Abstract
Many patient education guidelines for teaching heart failure patients recommend inclusion of the family; however, family-focused interventions to promote self-care in heart failure are few. This article reviews the state of the science regarding family influences on heart failure self-care and outcomes. The literature and current studies suggest that family functioning, family support, problem solving, communication, self-efficacy, and caregiver burden are important areas to target for future research. In addition, heart failure patients without family and those who live alone and are socially isolated are highly vulnerable for poor self-care and should receive focused attention. Specific research questions based on existing science and gaps that need to be filled to support clinical practice are posed.
Keywords: caregiver outcomes, family functioning, family support, heart failure, patient education, self-care, self-management
Efforts to bolster self-care in heart failure (HF) patients are paramount to improving behaviors related to diet and medication adherence, reducing hospitalization, and enhancing overall outcomes. Self-care in HF is quite variable, and new approaches are needed to promote preventable hospitalizations, reduce symptoms, and improve quality of life. Published clinical practice guidelines suggest that both patients with HF and their family members or care-givers should receive individualized education and counseling that emphasizes self-care1; however, the data to guide family education and care in HF are sparse. This review will examine the literature related to HF self-care and family concepts including descriptive research on family variables and behaviors, the relationship of family variables to outcomes, and family intervention studies. Finally, recommendations for HF practice and future research will be presented.
The concept of family is highly relevant to self-care, and a recent framework published by Grey and colleagues2 outlines the relationships among family factors, individual, and family self-management of chronic illness. Using a structure, process, and out-comes framework, the model identifies family structural variables as risk and protective factors that influence individual and family self-care and self-management behaviors as part of health promotion or chronic disease care. These behaviors, such as healthy eating or medication-taking activities, then lead to clinical outcomes. Family functioning (which has dimensions of adaptability, problem solving, and communication and roles) in this model also is viewed as an outcome of self-management; however, in other chronic illness populations, family functioning is often understood as a precursor to effective self-care. Regardless of where it is placed in models, when family functioning is not optimal, managing a complex self-care regimen, such as that prescribed for HF patients, will not be as effective as it could be. Better family functioning and structure leads to better over-all family health in HF families.3 Many educational interventions fail because the family and social contexts in which the individual with chronic illness is to perform self-care have not been taken into account.
Some family characteristics have been linked to poor chronic disease process and outcomes, and a greater understanding of these factors in HF is needed. The ones considered most powerful and consistent across chronic illnesses and age include poor conflict resolution, poor problem solving, low relationship satisfaction, high conflict and criticalness, high hostility, and low congruence in disease beliefs and expectations.4,5 The review of the HF literature in relation to these family factors suggests that more effort has been exerted toward studies examining the relationships between family context and self-care variables than testing interventions. A list of family concepts that are likely to affect self-care in HF patients is presented in Table 1.
TABLE 1.
Family Concepts Related to Self-care
| Family functioning |
| Family structure |
| Family social support |
| Family communication patterns |
| Family problem-solving |
| Family and caregiver self-efficacy |
| Family knowledge and skills |
Family Context and Self-care
Family Structure and Relationships
There is growing evidence that social support is associated with better outcomes of cardiovascular disease in general. Frequently, marital status is viewed as a proxy for social support. As has been noted in studies of other cardiac populations, social isolation and living alone are associated with increased HF mortality and morbidity. Increased morbidity in unmarried HF patients has been reported,6 and this association persists even when controlling for possible contributing factors, such as depression and HF severity. 7,8 Patients with HF who are not married report greater depression,9 lower quality of life especially with regard to future expectations,10 and more rehospitalizations. 10,11 The mechanism by which marital or partnered status affects such outcomes is believed to be through social support for enhanced self-care.
Some evidence for this is found in a recent report by Chung and colleagues,12 who examined medication adherence, an important self-care behavior for HF patients, by comparing patients with and without a spouse. Patients with a spouse took 90% of their HF medications as prescribed, whereas patients with-out a spouse took only 80% of medications as prescribed. In addition, patients with a spouse took more doses on schedule more often than patients without a spouse. Even though taking medications on time was a problem in both groups, patients with a spouse took 70% of medication on time, but patients without a spouse only took 49% of doses on time.12
The quality of the relationship may be more pertitinent than marital status alone for predicting some HF outcomes. Coyne and colleagues13 conducted a 4-year follow-up of HF patients, about 32%of whom were in New York Heart Association (NYHA) class III and IV and examined marital quality using home assessments, interviews, and videotaped interactions that were scored according to a standard coding system. Marital quality assessments included aspects of marital satisfaction, marital routines, useful illness discussions, and positive/facilitative rather then aversive interpersonal behaviors. Marital quality and NYHA class were independent predictors of 4-year survival, although the impact of marital quality was stronger for women than men. Rohrbaugh and colleagues14 followed the same cohort for 8 years and found that NYHA class was again a predictor; however, marital quality predicted 8-year survival only for women. A number of other psychosocial variables such as optimism, neuroticism, and hostility were examined, and only self-efficacy for managing HF was a predictor of survival. The findings of these 2 studies suggest that marital quality, defined as talking about the illness and positive interactions, has prognostic significance for survival with HF, and these interactions are more relevant to women with HF than men. A number of unanswered questions are raised by these studies, such as the influence of medications, the one-time assessment of marital quality versus examining the marital trajectory over time, the underlying mechanisms, and the influence on self-care. Nevertheless, the data underscore the significant prognostic implications of the quality of family relationships.
