Abstract
Objective
To assess the impact of using wireless e-mail for clinical communication in an intensive care unit (ICU).
Design
The authors implemented push wireless e-mail over a GSM cellular network in a 26-bed ICU during a 6-month study period. Daytime ICU staff (intensivists, nurses, respiratory therapists, pharmacists, clerical staff, and ICU leadership) used handheld devices (BlackBerry, Research in Motion, Waterloo, ON) without dedicated training. The authors recorded e-mail volume and used standard methods to develop a self-administered survey of ICU staff to measure wireless e-mail impact.
Measurements
The survey assessed perceived impact of wireless e-mail on communication, team relationships, staff satisfaction and patient care. Answers were recorded on a 7-point Likert scale; favorable responses were categorized as Likert responses 5, 6, and 7.
Results
Staff sent 5.2 (1.9) and received 8.9 (2.1) messages (mean [SD]) per day during 5 months of the 6-month study period; usage decreased after study completion. Most (106/125 [85%]) staff completed the questionnaire. The majority reported that wireless e-mail improved speed (92%) and reliability (92%) of communication, improved coordination of ICU team members (88%), reduced staff frustration (75%), and resulted in faster (90%) and safer (75%) patient care; Likert responses were significantly different from neutral (p < 0.001 for all). Staff infrequently (18%) reported negative effects on communication. There were no reports of radiofrequency interference with medical devices.
Conclusions
Interdisciplinary ICU staff perceived wireless e-mail to improve communication, team relationships, staff satisfaction, and patient care. Further research should address the impact of wireless e-mail on efficiency and timeliness of staff workflow and clinical outcomes.
Introduction
Clinical communication in hospitals consists of information exchanges between healthcare workers and includes face-to-face conversations, telephone calls, and e-mail. 1 Such exchanges are voluminous, often complex, and vital for patient care. However, clinical communication is frequently interrupted and of poor quality, 2 leading to inefficiencies in care delivery, 3,4 preventable medical error, 5–10 and frustration in medical staff. 4,11 These issues are particularly important in an intensive care unit (ICU), which may have even more interrupted communications than other healthcare settings 12 and where rapid and accurate communication is essential to delivering safe patient care. 2
Given these issues, optimizing clinical communication may improve the quality of patient care. An ideal communication tool would enable bidirectional, rapid, secure, and nondisruptive transmission of content-rich messages. Current hospital-based communication methods rely primarily on numeric paging, which falls short of this ideal. 13–15 Providers have attempted to mitigate these limitations in selected clinical situations by implementing automated wireless alerting systems using alphanumeric paging, 16–21 user-initiated alphanumeric paging of physicians, 22 and wireless voice systems. 23 While offering some advantages, these systems lack bidirectional communication capacity (paging), user-initiated messages (some alphanumeric paging systems), or capability for non-simultaneous communication (voice). One potential communication tool that may overcome these limitations is real-time or push wireless e-mail, which has been widely adopted in business. 24
Our initial interest in wireless e-mail as an interdisciplinary communication strategy arose from a critical incident at the study hospital in which an intensivist was handling multiple simultaneous (nonurgent) queries from nursing staff while reviewing a chest radiograph for feeding tube placement. He became distracted by these multiple tasks and missed the radiographic diagnosis of intrapulmonary feeding tube placement. In a community ICU without house staff, situations of multiple competing time demands on one physician provider are common, in our experience. Our objective was to implement wireless e-mail to facilitate communication among members of an interdisciplinary healthcare team in a large community hospital ICU. At the end of the implementation period, we developed and administered a questionnaire to ICU staff to evaluate the perceived impact of wireless e-mail on communication, team relationships, job satisfaction, and patient care. We also recorded the number of e-mails transmitted and received during and after the study period.
Background
Communication Tasks in the ICU
Effective care of the critically ill patient requires communication among all participants in the patient's care, including physicians (intensivists, consultants, house staff in a teaching hospital), nurses, pharmacists, respiratory therapists, and other allied health personnel (physiotherapists, dieticians, social workers). 25–27 All these healthcare workers are mobile, traveling both within and outside the ICU. The traditional forum for patient assessment and interdisciplinary communication is bedside rounds, which typically occur at least once daily. 28,29 However, substantial clinical activity occurs outside of rounds: new patients are assessed and admitted, patients who have recovered sufficiently are discharged, current patients have ongoing care needs, and care is transferred from one provider to another (for example, between nurses when one takes a break). These clinical episodes lead to interdisciplinary communication events, for example, between nurses and physicians, between nurses, or between nurses and respiratory therapists. 3,12,30 Examples include notification of a minor or major clinical deterioration, planning for intrahospital transport for a test, scheduling of a family meeting, or temporary transfer of care.
