Abstract
Objectives
Even when health insurance coverage is available, health policies may not be effective at increasing coverage among vulnerable populations. New approaches are needed to improve access to care. We experimentally introduced a novel intervention that uses Policy Navigators to increase health insurance enrollment in a poor population.
Methods
We used data from the Quality Improvement Demonstration Study (QIDS), a randomized experiment taking place at the district level in the Visayas region of the Philippines. In two arms of the study, we compared the effects of introducing Policy Navigators to controls. The Policy Navigators advocated for improved access to care by providing regular system-level expertise directly to the policy-makers, municipal mayors and governors responsible for paying for and enrolling poor households into the health insurance program. Using regression models, we compared levels of enrollment in our intervention versus control sites. We also assessed the cost effectiveness of marginal increases in enrollment.
Results
We found that Policy Navigators improved enrollment in health insurance between 39 and 102% compared to the controls. Policy navigators were cost-effective at $0.86 USD per enrollee. However, supplementary national government campaigns, which were implemented to further increase coverage, attenuated normal enrollment efforts.
Conclusion
Policy Navigators appear to be effective in improving access to care and their success underscores the importance of local-level strategies for improving enrollment.
Introduction
Poor individuals most in need of protection from financial catastrophe have the least access to health insurance or risk-sharing.1 Affordability is assumed to be a major barrier to obtaining health insurance but other systemic elements of access may be equally important.2 Access is understood as a multidimensional concept that is challenged by both political and operational barriers.3 Health policy affects two key inputs: the characteristics of the health care delivery system and the population at risk. These, in turn, affect two outcomes: the use of health care services, and satisfaction with the services.3 Accordingly, even when enabling or impeding characteristics such as health insurance coverage are already affordable, health policies may not be effectively implemented to further improve a population's access to care.
Efforts to improve health policy and increase access to health care and health insurance have typically centered on policies that alter an individual's consumer incentives. For example, policy and incentive strategies designed to extend health insurance coverage to poor children in the United States have provided financial incentives for Medicaid eligible parents of children to purchase coverage or provided time-limited subsidies for workers and their families to purchase insurance when they are between jobs.4 Other countries have attempted to increase enrollment through similar policy initiatives such as government subsidy programs that insure children who have enrolled in school.5 While these strategies can be effective, they can also be difficult and cumbersome to replicate in developing countries, where attempts to cover vulnerable populations have been increasing.6 To an even greater extent than wealthier countries, these subsidies are hampered by bureaucratic requirements, minimal infrastructure, extent of financial solidarity, or limited school enrollment that impede the implementation of subsidized health insurance.7
New approaches are needed to overcome non-financial impediments to improve access to care. In particular, we are especially interested in introducing ‘Policy Navigators’ as a possible method for overcoming limited access to care in a vulnerable population. Policy Navigators, in brief, are individuals who develop relationships with fund holders and policy makers, and provide them with information on the benefits of health insurance coverage, the bureaucratic mechanics of the newly implemented health reform and enrollment package and the financial benefits of expanded enrollment in health insurance. We were particularly interested to learn if Policy Navigators would be a practical solution that could quickly and reasonably address undercoverage of children. We reasoned that if leaders in civil society were better informed and had an easier time understanding and implementing health insurance and health policy, health coverage would increase.
The Quality Improvement Demonstration Study (QIDS) is a longitudinal, population-based study that evaluates the impact of two major health care policy reforms in the Philippines implemented at the district-level: expanded insurance coverage to increase access to care, and bonus payments paid to physicians who provide high quality care.8 At the field level for the access to care intervention, QIDS is implemented through Policy Navigators. Using data from this study, we evaluate here whether individualized marketing efforts of QIDS Policy Navigators have an incremental benefit in improving enrollment in health insurance beyond the national and local enrollment drives. We also discuss the cost-effectiveness of the one-on-one marketing approach and consider these relative to the impact of national government policies on local and grassroots initiatives.
Background
Social Health Insurance in the Philippines
The 1987 Constitution of the Republic of the Philippines declared that “the State shall adopt an integrated and comprehensive approach to health development which shall endeavor to make essential goods, health and other social services available to all the people at affordable cost”.9 It further asserted that the State would provide free medical care to the poor. Under these guiding principles, the National Health Insurance Act was passed in 1995, creating PhilHealth as the entity responsible for developing and handling the National Health Insurance Program (NHIP).10 Insurance benefits provided by NHIP are primarily for inpatient services, including room and board; services of health care professionals; diagnostic, laboratory, and other medical examination services; prescription drugs; and inpatient education packages. The rules governing indigent coverage (health coverage to poor households) are complex; for example, government municipalities are graded by income class, which in turn affects premium subsidies paid by each municipality.
