Abstract
Technology has great potential to reduce medication errors in hospitals. This case report describes barriers to, and facilitators of, the implementation of a pharmacy bar code scanning system to reduce medication dispensing errors at a large academic medical center. Ten pharmacy staff were interviewed about their experiences during the implementation. Interview notes were iteratively reviewed to identify common themes. The authors identified three main barriers to pharmacy bar code scanning system implementation: process (training requirements and process flow issues), technology (hardware, software, and the role of vendors), and resistance (communication issues, changing roles, and negative perceptions about technology). The authors also identified strategies to overcome these barriers. Adequate training, continuous improvement, and adaptation of workflow to address one's own needs mitigated process barriers. Ongoing vendor involvement, acknowledgment of technology limitations, and attempts to address them were crucial in overcoming technology barriers. Staff resistance was addressed through clear communication, identifying champions, emphasizing new information provided by the system, and facilitating collaboration.
Introduction
Patient safety has become a hot-button topic in research and media during recent years. Patient injuries are most commonly due to adverse drug events (ADEs), which occur at a rate of 6.5% or approximately 1,900 ADEs per hospital per year. 1–3 Many of these ADEs are caused by medication errors and are by definition preventable. These errors may occur during any stage of the medication use process including ordering, transcribing, dispensing, administering, and monitoring. Most of the solutions to medication errors, such as computerized physician order entry (CPOE) systems, have focused on reducing errors at the medication ordering stage. 4,5 However, dispensing errors are estimated to occur at a rate of nearly 4%, of which only 80% are intercepted. In a large hospital, these error rates can translate to more than 45,000 undetected dispensing errors annually. 6–8
Pharmacy bar code scanning technology offers a new strategy to address medication errors in the hospital setting. It seeks to ensure that the correct medications are dispensed to patient care units and that they carry a bar code for nurses to scan before administering the dose to a patient. The successful implementation of this technology has been shown to reduce medication dispensing errors alone by 85%. 7,9,10 In addition, emerging evidence indicates minimal impact on nursing workflow, 11,12 and a positive financial return on bar code scanning technology 13 from the hospital's perspective.
Despite these promising results, few hospital pharmacies have implemented bar code scanning technology. In general, problems that occur during implementation have led to complete halt of the project, 14 staff revolt, 15 or even poor patient outcome. 16–19 The literature documents success factors for the implementation of hospital information systems 2,20–34 such as organizational leadership, the availability of capital, and product/vendor maturity. Successful pharmacy bar code scanning system implementation must address not only these considerations, but also the high dispensing volume in a hospital pharmacy and the role of pharmacists as consultants to other clinicians. The literature on pharmacy bar code scanning technology is sparse 9,10,35 and focuses on clinicians' use of these systems after they have been implemented 36–38 rather than on the implementation process itself. We present this case report to capture our lessons learned during a recent successful implementation of a pharmacy bar code scanning system at a large academic center.
Case Description
The case site is a 750-bed tertiary care Academic Medical Center in Boston, MA, where approximately 5.9 million doses of medications are dispensed per year from the central inpatient pharmacy. The hospital pharmacy employs sixty-one full time equivalent pharmacists and 45 full time equivalent pharmacy technicians. In Nov and Dec 2003, the hospital pharmacy converted to a bar code–assisted medication dispensing process. This pharmacy initiative occurred as part of the implementation of bar code scanning systems at the bedside, and the project was a major joint initiative between the pharmacy and the nursing staff.
The initial implementation of the pharmacy bar code scanning technology required a dedicated pharmacy-based medication repackaging center, which affixed two-dimensional bar codes onto the lowest unit dose of every medication that did not already have a bar code from the manufacturer. 7 As the medications were picked from inventory, pharmacy technicians scanned each bar code to match the medication, strength, and dose with the pharmacist-approved physician order. The medications were then sent to the patient care areas and rescanned by nurses at the point of care to further reduce medication administration errors.