Current Methods of Communication in the ICU
The substantial volume of communication generated by acute patient care must be integrated into the workflow of busy and mobile clinical staff. 12,31–34 Commonly used communication tools have significant limitations, integrating poorly with clinical workflow and reducing healthcare team effectiveness. 35 The most prevalent of these tools, the numeric pager, is limited by low information content. Paging of healthcare workers has been reported to disrupt patient care and teaching rounds. 13–15 Although approximately one-third of pages require a timely response and lead to a change on patient care, 14,15 traditional numeric paging offers no triage mechanism, leading to frustration for clinical staff. 11
Direct communication between healthcare workers by face-to-face or telephone conversation results in rapid information transfer, but misunderstandings may lead to errors in a high-risk ICU environment. 5–10 Factors contributing to verbal miscommunications may include the requirement for simultaneous attention of both parties for information transfer (synchronous communication), which can interrupt clinical activities already in progress, failure to accurately recall the information in the conversation, and lack of specificity of the actual message. 2
Other methods of communication also have disadvantages. Physician “ask lists” (written notes left at a patient's bedside or nursing station) may be difficult to locate and inappropriate for urgent messages. Overhead paging has limited geographic reach, cannot communicate long or sensitive messages, and may be disruptive to patients and staff. In-person searches for staff members, even if successful, can be time-consuming and may interrupt current tasks for both parties. Desktop computer-based e-mail requires frequent checking for new messages. Implementation of alphanumeric text paging systems has increased the information content of messages and allowed for triage of message urgency, but has not eliminated the need for direct communication between healthcare workers. 22
A review of mobile healthcare information communication technologies discussed devices to facilitate clinician access to patient information, but did not consider technology to push information to clinicians or allow interclinician communication. 36 Similarly, we found no published reports of wireless push e-mail in healthcare team communication. We searched Ovid MEDLINE (1950−) on Mar 4, 2009 using the strategy “exp Electronic Mail/and wireless.mp” and retrieved 3 relevant citations discussing transmission of medical images 37,38 or recording of educational experiences. 39 Although other studies have described automated wireless alerting systems using alphanumeric paging, 16–21 user-initiated alphanumeric paging of physicians, 22 wireless voice systems, 23 and wireless personal digital assistants, 40 we could find no description of wireless e-mail communication among healthcare team members.
Rationale for Wireless E-Mail in the ICU
Several attributes of wireless e-mail make it well-suited to healthcare communication: information-rich, specific, legible, and time-stamped messages can be sent almost instantaneously to one or many healthcare workers. These characteristics have been endorsed in reports of healthcare workers' stated communication needs 11,41 and in feedback after implementation of alphanumeric text paging. 22 Although notification of a new wireless e-mail by sound or device vibration creates a brief interruption, wireless e-mail itself does not require simultaneous communication involving both parties. The handling of the message content is therefore an asynchronous process and less likely to disrupt the recipient's current task compared to synchronous communication tools such as telephone or face-to-face discussion. 1 The transmission of specific information facilitates rapid triaging of messages, enabling better organization of personal workflow. The information in messages remains available for future review, which facilitates accurate information transfer and subsequent inclusion in the patient chart. Finally, in our preliminary experience, the recipient could often address the issues in the message by responding with a return wireless e-mail. The rapid, accurate, and nondisruptive information exchange via wireless e-mail makes it an attractive communication tool in the information-laden environment of hospital patient care.
Methods
Setting
We conducted this study in a 26-bed medical-surgical ICU in a community hospital in Mississauga, ON, Canada. The ICU operated using an intensivist-led interdisciplinary team model. The ICU, containing only individual patient rooms and 2 nursing stations, is physically divided into two geographic areas separated by approximately 150 m: one 20-bed unit and one 6-bed satellite unit. The area of the main ICU is approximately 480 m2. The study population consisted of 4 intensivists and 121 interdisciplinary staff members (nurses, respiratory therapists, pharmacists, social workers, unit clerks, and ICU nurse-leaders) who worked daytime shifts. Night staff did not participate in the trial. With the exception of respiratory therapists, who worked in all hospital departments, staff members worked almost exclusively in the ICU.
Baseline Communication Methods
Prior to study implementation, ICU staff members used various communication methods, including receive-only numeric pagers, overhead paging, physical searches for staff, handwritten messages left in or near patient charts, and e-mail, which required the use of the hospital e-mail system (Meditech, Westwood, MA) and could only be accessed using desktop computers. Intensivists acquired personal wireless e-mail devices (BlackBerry, Research in Motion [RIM], Waterloo, ON) at their own expense over a six-month period before the start of the trial.
All baseline communication methods remained available during the study period. ICU staff members were free to choose the method of communication depending on the clinical situation and could use several different methods if needed. For example, the initial notification of a problem could be via wireless e-mail with a preliminary response via wireless e-mail followed by subsequent direct in-person communication. We did not record usage data of baseline communication methods before, during or after the study period, but subjective experience suggests that all methods were used throughout the study depending on the clinical context.
Intervention
During the study, staff accessed wireless e-mail using BlackBerry 7,290 handheld devices using cellular phone frequencies (Global System for Mobile Communications [GSM] 850/1900 MHz) with maximum power output of 2 W at 850 MHz and 1 W at 1,900 MHz. This wireless device uses push technology to send e-mails without delay to the recipient's device, eliminating the need for users to log into an account to check for new messages. In this study, device vibration alerted users to the receipt of a new message. Messages could be sent to one or multiple recipients. A server encrypted all messages to ensure secure message transmission and compliance with provincial and national privacy regulations. All devices were password-protected, with a 1-hour time-out period, and stored data could be remotely erased from any device by an administrator in the event of loss. Because of these security measures, there were no restrictions on the inclusion of personal health information in messages. We did not use other device functionality such as voice or calendar capabilities.
We used wireless e-mail as our method for real-time push text communication for the following reasons: (1) security (as discussed above), (2) form factor: the selected devices had a full character keyboard that facilitated text entry, and (3) integration with hospital e-mail system: e-mails created with the wireless device were also stored on the hospital e-mail server. In contrast, other methods of text communication, such as text messaging from mobile phones (short message service, or SMS), are limited by lack of encryption, slow message creation using numeric key pads, and lack of integration with the hospital e-mail system.