Family and Social Support in HF
Social support from family and friends has been linked to lower readmission rates and better medication adherence, whereas lack of emotional support and living alone is related to psychosocial distress in HF patients.11,15–19 A focus group study of perceptions of HF patients on measured medication adherence revealed that social support from family and friends as well as confidence in and communication with providers were perceived to facilitate medication-taking behavior and knowledge.20 The literature is limited in studies that actually measured self-care behaviors and social support. In addition, variations in the approaches to defining and measuring social support in HF studies limit the usefulness of translating findings into interventions.21
Family Communication and Self-care
A number of studies have provided evidence that family support has a positive influence on adoption and maintenance of health behaviors.22,23 In contrast, perceived family criticism is associated with adverse health behavior and relapse in diet and health behaviors in patients with diabetes, attempting weight loss, and asthma.24 Considerable family research has documented the deleterious effect of personal and rejecting criticism on children and patients with schizophrenia, bipolar disorder, depression, diabetes, and obesity.25 Criticism provokes distress and reduces the ability to cope with the confronting illness, and it is theorized to be related to overall family functioning.25
Autonomy support, a concept from self-determination theory,26,27 is viewed as being the opposite of criticism in terms of the tenor of communication patterns. Autonomy support from family members, health providers, and significant others promotes a sense of choice that allows individuals to engage in behavior according to their values versus doing certain things because of controlling demands or threats from others.27 Patients who perceive their family members as supportive, encouraging, conveying confidence, and providing choices engage in more positive health behaviors and behavior change. These communication influences from the family on health behaviors are similar to the effects seen with physicians who use autonomy supportive approaches.28,29 Autonomy supportive communication and approaches can be taught to spouses, partners, and adult children who might serve as caregivers in HF.30
Perceived family criticism, coercive language, and control are thought to negatively influence an individual’s health behaviors through depression,24,25,31 and depression is associated with poor adherence to self-management and health behaviors in a number of chronically ill populations.32,33 In HF patients, mental health status has been associated with overall adherence to the self-care regimen and specifically with diet and exercise adherence.34 Some controversy exists, however, in that one study did not show a relationship between depression and exercise adherence,35 whereas another study reported that anxiety was more pertinent than depression in adherence to self-care behaviors in HF.36 The different levels of depressive symptoms in the studies may have accounted for the varied findings.
Role of the Family and Symptom Management
Family members who are involved in symptom evaluation, interpretation, and response can alter the process the patient is experiencing.37,38 Lack of cooperation and/or concern about causing worry among family members and cardiovascular patients has been shown to lead to inaction when intervention was actually necessary.38–41 In other chronic illnesses, discordance between patient and family members has been associated with higher levels of distress within the dyad,42 overestimation of symptoms such as pain intensity,43,44 and higher levels of fatigue and anger.45 Focus group discussion with HF patients and family members regarding symptoms and approaches revealed similar perspectives between patients and family members on the most common symptoms such as dyspnea, fatigue, and emotional distress with the exception of differences in perceptions of cognitive deficits of concentration, attention, and memory. 46 Family members tended to identify cognitive changes more frequently than the HF patients.
A current study being conducted to examine congruence in symptom assessment between HF patient-family members has revealed some interesting preliminary findings.47 In one dyad, congruence was present for frequency and severity of depressive symptoms but not for certain physiological symptoms such as dyspnea at rest. In another dyad case, the HF patient and family member were discordant on assessing the frequency and severity of lower extremity swelling and fatigue. It may be that some symptoms are more salient for the patient than family member, and the theoretical factors involved in the level of congruence may include such things as family functioning and communication as well as education for HF symptom assessment.47 Examination of the full set of data from this study should prove enlightening.
HF Caregiver Burden and Outcomes
The responsibilities for providing care for a chronically ill family member can be overwhelming, may lead to exhaustion and depression, and can affect the health of the caregiver.48 Informal caregivers of HF patients are involved in care-giving tasks related to monitoring complex medical and self-care regimens, assisting with low-sodium diets and fluid management, assessing and managing symptoms (eg, shortness of breath and disturbed sleep), and dealing with frequent hospitalizations of patients and increasingly complex treatment devices.49 Family members providing care for HF patients have indicated that it is difficult, demanding, and associated with increased caregiver stress and anxiety and reduced QOL.50–54 Increased perceived caregiver burden is related to higher levels of caregiver depression as well as HF patient depression.55
The prevalence of emotional distress (eg, depression and anxiety), low perceived control, and negative perceived caregiving outcomes are comparable to those caring for patients with chronic conditions known to detrimentally affect informal caregivers.49,52,56,57 Caregivers of HF patients have indicated that they have specific needs and desires for improved patient-partner communication58; involvement with others to reduce social isolation59; and greater understanding of the condition, treatment, prognosis, and services available to them.60 Caregivers of elders also report issues of social isolation and do not perceive adequate ongoing professional support or resources for implementing the self-care regimen or understanding the trajectory of HF.61,62 Barnes et al61 noted in a study of caregivers of elderly HF patients that, like other chronic illnesses, caregivers tend to be women, and for HF patients, they may be elderly women with multiple health problems of their own. All of these factors have the potential for negative influences on family self-management of HF if left unaddressed.