PhilHealth Sponsored Program – Regular Track
The Regular Track Sponsored Program (SP) aims to provide PhilHealth privileges to the marginalized sector of the Filipino society. The program targets households belonging to the lowest 25% of the income distribution, also known as indigent households. The Sponsored Program is unique in that it is implemented in partnership with provincial districts, or local government units (LGUs). After signing a Memorandum of Agreement, an LGU shares the 1,200PhP (about 25 USD) annual premium per indigent household with the national government through PhilHealth. The premium sharing is based on the income classification of the LGU where the indigent resides, and ranges from 10%/90% to 50%/50% LGU to national government sharing.
National Enrollment Programs
Local and national government provide additional support for free indigent health care insurance coverage as part of the overall strategy to provide universal coverage by the year 2012. To attain this goal, three recent initiatives that have their own rules and requirements have been introduced on an immediate and temporary basis to expand enrollment on a temporary basis. Just prior to the start of QIDS, in 2002, the Philippine Charity Sweepstakes Office (PCSO), PhilHealth, the LGUs, and other national government agencies came together to support the state enrollment of 500,000 indigent families for one year. In 2004 another PCSO-led effort was launched, aimed at enrolling 5 million indigent families in PhilHealth for another year. In September 2005, yet another effort to use national sources to fully subsidize indigents was launched, however this time only 2.5 million families were covered. While there were no national led programs initiated in 2006 or 2007, enrollment data show that some families were still being covered under the previous national level campaigns. Overall, national level initiatives were intermittent and were not applied with consistent effort. In this paper, we will refer to the three phases of the PCSO program collectively as the National Government Campaign (NGC).
Methods
Setting and Funding
With funding from the U.S. National Institutes for Health (R01 HD042117), a collaboration of researchers from the University of the Philippines School of Economics and University of San Francisco's Institute for Global Health partnered with the PhilHealth and the Department of Health to establish QIDS. PhilHealth is a key partner in QIDS, as it is the NHIP administrator and the largest third party payer for inpatient care. The study was approved by the Ethics committees at the University of the Philippines and the University of California, San Francisco.
Study Site and Population
QIDS encompasses 30 districts within 11 provinces in the Visayas and Northern Mindanao, the central region of the Philippines, targeted by the HSRA. The 11 provinces included are Capiz, Iloilo, and Negros Occidental in Region 6, Bohol, Cebu, Negros Oriental, and Siquijor in Region 7, North Leyte, Eastern Samar, and Naval in Region 8, and Camiguin in Region 10. The catchment areas of the 30 district hospitals contain approximately one million households.
Study Design in Accordance with CONSORT Guidelines
A key advantage of QIDS is its experimental design, with randomization of two policy interventions and a control group to the 30 districts in the Visayas. The policy interventions in QIDS are made at the provincial district level, an administrative unit that manages the delivery of health and social services in a province. To avoid selection bias and confounding, we identified similar districts in the Visayas region of the country before randomizing. Districts were matched in blocks of three on the basis of shared population and system characteristics: the population characteristics were obtained from national census and local data and capture the diversity of the population of the Visayas, such as population size, average income, labor force participation rate, functional literacy, infant mortality rate, maternal mortality rate, and percentage of the population with insurance; the system characteristics used were geographic size, proportion of the population that is rural, proximity to Manila, number of physician specialists, and the existence of a regional or specialist hospital. Within each matched block of three districts, sites were randomly chosen for study—one set of communities received the expanded insurance (Access Intervention), another the bonus payments (Bonus Intervention), and the third set of communities became the Control sites, to which no changes were made to the current health care scheme. The Access Intervention is two-pronged with the goal of expanding insurance: (1) increased health care enrollment through the use of Policy Navigators and (2) assured financial access through a zero co-pay system for indigent children under 6 years of age. In Control sites and Bonus sites promotion of enrollment into PhilHealth was carried out by the usual means through local media sources and word of mouth. The intervention sites are geographically isolated and administrated separately and thus have little chance of impacting each other. Furthermore, there were no statistical differences in the system and population characteristics between the intervention and control groups. Sample size calculations were conducted prior to the study to ensure that the anticipated effect sizes, which in this case is enrollment in PhilHealth, were adequately powered (0.80) to detect meaningful differences in enrollment coverage of 12%.