While this technology has significantly reduced medication dispensing errors 7 and produced a positive return on investment for the hospital, 13 the implementation team initially encountered significant challenges, which they ultimately overcame. To capture some of the lessons learned, we interviewed pharmacy leaders, pharmacists and pharmacy technicians about their experiences during the implementation process. We conducted a qualitative analysis of the barriers to, and facilitators of, the pharmacy bar code scanning system implementation, taking a close look at sources of resistance and how to overcome them.
Methods
To understand the barriers to and facilitators of this implementation, we conducted interviews of pharmacy staff, supplemented by a review of project documentation.
Interview Instrument
Based on prior work related to the implementation of both CPOE 2,24,39,40 and the bar code scanning system, we developed a semi-structured interview instrument to elicit the pharmacy staff's perceptions of barriers to, and facilitators of, the bar code scanning system implementation in the hospital pharmacy. Interviews took place during a 1-year period following system implementation. Each interview lasted approximately one-half hour and was conducted by at least one investigator who recorded field notes during the interview.
Identifying Informants
We contacted pharmacy personnel who were either using the bar code scanning system or involved in its implementation. The initial set of interviewees was selected by pharmacy leaders from a total of 150 potential informants. As the interviews progressed, we asked our informants to help identify other staff members who were knowledgeable about the process. We continued the interviews until we were no longer gaining new information or insights from successive informants. Written consent was obtained from all participants with the understanding that they were able to withdraw from the study at any time. Institutional review board approval was obtained at the study site.
Ten interviews were conducted by two investigators between Dec 2004 and Aug 2005. Two interviewees were pharmacy leaders, four were pharmacists and four were technicians. We presented our findings to the pharmacy leaders to verify our results.
Code List
We analyzed the interview notes for common themes with the aid of ATLAS.ti software (Scientific Software Development, Berlin). Through five iterative readings of the field notes, we developed a code list to characterize the factors that influenced the system implementation. Using this code list, two independent reviewers iteratively coded a subset of three transcripts, modifying the code list and the code definitions as necessary, until they reached 89% reliability, defined as the fraction of phrases that were coded in an identical manner by both reviewers. 41 One reviewer subsequently coded the entire set of field notes. The reviewer met regularly with coinvestigators to discuss emerging themes, organize the code list under these themes, and further delineate the relationships among these themes. Meeting minutes of weekly implementation team meetings from Jan to August 2004 were also reviewed to confirm the themes and to clarify relationships between themes.
Findings
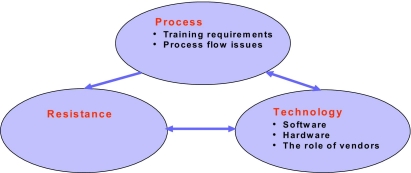
We identified three main barriers (▶) to pharmacy bar code scanning technology implementation at our hospital and strategies to overcome them.
Figure 1.
Barriers to Barcode System Implementation.
Process
Training
As with any system implementation, training must be initiated early on. In an effort to get the pharmacy technicians familiar with scanning, the pharmacy implemented bar code-assisted dispensing for medications destined for the neonatal intensive care unit (NICU) 1 year before full deployment of the bar code scanning system. As there were usually expert system users available, and the volume of medications requiring scanning during the NICU-pilot was low, training was on-the-job, without formal classes. However, the volume of drugs requiring scanning increased dramatically after full system deployment. Even though most technicians were familiar with scanning and were given additional informal training, this was a challenging period.
Certain pharmacy technicians thought that they were not adequately trained and identified this as an obstacle to system implementation. Although the addition of formal training may have helped, limited computer literacy and language barriers made this challenging. Increased time and resources would have been required to ensure that the training was appropriate for a range of skill sets and tailored to individual differences in learning curves. Pharmacy leaders also recognized the importance of training to the system implementation process. One leader explained that “Scanning is an art. People need to practice to get used to the technique.” Consequently, as the technicians gained more experience with scanning, their comfort level with the new system increased.