Caregiver burden is a salient outcome of HF care, but it has not been well studied and is not tracked clinically. Caregivers of HF patients are required to do many activities similar to caregivers in other chronic illnesses, but these tasks differ from caregiving with dementia and stroke patients, for example, in that many of the recommendations for HF patients may benefit the caregiver as well, such as decreasing dietary sodium and increasing physical activity. Caregivers must be motivated to make changes as well, or it will result in increased work such as cooking separate meals. HF caregivers report that it takes extra time to shop for low-sodium foods until they establish a routine and, many times, adjust their own schedules to support patients in their daily activities.58 Families can become frustrated that HF patients do not take care of themselves and especially when nonadherent behaviors result in hospitalizations, which are stressful on both the patient and family caregiver. A recent study has noted the increased vulnerability of spousal caregivers when their partners with HF are hospitalized.63 If the HF patient can be motivated to establish strong and consistent self-care behaviors and is able to remain out of hospital, then caregiver burden may be lower. Caregiver burden also is influenced by the support the family member gets from other family members as well.
Other caregiver factors may influence optimal self-care in HF and outcomes. For example, spousal self-efficacy (ie, spousal confidence to manage the various aspects of HF regimen) has been related to HF patient survival.14,64 Negative caregiver problem-solving abilities have been found to be significantly predictive of higher levels of depression and decreased life satisfaction in the patient with HF.65 Thus, the caregiver’s preparation, confidence, and problem-solving approach influence the self-care outcomes directly or may possibly affect the patient’s emotional state and their subsequent self-care activities.
Caregivers may experience increased burden when new devices or treatment practices are introduced, 66,67 and, for example, a study of home-based exercise to improve functional status of the HF patient resulted in increased caregiver burden.68 Caregivers may also experience distressing symptoms such as sleep difficulties related to the HF patient’s sleep apnea or sleep difficulties.69–71
A Family-Focused HF Self-care Conceptual Framework
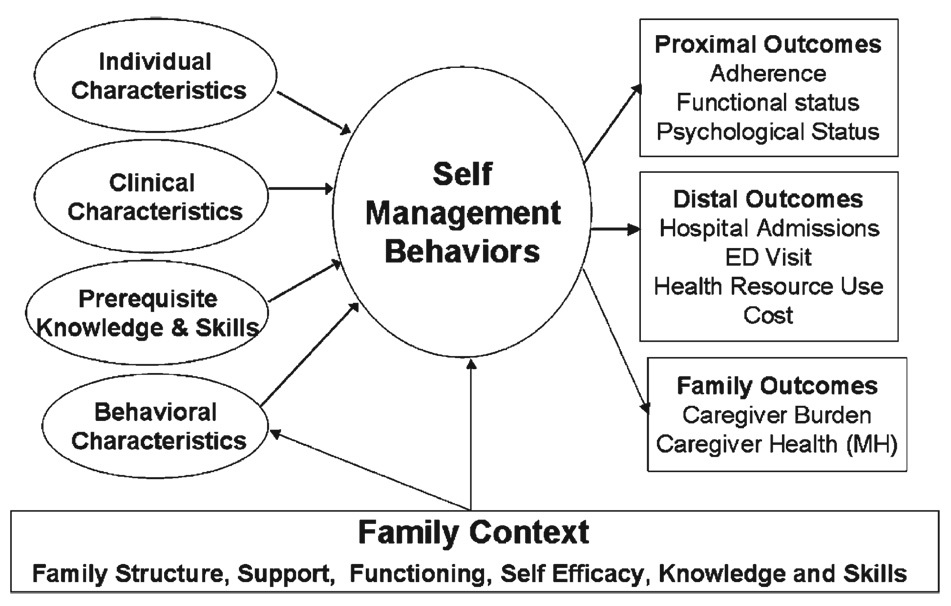
To synthesize the literature, a conceptual framework that depicts the relationships among the antecedent individual and clinical factors, processes of HF self-management, and outcomes of HF self-care in a family context is posed (see Figure 1). Self-management, that is, those activities that involve self-care decisions and actions around the recommended HF self-care behaviors, is viewed to be influenced by individual characteristics (age, sex, ethnicity, preferences, and patterns); the HF patient’s clinical characteristics (severity of illness including NYHA class and ejection fraction, cognitive status, comorbidities, and complex self-care regimens such as managing a diabetic diet as well as low-sodium diet); the HF patient’s behavioral characteristics such as motivation, self-efficacy or confidence, mood states, and ability to attend to the behaviors that might be altered by depression or anxiety; and the prerequisite knowledge and skills to perform the behaviors. For example, appropriate dietary self-care requires understanding the role of dietary sodium in HF, recognizing high-sodium foods and alternatives, and acquiring skills of label reading and alternative food preparation. Outcomes of successful self-management and self-care include markers of adherence accompanied by improved functional status in both physical and psychological states. More distal outcomes are likely to include reduced health resource use and cost of care—as self-care behaviors have been linked to these outcomes.
FIGURE 1.
Framework for heart failure self-management and family variables.
All of this self-management and self-care activity usually takes place in a family context. Thus, the family structure, family functioning (eg, communication, adaptability, and problem solving), and family support are hypothesized to specifically influence the HF patient’s behavioral characteristics as well as directly affect self-care.31,64,65,72 Caregiver outcomes are important as well and include caregiver burden and health status.49,57 In many of the HF caregiver studies, the focus has been on emotional state; however, physical health is also important, especially with elderly caregivers. The model provides direction for family-focused interventions that target the HF patient and family knowledge and skills, family support and functioning, motivation, and behavior, as well as the family context to improve self-care and, ultimately, overall outcomes.
Intervention Studies
Only 2 intervention studies related to HF families and self-care were found in the current literature. One is the report of a pilot study on a family partnership intervention to promote adherence to dietary sodium,73 and the other is a qualitative report of an ongoing family dyad group intervention led by a clinical nurse specialist.74 Both of these projects are described here with identification of their contributions to the state of the science in the area.