Devices were assigned to specific roles or to individual ICU leadership staff. The former category comprised 28 devices, distributed to bedside nurses (up to 19/daytime shift), the charge nurse (n = 1), respiratory therapists (n = 2), social worker (n = 1), pharmacists (n = 2), and unit clerks (n = 3). These users received a specific device at the beginning of the shift and returned it at the end of the shift. Six devices were assigned to leadership staff members, who retained the same device for the entire study period. This category included clinical educators (n = 2), clinical leaders (n = 2), ICU nursing director (n = 1), and ICU administrative assistant (n = 1). Intensivists (n = 4) supplied their own personal devices and cellular network access during the study period. They could send orders to specific nurses by wireless e-mail, which were transcribed into the hospital's paper chart.
Implementation
Prior to the study, we created an implementation group with 15 members representing all user types. The group met 4 times over 3 months before device deployment and developed policies regarding device use, message content, device security and implementation.
We introduced wireless e-mail into the ICU on Aug 1, 2005 for a 6-month study period. Implementation group members provided device training to ICU staff on an as-needed basis. Devices were used during the day 7:30 am to 7:30 pm shift only and charged at night.
Device Usage
We recorded the number of e-mail messages transmitted and received during approximately 5 months of the 6-month study period by reviewing the secure e-mail account associated with each role-specific device. We also recorded e-mail volume during a subsequent 5-month nonstudy period (Jan 6, 2007–Jun 6, 2007). Specific times that messages were received and opened by the recipient were not available from the wireless service provider or the local wireless e-mail server.
Questionnaire Development
We developed the questionnaire (see Appendix, available as an online data supplement at http://www.jamia.org) using standard survey methodology. 42,43 We first generated survey items by searching MEDLINE (1966 to second week October 2005) for papers on wireless communication in the hospital (search terms included e-mail, wireless e-mail, BlackBerry, communication) and by conducting semi-structured interviews with 12 ICU staff (nursing, ICU leadership, pharmacy and respiratory therapy) and 4 ICU physicians. We developed content areas of interest (domains) and specific questions (items) within domains. Questions contained stems with ordinal response frames using 7-point Likert scales, with 7 indicating the highest level of agreement or most favorable response, 1 indicating the least favorable response, and 4 indicating a neutral response. Three intensivists with methodology training (NA, JF, DS) reviewed the instrument for redundant items, face and content validity, comprehensiveness, and clarity. A focus group of 17 ICU staff led by the hospital patient safety director provided a similar review. We then pretested the penultimate version using 11 members of the implementation group and 18 attendees at an interdisciplinary staff meeting. Finally, we assessed clinical sensibility of the final draft by administering it to 5 ICU staff and obtaining feedback using a 6-question instrument. The final questionnaire comprised 49 questions.
Questionnaire Administration
A unit clerk administered the questionnaire to ICU staff, tracked respondents, and collected completed forms over a 5-week period (Dec 22, 2005–Jan 27, 2006). Completion of the questionnaire was voluntary, and all responses were confidential. We provided an incentive (Can $2 gift certificate for coffee) for questionnaire completion. The hospital research ethics board approved the study.
Data Analysis
We present e-mail usage data as the mean (standard deviation, SD) number of messages transmitted and received daily and survey responses as median (interquartile range, IQR) scores on 7-point ordinal Likert scales, unless otherwise stated. We used t tests to examine for differences in the number of e-mail messages sent and received during and after the study period. For each survey question, we used the sign test to test the null hypothesis that the median response equals 4, the neutral position on the Likert scale. All p values are two-sided. We also collapsed items on the Likert scales into categories representing favorable (Likert = 5,6,7) versus unfavorable (including neutral) responses (Likert ≤ 4). Graphical representations of our results were constructed. The small number of nonnursing respondents precluded reliable comparison of results among healthcare disciplines. Calculations were carried out using SAS 8.0 (Cary, NC).
Role of the Funding Sources
Research in Motion (RIM, Waterloo, ON) provided devices for the study on an unrestricted basis. Rogers Wireless (Toronto, ON) provided unlimited data communication over a local GSM cellular network on an unrestricted basis. After the study period, the hospital provided operational funds for ongoing wireless e-mail usage, but did not have to pay for the devices. The funding sources had no role in the conception, design, or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Results
Respondents
Most (106/125 [85%]) ICU staff members who used the devices during the study period completed the questionnaire; all available responses were analyzed. Respondents included physicians (n = 4), nurses (n = 66), ICU leaders (n = 4), RTs (n = 18), pharmacists (n = 2), social workers (n = 1), and unit clerks (n = 9). Two respondents did not report their occupation. Respondents had a median age of 37.5 (IQR 33, 43) years, with 11.5 (IQR 5, 16) years of experience. Most respondents used home information technology such as a computer (96%), wireless network (45%), or a laptop computer (44%). Home applications included e-mail (95%), Internet (89%), and word-processing (74%). Prior to the wireless e-mail trial, most respondents reported at least moderate familiarity with computers (62%) but not handheld computing devices (31%).
Wireless E-Mail Use, Usability, and Impact
ICU staff sent 5.2 (1.9) and received 8.9 (2.1) messages (mean [SD]) per day during 5 months of the 6-month study period (▶). In a subsequent 5-month period, the volume of messages sent and received decreased by 35% (p < 0.001) and 12% (p = 0.018), respectively.
