Abstract
Purpose
The clinical manifestations of BPH that are more likely to bring African-American men in for care have not been well characterized. In this study, we examined associations between lower urinary tract symptom severity measures on subsequent health care-seeking behavior in a population-based sample of African American men.
Methods
In 2000, 165 African-American men from Genesee County, Michigan aged 40-79 without a prior history of prostate cancer/surgery provided information on LUTS and health care-seeking behaviors. The associations between physician visits regarding LUTS and symptom frequency, perceived bother, impact on daily activities and quality of life were examined controlling for age and socio-demographic characteristics.
Results
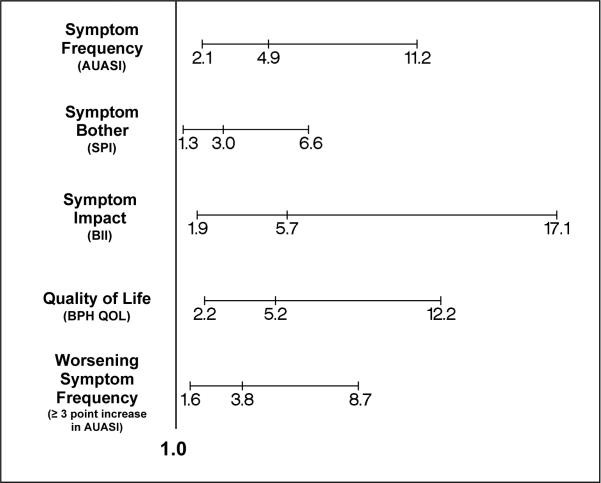
Overall, 22.2% of men sought medical advice for LUTS. Men with moderate/severe symptom severity and associated bother had 4.9- and 3.0-fold increased odds, respectively, of having sought medical care for their symptoms as compared to those with mild/no symptom severity or bother. Greater increases in physician visits were observed for increases in BPH impact (OR=5.7, 95%CI: 1.9, 17.1), QOL (OR=5.2, 95%CI: 2.2, 12.2) and worsening symptoms (OR=3.8, 95%CI: 1.6, 8.7). Health care-seeking was associated with irritative and obstructive symptom severity (OR=1.4, 95%CI: 1.2, 1.6 and OR=1.2, 95%CI: 1.1, 1.3), respectively.
Conclusion
In this population-based study of African-American men we found that worsening urinary symptoms, associated bother, impact and quality of life were significantly associated with health care-seeking behavior. Irritative symptom severity was most highly associated with health care-seeking behavior. Further evaluations are necessary to determine whether racial differences exist in health-seeking behavior for LUTS.
Keywords: LUTS, African-American, BPH, Health-seeking behavior
INTRODUCTION
Benign prostatic hyperplasia (BPH) is the most common benign neoplasm in American men and is characterized by the progressive development of lower urinary tract symptoms (LUTS).1 It has been documented that in Caucasian men, LUTS have a significant negative impact on quality of life leading many to seek medical treatment.2,3 While the diagnosis of BPH is associated with increased health care resource utilization in Caucasian men, a study using National Hospital Discharge Survey data demonstrated that hospital discharge rates for prostatectomy related to BPH were lower for African-Americans in the 1980s.4 Furthermore, prior work has demonstrated significant racial differences in LUTS severity with African-American men reporting greater LUTS severity but less bother for each unit increase in LUTS compared to Caucasian men.5 This finding may explain the racial variation in utilization rates for BPH therapy as this study suggests African-American men may be less bothered given the same severity of LUTS, which may in turn result in differential health seeking behavior.
Given the known racial inequities in health care, it would be beneficial to determine the factors that bring African-American men to care in a community setting. Therefore, the objective of the current study was to identify the impact of LUTS and socio-demographic characteristics on the likelihood of seeking health-care for BPH using the resources of The Flint Men's Health Study, a population-based cohort of African-American men aged 40-79 years.