Using the framework described above, a randomized study comparing an education and family partnership intervention was conducted with 61 HF patient and family member dyads for its effect on dietary sodium self-care behaviors and adherence.73 Dyads randomized to education received in-depth information from a nurse expert and a dietitian on dietary sodium, food preparation techniques, shopping and food selection, label reading, making healthy choices when dining in restaurants, and low-sodium food alternatives. Dyads randomized to the family partnership intervention received the same educational information plus additional counseling on how to enhance family support, use autonomy support approaches, and provide HF patients with choice and empathy.30 Dietary sodium adherence was measured by 3-day food records analyzed using a computerized program for nutrients, and a 24-hour urine specimen was analyzed for sodium at baseline before intervention and again at 3 and 6 months. Data analysis using regression models to predict 3-month urine sodium revealed a significant group-by-time interaction (P = .03) when accounting for time-varying measures of body mass index. The family-focused intervention was deemed as superior to education alone in reducing dietary sodium intake in persons with HF. Because both groups increased equally in knowledge, the effect was not attributed to increased information alone, and the family partnership group showed a trend for decreased perceived criticism by the HF patients.
This intervention had several strengths in that it assured that education was provided to the family member considered as the person who was most involved in the HF patient’s activities related to their self-care and was a theoretically driven intervention. It was well received by patients and family members. However, follow-up measures at 6 months revealed that the improvement in dietary sodium intake was not retained, indicating the need for a stronger and more sustained family intervention.75 This family partnership intervention is now being tested in a larger clinical trial with a more diverse population and with the addition of education and family partnership booster sessions to determine the effect on dietary sodium and medication adherence.76
Duhamel and colleagues74 conducted a qualitative evaluation through semistructured interviews, with 4 dyads participating in an experimental study of a family systems nursing intervention. The intervention was theoretically based and designed to focus on the interaction between family members and on the relationship between the course of HF and the family dynamics. Content analysis of the interviews suggested that the family nursing meetings allowed the couples to obtain a better understanding of each other’s experiences, revealed suffering from the perspective of each member of the dyad, and enhanced understanding of each other’s behavior. For example, by understanding the illness more, wives expressed more confidence, less worry, and greater support for the HF patient. This ongoing study will make a valuable contribution to the understanding of family dynamics in HF and may have implications for approaches to enhance family self-care.
Summary
Based on the review of the literature, several important conclusions can be drawn. First, the structure and nature of family relationships are important to mortality and morbidity in HF, and, although the exact mechanisms are unknown, one study demonstrated that structure in the form of marital status was important to medication adherence. Second, as we try to make our disease management programs more efficient, effective, and cost-effective, it is clear that those living alone are a vulnerable group to target. Third, isolation leads to depression, and in some studies, depression was related to poor self-care behaviors. Fourth, for family members and informal caregivers, caregiver demand and burden are high, which leads to increased caregiver and patient depression. Fifth, caregiver factors such as self-efficacy for the role as HF caregiver and problem-solving abilities influence self-care and patient out-comes. And finally, although family interventions have yielded improved outcomes and lower patient hospital readmission in other serious and chronic illnesses, 77–79 there are few family-tested interventions in HF. Thus, the replicated evidence for guiding practice on specific HF family interventions is in its infancy, and much work needs to be done to identify what components of patient education and counseling are most likely to lead to the best outcomes for HF patients and families. Researchers may want to test family interventions similar to those used to address other chronic health problems, which have generated evidence that a family-oriented approach is often more successful than patient-oriented interventions.80
The existing literature on family and HF self-care is limited by cross-sectional approaches in that most conducted only short-term or one-time assessments of family functioning, perceptions, and caregiver burden. Longitudinal studies that examine the family and self-care trajectory over time and the reciprocal relationships between the self-care demands and changes in family functioning would be enlightening. Few of the studies have conceptual frameworks or compare targets of change to determine which has biggest effect on clinical outcomes.
Recommendations for Future Research
In addition to family research that examines genetic and other markers for HF prevention, clinically relevant studies that are theoretically based but behaviorally focused are clearly needed to promote appropriate understanding of HF self-care. Key research areas for future investigations that build on the existing literature and address gaps in knowledge are listed in Table 2. For example, what family variables can be relied upon to improve self-care and which ones are likely to lead to detrimental self-care? If marital quality or family functioning is important to self-care behaviors, how should these be treated in research and clinical practice? How should social support best be tailored to those who are socially isolated and at risk for poor self-care?
TABLE 2.
Suggested Topics for Family and Self-care Research in Heart Failure
| ■ | How do both overall family functioning and components of family functioning (ie, problem solving, communication, and adaptability) affect heart failure (HF) self-care and outcomes? |
| ■ | How do marital status and marital quality affect self-care and outcomes in HF? How should these factors be addressed in HF care? |
| ■ | What family behaviors should be targeted to achieve the largest effect in improving self-care in HF? |
| ■ | What aspects of family and caregiver knowledge and skills are most facilitative of patient self-care and improved outcomes in HF? |
| ■ | What family and caregiver characteristics (ie, self-efficacy, caregiver burden, and health literacy) are most important to HF self-care outcomes? |
| ■ | Does reducing HF caregiver burden have a positive impact on family outcomes and patient self-care in HF? |
| ■ | What is the effect of tailoring self-care interventions in HF based on family variables? |
| ■ | How can families best be prepared for HF self-care in the context of complex comorbidities such as diabetes, chronic obstructive pulmonary disease, and others? |
| ■ | What is the impact of technology, telemonitoring, and Web-based interventions on family caregiver outcomes? |
| ■ | How does culture influence the key family variables that are important in HF self-care? How should HF family self-care interventions be modified based on these variables for different cultural groups? |
Dyad and family-based studies are complex and have additional challenges related to methods, recruitment of dyads, analysis of data, and increased costs.81 However, family-focused interventions that have been effective in other chronically ill and cardiovascular patients may be good models for HF. Likewise, interventions focused on improving caregiver self-efficacy and problem solving and reducing caregiver burden should be tested for the impact on improving self-care. In addition, because family structure, function, and roles are influenced by culture and world views, which in turn influence self-care behaviors, the meaning of HF and behaviors in families of various ethnic groups should be explored. Finally, as HF disease management incorporates more technology, automation, and Web-based intervention methods in the home, how will family variables influence its success and what is the impact of such technology on HF families?
