of the magnitude of difficulty and eccentric loading they experienced in performing the drop jump task. Perhaps the participants with ACL reconstruction required greater cocontraction and normalized gluteus maximus and rectus femoris EMG activation as an indication of greater difficulty in controlling the eccentric landing component of the drop jump compared with the healthy, noninjured group.2,25,26 In addition, increased cocontraction between agonists and antagonists has been associated with the process of learning new skills to simplify the task and increase lower extremity stability.44 Therefore, it may be possible that the increased EMG activity observed in the participants with ACL reconstruction would be an indication of such strategies to perform the drop jump successfully. Although no statistically significant differences were found for the hamstrings EMG data, the fact that the lateral and medial components of the hamstring muscle group play different roles in rotational stability of the knee needs to be taken into consideration.4,43 In this investigation, the EMG values of the medial and lateral hamstrings were averaged as a representation of the hamstring muscle on its entirety as developed by Lloyd and Buchanan.26 Future investigations should consider different components of the hamstring muscle group separately to describe more accurately the rotational control of the knee joint in young women with ACL reconstruction. In addition, given that 3 of the participants had ACL reconstruction with a semitendinosus-gracilis tendon autograft, this population needs special attention when evaluating EMG from the hamstring muscle group. Delayed firing rate and lesser neuromuscular activation between the medial hamstring and the lateral hamstring muscle groups4,43 are a special consideration in this population.
Kinetic comparisons between individuals with ACL reconstruction and noninjured participants showed varied results. The lower anterior-posterior shear forces observed in the group with ACL reconstruction compared with the noninjured group contradict the initial study hypothesis. However, the greater cocontraction ratios exhibited by the women with ACL reconstruction could explain these results. Increased cocontraction ratios have been shown to provide stability to the knee joint, decreasing anterior-posterior shear forces during athletic moments in all planes of motion.26 Pflum et al32 studied landing mechanics through computerized bio-mechanical modeling during a 60-cm bilateral drop jump task and concluded that the stresses to the ACL were not only related to position of the knee joint on landing but mainly to the compressive forces and the direction of the ground-reaction forces.32 Other kinematic variables that could influence landing mechanics such as trunk motion should be considered in future investigations.
Up-Down
Except for peak extension moments, the group with ACL reconstruction demonstrated in the up-down task that symmetrical landing mechanics and neuromuscular performance between the reconstructed and noninjured limb could be achieved by at least 1 year after surgical reconstruction. Because the uninjured limb exhibited greater joint extension moments, it is possible that increased loading to the ACL created by the activation of the quadriceps muscle group in the uninjured knee increased injury-predisposing loads during high–demand tasks.44
The lack of statistically significant differences between groups in the up-down hop task contradicted the study hypotheses. Kanisawa et al22 reported similar results for kinematics and kinetics comparing 12 noninjured subjects and 12 individuals with ACL reconstruction during a 25-cm walking step-up and step-down task. The investigators concluded that ACL reconstruction seemed to restore weightbearing function during step-up and step-down tasks that resembled the stepping strategies of non-injured individuals.22 Similar conclusions can be drawn from this investigation in spite of the greater physical demands required for the up-down task as compared with a step-up and step-down task. The up-down hop task was able to discriminate between levels of jumping ability31 and correlated with levels of ligamentous knee joint laxity.20,21 Therefore, it can be concluded that performance of such tasks can be restored in ACL-reconstructed women.