MATERIALS AND METHODS
Subjects
Many of the details have been previously published.6 Briefly, 730 age and race-eligible subjects with no history of prostate cancer or surgery completed a detailed in-home epidemiologic interview on risk factors for prostate disease. At the conclusion of the interview, subjects were asked to undergo a prostate cancer screening protocol, which included a serum prostate-specific antigen (PSA) measurement, uroflowmetry, digital rectal examination (DRE), and transrectal ultrasound (TRUS). Participants also completed self-administered questionnaires regarding LUTS experience. Men with an abnormal DRE and/or elevated total PSA concentration (≥ 4.0 ng/mL) were referred for prostate biopsy. A total of 379 men completed the protocol and 10 men were diagnosed with biopsy-confirmed prostate cancer and subsequently excluded from the study. Four years after baseline, 175 of the 369 men (47%) who participated in the baseline clinical exam were re-contacted and completed the same study protocol described above. Six men diagnosed with biopsy-confirmed prostate cancer at the 4-year follow-up and four men missing symptom information either at baseline or follow-up were excluded resulting in 165 men for whom we present data in the current study. (Table 1)
Urinary Symptom Measurements
Lower urinary symptom severity, perceived bother and impact from those symptoms, and quality of life were gathered using the American Urological Association Symptom Index (AUASI), Symptom Problem Index (SPI), BPH Impact Index (BII), and the single item Quality of Life (QOL) question by self-administered questionnaires from all subjects participating in the clinic phase in the FMHS. The AUASI is a self-administered questionnaire including elements about severity of urinary symptoms attributed to BPH.7 Seven questions elicited information about the frequency of specific urinary symptoms during the past month. Symptom frequency questions were measured on a 6-point scale from 0 (never) to 5 (always). The reliability and validity of these questions have been reported elsewhere.7-9 The SPI consists of seven questions and seeks to determine how much of a problem the urinary symptoms assessed by the AUASI are and is measured on a 5 point scale from 0 (no problem) to 4 (big problem).10 The BPH Impact Index (BII) was administered to assess impairment and bother due to BPH symptoms.10 The BII is a 4 question survey that is measured on a 4 to 5 point scale varying from none to a lot. Quality of Life Due to Urinary Symptoms (QOL Index) was ascertained by asking subjects how they would feel if they were to spend the rest of their life with their current urinary condition, and was scored on a 7-point scale from 0 (delighted) to 6 (terrible).11 Worsening symptoms were defined as greater than a three point increase in symptom score over the past four years.
Health Care-Seeking Behavior Measures
The primary endpoint in this study was the subject's self report of a physician visit for each of the seven specific symptoms of the AUASI during the past year.
Statistical Analysis
The primary outcome for all analyses was an affirmative response to any of the questions about seeking consultation from a physician in the last year. The proportion of men having sought medical care in the last year for their urinary symptoms was calculated by categories of socio-demographic characteristics at baseline and symptom characteristics at follow-up. Differences in proportions were tested with a χ2 statistic and trends in proportions across ordinal variables were tested with the Mantel Haenszel chi-square tests. LUTS severity was categorized as mild/none (AUASI≤7) and moderate/severe (AUASI>8). Moderate to severe bother and impact were defined as an SPI and BII score of >3 and ≥5, respectively. Quality of life was categorized as good (QOL<3) vs. poor (QOL≥3) and worsening symptoms were defined as greater than a 3 point increase in symptom score from baseline and dichotomized as yes vs. no. To quantify the ability of the AUASI, SPI, BII, QOL and worsening symptoms to identify the men who reported having sought medical care, receiver operator characteristic curves were constructed for each of the indexes, plotting sensitivity vs. 1-specificity.
Odds ratios and 95% confidence intervals were also calculated to examine the associations between individual symptom severity and healthcare-seeking behavior. Finally, multivariable-adjusted logistic regression models were built to evaluate associations between measures of symptom severity and health care-seeking behavior while controlling for age and employment status. A p-value of < 0.05 was considered statistically significant. All analyses were done using SAS Version 9.1.
