Abstract
The treatment of residual deformity following surgery for developmental dysplasia of the hip remains controversial. The rationale for the use of the rotational acetabular osteotomy (RAO) is that it increases the weight-bearing area by shifting the osteotomized acetabulum to cover the femoral head. This can improve joint function as well as achieve relief of pain. However, it is unclear if this osteotomy can improve a compromised hip when performed for the treatment of residual deformity and acetabular dysplasia after surgery for developmental dysplasia of the hip. We aimed to report the clinical outcome as assessed by need for total hip arthroplasty (THA) and by the Merle d’Aubigné and Postel scores. In addition, we tried to assess the radiographic outcomes as assessed by Tönnis’s classification. Only two hips required THA, which was performed in two patients at 11 and 12 years after RAO, respectively. The mean Merle d’Aubigné clinical score improved from 14.1 ± 2.3 points (range, 10 to 17) preoperatively to 15.8 ± 2.9 points (8 to 18) at final follow-up (p < 0.02). Radiological assessment at final follow-up showed the obvious progression of osteoarthritis in five hips. One patient in grade 1 preoperatively progressed into grade 3 at final follow-up; four patients in grade 2 preoperatively progressed into grade 3. In our study, this osteotomy prolonged the functional life of the hip, and only two hips needed THA after a mean follow-up of 11 years. We found that advanced arthritis pre-osteotomy is associated with progression of radiologic changes
Keywords: rotational acetabular osteotomy, residual deformity after surgery for developmental dysplasia of the hip
Introduction
Coexistence of femoral head deformity and acetabular dysplasia predisposes the hip joint to arthritis. In many patients with this condition, osteoarthritis of the hip joint shows a progressive course. It is essential to prevent the progression of osteoarthritic changes in such patients by joint-preserving surgery. Total hip arthroplasty (THA) is very effective for the treatment of advanced osteoarthritis of the hip joint, but there is a serious concern with regard to limited durability of the prosthesis in younger patients. The optimal treatment still needs to be determined when residual deformity including subluxation and acetabular dysplasia remains after surgery. Joint-preserving procedures which address residual deformity include femoral osteotomy [1], arthrodesis [2], and acetabular osteotomy [3]. Rotational acetabular osteotomy (RAO) has also been performed in patients with developmental dysplasia of the hip before the onset of osteoarthritic changes or in those with early osteoarthritis [4]. However, it is unclear if RAO can improve a compromised hip when performed for the treatment of residual deformity and acetabular dysplasia after surgery for developmental dysplasia of the hip (DDH). We performed RAO to treat residual deformity of dysplastic hips. We aimed to improve joint function as well as achieve pain relief by increasing the weight-bearing area by shifting the osteotomized acetabulum and improving the coverage of the femoral head. In this study, we aimed to report the clinical outcome as assessed by the Merle d’Aubigné and Postel score [5] and need for THA. Secondarily, we tried to assess the radiographic outcomes as assessed by Tönnis’s classification [6].
Patients and methods
Between August 1986 and July 2005, we performed rotational acetabular osteotomy according to the method of Ninomiya and Tagawa [6] in 351 patients (420 hips). Within this group, 25 patients (27 hips) had previously undergone surgical treatment for DDH. These patients constituted the study group for this project.
Assessment of degenerative changes of the hip joint was performed using the radiographic classification of Tönnis [7]. Grade 0 indicates no degenerative changes, despite the presence of acetabular dysplasia and incongruity of the hip. Grade 1 was defined by slight narrowing of the joint space, a widened zone of sclerosis, and minimal growth of osteophytes. In grade 2, moderate joint space narrowing and cystic change of the femoral head and/or the acetabulum were observed. Grade 3 indicated the presence of large cysts and severe narrowing or obliteration of the joint space. At the time of operation, ten hips were grade 0, eight hips were grade 1, and nine hips were grade 2 (Table 1).
Table 1.