According to Ristanis et al,33 individuals with ACL reconstruction exhibit rotational deficits after successful reconstruction in high-demand activities with large eccentric loads. They assessed men with ACL reconstruction at least one year after surgery, ACL-deficient men, and noninjured men during a 40-cm bilateral drop jump. On landing, participants were required to perform five 90° pivots to each side. The primary measure in this study was peak knee external rotation during the 90° pivoting maneuver. The ACL-reconstructed patients exhibited rotational deficits similar to those of ACL-deficient individuals, whereas both injured groups differed significantly from the control group. The authors concluded that although ACL reconstruction has been shown to stabilize the knee against any anterior-posterior displacement, ACL-reconstructed patients were not able to regain rotational stability during pivoting maneuvers.33 The investigators also mentioned that knee stability could be restored for low-demand activities in which no high-speed rotations are required.33
The up-down task is performed primarily in the sagittal plane and does not require sharp angle rotations during its execution. Therefore, based on previous statements, the up-down task does not have the sensitivity to identify rotational deficits in patients with ACL reconstruction. It seems that function in activities with minimal to moderate eccentric and rotational loads can be restored successfully after ACL reconstruction in young women. Pivoting and cutting maneuvers, especially side-stepping techniques, are the greatest external knee loading maneuvers in sports.25 Given that most sports require unanticipated cutting and pivoting maneuvers at high speeds during execution of specific movements, such as evading an opponent,2,3 full restoration of dynamic stability would be required to return to sports. Therefore, further research is necessary to address lower extremity biomechanics during cutting and pivoting maneuvers in young women after ACL surgery.
There are several limitations that need consideration before conclusions can be drawn from this investigation. Although the interest of this investigation was to draw conclusions about young female athletes, the level of athleticism of the participants was at a recreational level. Therefore, it can only be hypothesized that elite or highly competitive female athletes would exhibit the same landing mechanics and neuromuscular strategies as those of the women in this investigation. The mean and SD for time after surgery was 7.2 ± 4.2 years (range, 1−16 years) after reconstruction. This variability shows that the sample of women with ACL reconstruction was heterogeneous in relation to time after reconstruction. Given the size of the sample in this group, stratified analysis was not possible to determine if differences existed between time elapsed after ACL reconstruction. Therefore, further research is needed to assess landing mechanics at different times after ACL surgery in young women. Participants in this investigation were recruited by word of mouth. Therefore, ACL reconstruction was performed by different orthopaedic surgeons, making it impossible to control for these factors. In addition, the women with ACL reconstruction had different types of reconstructions (patellar graft, 9; Achilles tendon allograft, 2; gracilis-semitendinosus grafts, 3). Given the small sample size per group, comparisons between these 3 groups were not appropriate. Further research evaluating functional outcomes and landing mechanics in women with different types of ACL reconstruction is warranted.
Other studies have found that external varus and valgus moments cause ACL injury at the same magnitude during athletic maneuvers.3 This study only assessed peak knee valgus as external moments in the mediolateral plane. Assessment of varus moments during these tasks requires further exploration.
Women undergoing ACL reconstruction overcome a major surgery and long rehabilitation process. It is unknown how psychological factors affect landing mechanics and if they play a major role in neuromuscular adaptations during functional activities. Further research evaluating fear avoidance and psychological factors is warranted. Finally, the 2 tasks used in this investigation were planned activities. Unplanned athletic tasks in which individuals need to react to a surprising and sudden stimulus increase knee injury–predisposing factors.2,3 Hence, it is still unknown how women with ACL reconstruction will react to high-demand, unplanned athletic activities and if they will be able to perform at highly competitive levels with minimal risk of reinjury.
Despite these limitations, the information provided helps us understand several biomechanical and neuromuscular behaviors in women with ACL reconstruction compared to those of young women without knee injury. After taking into consideration the results and limitations of this study, several questions remain unanswered. Do women with different types of ACL reconstruction exhibit different biomechanical and neuromuscular landing strategies? Should specific rehabilitation protocols be developed for each specific surgical procedure to address the specific deficits of each reconstruction procedure? At what moment in time do biomechanical and neuromuscular compensations start to develop after ACL reconstruction?
CONCLUSION
This study suggests women with ACL reconstruction exhibit nearly symmetrical function between limbs during both tasks. In addition, young women with ACL reconstruction reveal different landing strategies when compared with noninjured women during a drop jump that requires high eccentric loads. However, in tasks with minimal to moderate eccentric and rotational loads such as the up-down, the women with ACL reconstruction present landing strategies similar to those of the noninjured group.