RESULTS
Overall, 37 (22%) of the 165 men reported seeing a physician in the prior year for treatment of urinary symptoms. (Table 2) The proportion of men seeking medical attention did not differ significantly by baseline age, income, education, health insurance or marital status (all p>0.05). Men who reported being employed in the previous 12 months at baseline, were significantly less likely to seek medical advice for their urinary symptoms as compared to men who were unemployed/retired (p=0.01).
In general, the proportion of men having sought medical care in the last year for their urinary symptoms increased significantly with severity of symptoms as measured by frequency (p=0.0001), bother (p=0.007), impact (p=0.001), quality of life (p=0.0002), and worsening of symptoms (p=0.0009). (Table 3)
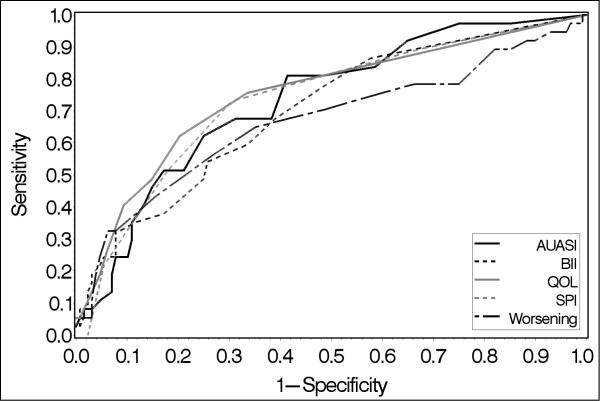
Symptom severity as measured by frequency, bother, impact, quality of life or worsening of symptoms over time, identified marginally well, men who reported health care-seeking behavior for urinary symptoms. (Figure 1) The mean area under the curve (AUC) was 0.73 for AUA symptom scores, 0.70 for bother scores and 0.67 for worsening of symptoms. The mean AUCs for impact and QOL scores appear slightly higher (AUC=0.75 and 0.73, respectively), however, these findings were not statistically significant (p>0.05).
FIGURE 1.
Receiver Operator Characteristic curves of symptom severity (frequency, bother, impact, quality of life scores and worsening of symptom frequency) and healthcare seeking behavior.
Frequencies of men who reported a physician visit for each individual symptom are summarized in Table 4. Overall 20% of men reported seeking medical attention for irritative urinary symptoms compared to 17% for obstructive symptoms. The symptoms with the greatest proportion of men having sought medical advice include: frequency, nocturia, incomplete emptying and urgency.
In separate multivariable logistic regression models controlling for age and employment during the past year, AUASI score, bother score, bother impact score, QOL score and worsening symptoms over the past 4 years were all significant predictors of health care-seeking behavior for urinary symptoms. (Figure 2) The association between employment during the past year at baseline remained significantly strong after controlling for age and symptom severity with an average 70% reduced odds of health care-seeking behavior in all models. (data not shown) Age was not significantly associated with health-seeking behavior in any of the models. (data not shown)
FIGURE 2.
Multivariable-Adjusted Odds Ratios (95% CI) of Symptom Characteristics and Health Care-Seeking Behavior
*Odds Ratios for moderate/severe vs. mild/none for Symptom Frequency, Bother and Impact; yes vs. no for Worsening Symptoms defined as =3 point increase in AUASI since baseline; Poor vs. Good for QOL; Adjusted for Baseline age and employment in past year in all models
DISCUSSION
In this population-based study of African-American men aged 40-79, we found that overall, symptom severity, whether measured by frequency, worsening symptoms, perceived bother, impact on daily activities or quality of life was significantly associated with having sought medical care for treatment of these problems in the last year. Of the various measures of symptom severity, impact on daily activities and quality of life scores appeared to better identify men who had sought medical care than AUA frequency scores. While these findings are consistent with those observed in Caucasian men,12 these data additionally demonstrate that worsening of symptoms over time significantly influences health care seeking behavior in African-American men. This association persisted and increased even after controlling for baseline symptom frequency (OR=5.4, 95%CI=2.1, 13.5).