Radiographic classification according to Tönnis
| Pre op | At final follow-up | |
|---|---|---|
| Grade 0 | 10 | 10 |
| Grade 1 | 8 | 7 |
| Grade 2 | 9 | 5 |
| Grade 3 | 0 | 5 |
There were 23 women and two men, and their mean age at the time of surgery was 26.8 years (range, 14 to 48 years). The mean follow-up period was 131.7 months (range, 37 to 241 months). Six patients had unilateral dysplasia, and 19 patients had bilateral dysplasia. As original treatment for DDH earlier in their childhood, open reduction (OR) only had been performed in four hips. Open reduction plus the shelf operation (SO) was performed in one hip, open reduction plus femoral osteotomy (FO) in three hips, and OR plus pelvic osteotomy (PO) in two hips. The SO alone had been performed in five hips, and the SO plus FO had been done in one hip. Pelvic osteotomy alone had been performed in three hips, and PO plus FO had been done in one hip. Femoral osteotomy had been performed alone in seven hips (Table 2).
Table 2.
Operations for DDH
| Operation | Hips |
|---|---|
| OR | 4 |
| OR+SO | 1 |
| OR+FO | 3 |
| OR+PO | 2 |
| SO | 5 |
| SO+FO | 1 |
| PO | 3 |
| PO+FO | 1 |
| FO | 7 |
OR open reduction, SO shelf operation, FO femoral osteotomy, PO pelvic osteotomy
Radiological evaluation was performed by two coauthors (M.N. and K.M.). To compare coverage of the femoral head by the acetabulum before and after this secondary acetabular rotational osteotomy, we measured the center-edge (CE) angle of Wiberg [8] and calculated the acetabular head quotient (AHQ) of Heyman and Herndon [9]. To assess osteoarthritic changes, the width of the joint space at the weight-bearing region was measured before surgery and at latest follow-up. Measurement was done at the lateral border, medial border, and center of the weight-bearing region, and the average value was calculated. To assess medialization of the femoral head, the postoperative change of the distance between the symphysis pubis and the medial border of the femoral head was measured. To assess distal translation of the femoral head, the distance between the lower margin of the lateral part of the pubis and the femoral head–neck junction was compared before and after surgery (Fig. 1). The inclusion criteria for this study were an age younger than 50 years and improvement of femoral head coverage, joint congruency, and widening of the joint space on preoperative anteroposterior (AP) plain radiographs with the hip in abduction among grade 0, grade 1, and grade 2 according to Tönnis’s classification. Clinically, all patients included in this series had complained of continuous hip pain. Hips with Tönnis grade 3 changes were not indicated for rotation acetabular osteotomy.
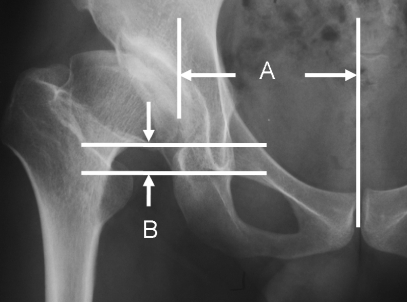
Fig. 1.
Diagram showing measurements of medial and distal displacement of the femoral head. A The distance between the symphysis pubis and the medial border of the femoral head. B The distance between the lower margin of the pubis at its lateral end and the head–neck junction
RAO was performed according to the method of Ninomiya and Tagawa [6]. An anterior curved incision was made from just below the iliac crest towards the distal aspect of the greater trochanter and the hip exposed anteriorly and posteriorly. In order to approach the superior aspect of the acetabulum, a limited detachment of gluteus medius and the tensor fascia lata from the ilium was performed. The base of the pubic bone was exposed between the anterosuperior and anteroinferior iliac spines, taking care to avoid injury to the lateral femoral cutaneous nerve. After dissection of the tensor fascia lata, separation of the posterior border of gluteus medius from the anterior border of gluteus maximus, and detachment of the short external rotators (except for quadratus femoris in order to prevent injury to the blood supply to the femoral head), exposure of the posterior portion of the acetabulum was completed. The osteotomy line was marked about 1 to 1.5 cm from the acetabular rim, and a straight osteotome was inserted into the bone to a depth of about 1.5 cm. Then a curved osteotome was used to complete the osteotomy through the inner wall of the ilium. After this was done, adequate coverage of the femoral head could be achieved by moving the acetabulum inferiorly and laterally. Capsulotomy was not performed. We inserted two to three cortical bone struts (about 5 mm thick) into the space between the rotated acetabulum and the ilium, and we supplemented these grafts with cancellous bone chips and sometimes added hydroxyapatite-tricalcium phosphate composite [4, 10]. Two Kirchner wires (2 mm in diameter) or absorbable polylactic acid screws (4.2 mm in diameter) were used to fix the rotated acetabulum and the cortical bone grafts to the ilium.