Table 1.
Table 1 Wireless E-Mail Device Usage Data
| User Group | Daily Messages Transmitted (Mean (SD)) |
Daily Messages Received (Mean (SD)) |
||||
|---|---|---|---|---|---|---|
| During Study Period | After Study Period | p Value | During Study Period | After Study Period | p Value | |
| All devices (n = 28; n = 29) ∗ | 5.2 (1.9) | 3.4 (1.1) | <0.0001 | 8.9 (2.1) | 7.8 (1.2) | 0.018 |
| Nurses (n = 19) | 5.7 (1.5) | 3.7 (0.7) | <0.0001 | 9.4 (1.4) | 7.7 (0.6) | < 0.0001 |
| Unit coordinators (n = 3) | 5.7 (1.2) | 2.4 (1.6) | 0.046 | 8.9 (1.3) | 6.3 (0.6) | 0.035 |
| Respiratory therapists (n = 2; n = 3) ∗ | 5.0 (0.3) | 2.3 (0.9) | 0.030 | 10.4 (0.3) | 8.3 (2.2) | 0.29 |
| Pharmacists (n = 2) | 4.6 (0.9) | 5.4 (0.1) | 0.34 | 7.5 (0.4) | 10.4 (0.2) | 0.012 |
| Social worker (n = 1) | 1.7 (n/a) | 2.5 (n/a) | n/a | 6.1 (n/a) | 7.0 (n/a) | n/a |
| Dietician (n = 1) | 0.3 (n/a) | 1.8 (n/a) | n/a | 1.2 (n/a) | 6.7 (n/a) | n/a |
∗ There were 3 devices for respiratory therapists after the study period.
Values represent mean (SD) daily messages during 5 months of the 6-month study period (154 d from Aug 29, 2005 to Jan 29, 2006) and after the study period (152 d from Jan 6, 2007 to Jun 6, 2007). Messages could be received from other devices or though the hospital e-mail system from desktop computers located at each patient's bedside. p values comparing during and after study periods are calculated using t tests.
Abbreviations: n/a = not applicable; SD = standard deviation.
Respondents took a median of 2 (IQR 1, 2.5) shifts to become comfortable using the devices, and only 4 (4%) remained uncomfortable at the end of the trial. Overall, respondents had positive perceptions of device usability, impact on ICU communication, team relationships and patient care, personal impact, and overall impact; these perceptions were statistically different from the neutral response (▶, p < 0.001 for all responses; ▶). Staff members reported that the device was easy to use (median Likert 6 [IQR 5, 7]), keep clean (median Likert 4.5 [IQR 4, 6]), and keep in their possession (median Likert 6 [IQR 4, 7]), and that it became more useful as usage increased (median Likert 6 [IQR 5, 7]). Respondents reported sending a median of 5 (IQR 3.5, 10) e-mails per shift, matching the actual usage data. No devices malfunctioned and there were no network outages; however, 1 device used by nursing was lost during the study period. There were no reports of any device-induced radiofrequency interference with medical devices during the trial.
Table 2.
Table 2 Perceptions of Wireless E-Mail Device Usability and Impact (n = 106)
| Survey Question | Response | Favorable Response (Number, %) |
|---|---|---|
| Device usefulness increases with use | 6 (5, 7) | 90 (85%) |
| Device is easy to use | 6 (5, 7) | 94 (89%) |
| Easy to keep track of device | 6 (4, 7) | 71 (67%) |
| Device is easy to keep clean | 4.5 (4, 6) | 59 (56%) |
| I had sufficient training | 5 (4, 6) | 53 (50%) |
| Improved speed of communication | 6 6,7 | 97 (92%) |
| Improved reliability of communication | 6 6,7 | 97 (92%) |
| Less effort required to communicate | 5 (3, 6) | 64 (60%) |
| Improved access to ICU team | 6 (5, 7) | 95 (90%) |
| Improved physician response times to routine issues | 6 (5, 7) | 91 (86%) |
| Improved physician response times to critical issues | 6 (5, 7) | 89 (84%) |
| I am less likely to delay contacting a physician | 6 (4.5, 7) | 78 (74%) |
| Improved nonphysician response times | 6 (5, 7) | 90 (85%) |
| Content of messages is useful | 6 (5, 7) | 93 (88%) |
| I resorted to overhead paging or numerical paging | 1 (1, 3) | 82 (77%) |
| Overall impact of wireless e-mail on communication | 6 (6, 7) | 94 (89%) |
| Improved job satisfaction | 6 (4, 6) | 78 (74%) |
| Improved my communication skills | 6 (5, 6) | 86 (81%) |
| Helped me take better care of my patients | 6 (5, 6) | 82 (77%) |
| Has made me more comfortable with using information technology for patient care | 5 (4, 6) | 65 (61%) |
| Has made my job less frustrating | 6 (4, 6) | 79 (75%) |
| Has a positive effect on team morale | 6 (4, 6) | 71 (67%) |
| Has enabled better coordination of ICU team members | 6 (5, 7) | 93 (88%) |
| Has enabled new ways of ICU team to work together | 6 (5, 6) | 80 (75%) |
| Has enabled greater awareness of ICU activity | 6 (4, 6) | 78 (74%) |
| Improved patient care | 6 (5, 6) | 94 (89%) |
| Improved patient safety | 6 (5, 6) | 80 (75%) |
| Enabled faster care | 6 (5, 7) | 95 (90%) |
| I would like to keep using wireless e-mail in the ICU | 7 (6, 7) | 92 (87%) |
| All physicians should use wireless e-mail | 6 (5, 7) | 90 (85%) |
Legend: Data are presented as median (interquartile range) on a 7-point Likert scale, with 7 indicating the highest degree of agreement or most favorable response, except for “Resorted to overhead paging or numerical paging”, where 7 indicates frequent use of paging. For each question, we calculated a p value (using the sign test) to test the null hypothesis that the median response equals 4, the neutral value on the Likert scale. All p values for these comparisons were < 0.001. A favorable response is defined as a Likert score of 5, 6 or 7, except for “Resorted to overhead paging or numerical paging” where it is defined as a Likert score of 1, 2, or 3.