ACKNOWLEDGMENT
We acknowledge Heidi Venegas, DrPH candidate from the School of Public Health at the University of North Texas and instructor at the School of Public Health of the University of Puerto Rico, for her assistance in statistical analyses. In addition, we thank Carlos Ortiz and Anadel Castro for their assistance with figures and graphical representation of results. This study was supported in part by an institutional grant (Research Enhancement Program) from Texas Woman's University. This investigation was supported, in part, by an RCMI Clinical Research Infrastructure Initiative (RCRCII) award, 1P20 RR11126, from the National Center for Research Resources (NCRR), National Institutes of Health.
Footnotes
No potential conflict of interest declared.
REFERENCES
- 1.Ageberg E. Consequences of a ligament injury on neuromuscular function and relevance to rehabilitation: using the anterior cruciate ligament–injured knee as model. J Electromyogr Kinesiol. 2002;12(3):205–212. doi: 10.1016/s1050-6411(02)00022-6. [DOI] [PubMed] [Google Scholar]
- 2.Besier TF, Lloyd DG, Ackland TR. Muscle activation strategies at the knee during running and cutting maneuvers. Med Sci Sports Exerc. 2003;35(1):119–127. doi: 10.1097/00005768-200301000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Besier TF, Lloyd DG, Ackland TR, Cochrane JL. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33(7):1176–1181. doi: 10.1097/00005768-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Boerboom AL, Hof AL, Halbertsma JP, et al. Atypical hamstrings electromyographic activity as a compensatory mechanism in anterior cruciate ligament deficiency. Knee Surg Sports Traumatol Arthrosc. 2001;9(4):211–216. doi: 10.1007/s001670100196. [DOI] [PubMed] [Google Scholar]
- 5.Bonfim TR, Jansen Paccola CA, Barela JA. Proprioceptive and behavior impairments in individuals with anterior cruciate ligament reconstructed knees. Arch Phys Med Rehabil. 2003;84(8):1217–1223. doi: 10.1016/s0003-9993(03)00147-3. [DOI] [PubMed] [Google Scholar]
- 6.Chappell JD, Yu B, Kirkendall DT, Garrett WE. A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Am J Sports Med. 2002;30(2):261–267. doi: 10.1177/03635465020300021901. [DOI] [PubMed] [Google Scholar]
- 7.Chong RW, Tan JL. Rising trend of anterior cruciate ligament injuries in females in a regional hospital. Ann Acad Med Singapore. 2004;33(3):298–301. [PubMed] [Google Scholar]
- 8.Cram JR, Kasman GS, Holtz J. Introduction to Surface Electromyography. Aspen; Gaithersburg, MD: 1998. [Google Scholar]
- 9.Croce RV, Russell PJ, Decoster LC. Knee muscular response strategies differ by developmental level but not gender during jump landing. Electromyogr Clin Neurophysiol. 2004;44:339–348. [PubMed] [Google Scholar]
- 10.Decker MJ, Torry MR, Noonan TJ, Riviere A, Sterett WI. Landing adaptations after ACL reconstruction. Med Sci Sports Exerc. 2002;34(9):1408–1413. doi: 10.1097/00005768-200209000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Demont RG, Lephart SM, Giraldo JL, Swanik CB, Fu FH. Muscle pre-activity of anterior cruciate ligament–deficient and –reconstructed females during functional activities. J Athl Train. 1999;34(2):115–120. [PMC free article] [PubMed] [Google Scholar]
- 12.Fithian DC, Paxton LW, Goltz DH. Fate of the anterior cruciate ligament–injured knee. Orthop Clin North Am. 2002;33(4):621–636. doi: 10.1016/s0030-5898(02)00015-9. [DOI] [PubMed] [Google Scholar]
- 13.Frank CB, Jackson DW. The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1997;79(10):1556–1576. doi: 10.2106/00004623-199710000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Friden T, Roberts D, Ageberg E, Walden M, Zatterstrom R. Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture. J Orthop Sports Phys Ther. 2001;31(10):567–576. doi: 10.2519/jospt.2001.31.10.567. [DOI] [PubMed] [Google Scholar]