Isometric exercises of quadriceps femoris were performed during the first 2 weeks after surgery. The patients were kept at bed rest for first 2 weeks. Transfer to a wheelchair was commenced at 2 weeks postoperatively, and non-weight-bearing walking on two crutches was begun at 3 weeks. Partial weight bearing was permitted after 2 months, while full weight bearing was resumed from 4 to 6 months after surgery [4].
At regular intervals with the minimum follow-up time of 1 year, patient symptoms and the findings on plain anteroposterior radiographs were recorded. Clinical data were obtained by interview and physical examination. The Hip Joint Scoring System of Merle d’Aubigné and Postel [5] was used to grade function preoperatively and at the latest follow-up (Table 3). A score of 18 points is considered excellent, 15 to 17 is good, 13 to 14 is fair, and less than 13 means a poor result.
Table 3.
Merle d’Aubigné score
| Pain | Mobility | Ability to walk | |
|---|---|---|---|
| 0 | Intense and permanent | Ankylosis with bad position of the hip | None |
| 1 | Severe even at night | No movement; pain or slight deformity | With crutches/walking device only |
| 2 | Severe when walking; prevents any activity | Flexion under 40° | With canes only |
| 3 | Tolerable with limited activity | Flexion between 40° and 60° | With one cane, less than 1 hr; very difficult without cane and with a limp |
| 4 | Mild when walking; it disappears in rest | Flexion between 60° and 80°; patients can reach his foot | A long time with a cane; short time without a cane and with a limp |
| 5 | Mild and inconstant; normal activity | Flexion between 80 and 90°; abduction of at least 15° | Without cane but with a slight limp |
| 6 | None | Flexion more than 90°; abduction to 30° | Normal |
Preoperative and follow-up clinical hip scores and the radiographic parameters of acetabular position were compared by using the paired t test. Significance was defined as a p value <0.05.
Results
No intraoperative or postoperative complications were observed, including perforation of the joint by the chisel, infection, avascular necrosis of the rotated acetabulum, or delayed union at the osteotomy site. Heterotopic ossification also did not occur.
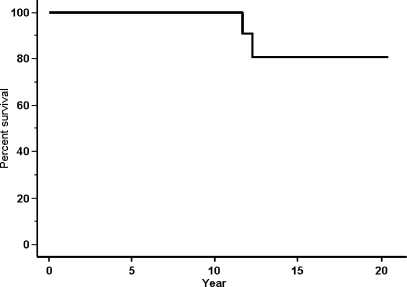
The mean Merle d’Aubigné clinical score improved from 14.1 ± 2.3 points (range, 10 to 17) preoperatively to 15.8 ± 2.9 points (8 to 18) at final follow-up (p < 0.02) mainly because of an improved score for pain. The mean pain score improved significantly from 3.9 ± 1.0 points (2 to 5) to 5.3 ± 1.1 points (2 to 6; p < 0.000009). Although the mean mobility score decreased slightly from 5.5 ± 0.9 points (3 to 6) to 5.2 ± 1.0 points (3 to 6; p = 0.25), the mean walking ability score increased slightly from 4.7 ± 1.1 points (2 to 6) to 5.1 ± 1.1 points (3 to 6; p = 0.18). The total score decreased in only three patients (three hips), declining from a mean of 14.6 points (12 to 16) to a mean of 10.0 points (8 to 15). The postoperative score was ≧15 points for 19 hips and ≧17 points for 15 hips, while it was <15 points for eight hips. At final follow-up, 25 of the 27 hips were still functioning, and only two hips had required THA, which was performed in two patients at 11 and 12 years after RAO, respectively (Fig. 2).
Fig. 2.