ICU = intensive care unit.
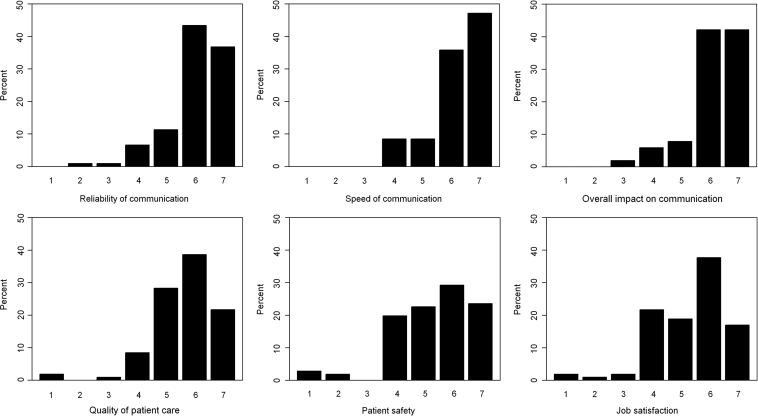
Figure 1.
Responses to selected questions from survey of healthcare workers (n = 106) about impact of wireless e-mail). The Likert scale had 7 points, with 7 indicating the most favorable response.
ICU staff reported a positive overall impact on communication (Likert 6 [IQR 6, 7]). Wireless e-mail was perceived to provide fast (Likert 6 [IQR 6, 7]) and reliable (Likert 6 [IQR 6, 7]) communication with improved physician response times (Likert 6 [IQR 5, 7] for both critical and routine issues) and nonphysician response times (Likert 6 [IQR 5, 7]). The content of wireless e-mail messages were perceived to contain useful content (Likert 6 [IQR 5, 7]), improve access to the ICU team (Likert 6 [IQR 5, 7]), and require less effort to use than alternate methods of communication (Likert 5 [IQR 3, 6]). A majority (n = 86 [81%]) reported experiencing no negative impact from using wireless e-mail. However, a minority (n = 19 [18%]) reported a small to moderate negative impact of wireless e-mail on quality of ICU communication (Likert 4 [IQR 2, 4]). The most frequent negative comments were reduced face-to-face communication among team members or between team members and patients' families (n = 7), and inappropriate use of devices for personal purposes (n = 3).
Respondents reported that wireless e-mail enabled new ways for the ICU team to work together (Likert 6 [IQR 5, 6]) and improved ICU team coordination (Likert 6 [IQR 5, 7]), in addition to improving personal job satisfaction (Likert 6 [IQR 4, 6]) and reducing job frustration (Likert 6 [IQR 4, 6]). The survey did not solicit examples of these improvements. Most respondents (n = 92 [87%]) perceived no negative impact on ICU team relationships, whereas only a minority (n = 13 [12%]) reported a moderate negative impact (Likert 3 [IQR 2.5, 4.5]), with the primary concern being a reduction of face-to-face interactions among team members.
Respondents believed that wireless e-mail improved patient care (Likert 6 [IQR 5, 6]) and patient safety (Likert 6 [IQR 5, 6]) and facilitated faster care (Likert 6 [IQR 5, 7]). Only 4 respondents (4%) reported any negative impact on patient care, describing 3 incidents where responses to messages were not received in a timely manner; no details of these incidents were provided. No specific adverse events as a result these message delays was reported. Most staff members (n = 92 [87%]) wished to continue using wireless e-mail after study completion.
Discussion
Summary of Principal Findings
We implemented wireless e-mail using a local GSM cellular network for interdisciplinary communication in an ICU without dedicated training or project management. Wireless e-mail users perceived a strongly positive impact on ICU communication, including increased speed and reliability of communication, improved message content, and faster response times, leading to more timely and safer patient care. Staff members also reported improved job satisfaction and team relationships. The easy implementation and favorable response to wireless e-mail technology in this ICU are atypical of initial experience with other healthcare information technology, 44,45 and may reflect the high clinical impact of timely communication combined with reliable and user-friendly technology.
Secondary Findings
Although our survey did not solicit examples of improved team collaboration, we anecdotally observed that wireless e-mail facilitated several novel activities. First, overnight charge nurses started to e-mail a summary of overnight nursing issues to the intensivist well before morning rounds, allowing for efficient triage of rounds workflow and organization of diagnostic tests and subspecialty consultations. Second, patient care became less interrupted during staff breaks, since the covering nurse could e-mail the primary nurse on break for patient care issues (for example, to confirm the time of a family meeting). Finally, staff perceived an improvement in overall safety since help could be rapidly summoned to very high-acuity events in the geographically sprawling ICU by e-mail notification (perceived to be less disruptive than overhead paging).