District-level participation in the QIDS study was strictly voluntary and written consent was obtained; these agreements were formalized through written Memorandums of Agreement between the QIDS study team and each of the 30 provincial district governors. Between the beginning of the study in 2003 to date, none of the districts have dropped out of the study, hence we continue to have all 30 enrolled sites randomized to the interventions.
District level enrollment in PhilHealth insurance—the outcome of interest—was monitored quarterly at all the study sites. We hypothesize that the unique enrollment strategy of individualizing marketing efforts to local government officers using Policy Navigators (Access Intervention) improves enrollment in PhilHealth insurance compared to controls (in this paper the Access Intervention is hereafter referred to as the “Intervention”). Further details on QIDS can be found in Shimkhada et al. (2008)8.
Policy Navigators
We dedicated three QIDS Policy Navigators to advocate and encourage enrollment in our intervention site catchment areas. All three Policy Navigators were physicians and employed by QIDS from November 2004 to June 2008. Their primary focus and priority is on enrollment of indigent families into PhilHealth. To do this, Navigators make monthly visits to the Mayors in each enrollment site. During visits, which last 20-45 minutes, the Navigators review indigent enrollment, explain the financial and health benefits of insurance coverage, identify administrative requirements and serve as liaisons with the National Health Insurance Program. As part of each visit a goal for enrolling a certain number of indigent families is decided upon, and the Mayors are asked to meet with the Budget Officer and refer their recommendation to the Municipal Council. The Navigators, upon invitation, make presentations to the councils and to the province Governors. They also relay the financial commitment to enroll indigents back to the National Insurance Program. All three Navigators were trained and meet on a regular basis to ensure uniformity in their work; furthermore, there are no differences in any other enrollment mechanisms between sites, such as staff or methodology.
Data Collection
From the 1st quarter of 2005 to the 2nd quarter of 2007, QIDS monitored enrollment in all 30 sites over a total of ten quarters. Enrollment data were collected at the municipal level, the administrative sub-unit of a district. Data were collected from all 139 municipalities (an average of four to five per district) in the QIDS districts.
Data collection is done in collaboration with the PhilHealth Regional Offices (PRO) who gather data on a monthly basis at the municipal level to monitor enrollment and their progress towards universal coverage. Collected data are submitted to the PhilHealth Head Office. The PhilHealth Program and Membership Department aggregates data received from all the regions to assess overall indigent membership for the entire country. Policy Navigators receive monthly reports from the Regional Offices' membership department and subsequently forward them to the QIDS study team for analysis. By comparing the actual enrolled indigent households to the total number of indigent households in the municipality, coverage rates down to the municipal level are calculated. The total number of indigent households per municipality is calculated by multiplying the total population by the municipal level poverty incidence and then dividing by 5 members.
Data Analysis
To establish the impact of both the Policy Navigator effect and the National Government Campaign on enrollment, we looked at enrollment trends from each funding track (i.e. Regular Track Sponsored Program (SP) and National Government Campaigns (NGC)) separately. We then estimated a regression model to determine the marginal effects of the various influences on Sponsored Program enrollment at the municipal level. The model can be summarized in the following equation:
where Enrollmentit is the number of indigent households enrolled under the PhilHealth Regular Track Sponsored Program of the ith municipality in quarter t; Ai is a dummy variable indicating where Policy Navigator were introduced; Ci is a dummy variable for QIDS control sites. The variables Reg7i and Reg8i are dummy variables indicating whether the municipalities belonged to Region 7 (Central Visayas) or Region 8 (Eastern Visayas); AiPt and CiPt are interaction terms between time in quarters (Pt) and intervention type; IncClass is a dummy variable indicating the income class of the municipality; and NGCi is a dummy variable indicating the presence of the National Government Campaign in the municipality. By modeling total enrollment as a function of both Regular Track Sponsored Program (SP) enrollment efforts (i.e., intervention and control variables) and National Government Campaign (NGC), we are able to test our hypothesis that NGC might create disincentives that decrease LGU Regular Track Sponsored Program enrollment.