- 15.Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Hoffman M, Schrader J, Koceja D. An investigation of postural control in postoperative anterior cruciate ligament reconstruction patients. J Athl Train. 1999;34(2):130–136. [PMC free article] [PubMed] [Google Scholar]
- 17.Huston LJ, Vibert B, Ashton-Miller JA, Wojtys EM. Gender differences in knee angle when landing from a drop-jump. Am J Knee Surg. 2001;14(4):215–220. [PubMed] [Google Scholar]
- 18.Hutchinson MR, Ireland ML. Knee injuries in female athletes. Sports Med. 1995;19(4):288–302. doi: 10.2165/00007256-199519040-00006. [DOI] [PubMed] [Google Scholar]
- 19.Ireland ML. The female ACL: why is it more prone to injury? Orthop Clin North Am. 2002;33(4):637–651. doi: 10.1016/s0030-5898(02)00028-7. [DOI] [PubMed] [Google Scholar]
- 20.Itoh H, Ichihashi N, Maruyama T, Kurosaka M, Hirohata K. Weakness of thigh muscles in individuals sustaining anterior cruciate ligament injury. Kobe J Med Sci. 1992;38(2):93–107. [PubMed] [Google Scholar]
- 21.Itoh H, Kurosaka M, Yoshiya S, Ichihashi N, Mizuno K. Evaluation of functional deficits determined by four different hop tests in patients with anterior cruciate ligament deficiency. Knee Surg Sports Traumatol Arthrosc. 1998;6(4):241–245. doi: 10.1007/s001670050106. [DOI] [PubMed] [Google Scholar]
- 22.Kanisawa I, Banks AZ, Banks SA, Moriya H, Tsuchiya A. Weight-bearing knee kinematics in subjects with two types of anterior cruciate ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. 2003;11(1):16–22. doi: 10.1007/s00167-002-0330-y. [DOI] [PubMed] [Google Scholar]
- 23.Keays SL, Bullock-Saxton J, Keays AC. Strength and function before and after anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2000;373:174–183. doi: 10.1097/00003086-200004000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Lilley K, Gass E, Locke S. A retrospective injury analysis of state representative female soccer players. Phys Ther Sport. 2002;3:2–9. [Google Scholar]
- 25.Lloyd DG. Rationale for training programs to reduce anterior cruciate ligament injuries in Australian football. J Orthop Sports Phys Ther. 2001;31(11):645–654. doi: 10.2519/jospt.2001.31.11.645. discussion 661. [DOI] [PubMed] [Google Scholar]
- 26.Lloyd DG, Buchanan TS. Strategies of muscular support of varus and valgus isometric loads at the human knee. J Biomech. 2001;34(10):1257–1267. doi: 10.1016/s0021-9290(01)00095-1. [DOI] [PubMed] [Google Scholar]
- 27.Manolopoulos E, Papadopoulos C, Kellis E. Effects of combined strength and kick coordination training on soccer kick biomechanics in amateur players. Scand J Med Sci Sports. 2006;16(2):102–110. doi: 10.1111/j.1600-0838.2005.00447.x. [DOI] [PubMed] [Google Scholar]
- 28.McHugh MP, Tyler TF, Browne MG, Gleim GW, Nicholas SJ. Electromyographic predictors of residual quadriceps muscle weakness after anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30(3):334–339. doi: 10.1177/03635465020300030601. [DOI] [PubMed] [Google Scholar]
- 29.McNitt-Gray JL. Musculoskeletal loading during landing. In: Zatsiorsky VM, IOC Medical Commission, International Federation of Sports Medicine, editor. Biomechanics in Sport: Performance Enhancement and Injury Prevention. Blackwell Science; Malden, Mass: 2000. pp. 523–549. [Google Scholar]
- 30.Myer GD, Ford KR, Hewett TE. Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes. J Athl Train. 2004;39(4):352–364. [PMC free article] [PubMed] [Google Scholar]
- 31.Ortiz A, Olson SL, Roddey TS, Morales J. Reliability of selected physical performance tests in young adult women. J Strength Cond Res. 2005;19(1):39–44. doi: 10.1519/14163.1. [DOI] [PubMed] [Google Scholar]