Drawbacks of wireless e-mail were uncommonly reported in this study and appeared relatively modest. The principal concerns related to a decrease in face-to-face clinician communication and inappropriate use of wireless e-mail for personal use. These issues underscore the need for continued face-to-face communication for more complex patient care issues, in addition to education and policy regarding appropriate use of wireless e-mail.
A particular concern about wireless e-mail using cellular frequencies is its potential for radiofrequency interference with medical devices. Our implementation was consistent with the study hospital's policy, which permitted the use of mobile phones and wireless e-mail devices further than 1 m from mechanical ventilators. We observed no episodes of radiofrequency interference in our 6-month trial, consistent with other reports of the safety of cellular communication devices in patient care environments, 46 including sensitive environments such as the operating room and ICU. 47 Our approach was consistent with a review recommending that hospitals balance the need to avoid electromagnetic interference with promotion of mobile communication technology used by healthcare workers to provide patient care. 48
Strengths and Weaknesses of This Study
Several aspects of our study enhance its internal validity. We developed our survey instrument using an accepted sequential approach including item generation and reduction, pretesting, and assessment of clinical sensibility, administered it to the entire eligible population, and achieved a very high response rate that exceeded the norm for healthcare provider surveys. 49 Our results are likely to be generalizable to other settings with large interdisciplinary healthcare teams. We did not purchase the devices for the study and did not perform a formal cost analysis. Nevertheless, we implemented wireless e-mail using local resources with no dedicated project management or training. The use of a local cellular GSM network eliminated the need for additional telecommunications infrastructure. In our ICU, we estimate the annual cost of wireless e-mail operations to be approximately Can$17,000, less than 0.2% of the ICU annual operating budget (Can$16 million).
A limitation of this study, common to all surveys, is that the responses reflect the subjective experiences of respondents rather than actual outcomes. We did not define any terms used in the survey; however, we attempted to clarify the meaning of summary questions about a domain (“Overall impact on communication”) with more specific questions about perceived impacts within a domain (“Improved speed of communication”). We are not aware of any validated survey tool to assess communication among members of healthcare teams. The subjective nature of our outcomes data makes our study hypothesis-generating and not definitive proof of actual benefit.
We did not directly measure the impact of wireless e-mail on ICU communication processes, such as message content or response times, missed or neglected messages, or on actual patient outcomes. Our subjective impression was that most messages were relatively brief (fewer than 50 words) and related to common issues in patient management such as low urine output, high blood pressure, and arranging of family meetings. Similarly, we did not assess the specific impact of wireless e-mail on other types of communication used in the ICU. Subjectively, we observed that wireless e-mail replaced the use of overhead and receive-only numeric paging. More routine patient care issues were addressed by wireless e-mail communications, allowing face-to-face interdisciplinary bedside rounds to focus on the more complex aspects of patient care. Comparing actual response times to messages sent using wireless e-mail to response times using traditional methods of communication could be an area of future research.
Our evaluation may overstate the potential benefits of wireless e-mail, given that we were responsible both for implementation and evaluation; the association of successful information technology applications with developer-led evaluation has been reported for clinical decision support systems. 50 Usage data showed that the number of messages transmitted and received decreased after the study period. This finding may reflect exaggerated usage during the study period (“Hawthorne effect”) or initial enthusiasm for a technology followed by a more tempered attitude as familiarity increased. We do not have more recent usage data, although the hospital budget continues to cover wireless device cellular charges, and the use of these devices has been extended to another medical ward.
Our findings may not be reproduced in other institutions because of the influence of technical and social environments on the uptake of any new technology. 51 Finally, we conducted no formal screen for episodes of radiofrequency interference. Although such episodes may have been underreported, it is highly unlikely that a clinically important event would have been undetected.
Future Research
Given the potential impact to improve patient safety by optimizing communication among members of healthcare teams, there are many opportunities for additional research. This study is limited to one community hospital; the effects of wireless e-mail on interdisciplinary communication should be studied in other academic and community hospital settings. The perceived positive impacts of our intervention may differ among healthcare disciplines, and could be reliably explored in a larger multicenter investigation. Other important and currently unaddressed issues include the effect of wireless e-mail and other communication methods on (1) healthcare worker efficiency, such as frequency and duration of interruptions during direct patient care, (2) timeliness and quality of clinical response to important patient care issues, (3) incidence of potentially unsafe verbal ordering practices, and (4) satisfaction of patients and their families. In addition, the optimal structure and content of written messages has received attention in care handoff situations 52,53 but remains to be defined for routine clinical care.
Conclusions
Interdisciplinary ICU team members using wireless e-mail over a 6-month period reported improved clinical communication compared to baseline communication methods that included numeric paging, overhead paging, physical searches for staff, handwritten messages, and desktop-based e-mail. They also perceived improvements in patient care, team relationships and staff satisfaction, without major safety concerns. Ease of implementation and high clinical impact make wireless e-mail an attractive tool for improving communication in other healthcare settings. More research is needed to assess the effects of wireless e-mail communication, compared to traditional communication methods, on clinically important outcomes.
Acknowledgments
The authors thank Karen Beardall for her invaluable help in distributing and collecting the survey and Ruxandra Pinto for conducting some of the statistical analyses.
Footnotes
Competing interests: Research In Motion (RIM, Waterloo, ON) provided devices for the study on an unrestricted basis. Rogers Wireless (Toronto, ON) provided unlimited data communication over a local GSM cellular network on an unrestricted basis. The funding sources had no role in the conception, design, or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. Chris O'Connor, Jan O. Friedrich, Damon C. Scales, and Neill K.J. Adhikari have no financial or other conflicts of interest relevant to the content of this manuscript to disclose.