A comprehensive set of behavioral approaches to deliver family interventions exists, including literature on conflict resolution, problem solving, communication theory, and family therapy; however little is used in HF self-care approaches because the greatest emphasis has been on trying to influence individuals to change their behaviors. Because cognition and motivation—two factors essential for self-care behavior—are interwoven with family and social situations, it is time to reconceptualize HF self-care as a family phenomenon.
Acknowledgments
This manuscript was partially supported by NINR R01 8800, A Family Partnership Intervention in Heart Failure and PHS Grant M01-RR00039, EmoryGeneral Clinical Research Center, NIH, adn NIH, NMR 732 NR009888 Symptom Management: Heart Failure patient’s and family caregivers.
Contributor Information
Sandra B. Dunbar, Nell Hodgson Woodruff School of Nursing, Emory University, Atlanta, Georgia..
Patricia C. Clark, Byrdine F. Lewis School of Nursing, Georgia State University, Atlanta..
Christina Quinn, Nell Hodgson Woodruff School of Nursing, Emory University, Atlanta, Georgia..
Rebecca A. Gary, Nell Hodgson Woodruff School of Nursing, Emory University, Atlanta, Georgia..
Nadine J. Kaslow, Department of Psychiatry and Behavioral Sciences, School of Medicine, Emory University, Atlanta, Georgia..
REFERENCES
- 1.Heart Failure Society of America. Development and implementation of a comprehensive heart failure practice guideline. J Card Fail. 2006;12(1):e3–e9. doi: 10.1016/j.cardfail.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Grey M, Knafl K, McCorkle R. A framework for the study of self- and family management of chronic conditions. Nurs Outlook. 2006;54(5):278–286. doi: 10.1016/j.outlook.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Astedt-Kurki P, Lehti K, Tarkka MT, Paavilainen E. Determinants of perceived health in families of patients with heart disease. J Adv Nurs. 2004;48(5):115–123. doi: 10.1111/j.1365-2648.2004.03178.x. [DOI] [PubMed] [Google Scholar]
- 4.Weihs K, Fisher L, Baird M. Families, health, and behavior: a section of the Commissioned Report by the Committee on Health and Behavior: Research, Practice, and Policy, Division of Neuroscience and Behavioral Health and Division of Health Promotion and Disease Prevention, Institute of Medicine, National Academy of Sciences. Fam Syst Health. 2002;20(1):7–46.
- 5.Fisher L. Research on the family and chronic disease among adults: major trends and directions. Fam Syst Health. 2006;24(4):373–380. [Google Scholar]
- 6.Chin MH, Goldman L. Correlates of early hospital readmission or death in patients with congestive heart failure. Am J Cardiol. 1997;79:1640–1644. doi: 10.1016/s0002-9149(97)00214-2. [DOI] [PubMed] [Google Scholar]
- 7.Murberg TA, Bru E. Social relationships and mortality in patients with congestive heart failure. J Psychosom Res. 2001;51:521–527. doi: 10.1016/s0022-3999(01)00226-4. [DOI] [PubMed] [Google Scholar]
- 8.Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152(5):940, e941–e948. doi: 10.1016/j.ahj.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 9.Havranek EP, Spertus JA, Masoudi FA, Jones PG, Rumsfeld JS. Predictors of the onset of depressive symptoms in patients with heart failure. J Am Coll Cardiol. 2004;44(12):2333–2338. doi: 10.1016/j.jacc.2004.09.034. [DOI] [PubMed] [Google Scholar]
- 10.Luttik ML, Jaarsma T, Veeger N, van Veldhuisen DJ. Marital status, quality of life, and clinical outcome in patients with heart failure. Heart Lung. 2006;35(1):3–8. doi: 10.1016/j.hrtlng.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Chin MH, Goldman L. Factors contributing to the hospitalization of patients with congestive heart failure. Am J Public Health. 1997;87(4):643–648. doi: 10.2105/ajph.87.4.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chung ML, Lennie TA, Riegel B, Moser DK. Spouses enhance medication adherence in patients with heart failure. Circulation. 2006;114(18) Suppl II:518. (abstract) [Google Scholar]
- 13.Coyne JC, Rohrbaugh MJ, Shoham V, Sonnega JS, Nicklas JM, Cranford JA. Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol. 2001;88(5):526–529. doi: 10.1016/s0002-9149(01)01731-3. [DOI] [PubMed] [Google Scholar]
- 14.Rohrbaugh MJ, Shoham V, Coyne JC. Effect of marital quality on eight-year survival of patients with heart failure. Am J Cardiol. 2006;98(8):1069–1072. doi: 10.1016/j.amjcard.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 15.Happ M, Naylor M, Roe-Prior P. Factors contributing to rehospitalization of elderly patients with heart failure. J Cardiovasc Nurs. 1997;11(4):75–84. doi: 10.1097/00005082-199707000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Vinson JM, Rich MW, Sperry JC, Shah AS, McNamara T. Early readmission of elderly patients with congestive heart failure. J Am Geriatr Soc. 1990;38(12):1290–1295. doi: 10.1111/j.1532-5415.1990.tb03450.x. [DOI] [PubMed] [Google Scholar]