The respondents who reported a desire to have more training available made suggestions ranging from formal training sessions to simulation laboratories to “super-users”. Super-users are peers who receive focused training and provide ongoing informal support to their colleagues. The superuser model functions synergistically with formal training, and was used to implement bar code-assisted medication administration for nurses in the patient care areas subsequent to the pharmacy system implementation. Although the pharmacy did not have the budget to implement the superuser model, technicians who had difficulties with scanning did receive one-on-one training.
Process Flow Issues
As with any large project, the pharmacy bar code scanning system implementation had to overcome a few unexpected challenges, which usually involved workflow redesign. For example, during the initial system implementation, three days worth of medication were dispensed at a time, known as a “three-day fill”. This practice was originally intended to limit the number of daily fills by increasing the volume of medications dispensed. However, since a significant proportion of patients remain in hospital for fewer than three days, many medications were returned and the patients' accounts were credited for unused medication. This crediting process led to increases in the overall workload for pharmacy technicians. Fortunately, pharmacy leadership elicited these concerns and changed the three-day fill to a two-day fill, decreasing the crediting requirements.
Many informants reported other cases where continuous improvement principles were successfully incorporated into the system implementation process. For example, the pharmacy information system was originally set up to dispense medications at standardized times each day. This was revised when pharmacists suggested that they would like the ability to schedule the first dose of a medication at a different time than the remaining doses. Another challenge surfaced when the pharmacy leaders realized that the technicians found it easier to use their laptops and scanners in central pharmacy locations than in the individual areas where each medication is housed. By allowing the technicians to optimize their own workflow, the pharmacy leaders overcame these unexpected challenges and fostered a collaborative working environment.
Technology
Like most implementations of a new technology, several technical problems affected system implementation. These included hardware and software problems, and the role of vendors. Hardware problems were largely related to scanning equipment. Common complaints included “bar codes not scanning” and the wireless scanner battery draining at inopportune times. One pharmacy leader explained that batteries drained because users were holding down the scan button continuously, causing bar codes to repeatedly scan. This behavior was unanticipated and therefore not addressed during the training process. However, the implementation team promptly identified the improper technique and technicians were appropriately re-educated.
The implementation team also noted that some of the medications encoded in the bar codes were missing from the dictionary of pharmaceutical products or mapped to incorrect products. To address this issue, pharmacy leaders created a process whereby technicians report all unscannable products to designated personnel who identified and corrected the problem. Another problem occurred when some products had bar codes on reflective surfaces that were difficult to scan. The pharmacy leaders identified alternate manufacturers with bar codes that were easier to scan. While these issues were promptly overcome, some respondents expressed frustration with the process, suggesting that more extensive testing before go-live might have uncovered these problems earlier.
To address many of these technology issues, pharmacists and pharmacy leaders identified the role of vendors as a critical success factor. Several strategies for choosing a vendor were suggested. First, the vendor should provide long-term on-site formal training and support that covers all shifts. Second, to maximize workflow customization and resolve problems that arise during the implementation process, the vendor must have the resources to work with the implementation team to make specific changes to its system as difficulties arise. This is especially important with the implementation of a relatively new technology like a bar code scanning system.
Staff Resistance
Staff resistance to bar code scanning system implementation was a prominent barrier identified in our interviews. Fortunately, the team also identified many strategies to overcome it.
Resistance was driven by three main factors: communication issues, staff feeling overwhelmed because of changing roles, and negative perceptions about technology.
Some pharmacists and pharmacy technicians perceived that the pharmacy staff was “led to believe that [the new system] would make the work a lot easier” when it in fact initially involved “a lot more work.” One pharmacy leader explained that “some of the technicians didn't see the big picture. Although it may initially take longer with the bar code scanning system, the entire process becomes more efficient. Maybe [the leadership] did not get as much buy-in up front as we could have.” Clear communication around workload expectations during the implementation process may mitigate much of these misunderstandings and the resulting staff resistance.