References
- 1.Coiera E. Communication system basicsIn: Coiera E, editor. Guide to health informatics. 2nd edition. New York: Oxford University Press; 2003. pp. 231-243.
- 2.Alvarez G, Coiera E. Interdisciplinary communication: An uncharted source of medical error? J Crit Care 2006;21(3):236-242Discussion: 242. [DOI] [PubMed] [Google Scholar]
- 3.Coiera E, Tombs V. Communication behaviours in a hospital setting: An observational study BMJ 1998;316(7132):673-676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams RG, Silverman R, Schwind C, et al. Surgeon information transfer and communication: Factors affecting quality and efficiency of inpatient care Ann Surg 2007;245(2):159-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhasale AL, Miller GC, Reid SE, Britt HC. Analysing potential harm in Australian general practice: An incident-monitoring study Med J Aust 1998;169(2):73-76. [DOI] [PubMed] [Google Scholar]
- 6.Wilson RM, Runciman WB, Gibberd RW, et al. The quality in Australian Health Care Study Med J Aust 1995;163(9):458-471. [DOI] [PubMed] [Google Scholar]
- 7.Donchin Y, Gopher D, Olin M, et al. A look into the nature and causes of human errors in the intensive care unit Crit Care Med 1995;23(2):294-300. [DOI] [PubMed] [Google Scholar]
- 8.Rothschild JM, Landrigan CP, Cronin JW, et al. The Critical Care Safety Study. The incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med 2005;33(8):1694-1700. [DOI] [PubMed] [Google Scholar]
- 9.Needham DM, Sinopoli DJ, Thompson DA, et al. A system factors analysis of “line, tube, and drain” incidents in the intensive care unit Crit Care Med 2005;33(8):1701-1707. [DOI] [PubMed] [Google Scholar]
- 10.Nast PA, Avidan M, Harris CB, et al. Reporting and classification of patient safety events in a cardiothoracic intensive care unit and cardiothoracic postoperative care unit J Thorac Cardiovasc Surg 2005;130(4):1137. [DOI] [PubMed] [Google Scholar]
- 11.McKnight L, Stetson PD, Bakken S, Curran C, Cimino JJ. Perceived information needs and communication difficulties of inpatient physicians and nurses Proc AMIA Symp 2001:453-457. [PMC free article] [PubMed]
- 12.Alvarez G, Coiera E. Interruptive communication patterns in the intensive care unit ward round Int J Med Inf 2005;74(10):791-796. [DOI] [PubMed] [Google Scholar]
- 13.Harvey R, Jarrett PG, Peltekian KM. Patterns of paging medical interns during night calls at two teaching hospitals CMAJ 1994;151(3):307-311. [PMC free article] [PubMed] [Google Scholar]
- 14.Katz MH, Schroeder SA. The sounds of the hospital. Paging patterns in three teaching hospitals. N Engl J Med 1988;319(24):1585-1589. [DOI] [PubMed] [Google Scholar]
- 15.Blum NJ, Lieu TA. Interrupted care. The effects of paging on pediatric resident activities. Am J Dis Child 1992;146(7):806-808. [DOI] [PubMed] [Google Scholar]
- 16.Major K, Shabot MM, Cunneen S. Wireless clinical alerts and patient outcomes in the surgical intensive care unit Am Surg 2002;68(12):1057-1060. [PubMed] [Google Scholar]
- 17.Reddy MC, McDonald DW, Pratt W, Shabot MM. Technology, work, and information flows: Lessons from the implementation of a wireless alert pager system J Biomed Inform 2005;38(3):229-238. [DOI] [PubMed] [Google Scholar]
- 18.Reddy MC, Pratt W, McDonald DW, Shabot MM. Challenges to physicians' use of a wireless alert pager AMIA Annu Symp Proc 2003;544:548. [PMC free article] [PubMed] [Google Scholar]
- 19.Poon EG, Kuperman GJ, Fiskio J, Bates DW. Real-time notification of laboratory data requested by users through alphanumeric pagers J Am Med Inform Assoc 2002;9(3):217-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oguz KK, Yousem DM, Deluca T, Herskovits EH, Beauchamp Jr NJ. Impact of pager notification on report verification times Acad Radiol 2002;9(8):954-959. [DOI] [PubMed] [Google Scholar]
- 21.Etchells E, Adhikari NK, Cheung CM, et al. Effect of an automated paging system on response to critical laboratory values J Gen Intern Med 2007;22(Suppl 1):124. [Google Scholar]
- 22.Nguyen TC, Battat A, Longhurst C, Peng PD, Curet MJ. Alphanumeric paging in an academic hospital setting Am J Surg 2006;191(4):561-565. [DOI] [PubMed] [Google Scholar]
- 23.Ruskin KJ. Communication devices in the operating room Curr Opin Anæsthesiol 2006;19(6):655-659. [DOI] [PubMed] [Google Scholar]
- 24.Budd C. Using a BlackBerry to support clinical practice CIN Comput Inform Nurs 2007;25(5):263-265. [DOI] [PubMed] [Google Scholar]
- 25.Leape LL, Cullen DJ, Clapp, MD, et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit JAMA 1999;282(3):267-270. [DOI] [PubMed] [Google Scholar]
- 26.Randolph AG, Pronovost P. Reorganizing the delivery of intensive care could improve efficiency and save lives J Eval Clin Pract 2002;8(1):1-8. [DOI] [PubMed] [Google Scholar]