- 17.Krumholz HM, Butler J, Miller J, et al. Prognostic importance of emotional support for elderly patients hospitalized with heart failure. Circulation. 1998;97(10):958–964. doi: 10.1161/01.cir.97.10.958. [DOI] [PubMed] [Google Scholar]
- 18.Schwarz KA, Elman CS. Identification of factors predictive of hospital readmissions for patients with heart failure. Heart Lung. 2003;32(2):88–99. doi: 10.1067/mhl.2003.15. [DOI] [PubMed] [Google Scholar]
- 19.Yu DSF, Lee DTF, Woo J, Thompson DR. Correlates of psychological distress in elderly patients with congestive heart failure. J Psychosom Res. 2004;57(6):573–581. doi: 10.1016/j.jpsychores.2004.04.368. [DOI] [PubMed] [Google Scholar]
- 20.Simpson SH, Farris KB, Johnson JA, Tsuyuki RT. Using focus groups to identify barriers to drug use in patients with congestive heart failure. Pharmacotherapy. 2000;20(7):823–829. doi: 10.1592/phco.20.9.823.35205. [DOI] [PubMed] [Google Scholar]
- 21.Luttik ML, Jaarsma T, Moser D, Sanderman R, van Veldhuisen DJ. The importance and impact of social support on outcomes in patients with heart failure: an overview of the literature. J Cardiovasc Nurs. 2005;20(3):162–169. doi: 10.1097/00005082-200505000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Wang C, Fenske M. Self care of adults with non insulin dependent diabetes mellitus: influence of family and friends. Diabetes Educ. 1996;22:465–470. doi: 10.1177/014572179602200506. [DOI] [PubMed] [Google Scholar]
- 23.Wang H-X, Mittleman MA, Orth-Gomer K. Influence of social support on progression of coronary artery disease in women. Soc Sci Med. 2005;60(3):599–607. doi: 10.1016/j.socscimed.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 24.Fiscella K, Campbell TL. Association of perceived family criticism with health behaviors. J Fam Pract. 1999;48(2):128–134. [PubMed] [Google Scholar]
- 25.Williams GC, Lynch MF, McGregor HA, Ryan RM, Sharp D, Deci EL. Validation of the “important others” climate questionnaire: assessing autonomy support for health-related change. Fam Syst Health. 2006;24(2):179–194. [Google Scholar]
- 26.Deci EL, Ryan RM. Intrinsic Motivation and Self Determination in Human Behavior. New York: Plenum; 1985. [Google Scholar]
- 27.Ryan R, Deci E. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 28.Williams G, Deci E, Ryan R. Suchman A, Hinton-Walker P, Botelho R, editors. Building health-care partnerships by supporting autonomy: promoting maintained behavior change and positive health outcomes. Rochester: University of Rochester Press; Partnerships in heatlhcare: transforming relational process. 1998:67–87.
- 29.Williams GC, Deci EL. Activating patients for smoking cessation through physician autonomy support. Med Care. 2001;39:813–823. doi: 10.1097/00005650-200108000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Clark PC, Dunbar SB. Family partnership intervention: a guide for a family approach to care of patients with heart failure. AACN Clin Issues. 2003;14(4):467–476. doi: 10.1097/00044067-200311000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Fiscella K, Franks P, Shields C. Perceived family criticism and primary care utilization: psychosocial and biomedical pathways. Fam Process. 1997;36:25–41. doi: 10.1111/j.1545-5300.1997.00025.x. [DOI] [PubMed] [Google Scholar]
- 32.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160(21):3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 33.Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17(7):504–511. doi: 10.1046/j.1525-1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Evangelista LS, Berg J, Dracup K. Relationship between psychosocial variables and compliance in patients with heart failure. Heart Lung J Acute Crit Care. 2001;30(4):294–301. doi: 10.1067/mhl.2001.116011. [DOI] [PubMed] [Google Scholar]
- 35.Corvera-Tindel T, Doering LV, Gomez T, Dracup K. Predictors of noncompliance to exercise training in heart failure. J Cardiovasc Nurs. 2004;19(4):269–277. doi: 10.1097/00005082-200407000-00006. quiz 278-269. [DOI] [PubMed] [Google Scholar]
- 36.Schweitzer RD, Head K, Dwyer JW. Psychological factors and treatment adherence behavior in patients with chronic heart failure. J Cardiovasc Nurs. 2007;22(1):76–83. doi: 10.1097/00005082-200701000-00012. [DOI] [PubMed] [Google Scholar]
- 37.Goodlin SJ. The patient knows best: perceptions of family versus patient report of symptoms. J Card Fail. 2004;10(4):s97. (abstract) [Google Scholar]
- 38.Maxwell L. Family processes and individual health-related decisions in response to heart-health initiatives [doctoral dissertation] British Columbia, Vancouver: University of British Columbia; 1997. [Google Scholar]
- 39.Dracup K, Moser DK, Eisenberg M, Meischke H, Alonzo AA, Braslow A. Causes of delay in seeking treatment for heart attack symptoms. Soc Sci Med. 1995;40(3):379. doi: 10.1016/0277-9536(94)00278-2. [DOI] [PubMed] [Google Scholar]