The cost-effectiveness of Policy Navigators can be subsequently calculated by comparing the cost of employing three Navigators per year, including their expenses, with the additional number of households enrolled in Intervention sites versus Control sites. The cost-benefit ratio herein is computed by multiplying the number of additional households enrolled by the premiums per household and then dividing this by the total costs of employing the Policy Navigator.
Results
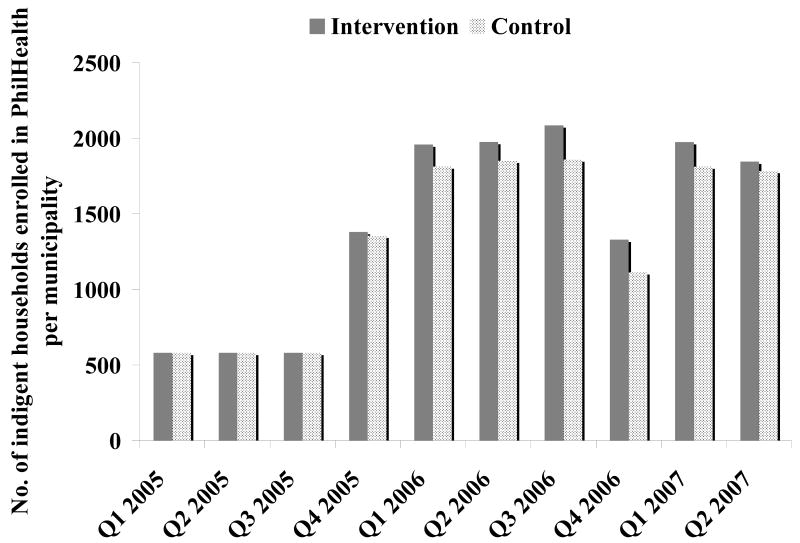
At baseline, there was no statistically significant difference (p>0.05) in enrollment levels in health insurance of indigent families between the Intervention and the Control sites (Figure 1). At baseline, defined as the 1st quarter of 2005 (Q1 2005), Intervention and the Control sites each had an average of 542 households enrolled in PhilHealth coverage per municipality. In both Intervention and Control sites, however, enrollment varied between municipalities due to differences in populations, budgets allocated for enrollment, and priority of enrollment within the municipality. In Intervention and Control sites, for example, some municipalities had zero families enrolled in insurance coverage. In contrast, large cities with sufficient funding and a commitment to enroll indigent members were able to enroll as many as 6,759 families.
Figure 1.
Average enrollment of indigent households per municipality in QIDS Intervention and Control sites
Enrollment during the 2nd and 3rd quarters of 2005 remained the same as they were at baseline for both Intervention and Control sites. Over time, however, we observed that insurance enrollment increased in Intervention and Control sites. These increases in insurance coverage coincided with the roll-out of the NGC, which began in the 4th quarter of 2005. Enrollment continued to increase in both Intervention and Control sites during the 1st and 2nd quarter of 2006, with Intervention sites enrolling approximately 125 additional households per municipality than Control sites. Peak enrollment occurred during the 3rd quarter of 2006 when there was an average of 2,086 households per municipality in Intervention sites and 1,860 households per municipality in Control sites. These results expose the secular trends of expanding and contracting policies to subsidize health care insurance. Moreover, efforts to implement NGC have not been applied consistently. PhilHealth records suggest that the spike in Q1 2007 in Figure 1 were driven by the application of residual NGC funds from Q3 2006.
The Effect of Policy Navigators
We disaggregated total enrollment figures based on the two enrollment tracks: Regular Sponsored Program (SP) enrollment (also called Regular Track) and National Government Campaign (NGC). Phase 3 of the NGC was a one-time installment of funding. We therefore expected minimal, if any, variation would occur in the NGC track during the one year these families were enrolled. We then focused our attention on the Regular Track enrollment, which was the target of the Policy Navigator intervention. Regular Track enrollment is amenable to changes at any given point during the year as it is not contingent on one-time NGC funds, but instead is financed by the local government, private sponsors, or legislative sponsors who choose to enroll in their own timing. Looking at the Regular Track Sponsored Programs (SP), the Intervention sites jumped from 33% coverage at baseline to 69% coverage in the 2nd quarter of 2007. Meanwhile, the Control sites only increased from 25% to 43% during the same time period (Table 1).