- 32.Pflum MA, Shelburne KB, Torry MR, Decker MJ, Pandy MG. Model prediction of anterior cruciate ligament force during drop-landings. Med Sci Sports Exerc. 2004;36(11):1949–1958. doi: 10.1249/01.mss.0000145467.79916.46. [DOI] [PubMed] [Google Scholar]
- 33.Ristanis S, Stergiou N, Patras K, Vasiliadis HS, Giakas G, Georgoulis AD. Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(11):1323–1329. doi: 10.1016/j.arthro.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 34.Rodacki AL, Fowler NE, Bennett SJ. Multi-segment coordination: fatigue effects. Med Sci Sports Exerc. 2001;33(7):1157–1167. doi: 10.1097/00005768-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Rodacki AL, Fowler NE, Bennett SJ. Vertical jump coordination: fatigue effects. Med Sci Sports Exerc. 2002;34(1):105–116. doi: 10.1097/00005768-200201000-00017. [DOI] [PubMed] [Google Scholar]
- 36.Ross MD, Irrgang JJ, Denegar CR, McCloy CM, Unangst ET. The relationship between participation restrictions and selected clinical measures following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2002;10(1):10–19. doi: 10.1007/s001670100238. [DOI] [PubMed] [Google Scholar]
- 37.Rudolph KS, Axe MJ, Buchanan TS, Scholz JP, Snyder-Mackler L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9(2):62–71. doi: 10.1007/s001670000166. [DOI] [PubMed] [Google Scholar]
- 38.Rudolph KS, Axe MJ, Snyder-Mackler L. Dynamic stability after ACL injury: who can hop? Knee Surg Sports Traumatol Arthrosc. 2000;8(5):262–269. doi: 10.1007/s001670000130. [DOI] [PubMed] [Google Scholar]
- 39.Rudolph KS, Eastlack ME, Axe MJ, Snyder-Mackler L. Basmajian Student Award Paper. Movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;1998;8(6):349–362. doi: 10.1016/s1050-6411(97)00042-4. [DOI] [PubMed] [Google Scholar]
- 40.Snyder-Mackler L, De Luca PF, Williams PR, Eastlack ME, Bartolozzi AR., III Reflex inhibition of the quadriceps femoris muscle after injury or reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1994;76(4):555–560. doi: 10.2106/00004623-199404000-00010. [DOI] [PubMed] [Google Scholar]
- 41.Soderberg GL, Knutson LM. A guide for use and interpretation of kinesiologic electromyographic data. Phys Ther. 2000;80(5):485–498. [PubMed] [Google Scholar]
- 42.Soderman K, Pietila T, Alfredson H, Werner S. Anterior cruciate ligament injuries in young females playing soccer at senior levels. Scand J Med Sci Sports. 2002;12(2):65–68. doi: 10.1034/j.1600-0838.2002.120201.x. [DOI] [PubMed] [Google Scholar]
- 43.Swanik CB, Lephart SM, Giraldo JL, Demont RG, Fu FH. Reactive muscle firing of anterior cruciate ligament–injured females during functional activities. J Athl Train. 1999;34(2):121–129. [PMC free article] [PubMed] [Google Scholar]
- 44.Teixeira da Fonseca S, Silva PL, Ocarino JM, Guimaraes RB, Oliveira MT, Lage CA. Analyses of dynamic co-contraction level in individuals with anterior cruciate ligament injury. J Electromyogr Kinesiol. 2004;14(2):239–247. doi: 10.1016/j.jelekin.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 45.Toth AP, Cordasco FA. Anterior cruciate ligament injuries in the female athlete. J Gend Specif Med. 2001;4(4):25–34. [PubMed] [Google Scholar]
- 46.Walsh M, Arampatzis A, Schade F, Bruggemann GP. The effect of drop jump starting height and contact time on power, work performed, and moment of force. J Strength Cond Res. 2004;18(3):561–566. doi: 10.1519/1533-4287(2004)18<561:TEODJS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 47.Wikstrom EA, Powers ME, Tillman MD. Dynamic stabilization time after isokinetic and functional fatigue. J Athl Train. 2004;39(3):247–253. [PMC free article] [PubMed] [Google Scholar]