- 40.Johansson I, Stromberg A, Swahn E. Factors related to delay times in patients with suspected acute myocardial infarction. Heart Lung. 2004;33(5):291. doi: 10.1016/j.hrtlng.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 41.Quinn JR. Delay in seeking care for symptoms of acute myocardial infarction: applying a theoretical model. Res Nurs Health. 2005;28(4):283–294. doi: 10.1002/nur.20086. [DOI] [PubMed] [Google Scholar]
- 42.Lobchuk MM, Kristjanson L, Degner L, Blood P, Sloan JA. Perceptions of symptom distress in lung cancer patients: I. Congruence between patients and primary family caregivers. J Pain Symptom Manage. 1997;14(3):136. doi: 10.1016/s0885-3924(97)00022-5. [DOI] [PubMed] [Google Scholar]
- 43.Clipp EC. Patients with cancer pain and their spouse caregivers. Cancer Metastasis Rev. 1992;69(4):1074–1079. doi: 10.1002/1097-0142(19920215)69:4<1074::aid-cncr2820690440>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 44.Porter LS, Keefe FJ, McBride CM, Pollak K, Fish L, Garst J. Perceptions of patients’ self-efficacy for managing pain and lung cancer symptoms: correspondence between patients and family caregivers. Pain. 2002;98(1–2):169–178. doi: 10.1016/s0304-3959(02)00042-8. [DOI] [PubMed] [Google Scholar]
- 45.Miaskowski C, Zimmer EF, Barrett KM, Dibble SL, Wallhagen M. Differences in patients’ and family care-givers’ perceptions of the pain experience influence patient and caregiver outcomes. Pain. 1997;72(1):217–226. doi: 10.1016/s0304-3959(97)00037-7. [DOI] [PubMed] [Google Scholar]
- 46.Bennett SJ, Cordes DK, Westmoreland G, Castro R, Donnelly E. Self-care strategies for symptom management in patients with chronic heart failure. Nurs Res. 2000;49(3):139–145. doi: 10.1097/00006199-200005000-00004. [DOI] [PubMed] [Google Scholar]
- 47.Quinn C. Symptom management: heart failure patients and family caregivers. 2007 NIH NINR F32 NR009888-01A1. [Google Scholar]
- 48.Schulz R, Beach SR. Caregiving as a risk factor for mortality. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 49.Molloy GJ, Johnston DW, Witham MD. Family caregiving and congestive heart failure. Review and analysis. Eur J Heart Fail. 2005;7(4):592–603. doi: 10.1016/j.ejheart.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 50.Karmilovich S. Burden and stress associated with spousal caregiving for individuals with heart failure. Prog Cardiovasc Nurs. 1994;9(1):33–38. [PubMed] [Google Scholar]
- 51.Evangelista LS, Dracup K, Doering L, Westlake C, Fonarow GC, Hamilton M. Emotional well-being of heart failure patients and their caregivers. J Card Fail. 2002;8(5):300–305. doi: 10.1054/jcaf.2002.128005. [DOI] [PubMed] [Google Scholar]
- 52.Dracup K, Evangelista LS, Doering L, Tullman D, Moser DK, Hamilton M. Emotional well-being in spouses of patients with advanced heart failure. Heart Lung. 2004;33(6):354–361. doi: 10.1016/j.hrtlng.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 53.Martensson J, Dracup K, Canary C, Fridlund B. Living with heart failure: depression and quality of life in patients and spouses. J Heart Lung Transplant. 2003;22(4):460–467. doi: 10.1016/s1053-2498(02)00818-5. [DOI] [PubMed] [Google Scholar]
- 54.Luttik ML, Jaarsma T, Veeger NJGM, van Veldhuisen DJ. For better and for worse: quality of life impaired in HF patients as well as in their partners. Eur J Cardiovasc Nurs. 2005;4(1):11–14. doi: 10.1016/j.ejcnurse.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 55.Hooley PJD, Butler G, Howlett JG. The relationship of quality of life, depression, and caregiver burden in outpatients with congestive heart failure. Congest Heart Fail. 2005;11(6):303–310. doi: 10.1111/j.1527-5299.2005.03620.x. [DOI] [PubMed] [Google Scholar]
- 56.Meagher-Stewart D, Hart G. Social support and the quality of life of individuals with heart failure and stroke and their family caregivers. Can J Cardiovasc Nurs. 2002;12(1):17–30. [Google Scholar]
- 57.Bakas T, Pressler SJ, Johnson EA, Nauser JA, Shaneyfelt T. Family caregiving in heart failure. Nurs Res. 2006;55(3):180–188. doi: 10.1097/00006199-200605000-00004. [DOI] [PubMed] [Google Scholar]
- 58.Luttik ML, Blaauwbroek A, Dijker A, Jaarsma T. Living with heart failure: partner perspectives. J Cardiovasc Nurs. 2007;22(2):131–137. doi: 10.1097/00005082-200703000-00010. [DOI] [PubMed] [Google Scholar]
- 59.Martensson J, Dracup K, Fridlund B. Decisive situations influencing spouses’ support of patients with heart failure: a critical incident technique analysis. Heart Lung J Acute Crit Care. 2001;30(5):341–350. doi: 10.1067/mhl.2001.116245. [DOI] [PubMed] [Google Scholar]
- 60.Boyd KJ, Murray SA, Kendall M, Worth A, Frederick Benton T, Clausen H. Living with advanced heart failure: a prospective, community based study of patients and their carers. Eur J Heart Fail. 2004;6(5):585–591. doi: 10.1016/j.ejheart.2003.11.018. [see comment] [DOI] [PubMed] [Google Scholar]