Kaplan–Meier survivor curve with total hip arthroplasty as end point
Radiological assessment at final follow-up showed the obvious progression of osteoarthritis in five hips, as reflected by narrowing of the joint space and enlargement of osteophytes or cysts. One patient in grade 1 according to classification of Tönnis preoperatively progressed into grade 3 at final follow-up; four patients in grade 2 preoperatively progressed into grade 3 (Table 2). In the remaining 22 hips, the width of the joint space was preserved. The mean correction of the CE angle achieved by RAO was 36 ± 14° (13° to 58°), with the mean angle being −1 ± 13.1° (−32° to 25°) preoperatively and 36 ± 12.1° (13° to 58°) postoperatively. The mean correction of the AHQ by RAO was 34 ± 13% (9% to 67%), with a mean value of 52 ± 12.4% (20% to 75%) preoperatively and 86 ± 12.2% (61% to 110%) postoperatively. The mean joint space width was 3.4 ± 1.5 mm (1 to 7.0 mm) preoperatively, and this decreased slightly to 2.8 ± 1.2 mm (0.5 to 5.0 mm) at the time of final follow-up (p = 0.11). The joint space was narrower after surgery in both hips that required THA. As for medialization of the femoral head, the mean change was 1.3 ± 5 mm (−7 to 15 mm). Seven hips showed medialization, and six hips showed lateralization. The mean change in the distance between the inferior margin of the lateral part of the pubis and the femoral head–neck junction after surgery was 5.6 mm (−3 to 25 mm), with the mean preoperative distance being 9.0 ± 6.2 mm (0 to 23 mm) and the mean postoperative distance being 3.4 ± 6.7 mm (−10 to 15 mm; p < 0.002). The preoperative distance was ≧20 mm in two hips and ≧10 mm in ten hips, while the postoperative distance was ≧10 mm in six hips (≧20 mm in none). Caudal shift was noted in 15 hips.