Changing roles were also an important cause of resistance among staff as some had entirely different job descriptions with the new system. As one pharmacist described, “They weren't embracing the system because they were accustomed to doing something for a long time and all of a sudden they had this thrown at them.” For example, pharmacy technicians who had previously spent a significant amount of time crediting unused medications had to eliminate that activity and learn how to use the bar code scanner. Also, the scanning system eliminated the pharmacists' need to spend a significant portion of time double-checking drugs that were manually dispensed or manually cross-checking the patient and medication. They were instead able to focus on collaborating with the technicians and resolving any discrepancies that the system revealed.
While the prospect of changing roles led to significant resistance in some cases, the change also presented an opportunity to identify new champions to help with the implementation process. Champions were well-respected pharmacists and technicians who took on leadership roles during system implementation by encouraging users to look beyond any immediate frustrations, working through hurdles with them, and reminding them of the system's downstream benefits. One pharmacy leader explained, “As roles changed, certain people embraced the changes more than others. We encouraged these people to become champions and placed them up on pedestals so that they could set an example for the others.”
Another contributor to resistance was negative perceptions about the technology. Three main negative perceptions were identified through the interviews: overdependence on technology, potential for harm, and concerns about increased performance monitoring. One respondent explained that the pharmacists “rely on the system more and more to be accurate … When it's down, (we) run into a hard time.” Another expressed a safety concern with the shift from manual checks to automated checks. She stated that “if a mistake is not caught [by the automated check], the patient might be at risk.” A pharmacy technician outlined her concerns about performance monitoring, saying that “some people think that this system was put into place as a way to track them and [their] performance.” These negative perceptions about technology were mitigated by its useful functionality. As users interacted with the new system, they discovered that it offered information that they previously lacked ready access to. For example, one informant explained, “the system allows me to track things better; if a medication is sent wrong, I can track who, what, when and why it happened.” Informants acknowledged the usefulness of the increased information in preventing medication errors. Another reported, “I now have the ability to see dosing frequencies and understand the principles of drug regimens!” Increased information empowered the technicians and pharmacists to be more involved in the pharmacy processes, leading to an increased sense of involvement in patient care.
The bar code scanning technology also facilitated collaboration and teamwork, which served as a catalyst for system adoption. Our informants reported that in situations where the staff had increased collaboration and teamwork in a new role, the response to change was a favorable one. As one technician stated, “With this system, there is involvement and I have a sense of working with the pharmacists rather than beneath them.” Another technician explained that “we have a better understanding of when the medications are needed [to be administered] up on the floors and that opens up our communication with the pharmacists regarding availability [of these medications]” A pharmacist reported that “there had to be more communication [with technicians] to ensure that we were getting patient meds to the unit correctly as well as identifying when things were not working as designed. I don't think it was the additional information on the labels [that changed how we work together but it was instead] a result of needing each other to get the system implemented.” This collaboration and teamwork further fostered self-motivation and information sharing. For example, another technician added, “My responsibilities have increased [to include checking the medication dose and frequency, tracking the medication and identifying and intercepting errors as opposed to just dispensing the medication] but not because someone told me to do something. It comes from my own doing. I take it upon myself to fulfill the responsibilities.”
Relationship among the Three Major Barriers
Staff resistance and process and technology barriers are interrelated and all lead to system flaws such as workarounds, in which users find creative ways to bypass the intended safety features of the system. For example, inadequate training, process flow issues, and technology shortcomings contributed to resistance as pharmacy staff felt overwhelmed and developed negative perceptions about the technology. This, in turn, encouraged users to find creative alternatives to scanning. As one technician reported, “If it didn't scan right away, we would manually override everything.” Another expressed a concern with scanning multiple doses of the same medication. Instead of scanning 25 separate tablets, she reported that “one tablet is being scanned 25 times.” Our pharmacy leaders dealt with this by being aware of these behaviors, continuously resolving any system issues that arose in a timely fashion and ensuring ongoing communication between pharmacy technicians, pharmacists and pharmacy leaders.