Table 1.
Percentage of indigent households in municipalities enrolled in PhilHealth's Regular Track Sponsored Program (SP) and the National Government Campaign (NGC), by intervention
| Q1 2005 | Q1 2006 | Q2 2006 | Q3 2006 | Q4 2006 | Q1 2007 | Q2 2007 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SP | SP | NGC | SP | NGC | SP | NGC | SP | NGC | SP | NGC | SP | NGC | |
| Intervention | 33% | 58% | 29% | 59% | 30% | 62% | 30% | 62% | 4% | 67% | 19% | 69% | 14% |
| Control | 25% | 33% | 35% | 32% | 35% | 32% | 36% | 32% | 9% | 38% | 25% | 43% | 25% |
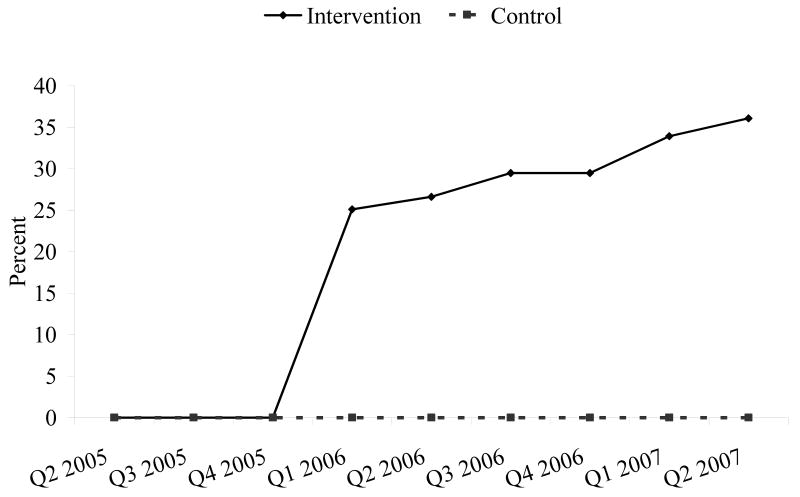
Figure 2 illustrates the impact of the Intervention. No statistically significant improvements in the control site enrollment in SP were seen over time (p>0.05). By contrast, after a short lag time from baseline, significant improvements (p<0.01) in enrollment were seen in the Intervention sites starting with the 1st Quarter of 2006. Beginning with the fourth quarter of 2005, enrollment in the Intervention sites has increased quarter after quarter.
Figure 2.
Percentage point increase of indigent households enrolled in PhilHealth's Regular Track Sponsored Program compared to baseline (1st quarter of 2005), by intervention
The Effect of a National Enrollment Campaign
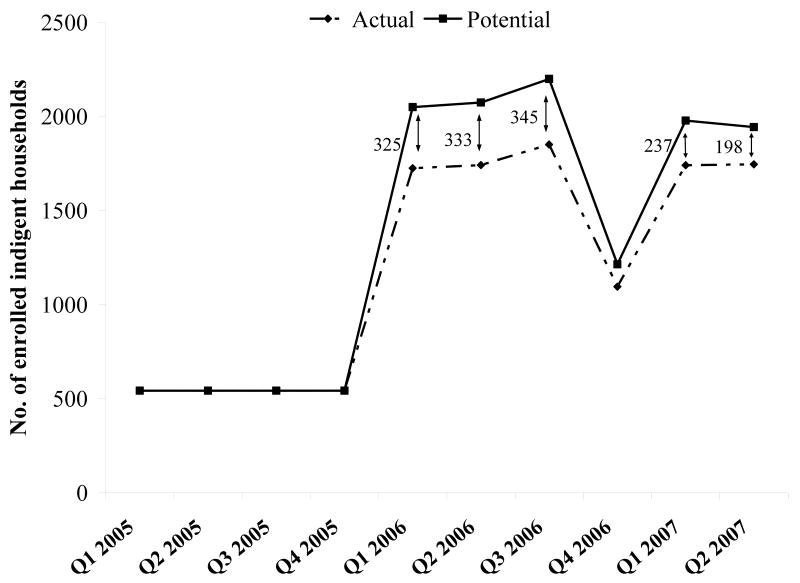
We also controlled for and assessed the effect of the NGC in our regression model. The NGC provided municipalities necessary funds to enroll additional members. We found, however, that with the NGC from 1st Quarter 2006 to 2nd Quarter of 2007, an average of 288 households that would have been enrolled through the Regular Track Sponsored Program, were not enrolled (p<0.001). Thus, while total enrollment increased with the NGC, the potential number of indigent families who would have been enrolled was reduced coincident with the introduction of the NGC (Figure 3). The gap between actual and potential indigent enrollment as shown in Figure 3 is the estimated NGC effect. For example, during the first quarter of 2006, an average of 2,125 indigent households were enrolled in each Intervention site. However, if the NGC did not create a disincentive to enroll families in the Regular Track Program, enrollment would have potentially have reached 2,049 households. By the end of 2006 and the beginning of 2007, NGC funding ceased, resulting in the diminishing gap seen in Figure 3 between actual and potential households enrolled.