In the patients who required THA, surgery was uneventful with no need for acetabular reconstruction, and there was no loosening of the acetabular component at latest follow-up. In these two patients, symptoms particularly in pain and range of motion had worsened as well as remarkable progression of radiographic findings at the time of revision surgery.
Discussion
We performed rotational acetabular soteotomy in patients with residual deformity from hip dysplasia in spite of prior surgical intervention. Our aim was to improve joint function as well as achieve relief of pain by redistributing the weight-bearing force by rotating the osteotomized acetabulum over the femoral head (Figs. 3, 4, 5, and 6). Additionally, we hoped to observe that the progression of arthritic changes in these compromised hips might be prevented or delayed by RAO.
Fig. 3.
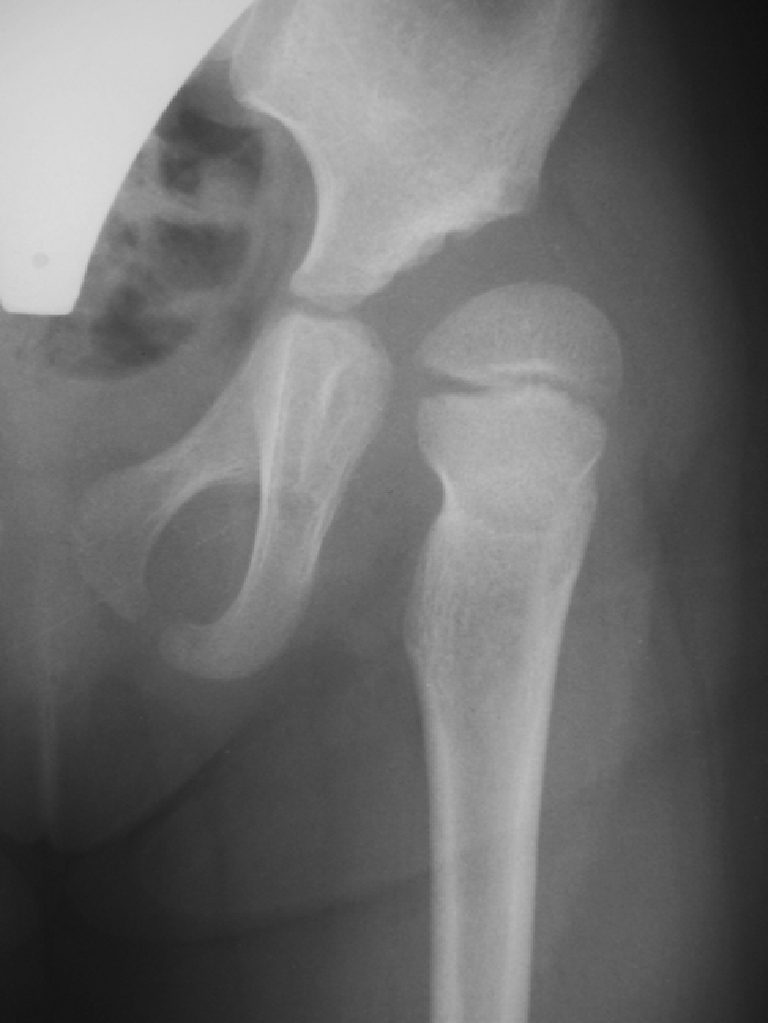
Radiograph of a 10-year-old girl with acetabular dysplasia shows subluxation of the femoral head and severe anterior torsion of the femoral neck. She had undergone open reduction of the left hip joint at the age of 1 year
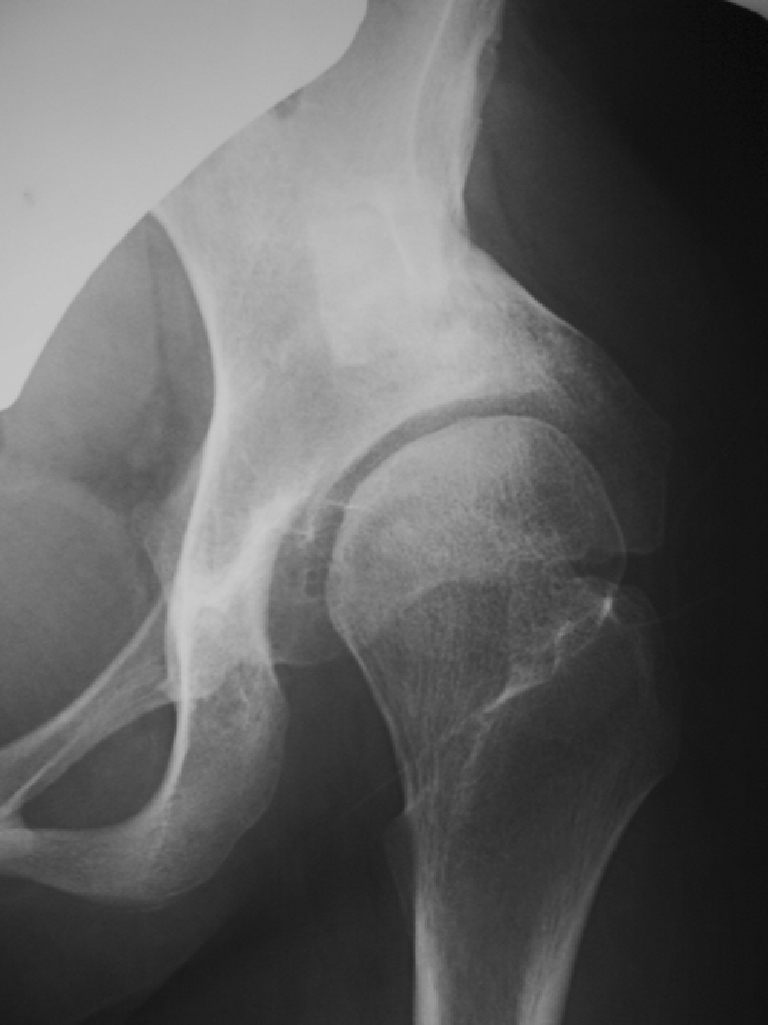
Fig. 4.

Radiograph of a patient at an age of 17 years shows progression of osteoarthritic changes and severe acetabular dysplasia associated with subluxation of the femoral head
Fig. 5.

The osteotomized acetabulum covers the femoral head adequately immediately after surgery
Fig. 6.
Remodeling of the hip joint has continued, and the joint space is wider at 2 years after surgery than in the early postoperative period
There are some limitations and weakness of our study. We were unable to perform an evaluation for the shape of the femoral head and could not reliably judge preoperative joint congruence in abduction. The series also comprised a relatively small number of patients. Nonetheless, this series of patients suggests that RAO can delay the progression of osteoarthritis in dysplastic hips for up to 10 years.