Discussion
Using a qualitative approach, we identified three major barriers to implementing pharmacy bar code scanning technology at our center: Processes, technology issues, and staff resistance. Although these barriers were significant, our informants identified strategies to overcome them.
Our results are consistent with barriers to CPOE system implementations that are reported in the literature. 18,24,25 Ash reported that when clinicians have access to more information with which to make decisions, and when the system fits with their workflow, they tend to use it. Miller stated that champions and positive physician attitudes toward technology were essential to successful CPOE implementation. Our case suggests that these principles hold true not only for physicians but also for pharmacists and pharmacy technicians with varying backgrounds, responsibilities and levels of education.
Our results are also consistent with problems with clinician use of bar code medication administration systems that are reported in the literature. 36 Our case suggests that many of the workarounds created by clinicians, such as omission of process steps or performing steps out of sequence 36 are also created by pharmacists and pharmacy technicians during the system implementation process. Important safety issues introduced by clinician use of bar code scanning systems, such as degraded coordination between nurses and physicians, 37 nurses dropping activities to reduce workload during busy periods 37 and changes in communication between nurses 38 have been reported in the literature. Many of the barriers we identified in the pharmacy environment are similar to these issues identified at the bedside and our solutions may be useful outside of the pharmacy.
Pharmacy bar code scanning systems present several unique implementation issues. For example, training requirements are less uniform than those of physicians during CPOE implementation due to a larger variation in education and skill level within a pharmacy. Furthermore, unlike physicians, pharmacy technicians are generally employees of the hospital and not as influential in the decision making process since their activities are not directly tied to hospital revenues. Although these differences represent unique organizational and interpersonal challenges that contribute to resistance, they can also be leveraged to overcome the resistance.
An interesting paradox was noted with pharmacy and pharmacy technicians' reactions to the increased information available to them through the new system. While some were concerned that the technology would allow their own work to be tracked, others welcomed the opportunity to be able to track a medication through it entire cycle in the hospital. As with other information systems, this tracking capability can be a double-edged sword, acting as either a barrier or facilitator to implementation.
In this case example, the hospital chose a “big-bang” approach by implementing the entire bar code scanning system within a short time frame. Although some pharmacists and technicians expressed preference for a more incremental implementation, pharmacy leaders preferred the big-bang approach because they felt they had the political capital to execute a series of significant workflow changes and that momentum for these changes would be lost if they were introduced individually. Also, in a geographically and organizationally coherent area like the pharmacy, systems may be so interconnected that it is impractical to implement components one at a time. Much debate around this issue has been documented in the literature. 17 Although our work cannot universally endorse the big bang approach, in this case it seemed to be a reasonable choice.
Many opportunities exist for hospital leaders and policy makers to facilitate the adoption of pharmacy bar code scanning systems. First, hospital leaders need to consider the true cost of technology implementation, beyond just software and hardware. The largest roadblocks are often related to process redesign and organizational resistance, and hospital leaders should devote sufficient financial resources and personal attention to this. Second, policy makers should actively promote knowledge sharing from the implementation process itself, as implementation challenges directly threaten the quality and safety of health information technology. 16,17 Health information technology projects sponsored by various agencies within the federal government such as the office of the national coordinator for health information technology (ONCHIT) and the Agency for Healthcare Research and Quality (AHRQ) provide ideal mechanisms for this information exchange. Third, a shift in workforce capacity may be necessary, with a focus on clinicians who understand workflow issues well enough to redesign processes and are also trained to select appropriate technologies and manage vendor relationships.
In summary, bar code scanning system implementation is a difficult process with several barriers involving processes, technology and organizational resistance. Fortunately, our informants identified many strategies to overcome these barriers. We hope that other health care centers can use these lessons learned to realize the full benefits of bar code scanning technology.