- 27.Durbin CG. Team model: Advocating for the optimal method of care delivery in the intensive care unit Crit Care Med 2005;34(3 Suppl)S12–7. [DOI] [PubMed]
- 28.Dutton RP, Cooper C, Jones A, et al. Daily multidisciplinary rounds shorten length of stay for trauma patients J Trauma 2003;55(5):913-919. [DOI] [PubMed] [Google Scholar]
- 29.Dodek PM, Raboud J. Explicit approach to rounds in an ICU improves communication and satisfaction of providers Intensive Care Med 2003;29(9):1584-1588. [DOI] [PubMed] [Google Scholar]
- 30.McFetridge B, Gillespie M, Goode D, Melby V. An exploration of the handover process of critically ill patients between nursing staff from the emergency department and the intensive care unit Nurs Crit Care 2007;12(6):261-269. [DOI] [PubMed] [Google Scholar]
- 31.Coiera EW, Jayasuriya RA, Hardy J, Bannan A, Thorpe ME. Communication loads on clinical staff in the emergency department Med J Aust 2002;176(9):415-418. [DOI] [PubMed] [Google Scholar]
- 32.O'Leary KJ, Liebovitz DM, Baker DW. How hospitalists spend their time: Insights on efficiency and safety J Hosp Med 2006;1(2):88-93. [DOI] [PubMed] [Google Scholar]
- 33.Chiu T, Old A, Naden G, Child S. Frequency of calls to “on-call” house officer pagers at Auckland City Hospital, New Zealand N Z Med J 2006;119(1231):U1913. [PubMed] [Google Scholar]
- 34.Lingard L, Espin S, Whyte S, et al. Communication failures in the operating room: An observational classification of recurrent types and effects Qual Saf Health Care 2004;13(5):330-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gurses AP, Xiao Y. A systematic review of the literature on multidisciplinary rounds to design information technology J Am Med Inform Assoc 2006;13(3):267-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martins HMG, Jones MR. What's so different about mobile information communication technologies (MICTs) for clinical work practices?. A review of selected pilot studies. Health Informatics J 2005;11(2):123-134. [Google Scholar]
- 37.Farman AG. Image communication: Mailed, wired, and wireless Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103(5):585-586. [DOI] [PubMed] [Google Scholar]
- 38.Yaghmai V, Salehi SA, Kuppuswami S, Berlin JW. Rapid wireless transmission of head CT images to a personal digital assistant for remote consultation Acad Radiol 2004;11(11):1291-1293. [DOI] [PubMed] [Google Scholar]
- 39.Garrett BM, Jackson C. A mobile clinical e-portfolio for nursing and medical students, using wireless personal digital assistants (PDAs) Nurse Educ Today 2006;26(8):647-654. [DOI] [PubMed] [Google Scholar]
- 40.Banitsas K, Georgiadis P, Tachakra S, Cavouras D. Mobile consultant: Evaluation of additional services Conf Proc IEEE Eng Med Biol Soc 2007:3709-3712. [DOI] [PubMed]
- 41.Volpp KG, Grande D. Residents' suggestions for reducing errors in teaching hospitals N Engl J Med 2003;348(9):851-855. [DOI] [PubMed] [Google Scholar]
- 42.Aday LA. Designing and Conducting Health Surveys: A Comprehensive Guide2nd edn. San Francisco: Jossey-Bass Publishers; 1996.
- 43.Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians CMAJ 2008;179(3):245-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ash JS, Gorman PN, Seshadri V, Hersh WR. Computerized physician order entry in US hospitals: Results of a 2002 survey J Am Med Inform Assoc 2004;11(2):95-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Valdes I, Kibbe DC, Tolleson G, Kunik ME, Petersen LA. Barriers to proliferation of electronic medical records Inform Prim Care 2004;12(1):3-9. [DOI] [PubMed] [Google Scholar]
- 46.Cohen T, Ellis WS, Morrissey JJ, et al. Safe use of cellular telephones in hospitals: Fundamental principles and case studies J Healthc Inf Manag 2005;19(4):38-48. [PubMed] [Google Scholar]
- 47.Soto RG, Chu LF, Goldman JM, Rampil IJ, Ruskin KJ. Communication in critical care environments: Mobile telephones improve patient care Anesth Analg 2006;102(2):535-541. [DOI] [PubMed] [Google Scholar]
- 48.Lapinsky SE, Easty AC. Electromagnetic interference in critical care J Crit Care 2006;21(3):267-270. [DOI] [PubMed] [Google Scholar]
- 49.Cummings SM, Savitz LA, Konrad TR. Reported response rates to mailed physician questionnaires Health Serv Res 2001;35(6):1347-1355. [PMC free article] [PubMed] [Google Scholar]
- 50.Garg AX, Adhikari NK, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: A systematic review JAMA 2005;293(10):1223-1238. [DOI] [PubMed] [Google Scholar]
- 51.Coiera E. When conversation is better than computation J Am Med Inform Assoc 2000;7(3):277-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gandhi TK. Fumbled handoffs: One dropped ball after another Ann Intern Med 2005;142(5):352-358. [DOI] [PubMed] [Google Scholar]
- 53.Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: Implications for patient safety and continuity of care J Am Med Assoc 2007;297(8):831-841. [DOI] [PubMed] [Google Scholar]