- 61.Barnes S, Gott M, Payne S, et al. Characteristics and views of family carers of older people with heart failure. Int J Palliat Nurs. 2006;12(8):380–389. doi: 10.12968/ijpn.2006.12.8.380. [DOI] [PubMed] [Google Scholar]
- 62.Aldred H, Gott M, Gariballa S. Advanced heart failure: impact on older patients and informal carers. J Adv Nurs. 2005;49(2):116–124. doi: 10.1111/j.1365-2648.2004.03271.x. [DOI] [PubMed] [Google Scholar]
- 63.Christakis NA, Allison PD. Mortality after the hospitalization of a spouse. N Engl J Med. 2006;354(7):719–730. doi: 10.1056/NEJMsa050196. [DOI] [PubMed] [Google Scholar]
- 64.Rohrbaugh MJ, Shoham V, Coyne JC, Cranford JA, Sonnega JS, Nicklas JM. Beyond the “self” in self-efficacy: spouse confidence predicts patient survival following heart failure. J Fam Psychol. 2004;18(1):184–193. doi: 10.1037/0893-3200.18.1.184. [DOI] [PubMed] [Google Scholar]
- 65.Kurylo M, Elliott TR, DeVivo L, Dreer LE. Caregiver social problem solving abilities and family member adjustment following congestive heart failure. J Clin Psychol Med Setting. 2004;11(3):151–157. [Google Scholar]
- 66.Albarran JW, Tagney J, James J. Partners of ICD patients — an exploratory study of their experiences. Eur J Cardiovasc Nurs. 2004;3(3):201–210. doi: 10.1016/j.ejcnurse.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 67.Tagney J, James JE, Albarran JW. Exploring the patient’s experiences of learning to live with an implantable cardioverter defibrillator (ICD) from one UK centre: a qualitative study. Eur J Cardiovasc Nurs. 2003;2(3):195–203. doi: 10.1016/S1474-5151(03)00061-6. [DOI] [PubMed] [Google Scholar]
- 68.Molloy GJ, Johnston DW, Gao C, et al. Effects of an exercise intervention for older heart failure patients on caregiver burden and emotional distress. Eur J Cardiovasc Prev Rehabil. 2006;13(3):381–387. doi: 10.1097/01.hjr.0000198916.60363.85. [DOI] [PubMed] [Google Scholar]
- 69.Brostrom A, Stromberg A, Dahlstrom U, Fridlund B. Congestive heart failure, spouses’ support and the couple’s sleep situation: a critical incident technique analysis. J Clin Nurs. 2003;12(2):223–233. doi: 10.1046/j.1365-2702.2003.00692.x. [DOI] [PubMed] [Google Scholar]
- 70.Brostrom A, Johansson P, Stromberg A, Albers J, Martensson J, Svanborg E. Obstructive sleep apnoea syndrome—patients’ perceptions of their sleep and its effects on their life situation. J Adv Nurs. 2007;57(3):318–327. doi: 10.1111/j.1365-2648.2006.04110.x. [DOI] [PubMed] [Google Scholar]
- 71.Rausch SM, Baker K, Boonmee J. Sleep disturbances in caregivers of patients with end-stage congestive heart failure: part I—the problem. Prog Cardiovasc Nurs. 2007;22(1):38–40. doi: 10.1111/j.0889-7204.2007.05818.x. [DOI] [PubMed] [Google Scholar]
- 72.Fisher L, Weihs KL. Can addressing family relationships improve outcomes in chronic disease? Report of the national working group on family-based interventions in chronic disease. J Fam Pract. 2000;49(6):561–566. [PubMed] [Google Scholar]
- 73.Dunbar SB, Clark PC, Deaton C, Smith AL, De AK, O’Brien MC. Family education and support interventions in heart failure: a pilot study. Nurs Res. 2005;54(3):158–166. doi: 10.1097/00006199-200505000-00003. [DOI] [PubMed] [Google Scholar]
- 74.Duhamel F, Dupuis F, Reidy M, Nadon N. A qualitative evaluation of a family nursing intervention. Clin Nurse Spec. 2007;21(1):43–49. doi: 10.1097/00002800-200701000-00009. [DOI] [PubMed] [Google Scholar]
- 75.Dunbar SB, Clark PC, Deaton C, De A, Smith AL. The effect of a family-focused intervention on self management of diet, medication-taking, and activity after six months. J Card Fail. 2003;9(5 suppl):S93. [Abstract] [Google Scholar]
- 76.Dunbar S. A Family Partnership Intervention in Heart Failure: National Institute of Nursing Research. 2004–2008 NR008800. [Google Scholar]
- 77.Given B, Sherwood PR. Family care for the older person with cancer. Semin Oncol Nurs. 2006;22(1):43–50. doi: 10.1016/j.soncn.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 78.Cole I, Chesla CA. Interventions for the family with diabetes. Nurs Clin North Am. 2006;41(4):625–639. doi: 10.1016/j.cnur.2006.07.001. vii. [DOI] [PubMed] [Google Scholar]
- 79.Hudson PL, Aranda S, Hayman-White K. A psycho-educational intervention for family caregivers of patients receiving palliative care: a randomized controlled trial. J Pain Symptom Manage. 2005;30(4):329–341. doi: 10.1016/j.jpainsymman.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 80.Martire LM. The “relative” efficacy of involving family in psychosocial interventions for chronic illness: are there added benefits to patients and family members? Fam Syst Health. 2005;23(3):312–328. [Google Scholar]
- 81.Northouse LL, Rosset T, Phillips L, Mood D. Research with families facing cancer: the challenges of accrual and retention. Rer Nurs Health. 2006;29:199–211. doi: 10.1002/nur.20128. [DOI] [PubMed] [Google Scholar]