Footnotes
This work was supported in part by a grant from the Agency for Healthcare Research and Quality # HS14053-02.
References
- 1.Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. J Am Med Assoc 1995;274:29-34. [PubMed] [Google Scholar]
- 2.Doolan DF, Bates DW. Computerized physician order entry systems in hospitals: Mandates and incentives Health Aff Millwood 2002;21:180-188. [DOI] [PubMed] [Google Scholar]
- 3.Leape LL, Bates DW, Cullen DJ, et al. Systems analysis of adverse drug events. ADE Prevention Study Group. J Am Med Assoc 1995;274:35-43. [PubMed] [Google Scholar]
- 4.Bates DW. Using information technology to reduce rates of medication errors in hospitals BMJ 2000;320:788-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gawande AA, Bates DW. The use of information technology in improving medical performance. Part II. Physician-support tools. Medgenmed Medscape Gen Med 2000:E13. [PubMed]
- 6.Cina J. How many hospital pharmacy medication dispensing errors go undetected? Joint Community J Qual and PT Saf 2006;32:73-80. [DOI] [PubMed] [Google Scholar]
- 7.Poon EG, Cina JL, Churchill W, et al. Medication dispensing errors and potential adverse drug events before and after implementing Bar code technology in the pharmacy. Ann Intern Med 19/9/06;145(6):426–434. [DOI] [PubMed]
- 8.Beso A, Franklin BD, Barber N. The frequency and potential causes of dispensing errors in a Hospital Pharmacy Pharm World Sci 2005;27:182-190. [DOI] [PubMed] [Google Scholar]
- 9.Douglas J, Larrabee S. Bring Barcoding to the bedside Nurs Manag 2003;34:36-40. [DOI] [PubMed] [Google Scholar]
- 10.Neuenschwander Practical guide to Bar coding for patient medication safety Am J Health Syst Pharm 2003;60:768-779. [DOI] [PubMed] [Google Scholar]
- 11.Poon E, Keohane CA, Featherstone E, et al. Impact of barcode medication administration technology on how nurses spend their time on clinical care AMIA Annu Symp Proc 2006:1065. [PMC free article] [PubMed]
- 12.Keohane CA, Bane A, Hurley AC, et al. Quantifying nursing workflow in medication administration J Nurs Admin 2008. [DOI] [PubMed]
- 13.Maviglia S, Yoo J, Franz C, et al. Analysis of a pharmacy barcode solution Proc of the AMIA Annu Spring Congress, AMIA 2006.
- 14.Morrissey J. Harmonic divergence. Cedars-Sinai joins others in holding off on CPOE. Mod Healthc 2004;34:16. [PubMed] [Google Scholar]
- 15.Massaro TA. Introducing physician order entry at a major Academic Medical Center. II. Impact on medical education. Acad Med 1993;68:25-30. [DOI] [PubMed] [Google Scholar]
- 16.Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors JAMA. J Am Med Assoc 2005;293:1197-1203. [DOI] [PubMed] [Google Scholar]
- 17.Han YY, Carcillo JA, Venkataraman ST, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system Pediatrics 2005;116:1506-1512. [DOI] [PubMed] [Google Scholar]
- 18.Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: The nature of Patient Care information system-related errors J Am Med Inform Assoc 2003:104-112Nov 21. [DOI] [PMC free article] [PubMed]
- 19.McDonald CJ. Computerization can create safety hazards: A Bar-coding near miss Ann Intern Med 2006;144:510-516. [DOI] [PubMed] [Google Scholar]
- 20.Browmann G. Improving clinical practice guidelines for the 21st century: Attitudinal barriers and not technology are the main challenges Int J Technol Assess Health Care 2000;16:959-968. [DOI] [PubMed] [Google Scholar]
- 21.McLane S. Designing an EMR planning process based on staff attitudes toward and opinions about computers in healthcare Comput Inform Nurs 2005;23:85-92. [DOI] [PubMed] [Google Scholar]
- 22.Nohr C. Development, implementation and diffusion of Ehr systems in Denmark Int J Med Inform 2005;74:229-234. [DOI] [PubMed] [Google Scholar]