Figure 3.
Actual and potential enrollment of indigent households in PhilHealth insurance in Intervention sites
Cost-Effectiveness of Policy Navigators
To estimate the cost effectiveness of Policy Navigators, we first calculated the total cost of using the Policy Navigators. Compensation and expenditures associated with developing relationships with local government and health officials, such as communication and travel expenses, were tracked. The cost of utilizing Policy Navigators included their total compensation, training, and liaison work of 32,000 PhP (669 USD) per month plus 4,800 PhP (100 USD) per month. During one year, the Policy Navigators made approximately 825 visits and presentations to Intervention sites, an average of 15 per site. We then calculated benefits, which were defined as additional households enrolled in the insurance program. In summary, 32,203 additional households were enrolled in the Intervention sites compared to the Control sites. The overall cost per additional household enrolled is 41.14 PhP (0.86 USD) (Table 2).
Table 2.
Cost-effectiveness and cost-benefit of QIDS Policy Navigators
| Number of indigent households enrolled in PhilHealth between Q3 2005 to Q3 2006 | ||
| Intervention | 81,623 | |
| Control | 49,420 | |
| Difference in number of households between Intervention and Control sites | ||
| Intervention-Control | 32,203 | |
| Total cost of Policy Navigators | ||
| Monthly expense per region (PhP) | 32,000 | |
| Monthly allowance | 4,800 | |
| Number of regions | 3 | |
| Months per year | 12 | |
| Total cost (PhP) | 1,324,800 | |
| Number of visits per site | 15 | |
| Total cost per additional household enrolleda | ||
| 41.14 PhP (0.86 USD) | ||
| Additional premiums paid to PhilHealth | ||
| 4,637,232 PhP (96,669.42 USD) | ||
| Cost-Benefit Ratio | ||
| 0.29 | ||
A household consists of 5 family members
Cost-Benefit Analysis
In addition to estimating the cost-effectiveness of the Policy Navigators, we analyzed their cost in comparison to the financial benefits PhilHealth would reap from the increase in enrollment. We found that the additional 32,203 indigent households enrolled in PhilHealth due to RPM one-on-one advocacy amounts to an increase of 4,637,232 PhP ($96,669.42 USD) in revenues for PhilHealth. Dividing this amount by the total cost of employing the Policy Navigators, we obtain a cost-benefit ratio of 0.29. If this benefit is extended over the two years of the study the cost-benefit ratio is 0.15.
Discussion
The unique experimental and longitudinal design of the Quality Improvement Demonstration Study (QIDS) allows a rigorous evaluation of the impact of health sector reform intended to increase health care coverage of children in the Philippines. In this paper we asked whether Policy Navigators increased enrollment beyond the usual enrollment efforts or the expanding and contracting national enrollment drives. We also considered the cost-effectiveness of this one-on-one marketing approach with policy makers and fund holders.
In comparisons of Intervention versus Control sites, we found that our one-on-one Policy Navigator strategy is effective at increasing enrollment. By the 3rd quarter of 2006, our Intervention sites' total enrollment had increased 39% more than our or control sites. The effectiveness of our strategy is even more dramatic when we compare only Regular Track enrollment. By the 4th quarter of 2006, Intervention site enrollment was 102% higher than Control sites.