In our study, arthritic changes progressed in nine hips (33%), which included four hips with insignificant changes. Among these nine hips, three presented with advanced degenerative changes on pre-op X-rays, while coverage of the femoral head that achieved rotational osteotomy was considered deficient in two hips. An unexpected shift of the acetabulum occurred postoperatively in one hip, and one patient gained a large amount of weight over time. Hellemondt et al. [11] treated 51 dysplastic hips by triple osteotomy and reported good to excellent results in 64% after a mean follow-up period of 15 years. The variables that predicted a poor long-term outcome in their series were the presence of osteoarthritic changes and a fair to poor clinical score preoperatively. Garras et al. [12] reported that Bernese periacetabular osteotomy provides good symptomatic relief for patients with little to no arthritis (Tönnis type 0 or 1), with an underlying deformity that can be corrected to a position of a stable, congruent hip joint. Similarly, Okano et al. [13] reported that a less spherical femoral head led to progression of osteoarthritis over the long term after RAO in patients with advanced osteoarthritis, and they concluded that postoperative results were dependent on the grade of femoral head deformity. In our study, we also found that advanced arthritis pre-osteotomy is associated with progression of radiologic changes but, other factors such as inadequate coverage of the femoral head by the RAO and post-op weight gain may also influence the progression of arthritic changes.
We tried to avoid muscle damage as far as possible, particularly to the abductor muscles. These muscles are sometimes injured by the initial operation during childhood, and we make every effort to avoid additional iatrogenic muscle injury. To facilitate recovery of quadriceps strength, we do not release the origin of rectus femoris when the base of the pubis is explored during surgery.
In this series, RAO prolonged the functional life of the hip, and only two hips needed THA after a mean follow-up of 11 years. Nevertheless, because of the young age of these patients, longer follow-up studies are needed to confirm the efficacy of RAO for delaying progression of osteoarthritic changes when residual deformity persists after early surgical correction of DDH.
In conclusion, in this series of young patients with residual deformity after surgery for congenital dislocation of the hip, RAO provided a satisfactory outcome at a mean of 11 years. THA after RAO was required in only two patients in this series, and we found that osteotomy did not adversely affect the acetabular anatomy or cause technical difficulties that compromised the outcome of total arthroplasty.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participating in the study was obtained.
References
- 1.Ottolenghi CE, Frigerio E (1962) Intertrochanteric osteotomies in osteo-arthritis of the hip: fundamentals, indications, techniques, and results. J Bone Joint Surg [Am] 44-A:855–1030 [PubMed]
- 2.Callaghan JJ, Brand RA, Pedersen DR (1985) Hip artrodesis. A long-term follow-up. J Bone Joint Surg [Am] 67-A:1328–1335 [PubMed]
- 3.Sutherland DH, Greenfield R (1977) Double innominate osteotomy. J Bone Joint Surg [Am] 59-A:1082–1091 [PubMed]
- 4.Nozawa M, Shitoto K, Matsuda K, Maezawa K, Kurosawa H (2002) Rotational acetabular osteotomy for acetabular dysplasia. J Bone Joint Surg [Br] 84-B:59–65 [DOI] [PubMed]
- 5.Merle d’Aubigné R, Postel M (1954) Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg [Am] 36-A:451–475 [PubMed]
- 6.Ninomiya S, Tagawa H (1984) Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg [Am] 66-A:430–4361 [PubMed]
- 7.Tönnis D (1987) Congenital dysplasia and dislocation of the hip in children and adults. Springer, New York, pp 165–171
- 8.Wiberg G (1939) Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand Suppl 83:1–135
- 9.Heyman CH, Herndon CH (1950) Legg–Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg [Am] 32-A:767–778 [PubMed]
- 10.Nozawa M, Shitoto K, Matsuda K, Maezawa K, Ogawa S, Yuasa T, Aritomi K, Kurosawa H (2006) Original methods to move femoral head medially and caudally after rotational acetabular osteotomy: especially to use ceramic spacer. Arch Orthop Trauma Surg 126:421–424 [DOI] [PubMed]
- 11.Hellemondt GG, Sonneveld H, Schreuder MHE, Kooijman MAP, De Kleuver M (2005) Triple osteotomy of the pelvis for acetabular dysplasia. J Bone Joint Surg [Br] 87-B:911–915 [DOI] [PubMed]
- 12.Garras DN, Crowder TT, Olson SA (2007) Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg [Br] 89-B:721–724 [DOI] [PubMed]
- 13.Okano K, Enomoto H, Osaki M, Shindo H (2008) Rotational acetabular osteotomy for advanced osteoarthritis secondary to developmental dysplasia of the hip. J Bone Joint Surg [Br] 90-B:23–26 [DOI] [PubMed]