These findings could be due to incorporation of an individual's perception of symptom bother, which may have been greater than symptom frequency. The amount of impact symptoms have on daily activities or quality of life appears to represent an additional dimension of symptoms not captured by the AUA frequency or bother scores. Similarly, the persistent significant association of worsening of symptoms over the past four years with health care-seeking behavior even after controlling for symptom severity, suggests that perceptions of changes in symptoms also play a role in seeking medical care for urinary problems. These findings are consistent with previous reports which suggest a more important role for psychosocial components of symptom experience in the decision to seek treatment.3,13-16
An increase in symptom severity in all of the individual symptoms was significantly associated with health care-seeking behavior. However, odds of physician visit were consistently greater for report of worsening irritative symptoms (frequency, nocturia, urgency) compared to progression of obstructive symptoms (incomplete emptying, straining, weak stream, intermittency). In a previously published report on concomitant longitudinal changes in LUTS frequency and associated bother, we found that symptoms that are irritative or socially embarrassing were more important in perceived bother.17 These previous findings may explain those of the current report which suggest irritative symptom severity to be more highly associated with report of physician visit.
Interestingly, the associations we observed between measures of symptom severity and health care-seeking behavior in African-American men appear to be greater than those reported in white men in the OCS.12 These observations suggest that some component(s) of lower urinary symptom experience is/are more likely to bring African-American men in for medical advice compared to their Caucasian counterparts. One potential explanation for any apparent differences could be due to the increased interest of African-American men to consult medical advice concerning urinary problems out of concern for prostate cancer. However, we found no significant associations between report of DRE or PSA testing during the last five years and physician visit for urinary symptoms. Moreover, adjustment for these additional measures of health seeking behavior did not significantly impact the magnitude or significance of the observed associations between measures of symptom severity and health-care seeking behavior suggesting that some other unmeasured component of health seeking behavior may be involved. It is also possible that the participants included in this analysis (i.e. men who returned for the second wave of the FMHS) were more worried or concerned about urologic conditions thereby increasing the likelihood of seeking care. These comparisons are based on observations of summary rates only and direct comparisons using individual level data are necessary to determine whether racial differences in health-seeking behavior for urinary symptoms do indeed exist.
Despite the significant findings regarding the associations between measures of symptom severity and health care-seeking behavior, a measurable proportion of our cohort reporting significant LUTS frequency (32.2%) and associated bother (33.6%) still did not report seeing a physician regarding their symptoms. The belief that urinary symptoms are just part of growing older may, in part, account for the overall failure of men to seek medical advice.13 Interestingly, we observed men who were employed were significantly less likely to visit a physician regarding their urinary symptoms regardless of the magnitude and type of symptom severity reported. This observation could be the result of men simply not having or taking the time to seek medical care due to employment obligations. It is also possible that non-employed men have more time to ruminate over symptoms and/or seek advice from friends or family with similar experience. Other reasons for the lack of seeking care could include perhaps that men might be postponing visits to their health care provider in an attempt to self manage symptoms by adjusting life style, or that embarrassment or shame from urinary conditions continues to inhibit patients from visiting their physicians.3,16,18
While our data indicate significant associations between measures of LUTS severity and health seeking behavior in African American men, several limitations should be considered. The FMHS protocol excluded all men who were previously diagnosed with prostate cancer and/or who had undergone prostate surgery. As current clinical practice suggests men with increased symptoms are more likely to receive surgical treatment, it is possible the magnitude of LUTS may have been underestimated in this cohort thereby excluding men who were eligible for operative treatment from the potential study sample leaving only men with less severe disease. This exclusion may have also resulted in the selection of men with severe disease who had, for some reason, already chosen not to seek treatment or consent to operative care. However, when we excluded men who had reported taking oral medications for BPH, including PSA-altering drugs, we found no effects on our estimates of association between LUTS parameters and health-seeking behavior.