When we compared the number of actual indigent households enrolled in Intervention sites versus Control sites, and accounting for the Policy Navigators salary and expenses, we found that Policy Navigator strategy appears to be cost-effective. At 41 PhP (0.86 USD) per household, increasing coverage for indigent families through one-on-one marketing appears quite attainable. We found that the enrollment benefit persisted for at least two years making Navigators even more affordable in the short run. It is unclear, at least from these data, whether this effect will persist beyond two years and needs to be monitored to determine the ultimate cost-effectiveness. Furthermore, while national government initiatives may increase overall enrollment, the funds targeted for these campaigns are not as effective as they might be if they were used to enroll families in the Regular Track SP. At a minimum, enrolling under the SP using Policy Navigators is one-third the cost of what the government pays to enroll one additional indigent household under the NGC driven program. With the goal, for example, of enrolling 2.5 million indigents in 2006, this would translate into a savings of between 197,500,000 PhP (4,129,207 USD) and 1,397,500,000 PhP (29,218,064 USD).
A confounding factor uncovered in our analysis was the effect of the NGC. The special campaigns compromise local municipalities' efforts as well as the QIDS intensification through Policy Navigators to promote municipalities to enroll indigents. The willingness of LGUs to sponsor indigent families dropped with the knowledge that the national government would fully subsidize premiums. The introduction of the NGC concurrently with the Regular Track Sponsored Program appears to weaken the credibility and more importantly, reduces the attractiveness of the cost-sharing scheme between national and local governments. While the QIDS Policy Navigator strategy has proven effective at increasing enrollment to a greater degree when compared to regular PhilHealth marketing efforts, these efforts have been hampered by the government's national campaigns. Although strategies to provide access to care for indigents will use different tactics, these findings show both an unintended consequence of a government's national campaign and the need to work in concert with local efforts to provide access to care to the greatest number of indigent households possible.
There are several factors that might explain the effectiveness of the Policy Navigators. As skilled professionals, Policy Navigators not only know the intricacies of how the care system works but also are also adept at moving through the different layers. Policy- and other decision-makers in the health arena work in complicated systems. The poor are particularly difficult to insure in the Philippines, as they require public subsidization of premiums and user fees. While PhilHealth coverage of formal sector workers has been fairly successful, coverage of poor individuals has been more difficult to achieve owing in part to the complex nature of the insurance financing scheme.11 Policy Navigators provide the necessary translation of the financing system into understandable terms; in other words, they simplify a complicated and ever changing arrangement that otherwise appears incomprehensible to policy makers. As specialists in the financing schemes, Policy Navigators are able to also coordinate with agencies to identify funding sources, which is difficult task for a non-specialist politician or administrator.
National enrollment drives, on the other hand, may provide substantial funding but they are not designed to address the questions and implementation concerns of specific municipalities. Some of these concerns could potentially be addressed by regional insurance staff responsible for enrollment and membership. However, this staff is not solely devoted to enrollment as they are also involved in ancillary activities such as distributing PhilHealth identification cards, monitoring payment of membership dues, and collecting fees.
QIDS Policy Navigators are unique in that they provide dedicated time to each assigned municipality (Intervention sites) on a continual basis to those actually responsible for funding enrollment. Their in-depth knowledge of insurance benefits and enrollment procedures allows them to address the specific obstacles each municipality faces with regards to increasing enrollment, whether it is lack of funds budgeted for enrollment or finding local sponsors to support a given number of families. While the knowledge the Policy Navigators provide to the local government officers is crucial, the actual relationships built with governors, mayors, budget officers, and other staff along with the continuity of monthly visits is a significant driving force of our Intervention. We viewed the lag in new enrollees seen during the 2nd and 3rd quarters of 2005 as evidence of the importance of the relationship in our Intervention. It takes time to build rapport and trust with key decision makers. The increases seen in our Intervention sites however, show that these crucial investments are effective. Similarly, with their frequent visits to policy makers, Policy Navigators provide continual promotion of access to health care. In this role, Policy Navigators function as dedicated advocates of health focusing on a community's need for improved access to care.
The literature on health care navigation is nascent but growing and demonstrates the positive potential for use in several areas in health care. Health care navigators have emerged from the multi-level barriers to care involving patient, provider, and system level barriers.12 Health navigation places emphasis on care management, utilizing advocacy and coordination activities to help patients maneuver the health care system to achieve specific goals.13 The available research on navigators, however, is largely confined to the hospital setting. Here, patient navigators are associated with improved rates of screening and follow-up, lower clinical stage of presentation, and higher patient satisfaction.11, 14, 15, 16 While these studies have shown the impact of navigation at the patient-level can be significant, in this study we find that health navigators need not be limited to providing services to patients; QIDS Policy Navigators, as we have referred to them, effectively work at the larger health-system level and provide advocacy and coordination to decision-makers, increase access to care, and thus impact communities as a whole.