- 23.Tonnesen AS, LeMaistre A, Tucker D. Electronic medical Record implementation barriers encountered during implementation Proc AMIA Annu Fall Symp 1999:624-626. [PMC free article] [PubMed]
- 24.Poon EG, Blumenthal D, Jaggi T, et al. Overcoming the barriers to implementing computerized physician order entry systems in US hospitals: Perspectives from senior management Health Aff 2004;23(4):184-190. [DOI] [PubMed] [Google Scholar]
- 25.Miller RH, Sim I. Physicians' use of electronic medical records: Barriers and solutions Health Aff Millwood 2004;23:116-126. [DOI] [PubMed] [Google Scholar]
- 26.Aarts J, Doorewaard H, Berg M. Understanding implementation: The case of a computerized physician order entry System in a Large Dutch university medical Center J Am Med Inform Assoc 2004;11:207-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ammenwerth E, Iller C, Mahler C. IT-adoption and the interaction of task, technology and individuals: A fit framework and a case study BMC Med Inform Decis Mak 2006;6:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ash JS, Stavri PZ, Kuperman GJ. A consensus statement on considerations for a successful CPOE implementation J Am Med Inform Assoc 2003;10:229-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ash JS, Fournier L, Stavri PZ, Dykstra RH. Principles for a successful computerized physician order entry implementation AMIA Annu Symp Proc 2003:36-40. [PMC free article] [PubMed]
- 30.Aydin CE, Forsythe DE. Implementing. Computers in ambulatory care: implications of physician practice patterns for system design. AMIA Annu Symp Proc 1997:677-681. [PMC free article] [PubMed]
- 31.Berg M. Implementing information systems in health care organizations: Myths and challenges Int J Med Inform 2001;64(2–3):143-156. [DOI] [PubMed] [Google Scholar]
- 32.Callen JL, Braithwaite J, Westbrook JI. Contextual implementation model: A framework for assisting clinical information system J Am Med Inform Assoc 2008;15(2):255-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lorenzi NM, Novak LL, Weiss JB, Gadd CS, Unertl KM. Crossing the implementation chasm: A proposal for Bold action J Am Med Inform Assoc 2008;15(3):290-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reddy MC, McDonald DW, Pratt W, Shabot MM. Technology, work, and information flows: Lessons from the implementation of a wireless alert pager system J Biomed Inform 2005;38(3):229-238. [DOI] [PubMed] [Google Scholar]
- 35.Wright A, Katz IB. Coding for patient safety N Engl J Med 2005;353:329-331. [DOI] [PubMed] [Google Scholar]
- 36.Koppel R, Wetterneck T, Telles JL, Karsh B-T. Workarounds to Barcode Medication Administration. Systems: Their occurrences, causes and threats to patient safety. J Am Med Inform Assoc 2008;15(4):408-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patterson E, Cook RI, et al. Improving patient safety by identifying side effects from introducing Bar coding in medication administration J Am Med Inform Assoc 2002;9:540-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Novak LL, Barcode Medication Administration Understanding patient safety risks Informatics Training Conference 2008.
- 39.Ash JS, Gorman PN, Hersh WR, Lavelle M, Poulsen SB. Perceptions of house officers who use physician order entry Proceedings AMIA Annual Symposium 1999:471-475. [PMC free article] [PubMed]
- 40.Dykstra Computerized physician order entry and communication: Reciprocal impacts Proc Annu AMIA Symposium 2002. [PMC free article] [PubMed]
- 41.Strauss A, Corbin J. Basics of Qualitative Research. Techniques and procedures for Developing Grounded Theory. 2nd edn. Sage Publications; 1998.