Second, there is a possibility of selection bias as a result of the limited response for the follow-up study. Due to the wording of the baseline consent and IRB determination, we were only allowed to re-contact the 369 men who participated in the clinical phase of the baseline study who were determined to be free of prostate cancer for participation in the follow-up. Of those 369 men, 52 had developed prostate cancer or died soon after the baseline study was completed and 142 refused or were lost to follow-up resulting in 175 men who agreed to participate in the follow-up study. When we examined those who participated in the follow-up (n=175) and compared them to those who refused or were lost to follow-up from 1) the 369 baseline clinic-based sample (n=194) and 2) the 730 baseline interview-based sample (n=555), we did not observe any significant differences in mean age and baseline AUASI scores. These data suggest that older men or men experiencing more significant urological problems were not more likely to participate in the follow-up study minimizing the potential for selection bias on estimates of AUASI scores.19
Despite these limitations, the results in this population-based study of LUTS in African-American men provide insight on the potential impact of LUTS severity on medical resource utilization in this population.
CONCLUSION
In this population-based study of African-American men we found that worsening urinary symptoms, associated bother and impact and quality of life were significantly associated with health care-seeking behavior. Frequency of irritative symptoms such as frequency, nocturia and urgency were most highly associated with health care-seeking behavior. Further evaluations are necessary to determine whether racial differences exist in health-seeking behavior for LUTS.
REFERENCES
- 1.Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. Journal of Urology. 1984;132:474. doi: 10.1016/s0022-5347(17)49698-4. [DOI] [PubMed] [Google Scholar]
- 2.Girman CJ, Jacobsen SJ, Tsukamoto T, Richard F, Garraway WM, Sagnier PP, et al. Health-related quality of life associated with lower urinary tract symptoms in four countries. Urology. 1998;51:428. doi: 10.1016/s0090-4295(97)00717-6. [DOI] [PubMed] [Google Scholar]
- 3.Roberts RO, Rhodes T, Panser LA, Girman CJ, Chute CG, Oesterling JE, et al. Natural history of prostatism: worry and embarrassment from urinary symptoms and health care-seeking behavior. Urology. 1994;43:621. doi: 10.1016/0090-4295(94)90174-0. [DOI] [PubMed] [Google Scholar]
- 4.Xia Z, Roberts RO, Schottenfeld D, Lieber MM, Jacobsen SJ. Trends in prostatectomy for benign prostatic hyperplasia among black and white men in the United States: 1980 to 1994. Urology. 1999;53:1154. doi: 10.1016/s0090-4295(98)00660-8. [DOI] [PubMed] [Google Scholar]
- 5.Sarma AV, Wei JT, Dunn RL, Roberts RO, Girman CJ, Lieber MM, et al. Comparison of lower urinary tract symtom severity and associated bother between community-dwelling black and white men: The Olmsted County Study of Urinary Symptoms and Health Status and the Flint Men's Health Study. Urology. 2003;61:1086. doi: 10.1016/s0090-4295(03)00154-7. [DOI] [PubMed] [Google Scholar]
- 6.Wei JT, Schottenfeld D, Cooper K, Taylor JM, Faerber GJ, Velarde MA, et al. The natural history of lower urinary tract symptoms in black American men: relationships with aging, prostate size, flow rate and bothersomeness. Journal of Urology. 2001;165:1521. [PubMed] [Google Scholar]