Conclusion
Our experience with health insurance enrollment of indigent households underscores the importance and cost-effectiveness of a Policy Navigator's one-to-one marketing efforts targeted to the key decision-makers. This effectiveness of this approach has mainly to do with the ability to deal with specific problems and the unique local context of protecting the indigent against the uncertainty of health care spending.
The national-level enrollment incentives introduced have also helped increase enrollment levels. However, we find evidence that some may have crowded out enrollment initiatives at the local level. It is thus important for policymakers to carefully program enrollment initiatives, especially when these could be launched at both national and local levels, given that objectives of national and local leaders could be widely divergent.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Musgrove P, Zeramdini R, Carrin G. Basic patterns in national health expenditure. Bulletin of the World Health Organization. 2002;80:134–142. [PMC free article] [PubMed] [Google Scholar]
- 2.Daniels N, Bryant J, Castano RA, Dantes OG, Khan KS, Pannarunothai S. Benchmarks of fairness for health care reform: a policy tool for developing countries. Bulletin of the World Health Organization. 2000;78(6):740–750. [PMC free article] [PubMed] [Google Scholar]
- 3.Aday LU, Andersen R. A framework for the study of access to medical care. Health Services Research. 1974;9(3):208–220. [PMC free article] [PubMed] [Google Scholar]
- 4.Thorpe KE. Incremental strategies for providing health insurance for the uninsured. Projected federal costs and number of newly insured. Journal of the American Medical Association. 1997;278(4):329–33. [PubMed] [Google Scholar]
- 5.Yip W, Berman P. Targeted health insurance in a low income country and its impact on access and equity in access: Egypt's school health insurance. Health Economics. 2001;10(3):207–20. doi: 10.1002/hec.589. [DOI] [PubMed] [Google Scholar]
- 6.Schieber G, Baeza C, Kress D, Maier M. Disease Control Priorities in Developing Countries. 2nd. New York: Oxford University Press; 2006. Financing Health Systems in the 21st Century; pp. 225–242. Chapter 12. [Google Scholar]
- 7.Carrin G. Social health insurance in developing countries: a continuing challenge. International Social Security Review. 2002;54(2):57–69. [Google Scholar]
- 8.Shimkhada R, Peabody JW, Quimbo S, Solon O. The Quality Improvement Demonstration Study: An example of evidence-based policy-making in practice. Health Research Policy and Systems. 2008;25(6):5. doi: 10.1186/1478-4505-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Philippine Health Insurance Corporation. Implementing Rules and Regulations (IRR) 2004. 2004. [Google Scholar]
- 10.The Republic of the Philippines. Republic Act 7875 – National Health Insurance Act of 1995. 1995 http://www.philhealth.gov.ph/download/IRR2004.pdf.
- 11.Obermann K, Jowett MR, Alcantara MO, Banzon EP, Bodart C. Social health insurance in a developing country: The case of the Philippines. Social Science & Medicine. 2006;62(12):3177–3185. doi: 10.1016/j.socscimed.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 12.Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. A patient navigation intervention. Cancer. 2007;109(2 Suppl):359–367. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- 13.Betancourt JR. Improving Quality and Achieving Equity: The Role of Cultural Competence in Reducing Racial and Ethnic Disparities in Health Care. The Commonwealth Fund, October 2006 2006 [Google Scholar]
- 14.Evidence report and evidence-based recommendations: Cancer prevention and treatment demonstration for ethnic and racial minorities. Centers for Medicare and Medicaid Services; Bethesda, MD: United States Department of Health and Human Services; 2003. [Google Scholar]
- 15.Dohan D, Schrag D. Using navigators to improve care of underserved patients. Cancer. 2005;104:848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen TU, Tanjasiri SP, Kagawa-Singer M, Tran JH, Foo MA. Community Health Navigators for Breast- and Cervical-Cancer Screening Among Cambodian and Laotian Women: Intervention Strategies and Relationship-Building Processes. Health Promotion Practice. 2006 doi: 10.1177/1524839906290251. Epub ahead of print, Dec 13, 2006. [DOI] [PubMed] [Google Scholar]