- 7.Barry MJ, Fowler FJ, Jr., O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148:1549. doi: 10.1016/s0022-5347(17)36966-5. [DOI] [PubMed] [Google Scholar]
- 8.Barry MJ, Fowler FJ, Jr., O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK. Correlation of the American Urological Association symptom index with self-administered versions of the Madsen-Iversen, Boyarsky and Maine Medical Assessment Program symptom indexes. Measurement Committee of the American Urological Association. J Urol. 1992;148:1558. doi: 10.1016/s0022-5347(17)36967-7. [DOI] [PubMed] [Google Scholar]
- 9.Barry MJ, O'Leary MP. Advances in benign prostatic hyperplasia. The developmental and clinical utility of symptom scores. Urol Clin North Am. 1995;22:299. [PubMed] [Google Scholar]
- 10.Barry MJ, Williford WO, Chang Y, Machi M, Jones KM, Walker-Corkery E, et al. Benign prostatic hyperplasia specific health status measures in clinical research: how much change in the American Urological Association symptom index and the benign prostatic hyperplasia impact index is perceptible to patients? Journal of Urology. 1995;154:1770. doi: 10.1016/s0022-5347(01)66780-6. [DOI] [PubMed] [Google Scholar]
- 11.Batista-Miranda JE, Diez MD, Bertran PA, Villavicencio H. Quality-of-life assessment in patients with benign prostatic hyperplasia: effects of various interventions. Pharmacoeconomics. 2001;19:1079. doi: 10.2165/00019053-200119110-00002. [DOI] [PubMed] [Google Scholar]
- 12.Jacobsen SJ, Guess HA, Panser LA, Girman CJ, Chute CG, Oesterling JE, et al. A Population-Based Study of Health Care-Seeking Behavior for Treatement of Urinary Symptoms. The Olmsted County Study of Urinary Symptoms and Health Status Among Men. Archives of Family Medicine. 1993;2:729. doi: 10.1001/archfami.2.7.729. [DOI] [PubMed] [Google Scholar]
- 13.Cunningham-Burley S, Allbutt H, Garraway WM, Lee AJ, Russell EB. Perceptions of urinary symptoms and health-care-seeking behaviour amongst men aged 40-79 years. Br J Gen Pract. 1996;46:349. [PMC free article] [PubMed] [Google Scholar]
- 14.Hunter DJ, Berra-Unamuno A. Treatment-seeking behaviour and stated preferences for prostatectomy in Spanish men with lower urinary tract symptoms. Br J Urol. 1997;79:742. doi: 10.1046/j.1464-410x.1997.00136.x. [DOI] [PubMed] [Google Scholar]
- 15.Macfarlane GJ, Sagnier PP, Richard F, Teillac P, Botto H, Boyle P. Determinants of treatment-seeking behaviour for urinary symptoms in older men. Br J Urol. 1995;76:714. doi: 10.1111/j.1464-410x.1995.tb00762.x. [DOI] [PubMed] [Google Scholar]
- 16.Mozes B, Shmueli A. Underutilization of health services among patients with urinary symptoms: results of a population-based survey in Israel. Prostate. 1997;33:246. doi: 10.1002/(sici)1097-0045(19971201)33:4<246::aid-pros4>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 17.Sarma AV, Jacobsen SJ, Girman CJ, Jacobson DJ, Roberts RO, Rhodes T, et al. Concomitant longitudinal changes in frequency of and bother from lower urinary tract symptoms in community dwelling men. J Urol. 2002;168:1446. doi: 10.1016/S0022-5347(05)64471-0. [DOI] [PubMed] [Google Scholar]
- 18.Scarpa RM. Lower urinary tract symptoms: what are the implications for the patients? Eur Urol. 2001;40(Suppl 4):12. doi: 10.1159/000049890. [DOI] [PubMed] [Google Scholar]
- 19.Heeringa SG, Alcser KH, Doerr K, Strawderman M, Cooney K, Medbery B, et al. Potential selection bias in a community-based study of PSA levels in African-American men. Journal of Clinical Epidemiology. 2001;54:142. doi: 10.1016/s0895-4356(00)00270-5. [DOI] [PubMed] [Google Scholar]